Key Points
Question
What are the clinical features in women who experience aortic dissection related to pregnancy?
Findings
In this cohort study, 29 women, representing 1% of women in the International Registry of Acute Aortic Dissection, experienced aortic dissection related to pregnancy. Most women had an underlying aortopathy condition, but many were previously unaware of this diagnosis.
Meaning
Aortic dissection is a rare complication of pregnancy that occurs in women with aortopathy conditions; the findings of this study suggest that these conditions are often not recognized until after the aortic dissection occurs.
Abstract
Importance
Women with aortopathy conditions are at risk for pregnancy-related aortic dissection, and these conditions may not be recognized until after the aortic dissection occurs.
Objective
To examine the clinical characteristics, imaging features, and outcomes in women with pregnancy-related acute aortic dissection.
Design, Setting, and Participants
A cohort study, comprising data from the International Registry of Acute Aortic Dissection (IRAD) (February 1, 1998, to February 28, 2018). The multicenter referral center study included 29 women with aortic dissection during pregnancy or less than 12 weeks post partum in IRAD from 1998 to 2018.
Main Outcomes and Measures
Clinical features of pregnancy-related aortic dissection to be studied included underlying aortopathy, aortic size, type of aortic dissection, timing of dissection, hypertension, and previous aortic surgery.
Results
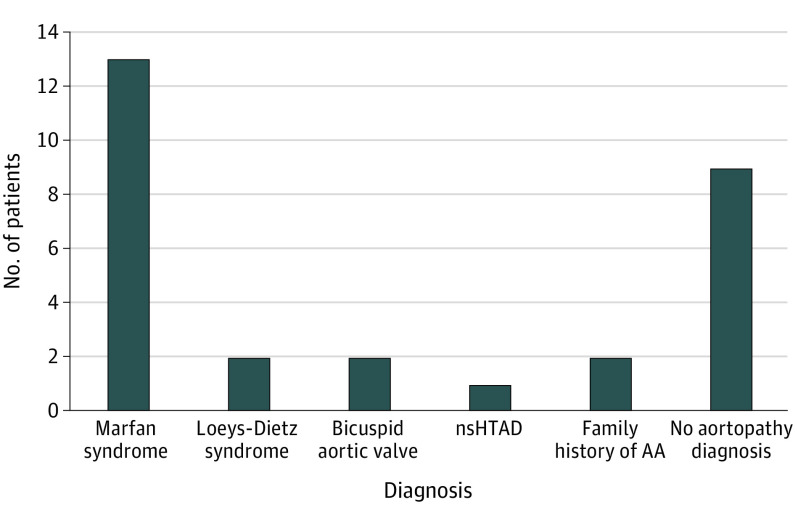
A total of 29 women (mean [SD] age, 32 [6] years) had pregnancy-related aortic dissection, representing 0.3% of all aortic dissections and 1% of aortic dissection in women in the IRAD. Among women younger than 35 years, aortic dissection was related to pregnancy in 20 of 105 women (19%). Thirteen women (45%) had type A aortic dissection, and 16 women (55%) had type B. Aortic dissection onset was known in 27 women (93%): 15 during pregnancy, 4 in the first trimester, and 11 in the third trimester; 12 were post partum, occurring a mean (SD) of 12.5 (14) days post partum. At type A aortic dissection diagnosis, the mean (SD) aortic diameters were sinus of Valsalva, 54.5 (5) mm and ascending aorta, 54.7 (6) mm. At type B aortic dissection diagnosis, the mean (SD) descending aortic diameter was 32.5 (5) mm. Twenty women (69%) had an aortopathy condition or a positive family history: 13 women (65%) with Marfan syndrome, 2 women (10%) with Loeys-Dietz syndrome, 2 women (10%) with bicuspid aortic valves, 2 women (10%) with a family history of aortic disease, and 1 woman (5%) with familial thoracic aortic aneurysm. Aortopathy was not recognized until after aortic dissection in 47% of the women. Twenty-eight women (97%) survived aortic dissection hospitalization.
Conclusions and Relevance
Aortic dissection complicating pregnancy is rare. Most pregnancy-related aortic dissection is due to an aortopathy often not diagnosed until after aortic dissection. In this study, type A aortic dissections were associated with a dilated aorta, and type B aortic dissections often were not. Recognition of underlying conditions and risks for aortic dissection may improve management of pregnancy in women with aortopathy.
This cohort study examines the presentation and outcomes of women who experience aortic dissection during pregnancy or within 12 weeks post partum.
Introduction
Aortic dissection is a rare, life-threatening complication of pregnancy. Women with Marfan syndrome, Loeys-Dietz syndrome, nonsyndromic heritable thoracic aortic disease (HTAD), vascular Ehlers-Danlos syndrome, Turner syndrome, bicuspid aortic valve (BAV) with aneurysm, and other aortopathies are at an increased risk of aortic dissection related to pregnancy.1 Women with significant aortic dilatation are advised to avoid pregnancy or undergo prophylactic aortic aneurysm surgery before conception.2,3,4 Multidisciplinary preconception counseling in at-risk women involves shared decision-making to discuss risks (including aortic dissection) and advise on optimal management, as well as when pregnancy is best avoided. However, many women with pregnancy-related aortic dissection are not recognized beforehand to be at risk. Our study examined the clinical features, aortic imaging characteristics, and outcomes of women with acute aortic dissection related to pregnancy listed in the International Registry of Acute Aortic Dissection (IRAD).
Methods
We analyzed 9707 patients enrolled in the IRAD from February 1, 1998, through February 28, 2019, to identify women who presented with aortic dissection during pregnancy or post partum (≤12 weeks). There are 3341 women enrolled in the IRAD and pregnancy/post partum aortic dissection status was available in 2788 women (83%), of whom 29 experienced an acute aortic dissection during pregnancy or post partum. Additional information was requested about these 29 patients from each IRAD investigator from the 17 sites reporting a pregnancy-related aortic dissection.
Aortic dissection was classified as type A (ascending aorta involved) or type B (ascending aorta not involved) based on the Stanford classification.5 Additional information included the presence or absence of a BAV, genetic test results, and specific aortopathy diagnosis. Aortic dissection occurrence was reported based on trimester or days post partum. Previous pregnancy was recorded, as was a history of hypertension or β-blocker use during pregnancy. Data on mode of delivery and maternal and fetal outcomes were collected. Management of the aortic dissection was reported as medical, endovascular, or surgical. Aortic diameters at aortic dissection diagnosis were reported at the sinuses of Valsalva (aortic root), ascending aorta, and proximal descending aorta in both type A and type B aortic dissections. Aortic measurements available during pregnancy or before aortic dissection were recorded. A history of aortic surgery or aortic dissection was recorded. The IRAD study was approved by the institutional review board of each contributing institution. Informed consent (oral or written) was obtained from study participants or, if applicable, a waiver/exemption of such consent was granted by the institutional review board of each institution.
Results
Between February 1, 1998, and February 28, 2019, 29 women in the IRAD experienced an aortic dissection associated with pregnancy: 0.3% (29/9707) of all cases in the IRAD and 1% (29/2788) of women in the IRAD with pregnancy data available. Among women younger than 35 years with available data, 20 of 105 aortic dissections (19%) occurred during pregnancy or within 12 weeks post partum. These women experienced aortic dissection at a mean (SD) age of 32 (6) years (range, 20-43 years). Details of each case are listed in Table 1.
Table 1. Clinical, Obstetric, and Aortic Imaging Data in Women With Pregnancy-Related Acute Aortic Dissection.
| Patient No. | Aortopathy diagnosis | Diagnosis Ghent or revised Ghent; genetic testing | Aortopathy diagnosis before vs after dissection | Prior aortic surgery | Aortic dissection type | Time of dissection | Treatment | Aortic diameter, mm | β-Blocker use | Hypertensiona | Mode of delivery | Prior pregnancy | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before aortic dissection | At time of diagnosis of aortic dissection | ||||||||||||
| 1 | Marfan | NA | NA | No | A | 3rd TM | Surgery | 47 SoV | 52 SoV; 53 AA | No | No | Cesarean | Yes |
| 2 | Marfan | Ghent FBN1 | Before | No | A | 28 d PP | Surgery | 45 SoV | 45 SoV; 48 AA; 35 DA | Yes | No | Vaginal | No |
| 3 | Marfan | Ghent | After | No | A | 6 d PP | Surgery | NA | 76 SoV; 70 AA | No | No | Cesarean | Yes |
| 4 | Marfan | Ghent FBN1 | Before | No | A | 3rd TM | Surgery | 41 SoV | 50 SoV; 42 AA; 27 DA | Yes | No | Cesarean | No |
| 5 | Marfan | Revised Ghent | After | No | A | 3rd TM | Surgery | NA | 52 SoV; 60 AA; 25 DA | No | No | Cesarean | Yes |
| 6 | Marfan | Revised Ghent FBN1 | After | No | A | 3rd TM | Surgery | NA | 60 SoV; 68 AA; 22 DA | No | No | Cesarean | Yes |
| 7 | Marfan | NA | NA | No | A | NA | Surgery | NA | 42 SoV; 50 AA; 24 DA | NA | NA | NA | NA |
| 8 | BAV | No genetic testing | After | No | A | 3rd TM | Surgery | No | 52 SoV; 46 AA; 24 DA | No | No | Cesarean | No |
| 9 | BAV | No genetic testing | After | No | A | 3rd TM | Surgery | NA | NA | No | Yes | Cesarean | No |
| 10 | FTAA | No genetic testing | After | No | A | 2 d PP | Surgery | NA | 60 SoV; 70 AA | No | No | Cesarean | No |
| 11 | +FH aortic disease | Genetic testing: no variants | NA | No | A | NA | Surgery | 41 SoV | 42 AA; 21 DA | No | Yes | Cesarean | Yes |
| 12 | None | NA | NA | No | A | 4 d PP | Surgery | NA | 63 SoV; 55 AA; 24 DA | No | No | Vaginal | No |
| 13 | None | NA | NA | No | A | 3rd TM | Surgery | NA | 47 SoV; 40 AA; 44 DA | NA | Yes | Cesarean | Yes |
| 14 | Marfan | Ghent FBN1 | Before | No | B | 10 d PP | Medical | NA | 39 SoV; 29 AA; 28 DA | NA | No | Vaginal | Yes |
| 15 | Marfan | Ghent FBN1 | Before | VSRR | B | 3rd TM | Medical | 20 DA | 35 SoV; 28 AA; 30 DA | Yes | No | Cesarean | Yes |
| 16 | Marfan | Revised Ghent FBN1 | Before | No | B | 5 d PP | Medical | 22 DA | 28 AA; 27 DA | Yes | No | Vaginal | Yes |
| 17 | Marfan | Revised Ghent FBN1 | Before | No | B | 1st TM | Surgery | NA | 40 SoV; 60 DA | Yes | Yes | Termination | Yes |
| 18 | Marfan | Revised Ghent FBN1 | After | No | B | 3rd TM | TEVAR | 36 SoV | 33 SoV; 24 AA; 23 DA | Yes | No | Cesarean | No |
| 19 | Marfan | Revised Ghent | NA | No | B | 5 d PP | Medical | 41 SoV | 38 SoV | Yes | No | Cesarean | Yes |
| 29 DA | |||||||||||||
| 20 | Loeys-Dietz | TGFBR1 | Before | No | B | 56 d PP | Surgery | 42 SoV; 30 AA; 36 DA | 47 SoV; 45 AA; 57 DA | Yes | No | Cesarean | No |
| 21 | Loeys-Dietz | TGFBR1 | Before | VSRR | B | 3 d PP | Surgery | 28 DA | 33 SoV; 35 AA; 32 DA | Yes | No | Cesarean | No |
| 22 | +FH aortic disease | Genetic testing: no variants | NA | No | B | 10 d PP | TEVAR | 22 DA | 27 SoV; 30 AA; 30 DA | No | No | Vaginal | Yes |
| 23 | None | NA | NA | VSRR | B | 3rd TM | Surgery | NA | 35 SoV | NA | NA | Cesarean | NA |
| 24 | None | Genetic testing: no variants | NA | None | B | 11 d PP | Medical | NA | 27 SoV; 26 AA; 24 DA | No | No | Vaginal | Yes |
| 25 | None | NA | NA | No | B | 1st TM | TEVAR | NA | 40 SoV; 39 AA; 27 DA | No | Yes | MC | Yes |
| 26 | None | NA | NA | No | B | 1st TM | Medical | NA | 31 SoV; 34 AA; 24 DA | No | No | Vaginal | No |
| 27 | None | NA | NA | Prior type B aortic dissection | B | 1st TM | Medical | NA | 24 AA; 29 DA | No | Yes | Termination | NA |
| 28 | None | NA | NA | No | B | 10 d PP | Medical | NA | 31 SoV; 36 AA; 31 DA | No | Yes, PE | Cesarean | Yes |
| 29 | None | COL5A1 VUS | NA | No | B | 3rd TM | Medical | NA | 26 SoV; 26 AA; 35 DA | No | No | Vaginal | Yes |
Abbreviations: AA, ascending aorta; BAV, bicuspid aortic valve; DA, descending aorta; +FH, positive family history; FTAA, familial thoracic aortic aneurysm; MC, miscarriage; NA, not available; PE, preeclampsia; PP, post partum; SoV, sinus of Valsalva; TEVAR, thoracic endovascular aortic repair; TM, trimester; VSRR, valve-sparing root replacement; VUS, variant of unknown significance.
Hypertension or hypertensive disorder during pregnancy.
Acute type A aortic dissection occurred in 13 women (45%) and type B aortic dissection occurred in 16 women (55%). Timing of aortic dissection was available in 27 women. Fifteen had aortic dissection during pregnancy (4 in the first trimester; 11 in the third trimester). Twelve women had aortic dissection post partum at a mean (SD) interval of 12.5 (14) days post partum (interquartile range, 4.5-10.5 days; range, 2-56 days). Of 11 women with timing of type A dissections known, 7 dissections (64%) occurred in the third trimester and 4 of dissections (36%) occurred post partum, while 8 of 16 type B dissections (50%) occurred post partum. Treatment strategies were reported for all women. All 13 with type A aortic dissections underwent surgical repair. Of 16 type B aortic dissections, 10 were treated medically, 3 had endovascular procedures, and 3 were treated surgically. All women sustaining aortic dissection in the third trimester underwent a cesarean delivery. Of the 4 women with type B aortic dissection in the first trimester, 1 developed an aortic dissection 4 days after a miscarriage, 2 terminated pregnancy after aortic dissection, and 1 carried the pregnancy to term. One woman with Loeys-Dietz syndrome and post partum type B aortic dissection was treated surgically. After acute dehiscence of the graft and aortic rupture, emergency endovascular repair was performed.6 Previous obstetric information was available for 26 women, of whom 10 were primipara and 16 were multipara (1-15 pregnancies) status. Aortic diameters at the time of aortic dissection are listed in Table 2.
Table 2. Aortic Diameter at the Time of Acute Aortic Dissection Diagnosis.
| Location | Aortic diameter, mm | |
|---|---|---|
| In women with type A dissection (n = 13) | In women with type B dissection (n = 16) | |
| Sinuses of Valsalva | ||
| Mean (SD) | 54.5 (5) | 34.4 (3) |
| IQR | 40.5-60 | 30-39 |
| Range | 42-76 | 26-47 |
| Ascending aorta | ||
| Mean (SD) | 54.7 (6) | 31 (3) |
| IQR | 47-64 | 26-35 |
| Range | 40-70 | 24-45 |
| Descending aorta | ||
| Mean (SD) | 26.9 (4) | 32.5 (5) |
| IQR | 22-32 | 27-32.5 |
| Range | 21-44 | 23-60 |
Abbreviation: IQR, interquartile range.
Twenty of the 29 women (69%) had an underlying thoracic aortic aneurysm disease or a family history of aortic disease (Figure). Seven of 11 type A dissections (64%) occurred in the third trimester and 4 of 11 type A dissections (36%) occurred post partum. Of the 16 type B aortic dissections, 4 (25%) occurred in the first trimester, 4 (25%) occurred in the third trimester, and 8 (50%) occurred post partum. Of the 15 of these 20 women for whom data were reported, 8 women (53%) were known to have a predisposing aortopathy condition prior to aortic dissection, while 7 women (47%) were discovered to have a specific aortopathy after the aortic dissection occurred. Of 6 women in the current series with Marfan syndrome whose onset of aortic dissection was known, 4 (66%) occurred in the third trimester. Eight women in this series with a type B aortic dissection had a syndromic aortopathy: 6 had Marfan syndrome and 2 had Loeys-Dietz syndrome; in 5 of these 8 cases (63%), the type B dissection occurred post partum. Two women with aortic dissection and a family history of aortic disease had normal genetic testing. Thus, it is possible that a total of 3 women (15%) had a nonsyndromic HTAD. The 2 women with BAV disease each had a type A aortic dissection. Aortic diameters at the time of aortic dissection were known for 1 patient: 52 mm at the sinus of Valsalva and 46 mm at the ascending aorta.
Figure. Aortopathy Diagnosis in Women With Pregnancy-Related Aortic Dissection.
AA indicates aortic aneurysm; nsHTAD, nonsyndromic heritable thoracic aortic disease.
In 9 women with pregnancy-related acute aortic dissection, data on aortic diameters before aortic dissection were available. Seven of these patients had syndromic aortopathy conditions (5 with Marfan syndrome; 2 with Loeys-Dietz syndrome), and aortic measurements were available during pregnancy (before aortic dissection) and after aortic dissection (Table 3). Eleven of 13 women (85%) with type A aortic dissection had an underlying aortopathy diagnosis established, while 7 of 16 women (44%) with type B aortic dissection did not. In 4 patients with type A aortic dissection, the mean (SD) aortic diameter at the sinuses of Valsalva during pregnancy and before the acute aortic dissection was 43.5 (2.5) mm (interquartile range, 41-46 mm; range, 41-47 mm). Three of the women with acute type A dissections had Marfan syndrome and their aortic root diameters before aortic dissection were 41, 45, and 47 mm. The fourth woman did not have an aortopathy diagnosis reported. Among 5 patients with type B dissection for whom preaortic dissection aortic measurements were available, the mean descending aortic diameter before aortic dissection was 25.5 (5.1) mm (interquartile range, 21-32; range 20-36 mm). Two of the women with type B aortic dissection had Marfan syndrome and their descending aortic diameters were 20 and 22 mm. Two women with type B aortic dissection had Loeys-Dietz syndrome and their descending thoracic aortic diameters were 28 and 36 mm. The fifth woman with a pregnancy-related type B aortic dissection had a predissection descending thoracic aortic diameter of 22 mm and did not have an aortopathy diagnosis reported. One woman with a type B aortic dissection underwent genetic testing with a COL5A1 variant of unknown significance reported.
Table 3. Aortic Diameters Before Acute Aortic Dissection in Patients With Syndromic Aortopathy Known Before Pregnancy.
| Patient No. | Aortopathy condition | Aortic dissection type | Aortic diameter before aortic dissection, mm | Location of aortic measurement |
|---|---|---|---|---|
| 1 | Marfan | A | 47 | Sinus of Valsalva |
| 2 | Marfan | A | 45 | Sinus of Valsalva |
| 4 | Marfan | A | 41 | Sinus of Valsalva |
| 15a | Marfan | B | 20 | Descending aorta |
| 16 | Marfan | B | 22 | Descending aorta |
| 20 | Loeys-Dietz | B | 36 | Descending aorta |
| 21a | Loeys-Dietz | B | 28 | Descending aorta |
Underwent previous valve-sparing root replacement for aortic root aneurysm.
Three women (1 each with Marfan syndrome, Loeys-Dietz syndrome, and no specific genetic aortopathy diagnosis) had previously undergone aortic root replacement for aneurysm and each experienced type B aortic dissection related to subsequent pregnancy. One woman with a previous type B aortic dissection who was without a syndromic aortopathy diagnosis or family history of aneurysm disease developed a second type B aortic dissection during the first trimester of pregnancy, with no additional phenotypic or genetic information available. This patient had uncontrolled hypertension and underwent elective termination of pregnancy. Of the 26 women with available data, 16 reported a family history of aortic disease: 10 had a family history of Marfan syndrome, 2 had Loeys-Dietz syndrome, 1 had nonsyndromic HTAD, 1 with BAV disease reported a family history of aortic disease, and 2 reported a family history of aortic disease, not further specified. It was not reported whether the family histories were known before pregnancy or after the aortic dissection.
Among 28 patients for whom data were available, 7 women (24%) had hypertension and 1 developed preeclampsia. Only 1 woman with a syndromic aortopathy (Marfan) and aortic dissection had hypertension. Data regarding medications prescribed during pregnancy were available for 26 patients. Nine were taking β-blockers, of whom 6 had Marfan syndrome, 2 had Loeys-Dietz syndrome, and 1 had no syndromic aortopathy. In the 9 women taking β-blockers during pregnancy, 2 had type A aortic dissections and 7 experienced type B aortic dissections.
Discussion
This IRAD study represents one of the largest analyses to date of pregnancy-related acute aortic dissection. Our findings document the strong link between underlying aortopathy and aortic dissection related to pregnancy. In our series, 20 of 29 women (69%) with pregnancy-related aortic dissection had an underlying HTAD (Marfan syndrome, Loeys-Dietz syndrome, or nonsyndromic HTAD), BAV with aneurysm, or a family history of aortic disease. Because the data do not include genetic analysis or phenotypic features for each patient, the incidence of underlying genetic aortic disease may be higher. Alternatively, women without features of syndromic aortopathy may have had subsequent evaluations for HTADs.7,8
Aortic dissection in pregnancy is rare, occurring in only 0.0004% of pregnancies.9 In the Nationwide Inpatient Sample of more than 10 million pregnancies and 41 000 aortic dissections from 1998 to 2008, only 44 cases of aortic dissection in pregnancy were reported, representing 0.1% of all cases of aortic dissection.9 Kamel et al10 reported 36 cases of aortic dissection during pregnancy or post partum out of 6 566 826 pregnancies (5.5 per million patients during pregnancy or post partum) from 2005 to 2013. Although rarely reported, pregnancy is associated with a significantly increased risk of aortic dissection, with an incidence that is approximately 4- to 25-fold higher than that observed in the nonpregnant state.10,11 In this analysis from the IRAD, aortic dissection related to pregnancy represented only 0.3% of all reported cases of aortic dissection. However, pregnancy was associated with 19% of aortic dissections in women younger than 35 years.
Hemodynamic stress and/or alterations in connective tissue related to hormonal changes may be responsible for increased susceptibility to aortic dissection during pregnancy or post partum.1 Pregnancy leads to an increase in sympathetic activity and activation of the renin-angiotensin-aldosterone system with increased cardiac output and blood volume, which are hemodynamic changes that peak in the third trimester and during labor and delivery.12 Alterations in pregnancy hormone levels may affect aortic wall infrastructure.13 Marfan mouse models theorize that oxytocin influences post partum aortic dissection risk.14 Aortic growth rates are variably reported during pregnancy in women with Marfan syndrome, but progressive aortic dilatation is associated with aortic dissection risk.15,16
Women with underlying aortopathies, such as Marfan syndrome, Loeys-Dietz syndrome, vascular Ehlers-Danlos syndrome, nonsyndromic HTAD, Turner syndrome, and BAV with aneurysm, are at increased risk of aortic dissection related to pregnancy.1,2,4,17,18,19,20,21 In the GenTAC registry, pregnancy in women with Marfan syndrome was associated with an 8-fold increase risk of aortic dissection compared with nonpregnant intervals.17 Features of genetic aortopathy may sometimes be subtle, and recognizing aortopathy phenotypes is important in appropriate disease management.22 In the GenTAC registry, only 42% of women with Marfan syndrome were aware of their diagnosis before pregnancy and only 3 of 7 women (43%) experiencing pregnancy-related aortic dissection had Marfan syndrome diagnosed before aortic dissection.17 In this IRAD cohort, 47% of women were not recognized as having an underlying aortopathy condition until after aortic dissection.
In case series of Marfan syndrome, aortic dissection related to pregnancy has been reported in 0 to 4.5% of women.23,24,25,26,27,28,29 Aortic dilatation and hypertension increase the risk of aortic dissection.10,15,30 The risk of type A aortic dissection is estimated to be 1% when the aortic root is less than 40 mm and 10% when the aortic root is greater than 40 mm.1,2,16,23,31 In women with Marfan syndrome and aortic diameters between 40 and 45 mm, some studies report no adverse outcomes with pregnancy while others report cases of type A aortic dissection.15,27,30,32 Aortic root replacement is recommended when the aortic diameter exceeds 40 to 45 mm in women with Marfan syndrome contemplating pregnancy, although international guidelines differ.2,3,4 Of 3 women in the present series with Marfan syndrome who had type A aortic dissections and for whom aortic diameters were available during pregnancy and before aortic dissection, all experienced dissection with an aortic root diameter greater than 40 mm (41, 45, and 47 mm)(Table 3). Thus, pregnancy in women with Marfan syndrome and moderate (ie, 40-45 mm) aortic root dilatation carries risk of aortic dissection.
Loeys-Dietz syndrome is associated with increased risk of pregnancy-related aortic dissection.6,19,33 Two women in the current series had Loeys-Dietz syndrome. One woman with a 42-mm aortic root and a 36-mm descending aorta during pregnancy had acute type B aortic dissection 8 weeks post partum. Another woman with a prior valve-sparing root replacement developed acute type B aortic dissection 3 days post partum with a predissection descending aortic diameter of 28 mm.6
Bicuspid aortic valve disease is often complicated by aortopathy.34 Despite a prevalence of 1%, BAV is rarely reported to underlie pregnancy-related aortic dissection unless associated with aneurysm, complex congenital disease, Turner syndrome, or Marfan syndrome.21,35,36 In this IRAD series, 2 women with BAV had acute type A aortic dissection and neither knew the BAV diagnosis before aortic dissection. In 1 of these women with BAV, the aortic diameters at time of aortic dissection were 52 mm at the sinuses of Valsalva and 46 mm in the ascending aorta. Accounting for aortic expansion related to the acute aortic dissection, this patient likely had at least moderate preexisting aortic dilatation.37
Many women with pregnancy-related aortic dissection are not diagnosed with an underlying aortopathy condition. Of 90 maternal cardiovascular deaths in the Netherlands, 20 women died from aortic dissection: 18% had a connective tissue disease and 41% had a hypertensive disorder of pregnancy.38 Nonsyndromic HTADs due to pathogenic genetic variants explain many cases of aortic aneurysm and aortic dissection.8 Because these conditions lack outward recognizable features, the initial presentation often involves acute aortic dissection. ACTA2 gene mutations explain about 15% of nonsyndromic HTAD, and 20% of aortic dissection among women with ACTA2 mutations occurred during pregnancy.20 However, even when a clearly familial pattern of thoracic aneurysm disease exists, only 20% to 30% of individuals with nonsyndromic HTAD are found to have a mutation in a gene associated with aortic aneurysm.8 In this series, 31% of women did not have an aortopathy diagnosis reported. While some cases occurred before the recognition of many genetic variants, genetic testing in 2 patients with a family history of aneurysm did not demonstrate a variant. When genetic testing of the proband is negative, imaging of first-degree relatives is recommended, as up to 20% will have thoracic aortic disease.8
Hypertension or a hypertensive disorder of pregnancy may be associated with an increased risk of pregnancy-related aortic dissection10,38,39 and may trigger aortic dissection at relatively small diameters in those with HTADs.20 In the Nationwide Inpatient Sample, hypertension (18%) and eclampsia (4.5%) accompanied pregnancy-related aortic dissection.9 In the present series, 24% had hypertension and 1 woman developed preeclampsia. Only 1 woman with syndromic aortopathy and aortic dissection had hypertension. There were no aortopathy diagnoses reported in 4 women with hypertension and aortic dissection. However, no information was available regarding subsequent genetic testing. While hypertension-related aortic dissection may differ from those related to a genetic trigger, evaluation for HTAD remains important for women with aortic dissection in pregnancy even when hypertensive disorders coexist.
Maternal outcomes with pregnancy-related aortic dissection include mortality in 6.8% to 24.6% of cases.9,40,41 In this IRAD study, the hospital mortality rate was 3% (1/29). Aortic dissections may occur throughout pregnancy but most cases occur in the third trimester and post partum.1,17,30,40 Postpartum cases represent 20% to 71% of pregnancy-related aortic dissections among women with genetic aortopathy disorders.1,17,20,40 In the present study, 41% of women experienced aortic dissection in the third trimester and 44% post partum.
Pregnancy-related aortic dissection is most commonly due to a type A dissection (57%-80%).30,40,42,43 In a report of 258 pregnancies in women with Marfan syndrome, 4 of 5 aortic dissections were type B.44 Of women in the present series with Marfan syndrome whose time at type A aortic dissection was known, 66% occurred in the third trimester. Eight women in this series with type B aortic dissection had a syndromic aortopathy (6 with Marfan syndrome, 2 with Loeys-Dietz syndrome) and, in 63% of these cases, the aortic dissection occurred post partum.
Prior root replacement may influence distal aortic events in Marfan syndrome with late type B aortic dissection (unrelated to pregnancy) occurring in 9%.45 Three women in our cohort experiencing type B aortic dissection had previously undergone aortic root replacement. Pregnancy after root replacement in women with aortopathy carries a risk of type B aortic dissection.6,44,46 In the present series, most women with Marfan syndrome did not have significant enlargement of the descending aorta at the time of type B aortic dissection. Thus, aortic imaging surveillance may not accurately estimate the probability of pregnancy-related type B aortic dissection. Educating women with aortopathy and their health care professionals about risk for aortic dissection and typical symptoms may improve outcomes.
Women with aortopathies should receive multidisciplinary evaluation and counseling before pregnancy, including maternal and fetal risk.1,4,17,47 Genetic testing before pregnancy is recommended when the diagnosis of a specific HTAD is uncertain because risks of pregnancy may differ among aortopathy conditions. In women with HTAD, prepregnancy imaging of the entire aorta with magnetic resonance angiography is recommended.4 β-blocker use in pregnant women with aortopathy has not been systematically studied, but is recommended to lessen risk of aortic dissection during pregnancy.2,4,47 In our series, 8 women with connective tissue disease (6 with Marfan and 2 with Loeys-Dietz) experienced aortic dissection despite β-blocker use. During pregnancy, monitoring of the aortic root and ascending aorta with an echocardiogram every 4 to 12 weeks is recommended depending on individual circumstances. If the aortic arch and/or descending aorta is dilated, noncontrast magnetic resonance imaging is recommended.
For some women with significant aortic dilatation, prophylactic aortic root and/or ascending aortic replacement before pregnancy is recommended; for other women, pregnancy should be avoided.1,2,4 However, as evidenced by the 3 women in the present series who underwent previous ascending aortic surgery and developed type B aortic dissection related to pregnancy, prophylactic ascending aortic surgery may not guarantee a risk-free pregnancy.6,46
Limitations
The study had limitations. Retrospective data collection was limited by missingness. The IRAD is subject to incomplete or missing reports of events. Data on factors such as family history, phenotypic features, and pregnancy outcomes were not available for all patients. Aortic Z scores were not available for women in whom aortic diameters were known before aortic dissection. Adjusting aortic diameters to body size is predictive of aortic dissection risk in certain populations, including Turner syndrome, and may be particularly important in individuals of small body size. The aortic diameter during pregnancy and before aortic dissection was known in only 9 cases, and serial imaging data during pregnancy were not available. A detailed phenotype and genotype assessment for each woman was not collected on enrollment in IRAD. Lactation history was not collected. The diagnoses of aortopathy conditions were reported by individual experts in aortic dissection from each IRAD site. The diagnosis of Marfan syndrome was based on investigator reporting and, in some cases, included genetic results or confirmation of Ghent or revised Ghent criteria.48
During the earlier years of the IRAD, many currently recognized HTAD conditions had not yet been discovered and routine genetic testing was not available. It is possible that some women from the earliest years of the data collection considered to have Marfan syndrome could have been subsequently diagnosed with Loeys-Dietz syndrome. It is also possible that a higher percentage of women were later discovered to have an underlying HTAD. Because not all of the patients had follow-up at the IRAD sites, subsequent genetic testing could have been performed or may have identified nonsyndromic HTAD conditions. In addition, management decisions were left to the clinicians at the sites. It is possible that additional factors besides those recorded contributed to treatment decisions.
Conclusions
Acute aortic dissection related to pregnancy is a rare complication, occurring in only 0.3% of all dissections and in 1% of women in the IRAD database. However, among women younger than 35 years, 19% of acute aortic dissections occurred during pregnancy or within 12 weeks post partum. While type A aortic dissections related to pregnancy were associated with a dilated ascending aorta, type B aortic dissections were often not associated with significant descending thoracic aortic dilation. Aortopathy conditions are present in most women with pregnancy-related aortic dissection, but many were not recognized to have an aortopathy disorder until after acute aortic dissection had occurred. Recognizing women with predisposition to aortic dissection, counseling them before conception, and monitoring the aorta throughout pregnancy may lessen the risk of this rare complication of pregnancy and improve outcomes.
References
- 1.Wanga S, Silversides C, Dore A, de Waard V, Mulder B. Pregnancy and thoracic aortic disease: managing the risks. Can J Cardiol. 2016;32(1):78-85. doi: 10.1016/j.cjca.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 2.Hiratzka LF, Bakris GL, Beckman JA, et al. ; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine . 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010;121(13):e266-e369. [DOI] [PubMed] [Google Scholar]
- 3.Silversides CK, Kiess M, Beauchesne L, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: outflow tract obstruction, coarctation of the aorta, tetralogy of Fallot, Ebstein anomaly and Marfan’s syndrome. Can J Cardiol. 2010;26(3):e80-e97. doi: 10.1016/S0828-282X(10)70355-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. ; ESC Scientific Document Group . 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39(34):3165-3241. doi: 10.1093/eurheartj/ehy340 [DOI] [PubMed] [Google Scholar]
- 5.Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg. 1970;10(3):237-247. doi: 10.1016/S0003-4975(10)65594-4 [DOI] [PubMed] [Google Scholar]
- 6.Braverman AC, Moon MR, Geraghty P, Willing M, Bach C, Kouchoukos NT. Pregnancy after aortic root replacement in Loeys-Dietz syndrome: high risk of aortic dissection. Am J Med Genet A. 2016;170(8):2177-2180. doi: 10.1002/ajmg.a.37694 [DOI] [PubMed] [Google Scholar]
- 7.Renard M, Francis C, Ghosh R, et al. Clinical validity of genes for heritable thoracic aortic aneurysm and dissection. J Am Coll Cardiol. 2018;72(6):605-615. doi: 10.1016/j.jacc.2018.04.089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinard A, Jones GT, Milewicz DM. Genetics of thoracic and abdominal aortic diseases. Circ Res. 2019;124(4):588-606. doi: 10.1161/CIRCRESAHA.118.312436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sawlani N, Shroff A, Vidovich MI. Aortic dissection and mortality associated with pregnancy in the United States. J Am Coll Cardiol. 2015;65(15):1600-1601. doi: 10.1016/j.jacc.2014.12.066 [DOI] [PubMed] [Google Scholar]
- 10.Kamel H, Roman MJ, Pitcher A, Devereux RB. Pregnancy and the risk of aortic dissection or rupture: a cohort-crossover analysis. Circulation. 2016;134(7):527-533. doi: 10.1161/CIRCULATIONAHA.116.021594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nasiell J, Lindqvist PG. Aortic dissection in pregnancy: the incidence of a life-threatening disease. Eur J Obstet Gynecol Reprod Biol. 2010;149(1):120-121. doi: 10.1016/j.ejogrb.2009.10.029 [DOI] [PubMed] [Google Scholar]
- 12.Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014;130(12):1003-1008. doi: 10.1161/CIRCULATIONAHA.114.009029 [DOI] [PubMed] [Google Scholar]
- 13.Manalo-Estrella P, Barker AE. Histopathologic findings in human aortic media associated with pregnancy. Arch Pathol. 1967;83(4):336-341. [PubMed] [Google Scholar]
- 14.Habashi JP, MacFarlane EG, Bagirzadeh R, et al. Oxytocin antagonism prevents pregnancy-associated aortic dissection in a mouse model of Marfan syndrome. Sci Transl Med. 2019;11(490):eaat4822. doi: 10.1126/scitranslmed.aat4822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuperstein R, Cahan T, Yoeli-Ullman R, Ben Zekry S, Shinfeld A, Simchen MJ. Risk of aortic dissection in pregnant patients with the Marfan syndrome. Am J Cardiol. 2017;119(1):132-137. doi: 10.1016/j.amjcard.2016.09.024 [DOI] [PubMed] [Google Scholar]
- 16.Goland S, Elkayam U. Pregnancy and Marfan syndrome. Ann Cardiothorac Surg. 2017;6(6):642-653. doi: 10.21037/acs.2017.10.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roman MJ, Pugh NL, Hendershot TP, et al. ; GenTAC Investigators . Aortic complications associated with pregnancy in Marfan syndrome: she NHLBI National Registry of Genetically Triggered Thoracic Aortic Aneurysms and Cardiovascular Conditions (GenTAC). J Am Heart Assoc. 2016;5(8):e004052. doi: 10.1161/JAHA.116.004052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Hagen IM, van der Linde D, van de Laar IM, Muiño Mosquera L, De Backer J, Roos-Hesselink JW. Pregnancy in women with SMAD3 mutation. J Am Coll Cardiol. 2017;69(10):1356-1358. doi: 10.1016/j.jacc.2016.12.029 [DOI] [PubMed] [Google Scholar]
- 19.Loeys BL, Schwarze U, Holm T, et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med. 2006;355(8):788-798. doi: 10.1056/NEJMoa055695 [DOI] [PubMed] [Google Scholar]
- 20.Regalado ES, Guo DC, Estrera AL, Buja LM, Milewicz DM. Acute aortic dissections with pregnancy in women with ACTA2 mutations. Am J Med Genet A. 2014;164A(1):106-112. doi: 10.1002/ajmg.a.36208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silberbach M, Roos-Hesselink JW, Andersen NH, et al. ; American Heart Association Council on Cardiovascular Disease in the Young; Council on Genomic and Precision Medicine; and Council on Peripheral Vascular Disease . Cardiovascular health in Turner syndrome: a scientific statement from the American Heart Association. Circ Genom Precis Med. 2018;11(10):e000048. doi: 10.1161/HCG.0000000000000048 [DOI] [PubMed] [Google Scholar]
- 22.Braverman AC. Heritable thoracic aortic aneurysm disease: recognizing phenotypes, exploring genotypes. J Am Coll Cardiol. 2015;65(13):1337-1339. doi: 10.1016/j.jacc.2014.12.056 [DOI] [PubMed] [Google Scholar]
- 23.Pyeritz RE. Maternal and fetal complications of pregnancy in the Marfan syndrome. Am J Med. 1981;71(5):784-790. doi: 10.1016/0002-9343(81)90365-X [DOI] [PubMed] [Google Scholar]
- 24.Rossiter JP, Repke JT, Morales AJ, Murphy EA, Pyeritz RE. A prospective longitudinal evaluation of pregnancy in the Marfan syndrome. Am J Obstet Gynecol. 1995;173(5):1599-1606. doi: 10.1016/0002-9378(95)90655-X [DOI] [PubMed] [Google Scholar]
- 25.Lipscomb KJ, Smith JC, Clarke B, Donnai P, Harris R. Outcome of pregnancy in women with Marfan’s syndrome. Br J Obstet Gynaecol. 1997;104(2):201-206. doi: 10.1111/j.1471-0528.1997.tb11045.x [DOI] [PubMed] [Google Scholar]
- 26.Lind J, Wallenburg HC. The Marfan syndrome and pregnancy: a retrospective study in a Dutch population. Eur J Obstet Gynecol Reprod Biol. 2001;98(1):28-35. doi: 10.1016/S0301-2115(01)00314-1 [DOI] [PubMed] [Google Scholar]
- 27.Meijboom LJ, Vos FE, Timmermans J, Boers GH, Zwinderman AH, Mulder BJ. Pregnancy and aortic root growth in the Marfan syndrome: a prospective study. Eur Heart J. 2005;26(9):914-920. doi: 10.1093/eurheartj/ehi103 [DOI] [PubMed] [Google Scholar]
- 28.Pacini L, Digne F, Boumendil A, et al. Maternal complication of pregnancy in Marfan syndrome. Int J Cardiol. 2009;136(2):156-161. doi: 10.1016/j.ijcard.2008.04.035 [DOI] [PubMed] [Google Scholar]
- 29.Donnelly RT, Pinto NM, Kocolas I, Yetman AT. The immediate and long-term impact of pregnancy on aortic growth rate and mortality in women with Marfan syndrome. J Am Coll Cardiol. 2012;60(3):224-229. doi: 10.1016/j.jacc.2012.03.051 [DOI] [PubMed] [Google Scholar]
- 30.Kim SY, Wolfe DS, Taub CC. Cardiovascular outcomes of pregnancy in Marfan’s syndrome patients: a literature review. Congenit Heart Dis. 2018;13(2):203-209. doi: 10.1111/chd.12546 [DOI] [PubMed] [Google Scholar]
- 31.Goland S, Elkayam U. Cardiovascular problems in pregnant women with Marfan syndrome. Circulation. 2009;119(4):619-623. doi: 10.1161/CIRCULATIONAHA.104.493569 [DOI] [PubMed] [Google Scholar]
- 32.Minsart AF, Mongeon FP, Laberge AM, Morin F, Dore A, Leduc L. Obstetric and cardiac outcomes in women with Marfan syndrome and an aortic root diameter ≤ 45mm. Eur J Obstet Gynecol Reprod Biol. 2018;230:68-72. doi: 10.1016/j.ejogrb.2018.09.012 [DOI] [PubMed] [Google Scholar]
- 33.Jondeau G, Ropers J, Regalado E, et al. ; Montalcino Aortic Consortium . International Registry of Patients Carrying TGFBR1 or TGFBR2 mutations: results of the MAC (Montalcino Aortic Consortium). Circ Cardiovasc Genet. 2016;9(6):548-558. doi: 10.1161/CIRCGENETICS.116.001485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Braverman AC. Aortic involvement in patients with a bicuspid aortic valve. Heart. 2011;97(6):506-513. doi: 10.1136/hrt.2009.183871 [DOI] [PubMed] [Google Scholar]
- 35.McKellar SH, MacDonald RJ, Michelena HI, Connolly HM, Sundt TM III. Frequency of cardiovascular events in women with a congenitally bicuspid aortic valve in a single community and effect of pregnancy on events. Am J Cardiol. 2011;107(1):96-99. doi: 10.1016/j.amjcard.2010.08.061 [DOI] [PubMed] [Google Scholar]
- 36.Yuan SM. Bicuspid aortic valve in pregnancy. Taiwan J Obstet Gynecol. 2014;53(4):476-480. doi: 10.1016/j.tjog.2013.06.018 [DOI] [PubMed] [Google Scholar]
- 37.Rylski B, Branchetti E, Bavaria JE, et al. Modeling of predissection aortic size in acute type A dissection: More than 90% fail to meet the guidelines for elective ascending replacement. J Thorac Cardiovasc Surg. 2014;148(3):944-8.e1. doi: 10.1016/j.jtcvs.2014.05.050 [DOI] [PubMed] [Google Scholar]
- 38.Lameijer H, Schutte JM, Schuitemaker NWE, van Roosmalen JJM, Pieper PG; Dutch Maternal Mortality and Morbidity Committee . Maternal mortality due to cardiovascular disease in the Netherlands: a 21-year experience. Neth Heart J. 2020;28(1):27-36. doi: 10.1007/s12471-019-01340-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Thalmann M, Sodeck GH, Domanovits H, et al. Acute type A aortic dissection and pregnancy: a population-based study. Eur J Cardiothorac Surg. 2011;39(6):e159-e163. doi: 10.1016/j.ejcts.2010.12.070 [DOI] [PubMed] [Google Scholar]
- 40.Ma WG, Zhu JM, Chen Y, et al. Aortic dissection during pregnancy and postpartum in patients with Marfan syndrome: a 21-year clinical experience in 30 patients. Eur J Cardiothorac Surg. 2020;58(2):294-301. doi: 10.1093/ejcts/ezaa048 [DOI] [PubMed] [Google Scholar]
- 41.Banerjee A, Begaj I, Thorne S. Aortic dissection in pregnancy in England: an incidence study using linked national databases. BMJ Open. 2015;5(8):e008318. doi: 10.1136/bmjopen-2015-008318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mimoun L, Detaint D, Hamroun D, et al. Dissection in Marfan syndrome: the importance of the descending aorta. Eur Heart J. 2011;32(4):443-449. doi: 10.1093/eurheartj/ehq434 [DOI] [PubMed] [Google Scholar]
- 43.Schoenhoff FS, Jungi S, Czerny M, et al. Acute aortic dissection determines the fate of initially untreated aortic segments in Marfan syndrome. Circulation. 2013;127(15):1569-1575. doi: 10.1161/CIRCULATIONAHA.113.001457 [DOI] [PubMed] [Google Scholar]
- 44.Cauldwell M, Steer PJ, Curtis SL, et al. Maternal and fetal outcomes in pregnancies complicated by Marfan syndrome. Heart. 2019;105(22):1725-1731. doi: 10.1136/heartjnl-2019-314817 [DOI] [PubMed] [Google Scholar]
- 45.den Hartog AW, Franken R, Zwinderman AH, et al. The risk for type B aortic dissection in Marfan syndrome. J Am Coll Cardiol. 2015;65(3):246-254. doi: 10.1016/j.jacc.2014.10.050 [DOI] [PubMed] [Google Scholar]
- 46.Williams D, Lindley KJ, Russo M, Habashi J, Dietz HC, Braverman AC. Pregnancy after aortic root replacement in Marfan’s syndrome: a case series and review of the literature. AJP Rep. 2018;8(4):e234-e240. doi: 10.1055/s-0038-1675347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.MacCarrick G, Black JH III, Bowdin S, et al. Loeys-Dietz syndrome: a primer for diagnosis and management. Genet Med. 2014;16(8):576-587. doi: 10.1038/gim.2014.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010;47(7):476-485. doi: 10.1136/jmg.2009.072785 [DOI] [PubMed] [Google Scholar]