Abstract
This review assesses the effectiveness of interventions to reduce physical restraint (PR) use in older people living in nursing homes or residential care facilities. A systematic search of studies published in four electronic databases (MEDLINE, CINHAL, PsycINFO, Cochrane Central Register of Controlled Trials). The review included individual and cluster randomized controlled trials that compared educational training and multicomponent programs to avoid PR use. Risk bias of randomized controlled trials (RCTs) was assessed according to the Cochrane Handbook for Systematic Reviews of Interventions. This review includes 16 studies in a qualitative synthesis that met the inclusion criteria, nine of them offered a multicomponent program and seven offered only educational training. The results of the 12 studies included in the meta-analysis showed a significant trend in favor of intervention over time and intensity of PR use tends to decrease. The review indicates that educational programs and other supplementary interventions should be effective, but the heterogeneous operative definition of physical restraints can make difficult data generalization.
Keywords: nursing homes, older people, physical restraint, systematic review, meta-analysis
1. Literature Review
Physical restraints (PR) are still commonly used worldwide in nursing homes and in residential care facilities, even if previous epidemiological studies showed wide differences between and within countries [1,2]. The main predictors of physical restraint use are patient’s impaired mobility, impaired cognitive status, and risk of falls; organizational policies can also determine their use. Health care professionals declared, as reported in different qualitative studies, that they use PR not only for preventing falls and injuries but also for controlling dangerous behaviors and for preventing interference with medical devices, such as urinary catheter and nasogastric tubes [3,4,5,6,7,8]. However, current evidence does not support PR effectiveness in reducing and preventing falls and fall-related injuries and questions their safety [3,9,10]. In the last years, a restraint-free nursing care environment has been recommended as a standard of care; therefore, policies and regulations aiming at reducing PR use have been implemented in many countries [11]. This topic is articulated and full of conceptual and operative details. An international consensus statement defines physical restraint as “any device, material or equipment attached to or near a person’s body and which cannot be controlled or easily removed by the person, and which deliberately prevents or is deliberately intended to prevent a person’s free body movement to a position of choice and/or a person’s normal access to their body” [12]. The most commonly methods used are bilateral bed rails, limb or trunk belts, fixed tables on a chair or chairs which prevent patients getting up on their own, and containment sheets and pajamas [3]. A European study conducted on nursing home residents suffering from dementia revealed a prevalence of physical restraints of 31.4%, with a country variation ranging from 6.1% to 83.2% [13]. However, in USA the prevalence ranged from 6.9% to 36.8% [7]; it was estimated at 31.4% in Canada and at 20.2% in China [1]. The differences in the observed occurrence of PR use are influenced by a variety of factors, such as population studied, clinical context, definition of PR and study design [14]. In recent years, restraint-free care has focused on what interventions or strategies can be employed to promote the reduction of physical restraint [15,16,17]. The use of PR is not without risks; adverse effects can be observed ranging from bodily injuries, decreased mobility, and reduced physiological well-being and up to death [3,18,19,20]. Morover PR use raises ethical issues affecting human rights and indeed several authors consider this practice as an approach that violates the freedom and dignity of restrained residents [15,21,22,23]. The persistent use of physical restraints in nursing homes requires effective interventions for educating nursing staff as well as all persons involved in healthcare, for example residents, relatives, nursing experts and nursing homes directors. Several and articulate interventions aimed to address nursing care and institution’s organizational culture about physical restraint use have been studied. However, previous systematic reviews have shown inconclusive evidence about the effectiveness of educational or multicomponent interventions for preventing and reducing the use of physical restraints in long term geriatric care [2,24]. Therefore, it is important to analyze the effectiveness of specific interventions, such as educational programs and consultation or guidance by an expert nurse, to reduce the use of PR in nursing home settings. The challenge of clinicians and researchers remains to find the ideal mix of interventions to avoid the use of physical restraints from clinical practice.
2. Materials and Methods
2.1. Aims
The aims of this systematic review are to assess the effectiveness of an educational training or multicomponent program: (1) in preventing the use of PR in nursing home, and (2) in changing (increasing or decreasing) the rate of patient falls and fall-related injuries.
2.2. Design
A systematic review with meta-analysis was conducted based on the Cochrane Handbook for Systematic Review for Intervention [25] and performed following the Guidelines for reporting Systematic Reviews and Meta-Analyses (PRISMA checklist criteria, see Supplementary File S1). This review protocol has been registered on the PROSPERO International prospective register of systematic reviews (PROSPERO 2018: CRD42019127963).
2.3. Search Methods
Studies published from 1996 to September 2019 were searched using four electronic databases (MEDLINE, CINAHL, the Cochrane Library, and PsycINFO). Other databases, such as www.ClinicalTrials.gov, EU Clinical Trial register, PROSPERO, and Cochrane Library, were searched for unpublished or ongoing studies, as well as reference lists of other studies, all of which were included in this study, were checked. The search strategy used is reported in Appendix A. The following word and MeSH terms were used: Restraint, Physical [Mesh]; Nursing Homes [Mesh] Residential Facilities [Mesh], “bed rail”, “side rail”, “coercion”, and “education”. Inclusion criteria were (a) published and unpublished studies that used cluster and individually randomized controlled trials and quasi-experimental research designs, (b) studies that compare educational training and multicomponent programs to avoid the use of PR on residents in nursing home settings were included in this study, (c) studies written in Italian and English language. The primary outcome was the status of PR as defined by Bleijlevens et al. [12] measured by number of patients who were physically restrained at the studies endpoint, assessed either by direct observation or from clinical documentation, or calculating restraint prevalence (number of restraints/number of residents × 100). Moreover, falls rate and falls- related-injuries) were assessed as secondary outcomes. Studies excluded were those that referred to psychiatric and critical populations in acute ward or home care.
2.4. Search Outcome
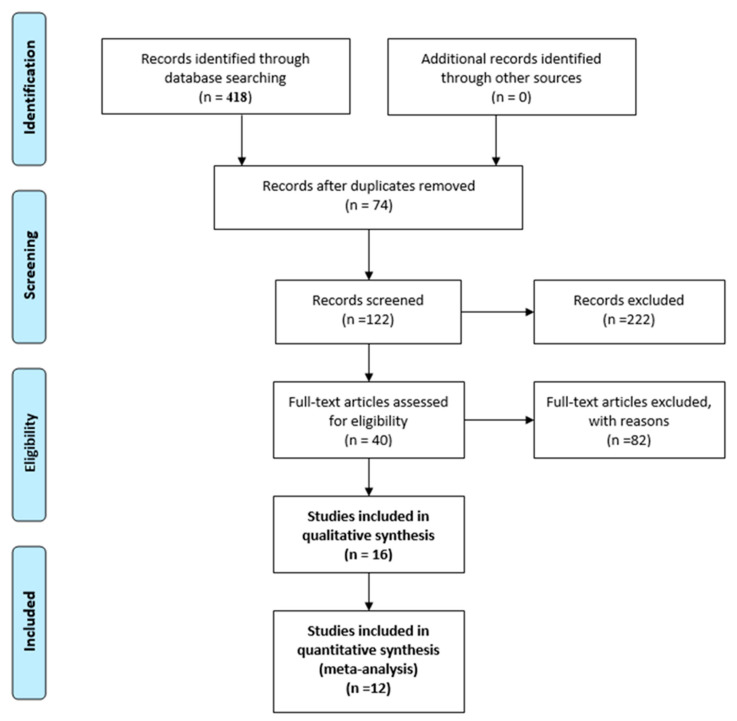
The electronic and manual reference list search revealed 418 publications. A total of 122 references that could meet the inclusion criteria were screened, and 222 publications were excluded; another 82 were excluded for outcomes other than “physical restraint rate”, incomplete data and being written in other languages (German and French). The full texts of the remaining 40 articles were reviewed, and of these, 16 were included in qualitative synthesis and 12 in meta-analysis (Figure 1. PRISMA Flow Diagram).
Figure 1.
PRISMA Flow Diagram.
2.5. Quality Appraisal
Two reviewers (Anna Brugnolli and Martina Debiasi) independently screened the title and abstracts that met the inclusion criteria, and then screened the full text of potentially included studies. The citations in full-text articles marked as included were retrieved and those citations that the reviewers were unsure of were excluded. Disagreements and discrepancies were resolved by consensus, and when necessary, by consultation and discussion within the reviewer teams during all stages of the review process (Federica Canzan, Luigina Mortari, Luisa Saiani and Elisa Ambrosi). Risk bias of randomized controlled trials (RCTs) was assessed according to the Cochrane Handbook for Systematic Reviews of Interventions [24]. For RCTs, we considered random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias. For cluster randomized trials we evaluated recruitment bias, baseline imbalance, loss of clusters, incorrect analysis, and comparability with individually RCTs.
2.6. Data Abstractions
For each included study data were extracted by two independent reviewers using a standardized form and checked for accuracy by a third reviewer. The results were discussed within the reviewers’ team. A descriptive summary of the included studies was created by drawing on two tables of evidence: a general Characteristics table that includes details about the study type, interventions, characteristics of the population, type of intervention and primary and secondary outcome measures with a parallel definition and measurement of restraint status in the studies included (Supplementary File S2), and a Results table that classified the results for each outcomes.
2.7. Synthesis and Supplementary Statistical Analysis
We conducted a meta-analysis using random or fixed effect model where possible, a narrative synthesis was conducted where there was insufficient data. We performed analysis at the level of cluster RCTs. For one study further detail have been requested about the data and effect size about PR used [26]. To assess statistical heterogeneity, we calculated the I2 using Review Manager 5.3 (RevMan, Copenhagen, Denmark); the primary analysis used a random-effects model (risk ratio, RR), which had the highest generalizability in our empirical examination of summary effect measures for meta-analyses [24]. If the heterogeneity with random-effect model was I2 < 50% we used fixed model to estimate the intervention effects, in contrast, if I2 > 50% we used random-effect model.
3. Results
3.1. Study Characteristics
Sixteen studies met the inclusion criteria as described in Table 1. Eleven were cluster RCTs [9,15,26,27,28,29,30,31,32,33,34]; one individual RCT [35]; three quasi-experimental design studies [36,37,38]; and one pre-posttest [39]. Twelve studies were conducted in nursing homes [15,28,30,31,32,33,34,35,36,37,38,39]; four of these had psychogeriatric units/wards dedicated to residents with dementia and behavioral disorders [29,30,31,37]. One study had a unit for people with dementia [9] and one unit in a care home for people with dementia was included because of its close similarities to a residential care facility [26].
Table 1.
Characteristics of included studies.
| Authors (Year) Study Design [Ref] | Country Setting | Sample | Interventions | Control | Follow-Up Period | Primary and Secondary Outcome | |||
|---|---|---|---|---|---|---|---|---|---|
| Education Training | Consultation (APN) and Guidance | Change Policy Implementation Guideline | Availability Alternative Intervention | ||||||
|
Abraham et al. (2019) [27] Pragmatic RCT |
Germany 120 NH |
N = 12,245 residents IG 1: 4126 IG 2: 3547 CG: 4572 |
✓ | ✓ | ✓ | Usual care | 6–12 months | Physical restraint use Falls Fall -related fractures Quality of life |
|
|
Capezuti et al. (2002) [39] Pre- and posttest design |
USA 4NH |
N = 251 residents (side rail use) IG: N = 130 Discontinued Side Rail Use IG: N = 121 Continued Side Rail Use |
✓ | Usual care | 1–12 months | Side rail use Incidence of falls |
|||
|
Evans et al. (1997) [28] Cluster randomized trial |
USA 3 NH |
N = 643 residents N = 463 complete data IGa: 152 IGb: 127 CG: 184 |
✓ | ✓ | Usual care | 6–9–12 months | Physical restraint use Restraint intensity Fall rate |
||
|
Gulpers et al. (2011) [37] Quasi-experimental longitudinal design |
Netherlands 26 psycho-geriatric NH |
N = 420 residents N = 405 complete data IG: 250 CG:155 |
✓ | ✓ | ✓ | ✓ | Usual care | 4–8 months | Belt restraint use Other types of physical restraint use Use of Psychoactive drugs f Falls Fall-related injuries |
|
Gulpers et al. (2012) [38] Quasi-experimental longitudinal study |
Netherlands 13 NH |
N = 104 newly admitted residents N = 82 complete data base line IG: t0 43–t1 29 CG: t0 39–t1 20 |
✓ | ✓ | ✓ | ✓ | Usual Care | 4–8 months | Belt restraints use e Other types of physical restrains use Use of psychoactive medication Falls Fall-related injuries |
|
Gulpers et al. (2013) [36] Quasi-experimental longitudinal study |
Netherlands 13 NH |
N = 225 panel group IG: N = 134 CG: N = 91 |
✓ | ✓ | ✓ | ✓ | Usual care | 24 months | belt restraints use Use of at least one physical restraint device |
|
Huizing et al. (2006) [29] Cluster randomized trial |
Netherlands 5 psycho-geriatric NH |
N = 145 residents with dementia N = 126 complete data IG: t0 83–t1 86 CG: t0 62–t1 58 |
✓ | ✓ | Usual care | 1 month | Physical restraint use Restraint intensity Restraint type |
||
|
Huizing et al. (2009a) [30] Cluster randomized trial |
Dutch 7 psycho-geriatric NH |
N = 432 psycho geriatric residents N = 241 complete data IG: N = 125 CG: N = 115 |
✓ | ✓ | Usual Care |
1–4–8 months | Physical restraint status, intensity Multiple restraint use |
||
|
Huizing et al. (2009b) [31] Cluster randomized trial |
Dutch 14 psycho-geriatric NH |
N = 138 newly admitted psychogeriatric residents N = 90 complete data base line IG: 53 CG: 37 |
✓ | ✓ | Usual Care | 1–4–8 months | Physical restraint status, intensity Multiple restraint use |
||
|
Koczy et al. (2011) [32] Cluster randomized trial |
Germany 45 NH |
N = 430 restrained residents N = 333 complete data IG: N = 208 CG: N = 125 |
✓ | ✓ | ✓ | Usual care | 3 months |
Cessation of physical restraints (100%)–bed rails were not included Falls Use of psychoactive medication |
|
|
Köpke et el. (2012) [15] Cluster randomized trial |
Germany 18 NH |
N = 4449 residents IG: N = 2283 CG: N = 2166 |
✓ | ✓ | Standard information | 3–6 months |
Physical restraint use (6 month) Physical restraint use (3 month) Falls Fall-related fractures Use of antipsychotropic therapy |
||
|
Pellfolk et al. (2010) [9] Cluster-randomized controlled trial |
Sweden 40 Units for people dementia |
N = 355 residents N = 350 residents complete data IG: Residents, N = 192 CG: Residents, N = 163 |
✓ | Usual care | 6 months |
Physical restraint use Falls (1 months) Use of antipsychotic therapy (Benzodiazepines–Narcoleptics) |
|||
|
Rovner et al. (1996) [35] Randomized controlled Trial (RCT) |
Baltimore (USA) A 250-bed community NH |
N = 89 residents randomized N = 81 complete data (91%) IG: N = 42 CG: N = 39 |
✓ | Usual care | 6 months |
Behavioral disorders Use of antipsychotic drugs Physical restraint use Cognition and level of nursing care |
|||
|
Testad (2005) [33] single-blind cluster Randomised controlled trial |
Norway 4NH |
N = 151 residents IG: N = 55 residents All complete data CG: N = 96 residents N = 87 complete data |
✓ | Usual care | 7 months |
Physical restraint use Agitation |
|||
|
Testad et al. (2010) [34] Single blind cluster randomized controlled trial |
Norway 4NH |
N = 211 residents IG: N = 113 residents N = 76–44 complete data CG: N = 98 residents N = 46 complete data |
✓ | Usual care | 6–12 months |
Structural restraint Interactional restraint (treatment and care giving activity such as force and pressure) Agitation Use of antipsychotic drugs |
|||
|
Testad et al. (2016) [26] Single-blind cluster randomized controlled trial |
Norway 24 care homes (citated by authors as NH) |
N = 274 residents IG: N = 118 residents with dementia N = 85 complete data CG: N = 156 residents N = 116 complete data |
✓ | Usual care | 7 months |
Physical restraint use Agitation Use of antipsychotic drugs |
|||
N = number of residents recruited at baseline; Complete data = residents at study endpoint; NH = nursing home; IG = intervention group; CG = control group.
3.2. Risk of Bias Assessment of the Included Studies
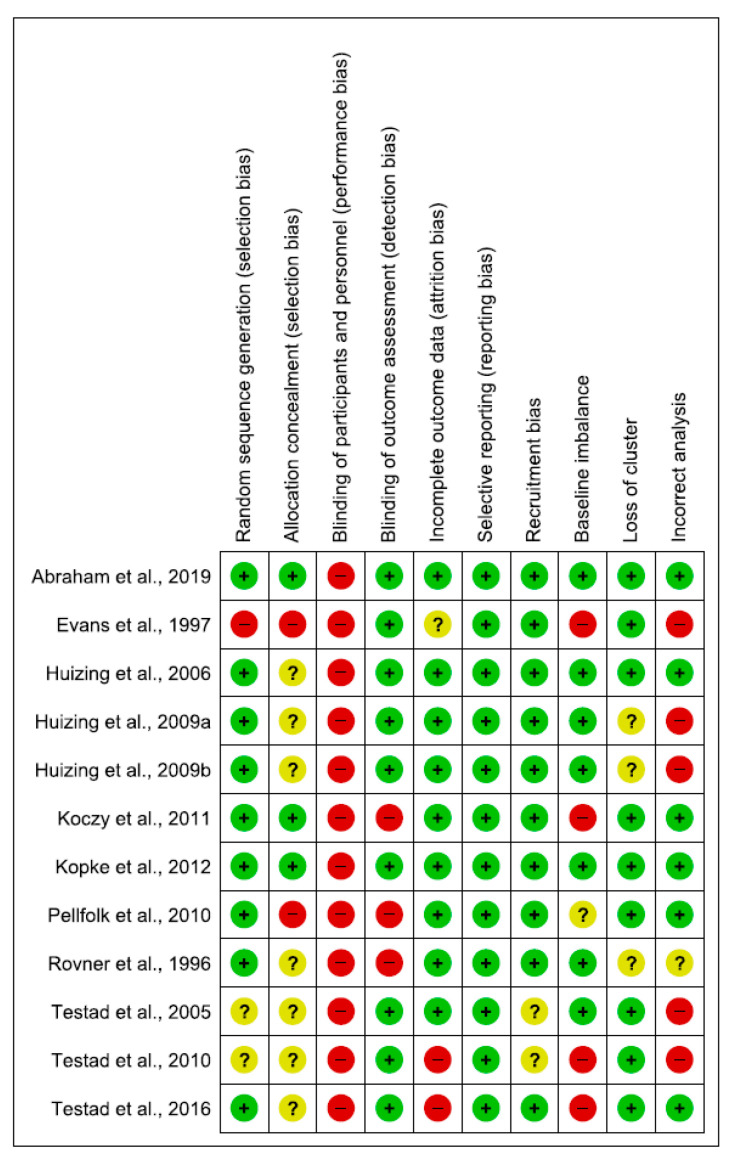
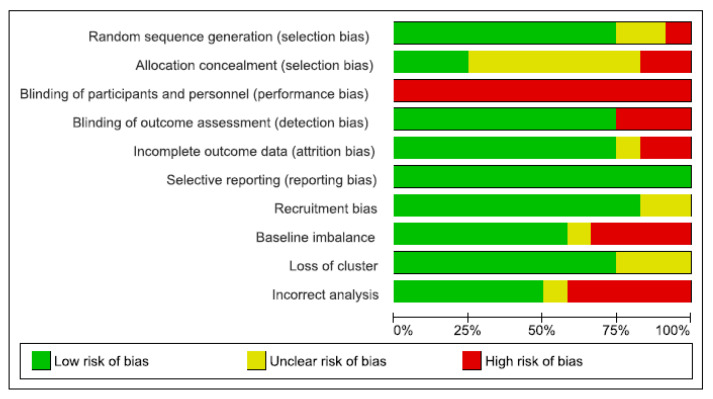
The quality of RCTs was moderate, while it was low for quasi-experimental studies. Of the 16 included studies, nine had adequate sequence generation. Only three reported allocation concealment [15,27,32], blinding of participants and personnel were not possible in any included studies. Ten studies had blinding of outcome assessment [15,26,27,28,30,31,33,34,37,38].
Two of the included studies were assessed as having addressed incomplete data reporting (high risk of bias) [26,34] and lacked an explanation of the choices that underlined the recruitment of the participants [33,34]. Four studies were high risk for baseline imbalance [26,28,32,34], and in one study this issue was not clear [9]. In half of the studies, the analyses were correctly performed, although in some studies, the modalities were not described in detail [28,30,31,33,34]. Methodological quality assessment of the meta-analysis included studies is reported in Figure 2 and Figure 3, and Appendix B.
Figure 2.
Risk of bias summary.
Figure 3.
Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
3.3. Types of Interventions
The characteristics of the intervention group are described in Table 1. Six studies offered only educational training [9,26,33,34,35,39]; and multicomponent programs were performed in ten studies [15,27,28,29,30,31,32,36,37,38]. There were seminars focusing on different topics and based on guideline or best practice followed by guidance or consultation [9,15,26,27]. Educational program changed in time from a minimum of six hours training course to a maximum of 6 months guidance and covering different themes about PR avoiding strategies. The arguments covered by the educational programs addressed the following topics:
-
-
Information on dementia, aggression, and challenging behavior (delirium), falls and fall prevention, care of people with dementia, complications in dementia, decision-making processes and alternatives [8,33];
-
-
Strategies for analyzing and managing aggression or challenging behaviors [9,28,30,32];
-
-
Information about legal implications, adverse effects, experience of feelings of being restrained [9,27,28,30,32];
-
-
Alternative strategies to the use of PR and decision-making processes [9,26,27,30,33,36];
- -
-
-
Overview of the current evidence about PR and summary of the guideline recommendations [27].
The multicomponent interventions included educational training and guide or consultation by a nurse specialist at the registered nurse level [30,31,36,37,38]; a master’s—prepared gerontological nurse such as an opinion leader [28]; an Advanced Practice nurse [39]; or a trained nurse with specific education (at least a Bachelor’s in Nursing) [27]. The consultations were structured as a monthly session supervision (from one hour to 12 h) or on demand. The multicomponent intervention in several studies provided for dissemination of the guideline’s content in clinical practice, availability of alternative interventions and/or introduction of at least a restraint policy [15,27,36,37,38].
3.4. Outcome Measures
Eight of the sixteen included studies had as the primary outcome the use of any PR [9,15,26,28,29,30,31,32,33,34,35]. Follow-up ranged from one to 24 months. Most of the studies provided a conceptual definition of PR (Supplementary File S2): fourteen studies used a comparable definition of PR even if incomplete; three of these studies did not define the devices of restraint [9,28,32] and other two reported only methods [29,39]. Two studies have not reported any definition [33,35]. Eight studies explored falls and injuries related falls; six studies evaluated the impact of a change in prescription of antipsychotic drugs [9,26,34,37,38]. This review analyzed the prevalence of restraint, but it would be relevant to break it down into time of permanence, duration (continuous/discontinuous) and type of restraints used.
3.5. Effect of Interventions
The overall results of the qualitative synthesis (16 studies), reported in Table 2, showed a significant trend in favor of interventions over time and intensity of PR use, except for Testad et al. (2016) [26], which found an increase in the use of containments over time in the intervention group and a tendency for a greater reduction in the control group. In contrast, in some RCTs [30,31], both groups, control and intervention, showed an increase in restraint intensity and multiple restraints over time. 12 RCTs of 16 studies were included in the meta-analysis and including 11 cluster-RCTs and 1 individual RCT [35]. The effects of interventions on the primary outcome were presented according to the type of intervention. The overall effect of the educational program (at study endpoint) in reducing PR use were analyzed a total of 1.186 patients (596 intervention and 590 control group) [9,26,28,33,34].
Table 2.
Results of included studies.
| Author (Year) [Ref] | MA * | Results on Physical Restraint Use | Results on Fall Rate–Fall-Related Injuries |
|---|---|---|---|
|
Abraham et al. (2019) [27] A pragmatic cluster of randomized controlled trial |
Y | Change in any physical restraint prevalence from baseline to follow-up CG −1.2; 95% CI −0.04 to 0.11; p = 0.294 IG 1 update version: −2.8; 95% CI −5.5 to −0.01; p = 0.042 IG 2 concise version: −3.9; 95% CI −6.8 to −1.0; p = 0.009 |
≥1 Fall 12 months OR (95% CI) IG1 vs. CG: 1.17 (0.89–1.53) OR (95% CI) IG2 vs. CG: 1.03 (0.79–1.35) ≥1 Fall- related fractures OR (95% CI) IG1 vs. CG: 1.31 (0.87–1.97) OR (95% CI) IG2 vs. CG: 1.11 (0.73–1.71) |
|
Capezuti et al. (2002) [39] Pre-Post test design |
N | Side rail use immediately post (1 month) e 12 months Statistically significant effects of time and site, indicating a change over time Only one NH Site 3 showed a statistically significant decrease in the rate of restrictive side rail use over time (p = 0.01) |
Fall rate 12 months reduced discontinue restrictive side rail group −0.053; 95% CI (−0.083 to −0.024) p-value < 0.001 continued restrictive side rail group −0,013; 95% CI (−0.056 to 0.030) p-value = 0.17 |
|
Evans et al. (1997) [28] Cluster RCT |
Y | Prevalence restraint use (Individual as units of analysis) 6 month CG:45% (83/184); IG: RE: 18% (27/152); REC: 16% (20/127) 9 month CG: 42% (77/184); IG: RE: 16% (24/152); REC: 12% (15/127) 12 month CG: 43% (79/184);IG: RE: 19% (29/152);REC: 14% (18/127) Nursing home as units of analysis 6 month CG:40%; IG: RE: 19%; REC: 18% 9 month CG: 40%; IG: RE: 17%; REC: 14% 12 month CG: 42%; IG: RE: 19%; REC: 16% |
Fall rate 3 months GC vs. RE or REC (64.7% vs. 41.5% or 42.5%) p < 0.001 6 months GC vs. RE or REC (53.3% vs. 32.2% or 37.8%) p-value < 0.001 |
|
Gulpers et al. (2011) [37] Quasi Experimental |
N | At least one physical restraint device 4 months CG 64%; IG 54%; p-value 0.06 8 months CG 69%; IG 54%; p-value 0.003 |
Falls 4 months GC 14%; GI 20%; p-value 0.10 8 months GC 16%; GI 16%; p-value 0.98 Fall-related injuries 4 months GC 8%; GI10%; p-value 0.44 8 months GC 11%; GI 10%; p-value 0.66 |
|
Gulpers et al. (2012) [38] Quasi Experimental |
N | At least one physical restraint device 4 months CG 31%; IG 30%; p-value 1.00 8 months CG 36%; IG 21%; p-value 0.15 |
Falls 4 months GC 40%; GI 38%; p-value 1.00 8 months GC 30%; GI 21%; p-value 0.51 Fall-related injuries 4 months GC 10%; GI 24%; p-value 0.28 8 months GC 10%; GI 14%; p-value 1.00 |
|
Gulpers et al. (2013) [36] Quasi experimental |
N | At least one physical restraint 24 months IG: 80/134 (60%); CG: 68/91 (75%) OR 0.50, 95% CI 0.28 to 0.90, p-value = 0.020 |
|
|
Huizing et al. (2006) [29] Cluster RCT |
Y | Restraint use (prevalence) CG 40/58; IG: 45/86 OR 0.50, 95% CI 0.24 to 0.99 p-value = 0.048 Restraint intensity over time CG t0 56% t1 70%; IG t0 54%–t1 56% p-value > 0.05 |
|
|
Huizing et al. (2009a) [30] cluster RCT |
Y | Change in restrain status CG 69/115 (60%); IG: 81/126(64%) IG change t0 54% vs. t3 (8 months) 64% (p = 0.02)—at post-test 2 there were no differences CG: t0 49% vs. t2 (4 months) 57% (p = 0.02); t3 60% (p = 0.007) |
|
|
Huizing et al.(2009b) [31] cluster RCT |
Y | Not restrained vs. restraint 1 month CG: 70% (14/20)–IG: 61.8% (21/34) vs. CG 30% (6/20)–IG 38,2% (13/34); p-value 0.541 4 months CG: 67.7% (21/31) – IG: 48.8% (21/43) vs. CG 32.3% (10/31) vs. IG: 51.2% (22/43) p-value 0.105 8 months GC 59.5% (22/37)–IG: 52.8% (28/53) vs. CG 40.5% (15/37)–IG 47.2% (25/53) p-value 0.53 |
|
|
Koczy et al. (2011) [32] cluster RCT |
Y | 100% not restrained (free) 3 months CG 8.8% vs. IG 16.8% OR 2.16 (IC 95% 1.05–4.46) Restraint 3 months CG: 114/125 (91.2%); IG: 173/208 (83.2%) |
Falls 3 months GI 16.3% vs. GC 8.0%; OR 2.08 (IC 95% 0.98–4.40) |
|
Köpke et al. (2012) [15] RCT |
Y | Any physical restraint 3 months CG 30.5 (26.6–34.4) vs. IG 23.9 (19.3–28.5) MD 6.6%; 95% CI (0.6–12.6) Cluster adjusted OR 0.72; 95% CI (0.53–0.97) p-value 0.03; ICCC 0.029 6 months Difference 6.5%; 95% CI (0.6–12.4) Cluster adjusted OR 0.71; 95% CI (0.52–0.97) p-value 0.03; ICCC 0.029 |
Residents ≥1 fall during period study Difference 3%; 95% CI (−3.5 to 9.4) Cluster adjustice OR 0.85; 95% CI (0.60 to 1.21) Fractures during period study Difference 0.5%; 95% CI (−0.5 to 1.4) OR (95% CI) = 0.76 (0.42 to 1.38) |
|
Pellfolk et al. (2010) [9] cluster RCT |
Y | Physical restraint 6 months CG 38.1% (53/139); IG 20.1% (30/149) p-Value baseline/ 6 months: 0.78/0.001 OR 0.21, 95% CI 0.08–0.57, p-value 0.002 restrained baseline vs. unrestraint 6 months CG 3.6% (n = 1/28) vs. IG 31.3% (n = 10/32) (p = 0.007). unrestrained baseline vs. restrained 6 months CG 23.4% (n26/111) vs. IG 6.8% (n8/117) (p-value 0.001). |
Falls 6 months IG 10.1% vs. CG 8.6% p-Value baseline/ Follow-Up: 0.45/0.68 |
|
Rovner et al. (1996) [35] RCT |
Y | Physical restraint 6 months CG 20/38 (52.6%) vs. IG 14/41 (34.1%) OR 0.47 [95% CI 0.19 to 1.16] p-value = 0.10 |
|
|
Testad et al. (2005) [33] RCT |
Y | Frequency of use of restraint–mean (range) 7 months CG 4/55; IG 2/96 CG 3.7 (0–25); GI 1.5 (0–10); p-value = 0.016 |
|
|
Testad et al. (2010) [34] RCT |
Y | Structural restraint 6 months CG 23/70 (33%); IG 48/75 (64%) 12 months CG 6/70 (13%) IG 8/75 (18%) |
|
|
Testad et al. (2016) [26] cluster RCT |
Y | Change in any physical restraint physical restraint prevalence from baseline to /7months CG t0 10.5% vs. t1 6.1% p < 0.001; IG t0 14.5% vs. t1 10.5% p-value 0.007 |
* MA, meta-analysis; Y, yes: studies included in meta-analysis; N, Not included; CG, control group; IC, intervention group; RE, educational rehabilitation; REC, educational rehabilitation with consultation.
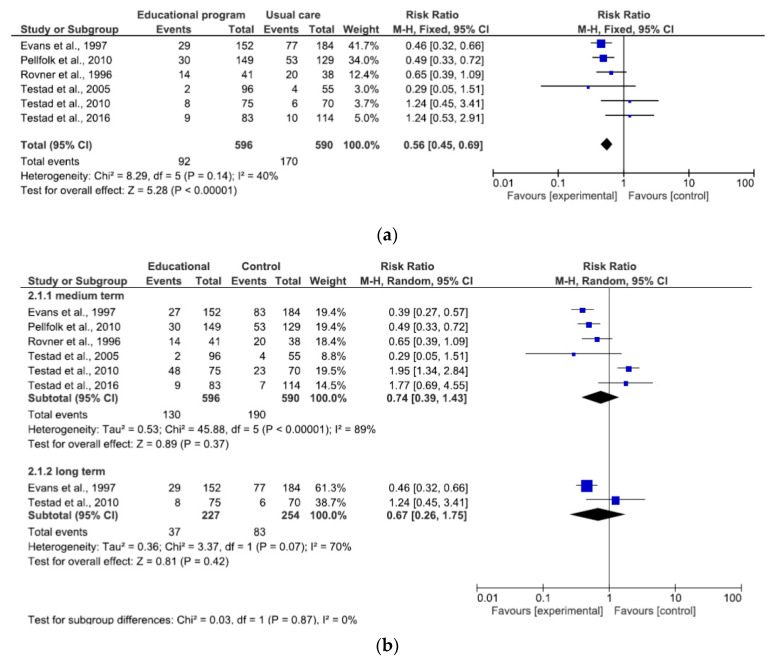
The combined estimated risk ratio (RR) of use of PR with an educational program was statistically significant (Figure 4a: 0.56, 95% CI 0.45–0.69). There was moderate overall heterogeneity (I2 = 40%). At medium term (6–8 months), RR of use of physical restraint is RR 0.74 (95% CI 0.39–1.43), and long term (12–24 months), RR 0.67 (95% CI 0.26–1.75). In both subgroups a substantial heterogeneity emerged (Figure 4b).
Figure 4.
(a) Effect of educational program at endpoint study on reducing PR use; (b) Effect of educational program at different follow-up on reducing PR use.
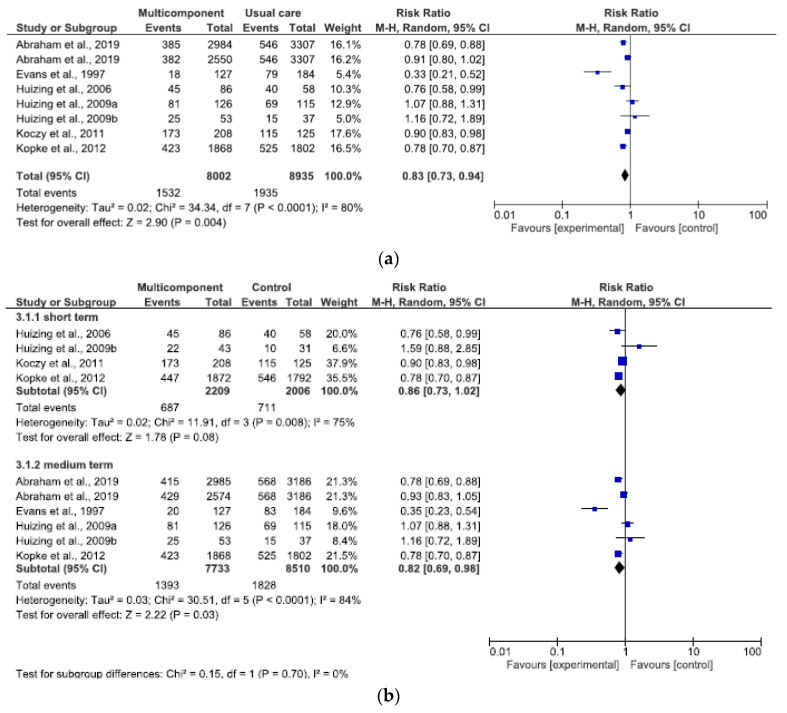
The overall effect of the multicomponent program (at endpoint studies) in reducing PR use were analyzed in a total of 16.937 patients (8.002 intervention vs. 8.935 control) [15,27,28,29,30,31,32]. The combined estimated RR of use of PR with a multicomponent program was statistically significant (Figure 5a: RR 0.83, 95% CI 0.73–0.94). There was an effect and statistically significant overall high heterogeneity (I2 = 80%). The results at short-term (1–4 months) and medium-term (6–8 months) were slightly statistically significant (Figure 5b). At short-term the RR of use of physical restraint is RR 0.86 (95% CI 0.73–1.02), and medium-term (RR 0.82, 95% CI 0.69–0.98). In both subgroups a substantial heterogeneity emerged (I2 = 75% and 84%).
Figure 5.
(a) Effect of a multicomponent program at endpoint study on reducing PR use; (b) Effect of a multicomponent program at different follow-up on reducing PR use.
3.6. Secondary Outcome Results
The results of secondary outcomes are reported in Table 2. The introduction of an educational or multicomponent intervention does not lead to a statistically significant increase in the rate of falls and fall-related injuries [32,33,36,37,38].
4. Discussion
This meta-analysis summarizes the evidence regarding the effectiveness of educational programs and multicomponent interventions on the use of mechanical restraints without an increase in falls, behavioral symptoms, or medication. The studies included in this review were adequate and had from low to moderate risk of bias; many of them demonstrated differences regarding the type of interventions and also most of the studies did not have an unvarying definition of physical restraint and methodologies for data collection. A previous Cochrane review underlines that there were insufficient evidence supporting the effectiveness of educational interventions for preventing or reducing the use of PR in geriatric long-term care [2]. In this systematic review emerged the effectiveness of the educational interventions at the endpoint study, and of the multicomponent program all the follow-up time (from 6 to 24 months), in reducing or preventing the use of PR in nursing home settings. More recent evidence of successful reduction efforts in use of restraints is evident from several countries, which used a multicomponent approach [15,27]. This approach demonstrated a reduction in physical restraint use within nursing home after 6- and 12-months post implementing both a detailed guideline and theory-based multicomponent interventions. Multicomponent educational interventions are designed to change the organizational culture towards a least-restraint policy. It is believed that leadership could essentially contribute to restraint-free nursing care by sensitizing nurses and creating optimal working conditions; nursing home staff profile and competencies are appropriate to meet the increasingly complex needs of residents with dementia [40,41]. Knowing that decision-making is mainly based on individual’s experiences and often is ambiguous, the development of evidence-based guidelines to support decision-making regarding the (non)-use of physical restraints is highly recommended [40]. The decision-making process concerning the application of physical restraints has always to respect the resident’s situation as well as nurse- and organization-related factors. The core educational component addresses the attitudes of nurses, physicians and other healthcare professionals who are involved in making decisions and conceiving policies about PR use. Additional components might target the care environment (e.g., environmental changes, adjustment of staff-patient ratios or staff skill mix, involvement of family members, advocacy), or the organizational culture (e.g., attitudes of the opinion leaders or the management), and may support the implementation of change in other ways (e.g., by providing supervision or guidance for healthcare professionals). Protection is a common reason for the use of PR, and the objective is to reduce the use of this method, while employing educational programs and consultation as strategies. In different countries these includes legislation and attention to creating or revising guidelines for nurses and institutions. In addition, it is important to pay attention to the barriers within long-term contexts that do not allow the reduction of PR; educational support is only a starting point and other interventions are needed. This is sure enough, as the results of the analyzed studies support the implementation of educational programs, even alone or with an expert in advanced clinical nursing capable to give consultation and to endorse changes. It is also important to underline that the effectiveness could be decrease in both approaches and is important a re-training to keep knowledge alive.
5. Study Limitations
Several limitations of this review have to be considered. The results have limited validity, transferability and generalizability due to the wide range of definitions of physical restraints, the variability of elements that performed a multicomponent program (guidance, consultation, policy or guideline) and/or different measurements in outcomes. Furthermore, the variability of the sample, in terms of baseline characteristics, high turnover, mortality and transfer drop-out or other factors led to an imbalance in the data when comparing the baseline with the data at the follow-up. Finally, there was a lack of data on the proportion of patients with dementia in most of the included studies.
6. Relevance to Clinical Practice
The results of this review will be highly relevant for clinical practice and help nurses’ decision-making. Information about effective interventions for preventing and reducing the use of PR in nursing homes may promote care with less or even without PR use which might increase the quality of care of older people. Nursing homes have an important role in the care of older people; the trajectory leading to use of restraint is complex, and the context and nursing factors could affect nurses’ decision-making [42]; further research is thus needed exploring how nurses can be empowered to deal more effectively with this important care issue. Future research is necessary to investigate the feelings and attitudes of healthcare professionals about PR and explore their knowledge of alternatives to PR use. Basic and continuous staff training is a key element in that it allows you to increase knowledge, change attitudes in favor of reducing restraint. This training should include legal, ethical and clinical aspects, with reference to possible alternative ways to avoid restraint in vulnerable people. However, based on the results, training represents a necessary but not enough element, on its own, to create a restraint free culture. In the future, multicomponent programs involving the whole team are needed; and create a multidimensional approach according to professionalism to provide the best patient assistance. Nursing home had to stimulate changes in policy and organizational procedure to reduce or prevent the use of physical restraints. In the included studies definitions of PR are inconclusive and unclear for example, bedside-rails were considered PR in some studies but not in others. Similarly, the educational programs are not always the same and have different elements and components and for these reasons, difficulties arise in comparing the results of the various studies and therefore results are not easy generalizable.
7. Conclusions
The results of this review underline that educational training and multicomponent programs could be effective in reducing the use of PR in nursing home settings. At the least, additional studies implementing an educational program alone or with consultation or guidance might provide further evidence of the effectiveness of these approaches on the reduction in the use of PR. The number of older patients with temporary or permanent cognitive impairment in general hospital settings will increase due to demographic change and medical progress. These patients have a higher risk of being restrained [43,44], and PR use may be associated with negative effects that may hamper recovery and rehabilitation. In contrast to geriatric long-term care settings, there is no high-quality systematic review about the effects of interventions intended to prevent or reduce PR use in older people in nursing home settings.
Acknowledgments
Chiara Gastaldon and Corrado Barbui given technical support in using Review Manager.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/18/6738/s1, Figure S1: Prisma check list, Table S1: Definition and measured status of restraint in included study.
Appendix A
Table A1.
Search strategy.
| Research Question | Elements of PICOS | Keywords |
|---|---|---|
| P | Restrained residents in nursing home | Residents in nursing home /Long term setting, residential care facilities |
| I | Educational or multicomponent program | Educational training or multicomponent program |
| C | Usual care | |
| O | Status of physical restraint | Physical restraints or coercion |
| S | Experimental studies | Randomized controlled trials, clinical trials, quasi experimental studies |
Search physical restraint (14,942)
Search “Restraint, Physical” [Mesh] (13,532)
Search nursing home (86,313)
Search “Nursing Homes” [Mesh] (37,522)
Search residential care facilities (4956)
Search “Residential Facilities” [Mesh] (50,272)
Search containment measure (393)
Search coercion (6417)
Search seat belt (4812)
Search side rail (74)
Search bedrail (41)
Search clinical trial (1,125,519)
Search randomized controlled trial (623,325)
Search quasi experimental (15,240)
Search (physical restraint) OR “Restraint, Physical” [Mesh] (14,942)
Search (((physical restraint) OR “Restraint, Physical” [Mesh])) AND “Nursing Homes” [Mesh] (490)
Search ((((physical restraint) OR “Restraint, Physical” [Mesh])) AND “Nursing Homes” [Mesh]) AND “Residential Facilities” [Mesh] (490)
Search (“Restraint, Physical” [Mesh]) AND “Residential Facilities” [Mesh] (517)
Search ((((((physical restraint) OR “Restraint, Physical” [Mesh])) OR bedrail) OR side rail) OR coercion) OR seat belt (25,952)
Search ((((((((physical restraint) OR “Restraint, Physical” [Mesh])) OR bedrail) OR side rail) OR coercion) OR seat belt)) AND ((“Restraint, Physical” [Mesh]) AND “Residential Facilities” [Mesh]) (517)
Search (((((((((((physical restraint) OR “Restraint, Physical” [Mesh])) OR bedrail) OR side rail) OR coercion) OR seat belt)) AND ((“Restraint, Physical” [Mesh]) AND “Residential Facilities” [Mesh]))) AND clinical trial) OR randomized controlled trial (623,335)
Search ((((((((((physical restraint) OR “Restraint, Physical” [Mesh])) OR bedrail) OR side rail) OR coercion) OR seat belt)) AND ((“Restraint, Physical” [Mesh]) AND “Residential Facilities” [Mesh]))) AND clinical trial (37)
Search ((((((((((physical restraint) OR “Restraint, Physical” [Mesh])) OR bedrail) OR side rail) OR coercion) OR seat belt)) AND ((“Restraint, Physical” [Mesh]) AND “Residential Facilities” [Mesh]))) AND randomized controlled trial (28)
Appendix B
Table A2.
Risk of bias of included studies.
| Abraham et al. (2019) [27] (Cluster Clinical Trial) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | One cluster was inadvertently allocated to another group as randomized but a sensitivity-analysis of the primary outcomes showed comparable results and we did not expect that this introduced a risk of bias. |
| Allocation concealment (selection bias) | Low risk | Clusters were randomly assigned to study groups by a person affiliated to the study center in Hamburg, but not involved in the study, using a computer-generated randomization list stratified by region with blocks of six, nine, and twelve nursing homes (generated by an independent external biometrician (BH)). One cluster at the study center Halle (Saale) that had been randomized to intervention group 1 was erroneously allocated to the control group due to miscommunication. |
| Blinding of participants and personnel (performance bias) | High risk | Not possible |
| Blinding of outcome assessment (detection bias) | Low risk | […] raters blinded to group allocation. Raters were trained using a standardized list of measures to be rated as physical restraints. We assessed blinding of research assistants at T2 with 53.7% (95% CI, 45.5 to 63.6) of correct ratings indicating successful blinding |
| Incomplete outcome data (attrition bias) | Low risk | |
| Selective reporting (reporting bias) | Low risk | |
| Recruitment bias | Low risk | Recruitment lasted from February to November 2015. All residents that were present in the nursing home on the day of data collection were included. Residents newly admitted during follow-up were also included |
| Baseline imbalance | Low risk | |
| Loss of cluster | Low risk | The interventions were implemented as planned with excep- tion of the one cluster discussed above. |
| Incorrect analysis | Low risk | |
| Evans et al., 1997 [28] (Cluster Clinical Trial) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | High risk | “Interventions were randomized to site using the sealed envelope technique” |
| Allocation concealment (selection bias) | High risk | Not done |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | “Observer nurses were unaware of the exact study design, interventions, and nursing home’s group assignment” |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported flow of study design and participants |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | low risk | |
| Baseline imbalance | high risk | statistically significant differences in baseline characteristics emerged concerning the prevalence of PR and the dependency level of participants |
| Loss of cluster | Low risk | no loss of cluster |
| Incorrect analysis | high risk | |
| Huizing et al., 2006 [29] (Cluster Randomized Controlled Trial) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | Done “wards were assigned at random to either educational intervention (3 wards) or control status (2 wards) |
| Allocation concealment (selection bias) | Unclear risk | Not reported method of concealment |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | “The observers (two nurses, one occupational therapist and one member of management) were not told to the exact design of the study, the intervention and the division into experimental and control wards” |
| Incomplete outcome data (attrition bias) | Low risk | During the study there were newly admitted patients both in control and intervention group. Dropped out 19 residents, new admitted 18 residents |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | Low risk | The wards were assigned at random to either educational intervention or control |
| Baseline imbalance | Low risk | baseline characteristics are quite similar, excepted in depression (statistically significant difference) |
| Loss of cluster | Low risk | no loss of cluster |
| Incorrect analysis | Low risk | Descriptive statistics were computed for the characteristics of the residents. Logistic regression analysis was used to compare restraint use post-intervention, controlling for characteristics of residents |
| Huizing et al., 2009a [30] (Cluster Randomized Study (RCT)) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | Not report methods of randomization |
| Allocation concealment (selection bias) | Unclear risk | Not reported method of concealment |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Trained observers (n511) blinded to the experimental and control conditions measured the use of physical restraints |
| Incomplete outcome data (attrition bias) | Low risk | During the study, 130 dropped out, mainly because of death (75%). The dropout rate includes that of one ward (n = 529 residents) whose staff was unable to attend the educational intervention because of lack of time. |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | Low risk | The wards were assigned at random to either educational intervention or control |
| Baseline imbalance | low risk | Baseline characteristic comparisons between residents who completed all four measurements and dropouts showed that these groups differed on most characteristics and is not use stratified or pair matched randomization |
| Loss of cluster | Unclear | One out of 15 clusters was lost to follow-up |
| Incorrect analysis | high risk | |
| Huizing et al., 2009b [31] (Cluster Randomized Study (RCT)) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | The 14 psycho-geriatric nursing home wards were randomly assigned to (..) |
| Allocation concealment (selection bias) | Unclear risk | Not reported method of concealment in report and protocol n. ISRCTN10117742. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | The observers were blinded to the experimental and control conditions. To measure the inter rater reliability, two of the eight observers were selected and they scored the same residents with restraints (k = 1.0). |
| Incomplete outcome data (attrition bias) | Low risk | 33 residents were not included in the analyses, mainly because these residents died or informed consent had not been obtained. A total of 105 residents were included in the analyses. |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | low risk | nursing home wards were randomly assigned to either educational intervention or control status. |
| Baseline imbalance | low risk | Not use stratified or pair matched randomization |
| Loss of cluster | unclear | “The study was part of a larger study focusing on the use of physical restraints on psychogeriatric nursing home residents (15 Dutch nursing home)”. One out of 15 clusters was lost to follow-up (Huizing et al., 2009a) |
| Incorrect analysis | high risk | |
| Koczy et al., 2011 [32] (Cluster Randomized Controlled Trial (RCT)) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | Despite the randomization, there were differences in baseline characteristics of participants between the two groups. |
| Allocation concealment (selection bias) | Low risk | An independent organization performed randomization according to nursing home after baseline assessment of all restrained residents. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Not done: “Data collection was, therefore, unblended” |
| Incomplete outcome data (attrition bias) | Low risk | Drop out 52 GI (19.4%), 30 GC (18.5%) |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | Low risk | Individual were not recruited after randomized cluster |
| Baseline imbalance | High risk | “Despite the randomization, there were differences in baseline characteristics of participants between the two groups. The sex ratio was unbalanced, and the number of restrained residents differed between the IG and the CG” |
| Loss of cluster | Low risk | No loss of cluster during study |
| Incorrect analysis | low risk | Before definitive analyses, potential cluster effects were estimated for all models. For all analyses, cluster (nursing home) effects of nursing homes accounted for approximately 1.5% of the total variance and individual effects for more than 98%, so clusters were not considered in the final analysis. |
| Kopke et al., 2012 (Cluster Randomized Study (RCT)) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | Computer generated randomization lists will be used for allocation of clusters in blocks of four, six and eight nursing homes. Randomization will be stratified by region |
| Allocation concealment (selection bias) | Low risk | Paper and Protocol ISRCTN 34974819: “Clusters will be allocated after collection of baseline and prevalence data by an external researcher, not involved in the study. The external researcher informs each cluster about its group assignment |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | The primary outcome of this study is obtained by trined external investigators. |
| Incomplete outcome data (attrition bias) | Low risk | No nursing home dropped from the study |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes like in Protocol. |
| Recruitment bias | low risk | Newly admitted patients in cluster during study, but individuals were not informed about the intervention or control group. |
| Baseline imbalance | Low risk | Randomized stratification |
| Loss of cluster | Low risk | No loss of cluster |
| Incorrect analysis | Low risk | Cluster adjusted 95% confidence intervals of prevalence data were estimated corresponding to the cluster size weighted prevalence estimation from cluster means taking into account variance of cluster means. |
| Pellfolk et al., 2010 [9] (Cluster Randomized Controlled Trial) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | “The randomization was based on a lottery system using identification codes” |
| Allocation concealment (selection bias) | High risk | Not done |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Not done |
| Incomplete outcome data (attrition bias) | low risk | |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | Low risk | |
| Baseline imbalance | unclear | At baseline, only age, sex, and wandering behavior differed between the groups, whereas at follow-up age, sex, and cognitive level were all significantly different. |
| Loss of cluster | Low risk | No loss of cluster |
| Incorrect analysis | Low risk | The difference between IG and CG was analyzed by incorporating potential confounders into a multiple logistic regression analyses with a backward selection algorithm and adjusted for the cluster effect |
| Rovner et al., 1996 [35] (Randomized Controlled Trial, RCT)—NOT Cluster | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | Done “The allocation procedure was a fixed, uniform randomization scheme by computer algorithm”. |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) | High risk | Not blinding |
| Blinding of outcome assessment (detection bias) | High risk | Not blind “nursing staff (nonblind) reported two or more behaviors on the PGDRS that were severe enough to require restraints on the nursing unit” |
| Incomplete outcome data (attrition bias) | Low risk | |
| Selective reporting (reporting bias) | Low risk | Report included primary and secondary outcomes. |
| Recruitment bias | Low risk | |
| Baseline imbalance | Low risk | no difference except for number of females in the intervention group |
| Testad et al., 2005 [33] (a Single-Blind Cluster Randomized Controlled Trial) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | The nursing homes were randomly assigned to the treatment intervention or control condition, two in each group, after stratification for size. |
| Allocation concealment (selection bias) | Unclear risk | Not reported in paper |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | Data were collected immediately before and after the intervention period by a trained rater who was blind to the study hypothesis and to treatment allocation. |
| Incomplete outcome data (attrition bias) | low risk | Drop out only 9 patient in control group for death |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | Unclear | unclear methods. Not report CONSORT flow diagram |
| Baseline imbalance | Low risk | At baseline, the number of restraint and BARS scores did not differ between the groups |
| Loss of cluster | Low risk | No loss of cluster |
| Incorrect analysis | high risk | |
| Testad et al., 2010 [34] (Cluster Randomized Controlled Trial) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Unclear | Not described |
| Allocation concealment (selection bias) | Unclear | Not reported in paper |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | “The administration of the outcome measures and drug recording were done by a trained research nurse who was uninformed” |
| Incomplete outcome data (attrition bias) | High risk | Drop out 61.1% in intervention group and 53.1% in usual care group. Reasons for drop-out were similar in both groups and mostly due to death and discharge |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | unclear | not described |
| Baseline imbalance | high risk | “were differences in proportion of using physical restraint, antipsychotics, and total CMAI score between the groups”. |
| Loss of cluster | low risk | |
| Incorrect analysis | high risk | |
| Testad et al., 2016 [26] (a Single-Blind Cluster Randomized Controlled Trial) | ||
| Bias | Authors’ Judgment | Support for Judgment |
| Random sequence generation (selection bias) | Low risk | Done “All homes in the geographical area were invited to participate following a list in randomized Order” |
| Allocation concealment (selection bias) | unclear risk | Not reported in paper and in protocol Clinical Trials NCT01715506 |
| Blinding of participants and personnel (performance bias) | High risk | Blinding of participants was not possible. Personnel were not blinded |
| Blinding of outcome assessment (detection bias) | Low risk | “All data in the 24 care homes were collected within 1 week by research assistants blind to the study |
| Incomplete outcome data (attrition bias) | High risk | Dropout from baseline to follow-up was 35 (30%) in the intervention group and 42 (26%) in the control group. Reasons unknown |
| Selective reporting (reporting bias) | Low risk | Reports included results both primary and secondary outcomes. |
| Recruitment bias | Low risk | Treatment allocation was revealed to the facilitating teams by the principal investigator, when baseline was completed. |
| Baseline imbalance | High risk | ”There were statistically significant differences between the intervention group and control group for age, ADL score, CMAI score, and NPI sum score”. “These confounders were included in a regression analysis to identify any impact on outcomes, which showed that difference in changes in agitation represented regression to the mean”. |
| Loss of cluster | Low risk | Not loss cluster |
| Incorrect analysis | Low risk | “The effect of clustering was taken into account and adjusted for when if the ICC had a value greater than 5%. Logistical regressions were performed to detect differences between groups and adjust for possible confounders” |
Author Contributions
Conceptualization, A.B., M.D. and F.C.; methodology, A.B., M.D. and F.C.; software, M.D.; formal analysis, A.B., M.D. and F.C.; investigation, A.B., M.D., F.C., L.M., L.S. and E.A.; resources, A.B., L.M., L.S.; data curation, A.B., M.D. and F.C.; writing—original draft preparation, A.B., M.D. and F.C.; writing—review and editing, L.M., L.S. and E.A.; visualization, A.B., M.D., F.C., L.M., L.S. and E.A.; project administration, M.D., A.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Feng Z., Hirdes J.P., Smith T.F., Finne-Soveri H., Chi I., Du Pasquier J.-N., Gilgen R., Ikegami N., Mor V. Use of physical restraints and antipsychotic medications in nursing homes: A cross-national study. Int. J. Geriatr. Psychiatry. 2009;24:1110–1118. doi: 10.1002/gps.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Richter T., Köpke S., Meyer G. Interventions for preventing and reducing the use of physical restraints in long-term geriatric care. Cochrane Database Syst. Rev. 2011;16:CD007546. doi: 10.1002/14651858.cd007546.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans D., FitzGerald M. The experience of physical restraint: A systematic review of qualitative research. Contemp. Nurse. 2002;13:126–135. doi: 10.5172/conu.13.2-3.126. [DOI] [PubMed] [Google Scholar]
- 4.Hamers J.P., Huizing A.R. Why do we use physical restraints in the elderly? Z. Gerontol. Geriatr. 2005;38:19–25. doi: 10.1007/s00391-005-0286-x. [DOI] [PubMed] [Google Scholar]
- 5.Heeren P., Van De Water G., De Paepe L., Boonen S., Vleugels A., Milisen K. Staffing levels and the use of physical restraints in nursing homes: A multicenter study. J. Gerontol. Nurs. 2014;40:48–54. doi: 10.3928/00989134-20140407-03. [DOI] [PubMed] [Google Scholar]
- 6.Hofmann H., Schorro E., Haastert B., Meyer G. Use of physical restraints in nursing homes: A multicentre cross-sectional study. BMC Geriatr. 2015;15:1–8. doi: 10.1186/s12877-015-0125-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luo H., Lin M., Castle N. Physical restraint use and falls in nursing homes: A comparison between residents with and without dementia. Am. J. Alzheimer’s Dis. Other Dement. 2011;26:44–50. doi: 10.1177/1533317510387585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer G., Köpke S., Haastert B., Mühlhauser I. Restraint use among nursing home residents: Cross-sectional study and prospective cohort study. J. Clin. Nurs. 2009;18:981–990. doi: 10.1111/j.1365-2702.2008.02460.x. [DOI] [PubMed] [Google Scholar]
- 9.Pellfolk T.J.-E., Gustafson Y., Bucht G., Karlsson S. Effects of a restraint minimization program on staff knowledge, attitudes, and practice: A cluster randomized trial. J. Am. Geriatr. Soc. 2010;58:62–69. doi: 10.1111/j.1532-5415.2009.02629.x. [DOI] [PubMed] [Google Scholar]
- 10.Sze T.W., Leng C.Y., Lin S.K.S. The effectiveness of physical restraints in reducing falls among adults in acute care hospitals and nursing homes: A systematic review. JBI Libr. Syst. Rev. 2012;10:307–351. doi: 10.11124/jbisrir-2012-4. [DOI] [PubMed] [Google Scholar]
- 11.Kong E.-H., Choi H., Evans L.K. Staff perceptions of barriers to physical restraint-reduction in long-term care: A meta-synthesis. J. Clin. Nurs. 2016;26:49–60. doi: 10.1111/jocn.13418. [DOI] [PubMed] [Google Scholar]
- 12.Bleijlevens M.H.C., Wagner L.M., Capezuti E.A., Hamers J.P.H. The international physical restraint workgroup physical restraints: Consensus of a research definition using a modified delphi technique. J. Am. Geriatr. Soc. 2016;64:2307–2310. doi: 10.1111/jgs.14435. [DOI] [PubMed] [Google Scholar]
- 13.Hofmann H., Hahn S. Characteristics of nursing home residents and physical restraint: A systematic literature review. J. Clin. Nurs. 2013;23:3012–3024. doi: 10.1111/jocn.12384. [DOI] [PubMed] [Google Scholar]
- 14.Beerens H.C., Sutcliffe C., Renom-Guiteras A., Soto M.E., Suhonen R., Zabalegui A., Bökberg C., Saks K., Hamers J.P. Quality of life and quality of care for people with dementia receiving long term institutional care or professional home care: The european RightTimePlaceCare Study. J. Am. Med. Dir. Assoc. 2014;15:54–61. doi: 10.1016/j.jamda.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Köpke S., Mühlhauser I., Gerlach A., Haut A., Haastert B., Möhler R., Meyer G. Effect of a Guideline-Based Multicomponent Intervention on Use of Physical Restraints in Nursing Homes. JAMA. 2012;307:2177–2184. doi: 10.1001/jama.2012.4517. [DOI] [PubMed] [Google Scholar]
- 16.Registered Nurses’ Association of Ontario Promoting Safety: Alternative Approaches to the Use of Restraints. [(accessed on 14 September 2020)]; Available online: http://rnao.ca/bpg/guidelines/promoting-safety-alternative-approaches-use-restraints.
- 17.Royal College of Nursing (RCN) Use of Restrictive Practices in Health and Adult Social Care and Special Schools. RCN; London, UK: Dec 19, 2013. [Google Scholar]
- 18.Bellenger E., Ibrahim J.E., Bugeja L., Kennedy B. Physical restraint deaths in a 13-year national cohort of nursing home residents. Age Ageing. 2017;46:688–693. doi: 10.1093/ageing/afw246. [DOI] [PubMed] [Google Scholar]
- 19.Berzlanovich A., Schöpfer J., Keil W. Deaths Due to Physical Restraint. Dtsch. Arztebl. Int. 2012;109:27–32. doi: 10.3238/arztebl.2012.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cadore E.L., Moneo A.B.B., Mensat M.M., Muñoz A.R., Casas-Herrero A., Rodríguez-Mañas L., Izquierdo M. Positive effects of resistance training in frail elderly patients with dementia after long-term physical restraint. Age. 2013;36:801–811. doi: 10.1007/s11357-013-9599-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gastmans C., Milisen K. Use of physical restraint in nursing homes: Clinical-ethical considerations. J. Med. Ethics. 2006;32:148–152. doi: 10.1136/jme.2005.012708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Möhler R., Meyer G. Attitudes of nurses towards the use of physical restraints in geriatric care: A systematic review of qualitative and quantitative studies. Int. J. Nurs. Stud. 2014;51:274–288. doi: 10.1016/j.ijnurstu.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Goethals S., De Casterlé B.D., Gastmans C. Nurses’ ethical reasoning in cases of physical restraint in acute elderly care: A qualitative study. Med. Health Care Philos. 2012;16:983–991. doi: 10.1007/s11019-012-9455-z. [DOI] [PubMed] [Google Scholar]
- 24.Lan S.-H., Lu L.-C., Lan A.S.-J., Chen J.-C., Wu W.-J., Chang S.-P., Lin L.-Y. Educational intervention on physical restraint use in long-term care facilities—Systematic review and meta-analysis. Kaohsiung J. Med. Sci. 2017;33:411–421. doi: 10.1016/j.kjms.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 25.Higgins J.P., Green S. Cochrane Handbook for Systematic Reviews of Interventions. John Wiley & Sons; Hoboken, NJ, USA: 2011. [Google Scholar]
- 26.Testad I., Mekki T.E., Førland O., Øye C., Tveit E.M., Jacobsen F., Kirkevold O. Modeling and evaluating evidence-based continuing education program in nursing home dementia care (MEDCED)-training of care home staff to reduce use of restraint in care home residents with dementia. A cluster randomized controlled trial. Int. J. Geriatr. Psychiatry. 2016;31:24–32. doi: 10.1002/gps.4285. [DOI] [PubMed] [Google Scholar]
- 27.Abraham J., Kupfer R., Behncke A., Berger-Höger B., Icks A., Haastert B., Meyer G., Köpke S., Möhler R. Implementation of a multicomponent intervention to prevent physical restraints in nursing homes (IMPRINT): A pragmatic cluster randomized controlled trial. Int. J. Nurs. Stud. 2019;96:27–34. doi: 10.1016/j.ijnurstu.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 28.Evans L.K., Strumpf N.E., Allen-Taylor S.L., Capezuti E.A., Maislin G., Jacobsen B. A clinical trial to reduce restraints in nursing homes. J. Am. Geriatr. Soc. 1997;45:675–681. doi: 10.1111/j.1532-5415.1997.tb01469.x. [DOI] [PubMed] [Google Scholar]
- 29.Huizing A.R., Hamers J.P., Gulpers M.J.M., Berger M.P.F. Short-term effects of an educational intervention on physical restraint use: A cluster randomized trial. BMC Geriatr. 2006;6:17. doi: 10.1186/1471-2318-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huizing A.R., Hamers J.P.H., Gulpers M.J.M., Berger M.P.F. A Cluster-Randomized Trial of an Educational Intervention to Reduce the Use of Physical Restraints with Psychogeriatric Nursing Home Residents. J. Am. Geriatr. Soc. 2009;57:1139–1148. doi: 10.1111/j.1532-5415.2009.02309.x. [DOI] [PubMed] [Google Scholar]
- 31.Huizing A.R., Hamers J.P., Gulpers M.J., Berger M.P.F. Preventing the use of physical restraints on residents newly admitted to psycho-geriatric nursing home wards: A cluster-randomized trial. Int. J. Nurs. Stud. 2009;46:459–469. doi: 10.1016/j.ijnurstu.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 32.Koczy P., Becker C., Rapp K., Klie T., Beische D., Büchele G., Kleiner A., Guerra V., Rißmann U., Kurrle S., et al. Effectiveness of a Multifactorial Intervention to Reduce Physical Restraints in Nursing Home Residents. J. Am. Geriatr. Soc. 2011;59:333–339. doi: 10.1111/j.1532-5415.2010.03278.x. [DOI] [PubMed] [Google Scholar]
- 33.Testad I., Aasland A.M., Aarsland D. The effect of staff training on the use of restraint in dementia: A single-blind randomised controlled trial. Int. J. Geriatr. Psychiatry. 2005;20:587–590. doi: 10.1002/gps.1329. [DOI] [PubMed] [Google Scholar]
- 34.Testad I., Ballard C., Brønnick K., Aarsland D. The Effect of Staff Training on Agitation and Use of Restraint in Nursing Home Residents with Dementia. J. Clin. Psychiatry. 2010;71:80–86. doi: 10.4088/JCP.09m05486oli. [DOI] [PubMed] [Google Scholar]
- 35.Rovner B.W., Steele C.D., Shmuely Y., Folstein M.F. A Randomized Trial of Dementia Care in Nursing Homes. J. Am. Geriatr. Soc. 1996;44:7–13. doi: 10.1111/j.1532-5415.1996.tb05631.x. [DOI] [PubMed] [Google Scholar]
- 36.Gulpers M.J., Bleijlevens M.H.C., Ambergen T., Capezuti E.A., Van Rossum E., Hamers J.P. Reduction of Belt Restraint Use: Long-Term Effects of the EXBELT Intervention. J. Am. Geriatr. Soc. 2013;61:107–112. doi: 10.1111/jgs.12057. [DOI] [PubMed] [Google Scholar]
- 37.Gulpers M.J., Bleijlevens M.H.C., Ambergen T., Capezuti E.A., Van Rossum E., Hamers J.P.H. Belt Restraint Reduction in Nursing Homes: Effects of a Multicomponent Intervention Program. J. Am. Geriatr. Soc. 2011;59:2029–2036. doi: 10.1111/j.1532-5415.2011.03662.x. [DOI] [PubMed] [Google Scholar]
- 38.Gulpers M.J., Bleijlevens M.H., Capezuti E.A., Van Rossum E., Ambergen T., Hamers J.P. Preventing belt restraint use in newly admitted residents in nursing homes: A quasi-experimental study. Int. J. Nurs. Stud. 2012;49:1473–1479. doi: 10.1016/j.ijnurstu.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 39.Capezuti E.A., Maislin G., Strumpf N., Evans L.K. Side Rail Use and Bed-Related Fall Outcomes among Nursing Home Residents. J. Am. Geriatr. Soc. 2002;50:90–96. doi: 10.1046/j.1532-5415.2002.50013.x. [DOI] [PubMed] [Google Scholar]
- 40.Bellenger E.N., Ibrahim J.E., Kennedy B., Bugeja L. Prevention of physical restraint use among nursing home residents in Australia: The top three recommendations from experts and stakeholders. Int. J. Older People Nurs. 2019;14:e12218. doi: 10.1111/opn.12218. [DOI] [PubMed] [Google Scholar]
- 41.Bellenger E.N., Ibrahim J.E., Lovell J.J., Bugeja L. The Nature and Extent of Physical Restraint–Related Deaths in Nursing Homes: A Systematic Review. J. Aging Health. 2017;30:1042–1061. doi: 10.1177/0898264317704541. [DOI] [PubMed] [Google Scholar]
- 42.Goethals S., De Casterlé B.D., Gastmans C. Nurses’ decision-making in cases of physical restraint: A synthesis of qualitative evidence. J. Adv. Nurs. 2011;68:1198–1210. doi: 10.1111/j.1365-2648.2011.05909.x. [DOI] [PubMed] [Google Scholar]
- 43.Heinze C., Dassen T., Grittner U. Use of physical restraints in nursing homes and hospitals and related factors: A cross-sectional study. J. Clin. Nurs. 2011;21:1033–1040. doi: 10.1111/j.1365-2702.2011.03931.x. [DOI] [PubMed] [Google Scholar]
- 44.Minnick A.F., Mion L.C., Johnson M.E., Catrambone C., Leipzig R. Prevalence and Variation of Physical Restraint Use in Acute Care Settings in the US. J. Nurs. Sch. 2007;39:30–37. doi: 10.1111/j.1547-5069.2007.00140.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.