Abstract
Background
High rate of cardiovascular disease (CVD) have been reported among patients with novel coronavirus disease (COVID-19). Meanwhile there were controversies among different studies about CVD burden in COVID-19 patients. Hence, we aimed to study CVD burden among COVID-19 patients, using a systematic review and meta-analysis.
Methods
We have systematically searched databases including PubMed, Embase, Cochrane Library, Scopus, Web of Science as well as medRxiv pre-print database. Hand searched was also conducted in journal websites and Google Scholar. Meta-analyses were carried out for Odds Ratio (OR) of mortality and Intensive Care Unit (ICU) admission for different CVDs. We have also performed a descriptive meta-analysis on different CVDs.
Results
Fifty-six studies entered into meta-analysis for ICU admission and mortality outcome and 198 papers for descriptive outcomes, including 159,698 COVID-19 patients. Results of meta-analysis indicated that acute cardiac injury, (OR: 13.29, 95% CI 7.35-24.03), hypertension (OR: 2.60, 95% CI 2.11-3.19), heart Failure (OR: 6.72, 95% CI 3.34-13.52), arrhythmia (OR: 2.75, 95% CI 1.43-5.25), coronary artery disease (OR: 3.78, 95% CI 2.42-5.90), and cardiovascular disease (OR: 2.61, 95% CI 1.89-3.62) were significantly associated with mortality. Arrhythmia (OR: 7.03, 95% CI 2.79-17.69), acute cardiac injury (OR: 15.58, 95% CI 5.15-47.12), coronary heart disease (OR: 2.61, 95% CI 1.09-6.26), cardiovascular disease (OR: 3.11, 95% CI 1.59-6.09), and hypertension (OR: 1.95, 95% CI 1.41-2.68) were also significantly associated with ICU admission in COVID-19 patients.
Conclusion
Findings of this study revealed a high burden of CVDs among COVID-19 patients, which was significantly associated with mortality and ICU admission. Proper management of CVD patients with COVID-19 and monitoring COVID-19 patients for acute cardiac conditions is highly recommended to prevent mortality and critical situations.
Keywords: COVID-19, Cardiovascular disease, Meta-analysis
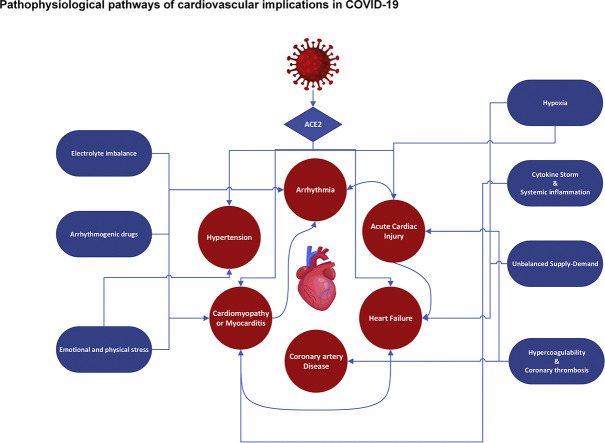
Graphical abstract
1. Introduction
Coronaviruses are enveloped positive sense single stranded RNA viruses which cause respiratory infections in human and animals ([1], [2], [3]). There were six coronaviruses known to cause infection in humans (4), including Sever Acute Respiratory Syndrome (SARS), China, 2002 (5) and Middle Eastern Respiratory Syndrome (MERS), Saudi Arabia, 2012 (6,7). The World Health Organization (WHO) reported cases of pneumonia with unknown source in Wuhan, China, December 2019 (8). Further investigations in samples of patients with respiratory infection, who were in contact with a seafood markets in Wuhan revealed a novel virus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (9). On 11th March, 2020 WHO declared the SARS-CoV-2 outbreak as a pandemic (10). It has been estimated that 1.7 billion people (22% world population) have at least one underlying condition, including cardiovascular diseases (CVD), which increases the risk of developing severe disease in case of coronavirus disease (COVID-19) (11).
There is a mutual relationships between CVD and infections (12,13), while the viral respiratory infectious diseases like influenza might increase the risk of myocardial infarction and cardiovascular events (13), underlying CVD might increase the risk of mortality among patients with infection (14).
Reports from COVID-19 disease including a large number of patients showed that fatality rate was 10.5% for CVD and 6.0% for hypertension among 72314 cases of COVID-19 (15). Studies indicated that there is an increased risk of mortality among hospitalized COVID-19 patients due to CVD ([16], [17], [18]).
Given the increasing number of COVID-19 patients besides from common clinical presentations of disease, CVD in COVID-19 infected patients are seems to be concerning (16). We aimed to assess the CVD burden of COVID-19, using a systematic review and meta-analysis method in this study.
2. Methods
2.1. Search strategy
In this study, Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline was used for study design, search strategy, screening and reporting. The research question has been developed using PECO; “P” stands for Patients, “E” as Exposure, “C” as Comparison and “O” as Outcome. PECO components were as follows: “P”; hospitalized COVID-19 patients, “E”; CVDs, “C”; no CVD, “O”; ICU admission/mortality. A systematic search was using all available MeSH terms and free keywords for “COVID-19”, “Cardiovascular Disease” “Myocardial Infarction”, “Heart Failure”, “Hypertension”, “Myocarditis”, “Arrhythmia”. Searched Databases included PubMed, Embase, Scopus, Web of Science, Cochrane Library, medRxiv pre-print database as well as Science Direct search engine. Hand search was done in publishers and journals databases including: Center for Disease Control and Prevention (CDC), The Journal of the American Medical Association (JAMA), The Lancet, The British Medical Journal (BMJ), Nature, Wiley, New England Journal of Medicine, Cambridge and Oxford. Our search included papers in all languages and there was no time limitation for publications. All original Cohort, Case Control, Cross-Sectional and Case-Series studies until 27th May 2020 were included.
2.2. Criteria for study selection
Two members of our team (F.P and A.H) selected the study independently and in case of disagreement R.A made the final decision. Studies met the following criteria included into systematic review: 1) Studies reporting characteristics of hospitalized COVID-19 patients; 2) Studies which reported any CVD in COVID-19 patients; 3) COVID-19 confirmed by Chest CT Scan, RT-PCR and hallmarks of the disease. Criteria for including studies into meta-analysis were: 1) Studies that reported CVD in COVID-19 patients admitted to ICU; 2) Studies reported the mortality rate of COVID-19 patients with underlying CVD; 3) Studies reported CVD among COVID-19 hospitalized patients. Studies were excluded if they: 1) Reported outpatients or asymptomatic COVID-19 patients; 2) Not reported CVDs; 3) Review papers, case reports, in vitro studies and animal studies.
2.3. Data extraction
Two investigators (F.P and A.H) have independently evaluated quality of publications and extracted data from included papers. In case of disagreement a supervisor (R.A) solved the issue and made the final decision. Data extraction included first author name, publication year, country and following data extracted for each group (Total Sample, ICU, Non-ICU, Mortality, Survival): Sample size, mean ± standard deviation (SD) of age, number of females, number of males, heart failure, hypertension, other cardiovascular disease, acute cardiac injury, cardiomyopathy, myocardial damage, heart palpitation, coronary heart disease, arrhythmia and acute cardiac injury. In cases that data was presented as median (interquartile range), a method by Wan et al. (19) was used to calculate mean ± SD.
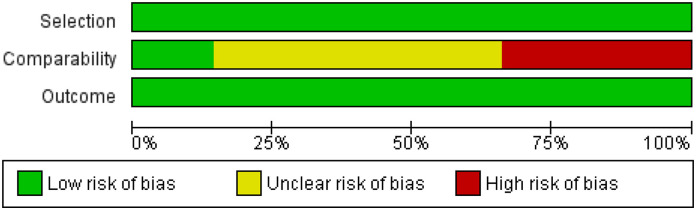
2.4. Risk of bias assessment
Newcastle-Ottawa Scale tool was used for risk of bias assessment of studies included into meta-analysis (20). Risk of bias only assessed for studies entered into meta-analysis main outcomes (ICU and mortality) of the study (Fig. 1 ).
Figure 1.
Summary of risk of bias.
2.5. Data analysis
Odds Ratio (OR) and pooled estimate prevalence rate with 95% confidence interval (CI), were calculated using statistical analysis Comprehensive Meta-Analysis (CMA) V.2. In order to assess the heterogeneity, I-square (I 2) test was used. In case of high heterogeneity (more than 50%) random effect model was used for meta-analysis. Publication bias has been assessed using Begg’s test.
3. Results
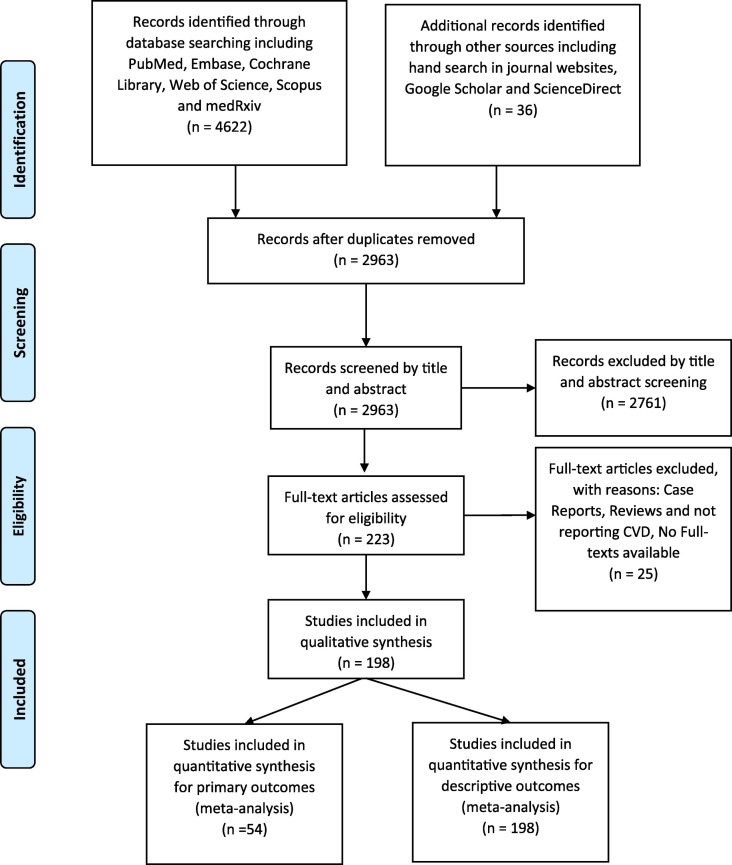
3.1. Study selection process
Our search through databases resulted in 4658 records. Duplicate records, including 1695 studies, have been excluded and after title and abstract screening, full texts of 2963 papers were assessed for eligibility. Four studies were excluded due to unavailability of the full-text. Finally, 56 papers ([21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76]) entered into meta-analysis for primary outcomes (mortality and ICU admission) and 198 papers [16,18,[21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74], [75], [76], [77], [78], [79], [80], [81], [82], [83], [84], [85], [86], [87], [88], [89], [90], [91], [92], [93], [94], [95], [96], [97], [98], [99], [100], [101], [102], [103], [104], [105], [106], [107], [108], [109], [110], [111], [112], [113], [114], [115], [116], [117], [118], [119], [120], [121], [122], [123], [124], [125], [126], [127], [128], [129], [130], [131], [132], [133], [134], [135], [136], [137], [138], [139], [140], [141], [142], [143], [144], [145], [146], [147], [148], [149], [150], [151], [152], [153], [154], [155], [156], [157], [158], [159], [160], [161], [162], [163], [164], [165], [166], [167], [168], [169], [170], [171], [172], [173], [174], [175], [176], [177], [178], [179], [180], [181], [182], [183], [184], [185], [186], [187], [188], [189], [190], [191], [192], [193], [194], [195], [196], [197], [198], [199], [200], [201], [202], [203], [204], [205], [206], [207], [208], [209], [210], [211], [212], [213], [214], [215]] for descriptive outcomes. PRISMA flow diagram for the study selection process is presented in Fig. 2 .
Figure 2.
PRISMA flow diagram.
3.2. Study characteristics
Out of 56 papers included into meta-analysis for primary outcomes, 2 studies were case-control, 1 case-cohort, 8 case series and 45 cohorts. The studies’ sample size ranged from 13 to 11,095 including 29,056 participants. One-hundred ninety-nine papers entered into meta-analysis for descriptive outcomes including 168 cohorts, 4 case-control, 4 cross-sectional, 21 case-series, 1 case-cohort. Studies sample size ranged from 10 to 27,584 including 159,698 patients.
3.3. Quality assessment
According to NOS tool for quality assessment, 56 studies earned the minimum eligibility score and entered into the meta-analysis for primary outcomes. Summary of risk of bias is presented in Fig. 2. Begg’s test showed that there was no publication bias (P = 0.7).
3.4. Mortality
The meta-analysis showed that prevalence of CVDs among COVID-19 patients with mortality were as follows: Acute Cardiac Injury (52%), Hypertension (51%), Arrhythmia (37%), Heart Failure (27%), Coronary Heart Disease (23%) and Cardiovascular Diseases (23%) (Table 1 ).
Table 1.
Meta-analysis of pooled estimate prevalence of CVDs among COVID-19 patients with mortality.
| Complication | Number of Studies | Heterogeneity |
Pooled prevalence (95% CI) | |
|---|---|---|---|---|
| I-squared, % | P-value | |||
| Acute cardiac injury | 13 | 64.33 | 0.00 | 0.52 (0.46, 0.59) |
| Arrhythmia | 4 | 89.08 | 0.00 | 0.37 (0.15, 0.67) |
| Coronary heart disease | 18 | 78.84 | 0.00 | 0.23 (0.18, 0.30) |
| Heart failure | 11 | 96.21 | 0.00 | 0.27 (0.17, 0.38) |
| Hypertension | 38 | 81.38 | 0.00 | 0.51 (0.47, 0.55) |
| Cardiovascular disease | 18 | 91.84 | 0.00 | 0.23 (0.17, 0.30) |
Results of meta-analysis indicated that presence of Acute Cardiac Injury, Coronary Artery Disease, Arrhythmia, Hypertension, Heart Failure, and Cardiovascular Disease were significantly associated with mortality in COVID-19 patients (Table 2 ).
Table 2.
Meta-analysis of OR of mortality in COVID-19 patients for CVDs.
| Complication | Number of studies | Heterogeneity |
Pooled OR (95% CI) | |
|---|---|---|---|---|
| I-Squared, % | P-value | |||
| Acute cardiac injury | 12 | 74.26 | 0.00 | 13.29 (7.35, 24.03) |
| Heart failure | 8 | 86.78 | 0.00 | 6.72 (3.34, 13.52) |
| Arrhythmia | 3 | 0.00 | 0.57 | 2.75 (1.43, 5.25) |
| Hypertension | 31 | 73.92 | 0.00 | 2.60 (2.11, 3.19) |
| Cardiovascular disease | 14 | 55.49 | 0.00 | 2.61 (1.89, 3.62) |
| Coronary heart disease | 16 | 76.20 | 0.00 | 3.78 (2.42, 5.90) |
3.5. Intensive care unit admission
Meta-analysis of pooled prevalence of cardiovascular implications in COVID-19 patients admitted to ICU showed that hypertension (43%) was the most prevalent cardiovascular complication followed by arrhythmia (33%), acute cardiac injury (33%), coronary artery diseases (20%) and heart failure (20%) (Table 3 ).
Table 3.
Meta-analysis of pooled estimate prevalence of CVDs among COVID-19 patients admitted to ICU.
| Complication | Number of studies | Heterogeneity |
Pooled prevalence (95% CI) | |
|---|---|---|---|---|
| I-squared, % | P-value | |||
| Acute cardiac injury | 8 | 51.15 | 0.04 | 0.33 (0.24, 0.43) |
| Arrhythmia | 3 | 71.88 | 0.02 | 0.33 (0.18, 0.51) |
| Coronary heart disease | 13 | 67.77 | 0.00 | 0.20 (0.15, 0.27) |
| Heart failure | 7 | 78.42 | 0.00 | 0.20 (0.09, 0.37) |
| Hypertension | 31 | 88.89 | 0.00 | 0.43 (0.37, 0.50) |
| Cardiovascular disease | 19 | 91.54 | 0.00 | 0.25 (0.16, 0.35) |
The meta-analysis on ICU outcome showed that the odds of ICU admission in COVID-19 patients is significantly associated with Acute Cardiac Injury, Arrhythmia, Coronary Heart Disease, Cardiovascular Disease and Hypertension. Heart Failure was not significantly associated with ICU admission in COVID-19 however, the effect size was considerable (Table 4 ).
Table 4.
Meta-analysis of OR for ICU admission outcome among COVID-19 patients.
| Complication | Number of studies | Heterogeneity |
Prevalence (95% CI) | |
|---|---|---|---|---|
| I-Square (%) | P-value | |||
| Coronary heart disease | 60 | 93.92 | 0.00 | 0.10 (0.09, 0.12) |
| Cardiovascular and cerebrovascular disease | 16 | 94.97 | 0.00 | 0.14 (0.09, 0.22) |
| Cardiovascular disease | 87 | 95.73 | 0.00 | 0.11 (0.09, 0.12) |
| Arrhythmia | 17 | 91.17 | 0.00 | 0.11 (0.07, 0.16) |
| Acute cardiac injury | 28 | 92.35 | 0.00 | 0.16 (0.13, 0.19) |
| Cardiomyopathy | 4 | 85.25 | 0.00 | 0.07 (0.01, 0.27) |
| Heart failure | 31 | 99.11 | 0.00 | 0.10 (0.07, 0.13) |
| Myocardial damage | 3 | 94.49 | 0.00 | 0.20 (0.06, 0.49) |
| Hypertension | 158 | 97.97 | 0.00 | 0.29 (0.27, 0.31) |
| Heart palpation | 6 | 85.06 | 0.00 | 0.06 (0.03, 0.13) |
| Heart valve disease | 3 | 87.00 | 0.00 | 0.09 (0.02, 0.36) |
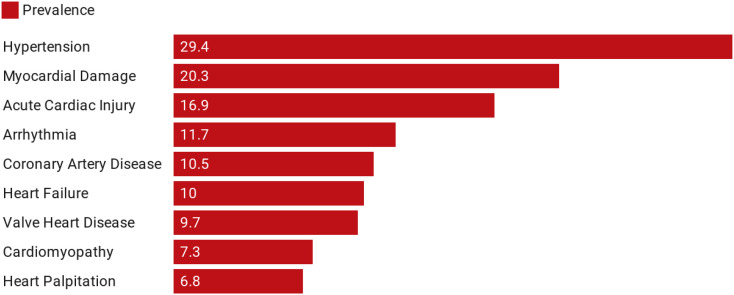
3.6. Cardiovascular complications
One-hundred ninety-eight studies have investigated for cardiovascular complications in the COVID-19 patients. Pooled prevalence of cardiovascular complications observed among patients with COVID-19 included hypertension (29%), cardiovascular and cerebrovascular disease (14%), heart failure (10%), acute cardiac injury (16%), coronary heart disease (10%), myocardial damage (20%), cardiovascular disease (11%), arrhythmia (11%), cardiomyopathy (7%), heart palpitation (6%) and heart valve disease (9%) (Table 5 , Fig. 3 ).
Table 5.
Pooled prevalence for cardiovascular complications among COVID-19 patients.
| Complication | Number of studies | Heterogeneity |
Pooled OR (CI 95%) | |
|---|---|---|---|---|
| I-squared, % | P-value | |||
| Acute cardiac injury | 6 | 61.73 | 0.02 | 15.58 (5.15, 47.12) |
| Arrhythmia | 2 | 32.22 | 0.22 | 7.03 (2.79, 17.69) |
| Coronary heart disease | 8 | 77.65 | 0.00 | 2.61 (1.09, 6.26) |
| Hypertension | 21 | 67.62 | 0.00 | 1.95 (1.41, 2.68) |
| Cardiovascular diseases | 12 | 71.01 | 0.00 | 3.11 (1.59, 6.09) |
Figure 3.
Prevalence of cardiovascular complications among COVID-19 patients.
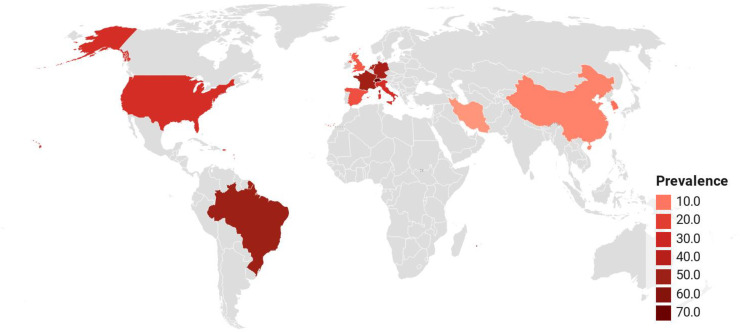
We have also analyzed pooled prevalence of cardiovascular disease in COVID-19 patient in different countries. Results of meta-analysis were as follows: Brazil (50.0%), China (7.8%), France (48.0%), Germany (45.5%), Iran (4.4%), Italy (24.7%), Netherlands (44.0%), South Korea (11.2%), Spain (16.9%), Switzerland (71.4%), United Kingdome (15.1%), and United States (24.4%) (Fig. 4 ).
Figure 4.
Cardiovascular disease burden among COVID-19 patients in different countries.
4. Discussion
The results of this meta-analysis indicated cardiovascular implications including acute cardiac injury, arrhythmia, coronary heart disease, hypertension and cardiovascular diseases were significantly associated with COVID-19 patient’s admission to the ICU. Comparing pooled estimate of OR for CVDs showed odds of ICU admission was significantly higher in acute cardiac injury and arrhythmia than hypertension, but there was no significant difference between other cardiovascular implications. Investigations have shown that mortality in patients with acute cardiac injury was significantly higher than coronary artery disease, arrhythmia, and hypertension. Comparing estimated frequency of different cardiovascular complications including acute cardiac injury, arrhythmia, cardiomyopathy, coronary heart disease, heart palpitation, hypertension, myocardial damage, heart failure and other cardiovascular diseases did not show any significant difference among them.
Cardiovascular complications have been previously reported in previous respiratory infections with similar etiology and their condition affects severity of the disease (17,216); so that even hospitalization for pneumonia is associated with long-term and short-term risk of CVD (12). Viral infections cause imbalance between cardiac supply and demand and increase in systemic inflammation. Therefore patients with pre-existing CVD have higher risks for acute cardiac conditions (217), thrombosis (218), infection, and develop severe conditions during the infection (219).
Acute myocardial injury was significantly associated with both ICU admission and mortality. There were several etiologies proposed for acute myocardial injury in these patients. The first possible mechanism is myocardial injury caused by cytokine storm as the results of systematic inflammation mediated by pathologic T-cells ([220], [221], [222]). Study by Chen et al. (25) showed elevated myocardial injury biomarkers including NT-proBNP, cTnI and hs-CRP were significantly correlated with COVID-19 severity. The second possible explanation is the imbalance between supply and demand caused by systemic infection along with hypoxia caused by respiratory infection, which lead to acute myocardial injury (220,222). There are evidences that shows SARS-CoV-2 binds to human angiotensin converting enzyme-2 (ACE2) to infect the cells (223), which being highly expressed in lungs and heart. The binding of SARS-CoV-2 to ACE2 in heart can results acute myocardial injury (220,224). COVID-19 has been associated with thrombotic events and coagulations disorders (225), which might lead to hypercoagulability and coronary thrombosis results in acute myocardial infarction (220,222).
SARS-CoV-2 binding to ACE2 causes activation of renin-angiotensin system and its complications including hypertension, heart failure, and atherosclerosis (219,226,227) as we resulted in our meta-analysis. These data could also suggest a reason for high prevalence of hypertension in our pooled estimate. Underlying CVDs like hypertension could higher the risk of infection and developing more severe symptoms in COVID-19 patients [219]. We showed in our meta-analysis that hypertension was significantly associated with ICU admission and mortality; therefore blood pressure control could be potentially beneficial to reduce disease burden (228). Using Angiotensin Receptor Blockers (ARBs) and ACE inhibitors in order to control hypertension have raised question in the era of the COVID-19 pandemic. Studies suggested that using ARBs and ACE inhibitors could potentially be harmful as they can cause up-regulation of ACE2, SARS-CoV-2 receptor, and lung injury (228,229); so, they should be carefully considered in COVID-19 patients [219]. This meta-analysis also indicated that mean age of COVID-19 patients admitted to ICU was significantly higher that non-ICU. An explanation to this condition by AlGhatrif et al. (230) suggested that elderly patients with hypertension are more likely to have down-regulation of ACE2 expression, due to viral binding, and up-regulated angiotensin II, which exaggerates pro-inflammatory condition, predisposing them to severe conditions and mortality (231).
Arrhythmia was significantly associated with ICU admission and mortality in our meta-analysis. There are pathophysiological mechanisms suggested for arrhythmia among COVID-19 patients; however, whether these patients had pre-existing arrhythmia or secondary to COVID-19 remains unknown (232). First, as any systematic infection COVID-19 can cause electrolyte imbalance, especially hypokalemia (233), which might contribute to arrhythmia in susceptible patients (220). Second, as we have discussed earlier myocardial injury has been an important subject in COVID-19 patients. It has been suggested that myocardial damage can be potentially triggers arrhythmia (234,235). Third, pharmacological therapies prescribed for these patients can be potential risk factors for arrhythmia. Hydroxychloroquine, as one the most common drugs which had been used in COVID-19, can triggers QT prolongation (235,236). Fourth, arrhythmia could also occur secondary to myocarditis by disrupting cardiomyocyte membrane and electrolyte imbalance, myocardial fibrosis, proinflammatory cytokines and edema of pericardium (232).
In our meta-analysis the prevalence of heart palpitation was relatively high and it has been reported as one the initial symptoms of the disease [133]. National Health Commission of China (NHC) reported that some patients have presented with heart palpitations and chest tightness instead of cough and fever as initial symptoms of COVID-19 [219]; so, heart palpitations in outpatients setting needs to carefully considered as potential symptom of COVID-19.
Heart failure was significantly associated with mortality in our meta-analysis, ranked after acute cardiac injury. The incidence of heart failure might be as the consequence of myocardial injury or myocarditis (237), which has been previously discussed. Increasing systemic metabolic demand as the results of systemic infection could also exacerbate previous stable heart failure (220). Right heart failure and pulmonary hypertension should be also carefully considered in patients with acute respiratory distress syndrome (ARDS) and parenchymal lung disease (234).
Cardiomyopathy has been also observed in COVID-19 patients in various forms. Takotsubo syndrome (TTS) or stress cardiomyopathy, characterized by transient left ventricular dysfunction, is triggered by emotional and physical stresses following to natural disasters (238), like COVID-19 pandemic. There were number of studies reported TTS in COVID-19 patients ([239], [240], [241], [242], [243]). Mechanism of stress cardiomyopathy in COVID-19 patients might be due to emotional distress caused by pandemic along with inflammatory and metabolic distress (241). Inflammatory cardiomyopathy or myocarditis was previously described in viral infections (244) as well as COVID-19 (245,246). Cardiomyocytes expresses ACE2 which is the receptor for SARS-CoV-2, so this virus could infects human heart which can even exacerbate in case of heart failure (232).
Coronary artery disease was significantly associated with mortality of COVID-19 patients in our study. In patients with previous coronary artery disease, inflammatory state and hemodynamic changes in infection can potentially increase the risk of plaque rupture (18,234,247). Coagulopathy in COVID-19 patients (225) can also cause acute coronary syndrome in these patients.
We have discussed cardiovascular implications among COVID-19 patients. Cardiovascular diseases have significant role in the outcome of COVID-19 patients. Therefore, careful consideration and management of cardiovascular disease, from diagnosis to bedside, among COVID-19 patients are necessary. Results of this study could help policy makers, physicians and healthcare workers in front line to make evidence-based decisions and reduce the mortality and morbidity of this 21st century pandemic.
Limitation of this study was high heterogeneity of studies in population. Compounding effects of other co-morbidities in ICU admission and mortality was not being considered. It is possible that other co-morbidities related to respiratory system, renal system and gastrointestinal system affects patient’s condition. Cardiovascular implications could be pre-existing in patients or either developed by the infection; so, we could not determine the casual relationship. However, given the burden and vital role of CVDs the importance does not differ. We only included studies of hospitalized adult COVID-19 patients and asymptomatic and outpatients are excluded. Data regarding to cardiovascular diseases in COVID-19 patients in some countries were missing.
5. Conclusion
In conclusion, CVD have a significant role in disease severity and mortality of COVID-19 patients. Hypertension, acute cardiac injury, coronary heart diseases in COVID-19 patient needs to be carefully monitored and managed in case of acute conditions. Other cardiovascular implications, including arrhythmia and heart failure also need to be considered since they can be fatal. Therefore, careful consideration and management of cardiovascular disease among these patients are necessary. Results of this study could help policy makers, physicians and healthcare workers in front line to make evidence-based decisions and reduce the mortality and morbidity of this 21st century pandemic.
Ethics approval and consent to participate
This study has been approved by the Ethics Committee of Mazandaran University of Medical Sciences (IR.MAZUMS.REC.1399.097).
Consent for publication
Not applicable.
Funding
Student Research Committee, Mazandaran University of Medical Sciences (code number: 7396).
Declaration of Competing Interest
None of authors have declared any conflicts of interest.
Acknowledgements
We acknowledge Student Research Committee of Mazandaran University of Medical Sciences for supporting this project (code number: 7396).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajem.2020.10.022.
Appendix A. Supplementary data
Supplementary Fig. S1: Meta-analysis of prevalence of cardiovascular diseases among COVID-19 patients with mortality
Supplementary Fig. S2: Meta-analysis of odds ratio of mortality among COVID-19 patients with cardiovascular diseases
Supplementary Fig. S3: Meta-analysis of prevalence of cardiovascular diseases among COVID-19 patients admitted to ICU
Supplementary Fig. S4: Meta-analysis of odds Ratio of ICU admission among COVID-19 patients with cardiovascular diseases
Supplementary Fig. S5: Meta-analysis of prevalence of cardiovascular complications among COVID-19 patients
Supplementary Table S1: Characteristics of studies included into meta-analysis
References
- 1.Cheng V.C.C., Lau S.K.P., Woo P.C.Y., Yuen K.Y. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin Microbiol Rev. 2007;20(4):660–694. doi: 10.1128/CMR.00023-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saghazadeh A., Rezaei N. Immune-epidemiological parameters of the novel coronavirus - a perspective. Expert Rev Clin Immunol. 2020;16(5):465–470. doi: 10.1080/1744666X.2020.1750954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Su S., Wong G., Shi W., Liu J., Lai A.C.K., Zhou J., et al. Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol. 2016;24(6):490–502. doi: 10.1016/j.tim.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peiris J., Guan Y., Yuen K. Severe acute respiratory syndrome. Nat Med. 2004;10(12):S88–S97. doi: 10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaki A.M., Van Boheemen S., Bestebroer T.M., Osterhaus A.D., Fouchier R.A. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 7.Lotfi M., Hamblin M.R., Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254–266. doi: 10.1016/j.cca.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . World Health Organization (WHO); 2020. Pneumonia of Unknown Cause–China. Emergencies Preparedness, Response, Disease Outbreak News. [Google Scholar]
- 9.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization . 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Geneva, Switzerland. [Google Scholar]
- 11.Clark A., Jit M., Warren-Gash C., Guthrie B., Wang H.H.X., Mercer S.W., et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020;8:e1003–e1017. doi: 10.1016/S2214-109X(20)30264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Corrales-Medina V.F., Alvarez K.N., Weissfeld L.A., Angus D.C., Chirinos J.A., Chang C.-C.H., et al. Association between hospitalization for pneumonia and subsequent risk of cardiovascular disease. JAMA. 2015;313(3):264–274. doi: 10.1001/jama.2014.18229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Madjid M., Miller C.C., Zarubaev V.V., Marinich I.G., Kiselev O.I., Lobzin Y.V., et al. Influenza epidemics and acute respiratory disease activity are associated with a surge in autopsy-confirmed coronary heart disease death: results from 8 years of autopsies in 34,892 subjects. Eur Heart J. 2007;28(10):1205–1210. doi: 10.1093/eurheartj/ehm035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dhainaut J.-F., Claessens Y.-E., Janes J., Nelson D.R. Underlying disorders and their impact on the host response to infection. Clin Infect Dis. 2005;41(Supplement_7):S481–S489. doi: 10.1086/432001. [DOI] [PubMed] [Google Scholar]
- 15.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 16.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T., et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madjid M., Safavi-Naeini P., Solomon S.D., Vardeny O. Potential effects of coronaviruses on the cardiovascular system: a review. JAMA Cardiol. 2020;5:831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 18.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F., et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 21.Argenziano M.G., Bruce S.L., Slater C.L., Tiao J.R., Baldwin M.R., Barr R.G., et al. Characterization and clinical course of 1000 Patients with COVID-19 in New York: retrospective case series. medRxiv. 2020 doi: 10.1136/bmj.m1996. (2020.04.20.20072116) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bonetti G., Manelli F., Patroni A., Bettinardi A., Borrelli G., Fiordalisi G., et al. Laboratory predictors of death from coronavirus disease 2019 (COVID-19) in the area of Valcamonica, Italy. Clin Chem Lab Med. 2020;58:100–1105. doi: 10.1515/cclm-2020-0459. [DOI] [PubMed] [Google Scholar]
- 23.Cao J., Hu X., Cheng W., Yu L., Tu W.J., Liu Q. Clinical features and short-term outcomes of 18 patients with corona virus disease 2019 in intensive care unit. Intensive Care Med. 2020;46(5):851–853. doi: 10.1007/s00134-020-05987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cao M., Zhang D., Wang Y., Lu Y., Zhu X., Li Y., et al. Clinical features of patients infected with the 2019 novel coronavirus (COVID-19) in Shanghai, China. medRxiv. 2020 [Google Scholar]
- 25.Chen C., Yan J., Zhou N., Zhao J., Wang D. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:E008. doi: 10.3760/cma.j.cn112148-20200225-00123. [DOI] [PubMed] [Google Scholar]
- 26.Chen C., Yi Z.J., Chang L., Shuo H.Z., Ming Z., Pei T., et al. The characteristics and death risk factors of 132 COVID-19 pneumonia patients with comorbidities: a retrospective single center analysis in Wuhan, China. medRxiv. 2020 (2020.05.07.20092882) [Google Scholar]
- 27.Chen R., Liang W., Jiang M., Guan W., Zhan C., Wang T., et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020;158:97–105. doi: 10.1016/j.chest.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen T., Wu D., Chen H., Yan W., Yang D., Chen G., et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368 doi: 10.1136/bmj.m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen X., Zheng F., Qing Y., Ding S., Yang D., Lei C., et al. Epidemiological and clinical features of 291 cases with coronavirus disease 2019 in areas adjacent to Hubei, China: a double-center observational study. medRxiv. 2020 [Google Scholar]
- 30.Conversano A., Melillo F., Napolano A., Fominskiy E., Spessot M., Ciceri F., et al. RAAs inhibitors and outcome in patients with SARS-CoV-2 pneumonia. A case series study. Hypertension. 2020;76:e10–e12. doi: 10.1161/HYPERTENSIONAHA.120.15312. [DOI] [PubMed] [Google Scholar]
- 31.Deng Q., Hu B., Zhang Y., Wang H., Zhou X., Hu W., et al. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. Int J Cardiol. 2020;311:116–121. doi: 10.1016/j.ijcard.2020.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deng Y., Liu W., Liu K., Fang Y.Y., Shang J., Zhou L., et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin Med J (Engl) 2020;133:1261–1267. doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Du R.H., Liang L.R., Yang C.Q., Wang W., Cao T.Z., Li M., et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J. 2020;55(5) doi: 10.1183/13993003.00524-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Du R.H., Liu L.M., Yin W., Wang W., Guan L.L., Yuan M.L., et al. Hospitalization and critical care of 109 decedents with COVID-19 pneumonia in Wuhan, China. Ann Am Thorac Soc. 2020;17:839–846. doi: 10.1513/AnnalsATS.202003-225OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ebinger J.E., Achamallah N., Ji H., Claggett B.L., Sun N., Botting P., et al. Pre-existing traits associated with Covid-19 illness severity. medRxiv. 2020 doi: 10.1371/journal.pone.0236240. (2020.04.29.20084533) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fan H., Zhang L., Huang B., Zhu M., Zhou Y., Zhang H., et al. Cardiac injuries in patients with coronavirus disease 2019: not to be ignored. Int J Infect Dis. 2020;96:294–297. doi: 10.1016/j.ijid.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferguson J., Rosser J.I., Quintero O., Scott J., Subramanian A., Gumma M., et al. Characteristics and outcomes of coronavirus disease patients under nonsurge conditions, Northern California, USA, March-April 2020. Emerg Infect Dis. 2020;26(8) doi: 10.3201/eid2608.201776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fu L., Fei J., Xiang H.-X., Xiang Y., Tan Z.-X., Li M.-D., et al. Influence factors of death risk among COVID-19 patients in Wuhan, China: a hospital-based case-cohort study. medRxiv. 2020 [Google Scholar]
- 39.Gagiannis D., Steinestel J., Hackenbroch C., Hannemann M., Umathum V.G., Gebauer N., et al. COVID-19-induced acute respiratory failure: an exacerbation of organ-specific autoimmunity? medRxiv. 2020 (2020.04.27.20077180) [Google Scholar]
- 40.Gaibazzi N., Martini C., Mattioli M., Tuttolomondo D., Guidorossi A., Suma S., et al. Lung disease severity, coronary artery calcium, coronary inflammation and mortality in coronavirus disease 2019. medRxiv. 2020 (2020.05.01.20087114) [Google Scholar]
- 41.Ge H., Zhu M., Du J., Zhou Y., Wang W., Zhang W., et al. Cardiac structural and functional characteristics in patients with coronavirus disease 2019: a serial echocardiographic study. medRxiv. 2020 (2020.05.12.20095885) [Google Scholar]
- 42.Gu T., Chu Q., Yu Z., Fa B., Li A., Xu L., et al. History of coronary heart disease increases the mortality rate of COVID-19 patients: a nested case-control study. medRxiv. 2020 doi: 10.1136/bmjopen-2020-038976. (2020.03.23.20041848) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guan W.J., Liang W.H., Zhao Y., Liang H.R., Chen Z.S., Li Y.M., et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5) doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.He X., Lai J., Cheng J., Wang M., Liu Y., Xiao Z., et al. Impact of complicated myocardial injury on the clinical outcome of severe or critically ill COVID-19 patients. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48:E011. doi: 10.3760/cma.j.cn112148-20200228-00137. [DOI] [PubMed] [Google Scholar]
- 45.Hong K.S., Lee K.H., Chung J.H., Shin K.C., Choi E.Y., Jin H.J., et al. Clinical features and outcomes of 98 patients hospitalized with SARS-CoV-2 infection in Daegu, South Korea: a brief descriptive study. Yonsei Med J. 2020;61(5):431–437. doi: 10.3349/ymj.2020.61.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ketcham S.W., Adie S.K., Malliett A., Abdul-Aziz A.A., Bitar A., Grafton G., et al. Coronavirus disease-2019 in heart transplant recipients in Southeastern Michigan: a case series. J Card Fail. 2020;26:457–461. doi: 10.1016/j.cardfail.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lagi F., Piccica M., Graziani L., Vellere I., Botta A., Tilli M., et al. Early experience of an infectious and tropical diseases unit during the coronavirus disease (COVID-19) pandemic, Florence, Italy, February to March 2020. Eurosurveillance. 2020;25(17) doi: 10.2807/1560-7917.ES.2020.25.17.2000556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Levy T.J., Richardson S., Coppa K., Barnaby D.P., McGinn T., Becker L.B., et al. Estimating survival of hospitalized COVID-19 patients from admission information. medRxiv. 2020 (2020.04.22.20075416) [Google Scholar]
- 50.Li K., Wu J., Wu F., Guo D., Chen L., Fang Z., et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Invest Radiol. 2020;55:327–331. doi: 10.1097/RLI.0000000000000672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu Q., Fang X., Tokuno S., Chung U., Chen X., Dai X., et al. Prediction of the clinical outcome of COVID-19 patients using T lymphocyte subsets with 340 cases from Wuhan, China: a retrospective cohort study and a web visualization tool. medRxiv. 2020 (2020.04.06.20056127) [Google Scholar]
- 52.Lodigiani C., Iapichino G., Carenzo L., Cecconi M., Ferrazzi P., Sebastian T., et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ni W., Yang X., Liu J., Bao J., Li R., Xu Y., et al. Acute myocardial injury at hospital admission is associated with all-cause mortality in COVID-19. J Am Coll Cardiol. 2020;76:124–125. doi: 10.1016/j.jacc.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nikpouraghdam M., Jalali Farahani A., Alishiri G., Heydari S., Ebrahimnia M., Samadinia H., et al. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: a single center study. J Clin Virol. 2020;127:104378. doi: 10.1016/j.jcv.2020.104378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peng Y., Meng K., Guan H., Leng L., Zhu R., Wang B., et al. Clinical characteristics and outcomes of 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48 doi: 10.3760/cma.j.cn112148-20200220-00105. [DOI] [PubMed] [Google Scholar]
- 56.Rentsch C.T., Kidwai-Khan F., Tate J.P., Park L.S., King J.T., Skanderson M., et al. Covid-19 testing, hospital admission, and intensive care among 2,026,227 United States veterans aged 54-75 years. medRxiv. 2020 (2020.04.09.20059964) [Google Scholar]
- 57.Sapey E., Gallier S., Mainey C., Nightingale P., McNulty D., Crothers H., et al. Ethnicity and risk of death in patients hospitalised for COVID-19 infection: an observational cohort study in an urban catchment area. medRxiv. 2020 doi: 10.1136/bmjresp-2020-000644. (2020.05.05.20092296) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shekhar R., Upadhyay S., Sheikh A., Atencio J., Kapuria D. Early experience with COVD-19 patients at tertiary care teaching hospital in southwestern United states. medRxiv. 2020 doi: 10.1080/23744235.2020.1774645. (2020.05.15.20094284) [DOI] [PubMed] [Google Scholar]
- 59.Shi S., Qin M., Cai Y., Liu T., Shen B., Yang F., et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41:2070–2079. doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sun H., Ning R., Tao Y., Yu C., Deng X., Zhao C., et al. Risk factors for mortality in 244 older adults with COVID-19 in Wuhan, China: a retrospective study. J Am Geriatr Soc. 2020;68:e19–e23. doi: 10.1111/jgs.16533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tai S., Tang J., Yu B., Tang L., Wang Y., Zhang H., et al. Association between cardiovascular burden and requirement of intensive care among patients with mild COVID-19. medRxiv. 2020 doi: 10.1155/2020/9059562. (2020.05.25.20111757) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wang D., Yin Y., Hu C., Liu X., Zhang X., Zhou S., et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Crit Care. 2020;24(1) doi: 10.1186/s13054-020-02895-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang K., Zuo P., Liu Y., Zhang M., Zhao X., Xie S., et al. Clinical and laboratory predictors of in-hospital mortality in patients with COVID-19: a cohort study in Wuhan, China. Clin Infect Dis. 2020:1–10. doi: 10.1093/cid/ciaa538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang L., He W., Yu X., Hu D., Bao M., Liu H., et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80(6):639–645. doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang L., He W.B., Yu X.M., Liu H.F., Zhou W.J., Jiang H. Prognostic value of myocardial injury in patients with COVID-19. Zhonghua Yan Ke Za Zhi. 2020;56(0):E009. doi: 10.3760/cma.j.cn112148-20200313-00202. [DOI] [PubMed] [Google Scholar]
- 67.Yang X., Yu Y., Xu J., Shu H., Liu H., Wu Y., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yao Q., Wang P., Wang X., Qie G., Meng M., Tong X., et al. Retrospective study of risk factors for severe SARS-Cov-2 infections in hospitalized adult patients. Pol Arch Intern Med. 2020;130:390–399. doi: 10.20452/pamw.15312. [DOI] [PubMed] [Google Scholar]
- 69.Zhang F., Yang D., Li J., Gao P., Chen T., Cheng Z., et al. Myocardial injury is associated with in-hospital mortality of confirmed or suspected COVID-19 in Wuhan, China: a single center retrospective cohort study. medRxiv. 2020 [Google Scholar]
- 70.Zhang J., Ding D., Cao C., Zhang J., Huang X., Fu P., et al. Myocardial characteristics as the prognosis for COVID-19 patients. medRxiv. 2020 (2020.05.06.20068882) [Google Scholar]
- 71.Zhang J., Lu S., Wang X., Jia X., Li J., Lei H., et al. Do underlying cardiovascular diseases have any impact on hospitalised patients with COVID-19? Heart. 2020;106:1148–1153. doi: 10.1136/heartjnl-2020-316909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhou X., Zhu J., Xu T. Clinical characteristics of coronavirus disease 2019 (COVID-19) patients with hypertension on renin-angiotensin system inhibitors. Clin Exp Hypertens. 2020:1–5. doi: 10.1080/10641963.2020.1764018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zou X., Li S., Fang M., Hu M., Bian Y., Ling J., et al. Acute physiology and chronic health evaluation II score as a predictor of hospital mortality in patients of coronavirus disease 2019. Crit Care Med. 2020;48:e657–e665. doi: 10.1097/CCM.0000000000004411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zheng Y., Xu H., Yang M., Zeng Y., Chen H., Liu R., et al. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J Clin Virol. 2020;127:104366. doi: 10.1016/j.jcv.2020.104366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Li J., Song H., Hu Z. Clinical features and outcomes of 2019 novel coronavirus-infected patients with cardiac injury. medRxiv. 2020 [Google Scholar]
- 77.Arentz M., Yim E., Klaff L., Lokhandwala S., Riedo F.X., Chong M., et al. Characteristics and outcomes of 21 critically Ill patients with COVID-19 in Washington State. JAMA. 2020;323(16):1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Barrasa H., Rello J., Tejada S., Martín A., Balziskueta G., Vinuesa C., et al. SARS-CoV-2 in Spanish intensive care units: early experience with 15-day survival in Vitoria. Anaesthesia Crit Care Pain Med. 2020;39:553–561. doi: 10.1016/j.accpm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Benetti E., Giliberti A., Emiliozzi A., Velentino F., Bergantini L., Fallerini C., et al. Clinical and molecular characterization of COVID-19 hospitalized patients. medRxiv. 2020 doi: 10.1371/journal.pone.0242534. (2020.05.22.20108845) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bhayana R., Som A., Li M.D., Carey D.E., Anderson M.A., Blake M.A., et al. Abdominal imaging findings in COVID-19: preliminary observations. Radiology. 2020:201908. doi: 10.1148/radiol.2020201908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bradley B.T., Maioli H., Johnston R., Chaudhry I., Fink S.L., Xu H., et al. Histopathology and ultrastructural findings of fatal COVID-19 infections. medRxiv. 2020 doi: 10.1016/S0140-6736(20)31305-2. (2020.04.17.20058545) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Brat G.A., Weber G.M., Gehlenborg N., Avillach P., Palmer N.P., Chiovato L., et al. International electronic health record-derived COVID-19 clinical course profiles: the 4CE consortium. medRxiv. 2020 doi: 10.1038/s41746-020-00308-0. (2020.04.13.20059691) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bravi F., Flacco M.E., Carradori T., Volta C.A., Cosenza G., De Togni A., et al. Predictors of severe or lethal COVID-19, including angiotensin converting enzyme inhibitors and angiotensin II receptor blockers, in a sample of infected Italian citizens. medRxiv. 2020 doi: 10.1371/journal.pone.0235248. (2020.05.21.20109082) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Buckner F.S., McCulloch D.J., Atluri V., Blain M., McGuffin S.A., Nalla A.K., et al. Clinical features and outcomes of 105 hospitalized patients with COVID-19 in Seattle, Washington. Clin Infect Dis. 2020:1–7. doi: 10.1093/cid/ciaa632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cai Q., Chen F., Wang T., Luo F., Liu X., Wu Q., et al. Obesity and COVID-19 severity in a designated hospital in Shenzhen, China. Diabetes Care. 2020;43:1392–1398. doi: 10.2337/dc20-0576. [DOI] [PubMed] [Google Scholar]
- 86.Cai Q., Huang D., Ou P., Yu H., Zhu Z., Xia Z., et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy. 2020;75:1742–1752. doi: 10.1111/all.14309. [DOI] [PubMed] [Google Scholar]
- 87.Casas Rojo J.M., Antón Santos J.M., Millán Núñez-Cortés J., Lumbreras Bermejo C., Ramos Rincón J.M., Roy-Vallejo E., et al. Clinical characteristics of patients hospitalized with COVID-19 in Spain: results from the SEMI-COVID-19 Network. medRxiv. 2020 doi: 10.1016/j.rce.2020.07.003. (2020.05.24.20111971) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Chen G., Wu D., Guo W., Cao Y., Huang D., Wang H., et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Investig. 2020;130(5):2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chen J., Fan H., Zhang L., Huang B., Zhu M., Zhou Y., et al. Retrospective analysis of clinical features in 101 death cases with COVID-19. medRxiv. 2020 [Google Scholar]
- 90.Chen J., Xu X., Hu J., Chen Q., Xu F., Liang H., et al. Clinical course and risk factors for recurrence of positive SARS-CoV-2 RNA: a retrospective cohort study from Wuhan, China. medRxiv. 2020 doi: 10.18632/aging.103795. (2020.05.08.20095018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen Q., Zheng Z., Zhang C., Zhang X., Wu H., Wang J., et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou, Zhejiang, China. Infection. 2020:1–9. doi: 10.1007/s15010-020-01432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Cui S., Chen S., Li X., Liu S., Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cummings M.J., Baldwin M.R., Abrams D., Jacobson S.D., Meyer B.J., Balough E.M., et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395:1763–1770. doi: 10.1016/S0140-6736(20)31189-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dai H., Zhang X., Xia J., Zhang T., Shang Y., Huang R., et al. High-resolution chest CT features and clinical characteristics of patients infected with COVID-19 in Jiangsu, China. Int J Infect Dis. 2020;95:106–112. doi: 10.1016/j.ijid.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Demelo-Rodríguez P., Cervilla-Muñoz E., Ordieres-Ortega L., Parra-Virto A., Toledano-Macías M., Toledo-Samaniego N., et al. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res. 2020;192:23–26. doi: 10.1016/j.thromres.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Du Y., Tu L., Zhu P., Mu M., Wang R., Yang P., et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med. 2020;201:1372–1379. doi: 10.1164/rccm.202003-0543OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Estebanez M., Ramirez-Olivencia G., Mata T., Marti D., Gutierrez C., De Dios B., et al. Clinical evaluation of IFN beta1b in COVID-19 pneumonia: a retrospective study. medRxiv. 2020 (2020.05.15.20084293) [Google Scholar]
- 99.Fei J., Fu L., Li Y., Xiang H.-X., Xiang Y., Li M.-D., et al. Reduction of lymphocyte at early stage elevates severity and death risk of COVID-19 patients: a hospital-based case-cohort study. medRxiv. 2020 doi: 10.5114/aoms.2020.99006. (2020.04.02.20050955) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Feng X., Li P., Ma L., Liang H., Lei J., Li W., et al. Clinical characteristics and short-term outcomes of severe patients with COVID-19 in Wuhan, China. medRxiv. 2020 doi: 10.3389/fmed.2020.00491. (2020.04.24.20078063) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Fogarty H., Townsend L., Ni Cheallaigh C., Bergin C., Martin-Loeches I., Browne P., et al. COVID-19 coagulopathy in Caucasian patients. Br J Haematol. 2020;189:1044–1049. doi: 10.1111/bjh.16749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fu J., Kong J., Wang W., Wu M., Yao L., Wang Z., et al. The clinical implication of dynamic neutrophil to lymphocyte ratio and D-dimer in COVID-19: a retrospective study in Suzhou China. Thromb Res. 2020;192:3–8. doi: 10.1016/j.thromres.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gao L., Jiang D., Wen X.S., Cheng X.C., Sun M., He B., et al. Prognostic value of NT-proBNP in patients with severe COVID-19. Respir Res. 2020;21(1) doi: 10.1186/s12931-020-01352-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Garcia-Olivé I., Sintes H., Radua J., Abad Capa J., Rosell A. D-dimer in patients infected with COVID-19 and suspected pulmonary embolism. Respir Med. 2020;169 doi: 10.1016/j.rmed.2020.106023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Giorgi Rossi P., Marino M., Formisano D., Venturelli F., Vicentini M., Grilli R. Characteristics and outcomes of a cohort of SARS-CoV-2 patients in the Province of Reggio Emilia, Italy. medRxiv. 2020 doi: 10.1371/journal.pone.0238281. (2020.04.13.20063545) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelli A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Han H., Xie L., Liu R., Yang J., Liu F., Wu K., et al. Analysis of heart injury laboratory parameters in 273 COVID-19 patients in one hospital in Wuhan, China. J Med Virol. 2020;92:819–823. doi: 10.1002/jmv.25809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Han Y., Zhang H., Mu S., Wei W., Jin C., Xue Y., et al. Lactate dehydrogenase, a risk factor of severe COVID-19 patients. medRxiv. 2020 doi: 10.18632/aging.103372. (2020.03.24.20040162) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.He R., Lu Z., Zhang L., Fan T., Xiong R., Shen X., et al. The clinical course and its correlated immune status in COVID-19 pneumonia. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Helms J., Tacquard C., Severac F., Leonard-Lorant I., Ohana M., Delabranche X., et al. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Hong N., Yu W., Xia J., Shen Y., Yap M., Han W. Evaluation of ocular symptoms and tropism of SARS-CoV-2 in patients confirmed with COVID-19. Acta Ophthalmol. 2020;98:e649–e655. doi: 10.1111/aos.14445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Huang J., Cheng A., Lin S., Zhu Y., Chen G. Individualized prediction nomograms for disease progression in mild COVID-19. J Med Virol. 2020;92:2074–2080. doi: 10.1002/jmv.25969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hui H., Zhang Y., Yang X., Wang X., He B., Li L., et al. Clinical and radiographic features of cardiac injury in patients with 2019 novel coronavirus pneumonia. medRxiv. 2020 [Google Scholar]
- 114.Inciardi R.M., Adamo M., Lupi L., Cani D.S., Di Pasquale M., Tomasoni D., et al. Characteristics and outcomes of patients hospitalized for COVID-19 and cardiac disease in Northern Italy. Eur Heart J. 2020;41(19):1821–1829. doi: 10.1093/eurheartj/ehaa388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Itelman E., Wasserstrum Y., Segev A., Avaky C., Negru L., Cohen D., et al. Clinical characterization of 162 COVID-19 patients in Israel: preliminary report from a large tertiary center. Isr Med Assoc J. 2020;22(5):271–274. [PubMed] [Google Scholar]
- 116.Jain S., Workman V., Ganeshan R., Obasare E.R., Burr A., DeBiasi R.M., et al. Enhanced ECG monitoring of COVID-19 patients. Heart Rhythm. 2020;17:1417–1422. doi: 10.1016/j.hrthm.2020.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Jeong E.K., Park O., Park Y.J., Park S.Y., Kim Y.M., Kim J., et al. Coronavirus disease-19: the first 7,755 cases in the Republic of Korea. Osong Public Health Res Perspect. 2020;11(2):85–90. doi: 10.24171/j.phrp.2020.11.2.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Khera R., Clark C., Lu Y., Guo Y., Ren S., Truax B., et al. Association of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers with the risk of hospitalization and death in hypertensive patients with coronavirus disease-19. medRxiv. 2020 doi: 10.1161/JAHA.120.018086. (2020.05.17.20104943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kim L., Garg S., O’Halloran A., Whitaker M., Pham H., Anderson E.J., et al. Interim analysis of risk factors for severe outcomes among a cohort of hospitalized adults identified through the U.S. coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET) medRxiv. 2020 doi: 10.1093/cid/ciaa1012. (2020.05.18.20103390) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D.A.M.P.J., Kant K.M., et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kolin D.A., Kulm S., Elemento O. Clinical and genetic characteristics of Covid-19 patients from UK Biobank. medRxiv. 2020 doi: 10.1371/journal.pone.0241264. (2020.05.05.20075507) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kuno T., Takahashi M., Obata R., Maeda T. Cardiovascular comorbidities, cardiac injury and prognosis of COVID-19 in New York City. Am Heart J. 2020;226:24–25. doi: 10.1016/j.ahj.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Lala A., Johnson K.W., Russak A.J., Paranjpe I., Zhao S., Solani S., et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. medRxiv. 2020 doi: 10.1016/j.jacc.2020.06.007. (2020.04.20.20072702) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Latif F., Farr M.A., Clerkin K.J., Habal M.V., Takeda K., Naka Y., et al. Characteristics and outcomes of recipients of heart transplant with coronavirus disease 2019. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.2159. e202159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lax S.F., Skok K., Zechner P., Kessler H.H., Kaufmann N., Koelblinger C., et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: results from a prospective, single-center, clinicopathologic case series. Ann Intern Med. 2020;173:350–361. doi: 10.7326/M20-2566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Li M., Dong Y., Wang H., Guo W., Zhou H., Zhang Z., et al. Cardiovascular disease potentially contributes to the progression and poor prognosis of COVID-19. Nutr Metab Cardiovasc Dis. 2020;30:1061–1067. doi: 10.1016/j.numecd.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Li R., Tian J., Yang F., Lv L., Yu J., Sun G., et al. Clinical characteristics of 225 patients with COVID-19 in a tertiary Hospital near Wuhan, China. J Clin Virol. 2020;127:104363. doi: 10.1016/j.jcv.2020.104363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y., et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J Allergy Clin Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lian J., Jin X., Hao S., Cai H., Zhang S., Zheng L., et al. Analysis of epidemiological and clinical features in older patients with corona virus disease 2019 (COVID-19) out of Wuhan. Clin Infect Dis. 2020;71:740–747. doi: 10.1093/cid/ciaa242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lian J., Jin X., Hao S., Jia H., Cai H., Zhang X., et al. Epidemiological, clinical, and virological characteristics of 465 hospitalized cases of coronavirus disease 2019 (COVID-19) from Zhejiang province in China. Influenza Other Respi Viruses. 2020;14:564–574. doi: 10.1111/irv.12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Liu F., Li L., Xu M., Wu J., Luo D., Zhu Y., et al. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Liu F., Xu A., Zhang Y., Xuan W., Yan T., Pan K., et al. Patients of COVID-19 may benefit from sustained lopinavir-combined regimen and the increase of eosinophil may predict the outcome of COVID-19 progression. Int J Infect Dis. 2020;95:183–191. doi: 10.1016/j.ijid.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Liu K., Fang Y.-Y., Deng Y., Liu W., Wang M.-F., Ma J.-P., et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl) 2020;133(9):1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Liu R., Ming X., Zhu H., Song L., Gao Z., Gao L., et al. Association of cardiovascular manifestations with in-hospital outcomes in patients with COVID-19: a hospital staff data. medRxiv. 2020 [Google Scholar]
- 135.Liu Y., Du X., Chen J., Jin Y., Peng L., Wang H.H.X., et al. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J Infect. 2020;81:e6–e12. doi: 10.1016/j.jinf.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lu L., Xiong W., Liu D., Liu J., Yang D., Li N., et al. New-onset acute symptomatic seizure and risk factors in corona virus disease 2019: a retrospective multicenter study. Epilepsia. 2020;61:e49–e53. doi: 10.1111/epi.16524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Menter T., Haslbauer J.D., Nienhold R., Savic S., Hopfer H., Deigendesch N., et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction. Histopathology. 2020;77:198–209. doi: 10.1111/his.14134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Miao C., Zhuang J., Jin M., Xiong H., Huang P., Zhao Q., et al. A comparative multi-centre study on the clinical and imaging features of comfirmed and uncomfirmed patients with COVID-19. medRxiv. 2020 [Google Scholar]
- 140.Middeldorp S., Coppens M., van Haaps T.F., Foppen M., Vlaar A.P., Müller M.C.A., et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020;18:1995–2002. doi: 10.1111/jth.14888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mo P., Xing Y., Xiao Y., Deng L., Zhao Q., Wang H., et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Murk J.L., van de Biggelaar R., Stohr J., Verweij J., Buiting A., Wittens S., et al. The first 100 COVID-19 patients admitted to the Elisabeth-Tweesteden Hospital, Tilburg, The Netherlands. Ned Tijdschr Geneeskd. 2020;164 [PubMed] [Google Scholar]
- 143.Nie S., Zhao X., Zhao K., Zhang Z., Zhang Z., Zhang Z. Metabolic disturbances and inflammatory dysfunction predict severity of coronavirus disease 2019 (COVID-19): a retrospective study. medRxiv. 2020 [Google Scholar]
- 144.Niu S., Tian S., Lou J., Kang X., Zhang L., Lian H., et al. Clinical characteristics of older patients infected with COVID-19: a descriptive study. Arch Gerontol Geriatr. 2020;89 doi: 10.1016/j.archger.2020.104058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Nunes Duarte-Neto A., de Almeida Monteiro R.A., da Silva L.F.F., Malheiros D., de Oliveira E.P., Theodoro Filho J., et al. Pulmonary and systemic involvement of COVID-19 assessed by ultrasound-guided minimally invasive autopsy. Histopathology. 2020;77:186–197. doi: 10.1111/his.14160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Öztürk F., Karaduman M., Çoldur R., İncecik Ş., Güneş Y., Tuncer M. Interpretation of arrhythmogenic effects of COVID-19 disease through ECG. Aging Male. 2020:1–4. doi: 10.1080/13685538.2020.1769058. [DOI] [PubMed] [Google Scholar]
- 147.Palaiodimos L., Kokkinidis D.G., Li W., Karamanis D., Ognibene J., Arora S., et al. Severe obesity is associated with higher in-hospital mortality in a cohort of patients with COVID-19 in the Bronx, New York. Metabolism. 2020;108 doi: 10.1016/j.metabol.2020.154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Pavoni V., Gianesello L., Pazzi M., Stera C., Meconi T., Frigieri F.C. Evaluation of coagulation function by rotation thromboelastometry in critically ill patients with severe COVID-19 pneumonia. J Thromb Thrombolysis. 2020;50:281–286. doi: 10.1007/s11239-020-02130-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Petrilli C.M., Jones S.A., Yang J., Rajagopalan H., O’Donnell L., Chernyak Y., et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. Bmj. 2020;369:m1966. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Piva S., Filippini M., Turla F., Cattaneo S., Margola A., De Fulviis S., et al. Clinical presentation and initial management critically ill patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in Brescia, Italy. J Crit Care. 2020;58:29–33. doi: 10.1016/j.jcrc.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Poyiadji N., Cormier P., Patel P.Y., Hadied M.O., Bhargava P., Khanna K., et al. Acute pulmonary embolism and COVID-19. Radiology. 2020:201955. doi: 10.1148/radiol.2020201955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Qi D., Yan X., Tang X., Peng J., Yu Q., Feng L., et al. Epidemiological and clinical features of 2019-nCoV acute respiratory disease cases in Chongqing municipality, China: a retrospective, descriptive, multiple-center study. medRxiv. 2020 [Google Scholar]
- 153.Qian G.-Q., Yang N.-B., Ding F., Ma A.H.Y., Wang Z.-Y., Shen Y.-F., et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM. 2020;113:474–481. doi: 10.1093/qjmed/hcaa089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Razavi A.C., Kelly T.N., He J., Fernandez C., Whelton P.K., Krousel-Wood M., et al. Cardiovascular disease prevention and implications of COVID-19: an evolving case study in the Crescent City. J Am Heart Assoc. 2020:e016997. doi: 10.1161/JAHA.120.016997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020:E1–E8. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sami R., Soltaninejad F., Amra B., Naderi Z., Haghjooy Javanmard S., Iraj B., et al. A one-year hospital-based prospective COVID-19 open-cohort in the Eastern Mediterranean region: the Khorshid COVID Cohort (KCC) study. medRxiv. 2020 doi: 10.1371/journal.pone.0241537. (2020.05.11.20096727) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Secco G.G., Tarantini G., Mazzarotto P., Garbo R., Parisi R., Maggio S., et al. Invasive strategy for COVID patients presenting with acute coronary syndrome: the first multicenter Italian experience. Catheter Cardiovasc Interv. 2020 doi: 10.1002/ccd.28959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Shao F., Xu S., Ma X., Xu Z., Lyu J., Ng M., et al. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation. 2020;151:18–23. doi: 10.1016/j.resuscitation.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J., et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Shi Q., Zhao K., Yu J., Feng J., Zhao K., Zhang X., et al. Clinical characteristics of 101 non-surviving hospitalized patients with COVID-19: a single center, retrospective study. medRxiv. 2020 [Google Scholar]
- 162.Shi Y., Yu X., Zhao H., Wang H., Zhao R., Sheng J. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1) doi: 10.1186/s13054-020-2833-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A., et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. 2020;28:1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Song F., Shi N., Shan F., Zhang Z., Shen J., Lu H., et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology. 2020;295(1):210–217. doi: 10.1148/radiol.2020200274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sun C., Zhang X., Dai Y., Xu X., Zhao J. Clinical analysis of 150 cases of 2019 novel coronavirus infection in Nanyang City, Henan Province. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43:E042. doi: 10.3760/cma.j.cn112147-20200224-00168. = Zhonghua Jiehe he Huxi Zazhi= Chinese Journal of Tuberculosis and Respiratory Diseases. [DOI] [PubMed] [Google Scholar]
- 166.Sun L., Shen L., Fan J., Gu F., Hu M., An Y., et al. Clinical features of patients with coronavirus disease 2019 (COVID-19) from a designated hospital in Beijing, China. J Med Virol. 2020;92:2055–2066. doi: 10.1002/jmv.25966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Vahidy F.S., Nicolas J.C., Meeks J.R., Khan O., Jones S.L., Masud F., et al. Racial and ethnic disparities in SARS-CoV-2 pandemic: analysis of a COVID-19 observational registry for a diverse U.S. metropolitan population. medRxiv. 2020 doi: 10.1136/bmjopen-2020-039849. (2020.04.24.20073148) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Vicenzi M., Di Cosola R., Ruscica M., Ratti A., Rota I., Rota F., et al. The liaison between respiratory failure and high blood pressure: evidence from COVID-19 patients. Eur Respir J. 2020 doi: 10.1183/13993003.01157-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Wan S., Xiang Y., Fang W., Zheng Y., Li B., Hu Y., et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol. 2020;92:797–806. doi: 10.1002/jmv.25783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wang K., Kang S., Tian R., Zhang X., Wang Y. Imaging manifestations and diagnostic value of chest CT of coronavirus disease 2019 (COVID-19) in the Xiaogan area. Clin Radiol. 2020;75(5):341–347. doi: 10.1016/j.crad.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wang W., He J., Wu S. The definition and risks of cytokine release syndrome-like in 11 COVID-19-infected pneumonia critically ill patients: disease characteristics and retrospective analysis. medRxiv. 2020 doi: 10.1093/infdis/jiaa387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Wang X., Fang J., Zhu Y., Chen L., Ding F., Zhou R., et al. Clinical characteristics of non-critically ill patients with novel coronavirus infection (COVID-19) in a Fangcang Hospital. Clin Microbiol Infect. 2020;26:1063–1068. doi: 10.1016/j.cmi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Wang Z., Yang B., Li Q., Wen L., Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. 2020;71:769–777. doi: 10.1093/cid/ciaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wei J.F., Huang F.Y., Xiong T.Y., Liu Q., Chen H., Wang H., et al. Acute myocardial injury is common in patients with covid-19 and impairs their prognosis. Heart. 2020;106:1122–1124. doi: 10.1136/heartjnl-2020-317007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Wright F.L., Vogler T.O., Moore E.E., Moore H.B., Wohlauer M.V., Urban S., et al. Fibrinolysis shutdown correlates to thromboembolic events in severe COVID-19 infection. J Am Coll Surg. 2020;231 doi: 10.1016/j.jamcollsurg.2020.05.007. 193-203.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Wu C., Hu X., Song J., Du C., Xu J., Yang D., et al. Heart injury signs are associated with higher and earlier mortality in coronavirus disease 2019 (COVID-19) medRxiv. 2020 [Google Scholar]
- 178.Wu J., Liu J., Zhao X., Liu C., Wang W., Wang D., et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu province: a multicenter descriptive study. Clin Infect Dis. 2020;10 doi: 10.1093/cid/ciaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Xi A., Zhuo M., Dai J., Ding Y., Ma X., Ma X., et al. Epidemiological and clinical characteristics of discharged patients infected with SARS-CoV-2 on the Qinghai plateau. J Med Virol. 2020;92:2528–2535. doi: 10.1002/jmv.26032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Xu H., Hou K., Xu H., Li Z., Chen H., Zhang N., et al. Acute myocardial injury of patients with coronavirus disease 2019. medRxiv. 2020 [Google Scholar]
- 181.Xu K., Chen Y., Yuan J., Yi P., Ding C., Wu W., et al. Factors associated with prolonged viral RNA shedding in patients with COVID-19. Clin Infect Dis. 2020;71:799–806. doi: 10.1093/cid/ciaa351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Xu S., Fu L., Fei J., Xiang H.-X., Xiang Y., Tan Z.-X., et al. Acute kidney injury at early stage as a negative prognostic indicator of patients with COVID-19: a hospital-based retrospective analysis. medRxiv. 2020 [Google Scholar]
- 183.Xu T., Chen C., Zhu Z., Cui M., Chen C., Dai H., et al. Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19. Int J Infect Dis. 2020;94:68–71. doi: 10.1016/j.ijid.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Xu X., Yu C., Qu J., Zhang L., Jiang S., Huang D., et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging. 2020:1–6. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Xu X.-W., Wu X.-X., Jiang X.-G., Xu K.-J., Ying L.-J., Ma C.-L., et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. bmj. 2020:368. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Yang A.P., Liu J.P., Tao W.Q., Li H.M. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int Immunopharmacol. 2020;84 doi: 10.1016/j.intimp.2020.106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yang F., Shi S., Zhu J., Shi J., Dai K., Chen X. Analysis of 92 deceased patients with COVID-19. J Med Virol. 2020;92:2511–2515. doi: 10.1002/jmv.25891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Yang Z., Shi J., He Z., Lu Y., Xu Q., Ye C., et al. Predictors for imaging progression on chest ct from coronavirus disease 2019 (covid-19) patients. Aging. 2020;12(7):6037–6048. doi: 10.18632/aging.102999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Yin L., Mou H., Shao J., Zhu Y., Pang X., Yang J., et al. Correlation between heart fatty acid binding protein and severe COVID-19: a case-control study. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Yu C., Qu J., Zhang L., Jiang S., Chen B., Guan W., et al. High resolution CT findings and clinical features of COVID-19 in Guangzhou. Chin J Radiol. 2020;54(4):314–317. [Google Scholar]
- 191.Yu X., Sun X., Cui P., Pan H., Lin S., Han R., et al. Epidemiological and clinical characteristics of 333 confirmed cases with coronavirus disease 2019 in Shanghai, China. Transbound Emerg Dis. 2020;67:1697–1707. doi: 10.1111/tbed.13604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Yuan J., Zou R., Zeng L., Kou S., Lan J., Li X., et al. The correlation between viral clearance and biochemical outcomes of 94 COVID-19 infected discharged patients. Inflamm Res. 2020;69(6):599–606. doi: 10.1007/s00011-020-01342-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Zangrillo A., Beretta L., Scandroglio A.M., Monti G., Fominskiy E., Colombo S., et al. Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy. Crit Care Resusc. 2020 doi: 10.1016/S1441-2772(23)00387-3. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Zeng L., Li J., Liao M., Hua R., Huang P., Zhang M., et al. Risk assessment of progression to severe conditions for patients with COVID-19 pneumonia: a single-center retrospective study. medRxiv. 2020 [Google Scholar]
- 195.Zhang B., Zhou X., Qiu Y., Feng F., Feng J., Jia Y., et al. Clinical characteristics of 82 death cases with COVID-19. medRxiv. 2020 doi: 10.1371/journal.pone.0235458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Zhang G., Hu C., Luo L., Fang F., Chen Y., Li J., et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Zhang J., Wang X., Jia X., Li J., Hu K., Chen G., et al. Risk factors for disease severity, unimprovement, and mortality in COVID-19 patients in Wuhan, China. Clin Microbiol Infect. 2020;26:767–772. doi: 10.1016/j.cmi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zhang J., Yu M., Tong S., Liu L.Y., Tang L.V. Predictive factors for disease progression in hospitalized patients with coronavirus disease 2019 in Wuhan, China. J Clin Virol. 2020;127 doi: 10.1016/j.jcv.2020.104392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.J-j Zhang, Dong X., Cao Y.-y., Yuan Y.-d., Yang Y.-b., Yan Y.-q., et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;75:1730–1741. doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 200.Zhang L., Feng X., Zhang D., Jiang C., Mei H., Wang J., et al. Deep vein thrombosis in hospitalized patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: prevalence, risk factors, and outcome. Circulation. 2020;142:114–128. doi: 10.1161/CIRCULATIONAHA.120.046702. [DOI] [PubMed] [Google Scholar]
- 201.Zhang X., Cai H., Hu J., Lian J., Gu J., Zhang S., et al. Epidemiological, clinical characteristics of cases of SARS-CoV-2 infection with abnormal imaging findings. Int J Infect Dis. 2020;94:81–87. doi: 10.1016/j.ijid.2020.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zhang Y., Cui Y., Shen M., Zhang J., Liu B., Dai M., et al. Association of diabetes mellitus with disease severity and prognosis in COVID-19: a retrospective cohort study. Diabetes Res Clin Pract. 2020;165:108227. doi: 10.1016/j.diabres.2020.108227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zhang Y., Deng A., Hu T., Chen X., Zhuang Y., Tan X., et al. Clinical outcomes of COVID-19 cases and influencing factors in Guangdong province. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:E057. doi: 10.3760/cma.j.cn112338-20200318-00378. = Zhonghua liuxingbingxue zazhi. [DOI] [PubMed] [Google Scholar]
- 204.Zhao S., Ling K., Yan H., Zhong L., Peng X., Yao S., et al. Anesthetic management of patients with suspected 2019 novel coronavirus infection during emergency procedures. J Cardiothorac Vasc Anesth. 2020;34:1125–1131. doi: 10.1053/j.jvca.2020.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Zhao W., Zhong Z., Xie X., Yu Q., Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (covid-19) pneumonia: a multicenter study. Am J Roentgenol. 2020;214(5):1072–1077. doi: 10.2214/AJR.20.22976. [DOI] [PubMed] [Google Scholar]
- 206.Zhao X.Y., Xu X.X., Yin H.S., Hu Q.M., Xiong T., Tang Y.Y., et al. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis. 2020;20(1) doi: 10.1186/s12879-020-05010-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Zhao Z., Xie J., Yin M., Yang Y., He H., Jin T., et al. Clinical and laboratory profiles of 75 hospitalized patients with novel coronavirus disease 2019 in Hefei, China. medRxiv. 2020 [Google Scholar]
- 208.Zheng F., Tang W., Li H., Huang Y.X., Xie Y.L., Zhou Z.G. Clinical characteristics of 161 cases of corona virus disease 2019 (COVID-19) in Changsha. Eur Rev Med Pharmacol Sci. 2020;24(6):3404–3410. doi: 10.26355/eurrev_202003_20711. [DOI] [PubMed] [Google Scholar]
- 209.Zheng Y., Sun L.J., Xu M., Pan J., Zhang Y.T., Fang X.L., et al. Clinical characteristics of 34 COVID-19 patients admitted to intensive care unit in Hangzhou, China. J Zhejiang Univ Sci B. 2020;21(5):378–387. doi: 10.1631/jzus.B2000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zhou B., She J., Wang Y., Ma X. The clinical characteristics of myocardial injury in severe and very severe patients with 2019 novel coronavirus disease. J Infect. 2020;81:147–178. doi: 10.1016/j.jinf.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Zhou F., Yu X., Tong X., Zhang R. Clinical features and outcomes of 197 adult discharged patients with COIVD-19 in Yichang, Hubei. medRxiv. 2020 [Google Scholar]
- 212.Zhou Y., He Y., Yang H., Yu H., Wang T., Chen Z., et al. Development and validation a nomogram for predicting the risk of severe COVID-19: a multi-center study in Sichuan, China. PLoS One. 2020;15(5) doi: 10.1371/journal.pone.0233328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Zhou Z., Zhao N., Shu Y., Han S., Chen B., Shu X. Effect of gastrointestinal symptoms in patients with COVID-19. Gastroenterology. 2020;158(8):2294–2297. doi: 10.1053/j.gastro.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Zhu Z., Cai T., Fan L., Lou K., Hua X., Huang Z., et al. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Dis. 2020;95:332–339. doi: 10.1016/j.ijid.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Zhu Z., Tang J., Chai X., Fang Z., Liu Q., Hu X., et al. How to differentiate COVID-19 pneumonia from heart failure with computed tomography at initial medical contact during epidemic period. medRxiv. 2020 [Google Scholar]
- 216.Badawi A., Ryoo S.G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Xiong T.-Y., Redwood S., Prendergast B., Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020;41:1798–1800. doi: 10.1093/eurheartj/ehaa231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E., et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art-review. J Am Coll Cardiol. 2020;75(23):2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Zheng Y.-Y., Ma Y.-T., Zhang J.-Y., Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr. 2020;14(3):247–250. doi: 10.1016/j.dsx.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Clerkin K.J., Fried J.A., Raikhelkar J., Sayer G., Griffin J.M., Masoumi A., et al. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 222.Bavishi C., Bonow R.O., Trivedi V., Abbott J.D., Messerli F.H., Bhatt D.L. Acute myocardial injury in patients hospitalized with COVID-19 infection: a review. Prog Cardiovasc Dis. 2020 doi: 10.1016/j.pcad.2020.05.013. (In Press, Corrected Proof; S0033-620(20)30123-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181 doi: 10.1016/j.cell.2020.02.052. 271-280.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Zhu H., Rhee J.-W., Cheng P., Waliany S., Chang A., Witteles R.M., et al. Cardiovascular complications in patients with COVID-19: consequences of viral toxicities and host immune response. Curr Cardiol Rep. 2020;22(5):32. doi: 10.1007/s11886-020-01292-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Connors J.M., Levy J.H. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Clerkin K.J., Fried J.A., Raikhelkar J., Sayer G., Griffin J.M., Masoumi A., et al. Coronavirus disease 2019 (COVID-19) and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 227.South A.M., Diz D., Chappell M.C. COVID-19, ACE2 and the cardiovascular consequences. Am J Physiol Heart Circ Physiol. 2020;318:H1084–H1090. doi: 10.1152/ajpheart.00217.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Schiffrin E.L., Flack J.M., Ito S., Muntner P., Webb R.C. Hypertension and COVID-19. Am J Hypertens. 2020;33(5):373–374. doi: 10.1093/ajh/hpaa057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8(4):e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.AlGhatrif M., Cingolani O., Lakatta E.G. The dilemma of coronavirus disease 2019, aging, and cardiovascular disease: insights from cardiovascular aging science. JAMA Cardiol. 2020;5:747–748. doi: 10.1001/jamacardio.2020.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Yazdanpanah F., Hamblin M.R., Rezaei N. The immune system and COVID-19: friend or foe? Life Sci. 2020;256:117900. doi: 10.1016/j.lfs.2020.117900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Siripanthong B., Nazarian S., Muser D., Deo R., Santangeli P., Khanji M.Y., et al. Recognizing COVID-19-related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17:1463–1471. doi: 10.1016/j.hrthm.2020.05.001. (S1547-5271(20)30422-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Lippi G., South A.M., Henry B.M. Electrolyte imbalances in patients with severe coronavirus disease 2019 (COVID-19) Ann Clin Biochem. 2020;57(3):262–265. doi: 10.1177/0004563220922255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G., et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Lazzerini P.E., Boutjdir M., Capecchi P.L. COVID-19, arrhythmic risk and inflammation: mind the gap! Circulation. 2020;142:7–9. doi: 10.1161/CIRCULATIONAHA.120.047293. [DOI] [PubMed] [Google Scholar]
- 236.Wu C.-I., Postema P.G., Arbelo E., Behr E.R., Bezzina C.R., Napolitano C., et al. SARS-CoV-2, COVID-19, and inherited arrhythmia syndromes. Heart Rhythm. 2020;17:1456–1462. doi: 10.1016/j.hrthm.2020.03.024. (S1547-5271(20)30285-X) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Tomasoni D., Italia L., Adamo M., Inciardi R.M., Lombardi C.M., Solomon S.D., et al. COVID-19 and heart failure: from infection to inflammation and angiotensin II stimulation. Searching for evidence from a new disease. Eur J Heart Fail. 2020;22:957–966. doi: 10.1002/ejhf.1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Medina de Chazal H., Del Buono M.G., Keyser-Marcus L., Ma L., Moeller F.G., Berrocal D., et al. Stress cardiomyopathy diagnosis and treatment. JACC State-of-thee-Art Review. J Am Coll Cardinol. 2018;72(16):1955–1971. doi: 10.1016/j.jacc.2018.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Pasqualetto M.C., Secco E., Nizzetto M., Scevola M., Altafini L., Cester A., et al. Stress cardiomyopathy in COVID-19 disease. Eur J Case Rep Intern Med. 2020;7(6):001718. doi: 10.12890/2020_001718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Roca E., Lombardi C., Campana M., Vivaldi O., Bigni B., Bertozzi B., et al. Takotsubo syndrome associated with COVID-19. Eur J Case Rep Intern Med. 2020;7(5):001665. doi: 10.12890/2020_001665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Giustino G., Croft L.B., Oates C.P., Rahman K., Lerakis S., Reddy V.Y., et al. Takotsubo cardiomyopathy in males with Covid-19. J Am Coll Cardiol. 2020;76:628–629. doi: 10.1016/j.jacc.2020.05.068. (S0735-1097(20)35551-0) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Nguyen D., Nguyen T., De Bels D., Castro Rodriguez J. A case of Takotsubo cardiomyopathy with COVID 19. Eur Heart J Cardiovasc Imaging. 2020;21:1052. doi: 10.1093/ehjci/jeaa152. jeaa152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Chadha S. ‘COVID-19 pandemic’ anxiety induced Tako-tsubo cardiomyopathy. QJM. 2020;113:488–490. doi: 10.1093/qjmed/hcaa135. hcaa135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Fung G., Luo H., Qiu Y., Yang D., McManus B. Myocarditis. Circ Res. 2016;118(3):496–514. doi: 10.1161/CIRCRESAHA.115.306573. [DOI] [PubMed] [Google Scholar]
- 245.Hu H., Ma F., Wei X., Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Zeng J., Liu Y., Yuan J., et al. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infection. 2020;28:773–777. doi: 10.1007/s15010-020-01424-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Corrales-Medina V.F., Madjid M., Musher D.M. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10(2):83–92. doi: 10.1016/S1473-3099(09)70331-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Fig. S1: Meta-analysis of prevalence of cardiovascular diseases among COVID-19 patients with mortality
Supplementary Fig. S2: Meta-analysis of odds ratio of mortality among COVID-19 patients with cardiovascular diseases
Supplementary Fig. S3: Meta-analysis of prevalence of cardiovascular diseases among COVID-19 patients admitted to ICU
Supplementary Fig. S4: Meta-analysis of odds Ratio of ICU admission among COVID-19 patients with cardiovascular diseases
Supplementary Fig. S5: Meta-analysis of prevalence of cardiovascular complications among COVID-19 patients
Supplementary Table S1: Characteristics of studies included into meta-analysis