Abstract
Toscana virus (TOSV) is an arthropod-borne virus, transmitted to humans by phlebotomine sandflies. Although the majority of infections are asymptomatic, neuroinvasive disease may occur. We report three cases of neuroinvasive TOSV infection detected in Croatia. Two patients aged 21 and 54 years presented with meningitis, while a 22-year old patient presented with meningoencephalitis and right-sided brachial plexitis. Cerebrospinal fluid (CSF), serum, and urine samples were collected and tested for neuroinvasive arboviruses: tick-borne encephalitis, West Nile, Usutu, TOSV, Tahyna, and Bhanja virus. In addition, CSF and serum samples were tested for the anti-viral cytokine response. High titers of TOSV IgM (1000–3200) and IgG (3200−10,000) antibodies in serum samples confirmed TOSV infection. Antibodies to other phleboviruses (sandfly fever Sicilian/Naples/Cyprus virus) were negative. CSF samples showed high concentrations of interleukin 6 (IL-6; range 162.32−2683.90 pg/mL), interferon gamma (IFN-γ; range 110.12−1568.07 pg/mL), and IL-10 (range 28.08−858.91 pg/mL), while significantly lower cytokine production was observed in serum. Two patients recovered fully. The patient with a brachial plexitis improved significantly at discharge. The presented cases highlight the need of increasing awareness of a TOSV as a possible cause of aseptic meningitis/meningoencephalitis during summer months. Association of TOSV and brachial plexitis with long-term sequelae detected in one patient indicates the possibility of more severe disease, even in young patients.
Keywords: Toscana virus, neuroinvasive disease, clinical presentation, virology, immunology, Croatia
1. Background
Toscana virus (TOSV) is an arthropod-borne virus, transmitted to humans by phlebotomine sandflies (Phlebotomus spp.). The virus can be transmitted transovarially in vectors, but its animal reservoir has not been identified yet. Three genetic lineages of TOSV, A, B, and C, have been identified so far. Although the seroprevalence studies indicate that the TOSV is endemic in the Mediterranean countries, the virus remains neglected since clinical cases of TOSV infection are rarely reported [1]. Infection rates are highest in summer months when the sandflies are most active. The majority of human TOSV infections are asymptomatic or presented as a non-specific febrile disease. However, neuroinvasive disease (meningitis, meningoencephalitis, encephalitis) may also occur [2]. Although self-resolving in most cases, TOSV infection of the central nervous system (CNS) may be severe in some patients [3,4]. Some rare or atypical clinical presentations caused by TOSV such as afebrile meningoencephalitis with transient central facial paralysis, aphasia, and paresis are also reported [5,6]. Since there are no clear clinical grounds to differentiate TOSV infections from other viral neuroinvasive infections, laboratory confirmation is required [7]. Diagnosis of TOSV can be confirmed by detection of TOSV RNA and/or detection of specific antibodies [8].
In Croatia, there is only one published report on clinical cases of TOSV infection. In 2007−2008, five cases of TOSV meningitis were confirmed at the Croatian littoral [9]. However, high seroprevalence rates were detected in 2012 among residents of Croatian islands (53.9%) and coastal area (33.6%), respectively. In addition, seropositive persons were also detected in the Croatian mainland (6.1%) indicating that TOSV is widespread in Croatia [10]. Phylogenetic analyses confirmed the co-circulation of two genetic lineages (B and C) in the coastal Croatian regions [9,11]. Anti-viral cytokine response was not measured.
We analyzed clinical, virological, and immunological findings in three cases of TOSV neuroinvasive infection detected during the two consecutive transmission seasons (2018−2019).
2. Case Reports
Patients’ demographic, epidemiological, and clinical data are presented in Table 1.
Table 1.
Epidemiological and Clinical Characteristics of Patients with Toscana Neuroinvasive Infection.
| Characteristic | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age | 21 years | 22 years | 54 years |
| Gender | Male | Female | Male |
| Area of residence | Croatian littoral (Middle Dalmatia) |
Croatian mainland (worked at the Croatian littoral; Middle Dalmatia from July 2019) |
Croatian littoral (stayed on holiday in Middle Dalmatia) |
| Time of disease onset | Late August | Late August | Mid October |
| Clinical presentation | Meningitis | Meningoencephalitis | Meningitis |
| Clinical symptoms | Fever (up to 38 °C), headache, nausea, vomiting, photophobia, weakness | Fever (up to 38 °C), headache, nausea, vomiting, photophobia, dizziness, weakness, arthralgia, maculopapular rash, right-sided brachial plexitis | Severe headache, vomiting, weakness |
| Duration of symptoms | 5 days | 20 days | 5 days |
| Outcome | Recovered | Improved | Recovered |
Case 1: In late August 2018, a 21-year-old male patient, inhabitant of the Croatian littoral was admitted to the Infectious Disease Clinic, University Hospital Center Split with a two-day history of fever (up to 38 °C), headache, nausea, vomiting, photophobia, and weakness. Physical examination was normal. Routine laboratory tests were normal. Cerebrospinal fluid (CSF) analysis revealed a WBC count of 175 cells/mm3 (76% lymphocytes), a protein level of 0.447 g/L (reference range 0.17–0.37 g/L), and a glucose level of 3.78 mmol/L (reference range 2.5−3.3 mmol/L). Brain computed tomography (CT) was normal. The patient recovered fully within few days.
Case 2: In late August 2019, a 22-year old female patient was admitted to the Infectious Disease Clinic, University Hospital Center Split with an eight-day history of fever (up to 38 °C), headache, nausea vomiting, photophobia, dizziness, and weakness. On the 6th day after disease onset, a maculopapular rash developed with arthralgia (wrists and ankles). Physical examination showed neck stiffness and right upper arm neuralgic pain that limited arm mobility and was diagnosed as brachial plexitis. Routine laboratory tests were normal. CSF analysis revealed a WBC count of 102 cells/mm3 (76% lymphocytes), a protein level of 0.993 g/L, and a glucose level of 3.0 mmol/L. Brain magnetic resonance imaging (MRI) showed two hyperintensities in the left frontal lobe (unidentified bright objects). Right brachial plexus MRI finding was normal and there were no signs of denervation on electroneurography. After three-week hospitalization symptoms improved and the patient was discharged with moderate pain and improved upper arm mobility.
Case 3: In mid-October 2019, a 54-year-old male patient was admitted to the Infectious Disease Clinic, Clinical Hospital Center Rijeka with a one-day history of severe headache, vomiting, and weakness. A week before, during his stay on Solta Island, he noticed redness and swelling on his face after a mosquito bite. Physical examination showed neck stiffness. Routine laboratory tests were normal. CSF analysis revealed a WBC count of 123 cells/mm3 (86% lymphocytes), a protein level of 1.065 g/L, and a glucose level of 4.05 mmol/L. Brain CT and CT angiography were normal. The patient recovered fully within few days.
2.1. Virology Results
Since the CSF findings were suggestive of aseptic meningitis, arboviral etiology was suspected. CSF, serum, and urine samples were collected and tested for the presence of neuroinvasive arboviruses: tick-borne encephalitis virus (TBEV), West Nile (WNV), Usutu (USUV), TOSV, Tahyna (TAHV), and Bhanja virus (BHAV). To exclude cross-reactivity with other phleboviruses, samples were also tested for sandfly fever Naples (SFNV), Sicilian (SFSV), and Cyprus (SFVC) virus. Serological tests were performed using commercial enzyme-linked immunosorbent assays (ELISA; TBEV, WNV, USUV, Euroimmun, Lübeck, Germany) or indirect immunofluorescence assays (IFA; sandfly fever mosaic, Euroimmun, Lübeck, Germany). In addition, CSF and serum samples were tested for the presence of viral RNA: TBEV [12], WNV [13], USUV [14], TOSV [15], TAHV [16], and BHAV [17].
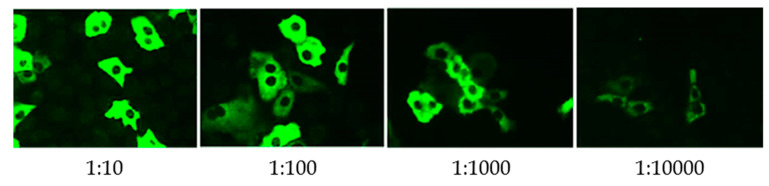
Virology results are presented in Table 2. High titers of both IgM and IgG to TOSV in serum samples indicated acute TOSV infection (Figure 1). TOSV RNA was not detected in CSF, serum, and urine samples by use of highly sensitive and specific real-time reverse transcriptase polymerase chain reaction (RT-qPCR) [15]. Antibodies to other phleboviruses were negative.
Table 2.
Virology Results in Patients with Toscana Neuroinvasive Infection.
| Virus | CASE 1 | CASE 2 | CASE 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ELISA IgM a/IgG b |
IFA IgM/IgG c | RT-qPCR | ELISA IgM a/IgG b | IFA IgM/IgG c | RT-qPCR | ELISA IgM a/IgG b | IFA IgM/IgG c | RT-qPCR | |
| TBEV | NegNeg | NT | Neg | Neg/Neg | NT | Neg | Neg/Neg | NT | Neg |
| WNV | Neg/Neg | NT | Neg | Neg/Neg | NT | Neg | Neg/Neg | NT | Neg |
| USUV | NT/Neg | NT | Neg | NT/Neg | NT | Neg | NT/Neg | NT | Neg |
| SFSV | NT | Neg/Neg | NT | NT | Neg/Neg | NT | NT | Neg/Neg | NT |
| SFNV | NT | Neg/Neg | NT | NT | Neg/Neg | NT | NT | Neg/Neg | NT |
| SFCV | NT | Neg/Neg | NT | NT | Neg/Neg | NT | NT | Neg/Neg | NT |
| TOSV | NT | 1000/3200 | Neg | NT | 3200/3200 | Neg | NT | 1000/10,000 | Neg |
| TAHV | NT | NT | Neg | NT | NT | Neg | NT | NT | Neg |
| BHAV | NT | NT | Neg | NT | NT | Neg | NT | NT | Neg |
TBEV = tick-borne encephalitis virus; WNV = West Nile virus; USUV = Usutu virus; SFSV = sandfly fever Sicilian virus; SFNV = sandfly fever Naples virus; SFCV = sandfly fever Cyprus virus; TOSV = Toscana virus; TAHV = Tahyna virus; BHAV = Bhanja virus; NT = not tested; a ratio < 0.8 negative, 0.8−1.1 borderline, ≥ 1.1 positive; b RU/mL < 16 negative, 16−22 borderline, ≥ 22 positive; c titer < 100 negative.
Figure 1.
Toscana virus IgG antibodies detected using indirect immunofluorescence assay in a patient (case 3) with neuroinvasive infection.
2.2. Anti-Viral Cytokine Response
To analyze the anti-viral cytokine response, a commercial multiplex assay was used for simultaneous detection of 13 cytokines in the CSF and serum samples: IL-5,IL-13, IL-2, IL-6, IL-9, IL-10, IFN-γ, TNF-α, IL-17A, IL-17F, IL-4, IL-21, and IL-22 (LEGENDplex™ Human Anti-Virus Response Panel, BioLegend, San Diego, CA, USA). In the CSF samples of all three cases, high concentrations of IL-6 (range 162.32−2683.90 pg/mL), IFN-γ (range 110.12−1568.07 pg/mL), and IL-10 (range 28.08−858.91 pg/mL) were found. Two samples (cases 2 and 3) showed elevated levels of IL-22 (28.49 and 45.24 pg/mL, respectively) as well, while one sample (case 3) showed elevated level of IL-13 (40.05 pg/mL). In serum samples, concentrations of cytokines were significantly lower than in CSF (Table 3).
Table 3.
Anti-Viral Cytokine Levels in Patients with Toscana Virus Neuroinvasive Infection.
| Cytokine (pg/mL) | Case 1 | Case 2 | Case 3 | Detection Limits (Minimum Detectable Concentrations + 2xSD, pg/mL) | |||
|---|---|---|---|---|---|---|---|
| Serum | CSF | Serum | CSF | Serum | CSF | ||
| IL-5 | Neg | Neg | 5.35 | Neg | Neg | 3.20 | 1.2 + 1.3 |
| IL-13 | Neg | Neg | 18.68 | Neg | 71.25 | 40.05 | 1.4 + 0.7 |
| IL-2 | 5.92 | Neg | Neg | Neg | Neg | 35.01 | 1.4 + 0.4 |
| IL-6 | Neg | 162.32 | 8.35 | 517.32 | 9.29 | 2683.90 | 1.0 + 0.8 |
| IL-9 | 5.51 | 5.01 | 4.80 | 2.13 | Neg | 7.62 | 1.7 + 1.4 |
| IL-10 | Neg | 199.99 | Neg | 28.08 | Neg | 858.91 | 0.7 + 0.4 |
| IFN-γ | Neg | 110.12 | 28.23 | 206.92 | Neg | 1568.07 | 1.1 + 0.7 |
| TNF-α | 13.75 | Neg | Neg | Neg | Neg | Neg | 0.7 + 0.5 |
| IL-17A | Neg | Neg | 32.94 | Neg | Neg | Neg | 1.9 + 0.6 |
| IL-17F | 15.21 | Neg | Neg | Neg | Neg | Neg | 0.8 + 0.7 |
| IL-4 | 18.43 | Neg | 5.97 | Neg | Neg | Neg | 1.0 + 0.8 |
| IL-21 | 78.13 | Neg | 10.98 | Neg | Neg | Neg | 6.0 + 3.0 |
| IL-22 | Neg | Neg | Neg | 28.49 | Neg | 45.24 | 1.5 + 0.5 |
3. Discussion
In Croatia, TBEV and WNV are the most commonly detected neuroinvasive arboviruses. Sporadic cases of USUV neuroinvasive disease were also reported [18,19,20]. So far, only few cases of TOSV infection are diagnosed and it is not a routine consideration in the differential diagnosis of viral meningoencephalitis. Since the TOSV seroprevalence rates are high in the inhabitants of the Croatian littoral, the true prevalence of the disease is probably underestimated.
Cases presented in this report developed symptoms of neuroinvasive disease in late August and mid-October. Taking into account the area of residence with documented high seropositivity to TOSV [10] and arbovirus transmission season, TOSV infection was suggested. In all patients, infection was confirmed by detection of high titers of both TOSV IgM and IgG antibodies, while qRT-PCR was negative. The results of a recently published study showed that specific antibody response develops rapidly in neuroinvasive TOSV infection. TOSV IgM and IgG antibodies were present at the onset of symptoms in 100% of patients [21], which could explain the negative RT-qPCR result in serum and CSF samples of the patients presented in this report.
Data on cytokine levels during TOSV infection are scarce [22,23]. In this study, a very high levels of IL-6, IFN-γ, and IL-10 were found in all three CSF samples, while in serum samples levels of cytokines were significantly lower. Moderate increase of IL-6, IFN-γ, and IL-10 was found in two and one serum samples, respectively. In one recently published study, increased levels of IFN-γ and IL-22 were found in serum samples of patients with TOSV infection while CSF samples were not available for testing [22]. None of the serum samples in the present study showed elevated levels of IL-22, however, elevated levels were detected in two CSF samples. In the other study, no difference was observed in the plasma levels of IL-6, IL-10, TNF-α, IFN-α, and IFN-γ between TOSV-infected patients and controls, however, levels of cytokines in the CSF was significantly higher in TOSV-infected patients. No difference was found in the CSF cytokine production in patients with meningitis and meningoencephalitis [23]. Similarly, our results showed no association of inflammatory markers in the CSF and disease severity. A high intrathecal production of IL-6, IFN-γ, and IL-10 suggests the activation of a selective antiviral and anti-inflammatory response in the CNS of TOSV-infected patients which is in correlation with observations in some other neuroinvasive arboviral infections (flaviviruses) where a strong inflammatory immune response in the CNS was found [23,24,25].
Two patients in this report presented with meningitis, while one patient presented with meningoencephalitis and brachial plexitis. Although the etiology of brachial plexitis is unknown, a viral etiology (association with recent viral infection or vaccination) was proposed. Viral causes reported so far include cytomegalovirus, coxsackieviruses, varicella-zoster virus, Epstein–Barr virus, and parvovirus B19. Recent viral infection has been associated to precede the development of the disease in 25−55% of patients [26,27].
Although clinical outcome of TOSV neuroinvasive disease is usually favorable with no long-term sequelae, compared to other arboviral infections such as TBEV and WNV, severe and fatal encephalitis was reported in elderly [28]. Despite a full recovery within a few weeks in most cases of TOSV infection [29], as in the two patients reported in this study, the presented cases highlight the need of increasing awareness of TOSV as a possible cause of aseptic meningitis/meningoencephalitis. The long-term sequelae (brachial plexitis) detected in one patient indicates the possibility of more severe disease, even in young patients.
Due to the similar clinical presentation and seasonal distribution, TOSV infection can be misdiagnosed with some other neuroinvasive viral infections such as TBEV, WNV, USUV [18,19,20], and enteroviruses [30]. In countries where several arboviruses co-circulate, TOSV should be included in the differential diagnosis of aseptic meningitis/meningoencephalitis, especially during the summer months.
4. Conclusions
Clinicians should consider TOSV in differential diagnosis of neuroinvasive disease during the arbovirus transmission season. Since Croatia is a touristic country, TOSV should also be considered as one of the viral pathogens causing aseptic meningitis in travelers returning from this area.
Acknowledgments
The authors thank Ljiljana Milasincic, Snjezana Artl, and Ljiljana Antolasic for technical assistance. The authors also thank the patients for informed consent. The Ethics Committee of the Croatian Institute of Public Health approved the study (Approval No. 80-1092/1-16).
Author Contributions
Conceptualization, T.V.-C. and S.Z.-L.; methodology, V.S. (Vladimir Savic), I.G., L.G., and V.S. (Vladimir Stevanovic); investigation, D.L., I.T., S.K., I.I., I.S., and M.B.; writing—original draft preparation, T.V.-C., S.Z.-L., I.T., S.K., and I.I., writing—review and editing, L.B.; all authors have read and agreed to the published version of the manuscript.
Funding
The study was supported by the Croatian Science Foundation, project No. 2016-06-7456: Prevalence and molecular epidemiology of emerging and re-emerging neuroinvasive arboviral infections in Croatia; CRONEUROARBO (to TVC) and by the by the European Virus Archive Global (EVA-GLOBAL) project that has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No. 871029.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- 1.Ayhan N., Prudhomme J., Laroche L., Bañuls A.L., Charrel R.N. Broader Geographical Distribution of Toscana Virus in the Mediterranean Region Suggests the Existence of Larger Varieties of Sand Fly Vectors. Microorganisms. 2020;8:114. doi: 10.3390/microorganisms8010114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cusi M.G., Savellini G.G., Zanelli G. Toscana virus epidemiology: From Italy to beyond. Open Virol. J. 2010;4:22–28. doi: 10.2174/1874357901004010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuhn J., Bewermeyer H., Hartmann-Klosterkoetter U., Emmerich P., Schilling S., Valassina M. Toscana virus causing severe meningoencephalitis in an elderly traveler. J. Neurol. Neurosurg. Psychiatry. 2005;76:1605–1606. doi: 10.1136/jnnp.2004.060863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papa A., Paraforou T., Papakonstantinou I., Pagdatoglou K., Kontana A., Koukoubani T. Severe encephalitis caused by Toscana virus, Greece. Emerg. Infect. Dis. 2014;20:1417–1419. doi: 10.3201/eid2008.140248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marlinge M.C., Crespy L., Zandotti C., Piorkowski G., Kaphan E., Charrel R.N., Ninove L. Afebrile meningoencephalitis with transient central facial paralysis due to Toscana virus infection, south-eastern France. Euro Surveill. 2014;19:20974. doi: 10.2807/1560-7917.ES2014.19.48.20974. [DOI] [PubMed] [Google Scholar]
- 6.Sanbonmatsu-Gámez S., Pérez-Ruiz M., Palop-Borrás B., Navarro-Marí J.M. Unusual manifestation of Toscana virus infection, Spain. Emerg. Infect. Dis. 2009;15:347–348. doi: 10.3201/eid1502.081001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayhan N., Charrel R.N. An update on Toscana virus distribution, genetics, medical and diagnostic aspects. Clin. Microbiol. Infect. 2020;26:1017–1023. doi: 10.1016/j.cmi.2019.12.015. [DOI] [PubMed] [Google Scholar]
- 8.Cusi M.G., Savellini G.G. Diagnostic tools for Toscana virus infection. Expert Rev. Anti-Infect. 2011;9:799–805. doi: 10.1586/eri.11.54. [DOI] [PubMed] [Google Scholar]
- 9.Punda-Polić V., Mohar B., Duh D., Bradarić N., Korva M., Fajs L., Saksida A., Avšič-Županc T. Evidence of an autochthonous Toscana virus strain in Croatia. J. Clin. Virol. 2012;55:4–7. doi: 10.1016/j.jcv.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 10.Punda-Polić V., Jerončić A., Mohar B., Šiško Kraljević K. Prevalence of Toscana virus antibodies in residents of Croatia. Clin. Microbiol. Infect. 2012;18:E200–E203. doi: 10.1111/j.1469-0691.2012.03840.x. [DOI] [PubMed] [Google Scholar]
- 11.Ayhan N., Alten B., Ivovic V., Martinkovic F., Kasap O.E., Ozbel Y., de Lamballerie W., Charrel R.N. Cocirculation of two Lineages of Toscana Virus in Croatia. Front. Public Health. 2017;5:336. doi: 10.3389/fpubh.2017.00336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwaiger M., Cassinotti P. Development of a quantitative real-time RT-PCR assay with internal control for the laboratory detection of tick-borne encephalitis virus (TBEV) RNA. J. Clin. Virol. 2003;27:136–145. doi: 10.1016/S1386-6532(02)00168-3. [DOI] [PubMed] [Google Scholar]
- 13.Tang Y., Anne Hapip C., Liu B., Fang C.T. Highly sensitive TaqMan RT-PCR assay for detection and quantification of both lineages of West Nile virus RNA. J. Clin. Virol. 2003;36:177–182. doi: 10.1016/j.jcv.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Nikolay B., Weidmann M., Dupressoir A., Faye O., Boye C.S., Diallo M., Sall A.A. Development of a Usutu virus specific real-time reverse transcription PCR assay based on sequenced strains from Africa and Europe. J. Virol. Methods. 2014;197:51–54. doi: 10.1016/j.jviromet.2013.08.039. [DOI] [PubMed] [Google Scholar]
- 15.Weidmann M., Sanchez-Seco M.P., Sall A.A., Ly P.O., Thiongane Y., Lô M.M., Schley H., Hufert F.T. Rapid detection of important human pathogenic Phleboviruses. J. Clin. Virol. 2008;41:138–142. doi: 10.1016/j.jcv.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Li H., Cao Y.X., He X.X., Fu S.H., Lyu Z., He Y., Gao X.Y., Liang G.D., Wang H.Y. Real-time RT-PCR Assay for the detection of Tahyna virus. Biomed. Environ. Sci. 2015;28:374–377. doi: 10.3967/bes2015.052. [DOI] [PubMed] [Google Scholar]
- 17.Matsuno K.M., Weisend C., Travassos da Rosa A.P., Anzick S.L., Dahlstrom E., Porcella S.F., Dorward D.W., Yu X.J., Tesh R.B., Ebihara H. Characterization of the Bhanja serogroup viruses (Bunyaviridae): A novel species of the genus Phlebovirus and its relationship with other emerging tick-borne phleboviruses. J. Virol. 2013;87:3719–3728. doi: 10.1128/JVI.02845-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ilic M., Barbic L., Bogdanic M., Tabain I., Savic V., Kosanovic Licina M.L., Kaic B., Jungic A., Vucelja M., Angelov V., et al. Tick-borne encephalitis outbreak following raw goat milk consumption in a new micro-location, Croatia, June 2019. Ticks Tick Borne Dis. 2020;11:101513. doi: 10.1016/j.ttbdis.2020.101513. [DOI] [PubMed] [Google Scholar]
- 19.Vilibic-Cavlek T., Kaic B., Barbic L., Pem-Novosel I., Slavic-Vrzic V., Lesnikar V., Kurecic-Filipovic S., Babic-Erceg A., Listes E., Stevanovic V., et al. First evidence of simultaneous occurrence of West Nile virus and Usutu virus neuroinvasive disease in humans in Croatia during the 2013 outbreak. Infection. 2014;42:689–695. doi: 10.1007/s15010-014-0625-1. [DOI] [PubMed] [Google Scholar]
- 20.Vilibic-Cavlek T., Savic V., Sabadi D., Peric L., Barbic L., Klobucar A., Miklausic B., Tabain I., Santini M., Vucelja M., et al. Prevalence and molecular epidemiology of West Nile and Usutu virus infections in Croatia in the “One Health” context, 2018. Transbound Emerg. Dis. 2019;66:1946–1957. doi: 10.1111/tbed.13225. [DOI] [PubMed] [Google Scholar]
- 21.Pierro A., Ficarelli S., Ayhann N., Morini S., Raumer L., Bartoletti M., Mastroianni A., Prati F., Schivazappa S., Cenni P., et al. Characterization of antibody response in neuroinvasive infection caused by Toscana virus. Clin. Microbiol. Infect. 2017;23:868–873. doi: 10.1016/j.cmi.2017.03.017. [DOI] [PubMed] [Google Scholar]
- 22.Rauch J., Zammarchi L., Corti G., Bartoloni A., Schlaphof A., Schmidt-Chanasit J., Tappe D. Serum cytokine and chemokine changes during Toscana virus meningitis. Med. Microbiol. Immunol. 2019;208:727–730. doi: 10.1007/s00430-019-00611-y. [DOI] [PubMed] [Google Scholar]
- 23.Varani S., Gelsomino F., Bartoletti M., Viale P., Mastroianni A., Briganti E., Ortolani P., Albertini F., Calzetti C., Prati F., et al. Meningitis caused by Toscana virus is associated with strong antiviral response in the CNS and altered frequency of blood antigen-presenting cells. Viruses. 2015;7:5831–5843. doi: 10.3390/v7112909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li H., Li Y., Wen B., Zhang J., Wang C., Song Z., Li S., Qu X., Huang R., Liu W. Dengue virus and Japanese encephalitis virus infection of the central nervous system share similar profiles of cytokine accumulation in cerebrospinal fluid. Cent. Eur. J. Immunol. 2017;42:218–222. doi: 10.5114/ceji.2017.69366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bogovič P., Lusa L., Korva M., Lotrič-Furlan S., Resman-Rus K., Pavletič M., Avšič-Županc T., Strle K., Strle F. Inflammatory immune responses in patients with tick-borne encephalitis: Dynamics and association with the outcome of the disease. Microorganisms. 2019;7:E514. doi: 10.3390/microorganisms7110514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miller J.D., Pruitt S., McDonald T.J. Acute brachial plexus neuritis: An uncommon cause of shoulder pain. Am. Fam. Physician. 2000;62:2067–2072. [PubMed] [Google Scholar]
- 27.Torres M.O., Gudlavalleti A., Mesfin F.B. Brachial Plexitis (Parsonage Turner Syndrome, Brachial Neuropathy, Brachial Radiculitis) [(accessed on 12 August 2020)]; [Updated 2020 July 19] Available online: https://www.ncbi.nlm.nih.gov/books/NBK448114/
- 28.Bartels S., de Boni L., Kretzschmar H.A., Heckmann J.G. Lethal encephalitis caused by the Toscana virus in an elderly patient. J. Neurol. 2012;259:175–177. doi: 10.1007/s00415-011-6121-y. [DOI] [PubMed] [Google Scholar]
- 29.Charrel R.N., Bichaud L., de Lamballerie X. Emergence of Toscana virus in the Mediterranean area. World J. Virol. 2012;1:135–141. doi: 10.5501/wjv.v1.i5.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cantu R.M., Das J.M. Viral Meningitis. [(accessed on 12 August 2020)]; Available online: https://www.ncbi.nlm.nih.gov/books/NBK545217/