Highlights
-
•
Duodenal diverticula is mostly found incidentally and it rarely complicates by perforation.
-
•
Treatment is only indicated in complicated duodenal diverticula.
-
•
Micro perforation in the absence of systemic signs are better treated with conservative management.
-
•
Among surgical options diverticulectomy and single layer closure was performed.
-
•
Other surgical intervention could involve segmental duodenectomy or pylorus-preserving duodeno-pancreatectomy.
Abbreviations: DD, duodenal diverticulum; ERCP, endoscopic retrogradecholangiograpgy; GI, Gastrointestinal; NG, Naso-Gastric; CRP, C-reactive protein; PCT, Procalcitonin
Keywords: Duodenal diverticulum, Perfortation, Diverticulectomy, Conservative management, Lebanese, Case report
Abstract
Introduction
Duodenal Diverticula is not uncommon and it is mostly found in the 2nd part of the duodenum. Despite the fact that it is mostly found incidentally, it can complicate however it rarely complicates by perforation. Treatment is indicated only in complicated cases and it is divided into conservative and surgical arms.
Presentation of case
It is a case of 78 years old Lebanese female that was diagnosed intra-operatively with a perforated duodenal diverticulum after presenting with post prandial abdominal pain, distention and pneumoperitoneum on imaging. Our case was consistent with previous reports where the diverticulum occurred in the second part of the duodenum. We opted for primary resection of the diverticulum and over-sewing. Moreover, patient had an uneventful post-operative course and progressed gradually to be discharged on day 10.
Conclusion
Our case aims to draw attention to a rare complication of duodenal diverticula and to widen the differential diagnosis of pneumoperitoneum thus concluding about the better treatment option. Previous reports show that proper management is still a controversial topic; however surgical approach is indicated in case of systemic signs.
1. Introduction
Duodenal Diverticula (DD) was first reported by a pathologist in 1710 and then diagnosed radiologically in 1913 [1]. Reviewing the literature, it is shown that only a handful of cases of DD are reported. However, with the advance and the increased indication of imaging and endoscopies, it is relatively becoming more common. Precisely, the actual prevalence and incidence of this entity is hard to identify due to the fact that it is mostly asymptomatic. For instance, a cadaveric study showed the prevalence of DD to be around 4.2% with the majority being found in the 2nd part of the duodenum [2].
Diverticular disease is more common in the large bowel compared to the small bowel. Precisely, duodenum has the highest rate of diverticular disease among the small bowel [3]. As it is the case with other diverticula; there are two types: congenital one having all 3 layers and acquired one lacking a muscular layer [4]. DD is mostly found incidentally with no symptoms during imaging, ERCP or upper GI series [1]. Indeed, it could complicate and present as diverticulitis, bleeding, perforation, or obstruction [4,5].
Interestingly, perforation is rare but it is the most dramatic complication of DD [5]. Interestingly, it resides mostly in the 2nd part of the duodenum [5]. Among the causes of perforation; the most common causes are diverticulitis, enterolithiasis, ulceration, and foreign bodies [4,5]. Clinically, physical exam may lack generalized peritonitis signs due to retroperitoneal perforation. Being so, nonspecific symptoms are the main constituents of the 'tableau clinique' as abdominal pain associated with nausea, vomiting and rarely including peritoneal signs [4].
This case was reported in accordance with the SCARE criteria [6].
2. Case description
We present a case of 78 years old female known to have coronary artery disease status post percutaneous coronary intervention and stent insertion around 1 year ago on dual anti platelets therapy. She also had thyroidectomy maintained on Levothyroxine tablets daily.
She presented with constant non-colicky abdominal pain mainly post-prandial and especially on fluids. It was associated with nausea and vomiting with no fever. Vital signs were within normal limits with blood pressure of 120/70 mmHg, pulse was 70 and saturation was 97%. Physical exam was remarkable for abdominal distention and diffuse abdominal tenderness. Moreover, blood tests lacked signs of systemic illness in which there was only mild increase in white blood cells or C-reactive protein (CRP). Table 1 shows the lab tests results.
Table 1.
Initial blood tests (Abbreviations: SGPT: serum glutamic pyruvic transaminase, SGOT: serum glutamic oxaloacetic transaminase, GGT: Gamma-glutamyltransferase, INR: international normalized ratio, PTT: partial thromboplastin time).
| Test | Results |
|---|---|
| Hematocrit | 33 |
| Hemoglobin | 11 |
| White blood cells | 11,000/mm3 |
| Neutrophils | 80% |
| Lymphocytes | 10% |
| Platelets | 200,000/mm3 |
| C- reactive protein | 10 mg/l (normal: 0–5) |
| Albumin | 3 g% (normal: 3.4–5) |
| Total Bilirubin | 0.9 mg% |
| Alkaline phosphatase | 40 U/I |
| SGPT | 20 U/I |
| SGOT | 25 U/I |
| GGT | 32 U/I |
| Amylase | 150 U/I |
| Lipase | 23 U/I |
| INR | 1.2 |
| PTT | 30 |
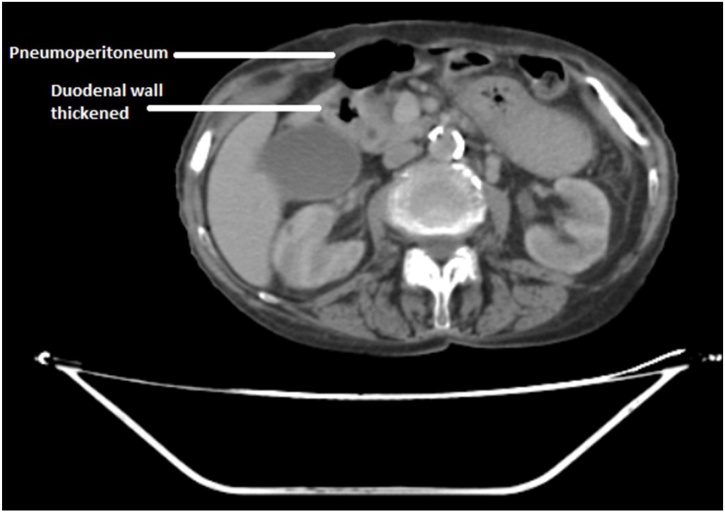
CT (Computed Tomography) scan of the abdomen and pelvis showed pneumoperitoneum with wall thickening at the duodenal and pre-pyloric area (Fig. 1).
Fig. 1.
CT scan showing deformed duodenal bulb and pneumoperitoneum.
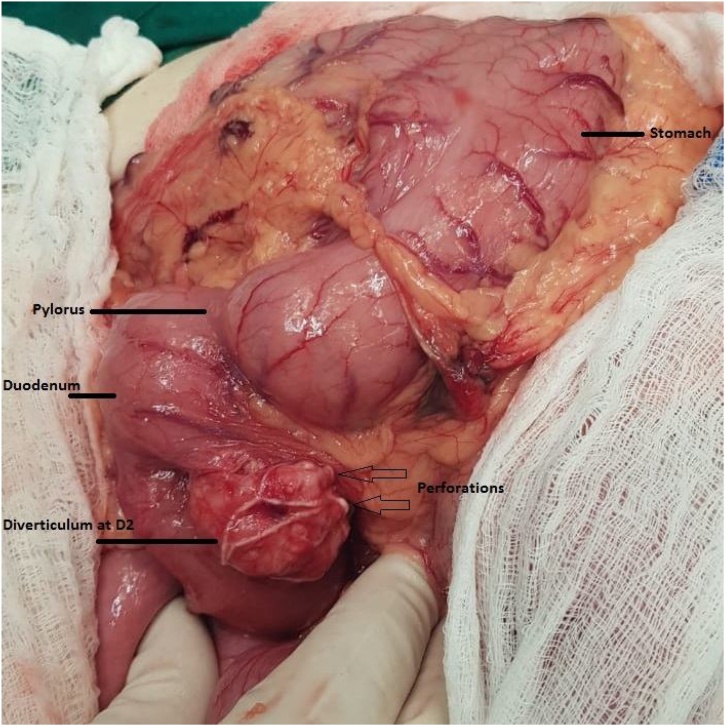
Preliminary diagnosis was perforated duodenal ulcer and we opted for laparotomy. During the operation, opening the peritoneum did not show fluid or peritoneal soiling. We inspected for gastric ulcer anteriorly and posteriorly by opening the lesser sac but gastric ulcer was ruled out. Examining the duodenum, inflammation was found, with dissection and performing Kocher maneuver we were able to identify a duodenal diverticulum at the D2 level at the antero-medial aspect as shown in (Fig. 2). It measured around 4 × 3 cm in diameter.
Fig. 2.
During laparotomy the stomach, pylorus, duodenum and duodenal diverticulum were identified with the perforation being witnessed as shown.
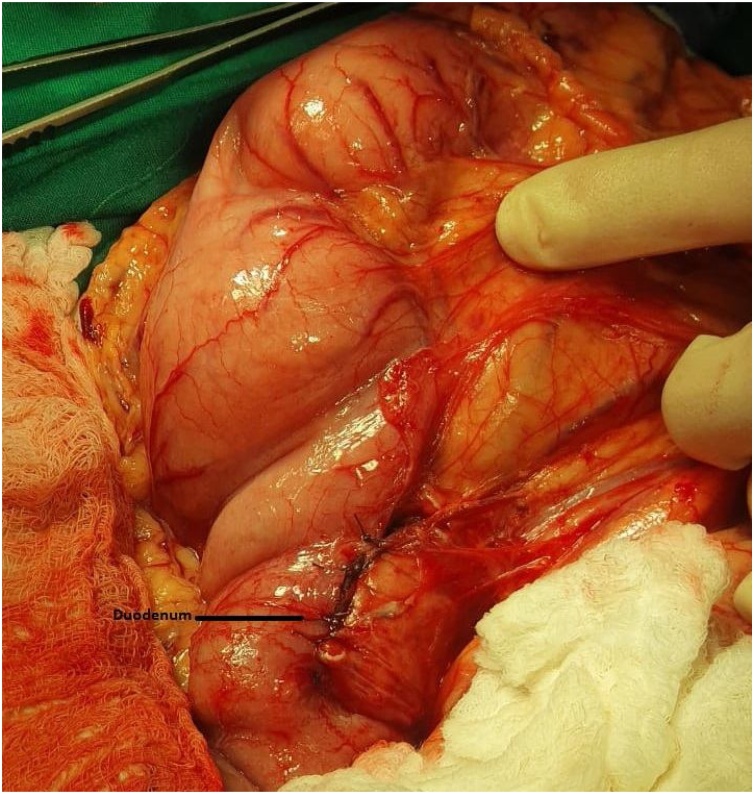
Moreover, decision to resection was made. We did Kocher maneuver to better manipulate the duodenum and resection of the diverticulum was carried out using GIA (Gasrto-Intestinal Anastomosis) linear stapler of 4.8 × 60 mm dimensions and over-sewing was carried out as shown in Fig. 3. Small bowel was rolled and other pathologies were ruled out. Drain was inserted near the anastomosis and NG (Naso-Gastric) tube was advanced to the duodenum for decompression.
Fig. 3.
Shows the duodenum after resection of the diverticulum and over-sewing.
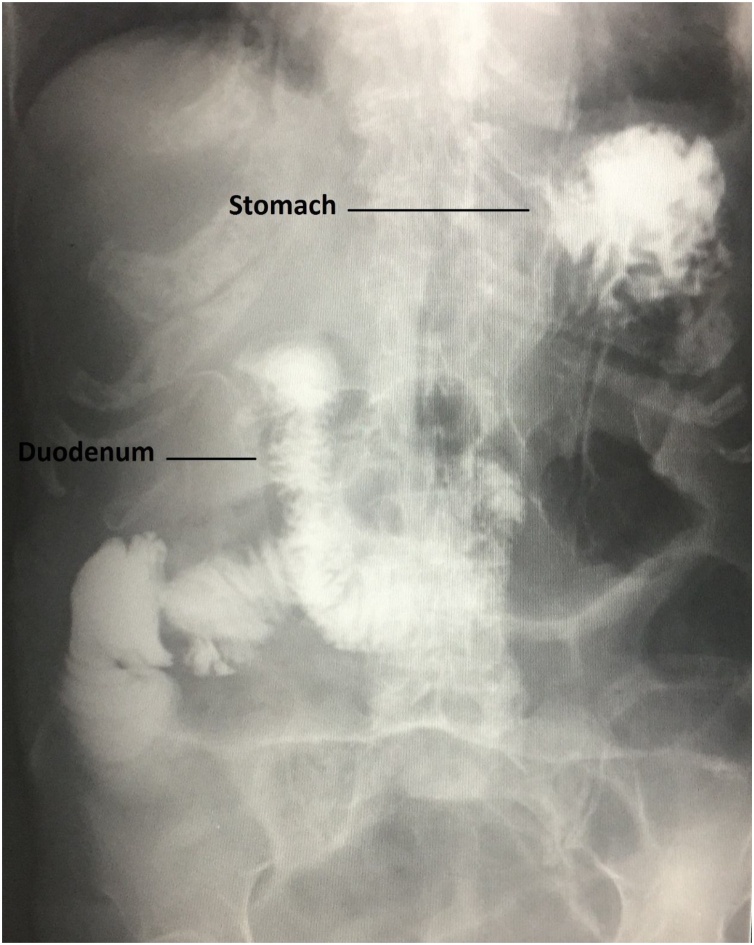
Post-operative period was uneventful and the patient was followed up with an upper GI series on post-operative day 5 as shown in Fig. 4 and discharged home on day 10 post operation. Pathology report confirmed our diagnosis being duodenal diverticulum with no signs of neoplasia.
Fig. 4.
an upper GI series on post-operative day 5 showing the duodenum ruling out leakage or stenosis.
3. Discussion
Uncomplicated DD requires no intervention [1]. On the other hand, cases reported vary in management of complicated DD especially perforated ones. One arm endorses conservative management as a primary treatment and others prefer surgical management. In our case we opted for surgical management because the diagnosis was not clear before the operation. Some agree that due to surgery complications, duodenal diverticula with micro perforation in the absence of systemic signs are better treated with conservative management as in cases with uncomplicated diverticulitis [5] and be followed by serial monitoring of CRP and PCT (Procalcitonin). However, others argue that retroperitoneal abscess may result post retroperitoneal perforation and contamination; not to mention that it may result in sepsis [4] and thus early surgical intervention would be a wise decision. Among surgical options diverticulectomy and single layer closure was performed as it is the case with our patient. Others reported that surgical intervention could involve segmental duodenectomy or pylorus-preserving duodeno-pancreatectomy [1]. Our case comes in accordance to previous reports being in the 2nd part of the duodenum. Precisely, concerning our case pre-operative imaging was not sufficient to document DD and thus conservative management was not considered. In the absence of sufficient data to endorse conservative management, one would question the influence on mortality.
4. Conclusion
This case draws attention to a rare complication in a relatively common disease. It aims to widen the differential diagnosis when encountering abdominal pain and pneumoperitoneum hence choosing the proper management being conservative or surgical.
5. Study limitations
As a case report aiming to drive attention on a relatively rare complication it needs to be endorsed by more sophisticated studies that help us know now how to manage effectively such a complication in the less morbidity possible.
Declaration of Competing Interest
This article has no conflict of interest with any parties.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
The study type is exempt from ethical approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author’s contribution
Writing the paper: Alaa Kansoun, Iyad Al Mohtar, Etienne El-Helou.
Data collection: Alaa Kansoun, Abdel Rahman Amiry, Marwan Bahmad, Khaled Rahal, Hasan Atwi.
Interpretation: Alaa Kansoun, Faisal Houcheimi, Nisreen Maanieh, Mouhamad Hazim, Walid Ambriss.
Supervision: Alaa Kansoun.
Registration of research studies
N/A.
Guarantor
Alaa Kansoun.
Acknowledgements
We would like to thank the Doctors and staff of our institute, and the members of our University, for their continuous support and guidance.
Contributor Information
Alaa Kansoun, Email: A.kanso@hotmail.com.
Etienne El-Helou, Email: Etienne-elhelou@hotmail.com.
Abdel Rahman Amiry, Email: Abdo414@hotmail.com.
Marwan Bahmad, Email: Bahmad.11.12@gmail.com.
Iyad Al Mohtar, Email: Iyadalmohtar@gmail.com.
Faisal Houcheimi, Email: Faisal.houcheimi@gmail.com.
Nisreen Maanieh, Email: Nisreen_m@live.com.
Mouhamad Hazim, Email: Mouhamad.a.hazim@gmail.com.
Khaled Rahal, Email: Khaled_rahal1@hotmail.com.
Hasan Atwi, Email: drhatwi@gmail.com.
Walid Ambriss, Email: Dr.ambriss@gmail.com.
References
- 1.Maingot R. Gastric and duodenal diverticula. In: Maingot R., editor. Abdominal-Operations. Appleton-Century-Crofts; New York, NY, USA: 1980. pp. 141–156. [Google Scholar]
- 2.Sakthivel Sulochana, Kannaiyan Kavitha, Thiagarajan Sivakami. Prevalence of duodenal diverticulum in south indians: a cadaveric study. ISRN Anat. 2013;2013:767403. doi: 10.5402/2013/767403. PMCID: PMC4392957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knoefel W.T., Ratttner D.W. Duodenal diverticula and duodenal tumours. In: Morris P.J., Malt R.A., editors. vol. 1. Oxford University Press; New York, NY, USA: 1994. pp. 943–946. (Oxford Text Book of Surgery). [Google Scholar]
- 4.Simões Vitor Costa, Santos Bruno, Magalhães Sara, Faria Gil, Silva Donzília Sousa, Davide José. Perforated duodenal diverticulum: surgical treatment and literature review. Int. J. Surg. Case Rep. 2014;5(8):547–550. doi: 10.1016/j.ijscr.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim K.H., Park S.H. Conservative treatment of duodenal diverticulitis perforation: a case report and literature review. Open Access Emerg. Med. 2018;10:101–104. doi: 10.2147/OAEM.S168487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]