Abstract
Specific return to sport criteria for children and adolescents after anterior cruciate ligament injury and reconstruction are unknown. The aim of this scoping review is to provide an overview of current tests regarding return to sport for children and adolescents. This scoping review was performed according to the PRISMA statement. A systematic search was performed on PubMed and EMBASE. The inclusion criteria were diagnostic and prognostic studies evaluating tests regarding return to sport after ACL injury and reconstruction in children/adolescents (age < 18 years). Twenty-six studies were included, of which 22 studies evaluated tests in the age category of 16 to 18 years. All studies evaluated tests after ACL reconstruction, no studies have been conducted in non-operative patients. Strength tests, movement quality and patient reported outcomes measures (PROMs) are investigated most frequently. Clearance for return to sport should be based on a test battery including strength tests, movement quality during sport-specific tasks and (paediatric) patient reported outcome measures. There are no recommendations on which specific tests regarding quantity and quality of movement should be used. Future research should aim at at developing and validating a test battery including movement quality and neuromotor control in a sport-specific context for both younger children and adolescents after both operative and non-operative treatment.
Keywords: “anterior cruciate ligament”, “Paediatric”, “Adolescent”, “return to sport”, “Scoping review”
Introduction
Anterior cruciate ligament (ACL) ruptures in children and adolescents are considered to be a severe injury of the knee in a vulnerable population with high rates of secondary ruptures after ACL reconstruction [1]. There are two possible treatment options for children with an ACL rupture according to the International Olympic Committee (IOC): conservative high quality rehabilitation or surgical ACL reconstruction plus high quality rehabilitation [1, 25]. The goal of either treatment regimen is to restore a stable, well-functioning knee, to reduce the risk of further meniscal or chondral injury and to successfully return to sport [1]. Successful return to sport can be defined as returning to the desired level of sport without sustaining a second ACL injury.
The IOC statement recommends using functional performance tests and return to sport criteria during rehabilitation [1]. The specific clinical and functional milestones described in the four-phased rehabilitation are based on the outcomes of a systematic review and practice guideline by Van Melick et al. [40] This systematic review, however, excluded skeletally immature children and it is therefore unknown if these milestones can be applied in the younger population [40].
The aim of this scoping review is to provide an overview of the current evidence of tests evaluating readiness for return to sport after ACL injury or ACL reconstruction in children and adolescents (age < 18 years). Based on the outcomes of this scoping review, the hiatus in the current evidence is shown and advice is given for future research.
Methods
This scoping review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement extension for scoping reviews [37]. The general purpose for inducting a scoping review is to identify and map the available evidence and not to produce a critically appraised and synthesised answer to a specific question [26].
Selection criteria
Articles included in the current scoping review had to meet the inclusion and exclusion criteria listed in Table 1.
Table 1.
Overview of inclusion and exclusion criteria for this scoping review
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Participants | Children (average age < 18 years) | Average age ≥ 18 years |
| Injury | ACL rupture or reconstruction | ACL revision surgery |
| Multi-ligament injury of the knee | ||
| Fractures | ||
| Tests | Any test concerning return to sport, including: | |
| - Strength tests | ||
| - Hop tests | ||
| - Movement quality tests | ||
| - Physical examination | ||
| - PROMs | ||
| Outcomes | Diagnostic values (e.g.,sensitivity, specificity) | |
| Prognostic information (e.g.,correlation coefficients, regression) | ||
| Study design | Cross-sectional studies | |
| Longitudinal studies |
Search strategy
At the 30th of March 2020, an information specialist (ED) performed a systematic literature search in PubMed (Medline) and EMBASE databases, as shown in Additional file 1. All published articles up to the 30th of March of 2020 were considered eligible. The following terms, including synonyms and closely related words, were used as index terms or free-text words: “anterior cruciate ligament injury”, “paediatric”, “adolescent” and “return to sport”. Studies written in other languages than English, Dutch and German were excluded. Duplicate articles were removed.
Study selection
Two researchers (MD, MB) independently screened the abstracts for eligibility by using the Rayyan QCRI app (rayyan.qrci.org) [28]. A full-text version of all eligible studies was reviewed. All references of these studies were screened for additional eligible articles. Any disagreements between the reviewers were resolved by discussion. Cohen’s kappa was calculated to measure inter-reviewer agreement in the selection process.
Data collection process
Two authors (MD, MB) extracted all relevant data. The data included specific details of the tests, population characteristics, interventions, study methods, follow-up period and outcomes of interest to the review question and research objectives. Any disagreements about the interpretation of the results were resolved by discussion. Due to the heterogeinity of the study designs and data and the aim of this scoping review, no risk of bias assessment was performed on the included studies.
Results
Search results
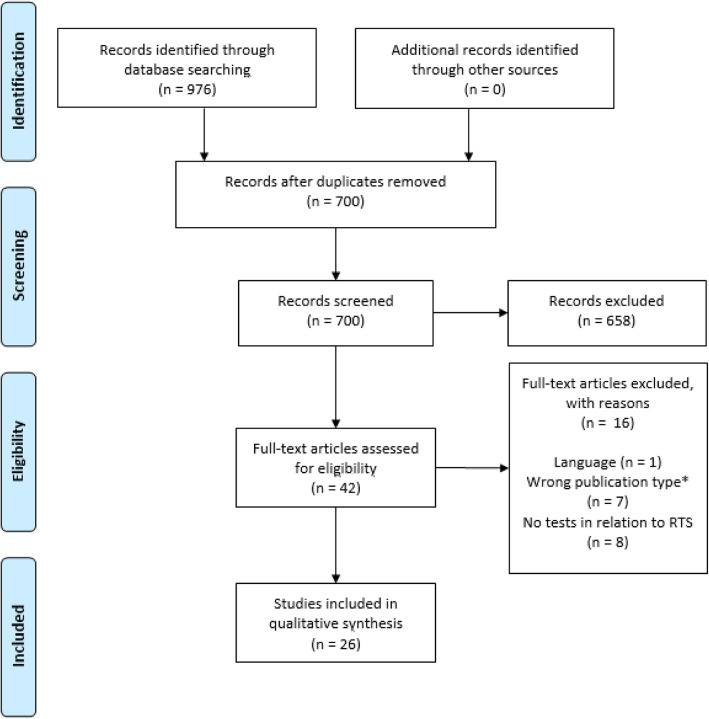
Twenty six studies were included in this scoping review (Fig. 1). The inter-reviewer agreement was almost perfect with a Cohen’s Kappa of 0.94. The 3 studies of conflict were resolved by discussion. All 26 studies are published in the last 10 years and 22 in the last 5 years.
Fig. 1.
PRISMA flow diagram of inclusion process. *including abstracts of presentations
Study characteristics
Fifteen studies had a cross-sectional design [4, 7, 9, 11, 14, 16, 18, 21, 27, 29, 32, 34, 35, 43, 44]. Eleven studies had a longitudinal design [3, 10, 12, 19, 20, 22, 23, 30, 31, 33, 36]. Sixteen of the 26 included studies were from the same research group from Cincinnati Children’s Hospital Medical Center [11, 14, 18–22, 27, 30–33, 35, 36, 44]. Ten of those sixteen studies reported to be part of a larger, prospective study on ACL reconstruction outcomes (ACL-RELAY study) [11, 18–20, 22, 30, 34–36, 44].
Demographic characteristics
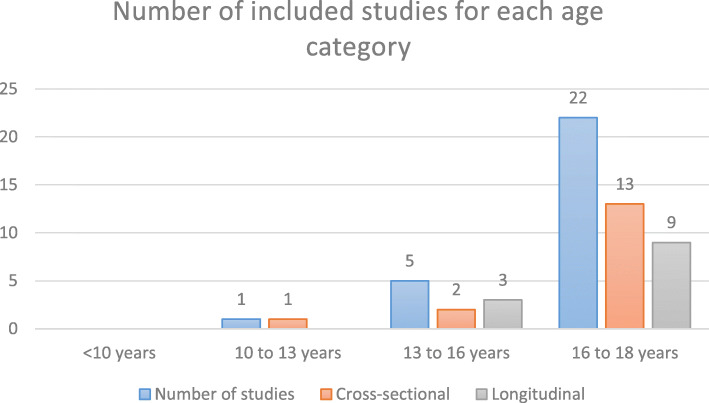
The exact number of included patients in this scoping review is difficult to estimate due to that some studies include participants from the same prospective study [11, 18–20, 22, 30, 34–36, 44]. The range of included patients are 14 to 384 [10, 29]. The number of patients for each study are shown in Additional file 2. The majority of the studies included participants of 16 to 18 years of age [4, 7, 10, 11, 14, 16, 18–23, 27, 29–36, 44]. Six studies included children younger than 16 years of age [3, 7, 12, 18, 31, 33]. Fig. 2 shows the number of studies for each age category.
Fig. 2.
Number (n = 26) of included studies for each mean age divided in categories. Two studies investigated two age categories which were presented seperately [7, 18].
Surgical procedures
All studies investigated patients after ACL reconstruction (ACLR). No study regarding return to sport testing after non-operative treatment were available for inclusion. Four studies evaluated tests in children who had undergone a physeal sparing or transphyseal procedure, as is shown in Table 2 [3, 7, 12, 18]. To reconstruct the ACL, a hamstring tendon autograft was used most frequently (n = 18), followed by patella tendon autograft (n = 16).
Table 2.
Overview of studies providing data on modifications of ACLR due to open physes
Tests regarding return to sport
Muscle strength tests
Thirteen of the 26 studies investigated the outcomes of muscle strength tests in relation to outcomes regarding return to sport [4, 9, 11, 14, 16, 18, 19, 21, 22, 29, 34–36]. In Additional file 2, the different muscle strength tests are shown for each study in Table 1. In all 13 studies quadriceps strength was evaluated. Isometric quadriceps strength was evaluated in 8 studies [4, 9, 14, 19, 21, 22, 34, 35]. Eight studies included isokinetic quadriceps strength tests [4, 9, 11, 16, 18, 22, 29, 36]. Hamstring strength was also tested in 8 studies, of which 2 studies evaluated isometric hamstring strength [4, 9] and 8 studies isokinetic hamstring strength [4, 9, 11, 16, 18, 22, 29, 36]. Hip abduction strength was tested in 4 studies [11, 14, 16, 22] and hip external rotation strength in one study [16]. Most studies evaluated the strength tests at return to sport (RTS) around 8 months post-ACLR. Six studies evaluated strength tests as a prognostic value for a variety of outcomes, such as movement quality outcomes, PROMs, re-ruptures and achieving RTS at follow up [9, 19, 21, 22, 29, 36]. One study evaluated the prognostic value of strength tests for achieving RTS and one study for sustaining an ipsilateral re-rupture [9, 29].
Hop tests
Four studies [4, 18, 36, 43] evaluated hop tests in regard to RTS, of which two studies [18, 36] tested Noyes’ hop test battery -single hop for distance, triple hop for distance, crossover hop and 6-m timed hop-. One study tested a single hop for distance [43]. One study analysed the hop test for distance, a vertical hop test and side hop test (see Additional file 2, Table 2) [4]. Testing occurred in two studies at RTS (around 8 months) and in one study before RTS (7 months). Toole et al. evaluated Noyes’ hop test battery as a prognostic value for achieving combined test crition cut-offs after 1 year follow-up post-RTS [36].
Movement quality
In 14 studies movement quality in relation to RTS was evaluated with a great variety of different parameters, as is shown in Additional file 2, Table 3 [7, 10, 11, 14, 16, 20, 21, 27, 29, 31–34, 43]. Eight studies tested different biomechanical variables during a landing task [14, 16, 20, 21, 27, 33, 34, 43]. In 11 of the 14 studies, testing was done at RTS (approximately 7 months post-ACLR) [7, 11, 14, 16, 20, 21, 29, 31–34]. Five studies evaluated movement quality as a prognostic factor after follow-up [10, 20, 29, 31, 33], of which four studies [10, 29, 31, 33] investigated movement quality as a prognostic value for sustaining re-ruptures and one study [20] as prognostic factor for outcomes of PROMs and hop tests.
Patient reported outcome measures
PROMs in relation to RTS were evaluated in 10 studies, as is shown in Additional file 2, Table 4 [3, 4, 9, 12, 18, 21, 23, 30, 36, 44]. The IKDC Subjective Knee Evaluation Form [21, 36, 44] and the ACL-RSI [4, 9, 23] are evaluated most frequently, followed by the Tegner Activity Scale [3, 4]. Of the paediatric PROMs, the Pedi-IKDC is tested in one study [9]. Seven studies evaluated PROMs at the moment of RTS (approximately 8 months post-ACLR) [3, 18, 21, 23, 30, 36, 44]. Prognostic values of PROMs were investigated in 7 studies [3, 9, 12, 21, 23, 30, 36], of which 4 studies [3, 12, 23, 30] tested the prognostic value of PROMs for developing a re-rupture, 2 studies [9, 12] for achieving RTS and one study for meeting combined test criterion cut-offs [36].
Physical examination
Outcomes of joint laxity tests and range of motion of joints in regard to RTS were investigated in respectively 3 [7, 22, 33] and 2 studies [16, 22], as shown in Additional file 2, Table 5. Laxity tests were performed with the KT-1000 arthrometer [7, 22, 33]. Two studies evaluated the prognostic values of laxity tests at the moment of RTS in relation to PROMs [22] and re-ruptures [33].
Test battery
Two studies tested the same test battery in relation to RTS, consisting of a combination of test criterion cut-off values of the IKDC, muscle strength LSI and hop tests LSI at RTS (see Additional file 2, Table 6) [18, 36]. Ithurburn et al. [18] analysed the proportions of participants meeting all RTS criterion cut-offs at RTS for each age category, while Toole et al. [36] analysed whether those proportions maintained the same level of sport participation after 1 year follow-up post-RTS.
Return to sport clearance criteria
Seven studies included a definition of their RTS clearance criteria, including objective and subjective criteria [3, 7, 9, 10, 16, 23, 29]. All 7 studies used a combination of different tests to assess readiness for RTS. Table 3 provides an overview of tests for each study.
Table 3.
Overview of tests used as RTS criteria. * including PROMs; ** including range of motion, effusion, laxity tests
Discussion
The most important finding of this scoping review was that many studies have evaluated strength tests, hop tests, movement quality and PROMs regarding return to sport in adolescents after ACL reconstruction, but that only few studies have been conducted in children/adolescents under 16 years of age. There is currently sparse evidence for specific testing regarding return to sport in younger children. However, in the category of 16 to 18 years many studies have been conducted, both comparing different tests at the moment of RTS as well as evaluating prognostic values of tests with regard to ACL graft rerupture, achieving return to preinjury sport level or subjective outcomes [3, 9, 10, 12, 19, 20, 22, 23, 29–31, 33, 36].
Successful return to sport is context- and outcome-dependent and has a different meaning for different people (including the patient, clinician and coach) [2]. Criteria of clearance RTS exist in great variability and it should be noted that a true clearance is multifactorial and complex [8]. This was reflected by the variability of tests and outcomes described in the included studies, including strength tests, hop tests, movement quality, PROMs and physical examination.
The 2018 IOC consensus statement on paediatric ACL recommends return to sport clearance criteria, including a LSI > 90% for strength and single-leg hop tests for adolescents, psychological factors, knowledge and gradual increase in sport specific training without pain and effusion [1]. All of the included studies which presented their RTS clearance criteria, used a combination of tests to determine whether the child or adolescent was ready to return to sport [3, 7, 9, 10, 16, 23, 29]. All of those studies used strength tests as a criterium [3, 7, 9, 10, 16, 23, 29]. Subjective outcomes and hop tests are used in only 2 studies respectively [7, 10]. One study used time as a criterium for RTS clearance, which is in contrast to the scoping review on RTS clearance after ACL reconstruction by Burgi et al. [7, 8] They found that 85% of the studies used time as the primary criterion to clear athletes (no age limits defined) to RTS [8]. Children and adolescents are at a higher risk of a second ACL injury, especially in the first year after ACL reconstruction [1]. It is therefore recommended to advise the child not to return to pivoting sport within 12 months after ACL reconstruction [1]. The timing of RTS testing in the included studies was approximately 7.5 months after ACL reconstruction, which seems to be early in this population. However, it is not known whether the child was allowed to return to pivoting sport.
Thirteen of the 26 included studies evaluated the outcomes of strength tests regarding to return to sport [4, 9, 11, 14, 16, 18, 19, 21, 22, 29, 34–36], of which one study compared strength tests in paediatric patients (mean 12 years of age) versus adolescents (mean 16.5 years of age) [18]. Besides, one study tested muscle strength in adolescents between 12 and 16 years of age [9]. All other studies evaluated strength tests in adolescents older than 16 years of age, which may resemble adults [1]. It is recommended that in the younger patients (< 12 years) less emphasis should be on muscle strength and hypertrophy [1]. Pre-pubertal children may benefit from resistance training, but the trainability of muscle strength increases with age [6]. During puberty, boys show an accelerated increase in muscle strength and girls continue to develop in a similar rate as pre-puberty [6]. Despite these gender-related differences in trainability and outcome, only one study evaluated the differences between males and females [36].
The included studies showed a great variety of measurements regarding the quantity of movement, including isokinetic and isometric strength tests and different hop tests. However, the LSI is often used as an outcome to describe symmetry during strength tests or hop tests. Caution must be taken when interpreting an LSI in absence of an accurate baseline measurement, which includes muscle strength LSI as well as hop tests LSI [5, 8, 38, 42, 43]. A normal LSI does not exclude postoperative deterioration of the uninvolved leg [8]. The IOC therefore recommends to focus on the quality of the movements during a single-leg hop test, instead of LSI [1]. Movement quality is the most frequently evaluated test category in the included studies, but also with a great variety of tests and outcomes [7, 10, 11, 14, 16, 20, 21, 27, 29, 31–34, 43]. Landing variables are evaluated most frequently and are advised to use as movement quality measurement. As ACL injuries are common in pivoting sport, stricter cut-offs for strength tests are recommended in case of a return to pivoting sport [40]. Furthermore, specific movement quality tests and outcomes might be relevant in return to pivoting sport because of the loss of normal knee proprioception, such as single leg movement including cutting mechanics. Based on a recent systematic review, RTS testing should include asymmetry in loading experienced by each limb rather than the movement patterns alone, as asymmetries between the limbs were more commonly identified in kinetic variables than in kinematic variables [17].
Besides strength tests, hop tests and movement quality, subjective outcomes such as PROMs might have an important role in determining readiness for return to sport. They offer a more complete picture of the patient’s perception on the actual recovery after ACL surgery [9]. Caution must be taken when interpreting PROMs scores in children and adolescents when adult PROMs are used in children instead of the specific paediatric PROMS due to problems in comprehensibility [13]. The Pedi-IKDC was described in one study, while the other studies used the (adult) IKDC and/or the KOOS [9, 18, 21, 36, 44]. Besides the IKDC and the KOOS, other PROMs are used and are not validated in children [9, 13, 30, 39]. This in accordance with the infrequent use of pediatric-specific instruments as outcomes measures in pediatric ACL literature [15]. The ACL-RSI is validated from the age of 16 years [41]. Specific paediatric versions of adult PROMS have been developed and should be used in evaluating children with knee injuries [13, 39]. One must note however, that in most of the included studies, the mean age is 17 years and that comprehensibility in that age category might not be a significant issue.
Limitations
The most important limitation of this review is that data from sixteen of the 26 included studies are from the same research group and ten of those sixteen are from the same prospective cohort study (ACL RELAY) [11, 18–20, 22, 30, 34–36, 44]. It is therefore difficult to determine whether the same patients are evaluated in more than one study. It is important to note however, that these studies are published from a well-known high-quality American ACL research group and the use of measurements is based on their professional opinions and experiences. This adds to the value of the described tests in relation to return to sport.
Another important limitation of this study is that the majority of the included participants were older than 16 years of age and it may therefore be difficult to draw conclusions about return to sport criteria for younger children. This emphasizes the necessity to aim further research at younger children. Especially since the incidence of ACL injuries in this vulnerable group of is increasing [1].
Recommendations for day-to-day practice
Clearance for RTS is a complex and multifactorial issue. The following recommendations for measurements in relation to RTS are made based on the results of this scoping review and expert opinions of the authors. It is important that rehabilitation must be guided by clinical and functional milestones as decribed in the IOC statement and to advise the child not to return to pivoting sports within 12 months after ACL reconstruction [1]. Tests regarding RTS clearance for adolescents (16–18 years old) should include quadriceps and hamstrings strength tests, hop tests, movement quality assessment during sport specific tasks and PROMs, which might in this age category be disputable whether paediatric of adult PROMs can be used. In the age category 12–16 years, testing should include hop tests, movement quality and paediatric PROMs [24]. Strengh tests in this age category are debatable as there is only sparse evidence of muscle strength tests and outcomes in this age category. In children younger than 12 years, there is currently very limited evidence and based on the physiological characteristics of this group, less emphasize should be on muscle strength and more on movement quality [1, 24]. In this age category, only paediatric PROMs are recommended to evaluate subjective outcomes [13]. Furthermore, it is important in all age categories to compare the postoperative values with preoperative test outcomes and/or reference values to assess postoperative deterioriation of muscle strength of the uninvolved limb. Normalized strength for body weight, compared to reference values, may also provide information about muscle strength [10].
Recommendations for further research
Future research should aim at validating specific tests in children after ACL injury and after ACL reconstruction. Validation includes measuring reliability, validity and responsiveness, as these variables are unknown of many RTS tests [8]. There should be more focus on the movement quality as a test for RTS clearance, as altered neuromuscular function and biomechanics could be a risk factor for a second ACL rupture [40]. Besides, there are individual differences in neuromotor learning capacity and flexibility, this underlines the importance of the shift from time-based rehabilitation to a patientspecific goal-based rehabilitation [40]. The aim should be to develop a test battery measuring clinical outcomes, strength tests, hop tests, movement quality and PROMs based on a goal-based rehabilitation in a sport-specific context [8, 40]. As most of the studies evaluated tests in an adolescent population, we also recommend to aim future research at younger children (< 16 years of age) and to evaluate differences between the sexes. Since no studies have been conducted in non-operative patients, future research should also aim at this population. Tests regarding RTS after non-operative treatment may especially be relevant for skeletally immature children, as these children are often treated non-operatively [1].
Conclusion
Many studies on tests regarding RTS have been conducted among adolescents after ACL reconstruction, while there are only few studies evaluating tests among younger children. Strength tests, movement quality and PROMs are most frequently evaluated and are useful to determine readiness for return to sport. Further research should aim at younger children and at developing and validating a test battery including movement quality and neuromotor control in a sport-specific context in both operative and non-operative patients.
Supplementary information
Acknowledgements
The authors of this paper would like to thank Roderick Wondergem, lecturer at Fontys University of Applied Sciences in Eindhoven, for providing valuable help at the start of this project.
Abbreviations
- ACL
Anterior cruciate ligament
- ACLR
Anterior Cruciate ligament reconstruction
- ACL RELAY
Anterior Cruciate Ligament REconstruction Long-term outcomes in Adolescents and Young adults
- ACL-RSI
Anterior Cruciate Ligament - Return to Sport after Injury
- (Pedi-)IKDC
(Paediatric) International Knee Documentation Committee Subjective Knee Form
- IOC
International Olympic Committee
- KOOS(−Child)
Knee injury and Osteoarthritis Outcome Score (−Child)
- KT-1000 Arthrometer
Knee laxity Testing device 1000 Arthrometer
- LSI
Limb Symmetry Index
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PROMs
Patient Reported Outcomes Measures
- RTS
Return To Sport
Authors’ contributions
MD was the main and corresponding author, participated in study selection and data collection process. MB was the initiator of the project, participated in study selection and data collection process. MvdS was a critical reviewer of the manuscript and contributed to the methods of this scoping review. ED was the information specialist performing the search and supported in the study selection process. RJ was also the initiator of the project, a critical reviewer based on clinical expertise and a native speaker. NvM was also the initiator of the project, a critical reviewer based on clinical expertise and participated in data collection process. The author(s) read and approved the final manuscript.
Funding
Have not received financial support.
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s40634-020-00298-8.
References
- 1.Ardern CL, Ekås GR, Grindem H, Moksnes H, Anderson AF, Chotel F, et al. 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. Br J Sports Med. 2018;52(7):422–438. doi: 10.1136/bjsports-2018-099060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ardern CL, Glasgow P, Schneiders A, Witvrouw E, Clarsen B, Cools A, et al. 2016 consensus statement on return to sport from the first world congress in sports physical therapy, BernBr. J Sports Med. 2016;50:853–864. doi: 10.1136/bjsports-2016-096278. [DOI] [PubMed] [Google Scholar]
- 3.Astur DC, Novaretti JV, Cavalcante ELB, Goes A, Jr, Kaleka CC, Debieux P, et al. Pediatric anterior cruciate ligament Reruptures are related to lower functional scores at the time of return to activity: a prospective, midterm follow-up study. Orthop J Sports Med. 2019;7(12):2325967119888888. doi: 10.1177/2325967119888888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beischer S, Hamrin Senorski E, Thomeé C, Samuelsson K, Thomeé R. How is psychological outcome related to knee function and return to sport among adolescent athletes after anterior cruciate ligament reconstruction? Am J Sports Med. 2019;47(7):1567–1575. doi: 10.1177/0363546519843073. [DOI] [PubMed] [Google Scholar]
- 5.Benjaminse A, Holden S, Myer GD. ACL rupture is a single leg injury but a double leg problem: too much focus on ‘symmetry' alone and that’s not enough! Br J Sports Med. 2018;52:1029–1030. doi: 10.1136/bjsports-2017-098502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bergeron MF, Mountjoy M, Armstrong N, Chia M, Côté J, Emer CA, et al. International Olympic Committee consensus statement on youth athletic development. Br J Sports Med. 2015;49(13):843–851. doi: 10.1136/bjsports-2015-094962. [DOI] [PubMed] [Google Scholar]
- 7.Boyle MJ, Butler RJ, Queen RM. Functional movement competency and dynamic balance after anterior cruciate ligament reconstruction in adolescent patients. J Pediatr Orthop. 2016;36(1):36–41. doi: 10.1097/BPO.0000000000000402. [DOI] [PubMed] [Google Scholar]
- 8.Burgi CR, Peters S, Ardern CL, Magill JR, Gomez CD, Sylvain J, Reiman MP. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br J Sports Med. 2019;53(18):1154–1161. doi: 10.1136/bjsports-2018-099982. [DOI] [PubMed] [Google Scholar]
- 9.Burland JP, Kostyun RO, Kostyun KJ, Solomito M, Nissen C, Milewski MD. Clinical outcome measures and return-to-sport timing in adolescent athletes after anterior cruciate ligament (ACL) reconstruction. J Athl Train. 2018;53(5):442–451. doi: 10.4085/1062-6050-302-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Capin JJ, Khandha A, Zarzycki R, Manal K, Buchanan TS, Snyder-Mackler L. Gait mechanics and second ACL rupture: implications for delaying return-to-sport. J Orthop Res. 2017;35(9):1894–1901. doi: 10.1002/jor.23476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clagg S, Paterno MV, Hewett TE, Schmitt LC. Performance on the modified star excursion balance test at the time of return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2015;45(6):444–452. doi: 10.2519/jospt.2015.5040. [DOI] [PubMed] [Google Scholar]
- 12.Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99(11):897–904. doi: 10.2106/JBJS.16.00758. [DOI] [PubMed] [Google Scholar]
- 13.Dietvorst M, Reijman M, van Groningen B, van der MC S, Janssen RPA. PROMs in pediatric knee ligament injury: use the Pedi-IKDC and avoid using adult PROMs. Knee Surg Sports Traumatol Arthrosc. 2019;27(6):1965–1973. doi: 10.1007/s00167-017-4687-3. [DOI] [PubMed] [Google Scholar]
- 14.Fryer C, Ithurburn MP, McNally MP, Thomas S, Paterno MV, Schmitt LC. The relationship between frontal plane trunk control during landing and lower extremity muscle strength in young athletes after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon) 2019;62:58–65. doi: 10.1016/j.clinbiomech.2018.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fabricant PD, Brusalis CM, Schachne JM, PLUTO Study Group. Matava MJ. Which metrics are being used to evaluate children and adolescents after ACL reconstruction? A systematic review. Arthrosc Sports Med Rehabil. 2020;2(4):e417–e428. doi: 10.1016/j.asmr.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hannon J, Wang-Price S, Swank C, Brizzolara K, Garrison C, Bothwell J, et al. The validity and reliability of the Vail sport test™ as a measure of performance following anterior cruciate ligament reconstruction. Phys Ther Sport. 2019;38:162–169. doi: 10.1016/j.ptsp.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Hughes G, Musco P, Caine S, Howe L. Lower limb asymmetry after anterior cruciate ligament reconstruction in adolescent athletes: a systematic review and meta-analysis. J Athl Train. 2020;55(8):811–825. doi: 10.4085/1062-6050-0244-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ithurburn MP, Paljieg A, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Strength and function across maturational levels in young athletes at the time of return to sport after ACL reconstruction. Sports Health. 2019;11(4):324–331. doi: 10.1177/1941738119849070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ithurburn MP, Altenburger AR, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):426–433. doi: 10.1007/s00167-017-4678-4. [DOI] [PubMed] [Google Scholar]
- 20.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes after anterior cruciate ligament reconstruction with single-leg landing asymmetries at the time of return to sport demonstrate decreased knee function 2 years later. Am J Sports Med. 2017;45(11):2604–2613. doi: 10.1177/0363546517708996. [DOI] [PubMed] [Google Scholar]
- 21.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am J Sports Med. 2015;43(11):2727–2737. doi: 10.1177/0363546515602016. [DOI] [PubMed] [Google Scholar]
- 22.Ithurburn MP, Paterno MV, Thomas S, Pennell ML, Evans KD, Magnussen RA, et al. Clinical measures associated with knee function over two years in young athletes after ACL reconstruction. Knee. 2019;26(2):355–363. doi: 10.1016/j.knee.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McPherson AL, Feller JA, Hewett TE, Webster KE. Psychological readiness to return to sport is associated with second anterior cruciate ligament injuries. Am J Sports Med. 2019;47(4):857–862. doi: 10.1177/0363546518825258. [DOI] [PubMed] [Google Scholar]
- 24.Moksnes H, Engebretsen L, Risberg MA. Performance-based functional outcome for children 12 years or younger following anterior cruciate ligament injury: a two to nine-year follow-up study. Knee Surg Sports Traumatol Arthrosc. 2008;16(3):214–223. doi: 10.1007/s00167-007-0469-7. [DOI] [PubMed] [Google Scholar]
- 25.Moksnes H, Engebretsen L, Risberg MA. The current evidence for treatment of ACL injuries in children is low: a systematic review. J Bone Joint Surg Am. 2012;94(12):1112–1119. doi: 10.2106/JBJS.K.00960. [DOI] [PubMed] [Google Scholar]
- 26.Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myer GD, Martin L, Jr, Ford KR, Paterno MV, Schmitt LC, Heidt RS, Jr, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012;40(10):2256–2263. doi: 10.1177/0363546512454656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan — a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Palmieri-Smith RM, Strickland M, Lepley LK. Hamstring muscle activity after primary anterior cruciate ligament reconstruction—a protective mechanism in those who do not sustain a secondary injury? A preliminary study. Sports health. 2019;11(4):316–323. doi: 10.1177/1941738119852630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paterno MV, Flynn K, Thomas S, Schmitt LC. Self-reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health. 2018;10(3):228–233. doi: 10.1177/1941738117745806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paterno MV, Kiefer AW, Bonnette S, Riley MA, Schmitt LC, Ford KR, et al. Prospectively identified deficits in sagittal plane hip–ankle coordination in female athletes who sustain a second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Clin Biomech (Bristol, Avon) 2015;30(10):1094–1101. doi: 10.1016/j.clinbiomech.2015.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Hewett TE. Altered postural sway persists after anterior cruciate ligament reconstruction and return to sport. Gait Posture. 2013;38(1):136–140. doi: 10.1016/j.gaitpost.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE. Strength asymmetry and landing mechanics at return to sport after ACL reconstruction. Med Sci Sports Exerc. 2015;47(7):1426–1434. doi: 10.1249/MSS.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42(9):750–759. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Toole AR, Ithurburn MP, Rauh MJ, Hewett TE, Paterno MV, Schmitt LC. Young athletes cleared for sports participation after anterior cruciate ligament reconstruction: how many actually meet recommended return-to-sport criterion cutoffs? J Orthop Sports Phys Ther. 2017;47(11):825–833. doi: 10.2519/jospt.2017.7227. [DOI] [PubMed] [Google Scholar]
- 37.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 38.Trulsson A. Additional perspectives on ‘ACL rupture is a single leg injury but a double leg problem … '. Br J Sports Med. 2018;53(16):993–995. doi: 10.1136/bjsports-2017-098974. [DOI] [PubMed] [Google Scholar]
- 39.van der Velden CA, van der Steen MC, Leenders J, van Douveren FQMP, Janssen RPA, Reijman M. Pedi-IKDC or KOOS-child: which questionnaire should be used in children with knee disorders? BMC Musculoskelet Disord. 2019;20(1):240. doi: 10.1186/s12891-019-2600-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Melick N, van Cingel RE, Brooijmans F, Neeter C, van Tienen T, Hullegie W, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506–1515. doi: 10.1136/bjsports-2015-095898. [DOI] [PubMed] [Google Scholar]
- 41.Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport. 2008;9(1):9–15. doi: 10.1016/j.ptsp.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 42.Wellsandt E, Failla MJ, Snyder-Mackler L. Limb symmetry indexes can overestimate knee function after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2017;47(5):334–338. doi: 10.2519/jospt.2017.7285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wren TAL, Mueske NM, Brophy CH, et al. Hop distance symmetry does not indicate Normal landing biomechanics in adolescent athletes with recent anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2018;48(8):622–629. doi: 10.2519/jospt.2018.7817. [DOI] [PubMed] [Google Scholar]
- 44.Zwolski C, Schmitt LC, Quatman-Yates C, Thomas S, Hewett TE, Paterno MV. The influence of quadriceps strength asymmetry on patient-reported function at time of return to sport after anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(9):2242–2249. doi: 10.1177/0363546515591258. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.