Introduction
The pharmacist role, especially in team-based primary care, has evolved tremendously over the past several years.1 The North York Family Health Team (NYFHT) is an urban family health team serving patients in the northern part of Toronto and surrounding areas. Since its inception in 2008, NYFHT has seen an increasing number of physicians and patients and, subsequently, an increase in staff, including pharmacists, over the years as a direct result of referral volume. There have been 3 full-time pharmacists since 2013 to provide clinical and other professional pharmacist services.
Pharmacist services at the NYFHT encompass a wide range of activities,2 including but not limited to providing drug information, offering pharmacotherapy consults, conducting medication reviews, supporting various FHT-wide chronic disease management programs, participating in quality improvement initiatives, assisting with data standardization and conducting practice-based research.2
The pharmacists are also involved in teaching and precepting medical and pharmacy learners at various levels of education. Teaching occurs via small group seminars as well as large lectures. Precepting occurs 1:1 with pharmacy students and residents.
The pharmacist role3 at the NYFHT is similar to others in primary care, but the provision of pharmacist services and how it is done is unique compared to what is often described in the literature. Developing the role of the pharmacist at the NYFHT has had some challenges, due to the size of the organization, which is composed of 90 physicians, 40 interprofessional health care providers and over 85,000 patients. The NYFHT physician offices are spread over 20 physical sites across North York, with 1 central interprofessional health office. The interprofessional health care providers include registered pharmacists, registered nurses, registered dietitians, social workers, nurse practitioners, a physician assistant, a case worker and a chiropodist.
Many primary care pharmacists function directly in the same clinic or building with physicians.4-6 Prior to 2013, 2 pharmacists were deployed to each individual NYFHT physician office, spending half a day to a full day, on a weekly to monthly basis. This led to inefficiency due to travel times as well as scheduling difficulties. To reduce travel time and accommodate staffing changes, from 2013 to 2017, pharmacist services were centralized at the interprofessional health office. Inevitably, feedback from some physicians was that this completely centralized model of practice presented a barrier for some patients to travel to the central interprofessional health office for services. In addition, it became difficult for physicians to collaborate with various interprofessional health care providers on direct patient care.
In 2018, a pilot to have interprofessional health care providers offer services at some physician offices was proposed. Owing to the success of the pilot, the 3 pharmacists at the NYFHT continue to provide pharmacy services at the central interprofessional health office but also remain situated in selected physician offices on a weekly basis, creating a hybrid model of pharmacy services. This hybrid model of pharmacy services is unique to our knowledge, and this article will further describe the experience in a large, multisite family health team.
Description
In 2018, when the idea to reconsider the existing model of interprofessional health services occurred, a survey was sent out by the NYFHT administration asking whether individual physician offices would like to have interprofessional health care providers work directly in their offices.
Five of the 20 NYFHT sites requested a pharmacist and were included in the pilot (Table 1, weekly pharmacist schedule).
Table 1.
Weekly pharmacist schedule
| Monday | Tuesday | Wednesday | Thursday | Friday | Total offsite physicians | |
|---|---|---|---|---|---|---|
| Pharmacist 1 | CS | CS | CS | CS | Offsite 7 physicians |
7 |
| Pharmacist 2 | CS | CS | Offsite 2 physicians |
Offsite 4 physicians |
CS | 6 |
| Pharmacist 3 | CS | CS | Offsite 2 physicians |
Offsite 3 physicians |
CS | 5 |
| 18 |
CS, central site.
As mentioned, prior to this pilot, the pharmacists primarily provided clinical services at the central interprofessional health office. The pharmacists have always participated in both supporting group programs as well as providing direct patient care. Here is a brief description of the hybrid model.
1. Centralized pharmacist services (highlights)
Diabetes Education Program
The Diabetes Education Program (DEP) offers patients with diabetes a multidisciplinary team visit composed of a nurse, dietitian and pharmacist for 1-hour sessions. Team visits allow the discussion and care plan to be tailored to the patient’s needs in a more consistent, coordinated manner. In collaboration with the other DEP team members, the pharmacist addresses patient concerns regarding medications, adjusts dosages and discusses potential options to help improve glycemic control. Pharmacists also cofacilitate monthly group classes for patients with diabetes at the central site.
Chronic Insomnia Program
The Chronic Insomnia Program provides deprescribing guidance for sedative-hypnotics as well as cognitive behavioural therapy for insomnia (CBT-I). For patients interested in tapering chronic use of sedative-hypnotics, the pharmacist will assist with a tapering schedule and monitor progress. CBT-I is offered in group classes run by the pharmacy and social work teams, as well as individual sessions. To help facilitate sedative-hypnotic deprescribing, the NYFHT pharmacists have be trained to provide CBT-I. Although not a traditional role of the pharmacist, providing CBT-I is an innovative way to help improve patient care.
Smoking Cessation Program and Lung Health Program (spirometry screening for chronic obstructive pulmonary disease)
Current Canadian Thoracic Society Guidelines recommend spirometry testing for people 40 years or older with a smoking history who have screened positive with the Canadian Lung Health Test. As Certified Respiratory Educators (CREs), the pharmacists are trained to perform and interpret spirometry. While patients can attend a traditional pulmonary function lab, office spirometry is offered at the central site to improve access. As a part of the Smoking Cessation Program (SCP), patients are screened and referred for spirometry. Equipment, such as the spirometer, is kept and used at the central site. This negates the cost and need for each pharmacist to carry equipment to the offices. Spirometry results and reports are then sent to the physicians via our electronic medical record (EMR). Further investigations and/or referral to a respirologist are advised for some patients with abnormal spirometry findings.
Lastly, at the central site, the pharmacists serve the other 72 physicians and their patients whose offices they do not directly visit. Pharmacist services predominantly involve pharmacotherapy consultations, which include management of side effects, drug interactions, labile international normalized ratios (INRs), renal and hepatic dosing adjustments, efficacy and so on. There is also substantial time spent on providing drug information and solving drug access issues, which includes exploring drug coverage (via public or private plans), navigating compassionate supply programs and providing guidance for drug recalls and drug shortages. In order to provide these pharmacy services to a large number of physicians and staff, consults come into a common virtual mailbox and are triaged by the next available pharmacist to improve efficiency and response time. Having pharmacists at the central site also allows for “drop-in” questions from interprofessional health care providers and/or patients so the team strives to have a minimum of 1 pharmacist at the central site on a daily basis.
2. Decentralized pharmacist services (highlights)
Individual practice sites differ tremendously in terms of practice size and physician practices. The number of physicians serviced at the 5 sites ranges from 2 to 7, with some practices focusing on obstetrics and newborns, while others see more older adults with complex comorbidities.
Several of the direct patient care pharmacy services done at the central site can be transferred to the individual physician offices. However, direct pharmacist presence helps with impromptu drug information requests and on-demand medication counselling, which includes discussing new medication initiations, providing dosing and administration instructions and counselling on side effects and drug interactions (especially herbal products and dietary supplements). The timeliness of medication reviews and hospital discharge medication reconciliation has also been improved at the offices that have a pharmacist present.
Another highlight of being located in the physician offices is the ability to work 1:1 with medical students and residents while they practise, as opposed to when they shadow a pharmacist at the central site. It provides a more real-life experience as to what interprofessional collaboration entails.
Results
There has been a significant increase in pharmacist consultations and referrals since the start of this hybrid model. Figure 1 depicts the cumulative number of referrals for distinct patients from 2016 to present. Figure 2 depicts the total cumulative number of pharmacist consultations from 2016 to present. The years 2016 and 2017 show overlapping data, as it was the time before the hybrid model was initiated. An increasing trend can be seen starting in mid-2018, when the hybrid model was adopted.
Figure 1.
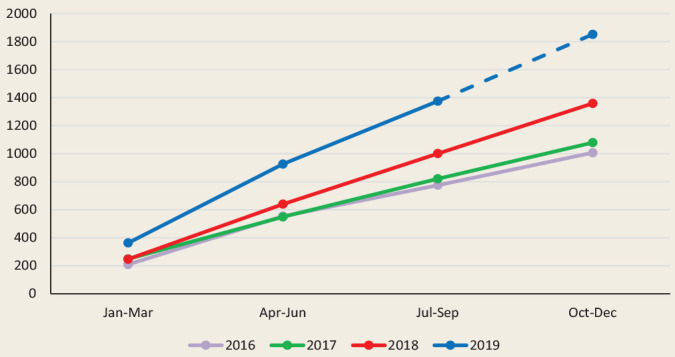
Total number of patients seen by a pharmacist
Figure 2.
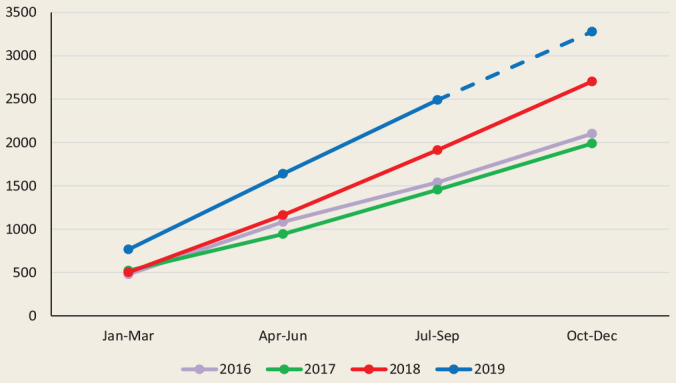
Total number of pharmacist consultations
The difference between the data in the 2 figures reflects the fact that some patients receive multiple consultations with a pharmacist. As the figures show, the number of distinct patients has grown from an average near 1000 to a projected estimate, shown by the dashed line, of ~1850 for 2019. Similarly, the number of consultations has grown from almost 2000 to a projected estimate of ~3250. The consultations include both in-person as well as telephone encounters.
Discussion
For the NYFHT, a hybrid model of practice has allowed the pharmacists to more effectively collaborate with participating physicians in providing patient care while still permitting pharmacists to participate in various group programs, quality improvement and research activities. Pharmacist services at the NYFHT are not volume based. The numbers presented above are used to illustrate the growth of pharmacist services since moving to a hybrid model. There may be selection bias and less generalizability to practices where collaboration is uncommon, as the physician offices in this pilot specifically requested a pharmacist to be present at their location.
Undeniably, there are several pros and cons of each model of pharmacy services as well as this hybrid model. Being highly visible and accessible is an important part of integrating pharmacists into primary care in order to ensure success.4-6 It has been suggested that proximity allows for improved team-based care,7 as demonstrated by the higher numbers of referrals and consultations when the pharmacists are in the physician offices. Further analysis of this effect on the health care system is required, as health outcome data were not collected during this pilot, but the literature has shown that consultation with a pharmacist can result in better health outcomes8,9 and reduce health care costs.9,10 With a large, multisite organization, it is almost impossible for 3 pharmacists to be present in all 20 NYFHT physician offices on a weekly basis. In addition, if the pharmacists were permanently located offsite at physician offices, it would be more difficult to participate in meetings and collectively work to produce documents, summaries, newsletters or references for the team. Opportunities to meet with each other, whether formal or informally, are also important for team building. A clinical pharmacist can also provide a unique perspective for FHT-wide initiatives such as quality improvement3 and data standardization, so it is important to include pharmacists in such meetings. Although there is an opportunity for teleconference, face-to-face time is valued as well. It would also be challenging to serve group programs and multidisciplinary patient visits if the pharmacists were no longer present at the central site.
It is important to note that when the pharmacists are not physically present in the 5 physician offices, they can still be reached through the EMR or telephone. This is particularly helpful if one particular pharmacist is off, as others can cover to prevent a delay in responses to that respective physician office.
When the pilot was first initiated, it was reportedly difficult to reach the pharmacists who were offsite, as they did not have access to their telephone lines and all EMR servers. With help from our Integrated Technology (IT) personnel, the pharmacists were provided with voiceover Internet phone lines that directly connected with our existing telephone extensions so they could be connected at all times. Similarly, remote server access was granted.
It was also a challenge at first for administrative assistants to know where each pharmacist was each day. This was resolved by creating a chart that detailed the weekly schedule (Table 1), as well as by using a capability in our EMR to note when, where and which pharmacist could provide services.
The last challenge identified is that pharmacists, along with other interprofessional health care providers, require office space to see patients and/or make telephone calls. In some physician offices, there is not enough working space to accommodate an additional team member. As such, some NYFHT physician groups are content with the central model of pharmacy services.
Conclusion
A hybrid model for pharmacist services is feasible and works effectively for a large, multisite family health team. Central pharmacist services are important for pharmacists supporting group programs and a large number of physicians, but it is also very worthwhile to have pharmacists work directly in physician offices. ■
Footnotes
This article was written in the Fall of 2019. Since the COVID-19 pandemic, the model of pharmacist services as changed once again.
ORCID iDs:Christine Truong, BScPhm, ACPR, RPh,  https://orcid.org/0000-0003-3470-1457
https://orcid.org/0000-0003-3470-1457
Eric Lui, MSc, PharmD, RPh,  https://orcid.org/0000-0003-1529-2096
https://orcid.org/0000-0003-1529-2096
References
- 1. Dolovich L. Ontario pharmacists practicing in family health teams and the patient-centered medical home. Ann Pharmacother 2012;46(4):S33-9. [DOI] [PubMed] [Google Scholar]
- 2. Lui E, Ha R, Truong C. Applying the pharmaceutical care model to assess pharmacist services in a primary care setting. Can Pharm J (Ott) 2017;150(2):90-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hadden H, Singh S. Five things you need to know about family health team pharmacists. Ontario Pharmacist. Published Summer 2017. Available: https://www.afhto.ca/wp-content/uploads/Evidence-of-Value-TOP-2017-Issue-2-FHT.pdf (accessed Oct. 10, 2019).
- 4. Ontario Pharmacist Association. Family health team resource kit. Available: http://www.impactteam.info/documents/fht_toolkit.pdf (accessed Oct. 10, 2019).
- 5. Jorgenson D, Dalton D, Farrell B, et al. Guidelines for pharmacists integrating into primary care teams. Can Pharm J (Ott) 2013;146(6):342-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Barry A, Pammett R. Applying the guidelines for pharmacists integrating into primary care teams. Can Pharm J (Ott) 2016;149(4):219-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zubin A. There is no “I” in “team”: the social psychology of team functioning in health care. Available: https://slideplayer.com/slide/6633177/ (accessed July 9, 2020).
- 8. Mendonca S, Melo A, Coelho Pereira GC, et al. Clinical outcomes of medication therapy management services in primary health care. BJPS 2016;52(3):365-73. [Google Scholar]
- 9. Isetts B, Schondelmeyer SW, Artz M, et al. Clinical and economical outcomes of medication therapy management services: the Minnesota experience. J Am Pharm Assoc 2008;48(2):203-14. [DOI] [PubMed] [Google Scholar]
- 10. Pringle J, Boyer A, Conklin MH, et al. The Pennsylvania Project: pharmacist intervention improved medication adherence and reduced health care costs. Health Affairs 2014;33(8):1444-52. [DOI] [PubMed] [Google Scholar]


