Abstract
Introduction: Population aging is increasing the needs and costs of healthcare. Both frailty and the chronic diseases affecting older people reduce their ability to live independently. However, most older people prefer to age in their own homes. New development of in-home monitoring can play a role in staying independent, active, and healthy for older people. This 12-month observational study aimed to evaluate a new in-home monitoring system among home-dwelling older adults (OA), their family caregivers (FC), and nurses for the support of home care.
Methods: The in-home monitoring system evaluated in this study continuously monitored OA's daily activities (e.g., mobility, sleep habits, fridge visits, door events) by ambient sensor system (DomoCare®) and health-related events by wearable sensors (Activity tracker, ECG). In the case of deviations in daily activities, alerts were transmitted to nurses via email. Using specific questionnaires, the opinions of 13 OA, 13 FC, and 20 nurses were collected at the end of 12-months follow-up focusing on user experience and the impact of in-home monitoring on home care services.
Results: The majority of OA, FC, and nurses considered that in-home sensors can help with staying at home, improving home care and quality of life, preventing domestic accidents, and reducing family stress. The opinion tended to be more frequently favorable toward ambient sensors (76%; 95% CI: 61–87%) than toward wearable sensors (Activity tracker: 65%; 95% CI: 50–79%); ECG: 60%; 95% CI: 45–75%). On average, OA (74%; 95% CI: 46–95%) and FC (70%; 95% CI: 39–91%) tended to be more enthusiastic than nurses (60%; 95% CI: 36–81%). Some barriers reported by nurses were a fear of weakening of the relationship with OA and lack of time.
Discussion/Conclusion: Overall, the opinions of OA, FC, and nurses were positively related to in-home sensors, with nurses being less enthusiastic about their use in clinical practice.
Keywords: gerontechnology, patient satisfaction, monitoring technologies, home care, older people
Introduction
The population is aging in Europe and worldwide (1), including in Switzerland in which people over 65 years of age are anticipated to account for more than 25% of the population by 2050 (2). Population aging combined with the high costs of healthcare brings many challenges for healthcare systems, long-term care, and management of age-related chronic diseases (3). A recent study underlines that 79% of health costs in Switzerland are linked to chronic diseases (4, 5). With population aging, the prevalence of chronic diseases is increasing, resulting in rising healthcare needs and increasing costs. Additionally, both frailty and chronic diseases affecting older people reduce their ability to live independently. However, most older people prefer to age in their own homes (6, 7).
In response to these challenges, monitoring, and assistive technologies, such as emergency help systems, vital sign monitoring, or fall detection systems, can be a solution to support home care of older people to help them stay independent and active for a longer time (8–11). Currently, ambient sensors (12–15), also known as ambient living sensors, and wearable devices (16, 17) are used in the homes of older people to monitor changes in health status, to detect falls, or to monitor activities of daily living (18–23). Such technologies can allow older people to better connect and communicate with their healthcare professionals as well as with their families.
A literature review on monitoring technologies has suggested that a combination of monitoring technologies including ambient and wearable sensors technologies is probably the most effective solution in independently living older people (24). However, such an in-home monitoring system needs to be evaluated in a real-life setting to demonstrate the potential to prolong independent living of older people (24).
The objective of this 12-month observational study was therefore to evaluate the usability, functionality, and effects of a new in-home monitoring system—combining ambient and wearable sensors—among home-dwelling older adults (OA), their family caregivers (FC), and nurses for the support of home care, focusing on their end user experience and the impact of these technologies on the daily practice in home care service (25).
Materials and Methods
Study Design and Setting
This 12-month observational study was conducted among older people living independently at home and followed by nurses from NOMAD, the Neuchâtel public home care association, located in Switzerland, between January 2017 and July 2018. The study was approved by the Ethics Committee of the canton of Vaud, Switzerland (CER-VD ID: 2016-00762), and conducted based on principles declared in the Declaration of Helsinki. A written informed consent was obtained from all participating patients before study participation. We obtained the copyright holder permission to use and publish on the ambient sensor system (DomoCare®) by DomoSafety S.A.
Study Participants and In-Home Monitoring System
Patients for participation were identified and recruited by NOMAD nurses in collaboration with a research assistant (BP) through the NOMAD database if they met the following inclusion criteria: (1) home-dwelling older adults (OA ≥70 years) living alone at home and without pets; (2) followed by nurses from NOMAD, Neuchâtel public home care association; (3) speak and read in French. Exclusion criteria were (1) severe cognitive impairment unable to follow study protocol (clock-drawing score ≥ 4); (2) skin problems, such as irritations, itching, serious redness; (3) undergoing dialysis; (4) not willing to comply with the study protocol; (5) unable to understand the study aim; (6) hospitalization planned in a short period of time.
After potential eligible patients' screening, patients who were likely to meet inclusion criteria were approached in person during a phone call or a visit of research assistant (BP), given an information letter if they expressed an interest in participating, and scheduled an appointment at home. Once the eligible patient agreed to participate and provided a written consent form, an in-home monitoring system comprising the ambient sensors [DomoCare®, DomoSafety S.A, Lausanne, Switzerland (26)] and wearable sensors (ECG, Activity tracker) was installed, respectively at home and on the patient's chest and wrist. In-home monitoring was conducted for 12 months.
Data Collection and In-Home Monitoring System
During the 12 months of follow-up, the in-home monitoring system continuously monitored different OA's daily activities (e.g., mobility, sleep habits, fridge visits, door events) by ambient sensors (DomoCare®) and health-related events (e.g., physical activity and mobility, heart rate, skin temperature) by wearable sensors (Activity tracker, ECG). More precisely, the following data were recorded by wearable sensors: ECG signal, heart rate, heart rate variability, skin temperature, and respiration rate, as well as physical activity and mobility detected by accelerometer. The ECG sensor of type Preventice BodyGuardian was composed of a small and light battery powered device that was directly applied on the chest of the OA using a dry electrode and silicone-based adhesive patch. The data of the ECG sensor was automatically collected and transferred wirelessly from the sensor to a dedicated mobile phone and uploaded to servers for further analyses. The wearable Activity tracker, worn on the wrist of OA, was recorded and transmitted physical activity data (e.g., movement, number of steps) as well as heart rate.
Ambient motion sensors, installed in each apartment, recorded the OA's daily activities by passive infrared sensor (PIR) technology placed in the living room, bedroom, kitchen, and bathroom. Additional sensors were placed on the fridge and entrance door, measuring opening and closing of the door, and under the bed mattress, measuring bed presence, sleep cycles, respiration, and vital signs. The collected data were transmitted to servers for analysis by a base station. Data were then interpreted and subjected to trend analysis to detect changes in ADL and prevent changes in health status. In case of deviations in activities of daily living (e.g., changes in mobility), alerts were transmitted to nurses via email, using a report with weekly patient's activity graph and information summarizing the deviation detected by ambient sensors (e.g., decrease of patient's mobility for 3 days).
Data Collection and Satisfaction of Home-Dwelling Older Adults, Family Caregivers, and Nurses
At the end of follow-up, specific self-administered mailed questionnaires were used to obtain users' satisfaction of OA, their family caregivers (FC), and nurses related to the in-home monitoring system and its impact on home care services. There were 20 nurses and 12 OAs. Nurses usually have care for several OAs and conversely OAs are usually cared for by more than one nurse. For each of the 20 nurses invited to respond to the questionnaire, an associated patient was randomly selected. Random selection was conducted by a statistician and restricted to combinations including the 12 OAs. This process had no impact on data collection.
Data were collected among 13 OA who completed the 1-year questionnaire, 13 family caregivers who play a central role as full partner in care and well-being of OA, and 20 nurses. Semi-structured interviews face-to-face or phone calls were conducted by a research assistant (BP) to complete the answers of the questionnaires described below.
The questionnaires filled by OA and nurses were based on the French version of the instrument titled the Quebec User Evaluation of Satisfaction with assistive Technology (QUEST) by Demers et al. (27), and the questionnaire filled by FC was based on the caregiver quality of life scale developed and validated in France from data of the Pixel studies (28). These three questionnaires included open- and closed-ended response options, with additional questions on OA, FC, and nurse opinions', satisfaction, and practical experiences related to the in-home monitoring.
The questionnaires assessed 4 items: (1) opinion on the usefulness of ambient and wearable sensors; (2) satisfaction of OA, FC, and nurse with ambient and wearable sensors; (3) impact of sensors on the relationship between OA, FC, and nurse; (4) impact on in home care practice (integration and barriers). Answers to questionnaires were dichotomous (yes/no) or graduated on a five-point Likert scale, ranging from “a lot” to “not at all.”
The construction, relevance, and comprehensiveness of questionnaires were assessed among five OA and one NOMAD nurse to ensure that they were easily understandable, well-defined, and accurately addressed the goals of the study.
Statistical and Data Analysis
Descriptive statistics were used to present baseline characteristics of OA and results related to ambient and wearable sensors as number, percentage, and score average. Overall opinion was calculated as weighted percentage. For the main results, 95% binomial confidence intervals (CI) were built around this percentage (command stata: cii proportion), i.e., the overall opinion and satisfaction of participants. All statistical analyses were performed using Stata software version 15.0 (Stata Corp, College Station, TX, USA) and Excel.
Results
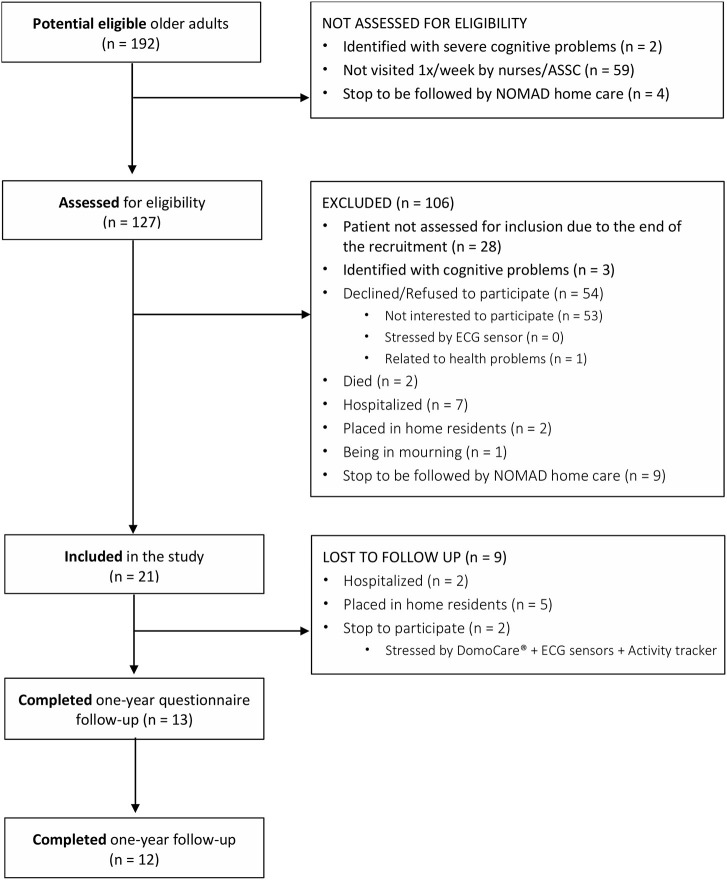
The study design and flow-chart of patients are presented in Figure 1. Among the 192 potential eligible OA, 127 OAs were assessed for eligibility, 54 (42.5%) refused to participate, and 52 (40.9%) were excluded during the process (e.g., hospitalization, cognitive problems, death, placed in home residents). A total of 21 were included in the study, and 12 completed the 1-year of follow-up. The remaining 9 patients could not be contacted as a result of hospitalization and institutionalization. A total of 13 patients completed the 1-year questionnaire follow-up.
Figure 1.
Flow diagram of home-dwelling older adults.
Characteristics of Patients
The baseline characteristics of the 21 included patients are shown in Table 1. The mean age was 85 years, half were men, and half received home care for more than 1 year. Patients took on average 9 drugs daily, 90% of patients were treated with 5 drugs or more per day, and 81% reported using a weekly pillbox to facilitate their drug intake. During the follow-up, 43% of patients were hospitalized at least once. Most patients were diagnosed with comorbidities, such as cardiovascular diseases, hypertension, dyslipidaemia, and diabetes.
Table 1.
Baseline characteristics of included older adults.
| Characteristics | |
|---|---|
| Number of patients | 21 |
| Men/women, n | 11/10 |
| Mean age, years (SD) [range] | 85 (7) [72–96] |
| Mean body mass index, kg/m2 (SD) | 26 (5) |
| Marital status | |
| Single, n (%) | 1 (5%) |
| Married, n (%) | 0 (0%) |
| Divorced, n (%) | 2 (10%) |
| Widowed, n (%) | 18 (86%) |
| Nationality | |
| Swiss, n (%) | 19 (90%) |
| No-Swiss, n (%) | 2 (10%) |
| Comorbidities | |
| Current smoker (≥1 cigarette/day), n (%) | 0 (0%) |
| Cardiovascular diseases, n (%) | 16 (76%) |
| Diabetes mellitus, n (%) | 4 (19%) |
| Hypertension, n (%) | 15 (71%) |
| Dyslipidaemia, n (%) | 8 (38%) |
| Chronic kidney disease, n (%) | 0 (0%) |
| Number of drugs, n (SD) [range] [median] | 9 (5) [3–20] [9] |
| Polymedication (5 drugs or more), n (%) | 19 (90%) |
| Using a weekly pillbox, n (%) | 17 (81%) |
SD, standard deviation.
Overall Opinion and Satisfaction
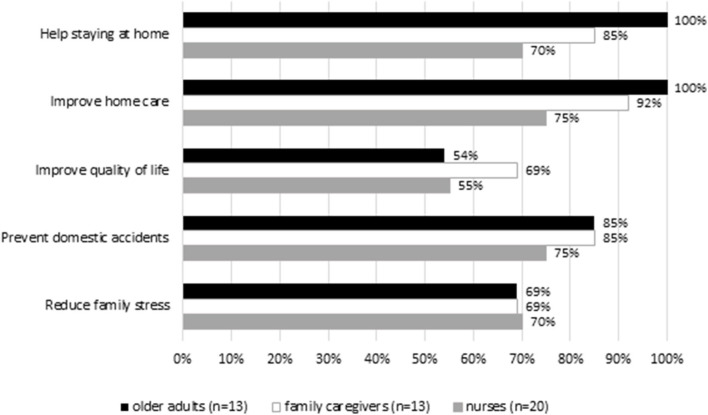
The majority of OA, FC, and nurses considered that in-home sensors (ambient and wearable) can help staying at home, improving home care and quality of life, preventing domestic accidents, and reducing family stress (Table 2). The opinion tended to be more frequently favorable toward ambient sensors (76%; 95% CI: 61–87%) than toward Activity tracker (65%; 95% CI: 50–79%) and ECG (60%; 95% CI: 45–75%). On average, OA (74%; 95% CI: 46–95%) and FC (70%; 95% CI: 39–91%) tended to be more enthusiastic than nurses (60%; 95% CI: 36–81%).
Table 2.
Opinion on the usefulness of ambient (DomoCare®) and wearable sensors (Activity tracker, ECG) to help staying at home, improving home care, improving quality of life, preventing domestic accidents, or reducing family stress.
| Older adults (n = 13) (%) | Family caregivers (n = 13) (%) | Nurses (n = 20) (%) | Average (n = 46) (%) | |
|---|---|---|---|---|
| DomoCare® | 82 | 80 | 69 | 76 |
| Activity tracker | 63 | 69 | 63 | 65 |
| ECG sensor | 76 | 60 | 49 | 60 |
| Average | 74 | 70 | 60 |
Opinion and Satisfaction on the Ambient Sensor System (DomoCare®)
As shown in Figure 2, most of OA and FC rated higher ambient sensors (DomoCare®) in helping staying at home (OA: 100%, FC: 85%), improving home care (OA: 100%; FC: 92%), preventing domestic accidents (OA: 85%; FC: 85%), and reducing family stress. The FC (69%) rated higher in-home sensors in improving quality of life compared to OA (54%) and nurses. More than half of OA (69%), FC (69%), and nurses (70%) considered ambient sensors can help reducing family stress. Overall, the majority of OA were satisfied with DomoCare®. Nurses tended to be less enthusiastic than OA, particularly regarding the technical (e.g., dimension, solidity) and practical settings of ambient sensors (e.g., ease of installation and use; Supplementary Figure 1).
Figure 2.
Opinion on the ambient sensor system (DomoCare®).
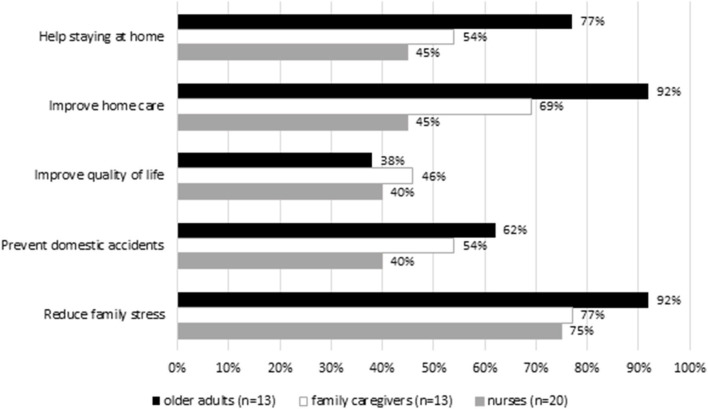
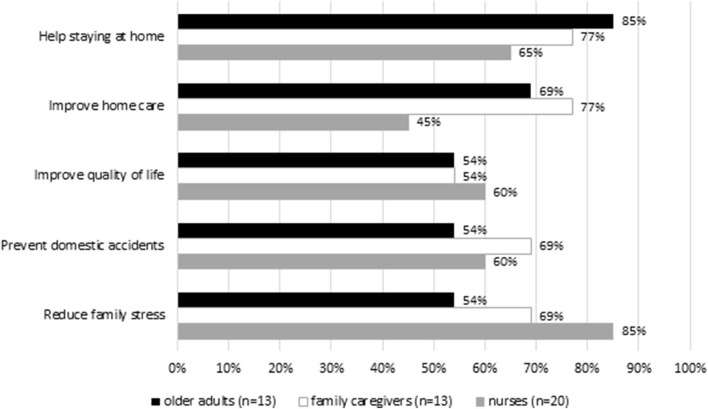
Opinion and Satisfaction on the Wearable Sensors (ECG and Activity Tracker)
Regarding the wearable sensors (Figures 3, 4), most of OA and FC rated higher activity tracker in helping staying at home (OA: 85%; FC: 77%) and improving home care (OA: 69%; FC: 77%) compared to ECG. Most nurses rated higher activity tracker in improving quality of life (60%) and reducing family stress (85%). Regarding the ECG, the majority of the OA (92%), FC (77%), and nurses (75%) underlined that ECG can help reduce family stress. More than half of OA, FC, and nurses were skeptical regarding the prevention of domestic accidents for the wearable sensors [activity tracker (OA: 54%; FC: 69%; nurses: 60%); ECG (OA: 62%; FC: 54%; nurses: 40%)]. Overall, OA and nurses were satisfied with the Activity tracker and ECG. However, nurses tended to be less enthusiastic than OA, particularly with ECG, reporting that wearable sensors should be made smaller, lighter, and more comfortable (Supplementary Figures 2, 3).
Figure 3.
Opinion on the wearable sensor (ECG).
Figure 4.
Opinion on the wearable sensor (Activity tracker).
Events and Nurse Interventions
A total of 76 events were detected by DomoCare® (on average 4 events/patients; range 0–12 events). Each of them generated a preventive report validated by a research assistant (BP) and was transferred to NOMAD nurses by email. Events corresponded to changes in mobility behavior (26/76, 34%), in toilet usage frequency (24/76, 32%), in fridge usage (11/76, 14%), in entrance door usage (4/76, 5%), in time spent out of home (2/76, 3%), and in time spent in bed (9/76, 12%). For all events, nurses followed up with a home visit.
Integration of In-Home Monitoring Technology in Home Care Practice
Overall, the majority of nurses considered in-home sensors (DomoCare®: 65%; ECG: 55%; Activity tracker: 70%) easily implementable in their practice. However, nurses considered work overload, lack of time, and cumbersome procedures, especially for DomoCare® and ECG, and fear of weakening of the relationship with OA, as barriers to implementing in-home sensors (Supplementary Figure 4). Less than 50% of nurses reported lack of remuneration as a barrier. Finally, the majority of OA, FC, and nurses reported that they would like to continue using in-home sensors in case of insurance reimbursement.
Discussion
This 12-month observational study showed that the majority of OA, FC, and nurses valued in-home monitoring systems including ambient and wearable sensors, notably to help staying at home, improving home care, preventing domestic accidents, and reducing family stress. On average, OA and FC tended to be more enthusiastic than nurses about this in-home monitoring system. Moreover, some barriers were reported by nurses, such as a fear of weakening of the relationship with OA and an excessive surveillance. Overall, the opinions of OA, FC, and nurses were positively related to in-home technology, with nurses being less enthusiastic about their use in clinical practice.
Comparison With Other Studies
Our findings suggested a variety of benefits and positive potential impacts of in-home monitoring on quality of life of OA and nursing home care services. As described by previous studies (29–34), the majority of OA, FC, and nurses were not familiar with in-home monitoring technologies. However, they considered that such technologies can be relevant in the future by improving the quality of care among OA living independently at home. Moreover, the previous studies underlined that the acceptance and the use of in-home technologies by OA were often influenced by social network and pointed work overload of nurses, cost, and lack of funding to be barriers to implement in-home monitoring technologies.
In our study, OA and FC tended to be more enthusiastic than nurses regarding new in-home technologies. These results are consistent with other studies (29–34) showing that OA perceived in-home technologies as a viable home care solution, which can prolong their time living at home, whereas nurses had concerns that such technology could weaken their relationship with OA and worsen their work conditions.
Strengths and Limitations of the Study
Strengths of our study are mainly (1) the close collaboration between OA, FC, nurses, researchers, and engineers; (2) the innovative use of assistive and digital technologies designed to support independent community older adults; and (3) the collection data on the use of in-home monitoring devices. Furthermore, all OA who completed the 12-month follow-up, all nurses, and all FC filled out the questionnaires. However, we acknowledge some limitations to our study. Due to logistical and financial reasons, the study sample was small. There was also a high loss to follow-up notably due to hospitalization and moving to a nursing home, which are frequent events among this type of patients. Furthermore, for logistical reasons, the study was conducted in only one place, which limits its external validity. Further studies are therefore needed to evaluate the transferability of our findings to other regions and populations. We did not use a specific theoretical acceptance model in this study, but further studies would gain from doing so. Finally, we tested one in-home monitoring system and a given set of sensors, and our findings may therefore not apply to other systems or individual sensors.
Future Perspective
In conclusion, OA, FC, and nurses were very or quite positively related to DomoCare®, Activity tracker, and ECG sensors and reported that in-home monitoring technologies may facilitate home care and opened good perspectives for use in home care practice. Further studies, at a larger scale, are needed to evaluate how this type of in-home monitoring can help patients stay longer at home, improve health care management, and reduce healthcare costs. Further, some manufacturing improvements (e.g., development of sensors that are smaller, lighter, and more user-friendly and comfortable for OA, as well as advances in machine learning for detection of specific events at home) and training of nurses in the use of these monitoring systems should be considered, to ease their use, increase comfort of end-users, and preserve and strengthen the relationship between OA and nurses are key for implementing these new technologies in nursing home care practice (32–39).
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.
Ethics Statement
The study was reviewed and approved by CER-VD: Cantonal Ethics Committee of Vaud on Research involving humans. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BP, PB, GD, TN, NS, HS, DG-P and VS designed and planned the study. DomoSafety S.A. installed and maintained the wearable sensors (ECG, Activity tracker) and ambient sensor system (DomoCare®) monitoring the participants. BP and NS measured participants. BP and VS analyzed data from the questionnaires filled out by the participants, their families and nurses at the end of follow-up, and wrote the manuscript. All authors reviewed and approved the final manuscript.
Conflict of Interest
PB and GD are employed by DomoSafety S.A., which is the manufacturer of the displayed ambient sensor system (DomoCare®). The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank the participants for their participation in this study as well as NOMAD, Neuchâtel Public Home care association, Hélène Reynaud Senes (NOMAD), Ms. Agnes Vrolixs (NOMAD), the team leaders, and the nurses for their support and contribution in recruitment and follow-up participants in the study. We also thank MySmartHeart AG for their support in using the ECG sensors. Finally, we thank Arnaud Chiolero for his assistance in statistical analyses. We certify that the original work presented in this paper has not been published previously and is not under consideration for publication elsewhere. Parts of these findings were submitted as an abstract and presented as a pitch presentation at the 12th European Public Health Conference in 2019, Marseille, France, on 20–23.11.2019 (25).
Footnotes
Funding. This study was funded by CTI/Innosuisse—the Swiss Innovation Agency—through the SWISKO project (17662.2 PFES-ES).
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.518957/full#supplementary-material
References
- 1.United Nations, Department of Economic and Social Affairs Population Division World Population Ageing 2013. ST/ESA/SER.A/348. (2013). Available online at: https://www.un.org/en/development/desa/population/publications/index.asp (accessed November 15, 2019).
- 2.Kucera J, Krummenacher A. La population de la Suisse 2016. Fédéral Statistique. (2017) 349–1600. [Google Scholar]
- 3.Stucki RA, Urwyler P, Rampa L, Müri R, Mosimann UP, Nef T. A web-based non-intrusive ambient system to measure and classify activities of daily living. J Med Internet Res. (2014) 16:e175. 10.2196/jmir.3465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. (2019) 374:1196–208. 10.1016/S0140-6736(09)61460-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wieser S, Riguzzi M, Pletscher M, Huber CA, Telser H, Schwenkglenks M. How much does the treatment of each major disease cost? A decomposition of Swiss National Health Accounts. Eur J of Health Econ. (2018) 19:1149–61. 10.1007/s10198-018-0963-5 [DOI] [PubMed] [Google Scholar]
- 6.Kane RL, Kane RA. What older people want from long-term care, and how they can get it. Health Aff (Millwood). (2001) 20:114–27. 10.1377/hlthaff.20.6.114 [DOI] [PubMed] [Google Scholar]
- 7.Oswald F, Wahl HW, Schilling O, Nygren C, Fange A, Sixsmith A, et al. Relationships between housing and healthy aging in very old age. Gerontologist. (2007) 47:96–107. 10.1093/geront/47.1.96 [DOI] [PubMed] [Google Scholar]
- 8.Boulos MN, Lou RC, Anastasiou A, Nugent CD, Alexandersson J, Zimmermann G, et al. Connectivity for healthcare and well-being management: examples from six European projects. Int J Environ Res Public Health. (2009) 6:1947–71. 10.3390/ijerph6071947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ni Q, García Hernando AB, de la Cruz IP. The elderly's independent living in smart homes: a characterization of activities and sensing infrastructure survey to facilitate services development. Sensors. (2015) 15:11312–62. 10.3390/s150511312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peek ST, Wouters EJ, van Hoof J, Luijkx KG, Boeije HR, Vrijhoef HJM. Factors influencing acceptance of technology for aging in place: a systematic review. Int J Med Inform. (2014) 83:235–48. 10.1016/j.ijmedinf.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 11.Uddin MZ, Khaksar W, Torresen J. Ambient sensors for elderly care and independent living: a survey. Sensors. (2018) 18:2027. 10.3390/s18072027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stefanov DH, Bien Z, Bang WC. The smart house for older persons and persons with physical disabilities: structure, technology arrangements, and perspectives. IEEE Trans Neural Syst Rehabil Eng. (2004) 12:228–50. 10.1109/TNSRE.2004.828423 [DOI] [PubMed] [Google Scholar]
- 13.Zouba N, Bremond F, Thonnat M. An activity monitoring system for real elderly at home: validation study. IEEE. (2010) 278–85. 10.1109/AVSS.2010.83 [DOI] [Google Scholar]
- 14.Kaye JA, Maxwell SA, Mattek N, Hayes TL, Dodge H, Pavel M, et al. Intelligent Systems For Assessing Aging Changes: home-based, unobtrusive, and continuous assessment of aging. J Gerontol B Psychol Sci Soc Sci. (2011) 66(Suppl. 1):i180–90. 10.1093/geronb/gbq095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Q, Karunanithi M, Rana R, Liu J. Determination of activities of daily living of independent living older people using environmentally placed sensors. Conf Proc IEEE Eng Med Biol Soc. (2013) 2013:7044–7. 10.1109/EMBC.2013.6611180 [DOI] [PubMed] [Google Scholar]
- 16.de Bruin ED, Hartmann A, Uebelhart D, Murer K, Zijlstra W. Wearable systems for monitoring mobility-related activities in older people: a systematic review. Clin Rehabil. (2008) 22:878–95. 10.1177/0269215508090675 [DOI] [PubMed] [Google Scholar]
- 17.Yilmaz T, Foster R, Hao Y. Detecting vital signs with wearable wireless sensors. Sensors (Basel). (2010) 10:10837–62. 10.3390/s101210837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel S, Park H, Bonato P, Chan L, Rodgers M. A review of wearable sensors and systems with application in rehabilitation. J Neuroeng Rehabil. (2012) 9:21. 10.1186/1743-0003-9-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rantz MJ, Skubic M, Miller SJ, Galambos C, Alexander G, Keller J, et al. Sensor technology to support aging in place. J Am Med Dir Assoc. (2013) 14:386–91. 10.1016/j.jamda.2013.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dasios A, Gavalas D, Pantziou G, Konstantopoulos C. Hands-on experiences in deploying cost-effective ambient-assisted living systems. Sensors. (2015) 15:14487–512. 10.3390/s150614487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nef T, Urwyler P, Büchler M, Tarnanas I, Stucki R, Cazzoli D, et al. Evaluation of three state-of-the-art classifiers for recognition of activities of daily living from smart home ambient data. Sensors. (2015) 15:11725–40. 10.3390/s150511725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pais B, Buluschek P, Nef T, Schütz N, Saner H, Gatica D, et al. De nouvelles technologies au service du maintien à domicile de la personne âgée. Rev Med Suisse. (2019) 1:1407–11. [PubMed] [Google Scholar]
- 23.Schütz N, Saner H, Rudin B, Botros A, Pais B, Santschi V, et al. Validity of pervasive computing based continuous physical activity assessment in community-dwelling old and oldest-old. Sci Rep. (2019) 9:9662. 10.1038/s41598-019-45733-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peetoom KK, Lexis MA, Joore M, Dirksen CD, De Witte LP. Literature review on monitoring technologies and their outcomes in independently living elderly people. Disabil Rehabil Assist Technol. (2014) 10:271–94. 10.3109/17483107.2014.961179 [DOI] [PubMed] [Google Scholar]
- 25.Pais B, Buluschek P, Nef T, Schütz N, Saner H, Gatica D, et al. In-home monitoring evaluation by home-dwelling older adults, caregivers and healthcare providers. 12th European Public Health Conference 2019. Nov 20-23, Marseille, France. Eur J of Public Health. (2019) 29:ckz185301. 10.1093/eurpub/ckz185.301 [DOI] [Google Scholar]
- 26.DomoSafety SA. Available online at: http://www.domo-safety.com/ (accessed November 15, 2019).
- 27.Demers L, Weiss-Lambrou R, Ska B. Development of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST). Assist Technol. (1996) 8:3–13. 10.1080/10400435.1996.10132268 [DOI] [PubMed] [Google Scholar]
- 28.Thomas P, Hazif-Thomas C, Delagnes V, Bonduelle P, Clément JP. La vulnérabilité de l'aidant principal des malades déments à domicile. l'étude pixel. Geriatr Psychol NeuroPsychiatr Vieil. (2005) 3:207–20. [PubMed] [Google Scholar]
- 29.Steele R, Lo A, Secombe C, Wong YK. Elderly persons' perception and acceptance of using wireless sensor networks to assist healthcare. Int J Med Inform. (2009) 78:788–801. 10.1016/j.ijmedinf.2009.08.001 [DOI] [PubMed] [Google Scholar]
- 30.Siegel C, Hochgatterer A, Dorner TE. Contributions of ambient assisted living for health and quality of life in the elderly and care services–a qualitative analysis from the experts' perspective of care service professionals. BMC Geriatr. (2014) 14:112. 10.1186/1471-2318-14-112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lind L, Carlgren G, Karlsson D. Old-and with severe heart failure: telemonitoring by using digital pen technology in specialized homecare: system description, implementation, and early results. Comput Inform Nurs. (2016) 34:360–8. 10.1097/CIN.0000000000000252 [DOI] [PubMed] [Google Scholar]
- 32.Peek ST, Luijkx KG, Rijnaard MD, Nieboer ME, van der Voort CS, Aarts S, et al. Older adults' reasons for using technology while aging in place. Gerontology. (2016) 39:272–93. 10.1159/000430949 [DOI] [PubMed] [Google Scholar]
- 33.Aamodt IT, Lycholip E, Celutkiene J, Strömberg A, Atar D, Sørum Falk R. health care professionals' perceptions of home telemonitoring in heart failure care: cross-sectional survey. J Med Internet Res. (2019) 21:e10362. 10.2196/10362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walker RC, Tong A, Howard K, Palmer SC. Patient expectations and experiences of remote monitoring for chronic diseases: systematic review and thematic synthesis of qualitative studies. Int J Med Inform. (2019) 124:78–85. 10.1016/j.ijmedinf.2019.01.013 [DOI] [PubMed] [Google Scholar]
- 35.Pol M, van Nes F, van Hartingsveldt M, Buurman B, de Rooij S, Kröse B. Older people's perspectives regarding the use of sensor monitoring in their home. Gerontologist. (2014) 56:485–93. 10.1093/geront/gnu104 [DOI] [PubMed] [Google Scholar]
- 36.Mortenson WB, Sixsmith A, Beringer R. No place like home? Surveillance and what home means in old age. Can J Aging. (2016) 35:103–14. 10.1017/S0714980815000549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meiland F, Innes A, Mountain G, Robinson L, van der Roest H, García-Casal JA, et al. Technologies to support community-dwelling persons with dementia: a position paper on issues regarding development, usability, effectiveness and cost-effectiveness, deployment, and ethics. JMIR Rehabil Assist Technol. (2017) 4:e1. 10.2196/rehab.6376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Greenhalgh T. How to improve success of technology projects in health and social care. Public Health Res Pract. (2018) 28:e2831815. 10.17061/phrp2831815 [DOI] [PubMed] [Google Scholar]
- 39.Quaosar GAA, Hoque MR, Bao Y. investigating factors affecting elderly's intention to use m-health services: an empirical study. Telemed e-Health. (2018) 24:309–14. 10.1089/tmj.2017.0111 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.