Highlights
-
•
Malian healthcare workers presented mental disorders in the early stage of COVID-19.
-
•
Nurses were at lower risk of mental health disorders than other worker categories.
-
•
Women were at greater risk of mental health disorders than men.
-
•
A lack of protection equipment and nurses was associated with mental disorders.
Keywords: Mali, COVID-19, Mental health, Healthcare workers, HIV
Abstract
Background and objectives
In Mali, the non-governmental association (NGO) ARCAD Santé PLUS launched the CovidPrev program in response to the COVID-19 outbreak to ensure continuity of HIV care-related activities. This study aimed to identify individual and structural factors associated with mental health disorders (MHD) in the NGO’s healthcare workers (HCW) in the early stage of the outbreak.
Methods
Data were collected between April 6 and 11, 2020 for 135 HCW in ARCAD Santé PLUS’s 18 community-based HIV care centers. Outcomes corresponded to the PHQ-9, GAD-7 and ISI instruments for depression, anxiety and insomnia, respectively. A general mixture model with a negative binomial distribution was implemented.
Results
Most HCW were men (60.7%) and median age was 40 years IQR[33-46]. Symptoms of depression, anxiety and insomnia were declared by 71.9, 73.3, and 77% participants, respectively. Women were at greater risk of MHD. A lack of personal protection equipment and human resources, especially nurses, was associated with a high risk of MHD.
Conclusions
Health policy must place non-front line HCW, including those in NGOs, at the core of the healthcare system response to the COVID-19 outbreak, as they ensure continuity of care for many diseases including HIV. The efficacy of public health strategies depends on the capacity of HCW to fully with and competently perform their duties.
1. Introduction
As of July 14, 2020, the COVID-19 case-fatality rate in Mali was the fifth highest in the World Health Organization’s (WHO) African region, and the third highest among West African countries, with deaths representing 5.0% of total cases behind 6.2% and 5.1% in Niger and Burkina Faso, respectively [1]. The first cases in Mali were observed on March 25, 2020, over a month after the continent’s first case, and 6 and 16 days after the two abovementioned countries, respectively. However, the number of cumulated cases in Mali was much higher up to July 14: 2423 cases versus 1037 and 1099 cases in Burkina Faso and Niger, respectively [1]. The lag between Africa’s first cases and those in Mali did not create the same opportunity – in terms of prompt emergency preparation – which the lag in 2014 created during the Ebola outbreak. Moreover, international aid has slowed down because of COVID-19s pandemic status. Data for Mali indicate that authorities’ proactive decisions to contain the disease’s spread, including commercial air traffic interruption, bans on mass gatherings and curfews, [2] have been insufficient. Furthermore, as observed elsewhere, the public health response is being undermined by poor adherence to social distancing for different reasons [3], [4]. However, the most likely explanation for Mali’s higher vulnerability and poorer medical outcomes is its inherently weak healthcare system. Compared with Niger and Burkina Faso, the shortage of healthcare workers (HCW), health expenditures and infrastructure is more acute in Mali [5]. More specifically, the country’s dependency on foreign aid, unreliable medical equipment, difficulties to procure drugs [6], staff attrition [7], shortage of human resources (HR) [8], [9] and resulting degradation of working conditions – including increased workload [10], [11], [12]- all contribute to putting HCW who are on the front line fighting COVID-19 under greater stress. Added to this is the fact that care for COVID-19 is only concentrated in 6 hospitals (5 in Bamako and 1 in Kati (19 Km from Bamako)) positioned at the top of the country’s 4-level healthcare pyramid [13]. The deleterious impact on HCW mental health [14], [15] because of the these structural problems and unpreparedness to contain COVID-19 constitutes a serious public health issue [16]. Unfortunately, data about mental health among HCW in Mali is inexistent. However, the WHO asserts that increasing terrorism and insecurity in Mali since 2012 are two factors that could have mental health implications for the general population [17], and therefore this would include HCW.
Lessons learned from previous disease outbreaks in the world, such as SARS-Cov-1 in 2003, which resulted in severe psychological damage in HCW, highlighted the need to strengthen HCW mental resilience and their preparation for new outbreaks, by providing psychological first aid [18], [19], [20], [21]. Despite this, a growing body of literature on the current COVID-19 outbreak indicates a high prevalence of mental health disorders (MHD) in HCW, suggesting they were not adequately prepared for the magnitude of this pandemic [22], [23], [24], [25], [26], [27], [28]. Studies found that between 20.1 and 64.7% of HCW had depressive symptoms, 35.1 to 51.6% anxiety symptoms, and 18.2 and 38.9% insomnia [25], [26], [27], [29]. MHD were often associated with gender, occupational differences, age [26], [27], [30], place of work, and poor social support [31]. Although structural factors were evoked in some cases as moderators of MHD risk [28], no study to date has adequately examined their effect on HCW psychological outcomes. The current unprecedented pandemic is expected to have a long-lasting effect on mental health, especially for HCW [32], [33]. Various studies all urge specific interventions to mitigate this effect, and to ensure HCW wellbeing during and after the pandemic [34], [35], [36]. Training, social support, communication, and effective health equipment procurement are the primary elements suggested [37], [38], [39], [40], [41], [42], [43]. However, most of the abovementioned studies concerned developed countries, and focused primarily on front-line HCW. Few studies to date have highlighted the importance of also taking into account non-front-line HCW, including community health workers (CHW) and other non-medical staff [39], [44]. Indeed, the absence of significant differences in psychological outcomes between these HCW and their front-line counterparts suggests that the risk of MHD during the current outbreak is similar in both groups [24], especially in low-income countries [21]. Furthermore, empirical studies performed to date were all conducted at an advanced stage (understood here as between 2 and 4 months after the outbreak started) in the countries investigated. They did not account for psychological profiles at outbreak onset (i.e., baseline) or in the early stage (understood here as the first 2 weeks). The mental health impact of COVID-19 might be more severe on HCW with a fragile baseline profile [19], [35]. Accordingly, while assessing MHD as the outbreak develops is vital to provide suitable psychological support, understanding profiles in the early stage is also essential to identify the most vulnerable HCW.
COVID-19′s rapid spread throughout the world raised the question early on of whether African countries, especially those in sub-Saharan Africa (SSA), were adequately prepared or not [45], [46], [47], [48]. Although the extent of the outbreak is currently less dramatic than initially feared, SSA authorities continue to give top priority to its containment, with little attention for preexisting serious public health concerns, especially the fight against malaria, tuberculosis and HIV. The potential interruption of prevention activities and treatment (e.g., antiretroviral treatment (ART)) could harm the advances already made by SSA countries in this fight [49], [50]. Fortunately, the work of non-governmental organizations (NGOs) – which play a crucial role in controlling these diseases in SSA countries – is, at least in part, compensating for this lack of attention. Furthermore, lessons learned by NGOs from previous outbreaks and epidemics, especially HIV, are invaluable, and must be integrated into the overall response to COVID-19 and future outbreaks [2], [51]. NGOs providing healthcare services in Mali are located at the bottom level of the country’s 4-level healthcare pyramid, specifically at the community level. Together with public community healthcare centers, they offer basic health services (e.g. essential medicines, maternity room, prevention and promotion of health, etc.) and are the main point of entry into the healthcare system. HCW in these healthcare structures screen for people with health conditions (e.g. people with COVID-19 symptoms) requiring referral to structures in the 3 higher levels of care (district, regional, or national) [52], [53].
The involvement of some Malian NGOs in health promotion and care activities has contributed to the achievement of important milestones in the country’s response to other epidemics, such as HIV. This is especially true of ARCAD Santé PLUS, the main Malian NGO working on improving access to healthcare for people living with HIV (PLWH) and other vulnerable populations since 1994. In December 2019, the number of PLWH receiving HIV care in the NGO’s 18 healthcare sites – located in 6 of the country’s 10 administrative regions – was close to 29 000, or 26% of the PLWH in Mali. This is a substantial figure when one considers that only 35% of all PLWH in Mali had access to ART in 2016 [54]. The main challenge faced by ARCAD Santé PLUS in the current context is how to adopt government indications to prevent COVID-19 in the workplace. This includes adjusting working hours and adapting HIV care centers’ opening hours to reduce patient flow, while guaranteeing continued prevention and care for HIV and other health problems. On April 1, 2020 (6 days after the first COVID-19 cases in Mali), ARCAD Santé PLUS launched the CovidPrev program whose main objective is to reduce the risk of COVID-19 infection in its HCW (whether salaried or volunteers) and in PLWH frequenting its centers [2].
CovidPrev’s planned reorganization of activities and the continued uncertainty surrounding the outbreak, together with the need to guarantee HIV care-related activities, constitute a double burden for the NGO’s workers. Although not on the front line in the fight against COVID-19, their mental health might be seriously harmed by these supplementary sources of MHD. Prospective research is vital for NGOs to achieve their objectives as part of national public health strategies. However, to our knowledge, no empirical evidence exists concerning the impact of COVID-19 on public health in Africa, and especially on the mental health of front-line and non-front-line HCW. ARCAD Santé PLUS’s activities directly related to the delivery of healthcare are performed by doctors, pharmacy doctors, midwives and nurses. Activities related to prevention (e.g., health awareness, support for treatment adherence) and social support (e.g., moral, material) are primarily performed by CHW (including community mobilizers and navigators) and psychosocial counselors. These two caregiver categories account for a large proportion of ARCAD Santé PLUS’s staff, and are continuously provided training for the promotion of health-, disease- and population-based issues, especially those related to HIV and STIs. Finally, administrative and logistics personnel ensure that the operation runs as smoothly as possible. In terms of the current COVID-19 pandemic, HCW proximity to people – indoors and outdoors – makes them an important vector for disseminating information about COVID-19 in order to protect PLWH and other vulnerable populations. As one of ARCAD Santé PLUS’s top priorities has always been to protect its HCW from health problems – in order to ensure they can optimally provide HIV prevention and care – just days after the NGO’s launch of its CovidPrev program, we implemented a public health and social sciences action research study aimed at providing the NGO with data about the current mental health state of its workforce, so that it could incorporate targeted measures in its CovidPrev Program to protect its HCW. More specifically, this study explored individual and structural factors associated with depression, anxiety and insomnia in this workforce.
2. Materials and methods
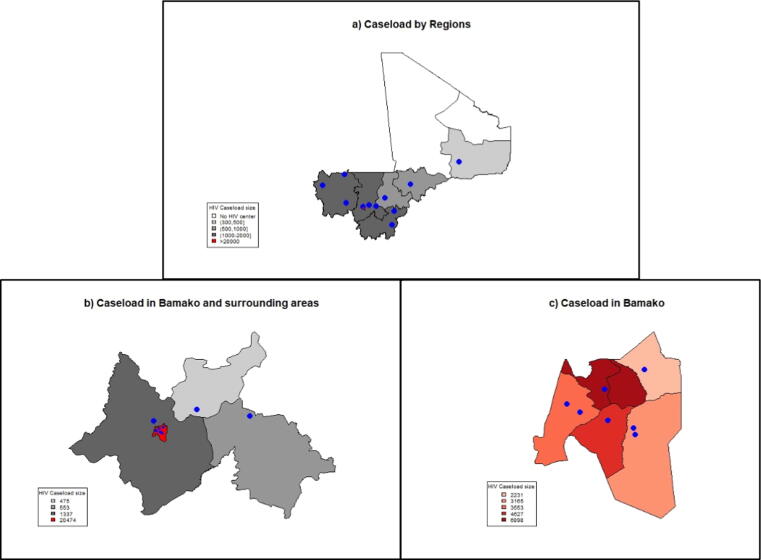
Data were collected from April 6 to 11, 2020 (i.e., two weeks after the first two COVID-19 cases in Mali) for HCW (salaried and volunteers) in ARCAD Santé PLUS’s 18 community-based HIV care centers, located in 6 administrative regions in Mali (Koulikoro, Kayes, Mopti, Ségou, Sikasso, Gao) and in the capital Bamako (Fig. 1).
Fig. 1.
Location of ARCAD Santé PLUS’s community-based HIV care centers in Mali and their caseloads: (a) by region; (b) in Bamako and surrounding areas; and (c) in Bamako.
To be eligible, participants had to be at least 18 years old, and planned to work throughout the outbreak. A self-administered questionnaire collected the following information: demographic and socioeconomic data, self-perceived health status, mental health data, and basic COVID-19 awareness. In addition, structural factors (characteristics) of the 18 HIV care centers (number of years open, HIV caseload, number of doctors, nurses, etc.) were provided by facility managers. Study approval was obtained from the Malian ethical committee (N°2020/57/CE/FMOS/FAPH).
2.1. Outcomes
Analyses were performed for three MHD. The 9-item Patient Health Questionnaire (PHQ-9) was used to assess depression and its severity [55] (total score from 0 to 27). The 7-item Generalized Anxiety Disorder Assessment (GAD-7) was used to measure anxiety [56] (from 0 to 21). Finally, the 7-item Insomnia Severity Index (ISI) assessed participant insomnia during the month preceding the survey [57] (from 0 to 28). All three tools were implemented in their validated French version [58], [59], [60]. Analyses were performed for the three continuous scores.
2.2. Individual characteristics
The following potential individual characteristics to explain individual variability in the outcomes were tested: age (continuous variable); gender (woman = 1 vs man = 0); marital status: married/cohabitating (=1) or single/separated/divorced/widowed (=0); a three-category variable for the number of financially dependent family members, constructed using the median as the cutoff (none, 1–7, and >7); self-perceived health status: “good” (=1) or “very good”/“excellent” (=0); worker type classified into a four-category variable as follows: (i) doctors, pharmacy doctors and midwives; (ii) nurses; (iii) CHW (including community mobilizers and navigators) and psychosocial counselors; (iv) other, including administrative and logistics personnel (secretary, driver, etc.). It is important to note that the worker type variable reflects not only the activity type, but is also a proxy of the worker’s education level: higher than high-school for nurses, midwives, pharmacy doctors and doctors; and lower than high-school for the other worker categories.
To measure preexisting (i.e., prior to the COVID-19 outbreak) serious work-related psychological damage resulting from ethical or moral transgression in the workplace, participants answered the 9-item Moral Injury Event Scale (MIES) [61]. Two sub-scores – perceived transgression (ranging from 1 to 36) and perceived betrayal (1–18) – were constructed, and specified as continuous variables. Finally, basic COVID-19 awareness was assessed using UNICEF’s “fact or fiction” 10-question quiz (Appendix 1) with a score ranging from 0 (no correct response) to 10 (all responses correct).
2.3. HIV care center characteristics
The following potential structural characteristics (all continuous variables) to explain variability in the outcomes due to differences between HIV care centers were tested: the number of years since the center opened, and 6 other variables assessing the density of personnel (per 100 patients) for 6 worker categories (required to permit separate analyses): (i) doctors, (ii) pharmacy doctors, (iii) midwives, (iv) nurses, (v) CHW and (vi) psychosocial counselors.
Healthcare supply characteristics were tested by constructing dichotomous variables indicating whether the center offered (=1) or not (=0) each of the following 12 services: (i) medical consultation for the general population, (ii) specific medical consultation for key populations, (iii) HIV screening, (iv) HIV care for adults and/or pediatric care, (v) delivery of ARV drugs, (vi) biomedical analyses, (vii) nursing care, viii) community-based talks and/or distribution of condoms and lubricants, (ix) psychological care, (x) HIV pre-exposure prophylaxis (PrEP) delivery, (xi) HIV post-exposure prophylaxis (PEP) delivery, and (xii) social/financial support.
Equipment characteristics were tested by constructing 5 dichotomous variables indicating whether each center had (=1) or not (=0) the following items: (i) an electricity generator, (ii) air conditioning, and (iii) a refrigerator. With regard to Personal Protective Equipment (PPE), dichotomous variables indicated the availability (=1) or not (=0) of: (i) face masks, (ii) gowns, (iii) safety goggles, and (iv) gloves.
Finally, an indicator recorded potential drug stock-outs during the previous 6 months (between October 2019 and March 2020) (yes = 1 or no = 0).
2.4. Statistical analyses
Descriptive statistics were calculated for the sample. For the PHQ-9, GAD-7 and ISI scores, statistics included the proportion of non-zero scores, their mean (standard deviation), and median with interquartile range [IQR]. Furthermore, for descriptive purposes only, cutoffs of ≥10, ≥7, and ≥15 were used to distinguish severity for depression, anxiety, and insomnia, respectively [55], [56], [57], [58], [59]. Estimations were performed with the outcomes specified as continuous dependent variables. A general mixture model (GMM) with a negative binomial (NB) distribution was used (see Appendix 2 for details on the estimation strategy).
All statistical analyses were conducted using R software, version 4.0.0 [62].
3. Results
3.1. Individual characteristics
Of the 188 workers identified in ARCAD Santé PLUS’s 18 community-based HIV care centers, 135 were working at the time of data collection and intended to continue working throughout the outbreak (Table 1) (study population). Most were men (60.7%) and median age was 40 years IQR [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46] (see Table 1 for more details on individual characteristics).
Table 1.
Characteristics of the study population (N = 135) and HIV care centers (N = 18).
| N | % | |
|---|---|---|
| Individual characteristics (categorical) | ||
| Sex | ||
| Men | 82 | 60.7 |
| Women | 53 | 39.3 |
| Marital status | ||
| Single/separated/divorced/widowed | 45 | 33.3 |
| Married/cohabitating | 90 | 66.7 |
| Number of economically-dependent family members | ||
| None | 14 | 10.4 |
| 1–7 | 59 | 43.7 |
| >7 | 62 | 45.9 |
| Self-perceived health status | ||
| Very good/excellent | 112 | 83.0 |
| Good | 23 | 17.0 |
| Worker’s position in the community-based HIV center | ||
| Doctor/pharmacy doctor/midwife | 35 | 25.9 |
| Nurse | 20 | 14.8 |
| CHW or psychosocial counselor | 52 | 38.5 |
| Other | 28 | 20.7 |
| Individual characteristics (continuous) | ||
| Age | ||
| Median [IQR] | 40 | [33–46] |
| Min: , Max: | 22 | 60 |
| MIES: Perceived moral transgression (range 1–36) | ||
| Median [IQR] | 15 | [6–26] |
| Min: , Max: | 1 | 36 |
| MIES: Perceived betrayal (range 1–18) | ||
| Median [IQR] | 6 | [3–10] |
| Min: , Max: | 1 | 18 |
| Index of COVID-19 awareness (range 0–10)a | ||
| Median [IQR] | 7 | [7–8] |
| Min: , Max: | 0 | 10 |
| PHQ-9 (depression) (range 0–27) | ||
| Proportion of non-zero scores: N (%) | 97 | 71.9 |
| Non-zero scores: mean (sd) | 6.5 | (4.3, 18.5) |
| MODERATE/severe (score ≥ 10)b | 25 | 18.5 |
| Median [IQR] | 3 | [0–8] |
| Min: , Max: | 0 | 19 |
| GAD-7 (anxiety) (range 0–21) | ||
| Proportion of non-zero scores: N (%) | 99 | 73.3 |
| Non-zero scores: mean (sd, var) | 5.6 | (4.5, 20.25) |
| Moderate/severe (score ≥ 7)b | 29 | 21.5 |
| Median [IQR] | 3 | [0–6] |
| Min: , Max: | 0 | 18 |
| ISI (insomnia) (range 0–28) | ||
| Proportion of non-zero scores: N (%) | 104 | 77.0 |
| Non-zero scores: mean (sd) | 6.1 | (4.0, 16.0) |
| moderate/severe (score ≥ 15)b | 3 | 2.2 |
| Median[IQR] | 4 | [1–7] |
| Min: , Max: | 0 | 20 |
| HIV center characteristics | Median | [IQR] |
| Number of years since opening | 8 | [7–10] |
| HR availability (per 100 PLWH) | ||
| Doctors | 0.13 | [0.06–0.20] |
| Pharmacy doctors | 0.09 | [0.04–0.18] |
| Midwivesc | – | – |
| Nurses | 0.10 | [0.02–0.20] |
| CHW | 0.01 | [0.01–0.37] |
| Psychosocial counselors | 0.06 | [0.0–0.17] |
| No of HIV care centers | No of participants (%) | |
| Healthcare supply | ||
| Medical consultation for general population | ||
| No | 3 | 15 (11.1) |
| Yes | 15 | 120 (88.9) |
| Specific medical consultation for key populations | ||
| No | 4 | 21 (15.6) |
| Yes | 14 | 114 (84.4) |
| HIV screeningd | ||
| No | – | – |
| Yes | 18 | 135 (100.0) |
| HIV care for adults and/or pediatric care | ||
| No | 2 | 20 (14.8) |
| Yes | 16 | 115 (85.2) |
| Delivery of antiretroviral drugs | ||
| No | 2 | 20 (14.8) |
| Yes | 16 | 115 (85.2) |
| Biomedical analyses | ||
| No | 5 | 37 (27.4) |
| Yes | 13 | 98 (72.6) |
| Nursing care | ||
| No | 5 | 19 (14.1) |
| Yes | 13 | 116 (85.9) |
| Community-based talks and/or distribution of condoms and lubricants | ||
| No | 2 | 9 (6.7) |
| Yes | 16 | 126 (93.3) |
| Psychological cared | ||
| No | – | – |
| Yes | 18 | 135 (100.0) |
| Delivery of HIV pre-exposure prophylaxis (PrEP) | ||
| No | 16 | 113 (83.7) |
| Yes | 2 | 22 (16.3) |
| Delivery of HIV post-exposure prophylaxis (PEP) | ||
| No | 5 | 27 (20.0) |
| Yes | 13 | 108 (80.0) |
| Social/financial support | ||
| No | 7 | 41 (30.4) |
| Yes | 11 | 94 (69.6) |
| Equipment in HIV care centers | ||
| Electricity generator | ||
| No | 14 | 86 (63.7) |
| Yes | 4 | 49 (36.3) |
| Air conditioning | ||
| No | 3 | 18 (13.3) |
| Yes | 15 | 117 (86.7) |
| Refrigeratord | ||
| No | – | – |
| Yes | 18 | 135 (100.0) |
| Personal protective equipment (PPE) | ||
| Face masks | ||
| No | 12 | 77 (57.0) |
| Yes | 6 | 58 (43.0) |
| Gownss | ||
| No | 13 | 93 (68.9) |
| Yes | 5 | 42 (31.1) |
| Safety gogglesd | ||
| No | 18 | 135 (100.0) |
| Yes | – | – |
| Gloves | ||
| No | 1 | 11 (8.1) |
| Yes | 17 | 124 (91.9) |
| Drug stock-outs | ||
| During the previous 6 months (October 2019–March 2020) | ||
| No | 10 | 64 (47.4) |
| Yes | 8 | 71 (52.6) |
Constructed using correct responses to UNICEF’s “Fact or fiction” quiz (see Appendix 1).
Presented only for descriptive purposes, as multivariable models were estimated using these scores as continuous variables.
Two HIV care centers declared 1 midwife. The density of midwives for these two centers was 0.01 and 0.02 per 100 PLWH, respectively, although the median and IQR were equal to 0.
These variables were not tested in the model as they were constant across all 18 HIV care centers (i.e., response was similar for all centers).
With respect to study outcomes, Table 1 shows that mean scores were lower than their corresponding variances, justifying the choice to use an NB distribution instead of a Poisson distribution (assuming equal mean and variance). PHQ-9, GAD-7 and ISI scores indicated high prevalences of depression, anxiety and insomnia symptoms in the study population (71.9%, 73.3% and 77%, respectively). Furthermore, 18.5% and 21.5% of all participants had moderate/severe depression and anxiety, respectively, whereas only 2.2% had severe/moderate insomnia.
3.2. HIV care center characteristics
Half the HIV care centers opened before 2012 (Table 1), the median years of activity being 8 IQR[7–12]. In terms of HR availability, median densities (all values per 100 patients) of doctors and nurses were 0.13 (IQR[0.06–0.20]) and 0.10 (IQR[0.02–0.20]), respectively. The most disadvantaged HIV care centers (i.e., the 25% corresponding to the 1st quartile) had extremely limited HR, especially nurses (<0.02) and CHW (<0.01), and no psychosocial counselors.
The most severe PPE shortages concerned goggles (no center), face masks (only 5 centers) and gowns (only 6 centers). Eight centers had experienced drug stock-outs in the 6 months preceding the survey, mostly of ARVs and drugs for opportunistic infections (see Table 1 for more details on services provided).
3.3. Do HIV center characteristics matter for workers’ mental health?
The LR-test comparing 1-level and 2-level null models concluded that variability in PHQ-9 (depression), GAD-7 (anxiety) and ISI (insomnia) scores were due to both individual characteristics and differences in HIV care center characteristics, as indicated by the ICC: 33%, 31% and 16% of the total variability, respectively (see bottom of Table 3).
Table 3.
Two-level model for the estimation of individual and structural factors associated with MHD among HCW (N = 135) in ARCAD Santé PLUS’s 18 HIV care centers.
|
PHQ-9 (Depression) |
GAD-7 (Anxiety) |
ISI (Insomnia) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| IRR | 95%CI | p-value | IRR | 95%CI | p-Value | IRR | 95%CI | p-Value | |
| 1-Level: Individual characteristics | |||||||||
| Gender (ref: Men) | |||||||||
| Women | 1.60 | (1.16–2.21) | 0.004 | 1.34 | (0.95–1.89) | 0.090 | 1.53 | (1.12–2.09) | 0.007 |
| Number of economically-dependent family members (ref: None) | |||||||||
| 1–7 | 2.15 | (1.12–4.11) | 0.021 | – | – | – | – | – | – |
| >7 | 2.48 | (1.31–4.68) | 0.005 | – | – | – | – | – | – |
| Perceived health status (ref: very good/excellent) | |||||||||
| Good | – | – | – | 1.52 | (1.05–2.22) | 0.028 | – | – | – |
| Worker’s position in the community-based HIV center (ref: other) | |||||||||
| Doctor/pharmacy doctor/midwife | 1.25 | (0.81–1.93) | 0.309 | – | – | – | 1.27 | (0.83–1.93) | 0.266 |
| Nurse | 0.40 | (0.20–0.77) | 0.006 | – | – | – | 0.51 | (0.29–0.93) | 0.027 |
| CHW or psychosocial counselor | 0.75 | (0.51–1.12) | 0.164 | – | – | – | 0.65 | (0.43–0.98) | 0.042 |
| Moral injury event scale (MIES) | |||||||||
| Perceived moral transgression (range 1–36) | 1.04 | (1.02–1.05) | <0.001 | 1.03 | (1.01–1.04) | 0.001 | – | – | – |
| Perceived betrayal (range 1–18) | – | – | – | – | – | – | 1.06 | (1.02–1.09) | 0.001 |
| 2-Level: Structural characteristics | |||||||||
| Healthcare supply | |||||||||
| Medical consultation for general population (ref: no) | 4.67 | (1.79–12.20) | 0.002 | – | – | – | – | – | – |
| Personal protective equipment (PPE) | |||||||||
| Face masks (ref: no) | 0.49 | (0.34–0.70) | <0.001 | 0.38 | (0.21–0.67) | 0.001 | 0.57 | (0.38–0.86) | 0.008 |
| HR availability (per 100 PLWH) | |||||||||
| Nurses | 0.09 | (0.01–0.57) | 0.011 | 0.05 | (0.01–0.62) | 0.020 | – | – | – |
| Random Effects (adjusted model) | |||||||||
| σ2 | 0.67 | 0.69 | 0.62 | ||||||
| τ00 | 0 | 0.12 | 0.04 | ||||||
| ICC | 0 | 0.15 | 0.07 | ||||||
| Random Effects (null model) | |||||||||
| σ2 | 0.78 | 0.75 | 0.71 | ||||||
| τ00a | 0.39 | 0.34 | 0.13 | ||||||
| ICC | 0.33 | 0.31 | 0.16 | ||||||
LR-test statistics comparing the 1-level vs the 2-level null models were 326.8 for depression, 298.4 for anxiety, and 231.2 for insomnia. The null hypothesis indicating that 2-level variability is equal to zero (H0: τ00 = 0) was rejected, as the LR-test statistics were higher than the value for the χ2(1) distribution at the 95% confidence level (3.94).
3.4. Depression (PHQ-9)
Bivariate analysis in Table 2 showed that the higher the number of financially-dependent family members, the higher the risk of depression (p = 0.037). This was similar for those who self-perceived good health status (versus very good/excellent, p = 0.029), and for those with a strong perception of work-related moral transgression (p < 0.001) and/or betrayal (p = 0.010). Nurses had the lowest risk of depression (p = 0.006). With regard to structural characteristics, medical consultations for the general population (p < 0.001) and ARV delivery (p = 0.036) were associated with a higher risk of depression. In contrast, depression was less likely in HCW in centers with a higher density of nurses (p = 0.045) and greater availability of face masks (p = 0.039).
Table 2.
Characteristics of the study population (N = 135) and HIV care centers (N = 18).*
| PHQ-9 (Depression) |
GAD-7 (Anxiety) |
ISI (Insomnia) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IRR | 95%CI | p-value | LR-test p-valuea |
IRR | 95%CI | p-Value | LR-test p-valuea |
IRR | 95%CI | p-Value | LR-test p-valuea |
|
| 1-Level: Individual characteristics | ||||||||||||
| Age | 1.01 | (0.99–1.03) | 0.482 | 0.008 | 1.00 | (0.98–1.02) | 0.938 | 0.007 | 1.01 | (1.00–1.03) | 0.131 | 0.021 |
| Gender (ref: Men) | ||||||||||||
| Women | 1.39 | (0.99–1.96) | 0.061 | 0.172 | 1.47 | (1.05–2.05) | 0.027 | 0.076 | 1.42 | (1.03–1.96) | 0.030 | 0.097 |
| Marital status (ref: Single/separated/divorced/widowed) | ||||||||||||
| Married/cohabitating | 1.12 | (0.77–1.63) | 0.557 | 0.291 | 1.30 | (0.90–1.88) | 0.160 | 0.464 | 1.12 | (0.79–1.58) | 0.534 | 0.271 |
| Number of economically-dependent family members (ref: None) | ||||||||||||
| 1–7 | 1.46 | (0.72–2.95) | 0.298 | 0.063 | 1.43 | (0.73–2.81) | 0.301 | 0.966 | 1.54 | (0.79–3.00) | 0.210 | 0.948 |
| >7 | 2.10 | (1.05–4.20) | 0.037 | 1.58 | (0.80–3.11) | 0.187 | 1.60 | (0.83–3.11) | 0.162 | |||
| Perceived health status (ref: very good/excellent) | ||||||||||||
| Good | 1.54 | (1.05–2.28) | 0.029 | 0.081 | 1.65 | (1.13–2.40) | 0.009 | 0.028 | 1.54 | (1.06–2.23) | 0.024 | 0.079 |
| Worker’s position in the community-based HIV center (ref: other) | ||||||||||||
| Doctor/pharmacy doctor/midwife | 1.03 | (0.66–1.60) | 0.902 | 0.043 | 1.01 | (0.64–1.59) | 0.976 | 0.775 | 1.16 | (0.75–1.80) | 0.490 | 0.260 |
| Nurse | 0.37 | (0.18–0.75) | 0.006 | 0.67 | (0.37–1.20) | 0.175 | 0.55 | (0.30–1.00) | 0.052 | |||
| CHW or psychosocial counselor | 0.91 | (0.60–1.38) | 0.655 | 0.87 | (0.57–1.33) | 0.526 | 0.85 | (0.56–1.30) | 0.458 | |||
| Moral injury event scale (MIES) score | ||||||||||||
| Perceived moral transgression (range 1–36) | 1.03 | (1.01–1.05) | 0.001 | 0.091 | 1.03 | (1.01–1.04) | 0.001 | 0.141 | 1.02 | (1.00–1.03) | 0.055 | 0.039 |
| Perceived betrayal (range 1–18) | 1.04 | (1.01–1.08) | 0.010 | 0.661 | 1.02 | (0.99–1.06) | 0.148 | 0.037 | 1.05 | (1.02–1.08) | 0.002 | 0.113 |
| COVID-19 | ||||||||||||
| Awareness index | 0.92 | (0.81–1.03) | 0.154 | 0.179 | 0.91 | (0.80–1.02) | 0.101 | 0.259 | 0.97 | (0.86–1.10) | 0.645 | 0.064 |
| 2-Level: HIV Center characteristics (using the best-fit model for 1-level variables) | ||||||||||||
| Number of years since center opened | 0.95 | (0.88–1.02) | 0.180 | 0.084 | 0.96 | (0.89–1.04) | 0.337 | 0.051 | 1.01 | (0.96–1.07) | 0.649 | 0.024 |
| Healthcare supply | ||||||||||||
| Medical consultation for general population (ref: no) | 5.49 | (1.98–15.16) | <0.001 | 0.001 | 1.89 | (0.69–5.17) | 0.214 | 0.143 | 1.23 | (0.62–2.46) | 0.553 | 0.740 |
| Specific medical consultation for key populations (ref: no) | 0.91 | (0.43–1.91) | 0.802 | 0.759 | 0.90 | (0.42–1.92) | 0.776 | 0.910 | 1.41 | (0.79–2.54) | 0.249 | 0.361 |
| HIV screening (ref: no)b | Not tested | Not tested | Not tested | |||||||||
| HIV care for adults/and pediatric (ref: no) | 2.29 | (0.96–5.45) | 0.061 | 0.057 | 2.27 | (0.96–5.40) | 0.063 | 0.064 | 1.17 | (0.62–2.20) | 0.636 | 0.630 |
| Delivery of antiretroviral drugs (ref: no) | 2.62 | (1.07–6.43) | 0.036 | 0.032 | 1.82 | (0.74–4.50) | 0.191 | 0.161 | 1.40 | (0.72–2.74) | 0.323 | 0.418 |
| Biomedical analyses (ref: no) | 1.22 | (0.62–2.38) | 0.562 | 0.808 | 1.36 | (0.69–2.68) | 0.374 | 0.462 | 0.81 | (0.48–1.36) | 0.419 | 0.601 |
| Nursing care (ref: no) | 0.85 | (0.42–1.74) | 0.658 | 0.798 | 1.16 | (0.53–2.54) | 0.709 | 0.656 | 1.22 | (0.69–2.15) | 0.491 | 0.696 |
| Community-based talks /distribution of condoms and lubricants (ref: no) | 1.48 | (0.48–4.57) | 0.494 | 0.257 | 1.67 | (0.51–5.49) | 0.396 | 0.200 | 1.57 | (0.66–3.72) | 0.306 | 0.251 |
| Psychological careb | Not tested | Not tested | Not tested | |||||||||
| Delivery of HIV pre-exposure prophylaxis (PrEP) (ref: no) | 1.49 | (0.64–3.46) | 0.360 | 0.299 | 1.33 | (0.54–3.27) | 0.539 | 0.403 | 1.37 | (0.77–2.44) | 0.280 | 0.442 |
| Delivery of HIV post-exposure prophylaxis (PEP) (ref: no) | 1.48 | (0.72–3.04) | 0.282 | 0.289 | 1.34 | (0.64–2.81) | 0.445 | 0.490 | 1.16 | (0.69–1.94) | 0.583 | 0.454 |
| Social/financial support (ref: no) | 1.22 | (0.66–2.26) | 0.532 | 0.944 | 1.28 | (0.67–2.47) | 0.458 | 0.625 | 1.04 | (0.65–1.64) | 0.878 | 0.295 |
| Equipment in HIV care centers | ||||||||||||
| Electricity generator(ref: no) | 1.17 | (0.60–2.28) | 0.655 | 0.769 | 1.26 | (0.64–2.51) | 0.500 | 0.608 | 1.14 | (0.71–1.83) | 0.595 | 0.399 |
| Air conditioning (ref: no) | 0.95 | (0.42–2.13) | 0.892 | 0.809 | 1.07 | (0.47–2.47) | 0.866 | 0.713 | 0.74 | (0.42–1.29) | 0.287 | 0.539 |
| Refrigerator (ref: no)b | Not tested | Not tested | Not tested | |||||||||
| Personal protective equipment (PPE) | ||||||||||||
| Face masks (ref: no) | 0.82 | (0.74–0.91) | 0.039 | 0.074 | 0.54 | (0.30–0.98) | 0.041 | 0.067 | 0.57 | (0.38–0.86) | 0.008 | 0.015 |
| Gowns (ref: no) | 1.49 | (0.79–2.81) | 0.217 | 0.298 | 1.29 | (0.66–2.54) | 0.455 | 0.608 | 1.37 | (0.86–2.17) | 0.283 | 0.394 |
| Safety goggles (ref: no) | 0.47 | (0.05–4.43) | 0.512 | 0.105 | Not converged | 1.23 | (0.24–6.23) | 0.804 | 0.220 | |||
| Gloves (ref: no) | 1.00 | (0.29–3.50) | 0.999 | 0.342 | 1.37 | (0.37–5.09) | 0.638 | 0.266 | 1.20 | (0.51–2.83) | 0.684 | 0.578 |
| Drug stock-outs | ||||||||||||
| During the previous 6 months (October 2019–March 2020) (ref: no) | 1.13 | (0.62–2.05) | 0.695 | 0.540 | 1.35 | (0.72–2.51) | 0.347 | 0.502 | 1.20 | (0.78–1.86) | 0.409 | 0.479 |
| HR availability (per 100 PLWH) | ||||||||||||
| Doctors | Not converged | Not converged | Not converged | |||||||||
| Pharmacy doctors | Not converged | Not converged | Not converged | |||||||||
| Midwives | Not converged | Not converged | Not converged | |||||||||
| Nurses | 0.08 | (0.01–0.94) | 0.045 | 0.012 | 0.54 | (0.03–8.45) | 0.657 | 0.102 | 1.70 | (0.24–11.97) | 0.593 | 0.150 |
| CHW | 0.64 | (0.29–1.43) | 0.277 | 0.281 | 0.83 | (0.37–1.83) | 0.637 | 0.663 | 1.30 | (0.76–2.24) | 0.339 | 0.647 |
| Psychosocial counselors | 1.04 | (0.07–16.46) | 0.980 | 0.114 | 1.08 | (0.06–18.20) | 0.959 | 0.111 | 1.10 | (0.15–8.03) | 0.926 | 0.175 |
For the 1-level variables, the restricted model for the LR-test was the null model. For the 2-level variables, the restricted model for the LR-test was the best-fit multivariable model for 1-Level variables.
These variables were not tested in the model as they were constant across HIV care centers (i.e. the response was similar for all 18 centers).
Results in bold correspond to the eligible variables tested in the multivariable model: either with p < 0.2 or LR-test p-value <0.1.
Multivariable analysis (see Table 3) showed that depression was 60% more likely in women than in men (IRR: 1.60, 95%CI(1.16–2.21)). The risk of depression also increased with the number of financially-dependent family members as follows: 2.15 and 2.48 times higher for those declaring 1–7 (IRR: 2.15, 95%CI(1.12–4.11)) and more than 7 (IRR: 2.48, 95%CI(1.31–4.68)) members, respectively, (versus participants reporting none). In terms of worker type, nurses were 60% less likely to have depression than all three other worker categories (IRR: 0.40, 95%CI(0.20–0.77)). Finally, the greater the perception of moral transgression in the workplace, the greater the risk of depression (4% per one-point increase in the associated sub-score, IRR: 1.04, 95%CI(1.02–1.05). With respect to structural characteristics, depression was 4.67 times more likely in HCW who worked in centers offering medical consultations for the general population than centers which did not (IRR: 4.67, 95%CI(1.79–12.20)). Workers in centers where face masks were available were 51% less likely to suffer from depression than their counterparts elsewhere (IRR: 0.49, 95%CI(0.34–0.70)). Finally, the risk of depression decreased by 91% globally across all worker categories per additional nurse per 100 PLWH (IRR: 0.09, 95%CI(0.01–0.57)).
3.5. Anxiety (GAD-7)
The bivariate analysis for anxiety (Table 2) shows that women were at higher risk than men (p = 0.027). Anxiety was also more likely in participants who perceived they had good health status (versus very good/excellent) (p = 0.009). In terms of structural characteristics, face mask availability was associated with a lower risk of anxiety in participants working in centers which provided them (p = 0.041).
The higher risk of anxiety in women was a tendency in the multivariable model (Table 3) (IRR: 1.34, 95%CI(0.95–1.89)). Participants perceiving good health status had a 52% higher risk of anxiety than those who felt they were in very good/excellent health (IRR: 1.52, 95%CI(1.05–2.22)). Finally, the risk of anxiety increased by 3% per one-point increase in the perceived moral transgression sub-score (IRR: 1.03, 95%CI(1.01–1.04)). Face mask availability was associated with a 62% lower risk of anxiety in participants working in centers which provided them (IRR: 0.38, 95%CI(0.21–0.67)). Furthermore, the risk of anxiety was lower in workers in HIV care centers with a higher density of nurses, decreasing by 95% per additional nurse per 100 PLWH (IRR: 0.05, 95%CI(0.01–0.62)).
3.6. Insomnia (ISI)
Sleeping disorders were more frequent in women (p = 0.030), in those perceiving good health status (p = 0.024), and in those perceiving work-related betrayal (p = 0.002) (Table 2). In terms of structural characteristics, insomnia was related to face mask availability (p = 0.008).
Multivariable analysis (Table 3) confirmed the higher risk of insomnia in women (53%) (IRR: 1.53, 95%CI(1.12–2.09)). Insomnia also increased by 6% per one-point increase in the perceived workplace betrayal score (IRR: 1.06, 95%CI(1.02–1.09)). Worker category was related with the risk of insomnia, which was 49% lower in nurses than other HCW (IRR: 0.51, 95%CI(0.29–0.93)). Finally, the only structural factor associated with insomnia was face mask availability. Participants working in care centers where they were available had a 43% lower risk of insomnia (IRR: 0.57, 95%CI(0.38–0.86)).
4. Discussion
MHD prevalence was high in our study population during the early stage (i.e., first 2 weeks) of the COVID-19 outbreak in Mali. More specifically, of ARCAD Santé PLUS’s 135 non-front-line HCW who participated in the present study, 71.9%, 73.3% and 77% declared at least one symptom of depression, anxiety, and insomnia, respectively. These figures are much higher than those in studies of front-line HCW [27], [29] (61.7%, 51.6% and 38.9%, respectively) performed in countries at an advanced stage (i.e., between 2 and 4 months) after the outbreak. Furthermore, these countries had relatively more developed healthcare systems. This result suggests that ARCAD Santé PLUS’s non-front-line HCW might be more vulnerable to deteriorating psychological outcomes as the current COVID-19 outbreak progresses and after it ends.
The present article demonstrates that MHD in HCW were related not only to individual characteristics, but also to HIV care center characteristics. Specifically, the risks of having these conditions were 51%, 62% and 43% lower, respectively, in people working in HIV care centers providing face masks than in people working elsewhere. A lack of masks was also the only structural factor linked to insomnia. Furthermore, depression and anxiety were 91% and 95%, respectively, less likely to occur in HCW in HIV care centers with a higher density of nurses.
Mental health in ARCAD Santé PLUS’s CHW in Mali seemed to be associated with uncertainty about COVID-19 at the beginning of the outbreak, as suggested by the relationship between the (un)availability of face masks and insomnia, depression, and anxiety. However, the risk of the latter two MHD seemed to be also related with preexisting contexts in HIV care centers, such as HR scarcity, especially nurses. The temporary reorganization of activities planned by ARCAD Santé PLUS as part of its purpose-built CovidPrev program – including fewer working hours, lower patient flow and a reduction of some services – should attenuate workers’ exposure to psychological disorders by reducing their workload [63]. However, it is vital to also include screening for psychological disorders and suitable treatment, as these same changes may themselves lead to psychological problems [64], [65], [66]. In addition, adequate PPE must be guaranteed for HCW, especially face masks, one of the most important tools in stopping the spread of COVID-19 [37].
The relationship discovered between the density of nurses in HIV care services and workers’ psychological outcomes not only highlights areas for improvement in the management of mental health among ARCAD Santé PLUS’s HCW during the current COVID-19 outbreak, but also provides insight into how these workers’ performance in HIV-related care could be improved in the short and long terms. Our results indicate that managers should investigate whether better reallocation of nursing resources is needed according to HIV caseload, whether more nurses need to be hired, and whether improvements in doctor-nurse task-shifting – an increasingly important care strategy, especially in SSA – is necessary, especially seeing as ARCAD Santé PLUS continues to expand its offer to include more non-HIV specific health-related services. Furthermore, including CHW as a full HCW category (albeit voluntary) in all organizational changes is crucial, both during and after the current COVID-19 outbreak, as these workers play an essential role in healthcare in SSA [67], [68], [69]. CHW account for a large proportion of ARCAD Santé PLUS’s staff (20% of respondents in the present article) and their activities are central to what makes this NGO attractive to people benefitting from its services. They are crucial in reaching key populations and promoting retention in HIV prevention and care programs. Their contribution to the introduction of pre-exposure prophylaxis (PrEP) for HIV among men having sex with men in Mali is just one example of this [70].
The role of CHW (not just in Mali) in connecting the most vulnerable people with healthcare systems during the current COVID-19 outbreak highlights the importance of strengthening CHW workforces long after this pandemic ends. This observation is not new to Africa, a continent where the work of CHW during the last decade in the field of HIV has led to successful testing of new task-shifting models and has strengthened the argument for the demedicalization of prevention and care [67], [68], [69], [71], [72], [73]. However, the success of any new healthcare service model which incorporates CHW as key actors, depends not only on financial sustainability, but also on the capability of the healthcare system to limit staff attrition and to protect them – and all HCW – from potential health problems, including MHD [7].
The abovementioned implications of the relationship between structural factors and HCW MHD are supported by our results for individual factors. Apart from nurses, all other worker categories – including CHW – were at greater risk of depression and insomnia (respectively, 60% and 49% more than nurses). These results confirm the importance of taking into account non-front-line HCW mental health in related analyses [39], [44]. The present work reflects the higher work-related psychological risk among women in healthcare-related professions observed in the literature [24], [63]. Despite their non-front-line status, this finding could be explained – at least partly – by both the importance which women in general seem to attach to psychosocial support [74], and occupational exposure related to HIV care delivery [75], [76], [77]. Furthermore, our results contribute to the existing literature by demonstrating that work-related factors are not the only source of MHD. Factors related to the day-to-day life of HCW were also strongly associated with the risk of depression. Indeed, depression was over twice as likely in participants with financially-dependent family members. Family responsibilities imply not only a supplementary workload, but also mental efforts that may lead to increased levels of depression [78].
The psychological distress related to medical decisions running counter to HCW morals and ethics is an important mental health dimension. In the present article, this distress was assessed using the Moral Injury Event Scale, as suggested by Greenberg et al., and Walton et al. [41], [44]. More specifically, our results showed that the risks of depression and anxiety were higher in workers who perceived work-related moral transgression, while the risk of insomnia was higher in those perceiving work-related betrayal. Given their non-front-line status in terms of COVID-19 care, and the fact that we assessed psychological outcomes during the early stage of the outbreak, this result would seem to be mostly explained by psychological distress linked to their HIV care-related activities. The complex context which these workers are confronted with may also result in their having to take decisions which run counter to their moral and ethical values. The lack of ARV delivery during stock-outs, the slowdown in international funding for the treatment of opportunistic infections, and external intimidation because of the services they offer (e.g., counseling for men who have sex with men), are three examples where such decisions might be made.
This present article has limitations. First, although the study sample was exhaustive – in that it included HCW in ARCAD Santé PLUS’s 18 healthcare services in Mali working in the early stage of the COVID-19 outbreak and reporting that they intended to continue to work throughout the outbreak – the sample size was nevertheless small. This meant that the relationship between certain structural factors and individual psychological outcomes could not be measured, as there was insufficient variability within some structures. However, the comparability of our results for individual factors with existing literature demonstrates that implementing suitable techniques – in our case GMM with an NB distribution – helped to overcome the limitations imposed by the small sample size.
Second, our sample was not representative of the population of Malian HCW. Despite the difficulties they face, the working conditions of ARCAD Santé PLUS’s non-front-line HCW are relatively less difficult than those of their counterparts in the general Malian health system. Considering that in Mali there is a greater-than-usual shortage of HR (0.036 medical professionals per 100 patients) with respect to ARCAD Santé PLUS HIV care centers (0.23 per 100 patients, which interestingly matches the minimum recommended by the WHO [79]), our results for non-front-line HCW most likely underestimate the current situation regarding mental health in the national healthcare system. Finally, the short questionnaire used prevented the collection of more detailed information about participants’ working and living conditions. However, the choice to use a short questionnaire was governed by necessity in order to limit desirability bias, and by a desire not to overburden respondents who were already having to adapt to constantly changing circumstances related to COVID-19.
Despite these limitations, the analyses conducted here provide evidence of non-negligible MHD affecting HCW in ARCAD Santé PLUS’s care network in the early stage of the COVID-19 outbreak. In light of this action research, results from the first analyses (carried out 1 week after data collection) prompted the NGO to add two new actions to its CovidPrev program: (i) the distribution of a large quantity of basic PPE, including face masks, gloves, and cleaning products; and (ii) the drafting and distribution of an information leaflet presenting the current mental health situation of its HCW, in order to promote self-help in this population through the program’s specifically developed fora, given governmental restrictions on movement. We aim to conduct further research to investigate whether and to what degree the COVID-19 outbreak aggravates MHD in this population. More broadly, the results of the present article provide evidence-based arguments that should be taken into account in Malian healthcare policy. Irrespective of the COVID-19 outbreak, conducting situational research is crucial to understand how and to what extent the physical and mental health of HCW is related to working and living conditions. Psychosocial support is a key element in the management of day-to-day work-related activities, and becomes indispensable during serious health shocks such as the current COVID-19 outbreak.
5. Conclusion
The long-established trustful relationship between ARCAD Santé PLUS and users of its HIV prevention and care services is a crucial factor in ensuring the dissemination of key COVID-19 messages in Mali. Indeed, the arrival of this new disease has underlined the huge importance of HCW – front-line and non-front-line – and has placed them at the core of health systems worldwide. However, the outbreak has also revealed weaknesses in integrating non-front-line HCW in the response to COVID-19, especially HCW in NGOs who perform crucial health-related activities. These people should have been integrated early on after the outbreak, not only as important vectors for information dissemination and prevention, but also as a group whose health and well-being are at stake and need to be protected. One of the main lessons to be learned from previous outbreaks and which the current COVID-19 pandemic reminds us of, is that “not being on the front line” does not mean “not needing support to reinforce the front line”. The effectiveness of the international response to pandemic outbreaks, and in general the effectiveness of public health strategies at national and local levels, depend on the capacity of HCW to fully and competently perform their duties within the healthcare system.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We wish to thank all the managers and healthcare workers in ARCAD Santé PLUS’s 18 community-based HIV centers throughout Mali for their involvement in this study. Our thanks also to Jude Sweeney (Milan, Italy) for the English revision and editing of this manuscript.
Appendix 1. UNICEF’s “fact or fiction” quiz for coronavirus awareness. (https://www.unicef.org/fr/coronavirus/faits-ou-fiction-quiz-sur-la-maladie-a-coronavirus-covid-19)
Quiz title:
“Fact or fiction: how much do you know about the coronavirus disease (COVID-19)?” (correct responses are in bold)
-
(1)How is the coronavirus disease (COVID-19) transmitted?
-
a.Respiratory droplets through coughing and sneezing
-
b.Touching surfaces contaminated with the virus and then touching your face
-
c.Both
-
a.
-
(2)Can I catch the coronavirus disease (COVID-19) from my pet?
-
a.Yes
-
b.No
-
a.
-
(3)What are the best ways to protect yourself from catching the coronavirus disease (COVID-19)?
-
a.Wash hands frequently using soap and water or an alcohol-based rub
-
b.Avoid close contact with anyone who has cold or flu-like symptoms
-
c.Avoid touching your face
-
d.All of them
-
a.
-
(4)Who does the coronavirus (COVID-19) affect?
-
a.Older people
-
b.Younger people
-
c.Everyone
-
a.
-
(5)What percentage alcohol in hand rubs and disinfectants is needed to kill de coronavirus disease (COVID-19)?
-
a.40%
-
b.50%
-
c.60%
-
a.
-
(6)Is there a vaccine or a specific medicine to prevent or treat the coronavirus disease (COVID-19)?
-
a.Yes
-
b.No
-
a.
-
(7)For how long should you wash your hands to kill the coronavirus disease (COVID-19)?
-
a.5 s
-
b.15 s
-
c.20 s
-
a.
-
(8)Is the coronavirus disease (COVID-19) the same as the flu?
-
a.Yes
-
b.No
-
a.
-
(9)Can the coronavirus disease (COVID-19) be transmitted in both hot and cold temperatures?
-
a.Yes
-
b.No
-
a.
-
(10)Can letters, products and packages be contaminated by the coronavirus (COVID-19) virus?
-
a.Yes
-
b.No
-
a.
Appendix 2. Strategy for the estimation of the individual and structural factors associated with depression, anxiety and insomnia
Estimations were carried out with the outcomes specified as continuous dependent variables to avoid any loss of information that might result from their dichotomization, that is to say, underestimation of the variability, and reduced power to estimate outcomes’ relationships with explanatory variables [80], [81]. However, this choice was methodologically challenging as it required us to implement a model adapted to non-negative dependent variables with skewed distributions and often overdispersed and zero-inflated. Given this context, the most suitable method to estimate the associated factors to the outcomes in this article was the general mixture model (GMM) with a negative binomial (NB) distribution [82], [83]. This was preferred to the Poisson-type distribution, as indicated by log-likelihood ratio test (LR-test), which rejected the null hypothesis where overdispersion is absent. GMM models have often been shown to be better adapted to non-count data, and a better alternative to Tobit and two-part models [83]. The restricted (residual) maximum likelihood estimation method was implemented in order to manage estimations with small samples [84], [85]. For each outcome the estimation strategy consisted in:
-
(1)
Verifying the pertinence of using a multilevel model. A 2-level null model with random intercepts was estimated and compared with a 1-level null model using the LR-test. This comparison allowed us to verify whether there was any outcome variability arising from differences between HIV care centers. The intra-class correlation coefficient (ICC) – adapted to the GMM – was estimated to assess the amount of outcome variability arising from structural differences [86], [87], [88].
-
(2)
Conducting bivariate analyses and construction of the final multivariable model. Single estimations were performed for each explanatory variable at the individual level. Each estimation was compared with the null model using the LR-test in order to assess the contribution of the corresponding explanatory variable. Eligibility of individual-level variables for inclusion in the multivariable model was based on the following criteria: p-value <0.2 and/or LR-test p-value <0.1 (i.e. significant contribution to the model fitting). The step-wise forward selection procedure was implemented and the final multivariable model for individual characteristics chosen on the basis of the AIC criterion. This best-fit model for individual factors was used to conduct a bivariate analysis for the structural factors (i.e., HIV care center structural characteristics). More specifically, the same tests and criteria as those for individual factors were used for these structural variables to be eligible for the 2-level part of the multivariable model, and also in order to construct the final model. Estimated incidence rate ratios (IRR), 95% confidence intervals and p-values are presented in the results section.
-
(3)
Verifying the need to use a zero-inflated model. The final multivariable models (estimated using negative binomial distribution) were re-estimated using zero-inflated negative binomial distribution (ZINB). These models were compared using the LR-test in order to verify whether using ZINB was necessary or not [89].
References
- 1.Coronavirus (COVID-19). WHO | Regional Office for Africa; n.d. https://www.afro.who.int/health-topics/coronavirus-covid-19 (accessed April 5, 2020).
- 2.Sagaon-Teyssier L., Yattassaye A., Bourrelly M., Dembélé Keïta B., Spire B. The COVID-19 response must integrate people living with HIV needs in Sub-Saharan Africa: the case of Mali. Trop Med Health. 2020;48:41. doi: 10.1186/s41182-020-00228-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jaja I.F., Anyanwu M.U., Iwu Jaja C.-J. Social distancing: how religion, culture and burial ceremony undermine the effort to curb COVID-19 in South Africa. Emerging Microbes Infect. 2020;9:1077–1079. doi: 10.1080/22221751.2020.1769501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fenichel E.P. Economic considerations for social distancing and behavioral based policies during an epidemic. J Health Econ. 2013;32:440–451. doi: 10.1016/j.jhealeco.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore M., Gelfeld B., Okunogbe A., Paul C. RAND Corporation; 2016. Identifying future disease hot spots: Infectious disease vulnerability index. https://doi.org/10.7249/RR1605. [PMC free article] [PubMed] [Google Scholar]
- 6.Stekelenburg J., Kyanamina S.S., Wolffers I. Poor performance of community health workers in Kalabo District, Zambia. Health Policy. 2003;65:109–118. doi: 10.1016/S0168-8510(02)00207-5. [DOI] [PubMed] [Google Scholar]
- 7.Olang’o C.O., Nyamongo I.K., Aagaard-Hansen J. Staff attrition among community health workers in home-based care programmes for people living with HIV and AIDS in western Kenya. Health Policy. 2010;97:232–237. doi: 10.1016/j.healthpol.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Barber S.L., Gertler P.J. Health workers, quality of care, and child health: Simulating the relationships between increases in health staffing and child length. Health Policy. 2009;91:148–155. doi: 10.1016/j.healthpol.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrier-Walker L. Focussing on the wellbeing of health care workers in sub-Saharan Africa. Int Nurs Rev. 2011;58:273–274. doi: 10.1111/j.1466-7657.2011.00933.x. [DOI] [PubMed] [Google Scholar]
- 10.Mæstad O., Torsvik G., Aakvik A. Overworked? On the relationship between workload and health worker performance. J Health Econ. 2010;29:686–698. doi: 10.1016/j.jhealeco.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Rajbhandary S., Basu K. Working conditions of nurses and absenteeism: Is there a relationship? An empirical analysis using National Survey of the Work and Health of Nurses. Health Policy. 2010;97:152–159. doi: 10.1016/j.healthpol.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Siukola A.E., Virtanen P.J., Luukkaala T.H., Nygård C.-H. Perceived working conditions and sickness absence – a four-year follow-up in the food industry. Saf Health Work. 2011;2:313–320. doi: 10.5491/SHAW.2011.2.4.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plan d’Actions pour la Prévention et la Réponse à la Maladie à COVID-19 (COVID-19). Mali: Ministère de la Santé et des Affaires Sociales; 2020.
- 14.Williamson V., Stevelink S.A.M., Greenberg N. Occupational moral injury and mental health: systematic review and meta-analysis. Br J Psychiatry. 2018;212:339–346. doi: 10.1192/bjp.2018.55. [DOI] [PubMed] [Google Scholar]
- 15.Mai Q.D., Jacobs A.W., Schieman S. Precarious sleep? Nonstandard work, gender, and sleep disturbance in 31 European countries. Soc Sci Med. 2019;237:112424. doi: 10.1016/j.socscimed.2019.112424. [DOI] [PubMed] [Google Scholar]
- 16.Paintsil E. COVID-19 threatens health systems in sub-Saharan Africa: the eye of the crocodile; 2020. 10.1172/JCI138493. [DOI] [PMC free article] [PubMed]
- 17.WHO | Mali. WHO; n.d. http://www.who.int/health-cluster/countries/mali/en/ (accessed September 23, 2020).
- 18.Maunder R.G. Was SARS a mental health catastrophe? Gen Hosp Psychiatry. 2009;31:316–317. doi: 10.1016/j.genhosppsych.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lancee W.J., Maunder R.G., Goldbloom D.S. Prevalence of psychiatric disorders among toronto hospital workers one to two years after the SARS outbreak. PS. 2008;59:91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W., Sham P.C., et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. 2007;52:241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 21.Shah K., Kamrai D., Mekala H., Mann B., Desai K., Patel R.S. Focus on mental health during the coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks. Cureus. 2020 doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bohlken J., Schömig F., Lemke M.R., Pumberger M., Riedel-Heller S.G. COVID-19-Pandemie: Belastungen des medizinischen Personals: Ein kurzer aktueller Review. Psychiat Prax. 2020;47:190–197. doi: 10.1055/a-1159-5551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.García-Fernández L., Romero-Ferreiro V., López-Roldán P.D., Padilla S., Calero-Sierra I., Monzó-García M., et al. Mental health impact of COVID-19 pandemic on Spanish healthcare workers. Psychol Med. 2020:1–3. doi: 10.1017/S0033291720002019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choudhury T., Debski M., Wiper A., Abdelrahman A., Chalil S., More R., et al. Covid-19 pandemic: Looking after the mental health of our healthcare workers. J Occup Environ Med. 2020 doi: 10.1097/JOM.0000000000001907. [Publish Ahead of Print] [DOI] [PubMed] [Google Scholar]
- 25.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. S088915912030845X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elbay R.Y., Kurtulmuş A., Arpacıoğlu S., Karadere E. Depression, anxiety, stress levels of physicians and associated factors in Covid-19 pandemics. Psychiatry Res. 2020;290:113130. doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang W., Wang K., Yin L., Zhao W., Xue Q., Peng M., et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020:1–9. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Spoorthy M.S., Pratapa S.K., Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J Psychiatry. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Albott C.S., Wozniak J.R., McGlinch B.P., Wall M.H., Gold B.S., Vinogradov S. Battle Buddies: Rapid deployment of a psychological resilience intervention for healthcare workers during the COVID-19 pandemic. Anesthesia Analgesia. 2020 doi: 10.1213/ANE.0000000000004912. [Publish Ahead of Print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barello S., Palamenghi L., Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kinman G., Teoh K., Harriss A. Supporting the well-being of healthcare workers during and after COVID-19. Occup Med. 2020:kqaa096. doi: 10.1093/occmed/kqaa096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gold J.A. Covid-19: adverse mental health outcomes for healthcare workers. BMJ. 2020:m1815. doi: 10.1136/bmj.m1815. [DOI] [PubMed] [Google Scholar]
- 36.Singh M., Sharda S., Gautam M., Hawa R. Optimal sleep health among frontline healthcare workers during the COVID-19 pandemic. Can J Anesth/J Can Anesth. 2020 doi: 10.1007/s12630-020-01716-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chirico F., Nucera G., Magnavita N. COVID-19: Protecting healthcare workers is a priority. Infect Control Hosp Epidemiol. 2020 doi: 10.1017/ice.2020.148. 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blake H., Bermingham F., Johnson G., Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: A digital learning package. Int J Environ Res Public Health. 2020;17:2997. doi: 10.3390/ijerph17092997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.049. S0889159120305237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Godderis L., Boone A., Bakusic J. COVID-19: a new work-related disease threatening healthcare workers. Occup Med. 2020:kqaa056. doi: 10.1093/occmed/kqaa056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 42.Iannone P., Castellini G., Coclite D., Napoletano A., Fauci A.J., Iacorossi L., et al. The need of health policy perspective to protect Healthcare Workers during COVID-19 pandemic. A GRADE rapid review on the N95 respirators effectiveness. PLoS ONE. 2020;15:e0234025. doi: 10.1371/journal.pone.0234025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang L., Yin J., Wang D., Rahman A., Li X. Urgent need to develop evidence-based self-help interventions for mental health of healthcare workers in COVID-19 pandemic. Psychol Med. 2020:1–2. doi: 10.1017/S0033291720001385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walton M., Murray E., Christian M.D. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J: Acute Cardiovasc Care. 2020;9:241–247. doi: 10.1177/2048872620922795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nuwagira E., Muzoora C. Is Sub-Saharan Africa prepared for COVID-19? Trop Med Health. 2020;48:18. doi: 10.1186/s41182-020-00206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gilbert M., Pullano G., Pinotti F., Valdano E., Poletto C., Boëlle P.-Y., et al. Preparedness and vulnerability of African countries against importations of COVID-19: a modelling study. The Lancet. 2020;395:871–877. doi: 10.1016/S0140-6736(20)30411-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kapata N., Ihekweazu C., Ntoumi F., Raji T., Chanda-Kapata P., Mwaba P., et al. Is Africa prepared for tackling the COVID-19 (SARS-CoV-2) epidemic. Lessons from past outbreaks, ongoing pan-African public health efforts, and implications for the future. Int J Infect Dis. 2020;93:233–236. doi: 10.1016/j.ijid.2020.02.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Agyeman AA, Laar A, Ofori‐Asenso R. Will COVID-19 be a litmus test for post-Ebola sub-Saharan Africa? Journal of Medical Virology n.d.; n/a. 10.1002/jmv.25780. [DOI] [PMC free article] [PubMed]
- 49.Wang J., Xu C., Wong Y.K., He Y., Adegnika A.A., Kremsner P.G., et al. Preparedness is essential for malaria-endemic regions during the COVID-19 pandemic. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Algarin A.B., Varas-Rodríguez E., Valdivia C., Fennie K.P., Larkey L., Hu N., et al. Symptoms, stress, and HIV-related care among older people living with HIV during the COVID-19 Pandemic, Miami, Florida. AIDS Behav. 2020 doi: 10.1007/s10461-020-02869-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chersich M.F., Gray G., Fairlie L., Eichbaum Q., Mayhew S., Allwood B., et al. COVID-19 in Africa: care and protection for frontline healthcare workers. Global Health. 2020;16:46. doi: 10.1186/s12992-020-00574-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.PSN 2026-2020.pdf; n.d. https://www.unicef.org/mali/media/2291/file/PSN%202026-2020.pdf [accessed September 21, 2020].
- 53.mli147674.pdf; n.d. http://extwprlegs1.fao.org/docs/pdf/mli147674.pdf [accessed September 21, 2020].
- 54.Mali | ONUSIDA; n.d. https://www.unaids.org/fr/regionscountries/countries/mali [accessed May 25, 2020].
- 55.Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 57.Morin C.M., Belleville G., Bélanger L., Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Arthurs E., Steele R.J., Hudson M., Baron M., Thombs B.D., Canadian Scleroderma Research Group (CSRG) Are scores on English and French versions of the PHQ-9 comparable? An assessment of differential item functioning. PLoS ONE. 2012;7:e52028. doi: 10.1371/journal.pone.0052028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Micoulaud-Franchi J.-A., Lagarde S., Barkate G., Dufournet B., Besancon C., Trébuchon-Da Fonseca A., et al. Rapid detection of generalized anxiety disorder and major depression in epilepsy: Validation of the GAD-7 as a complementary tool to the NDDI-E in a French sample. Epilepsy Behav. 2016;57:211–216. doi: 10.1016/j.yebeh.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 60.Chahoud M., Chahine R., Salameh P., Sauleau E.A. Reliability, factor analysis and internal consistency calculation of the Insomnia Severity Index (ISI) in French and in English among Lebanese adolescents. ENeurologicalSci. 2017;7:9–14. doi: 10.1016/j.ensci.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nash W.P., Marino Carper T.L., Mills M.A., Au T., Goldsmith A., Litz B.T. Psychometric evaluation of the moral injury events scale. Mil Med. 2013;178:646–652. doi: 10.7205/MILMED-D-13-00017. [DOI] [PubMed] [Google Scholar]
- 62.R Core Team. R: A language and environment for statistical computing. Vienna (Austria): R Foundation for Statistical Computing; 2020. https://www.R-project.org/.
- 63.Győrffy Z., Dweik D., Girasek E. Workload, mental health and burnout indicators among female physicians. Hum Resour Health. 2016;14:12. doi: 10.1186/s12960-016-0108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cesur R., Sabia J.J., Tekin E. The psychological costs of war: Military combat and mental health. J Health Econ. 2013;32:51–65. doi: 10.1016/j.jhealeco.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 65.Wagner S., Koehn C., White M., Harder H., Schultz I., Williams-Whitt K., et al. Mental health interventions in the workplace and work outcomes: a best-evidence synthesis of systematic reviews. Int J Occup Environ Med. 2016;7:1–14. doi: 10.15171/ijoem.2016.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Van Der Laan G. Tracing new occupational diseases, an introduction. Saf Health Work. 2012;3:50–51. doi: 10.5491/SHAW.2012.3.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fatti G., Monteith L., Shaikh N., Kapp E., Foster N., Grimwood A. Implementation and operational research: A comparison of two task-shifting models of pharmaceutical care in antiretroviral treatment programs in South Africa. J Acquir Immune Defic Syndr. 2016;71:e107–e113. doi: 10.1097/QAI.0000000000000912. [DOI] [PubMed] [Google Scholar]
- 68.Naburi H., Ekström A.M., Mujinja P., Kilewo C., Manji K., Biberfeld G., et al. The potential of task-shifting in scaling up services for prevention of mother-to-child transmission of HIV: a time and motion study in Dar es Salaam, Tanzania. Hum Resour Health. 2017;15 doi: 10.1186/s12960-017-0207-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Geldsetzer P., Francis J.M., Ulenga N., Sando D., Lema I.A., Mboggo E., et al. The impact of community health worker-led home delivery of antiretroviral therapy on virological suppression: a non-inferiority cluster-randomized health systems trial in Dar es Salaam, Tanzania. BMC Health Serv Res. 2017;17 doi: 10.1186/s12913-017-2032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Eubanks A., Dembélé Keita B., Anoma C., Dah E., Mensah E., Maradan G., et al. Reaching a different population of MSM in West Africa with the integration of PrEP into a comprehensive prevention package. (CohMSM-PrEP ANRS 12369 – Expertise France) JAIDS J Acquired Immune Deficiency Syndrom. 2020 doi: 10.1097/QAI.0000000000002453. [Publish Ahead of Print] [DOI] [PubMed] [Google Scholar]
- 71.Okuga M., Kemigisa M., Namutamba S., Namazzi G., Waiswa P. Engaging community health workers in maternal and newborn care in eastern Uganda. Global Health Action. 2015;8 doi: 10.3402/gha.v8.23968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pellecchia U., Baert S., Nundwe S., Bwanali A., Zamadenga B., Metcalf C.A., et al. “We are part of a family”. Benefits and limitations of community ART groups (CAGs) in Thyolo, Malawi: a qualitative study. J Int AIDS Soc. 2017;20 doi: 10.7448/IAS.20.1.21374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ellman T. Demedicalizing AIDS prevention and treatment in Africa. Https://Doi-OrgProxyInsermbiblioInistFr/101056/NEJMp1414730 2015. 10.1056/NEJMp1414730. [DOI] [PubMed]
- 74.Felice C., Di Tanna G.L., Zanus G., Grossi U. Impact of COVID-19 outbreak on healthcare workers in Italy: Results from a National E-Survey. J Community Health. 2020 doi: 10.1007/s10900-020-00845-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mossburg S., Agore A., Nkimbeng M., Commodore-Mensah Y. Occupational hazards among healthcare workers in Africa: A systematic review. Ann Global Health. 2019;85:78. doi: 10.5334/aogh.2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Akpuh N., Ajayi I., Adebowale A., Idris Suleiman H., Nguku P., Dalhat M., et al. Occupational exposure to HIV among healthcare workers in PMTCT sites in Port Harcourt, Nigeria. BMC Public Health. 2020;20:451. doi: 10.1186/s12889-020-08528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kabotho K.T., Chivese T. Occupational exposure to HIV among nurses at a major tertiary hospital: Reporting and utilization of post-exposure prophylaxis; A cross-sectional study in the Western Cape, South Africa. PLoS ONE. 2020;15:e0230075. doi: 10.1371/journal.pone.0230075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Juratovac E., Zauszniewski J.A. Full-time employed and a family caregiver: A profile of women’s workload, effort, and health. Women’s Health Issues. 2014;24:e187–e196. doi: 10.1016/j.whi.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 79.Nursing and midwifery personnel (per 10 000 population); n.d. https://www.who.int/data/maternal-newborn-child-adolescent/monitor [accessed June 27, 2020].
- 80.Altman D.G., Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332:332. doi: 10.1136/bmj.332.7549.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Royston P., Altman D.G., Sauerbrei W. Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med. 2006;25:127–141. doi: 10.1002/sim.2331. [DOI] [PubMed] [Google Scholar]
- 82.Santos Silva J.M.C., Tenreyro S. The log of gravity. Rev Econ Stat. 2006;4:641–658. [Google Scholar]
- 83.Motta V. Estimating Poisson pseudo-maximum-likelihood rather than log-linear model of a log-transformed dependent variable. RAUSP. 2019;54:508–518. doi: 10.1108/RAUSP-05-2019-0110. [DOI] [Google Scholar]
- 84.McNeish D. Small sample methods for multilevel modeling: a colloquial elucidation of REML and the Kenward-Roger correction. Multivariate Behav Res. 2017;52:661–670. doi: 10.1080/00273171.2017.1344538. [DOI] [PubMed] [Google Scholar]
- 85.Bolker B. Getting started with the glmmTMB package. n.d.:10.
- 86.Nakagawa S, Johnson PCD, Schielzeth H. The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. n.d.:11. [DOI] [PMC free article] [PubMed]
- 87.Tseloni A. Repeat personal victimization: random effects, event dependence and unexplained heterogeneity. Br J Criminol. 2004;44:931–945. doi: 10.1093/bjc/azh047. [DOI] [Google Scholar]
- 88.Aly S.S., Zhao J., Li B., Jiang J. Reliability of environmental sampling culture results using the negative binomial intraclass correlation coefficient. SpringerPlus. 2014;3:40. doi: 10.1186/2193-1801-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Allison P.D. 2nd ed. SAS Pub; Cary (N.C): 2012. Logistic regression using SAS: theory and application. [Google Scholar]