The ongoing COVID-19 pandemic is the only outbreak to date in which the time from identification of a pathogen to the presentation of the first clinical trial results for a specific vaccine against the pathogen was less than 9 months. By September, 2020, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine landscape included 39 candidates being tested in clinical trials and more than 200 candidates in preclinical development.1 It is generally accepted that only vaccines can halt the spread of the pandemic virus; thus, several groups have already published interim results of phase 1/2 clinical trials of SARS-CoV-2 vaccines generated on various vaccine platforms.2, 3, 4, 5, 6 It is critical to accumulate as many clinical data on the safety and immunogenicity of SARS-CoV-2 vaccines as possible, because this infection is new to the human population and all possible short-term or long-term rare adverse events are difficult to predict. In this regard, the study by Shengli Xia and colleagues7 is timely because it provides valuable evidence for the safety and immunogenicity of a β-propiolactone inactivated aluminium hydroxide-adjuvanted whole-virion SARS-CoV-2 vaccine candidate developed by China National Biotec Group and the Beijing Institute of Biological Products (BBIBP-CorV), which was tested in randomised, double-blind, placebo-controlled phase 1/2 clinical trials in healthy individuals aged 18 years and older.
Importantly, this was the first study of an inactivated SARS-CoV-2 vaccine to include participants older than 60 years—the most vulnerable age group for this infection. In the phase 1 dose-escalating trial, the vaccine was given at a two-dose schedule at three different concentrations (2 μg, 4 μg, and 8 μg per dose) and was well tolerated in both age groups (18–59 years and ≥60 years). The older age group had lower rates of solicited adverse events than the younger adults: the overall rates of adverse events within 28 days after vaccination were 34 (47%) of 72 participants in the group aged 18–59 years, compared with 14 (19%) of 72 participants in the group aged 60 years and older. At the same time, in both age groups the vaccine was similarly immunogenic: the geometric mean anti-SARS-CoV-2 neutralising antibody titres measured by a 50% virus neutralisation assay 14 days after the booster dose were 88, 211, and 229 in the group aged 18–59 years and 81, 132, and 171 in the group aged 60 years and older for 2 μg, 4 μg, and 8 μg vaccine doses, respectively. Moreover, the authors tested cross-reactivity of the neutralising antibodies against several drifted SARS-CoV-2 isolates and showed the potential of their vaccine to protect against evolutionary diverged viruses, should they appear in circulation.
The early phase 2 trial of the BBIBP-CorV vaccine in healthy adults aged 18–59 years assessed the effect of shortening the interval between two doses from 28 days to 14 days or 21 days on the vaccine's immunogenicity. The 4 μg dose of the vaccine was the most immunogenic when given at the 21-day interval (neutralising antibody titre 283), but its immunogenicity significantly decreased when the interval was reduced to 14 days (neutralising antibody titre 170), suggesting that the interval cannot be shorter than 3 weeks.
The current study is the second to report the interim results of safety and immunogenicity of inactivated SARS-CoV-2 vaccine, with the first being the another β-propiolactone inactivated aluminium-adjuvanted whole-virion SARS-CoV-2 vaccine developed by Wuhan Institute of Biological Products.6 Both studies showed very similar levels of adverse events and neutralising antibody titres post vaccination, which indicates the reproducibility of clinical results of similar vaccine modes produced by different manufacturers. Although the use of whole-virion vaccines ensures the presence of all potential immunogenic epitopes, a critical consideration for the safety and efficacy of the vaccines is the structural stability of the major antigenic determinants. As has been shown for other inactivated vaccines, improper inactivation processes can alter the antigenic properties of epitopes, resulting in the induction of non-neutralising antibodies, which can lead to the disease enhancement rather than protection.8 With this in mind, encouraging results have been obtained when testing BBIBP-CorV in various animal models, where no disease enhancement on SARS-CoV-2 challenge was found.9 However, we need to acknowledge that for this new infection, all possible animal models have not yet been worked out for simulating antibody-dependent disease enhancement in humans. Therefore, long-term careful monitoring of quantitative and qualitative characteristics of the induced SARS-CoV-2 antibodies after vaccination with inactivated SARS-CoV-2 vaccines is critically important. In addition, more studies are needed to establish whether the inactivated SARS-CoV-2 vaccines are capable of inducing and maintaining virus-specific T-cell responses, because CD4-positive T-cell help is important for optimal antibody responses, as well as for cytotoxic CD8-positive T-cell activation, which, in turn, are crucial for viral clearance if neutralising antibody-mediated protection is incomplete.10
Finally, because the correlates of protection afforded by inactivated SARS-CoV-2 vaccines are yet to be identified, the results of a phase 3 trial of BBIBP-CorV vaccine (currently underway in Abu Dhabi, United Arab Emirates; ChiCTR2000034780), will provide information on whether this vaccine is safe and efficacious against SARS-CoV-2 infection, and for how long the protective effect is maintained.
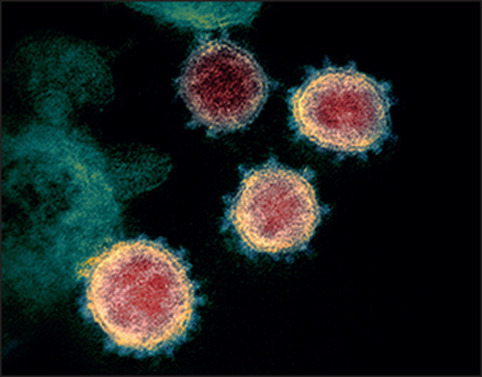
© 2020 Flickr - NIAID
Acknowledgments
We declare no competing interests.
References
- 1.Tregoning JS, Brown ES, Cheeseman HM. Vaccines for COVID-19. Clin Exp Immunol. 2020 doi: 10.1111/cei.13517. published online Sept 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jackson LA, Anderson EJ, Rouphael NG. An mRNA Vaccine against SARS-CoV-2 - Preliminary Report. N Engl J Med. 2020 doi: 10.1056/NEJMoa2022483. published online July 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu FC, Guan XH, Li YH. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2020;396:479–488. doi: 10.1016/S0140-6736(20)31605-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Folegatti PM, Ewer KJ, Aley PK. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396:467–478. doi: 10.1016/S0140-6736(20)31604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Logunov DY, Dolzhikova IV, Zubkova OV. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: two open, non-randomised phase 1/2 studies from Russia. Lancet. 2020;396:887–897. doi: 10.1016/S0140-6736(20)31866-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xia S, Duan K, Zhang Y. Effect of an inactivated vaccine against SARS-CoV-2 on safety and immunogenicity outcomes: interim analysis of 2 randomized clinical trials. JAMA. 2020;324:1–10. doi: 10.1001/jama.2020.15543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xia S, Zhang Y, Wang Y. Safety and immunogenicity of an inactivated SARS-CoV-2 vaccine, BBIBP-CorV: a randomised, double-blind, placebo-controlled, phase 1/2 trial. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30831-8. published online Oct 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanders B, Koldijk M, Schuitemaker H. Inactivated viral vaccines. In: Nunnally BK, Turula VE, Sitrin RD, editors. Vaccine analysis: strategies, principles, and control. Springer; Berlin, Heidelberg: 2015. pp. 45–80. Berlin, Heidelberg. [Google Scholar]
- 9.Wang H, Zhang Y, Huang B. Development of an inactivated vaccine candidate, BBIBP-CorV, with potent protection against SARS-CoV-2. Cell. 2020;182:713–721. doi: 10.1016/j.cell.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jeyanathan M, Afkhami S, Smaill F, Miller MS, Lichty BD, Xing Z. Immunological considerations for COVID-19 vaccine strategies. Nat Rev Immunol. 2020;20:615–632. doi: 10.1038/s41577-020-00434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


