Abstract
The SARS-CoV-2 pandemic has revealed that Africa needs a new public health order to be resilient, to adapt, and to cope with 21st-century disease threats. The new order will need strengthened continental and national public health institutions; local manufacturing of vaccines, therapeutics, and diagnostics; attraction, training, and retention of a public health workforce; and fostering of respectful local and international partnerships.
The SARS-CoV-2 pandemic has revealed that Africa needs a new public health order to be resilient, adapt, and cope with 21st-century disease threats. The new order will need strengthened continental and national public health institutions; local manufacturing of vaccines, therapeutics, and diagnostics; attraction, training, and retention of a public health workforce; and fostering of respectful local and international partnerships.
Main Text
Infectious diseases remain a great threat to Africa’s aspiration to achieve its 2063 developmental blueprint: “Agenda 2063: The Africa We Want.” Health, as a development issue, continues to have a significant impact on the economic and social security of countries and regions across Africa. Africa’s underlying burden of endemic diseases is the largest in the world. Infectious diseases play a particularly severe role on the continent. Every year they account for over 227 million years of health life lost and produce an annual productivity loss of over $800 billion (World Health Organization Regional Office for Africa, 2019). Moreover, outbreak-prone diseases are an increasingly devastating force. Of the estimated 10 million deaths per year resulting from infectious diseases, the majority occur in Africa.
The SARS-CoV-2 pandemic has clearly shown how infectious diseases are a serious threat to health, global economies, and security. Economically, the SARS-CoV-2 pandemic is forecast to cause a 5.2% contraction in global gross domestic product and to a 2.8% contraction in Sub-Saharan Africa in 2020 (World Bank, 2020). The SARS-CoV-2 pandemic has underlined the datum that disease does not respect boundaries. While we seek to flatten the epidemiological curve of SARS-CoV-2 globally, the virus has also “flattened the world.” It has shown us that we are more connected than we thought, that we are vulnerable regardless of where we live, and that we have tremendous shared responsibilities and vast inequalities.
In the midst of this, Africa has learned how fragile international cooperation can be when the world is collectively threatened and challenged by a common disease threat. For instance, the ease with which Africa was shoved out of the SARS-CoV-2 diagnostics market exposed how easily global cooperation and international solidarity can collapse (Nkengasong, 2020). Similarly, Africa could find itself at the end of the queue for access to any available vaccines against SARS-CoV-2 with the rise of global protectionism and vaccine nationalism (Callaway, 2020).
One of the greatest lessons learned by Africa is the urgent need to invest in its healthcare systems as a critical instrument to secure its economic development as it implements the African Continental Free Trade Area Agreement and other flagship projects of Agenda 2063. About 50 years ago, Julian Tudor-Hart proposed the principle of the inverse care law, stating that the availability of good medical or social care tends to vary inversely with the need of the population served (Hart, 1971). This principle vastly prevails in Africa today, and a new public health order must aim to deconstruct this law. Here, we provide a historical perspective of where Africa is coming from and where it might be heading to understand why we need a new public health order to fight the inverse care law. We propose that the new public health order must stand on four pillars: strengthened public health institutions; local manufacturing of vaccines, therapeutics, and diagnostics; a strengthened public health workforce; and respectful local and international partnerships.
Emerging Infectious Disease Patterns in Africa from Independence in the 1960s
Africa finds itself balancing its developmental aspirations with strengthening its health systems to help it fight synergistic concurrent epidemics (i.e., the “syndemic”). It is faced with a set of linked health problems that interact synergistically, contributing to its excess burden of disease: rising rates of non-communicable diseases, emerging and re-emerging infections, and endemic diseases. The syndemic is a result of five major factors: (1) the rapid population growth of the continent, resulting in rapid population movement across the continent (the estimated population of Africa was 280 million in 1960 and 1.2 billion in 2016 and is projected to be 2.4 billion by 2050; United Nations ECA, 2016) (Although Africa is still significantly rural, the continent is projected to be the world’s fastest-urbanizing population.); (2) widespread infectious disease, including endemic diseases such as HIV, TB, and malaria, which together account for more than 1.2 million deaths per year on the continent; emerging infectious pathogens; and the rising prevalence of antimicrobial resistance (AMR), which will cause an estimated 4 million deaths by 2050 (O’Neill, 2014); (3) increasing incidence of non-communicable diseases and injuries (Gouda et al., 2019); (4) persistently high maternal mortality rates; and (5) threats posed by environmental, climatic, and ecological changes.
As a result of this balancing act, over 30 novel infectious diseases have emerged over the last three decades. When most African countries gained independence in the 1960s, several of the major infectious diseases that threaten the society, economy, and security of the continent were unknown or were thought to have been brought under control. However, as the human population continues to expand, there is increased use of agricultural land, which increases the exposure of livestock and humans to infections in wildlife. Once these new infections enter the population, air traffic facilitates their rapid spread across the world. Climate change is also increasingly modifying the ecosystem and concentration of animal vectors, thereby introducing diseases to new geographic locations. However, these factors are just part of the story. Ultimately, the reasons for the rapid emergence of so many novel infectious diseases are multifactorial and also include microbial adaptation, poverty and social inequality, instability, and fragile health systems.
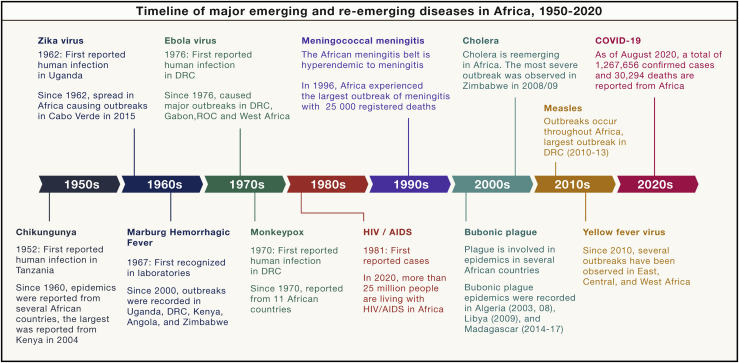
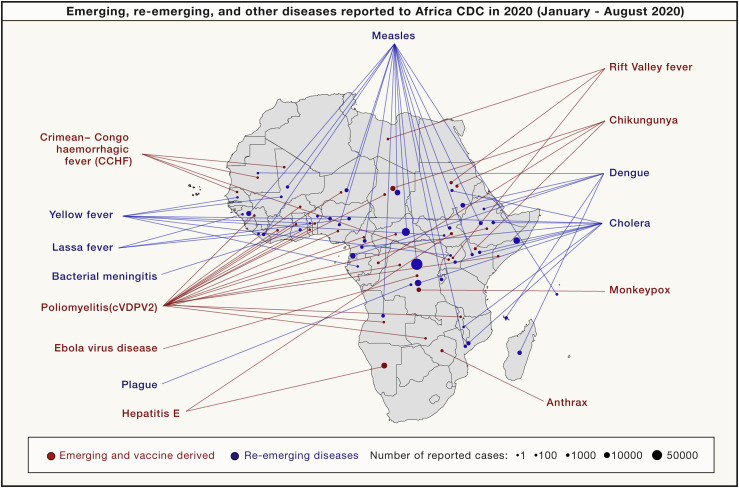
To emphasize the broad and enduring impact of infectious disease in Africa, we constructed a timeline of how some of the notable infectious diseases, with pandemic potential, have emerged and re-emerged in Africa since independence (Figure 1 ). These, together with emerging, re-emerging, and other diseases in Africa in 2020 (Figure 2 ), represent a wake-up call for the continent. Some of the infections are emerging and re-emerging more frequently.
Figure 1.
Timeline of Emerging and Re-emerging Infectious Diseases in Africa from 1950 to 2020
Figure 2.
A Map of Emerging, Re-emerging, and Other Diseases Reported to the Africa Centres for Disease Control and Prevention (Africa CDC) in 2020
The size of the circles corresponds to the number of reported cases compiled as of August 28, 2020.
Need for a New Public Health Order
Given the above, in order to secure its future and guarantee its development, Africa will need a new public health order to address infectious disease threats and the overall syndemic in the 21st century. This new order will necessitate (1) a strengthened Africa Centres for Disease Control and Prevention (Africa CDC) and national public health institutions (NPHIs); (2) local production of vaccines, therapeutics, and diagnostics; (3) investment in public health workforce and leadership programs; and (4) respectful partnerships.
A Strengthened Africa CDC and NPHIs
The Africa CDC must play a central role in the new public health order. To better understand the critical role that a well-resourced and enabled Africa CDC could potentially play in such a new public health order, it is important to look back on how some of the oldest public health institutions were established in response to challenges posed by disease threats of their time and have since transformed public health practice in those countries. The oldest public health institution in the world is the Brazilian Oswaldo Cruz Institute, founded in 1900 under the name “Instituto Soroterápico Federal” (Federal Serotherapic Institute). It was established as an immediate response to address several public health challenges, including the bubonic plague, yellow fever, and smallpox, which were Brazil’s greatest threats at the time. These diseases were decimating the population, hindering the economic and social development of the country. Foreign ships, the only international mechanism of transport at that time, were not allowed to anchor in Brazilian ports because of the potential risk of exporting these diseases—a situation similar to that of today, where air and sea transportation halted across the globe due to the SARS-CoV-2 pandemic. Today the institution has a remarkably broad range of public health responsibilities, including hospital and ambulatory care; health-related research; development and production of vaccines, drugs, reagents, and diagnostic kits; training of public health and health workers; and providing information and communications related to health, science, and technology. Another example is the United States Centers for Disease Control and Prevention (US CDC) that was founded in 1946 as the Communicable Disease Center in Atlanta, Georgia. Its work was initially focused on malaria control. It subsequently expanded its mandate to include all communicable diseases and supported all the States. In 1949 it launched the first-ever disease surveillance program. Subsequently, disease surveillance became the cornerstone of the CDC’s mission and, in time, changed the practice of public health. Strikingly, the start of the Korean War in 1950 was the stimulus for designing the CDC’s Epidemic Intelligence Service (EIS). The threat of biological warfare loomed, creating a need to train epidemiologists who would detect ordinary threats to public health while looking out for unfamiliar pathogens. This “disease detectives” program quickly became famous for “shoe-leather epidemiology,” through which they hunted out the cause of disease outbreaks. Other public health agencies have emerged fairly recently due to several disease challenges, including the China CDC in 2002, the Public Health Agency of Canada in 2003, and the European CDC in 2003, which were established as a consequence of the 2002 outbreak of Severe Acute Respiratory Syndrome (SARS).
The political leadership of Africa must learn lessons from these experienced institutions on how to support and resource the Africa CDC so that it can play a central role in the new public health order, safeguarding the health security and economic development of the continent (Nkengasong et al., 2017). African heads of state and governments established the Africa CDC following the largest Ebola virus disease (EVD) outbreak in West Africa, which resulted in over 28,000 infections and 11,300 deaths. The mission of the Africa CDC is to strengthen the capacity and capability of Africa’s public health institutions to detect and respond quickly and effectively to disease threats and outbreaks based on science, policy, and data-driven interventions and programs. In order to enable an effective response to disease threats, all five Africa CDC Regional Collaborating Centres (RCCs) should house a Regional Integrated Surveillance and Laboratory Network (Africa CDC RISLNET). The Africa CDC RISLNET is expected to leverage all existing public health assets in each region. The Africa CDC should then facilitate the establishment and/or strengthening of NPHIs in each African country, which will network with the RCCs. Functional NPHIs will then conduct core public health functions: surveillance, laboratory networking, innovative information management, workforce development, management of an emergency operation center, and conducting high-priority public health research.
Strong continental public health institutions are critical to harmonize and coordinate public health responses across sectors, disciplines, and borders. Below are some examples of how the Africa CDC has supported over 10 member states to respond to nearly 15 disease outbreaks over 4 years. Perhaps the greatest challenge the nascent organization has faced was the EVD outbreaks in North Kivu, Democratic Republic of the Congo. Africa CDC supported the government of the DRC in several key areas: by deploying over 65 epidemiologists, laboratory experts, logisticians, infection control experts, and risk communicators; conducting 170,500 contact tracings and/or supervisions; establishing 11 laboratories across the affected areas and testing over 35,000 samples; training about 3,100 health care workers, traditional rulers, and points of entry; and providing personal protective equipment to 14 health districts. Furthermore, in 2019, the Africa CDC convened a meeting of health ministers of the DRC and its nine neighboring countries to develop a cross-border collaboration framework on Ebola preparedness and response and other health security risks. In the current COVID-19 pandemic, Africa CDC mobilized a continent-wide response and held an emergency meeting of African health ministers that led to the adoption and approval of the Africa Joint Continental Strategy for COVID-19 (Massinga Loembé et al., 2020). Since then, the Africa CDC has trained more than 1,000 laboratory personnel and 9,000 public health and medical professionals on surveillance, infection prevention and control (IPC), risk communication, and case management. Africa CDC has distributed more than 5 million tests and provided over 10 million pieces of medical equipment across Africa, including personal protective equipment. Furthermore, Africa CDC deployed rapid responders (205) and community health workers (more than 10,000) to support COVID-19 testing and contact tracing across 22 member states.
Local Production of Vaccines, Therapeutic, and Diagnostics
Local production of vaccines, medicines, and diagnostics is critical to safeguard Africa’s health security. Despite the threats posed by infectious diseases in Africa, as outlined above, it is remarkable that the continent only produces 1% of its vaccines and lacks the adequate capacity to manufacture them at scale. Vaccines are essential to reduce mortality, improve life expectancy, and promote economic growth. The Global Alliance for Vaccines Immunization (GAVI) has been instrumental in introducing new vaccines in Africa. However, introducing new vaccines after countries graduate from eligibility for the GAVI program will be a challenge for the continent. The rapid population and economic growth in Africa make it a very attractive market for vaccine manufacturing. Therefore, African governments must invest in addressing barriers to local vaccine production, including process development and maintenance, production facilities, life cycle management, and product portfolio management. In addition, efforts like the African Vaccine Manufacturers Initiative must be promoted and encouraged. The geopolitics surrounding access to vaccines in the present SARS-CoV-2 pandemic further highlight the need for Africa to embark on local vaccine manufacturing to avoid depending on externalities for its health security.
Local production of medicines is equally critical. Africa imports between 70% and 90% of its drugs (Chaudhuri and West, 2015). This considerably exceeds the percentage of medicines imported into China (5%) and India (20%), despite comparable populations (McKinsey, 2019). Local pharmaceutical manufacturing is vital for Africa’s development; effective drugs against HIV infections became available in 1996 in developed countries and led to drastic decrease in mortalities from AIDS. However, these drugs only became accessible in Africa in 2002. As a result of the delay, millions of Africans died needlessly. The African Union’s initiative to establish the Africa Medicine Agency (AMA) must be fully supported as part of the new public health order. The goals of AMA are to (1) coordinate ongoing regulatory systems for drugs; (2) strengthen and harmonize drug-manufacturing efforts across the continent; (3) provide regulatory guidance; and (4) improve patients’ access to quality, safe, and efficacious medical products and health technologies on the continent. Africa’s high disease burden constitutes a great incentive and a significant market for the pharmaceutical industry. In 2017, the World Health Organization estimates that the annual earnings from substandard and/or counterfeit drugs were over US$30 billion (World Health Organization, 2017). Lastly, Africa needs to invest in the local production of diagnostics, especially for newly emerging pathogens. The present COVID-19 pandemic has revealed the serious challenges for the continent to quickly access diagnostics in the wake of an emerging disease threat (Nkengasong, 2020). In fact, prior to COVID-19, no African countries were investing in the local manufacturing of diagnostics.
Public Health Workforce
Adequate investment to develop and maintain a prepared cadre of public health experts and leaders will be fundamental for the continent to cope with its disease threats. The Africa CDC needs to be enabled to run a competency-based workforce development program similar to the US CDC’s EIS program. Africa needs about 6,000 field epidemiologists at both advanced and intermediate levels. However, there are only an estimated 1,900 epidemiologist graduates from various field epidemiology training programs across the continent. The continent also needs an estimated 25,000 frontline epidemiologists but currently has only trained about 5,000. Moreover, in 2017, the heads of state and government of the continent launched an initiative to deploy 2 million community healthcare workers who can help to transform the interface between public health services and communities. This cadre of workers can truly be the nexus between universal health coverage and health security, as they can improve access and uptake of health services, sanitation and hygiene, and primary health care to the community and improve overall health outcomes.
Africa must also prioritize training for the next generation of global health leaders to embrace a multi-dimensional approach to solving health challenges. This will include arming the next generation to understand that public health agendas must be pushed politically and diplomatically. They must aim at propelling any public health causes into political circles, because protecting Africa’s public health requires the promotion of evidence-based estimates to predict resource needs before a disease threat occurs. Unfortunately, because of the major competing emergencies that the continent faces, the risks of future diseases do not appear imminent; thus, convincing policy makers to invest in disease preparedness may be a challenge. The Africa CDC recently launched the Kofi Annan Global Health Leadership and Scholar Program, which is aimed at providing emerging public health leaders with such skill sets (Africa Union, 2020).
Trusting Partnerships
A new public order will require that Africa develop effective and trusting partnerships with the private sector and establish a new mechanism to ensure that efforts by donors and development partners are better coordinated and aligned with continental aspirations—Agenda 2063—and that African-originated and -defined health priorities and solutions are respected. Such coordination is critical to ensure efficiencies and to minimize fragmentation and duplications of efforts and undermining of African-driven agendas. The COVID-19 pandemic has clearly demonstrated how interrelated disease threats are with economies. As Africa implements the Africa Continental Free Trade Agreement, close collaboration with the Africa CDC is essential to ensure that public health and disease threats are central to its operations. Lastly, committed partnerships across the continent will be required to establish an Africa Disease Threat Fund, similar to The Global Fund, to effectively implement the new public health order in Africa.
References
- Africa Union African Union Commission announces the Africa CDC Kofi Annan Global Health Leadership Programme. 2020. https://au.int/en/pressreleases/20200525/african-union-commission-announces-africa-cdc-kofi-annan-global-health
- Callaway E. The unequal scramble for coronavirus vaccines—by the numbers. Nature. 2020;584:506–507. doi: 10.1038/d41586-020-02450-x. [DOI] [PubMed] [Google Scholar]
- Chaudhuri S., West A. Can local producers compete with low-cost imports? A simulation study of pharmaceutical industry in low-income Africa. Innov. Dev. 2015;5:23–38. [Google Scholar]
- Gouda H.N., Charlson F., Sorsdahl K., Ahmadzada S., Ferrari A.J., Erskine H., Leung J., Santamauro D., Lund C., Aminde L.N. Burden of non-communicable diseases in sub-Saharan Africa, 1990-2017: results from the Global Burden of Disease Study 2017. Lancet Glob. Health. 2019;7:e1375–e1387. doi: 10.1016/S2214-109X(19)30374-2. [DOI] [PubMed] [Google Scholar]
- Hart J.T. The inverse care law. Lancet. 1971;1:405–412. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- Massinga Loembé M., Tshangela A., Salyer S.J., Varma J.K., Ouma A.E.O., Nkengasong J.N. COVID-19 in Africa: the spread and response. Nat. Med. 2020;26:999–1003. doi: 10.1038/s41591-020-0961-x. [DOI] [PubMed] [Google Scholar]
- McKinsey Evaluating the sub-Saharan African pharmaceutical market. 2019. https://www.mckinsey.com/industries/public-and-social-sector/our-insights/should-sub-saharan-africa-make-its-own-drugs
- Nkengasong J. Let Africa into the market for COVID-19 diagnostics. Nature. 2020;580:565. doi: 10.1038/d41586-020-01265-0. [DOI] [PubMed] [Google Scholar]
- Nkengasong J.N., Maiyegun O., Moeti M. Establishing the Africa Centres for Disease Control and Prevention: responding to Africa’s health threats. Lancet Glob. Health. 2017;5:e246–e247. doi: 10.1016/S2214-109X(17)30025-6. [DOI] [PubMed] [Google Scholar]
- O’Neill J. Antimicrobial Resistance: tackling a crisis for the health and wealth of nations. 2014. https://amr-review.org/sites/default/files/AMR Review Paper - Tackling a crisis for the health and wealth of nations_1.pdf
- United Nations ECA . United National Economic Commission for Africa; 2016. The Demographic Profile of African Countries. [Google Scholar]
- World Health Organization . World Health Organization; 2017. A Study on the Public Health and Socioeconomic Impact of Substandard and Falsified Medical Products. [Google Scholar]
- World Health Organization Regional Office for Africa . WHO Regional Office for Africa; 2019. A Heavy Burden: The Productivity Cost of Illness in Africa. [Google Scholar]
- World Bank . The World Bank; 2020. Global Economic Prospects, June 2020. [Google Scholar]