Abstract
Background:
Neurocognitive dysfunction is a common complication of coronary artery bypass grafting (CABG) with incidence of 19–38%. The miniaturized cardiopulmonary bypass (MCPB) system was developed to reduce hemodilution and inflammation and provides better cerebral protection than conventional cardiopulmonary bypass (CCPB). In a meta-analysis, MCPB was associated with a 10-fold reduction in the incidence of strokes. However, its effect on postoperative cognitive decline (POCD) is unknown. We assessed if MCPB decreases POCD after CABG and compared the risk factors.
Methods:
A total of 71 Asian patients presenting for elective CABG at a tertiary center were enrolled. They were randomly assigned to MCPB (n = 36) or CCPB group (n = 35) and followed up in a single-blinded, prospective, randomized controlled trial. The primary outcome was POCD as measured by the repeatable battery of neuropsychological status (RBANS). Inflammatory markers (tumor necrosis factor-alpha and interleukin-6), hematocrit levels, and neutron-specific enolase (NSE) levels were studied.
Results:
Overall, the incidence of POCD at 3 months was 50%, and this was not significantly different between both groups (51.4 vs 50.0%, P = 0.90). Having <6 years of formal education [risk ratio (RR) = 3.014, 95% confidence interval (CI) = 1.054–8.618, P = 0.040] was significantly associated with POCD in the CCPB group, while the lowest hematocrit during cardiopulmonary bypass was independently associated with POCD in the MCPB group (RR = 0.931, 95% CI = 0.868–0.998, P = 0.044). The postoperative inflammatory markers and NSE levels were similar between the two groups.
Conclusions:
This study shows that the MCPB was not superior to CCPB with cell salvage and biocompatible tubing with regard to the neurocognitive outcomes measured by the RBANS.
Keywords: Cardiopulmonary bypass, postoperative cognitive decline, repeatable battery of neuropsychological status
Introduction
Postoperative cognitive dysfunction (POCD) is a common complication of cardiopulmonary bypass (CPB) with a reported incidence of 19–38%.[1] Cerebral microembolization,[2,3] perioperative hyperglycemia,[4] hypoperfusion, and inflammation have been implicated in the causation of POCD after cardiac surgery.
The miniaturized cardiopulmonary bypass (MCPB) system was developed to reduce hemodilution and inflammation[5] while providing the surgeons with the ideal operating conditions of a quiet heart. By eliminating the cardiotomy suction, utilizing biocompatible tubings, and reducing the exposure to foreign surface area in the MCPB circuit, it reduces the activation of intrinsic and adaptive immune response that is implicated in POCD.[6,7,8]
While there are reports suggesting that the MCPB system is associated with a 10-fold reduction in the incidence of postoperative strokes as compared to the conventional cardiopulmonary bypass (CCPB) system,[9] it is unclear if it is similar for POCD. It is also uncertain if risk factors for POCD between the patients undergoing MCPB vs CCPB are similar.
We aimed to study if MCPB reduces the rate of POCD as compared to CCPB and if the risk factors for POCD were similar between patients undergoing CCPB when compared to the MCPB group.
Methods
Study design and population selection
With institutional review board approval and written informed consent, 78 patients undergoing elective and isolated CABG surgery in a tertiary heart center in Singapore were recruited between February 2009 and December 2012. They were randomly assigned to the MCPB or CCPB group using the sealed envelope technique. This is a prospective single-blinded randomized controlled trial. This clinical trial was not registered before patient enrolment as the Singapore Clinical Trials Register was launched in the year 2012.
The inclusion criteria were patients aged between 21 and 85 years with no previous cardiac surgery done. The exclusion criteria were patients with poor left ventricular ejection fraction (<30%), immunologic disease or malignancies, acute inflammatory disease, coagulopathy, steroid treatment, significant carotid disease, and on dialysis.
Sample size calculation
We assumed a POCD rate of 40% at 3 months for the CCPB group and 10% for the MCPB group. Therefore, the required sample size for a power of 0.8 and α of 0.05 was 32 patients in each group. The final sample of 39 in each group included a 20% buffer.
MCPB system
The extra corporeal circuit optimized system is an integrated system developed specifically for miniaturized extracorporeal circulation. It is based on an integrated disposable set that is a closed loop, kinetically assisted active drainage system including a venous bubble trap, centrifugal pump, heat exchanger, and oxygenator, all integrated into a single device. The system includes a hardware platform based on the Stockert heart–lung machine, and is intended for use with a cell-saver system. The pump possesses excellent air-handling characteristics, a low index of hemolysis, and a low priming volume (800–900 mL). Patients can be safely perfused up to 5.0–5.5 L/min. The system is provided in a 100% phosphorylcholine-coated circuit (Phisio, Sorin Group, Mirandola, Italy). Blood in the surgical field was not returned to the MCPB system in order to reduce air–blood interface. Instead, a cell-saver device was used to suction blood from the field. Left ventricular venting was used in all patients, with the aspirated blood channeled to the cell-saver device.
CCPB System
The priming volume was between 1300 and 1400 mL. The bypass circuit consisted of a nonpulsatile roller pump (Stockert Instruments, Munich, Germany) and an identical oxygenator to that of the MCPB circuit. Vented blood was forwarded from the field to the hard-shell cardiotomy reservoir in the phosphorylcholine-coated tubing circuit. Suctioned blood from the field was directed to a cell saver (Electa, Sorin, Italy).
Anesthesia and surgical management
All patients underwent cross-clamp during CPB. Both groups received similar standardized anesthesia management, with the use of low-dose opioids (10–20 μg/kg) and inhalational agents during CPB. Aprotinin and/or antifibrinolytics were not given. The amount of fluid infused before commencement of CPB was limited to 500 mL in both groups. Small boluses of phenylephrine were used to support hemodynamics during autologous blood back-priming of the MCPB circuit with patients’ blood. Blood pressure and temperature control was proctocolized, with blood pressure kept within strict limits (mean arterial pressure kept between 50 and 80 mmHg) with mild hypothermia without active cooling to 34°C.
Measurement of POCD
POCD refers to a spectrum of postoperative central nervous system dysfunction. POCD was defined in accordance with the repeatable battery of neuropsychological status (RBANS) score.
The RBANS evaluates five domains, the immediate memory, delayed memory, attention, visuospatial ability, and language, of the patients. It was performed approximately 1 week before CPB by a research assistant who was trained to administer and score the neuropsychological performance. Postsurgical evaluation was completed 3 months after CPB. The RBANS score was converted into a scale that put the patients in one out of five categories in each of the five domains tested in the RBANS. A patient with a drop of one category in any domain of the RBANS was considered to have POCD. The analysis of RBANS was done by a psychologist with domain expertise in the use of RBANS.
Inflammatory and neuronal damage biomarkers
Venous blood samples were obtained for measuring tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). These were taken at induction of anesthesia (baseline), upon arrival at intensive care unit (ICU), and at 6, 12, 24, and 48 h in the ICU.
Blood for testing neuron-specific enolase (NSE) was taken during induction of anesthesia (baseline), and 24 and 48 h in the ICU. The marker levels were not corrected for hemodilution.
Statistical analyses
Demographics, clinical characteristics, and RBANS profiles of cognitive impairment were analyzed descriptively. To compare the two CPB groups, univariate analyses were done with the use of two-tailed unpaired t-test for continuous variables and the Chi-square test for categorical variables. Univariate and multivariate analyses were then done to identify the risk factors of POCD for each CPB group. Univariate factors with P < 0.1 were then added into the multivariate model. Multivariate analysis was performed using the Poisson regression model with robust estimator to estimate the adjusted relative risk (RR) for developing POCD for each CPB group of patients. The statistical significance was taken as P < 0.05. All statistical analyses were performed using PASW Statistics version 18 (IBM, New York, USA).
Results
Out of 78 patients, four patients were lost to follow-up and three patients died before follow-up. Therefore, data from 71 patients were analyzed. There were 35 patients in the CCPB group and 36 patients in the MCPB group [Figure 1].
Figure 1.
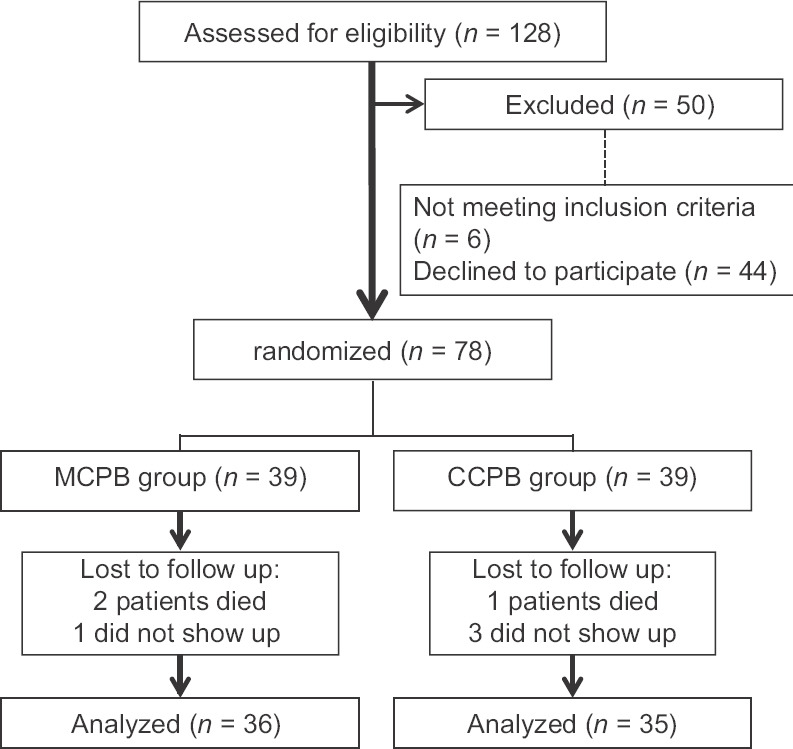
Flowchart representing patient selections
Demographic, clinical data, and perioperative characteristics
The demographic and clinical characteristics of the patients are summarized in Table 1. The patients were predominantly male and had an average age of 60 years. A large proportion of the cohort received <6 years of formal education and this did not differ between the two groups (P = 0.19). Patient risk profile according to the European System for Cardiac Operative Risk Evaluation (EuroSCORE) was similar between the two groups. The lowest and mean cardiac index was significantly lower in the MCPB group (P < 0.001), while the lowest hematocrit during CPB was significantly higher in the MCPB group (P < 0.001). There was no significant difference for the preoperative TNF-α and IL-6 levels between the two groups (P = 0.92; P = 0.55) [Table 1].
Table 1.
Univariate analysis of perioperative variables between MCPB and CCPB groups
| Perioperative variables | CCPB (n=35) | MCPB (n=36) | P |
|---|---|---|---|
| Demographics | |||
| Gender:male | 26 (74.3) | 25 (69.4) | 0.65 |
| Age (years) | 61.0±9.1 | 59.8±8.6 | 0.55 |
| Body mass index (kg/m2) | 22.5±4.5 | 23.9±3.1 | 0.14 |
| <6 years of formal education | 21 (60.0) | 16 (44.0) | 0.19 |
| Preoperative clinical characteristics | |||
| Hypertension | 28 (80) | 33 (91.7) | 0.19 |
| Diabetes mellitus | 16 (45.7) | 21 (58.3) | 0.29 |
| Acute myocardial infarction | 14 (40) | 15 (41.7) | 0.89 |
| EuroSCORE logistic | 1.2±0.7 | 1.1±0.6 | 0.41 |
| Preoperative markers | |||
| TNF-a level (ng/L) | 9.5±4.2 | 9.6±3.5 | 0.92 |
| IL-6 level (ng/L) | 2.2±1.7 | 2.5±1.9 | 0.55 |
| NSE level (mg/L) | 7.7±2.0 | 9.6±6.0 | 0.09 |
| Intraoperative variables | |||
| CPB time (min) | 97.3±17.6 | 102.9±33.1 | 0.37 |
| Aortic cross clamp time (min) | 51.4±11.3 | 58.2±26.3 | 0.16 |
| Hyperglycemia (≥11.1 mmol/L) | 1 (2.9) | 4 (11.1) | 0.56 |
| Intraoperative hemodilution | |||
| Prebypass hematocrit (%) | 37.2±5.2 | 35.3±4.9 | 0.12 |
| CPB lowest hematocrit (%) | 22.5±2.2 | 24.9±4.9 | 0.010 |
| Red blood cell transfusion | 11 (31.4) | 11 (30.6) | 0.94 |
| Perfusion during CPB | |||
| Lowest cardiac index during CPB (L/min/m2) | 2.4±0.1 | 2.1±0.3 | <0.001 |
| Mean cardiac index during CPB (L/min/m2) | 2.6±0.1 | 2.4±0.2 | <0.001 |
| Lowest SvO2 (%) | 63.9±10.3 | 69.5±5.9 | 0.006 |
| Postoperative markers | |||
| TNF-a level at 24 h in ICU (ng/L) | 12.7±5.2 | 12.0±4.6 | 0.56 |
| IL-6 level at 24 h in ICU (ng/L) | 160.7±146.7 | 182.3±99.1 | 0.47 |
| Highest postoperative NSE level (mg/L) | 18.0±7.1 | 18.3±7.5 | 0.89 |
| Postoperative outcomes | |||
| Postoperative cognitive dysfunction | 18 (51.4) | 18 (50.0) | 0.90 |
| Length of hospitalization (days) | 9.7±4.0 | 8.8±3.9 | 0.34 |
Figures are number (percent) or mean±standard deviation. CCPB: Conventional cardiopulmonary bypass, CPB: Cardiopulmonary bypass, MCPB: Miniaturized cardiopulmonary bypass, EuroSCORE: European System for Cardiac Operative Risk Evaluation, IL-6=interleukin-6, NSE: Neuron-specific enolase, SVO2: Mixed venous oxygen saturation, TNF-a: Tumor necrosis factor-alpha
Hyperglycemia and atheroma burden
Hyperglycemia, as defined by serum glucose ≥11.1 mmol/L, was similar between the two CPB groups (P = 0.56) [Table 1] and were not associated with POCD in either group (CCPB: P = 1.00; MCPB: P = 0.10).
Routine echocardiography was not done for all the patients. Out of the patients who underwent echocardiography, the atheroma burden was not significantly different between the two CPB groups (P = 0.22) and were not associated with POCD in either group (CCPB: P = 1.00; MCPB: P = 0.58).
Neurocognition and inflammation
A total of 36 patients had POCD after cardiopulmonary surgery (50.7%). There was no significant difference in the incidence of POCD between the two groups (P = 0.90). None of the patients had a stroke within 3 months after surgery and the highest postoperative NSE level was not significantly different between the CCPB and MCPB groups (P = 0.89) [Table 1].
Inflammation (measured by TNF-α and IL-6) was similar between the CCPB and MCPB groups [Table 1] and was not significantly associated with POCD in either of the CPB groups.
Risk factor for POCD
Having <6 years of formal education was independently associated with POCD in the CCPB group [RR = 3.014, 95% confidence interval (CI) = 1.054–8.618, P = 0.040] [Table 2].
Table 2.
Multivariate analysis for perioperative risk factors of POCD for the CCPB group
| Perioperative variables | Relative risk | 95% Confidence interval | P |
|---|---|---|---|
| <6 years of formal education | 3.014 | 1.054-8.618 | 0.040 |
| Diabetes mellitus | 2.131 | 0.987-4.601 | 0.05 |
| Prebypass hematocrit (%) | 1.006 | 0.960-1.054 | 0.80 |
CCPB: Conventional cardiopulmonary bypass
The lowest hematocrit during CPB was independently associated with POCD in the MCPB group (RR = 0.931, 95% CI = 0.868–0.998, P = 0.044) [Table 3].
Table 3.
Multivariate analysis for perioperative risk factors of POCD for the MCPB group
| Perioperative variables | Relative risk | 95% Confidence interval | P |
|---|---|---|---|
| Diabetes mellitus | 1.203 | 0.505-2.869 | 0.68 |
| Lowest hematocrit during CPB (%) | 0.931 | 0.868-0.998 | 0.044 |
CPB: Cardiopulmonary bypass, MCPB: Miniaturized cardiopulmonary bypass
Length of hospitalization
Patients with POCD had a significantly longer length of hospitalization of 10.2 ± 4.2 days compared to patients without POCD (8.3 ± 3.6 days, P = 0.048). However, there was no significant difference between the POCD patients in the CCPB or MCPB group (9.9 ± 3.6 days vs 10.4 ± 4.8 days, P = 0.75).
Discussion
POCD after cardiac surgery remains a problem despite advances in surgical techniques and care for patients, with the potential to adversely impact quality of life.[10,11,12] None of the patients in either the MCPB or CCPB group developed a stroke. The incidence of POCD in our study was 50% at 3 months postoperatively. This is higher than previous studies reporting an incidence of 3–38%.[1] There was no difference in the incidence of POCD between the MCPB and CCPB groups.
The higher incidence of POCD in our study could be due to the fact that the majority of patients in the study population received <6 years of formal education. This is a known risk factor for development of POCD.[13] Another reason for the higher incidence in our population is that we used the RBANS, which is a specific tool to detect POCD in patients with lower education levels. The RBANS comprises a reliable battery of tests that specifically corrects for the learning effect common in other standard neurocognitive tests, such as the Rey Auditory Verbal Learning Test, Trial making A and B, and Grooved Pegboard tests previously used to detect POCD.[14] Furthermore, the RBANS has been validated in the local population.[15]
A previous meta-analysis demonstrated a significant reduction in the incidence of stroke between the MCPB and CCPB groups[9] and the MCPB has been previously shown to have improved cerebral perfusion and reduced overall inflammation as compared to CCPB with neurocognitive outcomes.[16,17,18] However, we found that there was no significant difference for POCD between the two groups. This could be due to a number of reasons.
The pathophysiology of POCD is possibly different from stroke, which is largely due to hypoperfusion secondary to embolic phenomenon or thrombotic events.[19] We demonstrated that there was no correlation between NSE, an early marker of neuronal damage in stroke, and POCD; and this corroborates with a previous meta-analysis.[20] This suggests that the development of POCD might be via other mechanisms. While the exact mechanism of POCD is still unknown, Cibelli et al. demonstrated in animal studies that inflammation plays a critical role in the pathogenesis of POCD, as evidenced by the protection afforded to surgical animals by minocycline which was a nonspecific inhibitor of inflammation[21] and Ramlawi et al. demonstrated that the inflammatory response is significantly associated with POCD. The inflammatory response that elicited following CPB has been implicated in end-organ damage, via a complex sequence of events leading to the final activation of leukocytes and endothelial cells. This process has been postulated to be responsible for cell dysfunction in different organs.[22]
Inflammation and POCD
Inflammation plays an important role in POCD associated with cardiac surgery.[22] We looked at TNF-α and IL-6 as surrogate markers of the systemic inflammation that occurs during CCPB and MCPB and their relation to POCD. Similar to other studies,[5,23] we demonstrated an overall upward trend of the levels of TNF-α and IL-6 from the preoperative to postoperative period in both the CCPB and MCPB groups.
However, the inflammatory response and the incidence of POCD were similar between both groups. This is likely due to the CCPB modifications; and it concurs with a previous study which showed that the utilization of cell salvage instead of cardiotomy suction in the CCPB system resulted in a comparable systemic inflammation to that of the MCPB system.[23] Moreover, we used biocompatible tubing, which is known to reduce complement activation and proinflammatory cytokine production.[23,24] This further reduced the inflammatory reaction in patients using our modified CCPB system. This suggests that the modified CCPB system is comparable to the MCPB system in terms of the attenuation of the systemic inflammatory response associated with the use of CPB and subsequent development of POCD. Therefore, we were unable to demonstrate an association of inflammation and POCD between the two CPB groups.
Previous studies had shown that a low level of education is a risk factor for POCD, and this was corroborated by our results. Satz[25] had previously described a concept of brain reserve, where a greater brain reserve could serve as a protective factor against POCD whereas a lesser brain reserve is an indicator of vulnerability to POCD. This was further extended by Monk,[26] who postulated that the education level of a patient is a measure of the brain reserve. As such, the patients who had lower levels of education had a lower brain reserve making them more prone to getting POCD.
The hematocrit level in the blood is related to the oxygen carrying capacity in the blood, thereby affecting cerebral oxygenation. It has been shown that reduced cerebral oxygenation is a risk factor for POCD.[27] In our study, patients in the MCPB group who developed POCD had a significantly lower hematocrit level as compared to those who did not develop POCD.
We postulate that the lowest hematocrit on bypass together with the significantly lower cardiac index in the MCPB group may be insufficient for oxygen delivery to the brain. Although the lowest hematocrit of 23.1% in patients who developed POCD in the MCPB group is above the transfusion trigger, the low cardiac index would require higher volume resuscitation. In addition, this period of low cardiac index and borderline hematocrit may be prolonged, hence increasing the risk of POCD. This is in contrast to the CCPB system where the higher flows could compensate for the low hematocrit for adequate cerebral perfusion. As such, the hematocrit level that is required during MCPB for adequate oxygenation of the brain needs to be redefined. Strategies to counteract the reduced cardiac index should include restrictive crystalloid volume management or even blood transfusion to reduce the incidence of POCD in patients using the MCPB system during cardiac surgery.
Strengths and limitations
This study has several strengths. It is a randomized controlled trial and there is no treatment bias. The primary endpoint of POCD was clearly defined by the RBANS, which consists of a reliable battery of tests and specifically corrects for the learning effect common in other standard neurocognitive tests and has been validated in a local study for this study population.
Apart from looking at factors contributing to POCD in each arm, we also analyzed the various components of each circuit that could reduce the risk of POCD. This systematic approach and modification to the CCPB circuit with cell salvage and biocompatible tubing differentiates from other studies that did not attempt to attenuate the inflammatory response in the CCPB system.
Our study did not show that the MCPB was superior to the CCPB with regards to the RBANS, but instead highlighted the difference in risk factors for POCD for each group. A lower level of formal education was associated with POCD in the CCPB group, while the lowest hematocrit level was important in the MCPB group despite better preservation of hematocrit in this group of patients.
Only elective patients undergoing uncomplicated CABG were included in the study; therefore, the benefits of the MCPB may not have been apparent. Other methods of detecting POCD such as transcranial Doppler to detect cerebral desaturations can be employed in future studies.
Conclusion
This study shows that the MCPB was not superior to CCPB with cell salvage and biocompatible tubing with regard to the neurocognitive outcomes measured by the RBANS. There were differing risk factors of POCD for both groups of patients.
Financial support and sponsorship
This work was supported by the National Medical Research Council, Singapore (grant number: NMRC IRG07nov119).
Conflicts of interest
There are no conflicts of interest.
References
- 1.Toeg HD, Nathan H, Rubens F, Wozny D, Boodhwani M. Clinical impact of neurocognitivedeficits after cardiac surgery. J Thorac Cardiovasc Surg. 2013;145:1545–9. doi: 10.1016/j.jtcvs.2013.02.061. [DOI] [PubMed] [Google Scholar]
- 2.Hammon JW, Jr, Stump DA, Kon ND, Cordell AR, Hudspeth AS, Oaks TE, et al. Risk factors and solutions for the development of neurobehavioral changes after coronary artery bypass grafting. Ann Thorac Surg. 1997;63:1613–8. doi: 10.1016/s0003-4975(97)00261-0. [DOI] [PubMed] [Google Scholar]
- 3.Djaiani G, Fedorko L, Borger MA, Green R, Carroll J, Marcon M, et al. Continuous-flow cell saver reduces cognitive decline in elderly patients after coronary bypass surgery. Circulation. 2007;116:1888–95. doi: 10.1161/CIRCULATIONAHA.107.698001. [DOI] [PubMed] [Google Scholar]
- 4.Yan X, Gorman J, Hoffman SN, Zhang L, Boscarino JA. Perioperative hyperglycemia is associated with postoperative neurocognitive disorders after cardiac surgery. Neuropsychiatr Dis Treat. 2014;10:361–70. doi: 10.2147/NDT.S57761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fromes Y, Gaillard D, Ponzio O, Chauffert M, Gerhardt MF, Deleuze P, et al. Reduction of the inflammatory response following coronary bypass grafting with total minimal extracorporeal circulation. Eur J Cardiothorac Surg. 2002;22:527–33. doi: 10.1016/s1010-7940(02)00372-x. [DOI] [PubMed] [Google Scholar]
- 6.Baumgartner WA. Neurocognitive changes after coronary bypass surgery. Circulation. 2007;116:1879–81. doi: 10.1161/CIRCULATIONAHA.107.734087. [DOI] [PubMed] [Google Scholar]
- 7.Kumar RA, Cann C, Hall JE, Sudheer PS, Wilkes AR. Predictive value of IL-18 and SC5b-9 for POCD after cardiopulmonary bypass. Br J Anaesth. 2007;98:317–22. doi: 10.1093/bja/ael366. [DOI] [PubMed] [Google Scholar]
- 8.Ramlawi B, Rudolph JL, Mieno S, Khabbaz K, Sodha NR, Boodhwani M, et al. Serologic markers of brain injury and cognitive function after cardiopulmonary bypass. Ann Surg. 2006;2044:593–601. doi: 10.1097/01.sla.0000239087.00826.b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biancari F, Rimpiläinen R. Meta-analysis of randomised trials comparing the effectiveness of miniaturised versus conventional cardiopulmonary bypass in adult cardiac surgery. Heart. 2009;95:964–9. doi: 10.1136/hrt.2008.158709. [DOI] [PubMed] [Google Scholar]
- 10.Steinmetz J, Christensen KB, Lund T, Lohse N, Rasmussen LS ISPOCD Group. Long-term consequences of postoperative cognitive dysfunction. Anesthesiology. 2009;110:548–55. doi: 10.1097/ALN.0b013e318195b569. [DOI] [PubMed] [Google Scholar]
- 11.Jensen BO, Hughes P, Rasmussen LS, Pedersen PU, Steinbruchel DA. Health-related quality of life following off-pump versus on-pump coronary artery bypass grafting in elderly moderate to high-risk patients: A randomized trial. Eur J Cardiothorac Surg. 2006;30:294–9. doi: 10.1016/j.ejcts.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 12.Rumsfeld JS, Magid DJ, O’Brien M, McCarthy M, Jr, MaWhinney S, Scd, Shroyer AL, et al. Department of Veterans Affairs Cooperative Study in Health Services: Processes, Structures, and Outcomes of Care in Cardiac Surgery. Changes in health-related quality of life following coronary artery bypass graft surgery. Ann Thorac Surg. 2001;72:2026–32. doi: 10.1016/s0003-4975(01)03213-1. [DOI] [PubMed] [Google Scholar]
- 13.Newman MF, Kirchner JL, Phillips-Bute B, Gaver V, Grocott H, Jones RH, et al. Neurological Outcome Research Group and the Cardiothoracic Anesthesiology Research Endeavors Investigators. Longitudinal assessment of neurocognitive function after coronary-artery bypass surgery. N Engl J Med. 2001;344:395–402. doi: 10.1056/NEJM200102083440601. [DOI] [PubMed] [Google Scholar]
- 14.Murkin J, Newman S, Stump D, Blumenthal J. Statement of consensus on assessment of neurobehavioral outcomes after cardiac surgery. Ann Thorac Surg. 1995;59:1289–95. doi: 10.1016/0003-4975(95)00106-u. [DOI] [PubMed] [Google Scholar]
- 15.Lim ML, Collinson SL, Feng L, Ng TP. Cross-cultural application of the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): Performances of elderly Chinese Singaporeans. Clin Neuropsychol. 2010;24:811–26. doi: 10.1080/13854046.2010.490789. [DOI] [PubMed] [Google Scholar]
- 16.Alsatli RA. Mini cardiopulmonary bypass: Anesthetic considerations. Anesth Essays Res. 2012;6:10–3. doi: 10.4103/0259-1162.103364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bennett M, Weatherall M, Webb G, Dudnikov S, Lloyd C. The impact of haemodilution and bypass pump flow on cerebral oxygen desaturation during cardiopulmonary bypass-A comparison of two systems of cardiopulmonary bypass. Perfusion. 2015;30:389–94. doi: 10.1177/0267659114548256. [DOI] [PubMed] [Google Scholar]
- 18.Anastasiadis K, Argiriadou H, Kosmidis MH, Megari K, Antonitsis P, Thomaidou E, et al. Neurocognitive outcome after coronary artery bypass surgery using minimal versus conventional extracorporeal circulation: A randomised controlled pilot study. Heart. 2011;97:1082–8. doi: 10.1136/hrt.2010.218610. [DOI] [PubMed] [Google Scholar]
- 19.Mohr JP, Albers GW, Amarenco P, Babikian VL, Biller J, Brey RL, et al. American heart association prevention conference.IV. Prevention and rehabilitation of stroke. Stroke. 1997;28:1501–6. doi: 10.1161/01.str.28.7.1501. [DOI] [PubMed] [Google Scholar]
- 20.Peng L, Xu L, Ouyang W. Role of peripheral inflammatory markers in postoperative cognitive dysfunction (POCD): A meta-analysis. PLoS One. 2013;8:e79624. doi: 10.1371/journal.pone.0079624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cibelli M, Fidalgo AR, Terrando N, Ma D, Monaco C. Role of interleukin-1 beta in postoperative cognitive dysfunction. Ann Neurol. 2010;68:360–8. doi: 10.1002/ana.22082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ramlawi B, Rudolph JL, Mieno S, Feng J, Boodhwani M, Khabbaz K, et al. C-reactive protein and inflammatory response associated to neurocognitive decline following cardiac surgery. Surgery. 2006;140:221–6. doi: 10.1016/j.surg.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 23.Kiaii B, Fox S, Swinamer SA, Rayman R, Higgins J, Cleland A, et al. The early inflammatory response in a mini-cardiopulmonary bypass system: A prospective randomized study. Innovations (Phila) 2012;7:23–32. doi: 10.1097/IMI.0b013e3182552ade. [DOI] [PubMed] [Google Scholar]
- 24.Day JR, Taylor KM. The systemic inflammatory response syndrome and cardiopulmonary bypass. Int J Surg. 2005;3:129–40. doi: 10.1016/j.ijsu.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 25.Satz P. Brain reserve capacity on symptom onset after brain injury: A formulation and review of evidence for threshold theory. Neuropsychology. 1993;7:273–95. [Google Scholar]
- 26.Monk TG, Price CC. Postoperative cognitive disorders. Curr Opin Crit Care. 2011;17:376–81. doi: 10.1097/MCC.0b013e328348bece. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Browne SM, Halligan PW, Wade DT, Taggart DP. Postoperative hypoxia is a contributory factor to cognitive impairment after cardiac surgery. J Thorac Cardiovasc Surg. 2003;126:1061–4. doi: 10.1016/s0022-5223(03)00616-0. [DOI] [PubMed] [Google Scholar]


