Abstract
Background
Malaria is one of the major causes of morbidity and mortality among school-age children (SAC) in sub-Saharan Africa. SAC account for more than 60% of the reservoir of malaria transmission, but they are given less emphasis in prioritizing malaria prevention interventions. This study was aimed at assessing the ownership of long-lasting insecticide treated bed nets (LLINs), its utilization and factors associated with ownership of LLINs by households and LLINs utilization among SAC in malaria-prone areas of Dara Mallo and Uba Debretsehay districts in Southern Ethiopia, October to December 2019.
Methods
This study is part of a baseline assessment in a cluster-randomized controlled trial. The data was collected through interview and observation, following a structured questionnaire, of 2261 SAC households. Univariable and multivariable multilevel logistic regressions were used to assess the association between LLINs ownership and utilization and potential predictor variables. Odds ratio (OR) and corresponding 95% confidence interval (CI) were used to determine the strength and statistical significance of association.
Results
The ownership of at least one LLIN by households of SAC was about 19.3% (95% CI 17.7–21.0%) but only 10.3% % (95% CI 7.7–13.7%) of these households had adequate access of bed nets to the household members. Ownership of bed net was marginally affected by living in semi-urban area (adjusted OR = 2.6; 95% CI 1.0–6.9) and occupational status of the household head being a civil servant (adjusted OR = 2.7; 95% CI 0.9–7.9). About 7.8% (95% CI 6.7–10.0%) of all SAC participated in the study and 40.4% (95% CI 57.4–66.7%) of children in households owning at least one LLIN passed the previous night under LLIN. LLIN utilization by SAC conditional to presence of at least one net in the household was significantly correlated with education level of mother above grade 6 (adjusted OR = 3.4; 95% CI 1.3–9.3) and the household size to bed net ratio less than or equal to 2 (adjusted OR = 20.7; 95% CI 4.7–132.5).
Conclusion
Ownership of bed net was lower than universal coverage of at least one bed net for two individuals. It is important to monitor replacement needs and educate mothers with low education level with their SAC on the benefit of consistent utilization of bed nets.
Keywords: Llins ownership, Utilization, Associated factors, School-age children, Southern Ethiopia
Background
Malaria is one of the leading causes of morbidity and mortality among infectious diseases in the world [1]. It is caused by a protozoan parasite of the genus Plasmodium and transmitted through the bite of the female Anopheles mosquito. There are five known species of Plasmodium that cause malaria in humans: Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale, Plasmodium malariae, and Plasmodium knowlesi [2]. An estimated 228 million malaria cases and 405,000 malaria deaths occurred in the world in 2018. Of these, 93% of cases and 94% of deaths due to malaria occurred in the African region [3].
There has been substantial decrease in the prevalence of malaria globally and also in the African region in the last two decades. Between 2010 and 2015, malaria incidence rates (new malaria cases) fell by 21% and the malaria mortality rate by 31% in the African region [4]. However, the rate of change in decline of malaria incidence remained 57 per 1000 at-risk population per year from 2014 to 2018 [3].
Malaria is seasonal in most parts of Ethiopia with the highest transmission season between September and October following the main rainy season from June to August [4, 5]. A study carried out in North Gonder zone revealed that the highest incidence of malaria was observed between June and November while the lowest transmission period was from December to early April [6]. The number of malaria cases in September, October, November, May, June, and July were above the average malaria cases in Boricha district in Southern Ethiopia, while those in March, January, February, December, August, and April were below average [7].
The National Malaria Control Programme (NMCP) deployed by the Ethiopian government and partners has led to a promising decrease in the burden of malaria. As indicated by data collected from 41 hospitals in Ethiopia, the overall malaria inpatient cases were 54% lower and malaria deaths were 68% lower in 2011 than that predicted by the trends during 2001–2005 [8]. Moreover, in 2015, deaths due to malaria decreased by 40% compared to the number of deaths due to malaria in 2005 [9]. Decreased exposure of children under the age of 5 years resulted in delayed development of immunity in their growth and nowadays school-aged children (SAC) have become a highly susceptible group of people [10–12]. Stratified analysis of studies targeting the general population, as well as studies focused on SAC, revealed that the burden of malaria was higher among this group of the population in Ethiopia [13–15]. The consequence of malaria infection on children affects their physical growth, mental development and overall economic development of the country [16, 17]. Above all, they were responsible for about 60% of infection to the mosquito vector for the transmission of the disease in all seasons [18].
The long-lasting insecticide-treated net (LLIN) is the cornerstone of malaria prevention in sub-Saharan Africa (SSA). Its effectiveness was dependent on universal coverage as well as consistent utilization [4]. Utilization of LLINs reduces the clinical attack of malaria, Plasmodium infection and death due to malaria. It reduced child mortality of all causes by 17%, which corresponds to 5.6 lives each year for every 1000 children protected compared to those who did not use bed nets. In addition, it reduced incidence of uncomplicated episodes of falciparum malaria by almost half [19].
In Ethiopia, LLIN planning is based on the WHO recommendation of one net for 1.8 people. The nets are distributed through rolling mass campaign every 3 years [20]. National coverage of bed net ownership and utilization conditional to ownership in Ethiopia were 40% and 61%, respectively [13]. However, a cross-sectional survey conducted in different parts of the country targeting different population segments indicated that coverage and utilization differ widely. In Jima, for example, overall ownership and utilization were 70.9% and 38.4%, respectively, in the community [21]. Near Gilgel Gibe hydroelectric power project, 56.6% of the households owned at least one bed net and of those, 60% slept under bed nets on the night preceding the survey [22]. In Shashogo district in southern Ethiopia, ownership and utilization of bed nets was very low. Only 15.8% of pregnant women’s households owned a bed net and half of those owning bed nets utilized them [23]. However, the coverage and utilization were high in Mirab Abay district in Gamo Gofa zone with, respectively, 89.9% and 85.5% [24].
There are few studies that assessed the utilization of bed nets by SAC. In studies comparing bed-net utilization between SAC and other population segments, SAC less likely used bed nets [16, 17]. Despite SAC becoming at high risk of malaria and malaria-associated morbidities, their access to and benefit from existing malaria prevention interventions is not well addressed. Previous studies mainly focused on assessing access to malaria prevention interventions among pregnant women and children under 5 years old. LLINs are one of the major malaria prevention interventions in use in SSA. Assessing coverage of bed-net ownership and utilization by households of SAC, and their associated risk factors are important for optimizing malaria responses in Ethiopia and similar settings in SSA in light of targets set in for global technical strategy of malaria, 2016–2030. This study was conducted in Uba Debretsehay and Dara Mallo districts in the former Gamo Gofa Zone. These districts were selected based on the burden of malaria contribution to the total malaria cases in the Zones. Based on the recent annual report of the districts health offices in June 2020, there were a total of 8391 confirmed malaria cases out of a total of 63,953 people residing in malarious area in Uba Debretsehay district while the respective numbers in Dara Mallo district were 7666 and 38,043. A total of 14,440 bed nets which is equivalent to 96% coverage in Dara Mallo district and 32,500 bed nets that is equivalent to 100% coverage were distributed in June 2017.
Methods
Study setting
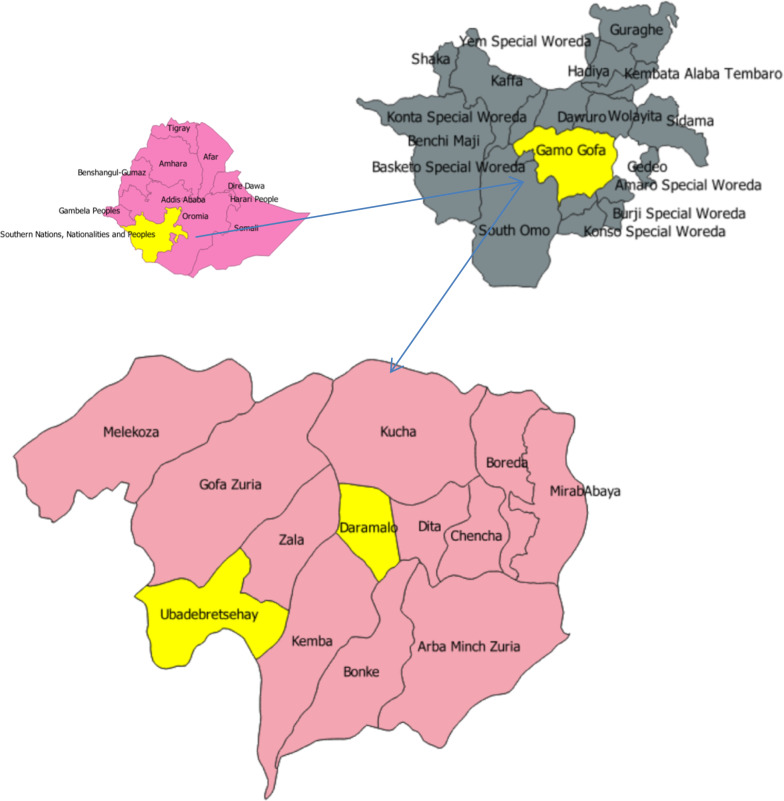
The study was conducted in Dara Mallo and Uba Debretsehay districts in Gamo and Gofa Zones. Both zones are found in Southern Nations, Nationalities and Peoples Region, which is the third populous region in Ethiopia. These districts are found in the western part of Arba Minch town, which is the capital of the former Gamo Gofa Zone (Fig. 1). Based on the 2007 national census, 150,145 people were living in the two districts, of whom 76,550 (51%) were male [25]. According to the recent update of the population by the respective districts, there were a total of 94,396 people in Uba Debretsehay district and 110,207 people in Dara Mallo district.
Fig. 1.
Location map of two districts selected from former Gamo Gofa zone, in Southern Nations, Nationalities and peoples region, Ethiopia
Study design and sample size
A cross-sectional study was undertaken by recruiting 2261 children from 32 schools in the study area. The number of participants involved in this study was about 98.1% of the estimated sample size. The sample size estimated was 2304 SAC and their households. The estimated sample size is used to evaluate the effect of malaria prevention education on malaria, anaemia and cognitive development among SAC in the study area. This sample size was estimated by using formula recommended to calculate sample size for cluster randomized controlled trials [26, 27] for each of the two parallel arms. The assumptions used were 11.04% and 18.4% prevalence of malaria with and without the intervention, respectively; 95% level of confidence, 80% power, 72 cluster size and 0.025 intraclass correlation coefficient (ICC) with the calculated design effect of 2.775 and 15% loss to follow-up or non-response rate.
Sampling techniques and data collection
A total of 3204 children attending primary education were approached at 32 primary schools. It had been planned to recruit 32 schools by using simple random sampling technique, but only 32 primary schools in malarious areas in the two districts could be recruited. Seventy-two children from grade 1 to 3 were selected using systematic random sampling technique from eligible children in each section of the students with a class roster as the sampling frame. All participants involved in the trial were included to address the research objective. The number of participants in the trial from each grade level (grade 1 to 3) was determined by the relative contribution of each grade level to the total enrolment of students in each school. Children who were attending their education in the schools during the data collection period were included in the study while those mentally not fit to respond to questions directed to them and with physical problems to measure their height were excluded from the study. Children enrolled to the study were used to trace their households. Participants’ households were approached by trained data collectors for interview. A pretested, structured questionnaire was used to collect data on demographics, water source, toilet structure, household assets and bed nets. The questions were adapted to local context from the Demographic and Health Surveys (DHS) malaria indicator survey household questionnaire [28]. The questionnaire was uploaded to tablets in Open Data Kit (ODK) data collection tool. The data collectors were trained on how to use the data collection tool and ethical procedures. They interviewed mothers or caregivers in conditions when the selected child mother was not alive, observed the toilet structure and the number and position (hung over sleeping place or not) of bed nets in the households.
Four indicators of malaria prevention measures by bed net utilization in the current study were used, but ownership and utilization of bed nets by SAC conditional to presence of at least one bed net in the household were dependent variables.
Indicator I: ownership, which is defined as SAC households those had at least one LLIN among SAC households participated in the survey.
Indicator II: utilization, which is defined as proportion of SAC passed the previous night under LLINs irrespective of ownership of LLINs.
Indicator III: conditional utilization, which is defined as proportion of SAC passed the previous night under LLINs conditional to presence of at least one LLIN in the household.
Indicator IV: access, which is defined as proportion of SAC households those had at least one bed nets for two household members among those owning at least one LLINs.
Indicator V: utilization conditional to access, which is defined as proportion of SAC passed the previous night under LLINs conditional to bed net access in the household [29].
In addition to SAC related indicators, any person from the household passed the previous night under bed net irrespective of presence or conditional to presence of at least one LLIN in the household were also assessed.
Indicator VI: any membered utilized, which is defined as any member of SAC household that passed the previous night under bed net among all surveyed SAC households.
Indicator VIII: conditional any membered utilized, which is defined as any member of SAC household that passed the previous night under bed net conditional to presence of at least one LLIN in the household.
Data analysis
The data collected by using ODK data collection tool with tablet apparatus were converted to Microsoft Excel using ODK Briefcase. These data are imported to RStudio version 4.0.0 statistical software and STATA version 14 to predict the principal components (PCA). The variables used in predicting the wealth index of the household were the type of toilet used by the household; the source of drinking water for the household; the presence of sponge mattress in the household, the floor of which the house is constructed; the outer cover of the house, the total number of milk cows in the house; the number of other cows in the house; the number of goats and the number of poultry in the households. The predicted index from PCA is categorized into 4 quartiles to determine the wealth index of the households. Cleaned data were subjected to descriptive statistical analysis, such as proportion for categorical variables and plots and descriptive measures for continuous data. The survey data used in this study indicate a hierarchical nature in which children included were nested within the schools. Children within the same school will be similar to each other than students in another school. Thus, mixed effects multilevel logistic regression with random intercepts by schools for the outcome variables was used to assess the individual level fixed effect of correlates on the outcome variables. In the analysis of factors influencing ownership and use of bed net glmer command in lme4 R package was used. In the analysis of factors influencing bed net utilization, children with at least one bed net in their household were included. Odds ratio (OR) and corresponding 95% level of confidence (CI) were used to assess the strength of association between bed-net ownership or utilization and potential predictor variables. Variables that are significantly associated with bed net ownership and utilization in univarite multilevel logistic regression were taken to multivariate multilevel logistic regression. The fit of the mode in predicting the outcome variables were checked by Akaike Information Criterion (AIC). The averages of the household coordinates taken by global positioning system (GPS) were used to represent the coordinates of each school. The geospatial data was added to Quantum Geographical Information System (QGIS) to present the ownership and utilization percentages at school level.
Ethical consideration
The trial was approved with written consent procedure to be followed by the Institutional Research Ethics review Board (IRB) in College of Medicine and Health Sciences, Arba Minch University with the reference number of IRB/154/12. Official permission letter to conduct the research was submitted to district health offices and education offices in Dara Mallo and Uba Debretsehay districts. Support letters written by the respective education offices were given to each participating school and written consent was obtained from school head teachers. Parents of the selected SAC were invited to come to the schools and written consent was obtained before data collection at school and household level, which was documented in College of Medicine and Health Sciences, Arba Minch University.
Results
A total of 2261 SAC and their households participated in this study: 1419 from Uba Debretsehay and 842 from Dara Mallo districts. Of participating SAC, 50.3% were female and 85.5% were from rural area. The mean age of children was 8.7 years with standard deviation (SD) of 1.6 years. Some 39.1, 28.1 and 32.8% of the children were attending education in grade 1, 2 and 3, respectively. The mean household size was 7.0 with the standard deviation of 2.0. The detailed socio-demographic characteristics of the participated SAC households were presented in Table 1.
Table 1.
Socio-demographic characteristics of participants involved in Dara Mallo and Uba Debretsehay districts, Southern Ethiopia, 2019
| Factor | Value categories | Frequency (%) |
|---|---|---|
| Place of residence | Rural | 1928 (85.3) |
| Semi-urban | 185 (8.2) | |
| Urban | 148 (6.5) | |
| Gender of household head | Male | 2103 (93.0) |
| Female | 158 (7.0) | |
| Age of household head | ≤ 34 | 584 (25.8) |
| 35–49 | 1501 (66.4) | |
| ≥ 50 | 176 (7.8) | |
| Occupation of household head | Farmer | 1852 (81.9) |
| Civil servant | 158 (7.0) | |
| Merchant | 115 (5.1) | |
| Housewife | 72 (3.2) | |
| Daily laborer | 31 (1.4) | |
| Others | 33 (1.5) | |
| Educational status of household head | Illiterate | 1311 (58.0) |
| Literate | 949 (42.0) | |
| Ethnicity | Gofa | 1156 (51.1) |
| Gamo | 928 (41.0) | |
| Amhara | 31 (1.4) | |
| Others | 146 (6.5) | |
| Age of child’s mother (caretaker) | ≤ 34 | 1472 (65.1) |
| 35–49 | 751 (33.2) | |
| ≥ 50 | 38 (1.7) | |
| Occupation of child’s mother (caretaker) | Housewife | 1867 (82.6) |
| Farmer | 189 (8.4) | |
| Merchant | 89 (3.9) | |
| Employee | 82 (3.6) | |
| Others | 34 (1.5) | |
| Educational status of mother (caretaker) | Illiterate | 1682 (74.4) |
| Literate | 579 (25.6) | |
| Gender of SAC | Female | 1137 (50.3) |
| Male | 1123 (49.7) | |
| Grade of SAC | Grade 1 | 884 (39.1) |
| Grade 2 | 635 (28.1) | |
| Grade 3 | 740 (32.8) | |
| Household size | Less than or equal to 5 | 457 (20.2) |
| Greater than 5 | 1804 (79.8) |
Ownership of LLINs
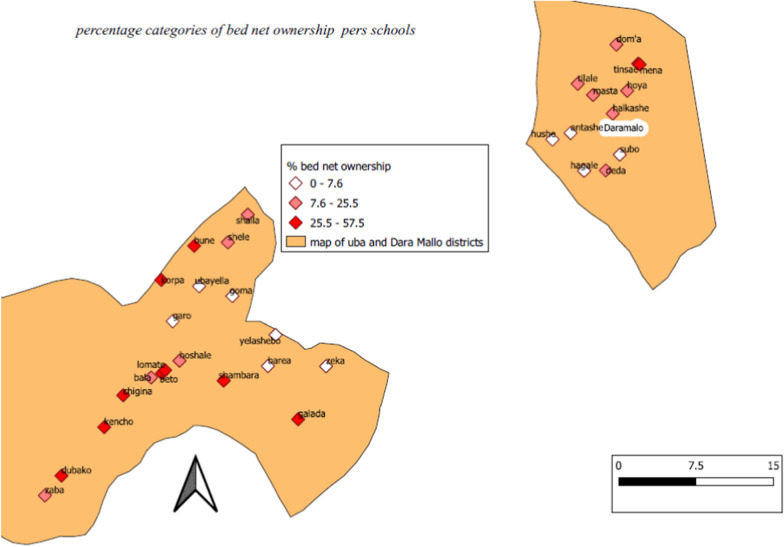
Ownership of at least one LLIN at household level was 19.3% with 95% CI of 17.7–21.0%. The mean number of bed nets in a household owning bed nets was 1.8 (SD = 0.9), while 45 of the participated SAC households had adequate numbers of bed nets (at least one bed net for 2 household members). Overall ownership of at least one bed net and adequate access per district were indicated in Table2. There was wide difference in ownership of bed nets in households per school where children attend education (Fig. 2).
Table 2.
Indicators of LLIN ownership, access and utilization of bed net by anyone from the household or SAC in Dara Mallo and Uba Debretsehay districts, Southern Ethiopia
| Indicator | Total | Uba Debretsehay | Dara Mallo | |||
|---|---|---|---|---|---|---|
| n/N | % (95% CI) | n/N | % (95% CI) | n/N | % (95% CI) | |
| Indicator I | 436/2261 | 19.3 (17.7–21.0) | 318/1419 | 22.4 (20.3–24.7) | 118/842 | 14.0 (11.8–16.6) |
| Indicator VI | 271/2261 | 12.0 (10.7–13.4) | 179/1419 | 12.6 (11.0–14.5) | 92/842 | 10.9 (8.9–13.3) |
| Indicator II | 176/2261 | 7.8 (6.7–9.0) | 133/1419 | 9.3 (7.9–11.0) | 43/842 | 5.1 (3.8–6.9) |
| Indicator III | 176/436 | 40.4 (35.8–45.2) | 133/318 | 41.8 (36.4–47.5) | 43/118 | 36.4 (27.9–45.9) |
| Indicator VII | 271/436 | 62.2 (57.4–66.7) | 179/318 | 56.3 (50.6–61.8) | 92/118 | 78.0 (69.2–84.9) |
| Indicator IV | 45/436 | 10.3 (7.7–13.7) | 21/318 | 6.6 (4.2–10.1) | 9/118 | 7.6 (3.8–14.4) |
| Indicator V | 30/45 | 66.7 (50.9–79.5) | 21/35 | 60 (42.2–75.6) | 9/10 | 90.0 (54.1–99.5) |
Fig. 2.
Percentage of bed net ownership among households per schools where participated children attend their education
In univarite multilevel logistic regression analysis, the ownership of bed nets was affected by characteristics related to place of residence, household head occupation, maternal (caretaker) occupation, household head education, maternal (caretaker) education, maternal (caretaker) education level and socio-economic status. SAC households living in semi-urban area, literate educational status of the household head, literate educational status of mother (caretaker), education level of mother (caretaker) higher than grade 6 and being employee occupational status of the mother (caretaker), being employee or other occupational status of the household head and being in the 2nd or 4th quartile of the household wealth index positively and statistically significantly affected ownership of LLINs by SAC households. However, after fitting the model to multivariable multilevel logistic regression, none of the above factors significantly influenced ownership of LLINs but being in semi-urban area (AOR = 2.6; 95% CI 1.0–6.9) and employee as occupation of the household head (AOR = 1.8; 95% CI 0.9–3.7) marginally significantly affected ownership of LLINs by SAC households. The crude and adjusted ORs and the corresponding 95% CI for each of variables were presented in Table 3.
Table 3.
Multilevel univariable and multivariable logistic regression analysis of factors affecting LLIN ownership of SAC households, 2019
| Factor | Value categories | Bed net owned | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| No (%) | Yes (%) | ||||
| Place of residence** | Rural | 1619 (84.0) | 309 (16.0) | 1 | 1 |
| Semi-urban | 121 (65.4) | 64 (34.6) | 2.6 (1.–12.4) | 2.6 (1.0–6.9) | |
| Urban | 85 (57.4) | 63 (42.6) | 2.3 (0.7–7.7) | 1.4 (0.5–4.4) | |
| Residence house is | Private | 1763 (81.3) | 405 (18.7) | 1 | |
| Not private | 62 (66.7) | 31 (33.3) | 1.2 (0.7–2.0) | ||
| Gender of household head | Male | 1701 (80.8) | 403 (19.2) | 1.2 (0.7–1.9) | |
| Female | 125 (79.1) | 33 (20.9) | 1 | ||
| Age of household head | ≤ 34 | 1 | |||
| 35–49 | 1 (0.76–1.32) | ||||
| ≥ 50 | 1 (0.6–1.5) | ||||
| Occupation of household head* | Farmer | 1563 (84.4) | 289 (15.6) | 1 | 1 |
| Civil servant | 52 (51.9) | 76 (48.1) | 2.6 (1.6–4.0) | 1.8 (0.9–3.7) | |
| Merchant | 81 (70.4) | 34 (29.6) | 1.6 (1.0–2.7) | 1.6 (0.8–1.6) | |
| Housewife | 56 (77.8) | 16 (22.2) | 1.2 (0.6–2.4) | 1.9 (0.6–5.6) | |
| Daily laborer | 25 (80.6) | 6 (19.4) | 0.7 (0.2–1.8) | 0.9 (0.2–4.0) | |
| Others | 18 (54.5) | 15 (45.5) | 2.5 (1.1–5.5) | 2.7 (0.9–7.9) | |
| Educational status of household head* | Illiterate | 1075 (84.9) | 188 (15.1) | 1 | 1 |
| Literate | 768 (75.6) | 248 (24.4) | 1.6 (1.2–2.1) | 0.7 (0.4–1.4) | |
| Age of child’s mother | ≤ 34 | 1188 (80.7) | 284 (19.3) | 1 | |
| 35–49 | 607 (80.8) | 144 (19.2) | 1.0 (0.7–1.2) | ||
| ≥ 50 | 30 (79.0) | 8 (21.0) | 0.9 (0.4–2.0) | ||
| Educational status of mother* | Illiterate | 1379 (84.1) | 260 (15.9) | 1 | |
| Literate | 446 (71.7) | 176 (28.3) | 1.8 (1.3–2.4) | ||
| Education level of mother* | < Grade 7 | 268 (78.0) | 76 (22.1) | 1 | 1 |
| ≥ Grade 7 | 138 (58.7) | 97 (41.3) | 1.7 (1.1–2.6) | 1.3 (0.8–2.1) | |
| Occupation of mother* | Housewife | 1526 (81.7) | 341 (18.3) | 1 | 1 |
| Farmer | 163 (86.2) | 26 (13.8) | 0.7 (0.3–1.3) | 0.6 (0.1–2.9) | |
| Merchant | 68 (76.4) | 21 (23.6) | 0.7 (0.4–1.3) | 0.7 (0.3–1.5) | |
| Employee | 47 (56.6) | 36 (43.4) | 2.0 (1.1–3.5) | 1.2 (0.6–2.3) | |
| Others | 21 (63.6) | 12 (36.6) | 1.4 (0.6–3.0) | 0.9 (0.3–3.0) | |
| Presence of pregnant mother | No | 1608 (81.0) | 377 (19.0) | 1 | |
| Yes | 217 (78.6) | 59 (21.4) | 1.2 (0.8–1.8) | ||
| Under-fives in household | Not present | 622 (81.4) | 142 (18.6) | 1 | |
| Present | 1203 (80.4) | 294 (19.6) | 1.1 (0.8–1.4) | ||
| Stagnant water around home | Not present | 1685 (81.0) | 394 (19.0) | 1 | |
| Present | 140 (76.9) | 42 (23.1) | 1.4 (0.8–2.3) | ||
| Wealth index in quartile* | First | 731 (85.7) | 122 (14.3) | 1 | 1 |
| Second | 203 (71.2) | 81 (28.5) | 1.6 (1.1–2.3) | 1.2 (0.6–2.3) | |
| Third | 407 (72.7) | 153 (27.3) | 1.3 (0.9–1.8) | 1.0 (0.6–1.8) | |
| Fourth | 484 (85.8) | 80 (14.2) | 1.6 (1.2–2.2) | 1.3 (0.8–2.2) | |
| Altitude of residence metres above sea level** | ≤ 1100 | 623 (73.8) | 221 (26.2) | 1 | 1 |
| (1100–1250) | 626 (83.2) | 126 (16.8) | 0.6 (0.4–0.9) | ||
| > 1250 | 575 (86.6) | 89 (13.4) | 0.5 (0.2–1.0) | ||
*Statistically significant at univariable analysis* and multivariable analysis**
LLINs utilization
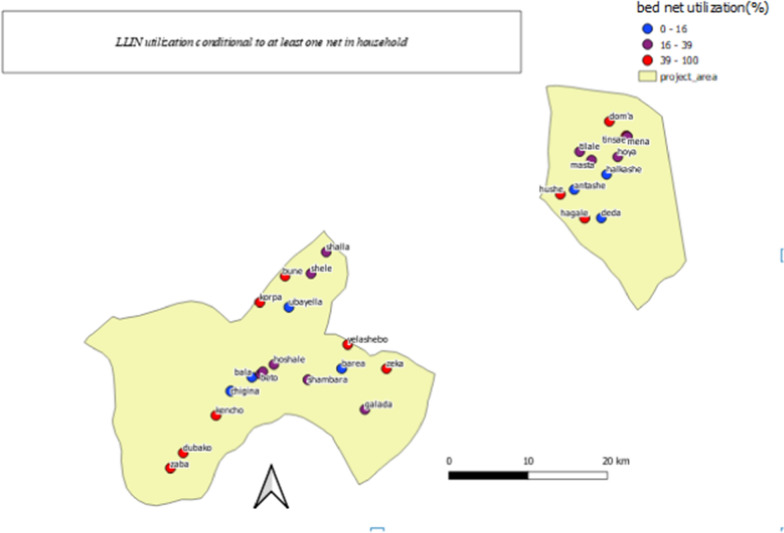
The percentage of any person passing the previous night under a bed net from the total participating households and households conditional to bed net ownership was 12.0% (95% CI 10.7–13.4%) and 62.2% (95% CI 57.4–66.7%) respectively. About 40.3% (95% CI 35.8–45.1%) of participating SAC in the households owned at least one bed nets and 7.8% (6.7–10.0%) of all participating SAC passed the previous night under a bed net irrespective of bed net ownership. The percentage of bed net utilization among SAC conditional to adequate access of bed net in their household was 66.7% (95% CI 50.9–79.5%). The frequency, percentage and 95% CI of bed net use to prevent malaria and other indicators per the study districts was depicted in Table 2 while percentage of bed net utilization conditional to at least one bed net in the household per study schools was depicted (Fig. 3).
Fig. 3.
Percentage of LLIN utilization conditional to at least one LLIN in households of SAC per schools where participated children attend their education
Passing the previous night under a bed net by SAC in univariable multilevel logistic regression analysis was affected by place of residence (COR = 4.1; 95% CI 1.5–12.4), employee being occupation of the child mother (caretaker) (COR = 3.4; 95% CI 1.4–8.1), education level above grade 6 for the child mother (caretaker) (COR = 3.9; 95% CI 1.8–9.4) and household size to bed net ratio less than or equal to 2 (COR = 4.0; 95% CI 1.8–9.8). However, after fitting the model to multivariable multilevel logistic regression, household size to bed net ratio less than or equal to 2 (AOR = 20.7; 95% CI 4.7–132.5) and child mother education level above grade 6 (caretaker) (AOR = 3.4; 95% CI 1.3–9.3) remained statistically significant. The crude and adjusted ORs and the corresponding 95% CI for each of variables assessed for bed net utilization of SAC was presented in Table 4.
Table 4.
Univariable and multivariable logistic regression analysis LLINs utilization by SAC conditional to its ownership, 2019
| Factor | Value categories | Bed net utilized | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| No (%) | Yes (%) | ||||
| Place of residence** | Rural | 187 (60.5) | 122 (39.5) | 1 | 1 |
| Semi-urban | 24 (37.5) | 40 (62.5) | 4.1 (1.5–12.4) | 2.6 (0.7–11.5) | |
| Urban | 49 (77.8) | 14 (22.2) | 2.3 (0.7–7.7) | 0.1 (0.01–0.4) | |
| Residence house | Private | 242 (59.8) | 163 (40.2) | 1 | |
| Not private | 18 (58.1) | 13 (41.9) | 1.2 (0.7–2.0) | ||
| Gender of SAC | Female | 133 (58.1) | 96 (41.9) | 1 | |
| male | 127 (61.4) | 80 (38.6) | 1.0 (0.6–1.5) | ||
| Age of the SAC | 7–9 | 200 (57.3) | 149 (42.6) | 1 | 1 |
| 10–14 | 60 (69.0) | 27 (31.0) | 0.8 (0.6–1.1) | ||
| Gender of household head | Male | 238 (59.1) | 165 (40.9) | 1.2 (0.7–1.9) | |
| Female | 22 (66.7) | 11 (33.3) | 1 | ||
| Age of household head | ≤ 34 | 77 (68.1) | 36 (31.9) | 1 | |
| 35–49 | 161 (57.3) | 120 (42.7) | 1.4 (0.8–2.4) | ||
| ≥ 50 | 22 (52.4) | 20 (47.6) | 1.4 (0.6–3.3) | ||
| Occupation of household head | Farmer | 174 (60.2) | 115 (39.8) | 0.6 (0.3–1.3) | |
| Civil servant | 40 (52.6) | 36 (47.4) | 1 | ||
| Merchant | 23 (67.6) | 11 (32.3) | 0.4 (0.1–1.1) | ||
| Others | 23 (62.2) | 14 (37.8) | 0.6 (0.2–1.6) | ||
| Educational status of household head | Illiterate | 112 (59.6) | 76 (40.4) | 1 | |
| Literate | 148 (59.7) | 100 (40.3) | 1.1 (0.7–1.9) | ||
| Age of child’s mother | ≤ 34 | 173 (60.9) | 111 (39.1) | 1 | |
| 35–49 | 83 (57.6) | 61 (42.4) | 1.0 (0.6–1.7) | ||
| ≥ 50 | 4 (50.0) | 4 (50) | 1.4 (0.2–8.2) | ||
| Educational status of mother | Illiterate | 157 (60.4) | 103 (39.6) | 1 | |
| Literate | 103 (58.5) | 73 (41.5) | 1.4 (0.8–2.4) | ||
| Education level of mother** | < Grade 7 | 54 (71.1) | 22 (28.9) | 1 | 1 |
| ≥ Grade 7 | 47 (48.1) | 50 (51.1) | 3.9 (1.8–9.4) | 3.4 (1.3–9.3) | |
| Occupation of mother* | Housewife | 203 (59.5) | 138 (40.5) | 1 | 1 |
| Employee | 14 (38.9) | 22 (61.1) | 3.4 (1.4–8.1) | 1.9 (0.6–6.7) | |
| Others | 43 (72.9) | 16 (27.1) | 0.8 (0.4–1.9) | 0.3 (0.1–0.9) | |
| Presence of pregnant mother | No | 229 (60.7) | 148 (39.3) | 1 | 1 |
| Yes | 31 (52.5) | 28 (47.5) | 0.7 (0.3–1.6) | ||
| Under-fives in the household | Not present | 83 (58.5) | 59 (41.5) | 1 | |
| Present | 177 (60.2) | 117 (39.8) | 1.1 (0.7–1.9) | ||
| Stagnant water around home | Not present | 234 (59.4) | 160 (36.6) | 1 | |
| Present | 26 (61.9) | 16 (38.1) | 1.4 (0.5–3.9) | ||
| Knowledge of mother or care taker as only mosquito bit transmits malaria | |||||
| No | 238 (62.3) | 144 (37.7) | 1 | ||
| Yes | 22 (40.7) | 32 (59.3) | 1.2 (0.6–2.2) | ||
| IRS last 12 months | No | 107 (55.7) | 85 (44.3) | 1 | |
| Yes | 153 (62.7) | 91 (37.3) | 0.7 (0.5–1.1) | ||
| IRS < 4 months | Yes | 85 (67.5) | 41 (32.5) | 1 | 1 |
| No | 68 (57.6) | 50 (42.4) | 1.7 (0.7–4.3) | ||
| Altitude of residence metres asl | ≤ 1100 | 139 (62.9) | 82 (37.1) | 1 | 1 |
| (1100–1250) | 77 (61.1) | 49 (38.9) | 0.9 (0.4–2.1) | ||
| > 1250 | 44 (49.4) | 45 (50.6) | 0.5 (0.1–2.1) | ||
| Wealth index in quartile | First | 96 (60.8) | 62 (39.2) | 1 | |
| Second | 40 (61.5) | 25 (38.5) | 1.1 (0.5–2.2) | ||
| Third | 59 (61.5) | 37 (38.5) | 0.9 (0.5–1.7) | ||
| Fourth | 65 (55.6) | 52 (44.4) | 1.6 (0.9–2.9) | ||
| Household size to bed net ratio** | > 2 | 245 (62.7) | 146 (37.3) | 1 | 1 |
| ≤ 2 | 15 (33.3) | 30 (66.7) | 4.0 (1.8–9.0) | 20.7 (4.7–132.5) | |
Statistically significant at univariable analysis* and multivariable variable analysis**
Discussion
In this survey, ownership of LLINs and sleeping under a LLIN on the night preceding the survey by SAC were assessed. The ownership of bed nets by the households where SAC were living in the study area was 19.3%. Among those owned at least one LLIN in the household, only 10.3% had adequate access to be used by all the household members. The ownership was positively affected by being resident in semi-urban area in the study area. The percentage of children that slept the previous night under a bed net was 7.8% among the total studied; 40.3% conditional to the presence of at least one bed net in the household and 66.7% among SAC who had adequate access. Bed net utilization by the SAC conditional to presence of at least one bed net in the household was positively affected by the household size to bed net ratio equal to or less than 2 in the households and child mother (caretaker) education level above grade six.
Household bed net ownership in the present study was much lower than the universal coverage target of the NMCP [30]. Access to the bed nets which is also one of the major indicators to assess effectiveness of bed net for the prevention of malaria [31] was also poor in the current study area. Ownership of bed nets was lower than coverage estimated in the most recent malaria indicator survey in Ethiopia [13] and most other studies conducted in Ethiopia [22, 25, 32, 33] except a study conducted among households of pregnant women in Shashogo district in Southern Ethiopia [23]. The finding from the present study was also lower compared to similar studies conducted outside Ethiopia, such as at national and district levels in Uganda [34–36], Madagascar [37], Ghana [38, 39], Zimbabwe [40], Equatorial Guinea [41] and in Kenya [42]. The lower ownership of bed nets in the current study area as compared to those reviewed might be difference in the length of time between the last distribution of bed nets and the data collection period as some might be damaged or lost because of different reasons. The other possible explanation for low ownership of bed net in the study area might be due to inaccessibility of the bed nets to purchase in the districts. The difference in finding from Shashogo district in Southern Ethiopia could be related to the level of endemicity of malaria transmission being higher in the current study area.
The bed net utilization by SAC conditional to owning at least one bed net in their household was about 40% in the current study which is lower than utilization by people living in malaria-endemic areas in Africa and the overall bed net utilization in Ethiopia [1]. However, their bed net utilization was improved when access to the bed net was increased in the households. In Uganda and Zimbabwe, bed net utilization was significantly influenced by density of bed nets in households [14, 40]. The lower bed net use by the children may be related to low awareness of the community regarding vulnerability of SAC for malaria and malaria prevention measures. Bed net utilizations among SAC in Tanzania [33] and in the highlands of western Kenya [43] were higher than the finding of this study. The result of this study was in agreement to the utilization of bed net by SAC in Côte d’Ivoire [44], but higher than findings revealed from implementing national school malaria survey in Kenya [45] and bed net use among SAC after universal bed net distribution campaign in Malawi [46]. The basic reason for low coverage of bed net utilization in the present study will be due to inadequate access to the bed nets. In conditions when bed net access was not sufficient for all household members, SAC were given the least priority. The higher bed net utilization in the current study as compared to children in Malawi and Kenya could be related to difference in the background malaria transmission endemicity or cultural difference in prioritizing available bed nets to be used.
One of the two factors determining bed net utilization by SAC in the study area was the household size to bed net ratio. In conditions where bed net was not adequate to the household members, bed net utilization was determined by who is given priority from the household. A qualitative study conducted in Kutcha district near the current study area shown us that SAC were given the last priority to utilize bed nets among the household members. Pregnant women, children age less than 5 years or the household head mainly the fathers were given priority than SAC. In Malawi and Uganda SAC less likely used bed net as compared to the other population segments [35, 46]. Children age less than 5 years and pregnant women, well known vulnerable people to malaria, were more benefited from bed net utilization for the prevention of malaria. However, the insignificant association between presence of pregnant mother and under five children in the household and bed net utilization in the current study might be related to absence of bed nets to be distributed to children age less than 5 years during immunization and ANC follow-up of pregnant women from the health facilities. This was witnessed by absence of be nets to demonstrate participants in the trial mentioned in “Methods” section of this manuscript.
Bed net utilization was also influenced by economic status of population since this would provide opportunity to purchase nets in areas where there was access, as revealed by the national malaria indicator survey in SSA [47]. The finding of the present study was in contrast to this where socio-economic status of the household had no statistically significant impact on the utilization of bed nets by SAC. Lack of insignificant statistical correlation between wealth index and bed net utilization in the present study might be further explained by lack of access to purchase bed nets in their vicinity. The other factor that influenced bed net utilization in the current study was the level of maternal (caretaker) education level. This could be due to good awareness of the mothers or caretakers with higher education level regarding prevention measures of malaria.
Note should be taken of the following limitations associated with this study. The first limitation was involving only school enrolled SAC to this study as the situation could be different for school non-enrolled children. The second limitation was the use of cross-sectional study as it is not strong in generating evidence for cause and effect relationship. The strengths of this study were that the research was undertaken in a hard-to-reach and underexplored area, and had good power of the study.
Conclusions
Ownership of bed nets, access to adequate numbers of bed nets in households of SAC and their utilization was lower than the target set to achieve universal coverage of bed nets to control malaria. It is important to monitor replacement needs of households, with main emphasis being given to households in urban area and rural areas as compared to semi-urban area. Utilization of bed nets conditional to the presence of at least one net in the household was affected by maternal education level and the density of bed nets in the household. Malaria prevention education to correct these barriers and increasing awareness about the benefit of effective and consistent utilization of insecticide treated bed nets should be given to children and mothers with low educational level to realize the elimination of malaria.
Acknowledgements
We would like to thank Arba Minch University for funding the research, Dara Mallo and Uba Debretsehay district health offices for informing lists of malaria endemic kebeles. Our sincere appreciation goes to school directors in involved in facilitating the data collection process, those involved in the data collection and parents for devoting their time to come to school to provide assent and interview.
Abbreviations
- AIC
Akaike Information Criterion
- AOR
Adjusted odds ratio
- CI
Confidence interval
- COR
Crude odds ratio
- DHS
Demographic and Health Surveys
- GPS
Global positioning system
- IRB
Institutional Research Ethics review Board
- IRS
Indoor Residual Spray
- LLINs
Long-lasting insecticide-treated Nets
- NMCP
National Malaria Control Programme
- ODK
Open Data Kit
- OR
Odds ratio
- QGIS
Quantum Geographical Information System
- SAC
School-aged children
- SD
Standard deviation
- SSA
Sub-Saharan Africa
Authors’ contributions
ZZ, JP, HD, SA and FM conceived the idea, designed the study, analyzed, interpreted and drafted the manuscript; MM, MS and YC conceived and involved in acquisition of the data; GB, AT and TY conceived the idea. All authors read and approved the final manuscript.
Funding
Arba Minch University financed the data collection process.
Availability of data and materials
The datasets used and/or analysed during the current study will be available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The trial mentioned above was approved with written consent procedure to be followed by the Institutional Research Ethics review Board (IRB) in College of Medicine and Health Sciences, Arba Minch University with the reference number of IRB/154/12. Official permission letter to conduct the research is submitted to district health offices and education offices in Dara Mallo and Uba Debretsehay districts. Support letter written by the respective education offices was given to each participating school to support and participate in the study and written consent was obtained from the school headmasters. Parents of the selected SAC were invited to come to the schools and written consent was obtained before data collection at school and household levels. Written informed consent was obtained from each of the selected students’ parent at school and documented in college of medicine and Health Sciences in Arba Minch University.
Consent for publication
Not applicable.
Competing interests
The authors declare that we have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO . World malaria report 2018. Geneva: World Health Organization; 2018. [Google Scholar]
- 2.WHO . World malaria report 2014. Geneva: Global Malaria Programme, World Health Organization; 2014. pp. 1–227. [Google Scholar]
- 3.WHO. World malaria report 2019. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO.
- 4.WHO. Fact sheet: World malaria report 2016. Up-dated 13 of December. 2016. https://www.who.int/malaria/media/world-malaria-report-2016/en/. Accessed 14 Oct 2017.
- 5.WHO. A framework for malaria elimination. Global Malaria Programme. Geneva: World Health Organization; 2017. https://www.who.int/malaria/publications/atoz/9789241511988/en/.
- 6.Taddese AA, Baraki AG, Gelaye KA. Spatial modeling, prediction and seasonal variation of malaria in northwest Ethiopia. BMC Res Notes. 2019;12:273. doi: 10.1186/s13104-019-4305-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dabaro D, Birhanu Z, Yewhalaw D. Analysis of trends of malaria from 2010 to 2017 in Boricha District, Southern Ethiopia. Malar J. 2020;19:88. doi: 10.1186/s12936-020-03169-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aregawi M, Lynch M, Bekele W, Kebede H, Jima D, Taffese HS, et al. Time series analysis of trends in malaria cases and deaths at hospitals and the effect of antimalarial interventions, 2001–2011, Ethiopia. PLoS ONE. 2014;9:e106359. doi: 10.1371/journal.pone.0106359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO . World malaria report 2015. Geneva: World Health Organization; 2016. [Google Scholar]
- 10.Ceesay SJ, Casals-Pascual C, Erskine J, Anya SE, Duah NO, Fulford AJ, et al. Changes in malaria indices between 1999 and 2007 in The Gambia: a retrospective analysis. Lancet. 2008;372:1545–1554. doi: 10.1016/S0140-6736(08)61654-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nankabirwa J, Brooker SJ, Clarke SE, Fernando D, Gitonga CW, Schellenberg D, et al. Malaria in school-age children in Africa: an increasingly important challenge. Trop Med Int Health. 2014;19:1294–1309. doi: 10.1111/tmi.12374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ethiopian Public Health Institute. Ethiopia National Malaria Indicator Survey 2015.
- 13.Ashton RA, Kefyalew T, Tesfaye G, Pullan RL, Yadeta D, Reithinger R, et al. School-based surveys of malaria in Oromia Regional State, Ethiopia: a rapid survey method for malaria in low transmission settings. Malar J. 2011;10:25. doi: 10.1186/1475-2875-10-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Golassa L, Baliraine FN, Enweji N, Erko B, Swedberg G, Aseffa A. Microscopic and molecular evidence of the presence of asymptomatic Plasmodium falciparum and Plasmodium vivax infections in an area with low, seasonal and unstable malaria transmission in Ethiopia. BMC Infect Dis. 2015;15:310. doi: 10.1186/s12879-015-1070-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brooks HM, Paul MK, Claude KM, Mocanu V, Hawkes MT. Use and disuse of malaria bed nets in an internally displaced persons camp in the Democratic Republic of the Congo: a mixed-methods study. PLoS ONE. 2017;12:e0185290. doi: 10.1371/journal.pone.0185290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nuwamanya S, Kansiime N, Aheebwe E, Akatukwasa C, Nabulo H, Turyakira E, et al. Utilization of long-lasting insecticide treated nets and parasitaemia at 6 months after a mass distribution exercise among households in Mbarara Municipality, Uganda: a cross-sectional community based study. Malar Res Treat. 2018;2018:4387506. doi: 10.1155/2018/4387506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coalson JE, Cohee LM, Buchwald AG, Nyambalo A, Kubale J, Seydel KB, et al. Simulation models predict that school-age children are responsible for most human-to-mosquito Plasmodium falciparum transmission in southern Malawi. Malar J. 2018;17:147. doi: 10.1186/s12936-018-2295-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Afoakwah C, Nunoo J, Andoh FK. Effect of insecticide-treated bed net usage on under-five mortality in northern Ghana. Malar J. 2015;14:309. doi: 10.1186/s12936-015-0827-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pryce J, Richardson M, Lengeler C. Insecticide-treated nets for preventing malaria. Cochrane Database Syst Rev. 2018;11:000363. doi: 10.1002/14651858.CD000363.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.States U. President’s Malaria Initiative Ethiopia Malaria Operational Plan FY 2020. www.pmi.gov. Accessed 2020.
- 21.Sena LD, Deressa WA, Ali AA. Predictors of long-lasting insecticide-treated bed net ownership and utilization: evidence from community-based cross-sectional comparative study, Southwest Ethiopia. Malar J. 2013;12:406. doi: 10.1186/1475-2875-12-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fuge TG, Ayanto SY, Gurmamo FL. Assessment of knowledge, attitude and practice about malaria and ITNs utilization among pregnant women in Shashogo District, Southern Ethiopia. Malar J. 2015;14:235. doi: 10.1186/s12936-015-0755-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tassew A, Hopkins R, Deressa W. Factors influencing the ownership and utilization of long-lasting insecticidal nets for malaria prevention in Ethiopia. Malar J. 2017;16:262. doi: 10.1186/s12936-017-1907-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.2Census 2007 Tables: Southern Nations, Nationalities, and Peoples'. https://en.wikipedia.org/wiki/Gamo_Gofa_ZoneRegion. Accessed 2 Mar 2019.
- 25.Ministry of Health. National Malaria Guidelines. 3rd edition. Addis Ababa: Federal Ministry of Health of Ethiopia; 2012. https://www.medbox.org/nationalmalaria-guidelines-ethiopia/download.pdf. Accessed 21 May 2019.
- 26.Hayes RJ, Bennett S. Simple sample size calculation for cluster-randomized trials. Int J Epidemiol. 1999;28:319–326. doi: 10.1093/ije/28.2.319. [DOI] [PubMed] [Google Scholar]
- 27.Rutterford C, Copas A, Eldridge S. Methods for sample size determination in cluster randomized trials. Int J Epidemiol. 2015;44:1051–1067. doi: 10.1093/ije/dyv113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.DHS. malaria indicator survey toolkit. MIS Household Questionnaire. 2016.
- 29.RBM . Guidelines for core population-based indicators. Geneva: RBM; 2009. [Google Scholar]
- 30.Koenker H, Arnold F, Ba F, Cisse M, Diouf L, Eckert E, et al. Assessing whether universal coverage with insecticide-treated nets has been achieved: is the right indicator being used? Malar J. 2018;17:355. doi: 10.1186/s12936-018-2505-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moscibrodzki P, Dobelle M, Stone J, Kalumuna C, Chiu YH, Hennig N. Free versus purchased mosquito net ownership and use in Budondo sub-county, Uganda. Malar J. 2018;17:363. doi: 10.1186/s12936-018-2515-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Finlay AM, Butts J, Ranaivoharimina H, Cotte AH, Ramarosandratana B, Rabarijaona H, et al. Free mass distribution of long lasting insecticidal nets lead to high levels of LLIN access and use in Madagascar, 2010: A cross-sectional observational study. PLoS ONE. 2017;12:e0183936. doi: 10.1371/journal.pone.0183936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nzobo BJ, Ngasala BE, Kihamia CM. Prevalence of asymptomatic malaria infection and use of different malaria control measures among primary school children in Morogoro Municipality, Tanzania. Malar J. 2015;14:491. doi: 10.1186/s12936-015-1009-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alemu MB, Asnake MA, Lemma MY, Melak MF, Yenit MK. Utilization of insecticide treated bed net and associated factors among households of Kola Diba town, North Gondar, Amhara region, Ethiopia. BMC Res Notes. 2018;11:575. doi: 10.1186/s13104-018-3697-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wanzira H, Katamba H, Rubahika D. Use of long-lasting insecticide-treated bed nets in a population with universal coverage following a mass distribution campaign in Uganda. Malar J. 2016;15:311. doi: 10.1186/s12936-016-1360-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.García-Basteiro AL, Schwabe C, Aragon C, Baltazar G, Rehman AM, Matias A, et al. Determinants of bed net use in children under five and household bed net ownership on Bioko Island, Equatorial Guinea. Malar J. 2011;10:179. doi: 10.1186/1475-2875-10-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nyavor KD, Kweku M, Agbemafle I, Takramah W, Norman I, Tarkang E, et al. Assessing the ownership, usage and knowledge of insecticide treated nets (ITNs) in malaria prevention in the Hohoe municipality, Ghana. Pan Afr Med J. 2017;28:67. doi: 10.11604/pamj.2017.28.67.9934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Diema Konlan K, Japiong M, Dodam Konlan K, Afaya A, Salia SM, Kombat JM. Utilization of insecticide treated bed nets (ITNs) among caregivers of children under five years in the Ho municipality. Interdiscip Perspect Infect Dis. 2019;2019:3693450. doi: 10.1155/2019/3693450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kanyangarara M, Hamapumbu H, Mamini E, Lupiya J, Stevenson JC, Mharakurwa S, et al. Malaria knowledge and bed net use in three transmission settings in southern Africa. Malar J. 2018;17:41. doi: 10.1186/s12936-018-2178-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gonahasa S, Maiteki-Sebuguzi C, Rugnao S, Dorsey G, Opigo J, Yeka A, et al. LLIN Evaluation in Uganda Project (LLINEUP): factors associated with ownership and use of long-lasting insecticidal nets in Uganda: a cross-sectional survey of 48 districts. Malar J. 2018;17:421. doi: 10.1186/s12936-018-2571-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-Eryani SM, Mahdy MA, Al-Mekhlafi AM, Abdul-Ghani R. Access to and use of long-lasting insecticidal nets and factors associated with non-use among communities in malaria-endemic areas of Al Hudaydah governorate in the Tihama region, west of Yemen. Malar J. 2017;16:244. doi: 10.1186/s12936-017-1894-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lencha B. Insecticide treated bed net utilization among under five children and household bed net ownership in Adami Tulu District, Oromia Regional State, Ethiopia. Doctoral Dissertation, Addis Ababa University. 2014.
- 43.Atieli HE, Zhou G, Afrane Y, Lee MC, Mwanzo I, Githeko AK, et al. Insecticide-treated net (ITN) ownership, usage, and malaria transmission in the highlands of western Kenya. Parasit Vectors. 2011;4:113. doi: 10.1186/1756-3305-4-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Houngbedji CA, N'Dri PB, Hürlimann E, Yapi RB, Silué KD, Soro G, et al. Disparities of Plasmodium falciparum infection, malaria-related morbidity and access to malaria prevention and treatment among school-aged children: a national cross-sectional survey in Côte d'Ivoire. Malar J. 2015;14:7. doi: 10.1186/1475-2875-14-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gitonga CW, Karanja PN, Kihara J, Mwanje M, Juma E, Snow RW, et al. Implementing school malaria surveys in Kenya: towards a national surveillance system. Malar J. 2010;9:306. doi: 10.1186/1475-2875-9-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Buchwald AG, Walldorf JA, Cohee LM, Coalson JE, Chimbiya N, Bauleni A, et al. Bed net use among school-aged children after a universal bed net campaign in Malawi. Malar J. 2016;15:127. doi: 10.1186/s12936-016-1178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Njau JD, Stephenson R, Menon M, Kachur SP, McFarland DA. Exploring the impact of targeted distribution of free bed nets on households bed net ownership, socio-economic disparities and childhood malaria infection rates: analysis of national malaria survey data from three sub-Saharan Africa countries. Malar J. 2013;12:245. doi: 10.1186/1475-2875-12-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study will be available from the corresponding author on reasonable request.