Abstract
Objectives
This study aims to compare the effectiveness of dry needling (DN) and kinesiotaping (KT) therapies on pain, quality of life, depression, and physical function in the treatment of myofascial pain syndrome (MPS).
Patients and methods
The study included a total of 60 patients (4 males, 56 females; mean age 31.2±9.8 years; range, 18 to 56 years) diagnosed with MPS between January 2014 and June 2014. The patients were randomly divided into two treatment groups: the DN group (n=30) and KT group (n=30). Both groups performed stretching and postural exercises. The scales used for measurements were the Visual Analog Scale (VAS) for pain, a pressure algometer for the pressure-pain threshold, the Short Form-36 (SF-36) for the quality of life, Beck Depression Inventory (BDI) for depression, and the Neck Pain and Disability Scale (NPDS) for physical function. The patients were evaluated by a single assessor three times: pre-treatment, at the end of the treatment, and two months after the treatment.
Results
Both DN and KT provided significant improvements for all baseline measurements (VAS, pressure pain threshold, all subscales of SF-36, BDI, and NPDS scores) at the end of the treatment and two months after the treatment (p<0.05). However, there was no significant difference between the groups in all measurements (p>0.05).
Conclusion
Kinesiotaping is as an effective method as DN in the treatment of MPS. It can be served as a non-invasive alternative to patients with needle phobia.
Keywords: Disability, dry needling, kinesiotaping, myofascial pain syndrome, quality of life
Introduction
Myofascial pain syndrome (MPS) is a common musculoskeletal disease characterized by local hypersensitive areas known as trigger points. Pain, muscular spasm, motion limitation and, rarely, autonomic dysfunction are some of the symptoms of MPS. These symptoms can affect the patients’ mood, quality of life (QoL), and health status.[1] Local pain or referred pain area is related to the trigger points localization and sensitivity. The exact etiology of MPS remains unknown. Therefore, the therapy is mainly based on improving muscle strength, thus providing a good posture and decreasing pain. The mechanism of MPS treatment is to inactivate the trigger points. Conservative treatments of MPS include transcutaneous electrical nerve stimulation, hot packs, ultrasound, laser, exercise, massage, stretching, local injection, dry needling (DN), drugs, acupuncture, and kinesiotaping (KT).
The DN has been used for pain management for almost two centuries in the Western medicine and it is still a widely used treatment method of MPS.[2] The DN is a therapeutic technique in which thin needles are inserted into the muscles/ligaments to reduce pain in neuromusculoskeletal disorders.[3,4] The DN mechanism is to destroy the trigger points mechanically without using any medication and to relieve pain.[3]
Recently, KT has become an increasingly popular treatment technique, particularly in sports injuries and many other musculoskeletal conditions. This method was originally developed by Dr. Kenzo Kase, a certified chiropractor.[5] It is an alternative taping method to the classic taping and, contrary to the classic taping, it does not restrict movement and improves the muscle performance, blood and lymphatic flow with pain relief and improved functional support.[6,7] The activation of skin receptors causes tactile stimulation from the bandage application, increasing the interstitial space.[7] As a result of the gate control mechanism, pain decreases by an increased afferent feedback system in the skin. Although there are many studies about the effect of KT on sports injuries, there is a limited number of data regarding its effectiveness in MPS.[8-10]
Considering the high prevalence of MPS and lack of a consensus regarding the most optimal treatment method, we hypothesized that both DN and KT would have short and also long-term therapeutic effects; however, the expected benefit from the DN group might be significantly higher.[1] Therefore, in this study, we aimed to compare DN and KT therapies in the treatment of MPS. Our primary objective was to investigate whether DN showed a better effect than KT on pain and physical function. Our secondary objective was to compare the effectiveness of DN and KT on the QoL and emotional state.
Patients and Methods
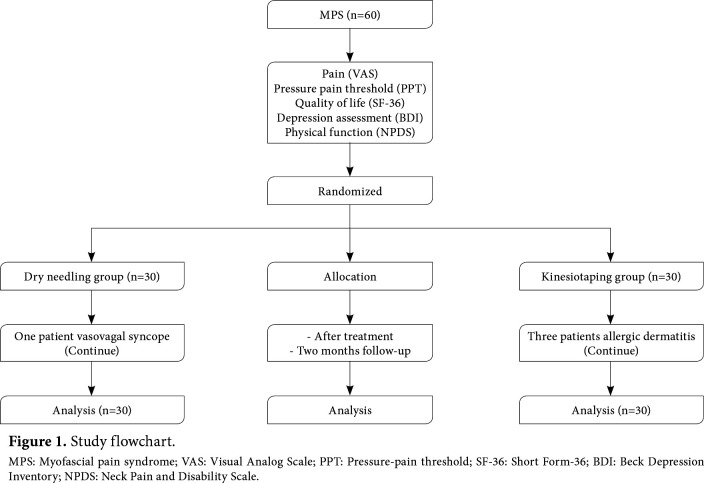
The prospective, randomized clinical study was conducted at Department of Physical Medicine and Rehabilitation of Medicine Faculty of Atatürk University between January 2014 and June 2014. A total of 60 patients (4 males, 56 females; mean age 31.2±9.8 years; range, 18 to 56 years) who were clinically diagnosed with MPS were included. The clinical diagnosis of MPS was based on the criteria by Travell and Simons (five major and at least one minor criteria are required for the diagnosis).[11] Inclusion criteria were as follows: having at least one active trigger point in the upper thoracic and cervical regions, age between 18 and 60 years, and a symptom duration of at least three months. Exclusion criteria were as follows: having cervical disc lesions, diagnosis of fibromyalgia syndrome, radiculopathy or myelopathy, trigger point injection within the past one month, neurological and inflammatory diseases, mental or psychotic diseases, malignancies, any allergic skin diseases (including metal allergy), severe cardiopulmonary problems, pregnancy, or a history of neck/shoulder surgery. The study flowchart is shown in Figure 1. A written informed consent was obtained from each patient. The study protocol was approved by the Medicine Faculty of Atatürk University Ethics Committee (No. 2013-6). The study was conducted in accordance with the principles of the Declaration of Helsinki.[12]
Figure 1. Study flowchart. MPS: Myofascial pain syndrome; VAS: Visual Analog Scale; PPT: Pressure-pain threshold; SF-36: Short Form-36; BDI: Beck Depression Inventory; NPDS: Neck Pain and Disability Scale.
Randomization
The patients were randomly divided into two treatment groups as DN (n=30) and KT (n=30). Randomization was done according to the order of admission to our outpatient clinic. We used the Visual Analog Scale (VAS) for pain, a pressure algometer for the pressure-pain threshold (PPT), Short Form-36 (SF-36) for the QoL, the Beck Depression Inventory (BDI) for the assessment of depressive symptoms, and the Neck Pain and Disability Scale (NPDS) for the physical function.
Group 1 were treated with DN (n=30). The patients of the DN group were carefully examined, and their two most painful trigger points received DN. To identify trigger points, taut bands were examined and the most painful area causing referred pain in a familiar pattern received needling. Trigger points’ dry needling process was performed by a three-year experienced physician in this field. We used a 0.25¥25 mm acupuncture needle and we applied DN three sessions with a five-day interval for a total of 15 days (Figure 2).
Figure 2. Dry needling technique of the trapezius muscle.

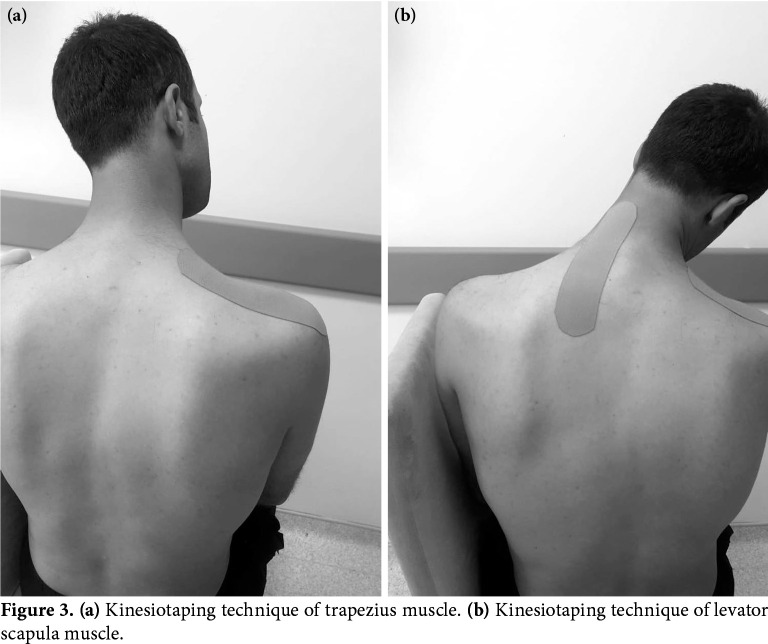
In Group 2, the patients were applied KT (Kinesio® Tex Gold, Kinesio Holding Corporation, Albuquerque NM, USA [2 inches ¥ 103.3 ft]) and treated with three sessions with a five-day interval for a total of 15 days. We used the muscle inhibition technique. We applied KT to the upper part of the trapezius and levator scapula muscles (Figure 3a, b).
Figure 3. (a) Kinesiotaping technique of trapezius muscle. (b) Kinesiotaping technique of levator scapula muscle.
Both groups were given a home-based exercise program including stretching and posture exercises (three intervals with 10 repetitions daily) for a total of two weeks. Non-steroidal anti-inflammatory drugs or other analgesics were not allowed during the treatment process.
Assessment tools
The VAS (10 cm straight-line with the end points defining extreme limits such as ‘no pain’ and ‘the worst possible pain’) was used for the pain assessment. The PPT on trigger points was measured with a pressure algometer (BASELINE trademark) that can be measured in kilograms (kg) and libres (Lb). The measurements were repeated three times, and the mean average score was recorded.
The QoL was assessed via SF-36. The SF-36 consists of 36 items questioning the patient’s perception of QoL in the following eight domains: physical function, role limitations due to physical problems (role physical), bodily pain, general health, vitality, social functioning, role limitations due to emotional problems (role emotional), and mental health. Subscale scores range from 0 to 100, with 100 as the most positive QoL in that area and 0 is the least; this scale has been validated in Turkish.[13]
Depressive symptoms of the individuals were evaluated by the Turkish version of BDI which was found valid and reliable. The BDI is a 21-item self- administered questionnaire with high scores reflecting a greater severity of depressed mood (range: 0 to 63). Each question consists of four statements about a particular symptom of depression, which is used to measure increased severity of depression. The answer to each question is scored between 0 and 3. A 0 to 13 points indicate no depression, 14 to 24 points suggest moderate depression, and scores higher than 25 points show severe depression.[14]
Physical function was evaluated with the NPDS. The NPDS is a 20-item self-report questionnaire designed to understand how much neck pain affects one’s ability to perform daily living activities. The total score ranges from 0 (no disability) to 100 (complete disability). We used the adapted Turkish version.[15]
Sociodemographic data and baseline VAS, PPT, SF-36, BDI, and NPDS scores were recorded. The same blinded assessor repeated the evaluations for the groups at the end of the treatment and two months after the treatment, twice in total.
Statistical analysis
Study power and sample size calculation were performed using the G*power version 3.1.2 software (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). For the VAS considered as the primary, a total of 60 patients were needed including 30 patients in each group with 80% power, 5% type 1 error and an effect size of 0.30.
Statistical analysis was performed using the IBM SPSS version 19.0 software (IBM Corp., Armonk, NY, USA). Descriptive statistics for continuous variables were expressed in mean ± standard deviation (SD) and median (min-max), while the categorical variables were expressed in number and frequency. Data normality was assessed with the Shapiro-Wilk test of normality. Independent samples t-test was used to compare normally distributed data. The chi-square test was used for categorical variables. We used two-way mixed analysis of variance (ANOVA) for normally distributed repeated data. The Friedman and Mann-Whitney U test for non- normally distributed repeated data. Bonferroni correction was used to keep type 1 error constant. A p value of <0.05 was considered statistically significant.
Results
Of a total of 60 patients, all completed the study. Only one patient from the DN group had vasovagal syncope and three patients from the KT group had allergic dermatitis due to the therapy; however, they all completed the therapies. There was no significant difference in the sex, age, body mass index, and symptom duration between the groups (p>0.05). Baseline sociodemographic characteristics of the patients are shown in Table 1.
Table 1. Baseline sociodemographic characteristics of the patients.
| Groups | ||||||||||||||||
| Dry needling Group (n=30) | Kinesiotaping Group (n=30) | Total | ||||||||||||||
| n | % | Mean±SD | Median | IQR | n | % | Mean±SD | Median | IQR | n | % | Mean±SD | Median | IQR | p | |
| Age (year) | 31.6±8.5 | 12-48 | 30.9±11.1 | 12-48 | 31.2±9.8 | 0,785 | ||||||||||
| Body mass index | 24.2±5.5 | 22.7±3.7 | 23.5±4.6 | 0,329 | ||||||||||||
| Symptom duration (month) | 24 | 12 | 15 | 12-48 0.567* | 12-48 0.567* | |||||||||||
| Sex | 0.612** | |||||||||||||||
| Female | 29 | 96,7 | 27 | 90 | 56 | 93,3 | ||||||||||
| Male | 1 | 3,3 | 3 | 10 | 4 | 6,7 | ||||||||||
| Education | 0.872** | |||||||||||||||
| Primary and secondary | 9 | 30 | 10 | 10 | 19 | 31,7 | ||||||||||
| High school | 7 | 23,3 | 9 | 8 | 15 | 25 | ||||||||||
| University | 14 | 46,7 | 12 | 12 | 26 | 43,3 | ||||||||||
| Marital status | 0.297** | |||||||||||||||
| Married | 19 | 63,3 | 15 | 50 | 34 | 56,7 | ||||||||||
| Single | 11 | 36,7 | 15 | 50 | 26 | 43,3 | ||||||||||
| Occupation | 0.121** | |||||||||||||||
| Employee | 12 | 40 | 5 | 16,7 | 17 | 28,3 | ||||||||||
| Student | 6 | 20 | 10 | 33,3 | 16 | 26,7 | ||||||||||
| Housewife | 12 | 40 | 15 | 50 | 27 | 45 | ||||||||||
| SD: Standard deviation; IQR: Interquartile range; Independent samples t test was used; * Mann Whitney U test was used; ** Chi-square test was used. | ||||||||||||||||
Both DN and KT demonstrated statistically significant improvements with VAS (p<0.001), PPT (p<0.001), all subscales of SF-36 (p<0.001), BDI (p<0.001) and NPDS (p<0.001) scores (Table 2).
Table 2. Pain, depression, and physical function assessments at baseline and after treatment.
| Groups | ||||||||||
| Dry needling Group (n=30) | Kinesiotaping Group (n=30) | Total | p2 | |||||||
| Mean±SD | Median | IQR | Mean±SD | Median | IQR | Mean±SD | Median | IQR | ||
| Visual Analog Scale | ||||||||||
| Baseline | 5.7±1.9a | 6.3±1.9a | 6.0±1.9a | 0.222 | ||||||
| 2nd assessment | 3.4±1.9b | 4.1±2.0b | 3.8±2.0b | 0.154 | ||||||
| 3rd assessment | 2.7±1.7b | 3.1±2.3c | 2.9±2.0c | 0.420 | ||||||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| Pressure pain threshold | ||||||||||
| Baseline | 5.4±1.9a | 5.1±1.7a | 5.3±1.7a | 0.743 | ||||||
| 2nd assessment | 7.6±2.1b | 7.5±1.9b | 7.6±2.0b | 0.719 | ||||||
| 3rd assessment | 8.8±1.5c | 8.4±1.6b | 8.6±1.6c | 0.623 | ||||||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| Beck depression inventory* | ||||||||||
| Baseline | 12.5 | 8-18a | 11.5 | 8-19a | 12 | 8-18a | 0.700 | |||
| 2nd assessment | 8 | 5-14a,b | 8.5 | 5-15a,b | 8 | 5-14b | 0.999 | |||
| 3rd assessment | 7 | 3-12b | 8 | 4-15b | 7.5 | 4-13c | 0.500 | |||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| Neck Pain and Disability Scale | ||||||||||
| Baseline | 56.5±17.0a | 55.4±19.2a | 56.0±18.0a | 0.815 | ||||||
| 2nd assessment | 43.5±19.2b | 39.5±21.6b | 41.5±20.4b | 0.448 | ||||||
| 3rd assessment | 35.5±17.5c | 35.1±22.9b | 35.3±20.2c | 0.935 | ||||||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
At the third follow-up visit, the improvement in the PPT and NPDS scores in the DN group and in those of VAS and the vitality subscale of SF-36 in the KT group sustained increasingly. However, these increments were not significantly different between the groups (p>0.05). In addition, no statistically significant difference was found between the DN and KT groups in terms of the all parameters either at the end of the treatment or two months after the treatment (Table 3).
Table 3. Short Form-36 subscales scores at baseline and after treatment.
| Groups | Total | p2 | ||||||||
| Dry needling Group (n=30) | Kinesiotaping Group (n=30) | |||||||||
| Mean±SD | Median | IQR | Mean±SD | Median | IQR | Mean±SD | Median | IQR | ||
| Physical function | ||||||||||
| Baseline | 59.6±20.3a | 66.2±17.2a | 62.9±19.0a | 0,223 | ||||||
| 2nd assessment | 71.0±16.5b | 73.3±18.5b | 72.2±17.4b | 0,462 | ||||||
| 3rd assessment | 75.9±13.1b | 77.5±16.2b | 76.7±14.7c | 0,552 | ||||||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| Role physical* | ||||||||||
| Baseline | 0 | 0-25a | 12,5 | 0-75a | 0 | 0-50a | 0,220 | |||
| 2nd assessment | 50 | 0-100a, b | 87,5 | 0-100a, b | 75 | 0-100b | 0,210 | |||
| 3rd assessment | 75 | 25-100b | 100 | 0-100b | 100 | 12.5-100b | 0,670 | |||
| p1 | <0.001 | 0,001 | <0.001 | |||||||
| Bodily pain* | ||||||||||
| Baseline | 31,5 | 22-41a | 26 | 22-41a | 31 | 22-41a | 0,385 | |||
| 2nd assessment | 56,5 | 41-62b | 51 | 41-72b | 51,5 | 41-62b | 0,765 | |||
| 3rd assessment | 62 | 51-74b | 56 | 41-84b | 61 | 42-74b | 0,566 | |||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| General health | ||||||||||
| Baseline | 49.9±18.7a | 49.6±20.0a | 49.7±19.0a | 0,807 | ||||||
| 2nd assessment | 60.7±22.4b | 57.3±20.8b | 59.0±21.5b | 0,491 | ||||||
| 3rd assessment | 64.1±15.5b | 62.8±22.4b | 63.5±19.1b | 0,941 | ||||||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| Vitality | ||||||||||
| Baseline | 38.2±17.0a | 35.7±20.3a | 37.0±18.6a | 0,588 | ||||||
| 2nd assessment | 50.7±19.2b | 50.3±18.6b | 50.5±18.7b | 0,911 | ||||||
| 3rd assessment | 54.7±14.4b | 58.2±17.7c | 56.5±16.1c | 0,592 | ||||||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| Social functioning* | ||||||||||
| Baseline | 50 | 25-62.5a | 56,25 | 25-75a | 50 | 25-75a | 0,484 | |||
| 2nd assessment | 75 | 50-87.5b | 62,5 | 50-87.5a, b | 68,75 | 50-87.5b | 0,759 | |||
| 3rd assessment | 75 | 62.5-87.5b | 87,5 | 50-87.5b | 75 | 56-87.5b | 0,946 | |||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| Role emotional* | ||||||||||
| Baseline | 0 | 0-100a | 33,3 | 0-100a | 33,15 | 0-100a | 0,688 | |||
| 2nd assessment | 66,7 | 0-100a, b | 100 | 0-100a, b | 100 | 0-100a, b | 0,281 | |||
| 3rd assessment | 100 | 66.7-100b | 100 | 66.7-100b | 100 | 66.7-100b | 0,985 | |||
| p1 | <0.001 | 0,021 | <0.001 | |||||||
| Mental health | ||||||||||
| Baseline | 53.5±17.0a | 50.6±17.2a | 52.1±17.0a | 0,481 | ||||||
| 2nd assessment | 60.5±14.7a, b | 61.2±18.6b | 60.9±16.6b | 0,624 | ||||||
| 3rd assessment | 65.0±11.2b | 63.3±16.6b | 64.1±14.0b | 0,608 | ||||||
| p1 | <0.001 | <0.001 | <0.001 | |||||||
| SD: Standard deviation; IQR: Interquartile range; p1: Within subject comparison; p2: Between-subject comparison. Two-way mixed ANOVA was used; * Friedman test for within subject comparison and Mann Whitney U test for between-subject comparison were used; a, b, c: Common letters in a column indicate statistical insignificance. | ||||||||||
Discussion
Myofascial pain syndrome is a painful disease originating from the trigger points in muscles. The main goal of the MPS treatment is to decrease the pain and regional muscle spasm by inactivating trigger points.[16]
In the literature, there are several randomized clinical studies and systematic reviews regarding the effectiveness of DN on MPS;[17-25] however, the number of studies on KT is limited.[8-10,26-28] In addition, there is no head-to-head study comparing DN and KT in MPS treatment.
In our study, DN and KT combined with posture and stretching exercises were both effective in improving pain, QoL, depression and physical function compared to baseline, and this effect sustained for over two months. However, there was no statistically significant difference between the treatment groups. The improved functionality and QoL may be a consequence of the decreased pain and the continuation of significant improvements at two months may be related to the improvement in muscle tone and elasticity after the treatment.
In a study, Rayegani et al.[29] investigated the effect of DN on pain intensity and PPT in patients with myofascial pain in the upper trapezius muscle. The authors observed similar improvements in the pain intensity and PPT after one session of DN compared to 10 physiotherapy sessions. Ozturk et al.[28] used KT to inactivate trigger points in patients with MPS and demonstrated a statistically significant improvement in pain intensity and strength of the upper trapezius muscle. In a study by Pecos-Martin et al.,[21] 72 patients with unilateral neck pain due to trigger points in the upper trapezius were randomly divided into two groups. The first group received DN in active trigger points in the trapezius, while the second group received DN in the trapezius muscle as well, but not at a trigger point. In both groups, pain, PPT, and disability scores were improved in one week and one month after the intervention controls (p<0.001). However, the DN to the trigger point showed more significant therapeutic effects (p<0.001). In a systematic review of randomized- controlled trials, Espejo-Antúnez et al.[22] examined the efficacy of DN in MPS treatment. Fifteen studies were evaluated, and the main outcome measures were the range of motion (ROM), pain, depression, QoL and disability. It was shown that DN provided pain relief, increased ROM, and improves the QoL, compared to no intervention/sham/placebo.[22]
Several KT banding techniques can be used in the correction of muscle tone disorders in MPS. In muscle problems due to overuse or tension, the inhibition technique can be preferred to inhibit the muscle function.[6] In the present study, DN was applied to the active trigger points in the trapezius muscle. In the KT group, the muscle inhibition technique was used to inhibit the trapezius and levator scapula muscles contraction.[6,21,26,30] The success of the present study is considered to be related to our application methods. Ay et al.[30] designed a double-blind, randomized, placebo-controlled study including 61 patients to investigate the effectiveness of KT in MPS treatment. The efficiency of KT was compared with sham taping. In both groups, there were statistically significant improvements on cervical ROM (except for rotation and lateral flexion) and disability (p<0.05). The KT showed more significant therapeutic effects on pain, PPT, and cervical flexion and extension (p<0.05). These results showed that KT had statistically significant effects on pain, PPT, and cervical ROM. However, in contrast to our study, disability was not affected by KT.[30] Saavedra-Hernández et al.[31] conducted a study in 36 patients and showed that both KT and cervical trust manipulation increased the ROM and provided a similar reduction in disability and pain severity.
Another study on different conventional modalities such as patient education, KT, spray- stretching, DN, eccentric exercise involved 156 patients with MPS in different body parts (cervicobrachial, n=102, lumbosacral, n=30, elbow, n=14, ankle and foot, n=10 and temporomandibular jaw, n=1). Statistically significant improvements (VAS ≥30 mm; p<0.001) were provided in 78.7% of the interventions. There was no statistically significant difference between the different body regions and different treatment modalities in the reduction of pain intensity.[32]
The main strength of the present study is the fact that it is the first study to compare the effectiveness of DN and KT in the treatment of MPS. Although both treatment modalities decreased pain, improved the QoL, and physical function, KT is a non-invasive and painless method for patients with needle phobia and DN itself may cause pain during the application. Additionally, depending on the muscle inhibition technique, KT may have anti-inflammatory and anti- edema effects, as well. Therefore, KT can be beneficial in acute painful periods in MPS.
The main limitations of this study include the lack of a third group which received exercises only. Besides, we followed our patients only for two months after the treatment. Longer follow-up period is needed to confirm these findings.
In conclusion, our study results show that KT is an effective alternative to DN in the treatment of MPS. Both treatments can reduce disability and pain and improve QoL in the short and long-term. Based on these results, we suggest that KT is a non-invasive and a painless alternative for patients, particularly those with a fear of needles. However, further large-scale, long-term, prospective studies are required to evaluate the long-term effects of these therapies.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.De Meulemeester KE, Castelein B, Coppieters I, Barbe T, Cools A, Cagnie B. Comparing Trigger Point Dry Needling and Manual Pressure Technique for the Management of Myofascial Neck/Shoulder Pain: A Randomized Clinical Trial. J Manipulative Physiol Ther. 2017;40:11–20. doi: 10.1016/j.jmpt.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Cheng KJ. Neuroanatomical basis of acupuncture treatment for some common illnesses. Acupunct Med. 2009;27:61–64. doi: 10.1136/aim.2009.000455. [DOI] [PubMed] [Google Scholar]
- 3.Dunning J, Butts R, Mourad F, Young I, Flannagan S, Perreault T. Dry needling: a literature review with implications for clinical practice guidelines. Phys Ther Rev. 2014;19:252–265. doi: 10.1179/108331913X13844245102034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dommerholt J, Fernandez-de-las-Penas C. Trigger point dry needling: An evidence and clinical-based approach. Edinburgh: Churchill Livingstone (Elsevier); 2013. [Google Scholar]
- 5.Fu TC, Wong AM, Pei YC, Wu KP, Chou SW, Lin YC. Effect of Kinesio taping on muscle strength in athletes-a pilot study. J Sci Med Sport. 2008;11:198–201. doi: 10.1016/j.jsams.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Kase K, Wallis J, Kase T, editors , editors. Clinical therapeutic applications of the kinesio taping method. 2. Tokyo: Ken Ikai Co. Ltd.; 2003. [Google Scholar]
- 7.Oliveira AK, Borges DT, Lins CA, Cavalcanti RL, Macedo LB, Brasileiro JS. Immediate effects of Kinesio Taping(®) on neuromuscular performance of quadriceps and balance in individuals submitted to anterior cruciate ligament reconstruction: A randomized clinical trial. J Sci Med Sport. 2016;19:2–6. doi: 10.1016/j.jsams.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Parreira Pdo C, Costa Lda C, Takahashi R, Hespanhol Junior LC, Luz Junior MA, Silva TM, et al. Kinesio taping to generate skin convolutions is not better than sham taping for people with chronic non-specific low back pain: a randomised trial. J Physiother. 2014;60:90–96. doi: 10.1016/j.jphys.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Bassett KT, Lingman SA, Ellis R. The use and treatment efficacy of kinaesthetic Taping for musculoskeletal conditions: A systematic review. New Zealand Journal of Physiotherapy. 2010;38:56–62. [Google Scholar]
- 10.Morris D, Jones D, Ryan H, Ryan CG. The clinical effects of Kinesio® Tex taping: A systematic review. Physiother Theory Pract. 2013;29:259–270. doi: 10.3109/09593985.2012.731675. [DOI] [PubMed] [Google Scholar]
- 11.Travell JG, Simons DG, editors . The Trigger Point Manual. Myofascial pain and dysfunction. Vol 1. Philadelphia: Lippincott Williams & Wilkins; 1992. The Trigger Point Manual. [Google Scholar]
- 12.General Assembly of the World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81:14–18. [PubMed] [Google Scholar]
- 13.Kaya BB, İçağasıoğlu A. Reliability and validity of the Turkish version of short form 36 (SF-36) in patients with rheumatoid arthritis. J Surg Med. 2018;2:11–16. [Google Scholar]
- 14.Hisli N. Beck Depresyon Envanterinin üniversite öğrencileri için geçerliği, güvenirliği. Psikoloji Dergisi. 1989;7:3–13. [Google Scholar]
- 15.Bicer A, Yazici A, Camdeviren H, Erdogan C. Assessment of pain and disability in patients with chronic neck pain: reliability and construct validity of the Turkish version of the neck pain and disability scale. Disabil Rehabil. 2004;26:959–962. doi: 10.1080/09638280410001696755. [DOI] [PubMed] [Google Scholar]
- 16.Giamberardino MA, Affaitati G, Fabrizio A, Costantini R. Myofascial pain syndromes and their evaluation. Best Pract Res Clin Rheumatol. 2011;25:185–198. doi: 10.1016/j.berh.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Tekin L, Akarsu S, Durmuş O, Cakar E, Dinçer U, Kıralp MZ. The effect of dry needling in the treatment of myofascial pain syndrome: a randomized double-blinded placebo-controlled trial. Clin Rheumatol. 2013;32:309–315. doi: 10.1007/s10067-012-2112-3. [DOI] [PubMed] [Google Scholar]
- 18.Ay S, Evcik D, Tur BS. Comparison of injection methods in myofascial pain syndrome: a randomized controlled trial. Clin Rheumatol. 2010;29:19–23. doi: 10.1007/s10067-009-1307-8. [DOI] [PubMed] [Google Scholar]
- 19.Kalichman L, Vulfsons S. Dry needling in the management of musculoskeletal pain. J Am Board Fam Med. 2010;23:640–646. doi: 10.3122/jabfm.2010.05.090296. [DOI] [PubMed] [Google Scholar]
- 20.Venâncio Rde A, Alencar FG, Zamperini C. Different substances and dry-needling injections in patients with myofascial pain and headaches. Cranio. 2008;26:96–103. doi: 10.1179/crn.2008.014. [DOI] [PubMed] [Google Scholar]
- 21.Pecos-Martín D, Montañez-Aguilera FJ, Gallego-Izquierdo T, Urraca-Gesto A, Gómez-Conesa A, Romero-Franco N, et al. Effectiveness of dry needling on the lower trapezius in patients with mechanical neck pain: a randomized controlled trial. Arch Phys Med Rehabil. 2015;96:775–781. doi: 10.1016/j.apmr.2014.12.016. [DOI] [PubMed] [Google Scholar]
- 22.Espejo-Antúnez L, Tejeda JF, Albornoz-Cabello M, Rodríguez-Mansilla J, de la Cruz-Torres B, Ribeiro F, et al. Dry needling in the management of myofascial trigger points: A systematic review of randomized controlled trials. Complement Ther Med. 2017;33:46–57. doi: 10.1016/j.ctim.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 23.Kietrys DM, Palombaro KM, Mannheimer JS. Dry needling for management of pain in the upper quarter and craniofacial region. Curr Pain Headache Rep. 2014;18:437–437. doi: 10.1007/s11916-014-0437-0. [DOI] [PubMed] [Google Scholar]
- 24.Mejuto-Vázquez MJ, Salom-Moreno J, Ortega-Santiago R, Truyols-Domínguez S, Fernández-de-Las-Peñas C. Short-term changes in neck pain, widespread pressure pain sensitivity, and cervical range of motion after the application of trigger point dry needling in patients with acute mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44:252–260. doi: 10.2519/jospt.2014.5108. [DOI] [PubMed] [Google Scholar]
- 25.Maher RM, Hayes DM, Shinohara M. Quantification of dry needling and posture effects on myofascial trigger points using ultrasound shear-wave elastography. Arch Phys Med Rehabil. 2013;94:2146–2150. doi: 10.1016/j.apmr.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 26.Azatcam G, Atalay NS, Akkaya N, Sahin F, Aksoy S, Zincir O, et al. Comparison of effectiveness of Transcutaneous Electrical Nerve Stimulation and Kinesio Taping added to exercises in patients with myofascial pain syndrome. J Back Musculoskelet Rehabil. 2017;30:291–298. doi: 10.3233/BMR-150503. [DOI] [PubMed] [Google Scholar]
- 27.Ata E, Kösem M, Adiguzel E. Does kinesiotaping increase the efficacy of lidocaine injection in myofascial pain syndrome treatment. A randomized controlled study. J Back Musculoskelet Rehabil. 2019;32:471–477. doi: 10.3233/BMR-171035. [DOI] [PubMed] [Google Scholar]
- 28.Öztürk G, Külcü DG, Mesci N, Şilte AD, Aydog E. Efficacy of kinesio tape application on pain and muscle strength in patients with myofascial pain syndrome: a placebo- controlled trial. J Phys Ther Sci. 2016;28:1074–1079. doi: 10.1589/jpts.28.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rayegani SM, Bayat M, Bahrami MH, Raeissadat SA, Kargozar E. Comparison of dry needling and physiotherapy in treatment of myofascial pain syndrome. Clin Rheumatol. 2014;33:859–864. doi: 10.1007/s10067-013-2448-3. [DOI] [PubMed] [Google Scholar]
- 30.Ay S, Konak HE, Evcik D, Kibar S. The effectiveness of Kinesio Taping on pain and disability in cervical myofascial pain syndrome. Rev Bras Reumatol Engl Ed. 2017;57:93–99. doi: 10.1016/j.rbre.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 31.Saavedra-Hernández M, Castro-Sánchez AM, Arroyo-Morales M, Cleland JA, Lara-Palomo IC, Fernández-de-Las-Peñas C. Short-term effects of kinesio taping versus cervical thrust manipulation in patients with mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2012;42:724–730. doi: 10.2519/jospt.2012.4086. [DOI] [PubMed] [Google Scholar]
- 32.Segura-Pérez M, Hernández-Criado MT, Calvo-Lobo C, Vega-Piris L, Fernández-Martín R, Rodríguez-Sanz D. A Multimodal Approach for Myofascial Pain Syndrome: A Prospective Study. J Manipulative Physiol Ther. 2017;40:397–403. doi: 10.1016/j.jmpt.2017.06.001. [DOI] [PubMed] [Google Scholar]