To the Editor:
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes the so-called coronavirus disease (COVID-19), which is characterized by a broad spectrum of clinical presentations ranging from asymptomatic patients to critically ill individuals with a high case fatality rate (1). The critical care community has increasingly recognized that cardiovascular and thrombotic complications are relatively common in COVID-19 (2). Indeed, direct involvement of the vascular endothelium was recently reported in a series of patients suffering from severe COVID-19 (3). The endothelial glycocalyx (eGC), which covers the luminal surface of endothelial cells, contributes to the maintenance of vascular homeostasis, whereas disruption of the eGC is observed early in critically ill patients and is associated with inferior outcomes (4, 5).
Here, we investigated in translational human and cellular studies whether injury to the eGC can be found in critically ill patients with COVID-19 early after admission to the ICU. We collected plasma and serum from 19 adult individuals within 24 hours after invasive ventilation for acute respiratory distress syndrome and from 10 healthy human donors after written informed consent of patients or their legal representative. The first patient was admitted on March 19, 2020, and the observation period was until May 17, 2020. The median (interquartile range) observation duration was 47 (40–54) days.
Baseline patient characteristics at study inclusion as well as a description of the further clinical course are summarized in Table 1. Organ failure was not restricted to the lungs, and multiorgan dysfunction was common both at inclusion and during the further clinical course. Surprisingly, global markers of endothelial injury such as Angpt-1 (angiopoietin-1) (control: 29 [26.2–30.9] ng/ml vs. COVID-19: 27.8 [23.4–36.2] ng/ml; P = 0.79) and Angpt-2 (control: 0.655 [0.336–1.113] ng/ml vs. COVID-19: 0.434 [0.035–1.338] ng/ml; P = 0.6) were unchanged in patients with COVID-19. In contrast, marked increases in the soluble form of the sTie2 (Tie2 receptor) (Figure 1A) and in syndecan-1 (Figure 1B)—indicating pathological shedding of transmembrane proteins involved in glycocalyx structure and processing—were observed. The key eGC sheddase Hpa-1 (heparanase-1) and its enzymatic activity were both not significantly increased (data not shown). To the contrary, the Hpa-1 counterpart, the protective Hpa-2 (heparanase-2), was pertinently reduced in all patients with COVID-19 (Figure 1C). Driven by this acquired Hpa-2 deficiency, the Hpa-1:Hpa-2 ratio was higher in patients with COVID-19 (P = 0.012; data not shown). Together, this indicates that critically ill patients with COVID-19 suffer from an acquired Hpa-2 deficiency that can contribute to the degradation of the eGC, maybe even before classical endothelial activation and injury. Next, eGC structure was analyzed in humans, employing sublingual sidestream darkfield (SDF) imaging. We quantified the size of the individual patients’ eGC using an indirect surrogate termed the perfused boundary region and found a decrease of perfused boundary region, indicating reduced eGC thickness in patients with COVID-19. To demonstrate that the deficiency of Hpa-2 is mechanistically involved in the degradation of the eGC, we used a microfluidic chamber with cultured endothelial cells (ECs) under flow that synthesize an intact and stable eGC under in vitro conditions. After stimulation with COVID-19 or control serum, the eGC was visualized by confocal microscopy followed by computerized three-dimensional reconstruction. Its thickness was then quantified by analyzing the heparan sulfate (HS)-positive area. We found that stimulation with COVID-19 was sufficient to severely damage the eGC (Figure 1E). The HS-positive area was reduced by 34% (control: 6.1 ± 0.9% vs. COVID-19: 4 ± 0.4% P < 0.001). Consistent with our observation in patients, we found that the transcription of Hpa-2 in COVID-19–stimulated ECs was significantly reduced after 6 hours (0.63 ± 0.02 relative expression to control; P = 0.003). Of note, transgenic overexpression of Hpa-2 in a lentivirus-transduced EC line was sufficient to reverse this phenotype, as the HS area in COVID-19 serum–treated lenti-control cells was 1.9 ± 0.6% but was 4.2 ± 1.2% in lenti-Hpa-2–overexpressing cells (P < 0.001). In other words, if ECs overexpress Hpa-2, the serum of patients with COVID-19 cannot degrade the eGC anymore.
Table 1.
Patient Characteristics at Study Inclusion and Further Clinical Course
| Characteristic | Results |
|---|---|
| Number of patients | 19 |
| Age, yr, median (interquartile range) | 57 (45–69) |
| Sex, n (%) | |
| M | 18 (95) |
| F | 1 (5) |
| BMI, kg/m2, median (interquartile range) | 27.8 (26.2–33.5) |
| Comorbidities, n (%) | |
| Asthma | 1 (5) |
| HTN | 10 (53) |
| CHF | 2 (11) |
| CAD | 1 (5) |
| Diabetes | 5 (26) |
| CKD | 1 (5) |
| Obesity | 7 (37) |
| Malignancy | 2 (11) |
| Immunosuppression | 2 (11) |
| Invasive ventilation, n (%) | 19 (100) |
| Time from hospital to ICU admission, d, median (interquartile range) | 0 (0–2) |
| Time from ICU admission to invasive ventilation, d, median (interquartile range) | 0 (0–0) |
| Respirator parameters, median (interquartile range) | |
| FiO2, % | 50 (30–60) |
| PEEP, mbar | 12 (12–15) |
| Pplat, mbar | 27 (23–30) |
| Oxygenation index (PaO2/FiO2), mm Hg, median (interquartile range) | 173 (152–260) |
| PaCO2, mm Hg, median (interquartile range) | 46 (40–51) |
| pH, median (interquartile range) | 7.36 (7.32–7.41) |
| Lactate, mmol/L, median (interquartile range) | 1.6 (1.5–2.9) |
| Vasopressor, n (%) | 16 (84.2) |
| Norepinephrine dose, μg/kg/min, median (interquartile range) | 0.083 (0.019–0.182) |
| Renal replacement therapy, n (%) | 3 (16) |
| vv-ECMO support, n (%) | 2 (11) |
| SOFA score, points, median (interquartile range) | 11 (9–14) |
| Organ-specific failures, n (%) | |
| Respiratory (PaO2/FiO2 < 300) | 19 (100) |
| Coagulation (thrombocytes < 100) | 1 (5) |
| Liver (bilirubin > 33 μmol/L) | 1 (5) |
| Cardiovascular (dobutamine or norepinephrine) | 16 (84) |
| Neurological (GCS < 13) | 19 (100) |
| Renal (creatinine > 170 μmol/L) | 4 (21) |
| Lab, median (interquartile range) | |
| CRP (normal: <5), mg/L | 174 (121–203) |
| PCT normal: <0.5), μg/L | 3.8 (0.5–10.9) |
| IL-6 (normal: <7), ng/L | 272 (142–541) |
| LDH (normal: <248), U/L | 548 (384–657) |
| D-Dimer (normal: <0.5), mg/L | 3.56 (0.84–8.88) |
| Troponin T (normal: <14), ng/L | 17 (11–23) |
| NT-proBNP (normal: <86), ng/L | 260 (82–1108) |
| Further clinical course, n (%) | |
| Prone position | 19 (100) |
| Inhaled NO | 4 (21) |
| vv-ECMO | 7 (37) |
| Renal replacement therapy | 8 (42) |
| Septic shock | 10 (53) |
| Died by end of observation period | 3 (16) |
| Still dependent on critical care | 6 (32) |
| Still dependent on mechanical ventilation | 2 (11) |
Definition of abbreviations: BMI = body mass index; CAD = coronary artery disease; CHF = congestive heart failure; CKD = chronic kidney disease; CRP = C-reactive protein; ECMO = extracorporeal membrane oxygenation; GCS = Glasgow Coma Scale; HTN = hypertension; LDH = lactate dehydrogenase; NT-proBNP = N-terminal pro–B-type natriuretic peptide; PCT = procalcitonin; PEEP = positive end-expiratory pressure; Pplat = plateau pressure; SOFA = Sequential Organ Failure Assessment; vv-ECMO = venovenous ECMO.
Demographic and clinical characteristics are given at the time of study inclusion as well as a description of the further clinical outcome within the observation period. Values are presented as median (interquartile range) or, if categorical, as numbers and percentages. Demographic characteristics for the control patients were as follows: age 32 (28–33) years and 9/10 male sex for laboratory investigation control patients; 39 (36–44) years and 5/10 male sex for sidestream darkfield imaging measurement control patients. All individuals of the control cohorts had no relevant medical preconditions.
Figure 1.
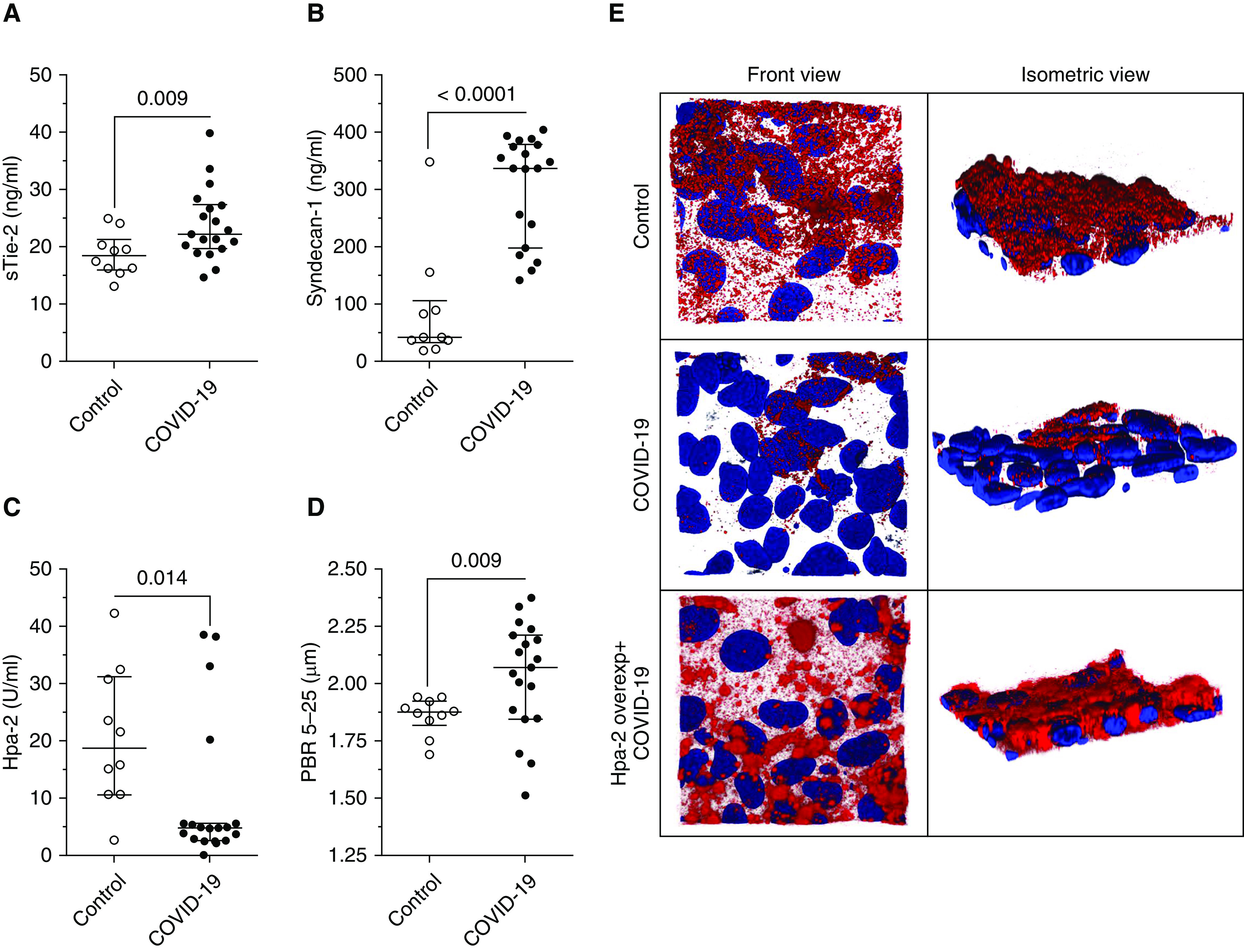
Injury to the endothelial glycocalyx in severe coronavirus disease (COVID-19). Scatter dot plots (median [interquartile range]) show (A) sTie-2 and (B) syndecan-1 concentrations for control and patients with COVID-19. Concentrations for both syndecan-1 (control: 41.5 [32.6–105.4] ng/ml vs. COVID-19: 336.5 [196.7–377.1] ng/ml) and sTie-2 (control: 18.4 [16–21.3] ng/ml vs COVID-19: 22.3 [19.7–27.3] ng/ml) were increased in patients with COVID-19. (C) Although both Hpa-1 (heparanase-1) concentration and activity were not significantly altered in comparison with control subjects, patients with COVID-19 showed an acquired deficiency in Hpa-2 (heparanase-2) (control: 18.7 [10.6–31.1] U/ml vs. COVID-19: 4.7 [2.6–5.1] U/ml). Consequentially, the Hpa-1:Hpa-2 ratio was higher in patients with COVID-19 (control: 0.08 [0.05–0.17] ng/U vs. COVID-19: 0.35 [0.27–0.66] ng/U). (D) Sidestream darkfield imaging in patients allows the quantification of endothelial glycocalyx thickness as indicated by increased perfused boundary region; this was increased in patients with COVID-19 (control: 1.9 [1.8–1.9] μm vs. COVID-19: 2.1 [1.8–2.2] μm), indicating reduced endothelial glycocalyx thickness. For comparison of groups, first, the normal distribution (D’Agostino-Pearson omnibus and Shapiro-Wilk normality test) of variables was tested, and then (A and D) two-sided unpaired t tests and (B and C) Mann-Whitney tests were used accordingly. (E) Exemplary three-dimensional reconstruction of the heparan sulfate (HS) layer images of naive endothelial cells in a microfluidic chip (HS in red; DAPI nuclei staining in blue) after perfusion with serum of a patient with COVID-19 (middle row) compared with a healthy control subject (upper row) in both front and isometric view angles demonstrates the diffuse loss of HS-rich glycocalyx layer in cells treated with COVID-19 serum. In Hpa-2–overexpressing endothelial cells (lower row), the HS surface layer is protected from injurious effects by perfusion with COVID-19 serum. overexp = overexpressing; PBR = perfused boundary region; sTie-2 = soluble Tie-2.
This exploratory study has obvious limitations, most importantly, its small sample size and hypothesis-generating nature. Injury to the eGC is not a finding specific for COVID-19 but can be found in a wide range of critically ill patients (5). Because only a small selection of molecules that may participate in endothelial injury have been investigated in this study, we cannot exclude that further mediators may play a critical role in endothelial and eGC injury in patients with COVID-19. In addition, because of concerns of viral transmission, SDF imaging values could not be obtained from the same control patients from whom blood analysis was performed but were obtained from a separate historic in-center control cohort. Both control cohorts were not matched to the individual patients in terms of age, but the control group that blood was collected from was matched in terms of male predominance.
In summary, we found injury of the eGC and speculate that this might represent a potentially critical hallmark of later widespread endothelial injury in severe COVID-19. Reduced eGC thickness was visualized in vivo by employing sublingual SDF imaging in patients. At the same time, increased syndecan-1 and sTie-2 concentrations in the blood of these patients indicated shedding of important endothelial transmembrane proteins responsible for building (5) and maintaining (6) the structure of the eGC, respectively. Interestingly, eGC shedding could be reproduced when patient blood was transferred ex vivo into an endothelial microcapillary chip model. Although Hpa-1 and its enzymatic activity (primarily responsible for HS degradation) (7) was found to be normal, Hpa-2, a protein that has been described as a protective antagonist of Hpa-1 (8, 9), was severely depleted in COVID-19. Importantly, degradation of the eGC after perfusion with COVID-19 serum could be attenuated in ECs overexpressing Hpa-2. We therefore postulate that acquired Hpa-2 deficiency might represent a potential mechanism of injury to the eGC, which could later progress to widespread endothelial dysfunction in COVID-19.
In conclusion, our data suggest that in critically ill patients with COVID-19, endothelial injury involves glycocalyx integrity, and acquired Hpa-2 deficiency might be a potential causative factor.
Supplementary Material
Acknowledgments
Acknowledgment
The authors thank Yvonne Nicolai for excellent technical support and Dr. Markus Busch and Dr. Olaf Wiesner and the nursing staff for their infrastructural support in conducting this study.
Footnotes
S.D. is supported by the German Research Foundation (DA 1209/4-3) and the German Center for Lung Research.
Authors Contributions: K.S., P.A.G., B.S., T.W., H.H., M.M.H., and S.D. obtained retrospective data. K.S., P.A.G., A.B., and S.D. performed sidestream darkfield imaging measurements. P.A.G. and T.P. performed ELISA measurements, and Y.K. performed and analyzed flow measurements. K.S., P.A.G., H.H., T.W., M.M.H., and S.D. analyzed and discussed the data and generated figures and tables. K.S., P.A.G., and S.D. wrote the manuscript; all authors proofread the manuscript.
Originally Published in Press as DOI: 10.1164/rccm.202007-2676LE on August 24, 2020
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, et al. Covid-19 in critically ill patients in the seattle region: case series. N Engl J Med. 2020;382:2012–2022. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmidt EP, Yang Y, Janssen WJ, Gandjeva A, Perez MJ, Barthel L, et al. The pulmonary endothelial glycocalyx regulates neutrophil adhesion and lung injury during experimental sepsis. Nat Med. 2012;18:1217–1223. doi: 10.1038/nm.2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Uchimido R, Schmidt EP, Shapiro NI. The glycocalyx: a novel diagnostic and therapeutic target in sepsis. Crit Care. 2019;23:16. doi: 10.1186/s13054-018-2292-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lukasz A, Hillgruber C, Oberleithner H, Kusche-Vihrog K, Pavenstädt H, Rovas A, et al. Endothelial glycocalyx breakdown is mediated by angiopoietin-2. Cardiovasc Res. 2017;113:671–680. doi: 10.1093/cvr/cvx023. [DOI] [PubMed] [Google Scholar]
- 7.Martin L, Koczera P, Zechendorf E, Schuerholz T. The endothelial glycocalyx: new diagnostic and therapeutic approaches in sepsis. BioMed Res Int. 2016;2016:3758278. doi: 10.1155/2016/3758278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levy-Adam F, Feld S, Cohen-Kaplan V, Shteingauz A, Gross M, Arvatz G, et al. Heparanase 2 interacts with heparan sulfate with high affinity and inhibits heparanase activity. J Biol Chem. 2010;285:28010–28019. doi: 10.1074/jbc.M110.116384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kiyan Y, Tkachuk S, Kurselis K, Shushakova N, Stahl K, Dawodu D, et al. Heparanase-2 protects from LPS-mediated endothelial injury by inhibiting TLR4 signalling. Sci Rep. 2019;9:13591. doi: 10.1038/s41598-019-50068-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


