Abstract
Purpose
To describe the technique of traumatic cyclodialysis cleft repair in the management of hypotony maculopathy using anterior placement of encircling scleral band-buckle.
Observations
A 51-year-old male who had sustained blunt trauma in the left eye two months prior to presentation in the clinics, presented with visual acuity of 20/200, a persistent cyclodialysis cleft with hypotony maculopathy and intraocular pressure (IOP) of 6 mm Hg. A silicone band-buckle was passed 360°; with its anterior edge hugging the insertion of rectus muscles along the ‘spiral of Tillaux’. Post-operative course showed closure of the cleft with an IOP of 20 mm Hg at day 4. Patient underwent cataract extraction with intraocular lens implantation at two months and improved to 20/40 at the last follow up visit with a normal IOP.
Conclusion and Importance
We successfully managed a case of hypotony maculopathy due to persistent cyclodialysis cleft using a circumferential band buckle. We avoided the use of cryopexy to avoid the potential risk of inflammation - further worsening choroidal effusion and rare occurrence of suprachoroidal hemorrhage.
Keywords: Blunt trauma, Cyclodialysis cleft, Hypotony maculopathy, Band buckle, Traumatic cataract
1. Introduction
Cyclodialysis cleft arises from the focal disinsertion of the meridional ciliary muscle fibers from the scleral spur.1 It may be traumatic or iatrogenic, i.e. following various anterior segment surgeries. While small clefts may close spontaneously, persistent clefts may result in several complications. The cyclodialysis cleft forms an abnormal secondary pathway for the drainage of aqueous humor into the suprachoroidal space.1,2 A combination of increased uveoscleral outflow and decreased aqueous secretion by the detached ciliary body, can cause persistent hypotony eventually leading to maculopathy. Two definitions of hypotony maculopathy exist: (1) statistical hypotony maculopathy is defined as intraocular pressure (IOP) below 6.5 mmHg, and (2) clinical hypotony maculopathy is IOP low enough to cause vision loss.3
Chronic hypotony can result in choroidal effusion, disc edema, shallowing of the anterior chamber, cataract, retinal and choroidal folds, vascular tortuosity, hypotony maculopathy, cystoid macular edema, cataract, relative hyperopia or loss of vision.4
Diagnosis is confirmed by direct visualization of cyclodialysis cleft on gonioscopy, ultrasound biomicroscopy (UBM) or anterior segment optical coherence tomography (AS-OCT).5,6
Several management techniques have been described in the literature for cyclodialysis cleft repair. These include suture cyclopexy,7 scleral buckling,8 vitrectomy with gas tamponade,9 ciliochoroidal cryotherapy,10 argon laser photocoagulation,11 trans-scleral YAG or diode laser cyclophotocoagulation and diode laser endophotocoagulation.12
The goal of treatment is to cause anatomical closure of the cleft and restore the apposition of the ciliary body to the sclera in order to prevent enhanced aqueous outflow and regain ciliary body functioning. This would result in improvement of visual acuity and prevent further complications.
We report a case of traumatic cyclodialysis cleft with hypotony maculopathy and posterior subcapsular cataract managed by anterior placement of 240-style silicone band-buckle encriclage, followed by successful cataract surgery and in the bag placement of intra-ocular lens.
2. Case report
A 51-year-old male presented with reduced vision in the left eye (OS) for two months, which occurred immediately following blunt trauma to the eye. The patient had sought medical care elsewhere, where he was diagnosed with hyphema in OS and was treated with cycloplegics and oral and topical steroids. Patient was a known hypertensive but had no history of any other systemic illness.
On ocular examination, BCVA was 20/20 in the right eye (OD) and 20/200 OS with no improvement on pinhole. Intraocular pressure (IOP) was 6 mm of Hg (OS) and 16 mm of Hg OD. Central corneal thickness was slightly elevated at 572 μm indicating corneal edema in OS.
Slit lamp examination revealed no abnormal findings in OD. There was a traumatic posterior subcapsular rosette cataract in OS. Slit lamp retro-illumination showed sectoral iridodialysis of 1.5 clock hours from 6:30 to 8 o'clock in OS (Fig. 1A). Fundus examination (OS) and color fundus photography showed vascular tortuosity. Increased choroidal thickness was documented on USG B-scan which was suggestive of generalized choroidal effusion. The posterior pole and disc appeared blurry due to the presence of traumatic cataract; the retina was attached (Fig. 1B).
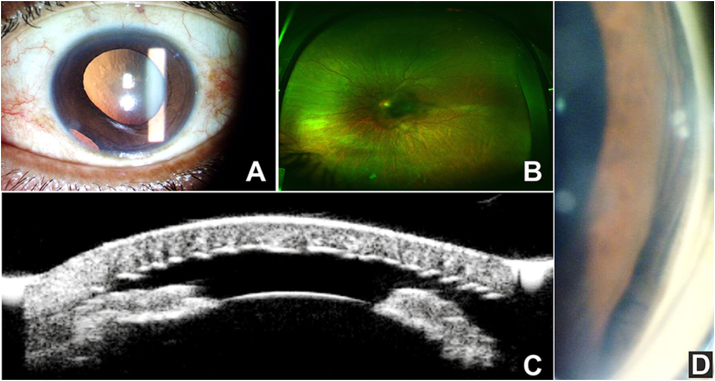
Fig. 1.
Preoperative slit lamp photo showing the iridodialysis and cataract (A), fundus picture demonstrating disc edema and vascular tortuosity (B), ultrasound biomicroscopy and gonioscopy showing the cyclodialysis cleft (C, D).
Ultrasound biomicroscopy (UBM) of OS revealed a cyclodialysis cleft (Fig. 1C). Gonioscopy of OD was normal. Gonioscopy of OS revealed the presence of iris root detachment corresponding to the iridodialysis seen on anterior segment examination and the presence of ciliary body detachment from the scleral spur (Fig. 1D). A diagnosis of traumatic persistent cyclodialysis cleft with hypotony maculopathy and traumatic posterior subcapsular rosette cataract OS was made. Since the IOP had not improved, even after two months of medical management, surgical options were considered.
2.1. Surgical technique
Relative to the equatorial plane, anterior placement of a scleral band-buckle encirclage was performed in OS. A 360° conjunctival peritomy was performed under local peribulbar anesthesia. All four rectus muscles were bridled, and scleral surface was examined in all four quadrants after clearing away Tenon's capsule. A 240-style silicone band (Labtician®) was used, whose posterior edge was placed at 9 mm from limbus (to support the ciliary body in its posterior extent) and anteriorly hugging the insertion of all four rectus muscles along the ‘spiral of Tillaux’. Band was secured using 5-0 braided polypropylene (Dacron®) mattress sutures in each quadrant. Band was tied end-to-end in the lower-nasal quadrant; care was taken not to over-tighten the band inadvertently since the eye was already in the state of hypotony. Intraocular pressure was digitally assessed, and the conjunctiva was closed using 7–0 coated polyglactin (Vicryl®) sutures.
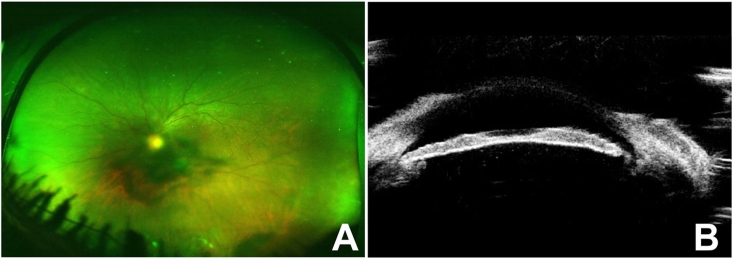
On first post-operative day, IOP improved to 14 mm of Hg. BCVA remained at 20/200 in OS; disc edema and ILM-folds were still present (Fig. 2A). On fourth post-operative day, IOP in OS improved to 20 mm of Hg. Dynamic UBM-scan showed the presence of scleral band indentation at the location of cyclodialysis cleft, thereby assisting closure of cleft (Fig. 2B). The patient was followed up at two months and showed stable clinical course in post-operative period. However, the visual acuity did not improve due to presence of cataract. Cataract surgery with successful implantation of intra-ocular lens was performed two months after the band-encirclage surgery, which led to a final visual acuity of 20/40. We did not undertake iridodialysis repair since it was small and visually insignificant and additional surgical manipulation could thus be avoided.
Fig. 2.
Postoperative fundus photograph (A) and ultrasound biomicroscopy demonstrating closure of the cyclodialysis cleft (B).
3. Discussion
Cyclodialysis cleft is an uncommon ophthalmic finding that can be challenging to diagnose and treat. Spontaneous closure of cyclodialysis clefts and subsequent resolution of ocular hypotony is rare and occurs mostly in smaller clefts. Prolonged hypotony can lead to irreversible maculopathy, fibrosis, vision loss and eventually phthisis bulbi. Furthermore, in eyes with cyclodialysis cleft and persistent hypotony maculopathy, closure of the cleft is indicated in order to normalize intraocular pressure, restore visual acuity and prevent permanent vision loss.
Conservative management includes treatment with topical 1% atropine for 6–8 weeks. Atropine relaxes the ciliary muscle and allows for apposition of the detached meridional fibers to the scleral spur. When conservative medical treatment fails, management with laser photocoagulation, cryotherapy, or trans-scleral diathermy are often attempted. These methods are reported to aid in the closure of small clefts by inducing a localised inflammatory reaction and scarring.11
Surgical repair is the option of choice for larger clefts, where conservative medical management, cryotherapy or photocoagulation have proven ineffective.13,14 However, due to the lack of published data on outcome following cyclodialysis cleft repair, a surgical gold standard for management of such cases has not been established and varies from case to case depending on surgeon experience and case profile.
Among various surgical interventions, direct cyclopexy through a partial- or full-thickness limbal scleral flap has been used. Limbal based scleral flap technique can be either a thick lamellar flap or double-lamellar limbus-based scleral flap in the area of the cyclodialysis cleft extending 3–4 mm posterior to the limbus. Surgeon can directly visualise the cleft after incising sclera up to 1 mm posterior to the scleral spur and hence ciliary body/muscles can be sutured to the scleral spur and/or to the deep scleral flap, depending on type of flap technique used, using 9–0 or 10–0 nylon sutures.
Kuchle reported successful cyclodialysis cleft closure in 28 of 29 cases following direct cyclopexy using full-thickness scleral flap.7 Agrawal and Shah reported successful cleft closure in 11 of 12 patients who underwent direct cyclopexy using a partial-thickness technique.14 In patients that have direct surgical cyclopexy, closure often results in painful post-operative spikes in IOP (up to 70 mm of Hg) and can be high enough to dehisce the surgical wound if not tightly secured.1,7,14 In most cases, the pressure resolves and long-term anti-glaucoma medication is not required.
Unsuccessful cases of cleft repair continue to be reported. Additionally, intraocular surgery presents with risks of hemorrhage, infection and retinal detachment.15 A number of reports propose several alternative approaches to the traditional surgical management. Mandava et al. reported successful closure of a cyclodialysis cleft via anterior buckling. In this particular method, a set of mattress sutures to hold two anterior sponges in places above the cleft were used.8
Recently, Sood et al.16 compared encirclage and cryotherapy with argon-laser cyclopexy and observed that both groups had similar anatomical and functional successes. The authors have not reported any major complications in their study; we however avoided the use of cryopexy in order to prevent inducing inflammation, which could potentially result in worsening of choroidal effusion, ultimately resulting in frank choroidal detachment. Also, freeze-thaw cycle of cryo-probe needs to be done extremely carefully in an eye with hypotony and choroidal effusion because the risk of suprachoroidal and sub-retinal hemorrhage is real and can be devastating in an already compromised eye.17, 18, 19
Hence, the index case was managed differently wherein only an encircling scleral band explant was used for appositional closure of the cyclodialysis cleft and use of cryopexy was altogether avoided in an eye with hypotony and choroidal effusion.
Additionally, the possibility of conjunctival erosion and explant extrusion would be lesser compared to sponges since the silicone-band encirclage was performed beyond and beneath the rectus muscles insertion and was adequately covered by a layer of conjunctiva and Tenon's capsule. The silicone material of the band makes it less predisposed to infection and conjunctival or scleral erosion. This technique also finds a potential utility in closing larger cyclodialysis clefts where placement of larger sponges would be difficult and direct cyclopexy would have an increased potential for complications. Another benefit of band encirclage is the effortless management of clefts located in the same clock hour as the rectus muscle insertion, wherein the sponge placement may be technically difficult.
The limitation of this technique may be the requirement of an experienced surgeon since the titration of the band tightening is essential to ensure cleft apposition and prevent severe IOP rise post-operatively and hour-glass deformation of globe resulting in myopic shift. This is due to inadvertently excessive band tightening in an eye with hypotony. Inferonasal location of the cleft itself seems a favourable factor for the successful outcome of this case with anterior placement of encirclage, however other location of the cleft might have affected the final outcomes.
4. Conclusion
An encircling silicone band could be considered a safe and effective alternative surgical treatment modality for traumatic, non-resolving cyclodialysis cleft with persistent hypotony. This technique may form the first line of surgical management after unsuccessful medical management. Invasive intraocular surgery may be undertaken in recalcitrant cases which fail to respond to extraocular procedures. However, larger comparative studies need to be undertaken in future in order to confirm these findings.
Patient's consent
Consent to publish the case report was obtained. This report does not contain any personal information that could lead to the identification of the patient.
Funding
No funding or grant support
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The authors have no financial disclosures or conflicts of interest.
Acknowledgements
None.
References
- 1.Ioannidis A.S., Barton K. Cyclodialysis cleft: causes and repair. Curr Opin Ophthalmol. 2010;21(2):150–154. doi: 10.1097/ICU.0b013e3283366a4d. [DOI] [PubMed] [Google Scholar]
- 2.Shaffer R.N., Weiss D.L. Concerning cyclodialysis and hypotony. Arch Ophthalmol. 1962;68:55–61. doi: 10.1001/archopht.1962.00960030029006. [DOI] [PubMed] [Google Scholar]
- 3.Ritch R., Krupin T., Shields M.B. Ocular hypotony. In: Pederson J.E., editor. The Glaucomas. 2. Mosby; St. Louis: 1996. pp. 385–395. [Google Scholar]
- 4.Ormerod L.D., Baerveldt G., Green R.L. Open Angle Glaucoma Churchill Livingstone. 1986. Cyclodialysis clefts: natural history, assessment and managementIn: weinstein GW; pp. 201–225. New York, NY, USA. [Google Scholar]
- 5.Mateo-Montoya A., Dreifuss S. Anterior segment optical coherence tomography as a diagnostic tool for cyclodialysis clefts [letter] Arch Ophthalmol. 2009;127:109–110. doi: 10.1001/archophthalmol.2008.561. [DOI] [PubMed] [Google Scholar]
- 6.Hwang J.M., Ahn K., Kim C., Park K.A., Kee C. Ultrasound biomicroscopic evaluation of cyclodialysis before and after direct cycloplexy. Arch Ophthalmol. 2008;126:1222–1225. doi: 10.1001/archopht.126.9.1222. [DOI] [PubMed] [Google Scholar]
- 7.Kuchle M., Naumann G.O.H. Direct cycloplexy for traumatic cyclodialysis with persisting hypotony; report in 29 consecutive patients. Ophthalmology. 1995;102 doi: 10.1016/s0161-6420(95)31021-4. 322–233. [DOI] [PubMed] [Google Scholar]
- 8.Mandava N., Kahook M.Y., Mackenzie D.L., Olson J.L. Anterior scleral buckling procedure for cyclodialysis cleft with chronic hypotony. Ophthalmic Surg Laser Imag. 2006;37:151–153. [PubMed] [Google Scholar]
- 9.Hoerauf H., Roider J., Laqua H. Treatment of traumatic cyclodialysis with vitrectomy, cryotherapy, and gas endotamponade. J Cataract Refract Surg. 1999;25:1299–1301. doi: 10.1016/s0886-3350(99)00160-1. [DOI] [PubMed] [Google Scholar]
- 10.Krohn J. Cryotherapy in the treatment of cyclodialysis cleft induced hypotony. Acta Ophthalmol Scand. 1997;75:96–98. doi: 10.1111/j.1600-0420.1997.tb00260.x. [DOI] [PubMed] [Google Scholar]
- 11.Aminlari A., Callahan C.E. Medical, laser, and surgical management of inadvertent cyclodialysis cleft with hypotony. Arch Ophthalmol. 2004;122:399–404. doi: 10.1001/archopht.122.3.399. [DOI] [PubMed] [Google Scholar]
- 12.Saha N., MacNaught A.I., Gale R.P. Closure of cyclodialysis cleft using diode laser. Eye. 2003;17:527–528. doi: 10.1038/sj.eye.6700407. [DOI] [PubMed] [Google Scholar]
- 13.Spiegel D., Katz L.J., McNamara J.A. Surgical repair of a traumatic cyclodialysis cleft after laser failure. Ophthalmic Surg. 1990;21(5):372–373. [PubMed] [Google Scholar]
- 14.Agrawal P., Shah P. Long-term outcomes following the surgical repair of traumatic cyclodialysis clefts. Eye (Lond). 2013;27(12):1347–1352. doi: 10.1038/eye.2013.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patte M., Bonicel P., Bacin F. Treatment of post-traumatic cyclodialysis using by direct cyclopexy. J Fr Ophtalmol. 2001 Mar;24(3):282–285. [PubMed] [Google Scholar]
- 16.Sood G., Rajendran V., George R., Sharma T., Raman R. Comparison of encirclage and cryotherapy with argon laser in the management of traumatic cyclodialysis cleft. Int J Ophthalmol. 2019;12(1):165–168. doi: 10.18240/ijo.2019.01.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kimura M., Yasukawa T., Ogura Y. A simple lens-sparing technique to treat hypotonic maculopathy secondary to large cyclodialysis. American journal of ophthalmology case reports. 2018 Jun 1;10:300–303. doi: 10.1016/j.ajoc.2018.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gressel M.G., Parrish R.K., 2nd, Heuer D.K. Delayed nonexpulsive suprachoroidal hemorrhage. Arch Ophthalmol. 1984;102(12):1757–1760. doi: 10.1001/archopht.1984.01040031421015. [DOI] [PubMed] [Google Scholar]
- 19.Patelli F., Rizzo S., editors. Management of Complicated Vitreoretinal Diseases. Springer International Publishing; 2015 May 20. p. 112. [Google Scholar]