Abstract
Objective
Age-related cognitive decline is the deterioration in functions such as memory and executive function faced by most older adults and affects function and quality of life. No approved treatments exist for age-related cognitive decline. Computerized cognitive training has been shown to provide consistent albeit modest improvements in cognitive function as measured by neuropsychological testing. Vortioxetine, an antidepressant medication, has putative pro-cognitive and pro-neuroplastic properties; it therefore might be able to augment cognitive training.
Methods
We tested the cognitive benefits of vortioxetine added to cognitive training for adults aged 65+ with age-related cognitive decline. After a two-week lead-in period of cognitive training, 100 participants were randomized to vortioxetine vs. placebo, added to cognitive training, for 26 weeks. The primary outcome measure was global cognitive performance, assessed by the NIH Toolbox Cognition Battery fluid cognition composite. The secondary outcome was functional cognition, assessed by the UCSD Performance-based Skills Assessment (UPSA). All participants received motivational messaging and support from study staff to maximize adherence to the training.
Results
Older adults receiving vortioxetine added to cognitive training showed a greater increase in global cognitive performance, compared to those receiving placebo added to cognitive training. This separation was significant at week 12 but not other timepoints. Both groups showed improvement in the secondary outcome measure of functional cognition with no significant difference between groups.
Conclusions
Vortioxetine may be beneficial for age-related cognitive decline when combined with cognitive training. These findings provide new treatment directions for combatting cognitive decline in older adults.
Introduction
Most older adults experience deterioration in cognitive function.1,2 This age-related cognitive decline varies between individuals, with individual differences related to preclinical Alzheimer’s pathology, cerebrovascular disease, and educational and lifestyle differences.3 Age-related cognitive decline can have negative impact on quality of life, interpersonal relationships, and capacity for making decisions about finances, health care, retirement, and other issues important to older adults.4
One tool for addressing cognitive decline is cognitive training.5 This therapeutic procedure typically relies on activation of neural circuitry known to be impaired in illness, at-risk for decline, or compensatory for other cognitive functions. Neuroplasticity is achieved through repetitive drill and practice exercises that require the patient to perform cognitive operations that are slightly above their current ability threshold. Several studies find support for its use in age-related cognitive decline.6 For example, the ACTIVE study (Advanced Cognitive Training for Independent and Vital Elderly), a large randomized trial of a cognitive intervention in an older population with normal cognitive ability, showed that cognitive training has beneficial effects on specific functions that last at least five years.7 Cognitive training also shows benefits in cognitively compromised populations, including mild cognitive impairment, dementia, major depression, and schizophrenia.8,9 However, a concern with cognitive training is a small overall effect size and limited evidence of transfer effects to everyday cognitive tasks (i.e., improvement in “functional cognition”).10
Several pharmacological therapies have been tried for memory enhancement, but no treatment is currently approved for age related cognitive decline. Trials have included medications typically used for Alzheimer’s disease11, antidepressants12 and nutritional supplements.13 Vortioxetine is a medication that is approved for the treatment of major depression. Unlike most other serotonin reuptake inhibitors, vortioxetine is a potent antagonistic of postsynaptic 5-HT3 and 5-HT7 receptors, which has been proposed to indirectly increase dopaminergic, cholinergic, and histaminergic transmission which are involved in cognitive function.14
Preclinical research demonstrated vortioxetine’s pro-cognitive effects, putatively related to these postsynaptic receptor effects.14 It has shown both subjective and objective cognitive benefits in depression clinical trials. It was shown to be superior to placebo and to an active control for improved neuropsychological functioning in older adults with MDD15 and in working adults with MDD,16 and a recent human neuroimaging study found that vortioxetine has effects on the neural circuitry supporting cognitive function.17 These pro-cognitive effects were independent of vortioxetine’s effect on depressive symptoms.
The rationale for combining vortioxetine with a cognitive training program is to improve the cognitive abilities of older adults to a greater degree than with training alone.18 Vortioxetine in combination with cognitive training could robustly drive beneficial plasticity of the aging brain, resulting in significant improvement in memory and executive function of older adults, thereby remediating age-related cognitive decline. Both of these interventions have shown limited success in transfer to using cognition in everyday tasks (i.e., “functional cognition”) in healthy adults.
Therefore, we tested the efficacy of vortioxetine added to a cognitive training program, to remediate age-related cognitive decline, in a randomized clinical trial. We randomized 100 participants aged 65 and older with age-related cognitive decline to vortioxetine or placebo, while all participants also underwent computerized cognitive training for 6 months. We hypothesized that those randomized to vortioxetine in combination with cognitive training would show a greater improvement in (1) global cognitive performance on a battery of memory and executive function measures and (2) functional cognition, compared to those randomized to placebo plus cognitive training.
Methods
This study was a randomized controlled clinical trial with two parallel groups (vortioxetine vs. placebo; both groups received computerized cognitive training) and blinded outcome assessments. The study was approved by Washington University’s institutional review board. Potential participants were enrolled after providing university-approved written informed consent.
Participants
From August 2016 to July 2018, community-living adults aged 65+ were recruited through Washington University’s research participant registry, and public advertisements in the St. Louis, Missouri region.
Inclusion criterion were: age 65 and older, with age-related cognitive decline as defined by (a) self-reported cognitive dysfunction that is attributed to the aging process (in response to screening questions to the participant); (b) scoring within ±1 standard deviation of age-matched mean on the NIH Toolbox Cognition Battery fluid cognition composite at both baseline and after the two-week cognitive training lead-in. Both a lower limit (to exclude dementia and mild cognitive impairment) and upper limit (to avoid ceiling effects) were used. An upper limit of “at, but not above“ age-matched norms reflects that with typical aging, older adults have declines in the domains of memory, executive functioning, and information processing speed compared to younger cohorts (and thus have age-related cognitive decline).
Exclusion criteria were: (1) Known dementia or other clinical neurodegenerative illness (e.g., Parkinson’s disease, cerebrovascular disease) per self-report or medical records. (2) To clarify that vortioxetine pro-cognitive effects were not secondary to antidepressant or related effects, psychiatric exclusion were current major depressive episode, current or past mania or hypomania, lifetime psychotic symptoms, current alcohol or substance use disorder, and Generalized Anxiety Disorder. (3) Medical conditions that suggest shortened lifespan, such as metastatic cancer, or would prohibit safe participation such as narrow angle glaucoma (relative contraindication to vortioxetine). (4) Sensory impairment that would prevent participation. (5) Estimated IQ < 70 as measured by the Wechsler Test of Adult Reading.19 (6) Alcohol or substance abuse within 6 months. (7) Concurrent cognitive training, such as brain-training software, or other interventions expected to affect neuroplasticity. (8) Psychotropic medications or those with likely CNS effects, with the exception of low-dose trazodone at night for sleep, or any drug that interacted pharmacokinetically with vortioxetine.
Cognitive training lead-in phase
All participants received cognitive training using a well-validated program, “Scientific Brain Training Pro” (www.scientificbraintrainingpro.com).20–22 Prior to randomization, all participants received two weeks of cognitive training (with their home computer), five times weekly for 30 minutes/day. This cognitive training lead-in, prior to randomization, was a key design feature similar to augmentation designs in depression and other CNS clinical trials.23 The lead-in phase allowed for an examination of participants’ motivation and willingness/ability to undergo cognitive training. Those unable or unwilling to do so, or who reached >1 standard deviation above normal on the NIH Toolbox Cognition Battery fluid cognition composite after two weeks of cognitive training, were removed from the study prior to randomization.
Description of the cognitive training program
Cognitive training was delivered in a protocolized format, where 25 different cognitive exercises are made available for the participants. Training progresses from basic (i.e., processing speed, attention) to more complex (i.e., working memory, executive functions) cognitive functions. Each cognitive training exercise has 30 levels of difficulty, which change adaptively by increasing following consecutive trials of 80% success or better and decreasing following consecutive trials of 70% success or lower. Automated feedback is provided after each trial, and participants have access to visual displays of their progress on each task throughout their training period.
Training and fidelity of study staff, for the standardized psychoeducation and motivation of participants, was conducted by author CRB, an expert in cognitive training, following a standardized manual. Trainers (bachelor’s level individuals) met with each participant for approximately 1 hour to demonstrate the program, explain the task purpose and instructions and provide the schedule of training (a target of 150 minutes/week). This included psychoeducation to the purpose of improving cognition, which is integrated into the participant’s own profile of cognitive strengths and limitations and their self-defined goals for functioning. A manual provided participants with clear instructions, goals, and strategies for each of the exercises. The amount of effort participants put into the program was emphasized rather than level achievement.
Trainers provided motivational calls if a participant had not logged onto the program in 3+ consecutive days or if logged under 120 minutes (80% of the target number) for their week-unless known to be on vacation/family emergency/etc. Motivational calls were also utilized to encourage variety if a participant appeared to only be playing the exercises of one cognitive domain. Motivational calls primarily consisted of a reminder of the number of target minutes (150/week) and why this was important (to challenge cognition and maintain any gains achieved), as well as a reminder to contact study staff if experiencing any technical difficulties or if they had any questions. There was no significant difference in the amount of motivational calls provided between treatment groups: Mean(SD) Placebo =1.57(2.21); Vortioxetine=1.76(2.46); t (df=98)=0.41, p=0.68.
Randomization
The randomized phase was 26 weeks long, during which participants self-administered either a 10mg vortioxetine tablet daily or placebo, and all participants also received cognitive training.
The study statistician generated the random allocation sequence, pre-set to 50% allocated to each group. Enrollment of participants and allocation to study conditions were conducted by study staff; randomization assignment was concealed by using drug and placebo tablets of matching appearance. Randomization was blocked within strata using random permuted blocks.
The study team monitored and supported participants’ adherence to both the cognitive training program and the study medication. The cognitive training program has built-in adherence monitoring, and study staff also provided motivational calls. Motivational feedback included assistance with any technical difficulties, explanations of instructions and a reminder of weekly total minutes, in order to get training up to 150min/week or at least 80% of the 150-minute target.
Vortioxetine was initiated at 10mg, with no titration period. We examined medication adherence via self-report and pill count. The MD who prescribed the medication (EJL) was a board-certified geriatric psychiatrist whose only contact with participants was at study baseline during the assessment for inclusion into the study.
Schedule of assessments
Our primary outcome measure was the NIH Toolbox Cognition Battery fluid cognition composite. The NIH Toolbox Cognition Battery is a computer-based instrument assessing five cognitive subdomains and measures both crystalized and fluid cognition. Unlike tests such as the Mini-Mental State Examination or the Montreal Cognitive Assessment which screen for global cognitive impairment, the NIH Toolbox Cognition Fluid Cognition Composite is specific to fluid abilities. These abilities are used throughout life to solve problems, think and act quickly, and adapt to new situations in everyday life; and they correlate strongly and negatively with age24 and are therefore highly relevant to age-related cognitive decline. The NIH Toolbox Cognition Battery fluid cognition composite is based on five measures of global cognitive performance: The Flanker Inhibitory Control test (measuring attention and inhibitory control) requiring participants to focus on a given stimulus (an arrow) while inhibiting attention to the stimuli flanking it; the Dimensional Change Card Sort test (measuring cognitive flexibility) which asks participants to match a series of bivalent test pictures to the target pictures, switching between the dimensions of color and shape; the List Sorting Working Memory test which has participants order objects (either food or animals) in size from smallest to largest, and they are then presented with food + animals and report food in size order then animals in size order; the Picture Sequence Memory test, an episodic memory test where participants recall a series of illustrated objects and activities that increase in length and are presented in a particular order on the computer screen; and the Pattern Comparison Processing test measuring processing speed, which asks participants to discern whether two side-by-side objects are the same or not, in a 90-second period.24
This cognitive battery was carried out at the beginning of the lead-in phase (to establish a pre-training baseline and clarify inclusion into the study), beginning of the randomized phase, and at 4, 12, and 26 weeks post-randomization. We used the age-corrected standard score. As a secondary outcome, we assessed functional cognition using the UCSD Performance-Based Skills Assessment (UPSA), at randomization and at 26 weeks post-randomization. The UPSA is a validated test that uses role-plays and props that require participants to demonstrate their competence to perform everyday functioning tasks in domains such as comprehension and planning, finance, transportation, and communication. All outcomes were measured by assessors blind to treatment condition.
Safety and adverse events
We assessed all participants prior to randomization with medical history and physical examination and routine safety laboratories (electrolytes, liver/kidney function, thyrotropin). We assessed vital signs at all in-person visits and, post-randomization, assessed for study medication side effects at all visits by asking patients if they experienced any problems since last visit. We assessed for and recorded adverse events throughout the trial.
Other assessments
At baseline, we confirmed absence of psychiatric illness with the Structured Clinical Instrument for DSM-5 Axis I disorders25 and demonstrated absence of current depressive and anxiety symptoms with the Patient Health Questionnaire 9-item (PHQ-9)26 and Penn State Worry Questionnaire-Abbreviated.27
Statistical analyses
Study data were managed using REDCap.28 Analyses were performed using R version 3.5.2 and SAS 9.4. (SAS Institute Inc., Cary, North Carolina). All reported p-values are 2-tailed, with significance level for all tests at p≤0.05. The primary efficacy analysis was neurocognitive changes and the secondary efficacy analysis was functional changes.
For a simple t-test the sample size of 100 with 80% power (at 2-tailed p<0.05) allowed the detection of a moderate effect size (d=0.55) for greater cognitive improvement in the vortioxetine group compared to the placebo group. We used the intention-to-treat principle in examining vortioxetine’s efficacy: all randomized participants were included. Due to15 patients who withdrawing consent after randomization (Figure 1), PROC MIXED procedure in SAS used 376 observations (94%) for the primary analysis and 185 observations (92.5%) for secondary analysis. Our analytic strategy was a restricted maximum likelihood-based mixed model for repeated measures (MMRM) approach, where treatment-by-week interaction (from baseline to post treatment) was the key analysis in a model including weeks, treatment group and treatment-by-week interaction. When the treatment-by-week interaction was significant, contrasts were used to test comparisons of the mean change over time between two treatment groups. The mean change over time differences between treatment groups were estimated based on the least squares (LS) means for the treatment-by-week interaction in the MMRM-model. With this approach, the primary analysis was the mean change from baseline to week 4, week 12 and week 26 in NIH Toolbox Cognition Battery fluid cognition composite; the secondary outcome was the mean change from the baseline to week 26 in UPSA.
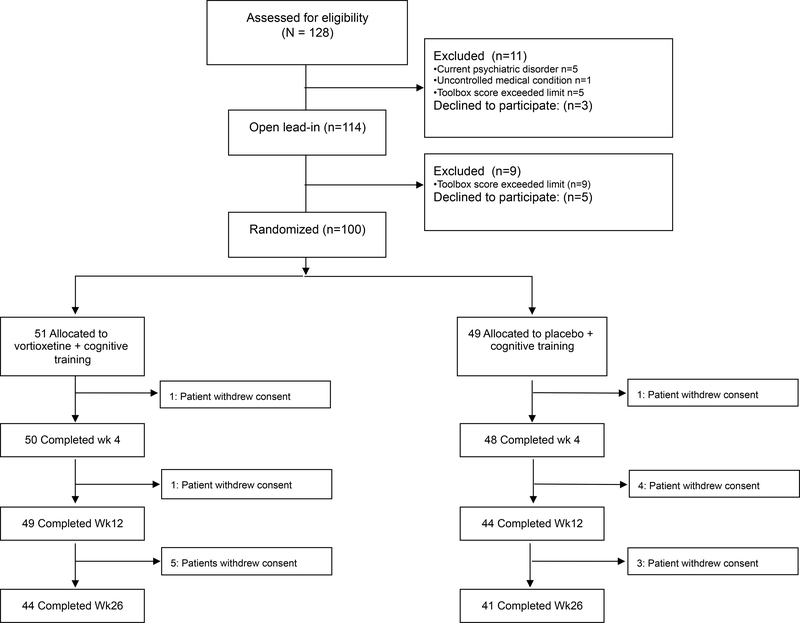
Figure 1:
CONSORT Diagram
To examine adherence to online cognition training, we used t-test to compare the mean difference in total cognition training time from week 0 to week 26 between vortioxetine and placebo. For the safety evaluation, the analysis was based on all randomized patients who had at least one self-reported adverse effects. We compared the proportions of adverse effects between vortioxetine and placebo group, using Fisher exact tests.
Results
We screened 128 age-eligible patients for study eligibility; 11 were ineligible (due to a current psychiatric disorder, current uncontrolled medical condition or a Toolbox Cognitive Battery fluid cognitive composite score that exceeded 1 SD above the age-matched norm), three refused to participate, and 114 entered the study. Of these 114 participants, five withdrew consent prior to completing the 2-week open lead-in phase and nine were excluded because they had scores above the predetermined ceiling of 1 SD above age-matched norm and were removed from the study, leaving 100 randomized (51 to vortioxetine + cognitive training; 49 to placebo + cognitive training). Table 1 shows this randomized sample’s baseline characteristics. Figure 1 shows the CONSORT diagram of study flow.
Table 1:
Baseline characteristics of randomized participants
| Characteristics | Total (n = 100) |
Placebo (n = 49) |
Vortioxetine (n = 51) |
|||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | 71.78 | 5.01 | 71.88 | 5.30 | 71.68 | 4.77 |
| Year of Schooling | 16.72 | 2.87 | 16.63 | 3.24 | 16.80 | 2.48 |
| Wechsler’s Test of Adult Reading | 112.86 | 9.70 | 112.43 | 10.15 | 113.27 | 9.32 |
| Penn State Worry Questionnaire-Abbreviated | 15.08 | 6.72 | 15.22 | 6.52 | 14.94 | 6.96 |
| Patient Health Questionnaire nine-item | 2.30 | 2.57 | 2.39 | 2.88 | 2.22 | 2.26 |
| Body Mass Index | 29.34 | 6.03 | 29.63 | 6.55 | 29.05 | 5.52 |
| Cumulative Illness Rating Scale for Geriatrics score | 7.31 | 3.22 | 7.20 | 3.11 | 7.41 | 3.34 |
| UCSD Performance-Based Skills Assessment score | 81.13 | 9.24 | 81.47 | 8.73 | 80.80 | 9.79 |
| NIH Toolbox Cognition Battery Fluid Cognition Composite | ||||||
| Pre-study | 95.74 | 13.59 | 95.61 | 12.48 | 95.86 | 14.71 |
| Baseline/Time of Randomization | 101.05 | 13.86 | 102.57 | 12.70 | 99.59 | 14.87 |
| N | % | N | % | N | % | |
| Gender | ||||||
| Female | 51 | 51.00 | 23 | 46.94 | 28 | 54.90 |
| Male | 49 | 49.00 | 26 | 53.06 | 23 | 45.10 |
| Race | ||||||
| Asian | 1 | 1.00 | 1 | 2.04 | 0 | 0.00 |
| More than one race | 3 | 3.00 | 1 | 2.04 | 2 | 3.92 |
| Black or African American | 18 | 18.00 | 9 | 18.37 | 9 | 17.65 |
| White | 78 | 78.00 | 38 | 77.55 | 40 | 78.43 |
| Ethnicity | ||||||
| Hispanic or Latino | 2 | 2.00 | 1 | 2.04 | 1 | 1.96 |
| Not Hispanic or Latino | 98 | 98.00 | 48 | 97.96 | 50 | 98.04 |
| Level of Education | ||||||
| Less than HS graduate | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 |
| HS graduate, GED or equivalent | 7 | 7.00 | 3 | 6.12 | 4 | 7.84 |
| Some college, AA or technical degree | 24 | 24.00 | 15 | 30.61 | 9 | 17.65 |
| Bachelor’s degree (BA, BS, BFA) | 18 | 18.00 | 8 | 16.33 | 10 | 19.61 |
| Some post-graduate work, Master’s degree | 41 | 41.00 | 16 | 32.65 | 25 | 49.02 |
| Professional degree (JD, MD, PhD) | 10 | 10.00 | 7 | 14.29 | 3 | 5.88 |
Primary outcome: global cognitive performance
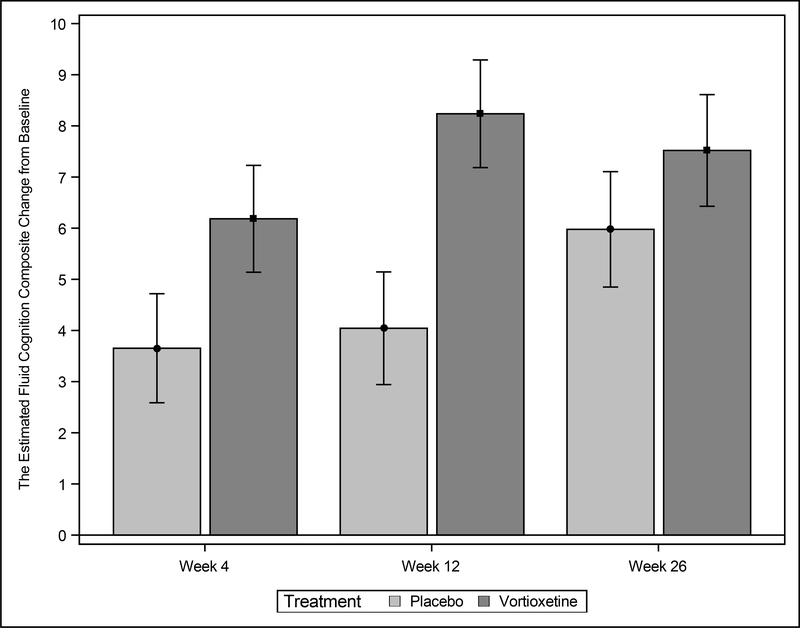
Figure 2 shows changes in the NIH Toolbox Cognition Battery fluid cognition composite, our primary outcome measure, over 26 weeks of randomized treatment, as well as during the 2-week cognitive-training only lead-in. As the figure shows, the vortioxetine + cognitive training group had greater improvement in cognitive function than cognitive training alone. Individual timepoint differences were, week 4 (week 12 timepoint (+6.18 [SE 1.04]+8.23 [SE 1.05] points vs. +4.04 [SE 1.10] points (p=0.0063) Of the three individual time points (week 4, 12, and 26), only week 12 showed a significant separation of vortioxetine from placebo. Between-group differences in the individual Toolbox Cognitive Battery tests were statistically significant only for the Dimensional Change Card Sort at week 12; these individual test statistics can be found on the online supplement.
Figure 2: Improvement in global cognitive performance with cognitive training + vortioxetine, compared to cognitive training + placebo, over 26 weeks of randomized intervention.
The figure shows greater improvement, as measured by the NIH Toolbox Cognitive Battery, in the vortioxetine + cognitive training group, which was significant in the overall model. For specific timepoints, the vortioxetine:placebo difference was significant at week 12 (+4.19 favoring vortioxetine [SE 1.52], p=0.0063, effect size [Cohen’s d]=0.57), but not at week 4 (+2.53 [SE 1.49], p=0.091, effect size=0.34) or at week 26 (+1.54 [SE 1.57], p=0.33, effect size=0.21). All reported effect sizes are with the change scores.
Secondary outcome: functional cognition
The UPSA, measuring functional cognition, showed significant improvement from baseline to week 26 in both the vortioxetine group: +3.22 (SD 1.19); and the placebo group: +1.39 (SD 1.23); the change in the two groups was not significantly different (p=0.29).
Safety and tolerability
Table 2 shows adverse event data in the vortioxetine vs. placebo groups. Nausea was significantly more common in the vortioxetine group.
Table 2:
Adverse Effects
| Placebo (n=49) |
Vortioxetine (n=51) |
p-value | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| >=1 adverse effect | 21 | 42.9 | 31 | 60.8 | 0.07 |
| Withdrew due to AE | 1 | 2.0 | 0 | 0.0 | 0.49 |
| Most common adverse effects: | |||||
| Nausea | 2 | 4.1 | 15 | 29.4 | 0.0009 |
| Viral illness | 8 | 16.3 | 9 | 17.7 | 0.86 |
| Rashes or pruritus | 3 | 6.1 | 5 | 9.8 | 0.72 |
| Constipation | 1 | 2.0 | 4 | 7.8 | 0.36 |
| Diarrhea | 3 | 6.1 | 3 | 5.9 | 1.00 |
| Dizziness | 0 | 0.0 | 3 | 5.9 | 0.24 |
| Musculoskeletal aches | 3 | 6.1 | 3 | 5.9 | 1.00 |
| Dental infections/aches | 1 | 2.0 | 3 | 5.9 | 0.62 |
| Vomiting | 0 | 0.0 | 2 | 3.9 | 0.50 |
Treatment guess
For those who were randomized to vortioxetine, the treatment guess was 63% vortioxetine (n=32) and 37% placebo (n=19). This was not different from those who were randomized to placebo, in whom the treatment guess was 67% vortioxetine (n=33) and 33% placebo (n=16).
Online Cognitive training adherence
There was no significant difference in the mean of total training time between vortioxetine and placebo groups (mean 3673.5 minutes [SD 1506.3] vs. 3457.3 minutes [SD 1376.5], p=0.4560). The supplementary file depicts cognitive training adherence over time in both groups.
Discussion
This randomized trial evaluated the effects of combining vortioxetine, a putative pro-cognitive and pro-neuroplastic medication, with computerized cognitive training, for older adults with age-related cognitive decline. Our main finding is that the combination of vortioxetine with cognitive training showed greater improvement in global cognitive performance, compared to cognitive training with placebo. The groups separated in efficacy at the week 12 timepoint only. This treatment combination was feasible and well-tolerated, and participants carried out this combined intervention with generally good adherence to both the medication and the training. We attribute the positive effects to the pharmacological pro-cognitive effects of vortioxetine, which created a beneficial increase in plasticity in key brain regions which had a synergistic effect by which cognitive training was more effective. Alternatively, the two interventions simply had additive pro-cognitive effects. These findings are important because this is the first study, to our knowledge, to demonstrate that a putative pro-cognitive drug could be combined with cognitive training in age-related cognitive decline to provide a greater improvement than can be achieved by cognitive training alone.
This clinical trial was specifically designed to test pro-cognitive benefits of a pharmacological agent when combined with cognitive training. Therefore, it included a lead-in cognitive training phase to clarify whether participants could engage in cognitive training; the subsequent randomized phase demonstrated good adherence and relatively low dropout. This lead-in phase also repeats the cognitive outcome assessment prior to randomization and therefore reduces the potential confound of practice effects which occur in treatment studies which use cognitive or other performance assessments as an outcome and are greatest between the first and second iteration of the assessment. Our primary outcome measure was a neuropsychological composite, rather than a single test, as endpoint, which provide greater statistical power for demonstrating a cognitive benefit.29 A further implication of our study design is the importance of measuring an outcome repeatedly over the intervention period. This design might be a blueprint for testing pro-cognitive drugs’ benefits in age-related cognitive decline. As such, while the sample size was determined based on a medium effect size of the vortioxetine:placebo difference for Toolbox fluid cognition composite change, at two of the three outcome timepoints (weeks 4 and 26) we observed a small effect size (Cohen’s d 0.2–0.3). For RCTs in age-related cognitive decline, a small effect size of a pro-cognitive intervention may be appropriate to expect, and so future studies may need larger sample sizes (150 or more per group) to be adequately powered.
Functional cognition, as measured by the UPSA, improved in both groups. It is unknown whether this increase in scores represented a true improvement in functional cognitive ability attributable to 26 weeks of cognitive training, or a practice effect. We found no significant interaction effects between the vortioxetine and placebo groups. One explanation of this is a true negative finding: drug augmentation of training by itself produces no transfer to function, and patients might need specific therapeutic help (known as cognitive remediation) to produce this transfer.6,8,9,22 There are other possible explanations: the study may have been underpowered to detect an effect on functional cognition; or, the UPSA may have limitations in measuring functional cognition, including outdated tests of functional abilities not used by most contemporary populations (such as using 4–1-1 to call directory assistance or utilizing a bus schedule). Thus, further study is necessary to characterize the functional benefits of cognitive training when combined with vortioxetine.
Some limitations should be noted. This study was conducted at a single site. The study is positive in terms of the overall significant finding from the mixed effect model, but the only significant individual timepoint was week 12; thus, a confirmatory study is needed which could also determine the optimal duration of treatment. It may be that the true effect is largest after three months’ treatment, or that a larger study would show similar effects at all timepoints. Further, at present we know little about the sensitivity to change or to intervention effects of the Toolbox fluid cognition composite. The study also cannot address whether vortioxetine and cognitive training have an additive or interactive effect, such as vortioxetine driving beneficial plasticity such that the training is more efficient; a different study design such as a factorial trial would be needed to examine these possibilities. Also, the study leaves unclear the functional benefits of adding vortioxetine to cognitive training. Additionally, we studied the remediation of cognitive function but we did not address the long-term implication – namely, age-related cognitive decline is a chronic, and in many cases progressive condition, with heightened risk for dementia. This raises the question: for what period of time might older adults need to continue to practice cognitive training and vortioxetine in order to continue to see benefits and slow cognitive decline? For clinical trials testing prevention of cognitive decline, large sample sizes and years-long per-protocol follow-up are needed.30 Nevertheless, the current study suggests that a longer-term study is feasible and promising, given high adherence and retention in follow-up out to 26 weeks. Other strengths were the maintenance of the blind and the good tolerability of vortioxetine, which are likely related as a drug with significant side effects would be more difficult to mask. The high tolerability of vortioxetine at this dose in older adults suggests that higher doses could be investigated to optimize the pro-cognitive effects.
In summary, cognitive training in combination with vortioxetine is efficacious for improving global cognitive function in adults aged 65+ with age-related cognitive decline. This finding is important because computerized cognitive training programs offer a feasible and scalable combination with pharmaceutical treatment for older adults. Further research is needed to replicate this finding and clarify its long-term and real-world benefits for the growing population of older adults.
Supplementary Material
Acknowledgements
this study was supported by an investigator-initiated grant from Takeda and Lundbeck. Additional funding came from R01 AG049689, UL1TR002345, and the Taylor Family Institute for Innovative Psychiatric Research and the Center for Brain Research in Mood Disorders at Washington University.
Disclosure: Dr. Lenze has received grant support from Takeda and Lundbeck (this study), Aptynx, Alkermes, Janssen, MagStim, the Patient Centered Outcomes Research Institute, the McKnight Brain Research Foundation, and Washington University School of Medicine. He has been a consultant for Janssen and Jazz Pharmaceuticals. Dr. Bowie has grant support from Takeda, Pfizer, and Lundbeck and has been a consultant for Pfizer, Boehringer Ingelhiem, and Lundbeck. The other authors have no conflicts to disclose.
Footnotes
ClinicalTrials.gov Identifier: NCT03272711
Contributor Information
Eric J. Lenze, Washington University School of Medicine -- Healthy Mind Lab, Department of Psychiatry
Angela Stevens, Washington University School of Medicine -- Healthy Mind Lab, Department of Psychiatry.
Jill D. Waring, St Louis University Department of Psychology, St Louis, MO
Vy T. Pham, Washington University School of Medicine -- Healthy Mind Lab, Department of Psychiatry
Rita Haddad, Washington University School of Medicine -- Healthy Mind Lab, Department of Psychiatry
Josh Shimony, Department of Radiology, St Louis, Missouri
J. Philip Miller, Division of Biostatistics, St Louis, Missouri.
Christopher R. Bowie, Queen’s University Department of Psychology, Kingston, Ontario
References
- 1.Bettio LEB, Rajendran L, Gil-Mohapel J. The effects of aging in the hippocampus and cognitive decline. Neurosci Biobehav Rev. 2017;79:66–86. [DOI] [PubMed] [Google Scholar]
- 2.Salthouse TA, Babcock RL. Decomposing adult age differences in working memory. Mem Cognit. 1991;27(5):763. [Google Scholar]
- 3.Dause TJ, Kirby ED. Aging gracefully: social engagement joins exercise and enrichment as a key lifestyle factor in resistance to age-related cognitive decline. Neural Regen Res. 2019;14(1):39–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hudes R, Rich JB, Troyer AK, Yusupov I, Vandermorris S. The impact of memory-strategy training interventions on participant-reported outcomes in healthy older adults: A systematic review and meta-analysis. Psychol Aging. 2019. [DOI] [PubMed] [Google Scholar]
- 5.Park DC, Bischof GN. The aging mind: neuroplasticity in response to cognitive training. Dialogues Clin Neurosci. 2013;15(1):109–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gates NJ, Rutjes AW, Di Nisio M, et al. Computerised cognitive training for maintaining cognitive function in cognitively healthy people in late life. In: Cochrane Database of Systematic Reviews; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ball K, Berch DB, Helmers KF, et al. Effects of cognitive training interventions with older adults: a randomized controlled trial. JAMA. 2002;288(18):2271–2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher M, Holland C, Subramaniam K, Vinogradov S. Neuroplasticity-based cognitive training in schizophrenia: an interim report on the effects 6 months later. Schizophr Bull. 2010;36(4):869–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mahncke HW, Kim SJ, Rose A, et al. Evaluation of a plasticity-based cognitive training program in schizophrenia: Results from the eCaesar trial. Schizophr Res. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lampit A, Hallock H, Valenzuela M. Computerized cognitive training in cognitively healthy older adults: a systematic review and meta-analysis of effect modifiers. PLoS Med. 2014;11(11):e1001756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farah MJ, Illes J, Cook-Deegan R, et al. Neurocognitive enhancement: what can we do and what should we do? Nature Reviews Neuroscience. 2004;5(5):421–425. [DOI] [PubMed] [Google Scholar]
- 12.Nierenberg AA, Loft H, Olsen CK. Treatment effects on residual cognitive symptoms among partially or fully remitted patients with major depressive disorder: A randomized, double-blinded, exploratory study with vortioxetine. J Affect Disord. 2019;250:35–42. [DOI] [PubMed] [Google Scholar]
- 13.Gold PE, Cahill L, Wenk GL. Ginkgo biloba: A Cognitive Enhancer? Psychol Sci Public Interest. 2002;3(1):2–11. [DOI] [PubMed] [Google Scholar]
- 14.Sanchez C, Asin KE, Artigas F. Vortioxetine, a novel antidepressant with multimodal activity: review of preclinical and clinical data. Pharmacol Ther. 2015;145:43–57. [DOI] [PubMed] [Google Scholar]
- 15.Mahableshwarkar AR, Zajecka J, Jacobson W, Chen Y, Keefe RS. A Randomized, Placebo-Controlled, Active-Reference, Double-Blind, Flexible-Dose Study of the Efficacy of Vortioxetine on Cognitive Function in Major Depressive Disorder. Neuropsychopharmacology. 2015;40(8):2025–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McIntyre RS, Florea I, Tonnoir B, Loft H, Lam RW, Christensen MC. Efficacy of Vortioxetine on Cognitive Functioning in Working Patients With Major Depressive Disorder. J Clin Psychiatry. 2017;78(1):115–121. [DOI] [PubMed] [Google Scholar]
- 17.Smith J, Browning M, Conen S, et al. Vortioxetine reduces BOLD signal during performance of the N-back working memory task: a randomised neuroimaging trial in remitted depressed patients and healthy controls. Mol Psychiatry. 2018;23(5):1127–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McClure MM, Graff F, Triebwasser J, et al. Guanfacine Augmentation of a Combined Intervention of Computerized Cognitive Remediation Therapy and Social Skills Training for Schizotypal Personality Disorder. Am J Psychiatry. 2019;176(4):307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holdnack HA. Wechsler Test of Adult Reading: WTAR. In. San Antonio: The Psychological Corporation; 2001. [Google Scholar]
- 20.Bowie CR, Grossman M, Gupta M, Holshausen K, Best MW. Action-based cognitive remediation for individuals with serious mental illnesses: Effects of real-world simulations and goal setting on functional and vocational outcomes. Psychiatr Rehabil J. 2017;40(1):53–60. [DOI] [PubMed] [Google Scholar]
- 21.Bowie CR, Gupta M, Holshausen K, Jokic R, Best M, Milev R. Cognitive remediation for treatment-resistant depression: effects on cognition and functioning and the role of online homework. J Nerv Ment Dis. 2013;201(8):680–685. [DOI] [PubMed] [Google Scholar]
- 22.Bowie CR, McGurk SR, Mausbach B, Patterson TL, Harvey PD. Combined cognitive remediation and functional skills training for schizophrenia: effects on cognition, functional competence, and real-world behavior. Am J Psychiatry. 2012;169(7):710–718. [DOI] [PubMed] [Google Scholar]
- 23.Trivedi MH, Kocsis JH, Thase ME, et al. REVAMP - Research Evaluating the Value of Augmenting Medication with Psychotherapy: rationale and design. Psychopharmacol Bull. 2008;41(4):5–33. [PubMed] [Google Scholar]
- 24.Heaton RK, Akshoomoff N, Tulsky D, et al. Reliability and validity of composite scores from the NIH Toolbox Cognition Battery in adults. Journal of the International Neuropsychological Society : JINS. 2014;20(6):588–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.First MB. Structured Clinical Interview for the DSM (SCID). In: Cautin RL, Lilienfeld SO, eds. The Encyclopedia of Clinical Psychology.2015. [Google Scholar]
- 26.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crittendon J, Hopko DR. Assessing worry in older and younger adults: Psychometric properties of an abbreviated Penn State Worry Questionnaire (PSWQ-A). J Anxiety Disord. 2006;20(8):1036–1054. [DOI] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Donohue MC, Sperling RA, Salmon DP, et al. The preclinical Alzheimer cognitive composite: measuring amyloid-related decline. JAMA Neurol. 2014;71(8):961–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ritchie CW, Terrera GM, Quinn TJ. Dementia trials and dementia tribulations: methodological and analytical challenges in dementia research. Alzheimers Res Ther. 2015;7(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.