Abstract
A 65-year-old woman was addressed for clinical and biological suspicion of ovarian cancer relapse. 18F-FDG PET/CT revealed massive peritoneal carcinomatosis. Post-chemotherapy PET/CT showed complete metabolic response in initial localizations albeit three new 18F-FDG uptakes appeared in the mesentery and in the retro-hepatic space. Close follow-up (including PET/CT scan) and surgical examination of the abdominal cavity confirmed the absence of malignancy and the benign nature of these lesions, which appeared to be peritoneal fibrosis mimicking persistent carcinomatosis.
Keywords: 18F-FDG PET, Peritoneal carcinomatosis, Peritoneal fibrosis, Metastatic ovarian cancer
Introduction
Due to its non-specific uptake in peritoneal lesions, 18F-FDG can mimic peritoneal carcinomatosis. Differential diagnosis is challenging in gynecological malignancies and surgical confirmation is warranted.
Case Report
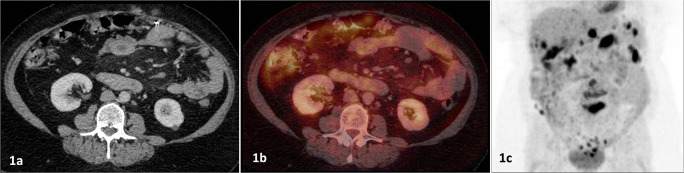
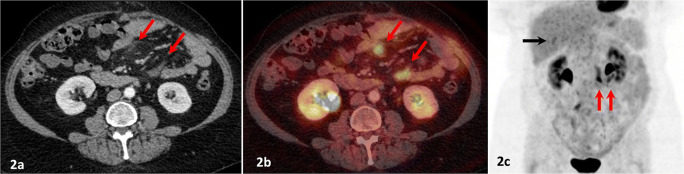
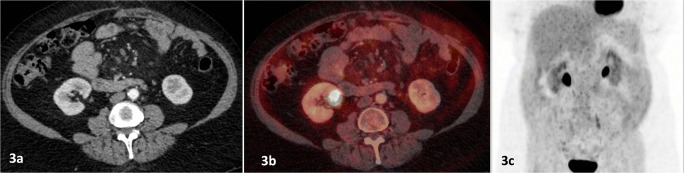
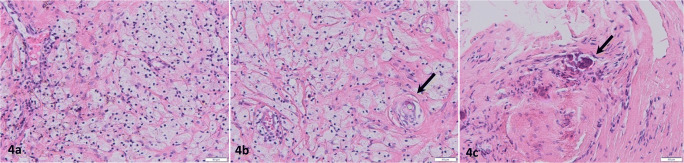
A 65-year-old woman previously treated for FIGO IIIB ovarian papillary serous carcinoma (surgery and chemotherapy) was referred to our institution for evaluation of abdominal pain and tumor markers increase (CA-125, 74 U/ml; reference, < 35), suggesting ovarian cancer relapse. In addition to oncological laparotomy, the patient has been through abdominal surgeries for eventration and hernia repair. 18F-FDG PET/CT demonstrated massive hypermetabolic peritoneal carcinomatosis (Fig. 1c; SUVmax 17.5). Chemotherapy was initiated (carboplatin and doxorubicin): 6 months later and after 6 cycles, markers dropped (CA-125, 11 U/ml) and 18F-FDG PET/CT showed complete metabolic response in all initial localizations. However, two isodense ill-defined and hypermetabolic tissue infiltrations appeared in the mesentery (Fig. 2a–c, red arrows; SUVmax 9.4). Another peritoneal 18F-FDG uptake without radiological substratum was identified on the posterior side of the liver (Fig. 2c, black arrow; SUVmax 5.2). In order to explore these new lesions, surgical examination of the abdominal cavity was decided rather than initiating maintenance treatment with PARP inhibitor. Laparoscopic exploration found calcified fibrotic lesions in the peritoneum, and lavage cytology found no neoplastic lesion. Histopathological examination of biopsies of the peritoneal cavity disclosed a background of fibrosis with mononucleated foamy macrophagic infiltrate (Fig. 3a), multinucleated giant cells incorporating some birefringent foreign bodies (Fig. 3b, arrow), and fibrosis containing some calcifications and psammoma bodies (Fig. 3c, arrow). In light of those results combined with tumor markers drop (CA-125, 9 U/ml), close follow-up was decided. Three months later, follow-up with 18F-FDG PET/CT showed spontaneous regression of these lesions and complete metabolic response (Fig. 4a–c). It is noteworthy that during follow-up (1-year period), no clinical nor biochemical recurrence had occurred.
Fig. 1.
Pre-therapeutic 18F-FDG PET/CT: contrast-enhanced CT (a), fused PET/CT (b), and MIP (c)
Fig. 2.
18F-FDG PET/CT after 6 cycles of chemotherapy (6 months later): contrast-enhanced CT (a), fused PET/CT (b), and MIP (c)
Fig. 4.
Follow-up 18F-FDG PET/CT (9 months after treatment initiation): contrast-enhanced CT (a), fused PET/CT (b), and MIP (c)
Fig. 3.
Histopathological examination of biopsies of the peritoneal cavity : mononucleated foamy macrophagic infiltrate (a), multinucleated giant cells (b, arrow), and fibrosis with calcifications and psammoma bodies (c, arrow)
Discussion
This clinical scenario strongly suggests that 18F-FDG PET/CT examination at the end of the chemotherapy was a false positive examination. It also emphasizes the concept that inflammatory peritoneal lesions can persist for a long time in a random way and hypermetabolic foci should be extensively investigated before therapeutic decision. Indeed, a variety of 18F-FDG-avid physiological, benign (inflammatory and/or infectious), or malignant conditions can be involved in the peritoneum [1–5]. No quantitative uptake cut-off can be used for differential diagnosis, because inflammatory lesions also exhibit high 18F-FDG uptake due to the overexpression of GLUT-1 in macrophages [6]. Davidson et al. [7] have described years-lasting 18F-FDG uptake by fat necrosis in a post-surgical setting in a series of patients. Unlike in our case (Fig. 3), no cytological and/or histopathological confirmation of absence of malignancy was available. Even if careful radiological interpretation must allow differential diagnosis, contrast-enhanced CT appearance of the lesions showed no distinctive feature of benign inflammatory process (no typical fatty core with surrounding rim nor calcifications). Also, while peritoneal inflammation such as mesenteric panniculitis is a diagnostic challenge in an oncological setting [8], peri-hepatic localizations have not been reported before as a potential pitfall for differential diagnosis of peritoneal carcinomatosis on 18F-FDG PET/CT. The integration of the clinical and biological context in a thorough interpretation of follow-up examinations (spontaneous size reduction on CT and no increase in 18F-FDG uptake in post-surgical inflammatory changes) is essential in order to avoid misdiagnosis.
Acknowledgments
I would like to offer my special thanks to all co-authors.
Compliance with Ethical Standards
Conflict of Interest
Benjamin Leroy-Freschini, Véronique Lindner, Thomas Boisramé and Martin Demarchi declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed Consent
The requirement to obtain informed consent was waived.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Benjamin Leroy-Freschini, Email: b.leroy-freschini@icans.eu.
Véronique Lindner, Email: veronique.lindner@chru-strasbourg.fr.
Thomas Boisramé, Email: Thomas.boisrame@chru-strasbourg.fr.
Martin Demarchi, Email: m.demarchi@icans.eu.
References
- 1.Agarwal Sharma R, Lee EY, Vardhanabhuti V, Khong PL, Ngu SF. Unusual case of postmenopausal diffuse endometriosis mimicking metastatic ovarian malignancy. Clin Nucl Med. 2016;41:e120–e122. doi: 10.1097/RLU.0000000000001038. [DOI] [PubMed] [Google Scholar]
- 2.Kim BW, Kim HW, Won KS, Kang YN, Choi BW. Colonic parasitic infection mimicking peritoneal seeding on 18F-FDG PET/CT. Clin Nucl Med. 2017;42:e365–e366. doi: 10.1097/RLU.0000000000001709. [DOI] [PubMed] [Google Scholar]
- 3.Agrawal K, Sajjan RS, Saad ZZ, Groves A, Bomanji J, Syed R. Transposed ovary mimicking a peritoneal implant on FDG PET/CT in a patient with carcinoma of the rectum. Eur J Nucl Med Mol Imaging. 2014;41:1642–1643. doi: 10.1007/s00259-014-2767-x. [DOI] [PubMed] [Google Scholar]
- 4.Dubreuil J, Giammarile F, Rousset P, Rubello D, Bakrin N, Passot G, et al. The role of 18F-FDG PET/ceCT in peritoneal mesothelioma. Nucl Med Commun. 2017;38:312–318. doi: 10.1097/MNM.0000000000000649. [DOI] [PubMed] [Google Scholar]
- 5.Watanabe T, Terai S, Tsukada T, Takeshita M, Matsui K, Amaya K, et al. Sclerosing mesenteritis mimicking metachronous peritoneal metastases from descending colon adenocarcinoma. World J Surg Oncol. 2017;15:142. doi: 10.1186/s12957-017-1214-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mochizuki T, Tsukamoto E, Kuge Y, Kanegae Y, Zhao S, Hikosaka H, et al. FDG uptake and glucose transporter subtype expressions in experimental tumor and inflammation models. J Nucl Med. 2001;42:1551–1555. [PubMed] [Google Scholar]
- 7.Davidson T, Lotan E, Klang E, Nissan J, Goldstein J, Goshen E, et al. Fat necrosis after abdominal surgery: a pitfall in interpretation of FDG-PET/CT. Eur Radiol. 2018;28:2264–2272. doi: 10.1007/s00330-017-5201-5. [DOI] [PubMed] [Google Scholar]
- 8.Makis W. Progressing sclerosing mesenteritis (mesenteric panniculitis) mimics progression of malignancy after neoadjuvant chemotherapy for gastric adenocarcinoma on serial 18F-FDG PET/CT. Clin Nucl Med. 2016;41:313–316. doi: 10.1097/RLU.0000000000000965. [DOI] [PubMed] [Google Scholar]