Abstract
Uterine arteriovenous malformation (AVM) is an uncommon but potentially life-threatening cause of postpartum hemorrhage (PPH). AVMs often present with intermittent or profuse vaginal bleeding in a woman with a history of uterine instrumentation. Transvaginal ultrasound is the initial imaging method used for diagnosis. Management depends on the patient's hemodynamic stability and desire for future pregnancy. Uterine artery embolization (UAE) is the initial treatment option for women of reproductive age. Due to limited evidence, there are no guidelines for the management of failed UAE. Here we report a case of uterine AVM following a cesarean section that failed initial management with UAE and required emergency hysterectomy.
Keywords: Uterine arteriovenous malformation, Uterine artery embolization, Postpartum hemorrhage
Abbreviations: AVM, Arteriovenous malformation; UAE, Uterine artery embolization; PPH, postpartum hemorrhage
Highlights
-
•
Uterine arteriovenous malformation (AVM) is a rare cause of postpartum hemorrhage.
-
•
Acquired uterine arteriovenous malformations are associated with a history of surgical instrumentation of the uterus.
-
•
Transvaginal ultrasound is the initial imaging method used for diagnosis.
-
•
Uterine artery embolization is the first-line treatment for uterine arteriovenous malformations.
-
•
Hysterectomy is a definitive treatment for uterine arteriovenous malformations refractory to embolization.
1. Introduction
Uterine arteriovenous malformation (AVM) is a rare but potentially life-threatening cause of postpartum hemorrhage (PPH) [1]. Defined as an anomalous vascular communication between the uterine arterial and venous systems, uterine AVMs are traditionally categorized as congenital or acquired. Congenital uterine AVM is postulated to arise from a failure of differentiation during fetal angiogenesis [2,3]. Acquired uterine AVMs predominantly occur in women of reproductive age with a history of surgical instrumentation of the uterus, such as cesarean section or dilation and curettage (D&C) [1,3]. Transvaginal ultrasound with color flow and spectral analysis is the preferred initial imaging modality for diagnosis [2,4,5]. Conventional angiography is the reference standard for diagnosis but is primarily utilized for uterine artery embolization (UAE), particularly in women who wish to preserve fertility [2,3]. Here we report a case of life-threatening PPH secondary to an acquired uterine AVM that failed initial management with UAE and subsequently required emergency hysterectomy.
2. Case Presentation
A 26-year-old primigravida with a low-risk pregnancy presented to labor and delivery for induction of labor at 39 weeks and 3 days of gestation. She experienced arrest of descent in the second stage of labor and underwent a primary low transverse cesarean section. The procedure was complicated by a left-sided hysterotomy extension and uterine atony with an estimated blood loss of 1200 ml. She otherwise had an uncomplicated hospital course and was discharged on postpartum day (PPD) 3.
On PPD 8 she presented with vaginal bleeding and was admitted for presumed endometritis. She was treated with intravenous antibiotics and had no further episodes of vaginal bleeding. Two days later she was discharged in stable condition.
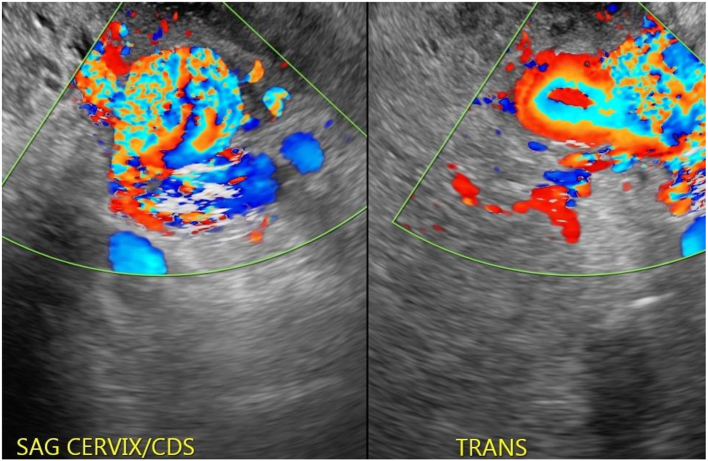
On PPD 14 she presented to the obstetrical triage unit with heavy vaginal bleeding. Her hemoglobin was 9.1 g/dl. Transvaginal ultrasound demonstrated a left-sided 27x16x30mm hypervascular mass with multidirectional flow adjacent to the cervix concerning for a uterine AVM (Fig. 1). Interventional radiology was consulted for diagnostic confirmation and possible UAE. Angiography confirmed the presence of an AVM (Fig. 2), which was fed by the left uterine artery with collateral flow from the vesicular artery. Injection of contrast dye into the right internal iliac artery demonstrated no filling of the malformation. Therefore, selective embolization of the left uterine and vesicular artery was performed with Gelfoam.
Fig. 1.
Transvaginal US with color flow demonstrating a hypervascular lesion with turbulent blood flow.
Fig. 2.
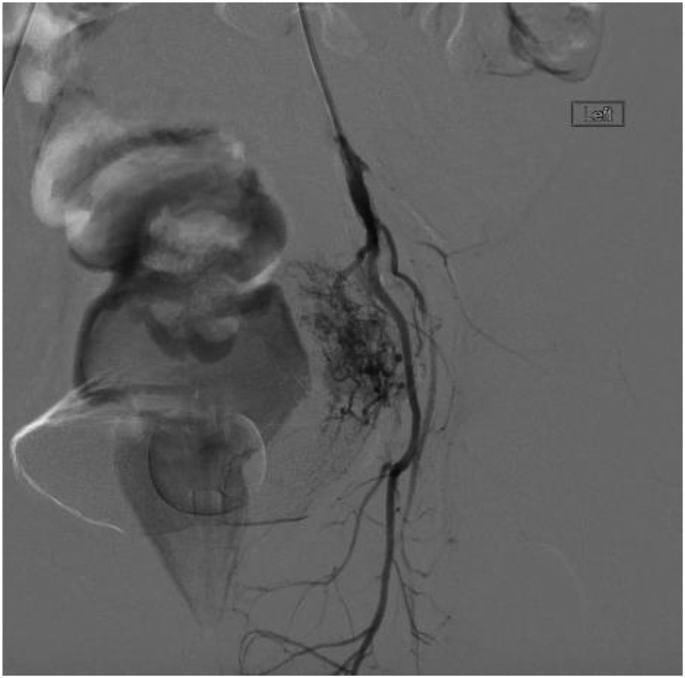
Angiography demonstrating the uterine AVM.
The procedure was technically successful with no flow visible to the AVM after embolization (Fig. 3). However, shortly after arrival to the medical floor the patient developed brisk vaginal bleeding accompanied by hypotension and tachycardia suggesting rupture of the AVM. Fluid resuscitation was initiated with isotonic saline and transfusion of two units of packed red blood cells. Her repeat hemoglobin was 5.6 g/dl, prompting activation of the massive transfusion protocol. Given her ongoing vaginal bleeding with concomitant hemodynamic instability, the decision was made to proceed with emergency hysterectomy. The procedure was uncomplicated. Intraoperative blood loss was 500 ml. An additional 1500 ml of blood loss was estimated to have occurred prior to the procedure. After surgery, the patient was transferred to the intensive-care unit. She remained hospitalized until postoperative day 7, when she was discharged home in stable condition.
Fig. 3.
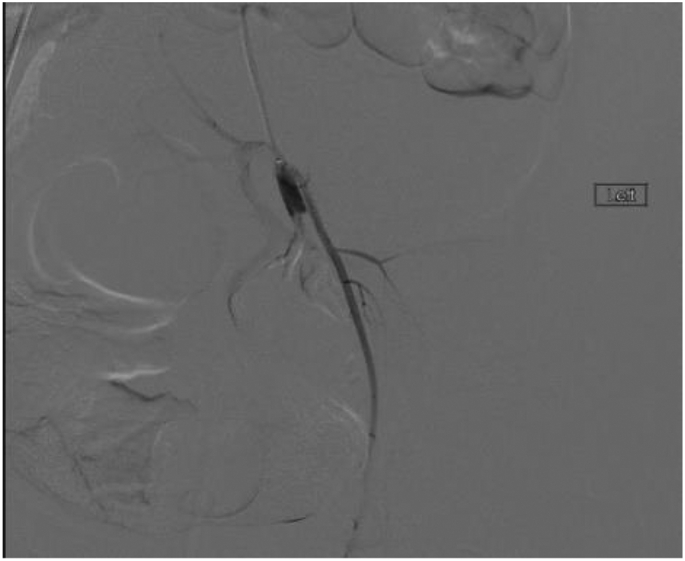
Angiography demonstrating successful embolization of the uterine AVM.
3. Discussion
Uterine AVM is a rare cause of PPH. The true incidence of the condition is not well established, with just over 100 cases being reported in the literature [5]. By convention, these lesions are categorized as congenital or acquired. The congenital variant is thought to arise from a defect in the differentiation of the primitive fetal vasculature. The acquired form is the corollary of a traumatic insult to the uterine vasculature. Acquired AVMs have been associated with D&C, cesarean section, uterine myomectomy, gestational trophoblastic disease, uterine infection, and gynecological malignancy [1,3]. As this patient's uterine AVM became apparent 8 days after a cesarean section that was complicated by a hysterotomy extension, we believe this case represented an acquired uterine AVM.
In the postpartum period, uterine AVM presents with intermittent or profuse vaginal bleeding [1,3]. Anemia and hemodynamic compromise may occur with up to 30% of cases requiring transfusion of blood products [6]. Interventions aimed at terminating postpartum bleeding, such as D&C, could prove catastrophic due to disruption of the delicate vessel mass, and therefore should be avoided [3,6].
Diagnosis of uterine AVM cannot be established on clinical grounds. Thus, imaging is necessary for prompt detection and management [4]. The preferred initial imaging modality for diagnosis is transvaginal ultrasound with color doppler and spectral analysis [2,4,5]. Sonographic grayscale findings of anechoic or hypoechoic tubular structures within the myometrium are suggestive, but nonspecific for diagnosis [2]. Consequently, the addition of color doppler is necessary for confirmation [4]. Characteristic findings include a hypervascular lesion with low resistance and high peak systolic velocity [4,6]. Digital subtraction angiography remains the reference standard for diagnosis, but is more commonly performed with the intent of therapeutic intervention [1,3]. Computed tomography (CT) and magnetic resonance imaging (MRI) offer additional noninvasive methods for diagnosis, which also permit evaluation of the extent of the AVM and adjacent pelvic structures [2].
Therapeutic options for uterine AVM are determined by the hemodynamic stability of the patient as well as their desire to preserve fertility. In the setting of hemorrhage, efforts are directed at resuscitation with emphasis on achieving hemostasis and maintaining tissue perfusion [3].
tWith the emergence of transcatheter UAE, surgical therapies have largely been supplanted as the initial treatment option [1,2]. UAE has demonstrated excellent efficacy, with a success rate of 91% [2]. Furthermore, the procedure lacks the invasiveness of surgery and gives the patient the ability to retain her reproductive capacity [3]. Nevertheless, some patients may require repeat embolization or other therapies. In a systematic review by Yoon et al. [2], 14.8% of patients who initially underwent UAE for uterine AVM ultimately required surgical intervention. Presently, no guidelines exist for those who fail initial embolization as no comparative studies have been conducted evaluating the effectiveness of repeat embolization versus medical therapy or hysterectomy [2].
Hysterectomy is a definitive treatment for uterine AVM, but it is primarily utilized in resource-poor settings or when a contraindication to UAE exists. It also remains a viable option for those who no longer desire fertility or, as in our case, when UAE fails [3]. Less commonly used surgical techniques for the treatment of uterine AVM include ligation of the uterine or internal iliac arteries, laparoscopic excision, operative hysteroscopy, or laparoscopic bipolar coagulation of the uterine arteries [1,3].
4. Conclusion
Early detection of uterine AVM in the postpartum patient with undifferentiated bleeding is necessary to mitigate morbidity primarily attributed to hemorrhage. All women with PPH and a history of uterine instrumentation should undergo transvaginal ultrasound with color doppler to exclude the possibility of this potentially life-threatening abnormality. UAE should be the first-line treatment option for uterine AVM, but obstetricians should be prepared to intervene should embolization fail to resolve bleeding.
Acknowledgments
Contributors
Nathaniel Gallagher drafted and reviewed the manuscript.
Matthew Cincotta drafted and reviewed the manuscript.
Hisham Keblawi reviewed and revised the manuscript.
David Jude reviewed the manuscript.
Michael Korona assisted with review of the manuscript as well as imaging interpretation and selection.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
No source of funding supported the publication of this case report.
Patient Consent
Obtained.
Provenance and Peer Review
This case report was peer reviewed.
References
- 1.Grivell Rosalie M., Kym M., Reid, Mellor Amy. Obstetrical and Gynecological Survey 60, no. 11. November 2005. Uterine arteriovenous malformations: a review of the current literature; pp. 761–767. [DOI] [PubMed] [Google Scholar]
- 2.Yoon Daniel, Jones Megan, Taani Jamal, Buhimschi Catalin, Dowell Joshua. A systematic review of acquired uterine arteriovenous malformations: pathophysiology, diagnosis, and Transcatheter treatment. Am. J. Perinatol. Rep. October 12, 2015;06(01) doi: 10.1055/s-0035-1563721. e6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Annaiah Katimada, Thangamma, Sreenivasan Sreejith Kodakkattil. Uterine arteriovenous malformations: clinical implications. Obstet. Gynaecol. October 2015;17(4):243–250. doi: 10.1111/tog.12218. [DOI] [Google Scholar]
- 4.Kelly S.M., Belli A.M., Campbell S. Arteriovenous malformation of the uterus associated with secondary postpartum hemorrhage. Ultrasound Obstet. Gynecol. June 2003;21(6):602–605. doi: 10.1002/uog.148. [DOI] [PubMed] [Google Scholar]
- 5.Scribner Drew, Fraser Robert. Diagnosis of acquired uterine arteriovenous malformation by Doppler ultrasound. J. Emergency Med. August 2016;51:168–171. doi: 10.1016/j.jemermed.2016.04.028. no. 2. [DOI] [PubMed] [Google Scholar]
- 6.Timmerman D., Wauters J., Van Calenbergh S., Van Schoubroeck D., Maleux G., Van Den Bosch T., Spitz B. Color doppler imaging is a valuable tool for the diagnosis and management of uterine vascular malformations. Ultrasound Obstet. Gynecol. June 2003;21(6):570–577. doi: 10.1002/uog.159. [DOI] [PubMed] [Google Scholar]