Abstract
Purpose
Measuring range of motion (ROM) in the wrist joint is an essential part of hand and wrist functional evaluations, especially before and after surgery. However, accurate measurements require experience and time. To reduce patient and surgeon burdens related to ROM measurement, a smartphone-based system, which enables participants to measure the ROM of the wrist joint semiautomatically using self-taken pictures on a smartphone, was developed and evaluated in this study.
Methods
In the developed system, participants were asked to take a picture of their wrist by using the other hand to position the joint first into full flexion and then into full extension. The hand and arm regions were automatically extracted in the program, and the ROM was estimated after the area of the hand and forearm was cropped. To verify the accuracy of ROM measurements in this system, the proposed method was tested on 66 images of hands from 33 participants; measurements were compared with those taken by hand surgeons. A limit of agreement and an intraclass correlation coefficient (ICC) were used for evaluation.
Results
The smallest averages (95% limits of agreement) of flexion and extension were 11.32° (95% confidence interval [CI], 8.88° to 13.76°) and 11.01° (95% CI, 8.64° to 13.39°), respectively. The ICC (1,1) for 3 measurements taken by one assessor was 0.99 (95% CI, 0.986–0.992), and the ICC (2,1) for 2 measurements taken by both assessors was 0.97 (95% CI, 0.947–0.977).
Conclusions
In this study, we developed a system to measure the semiautomatic ROM of the wrist joint using a smartphone image. Its accuracy was within a clinically usable error range that was comparable with that of a hand surgeon.
Clinical relevance
This system can reduce the burden of ROM measurement for both patients and doctors.
Key words: Automatic measurement, Range of motion in wrist joint, Smartphone
Measuring range of motion (ROM) in the wrist joint is an essential method to evaluate hand and wrist functions.1,2 The goniometer is a standard and reliable tool for measuring ROM; however, it is difficult for patients to measure ROM in the wrist joint themselves using a goniometer because some experience is needed for precise evaluation.3,4 Furthermore, few patients have their own goniometers at home. Even for medical experts, measuring ROM precisely during every patient visit takes effort and time. If patients could measure ROM in the wrist joint independently, they would have the ability to assess their status spontaneously. They could then track the progression of rehabilitation or recovery from surgery, and surgeons might access daily data and examine the status remotely. This would help surgeons manage patient visits, even in the current situation of dealing with the spread of the novel coronavirus infection.5
To reduce both patients’ burden of traveling to the hospital and surgeons’ burden of measuring ROM during the recovery period, automated measuring methods that do not require the intervention of surgeons or medical staff have been suggested.6, 7, 8 Owing to advancements in digital devices such as cameras and smartphones, a high-pixel picture of the wrist is easily obtained and sent to doctors; however, the automated measuring method of ROM has not been well-established. Most studies involved in ROM measurements use images traced by hand from a printed photograph or a personal computer monitor, and the accuracy of these methods remains controversial.9 Furthermore, this method does not reduce the burden on medical staff.
In this study, based on advanced data processing techniques, the aim was to develop a smartphone-based system for taking individual photographs of the wrist joint and measuring ROM of the wrist joint in flexion and extension using a semiautomated method. The accuracy of measurements was also examined to ensure this application’s applicability in clinical practice in the near future. In this study, we tested the hypothesis that the newly developed measurement system would be as accurate as the hand surgeon’s measurements.
Materials and Methods
Participant recruitment
This study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the institutional review board of Tokyo Medical and Dental University. Written informed consent was provided by all participants. Healthy volunteers aged greater than 18 years without a history of upper-extremity injury or surgery were recruited as participants. The study included 66 hands of 33 participants (aged 20–50 years).
Outcome measurement
In this study, participants were asked to take a side picture of each wrist in complete flexion and extension (2 images/side; 4 images/participant). Participants were asked to take the pictures by themselves in a seated position and to rest the hand on a table. They were instructed to take a picture of the whole hand and forearm with a smartphone camera (Xperia, Sony, Tokyo, Japan) using the other hand (Fig. 1A). Immediately after participants took the picture, they remained in the same position, and a hand surgeon measured the ROM of the wrist joint using a goniometer. The proximal arm of the goniometer was parallel to the lateral midline of the ulna, and the distal arm was parallel to the dorsal aspect of the third metacarpal on the radial side of the hand and forearm with the forearm in the neutral position, 1 to 2 cm away from the skin of the forearm, as previously described.10 The values were read directly off the goniometer, and ROM was recorded as the true value.
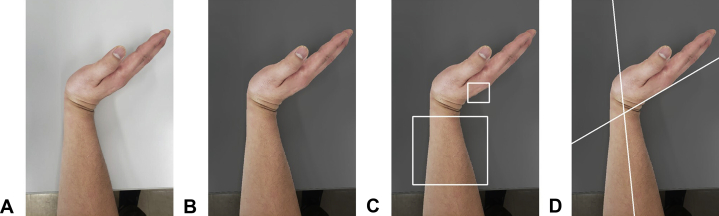
Figure 1.
Proposed measurement flow. A The input image. B Hand and arm extraction. C Manual annotation. D Range of motion estimation.
The method used to estimate ROM from input images taken by the participants is described here. The entire image analysis program was implemented in the OpenCV library with Python. The flow of image analysis adhered to the following process (Fig. 1): First, the hand and arm regions were automatically extracted from the input image (Fig. 1A). After the luminance (brightness) was set to the maximum value (255 in the case of OpenCV) in the YCbCr color space, the image was binarized using Otsu’s11 binarization method. The effect of shadows was reduced by maximizing the luminance. GrabCut12 was then performed to improve the accuracy of hand and arm extraction, and the small hand and arm regions were deleted using connected-component labeling. The result of automatic hand and arm extraction was summarized (Fig. 1B). Pixels determined to be part of the background were darkened.
The angle of flexion and extension in the wrist joint was defined as the angle between the long axis of the radius and the third metacarpal. In this study, the long axis of the radius was approximated by the midline of the arm, and the third metacarpal was approximated by a line along the back of the hand. The assessor was required to annotate 2 bounding boxes on the binarized image to calculate the 2 lines (Fig. 1C). Note that the assessor was not a surgeon, but a computer engineer. No training was necessary before assessment. The midline of the arm was fitted to the averaged pixel positions of the foreground in the arm-bounding box. The pixel positions were averaged in the x axis direction. The line along the back of the hand was fitted to the pixel positions at the boundary between the foreground and the background in the hand-bounding box. We then calculated ROM from the slopes of the 2 lines. After the assessor annotation, the result was displayed (Fig. 1D).
Data analysis
We used a Bland–Altman (BA) plot13 to evaluate the accuracy of the estimation by comparing the true ROMs (measured by a hand surgeon who was board certified for hand surgery) with ROMs estimated by the proposed method. Bland-Altman analysis involves methods that examine whether systematic errors have occurred. Two assessors measured the ROM of 132 images (33 participants; 4 images/person) in a blinded manner using computer software.14
To test intraobserver reliability, one of the assessors measured the ROM 3 times continuously, and the intraclass correlation coefficient (ICC) (1,1) was calculated for the 3 measurements.15 Moreover, to test for interobserver reliability, was calculated the ICC (2,1) for both assessors’ measurements. Note that the 2 assessors were not surgeons. We used the ICC (1,1) to calculate intraobserver reliability when one assessor evaluated multiple subjects and ICC (2,1) for interobserver reliability when multiple assessors evaluated multiple subjects.16
We performed an analysis to determine the sample size before the experiments. A 5° change in ROM was considered to be clinically meaningful when measuring ROM in the wrist joint.4,7,17 This was calculated with a sample size of 66 participants (33 participants/treatment group), giving the study 80% power to detect a 5° mean change in ROM of the wrist joint, with a type I error of 5%.18,19
Results
Accuracy of ROM estimation
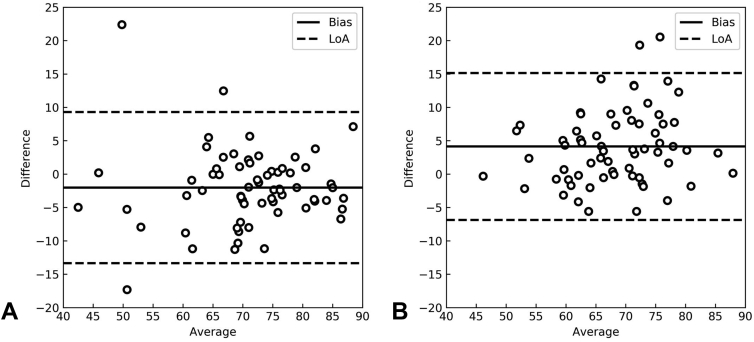
The Bland–Altman plots with the smallest average (95% limit of agreement for wrist flexion and extension) among the 4 measurements taken by the assessors are shown in Figure 2. The limit of agreement for wrist flexion was 11.32° (95% confidence interval [CI], 8.88° to 13.76°) and that of extension was 11.01° (95% CI, 8.64° to 13.39°). The ROM of flexion measured by the assessors tended to be larger than that measured by the hand surgeon, whereas the ROM of extension tended to be smaller.
Figure 2.
Bland–Altman plot with the smallest average of 95% limit of agreement (LoA). Representative measurements were plotted in A flexion and B extension. In these scatterplots, differences between measured values and predicted values were plotted on the y axis and averages of measured values and predicted values were plotted on the x axis. Bias was calculated as the average of the differences.
Intraclass correlation coefficient
The ICC (1,1) for the 3 measurements taken by a single assessor was 0.99 (95% CI, 0.986–0.992) and the ICC (2,1) for the 2 measurements taken by both assessors was 0.97 (95% CI, 0.947–0.977).
Discussion
In this study, we developed a smartphone-based system that enabled participants to measure ROM in the wrist joint independently. The results of this study showed that the accuracy of ROM measurements using this system was tantamount to the accuracy of measurements taken by medical experts. The values of the ICC indicated that both intraobserver and interobserver measurement variabilities were small.
With advancements in technology, trials to measure the ROM of joints remotely are gaining popularity; 3 methods are used widely. The first one uses sensors that are attached to the body.20,21 In this method, detailed and precise joint ranges can be measured; however, devices such as inertial measurement units and stretch sensors are required, which makes this method less accessible to medical practitioners and difficult to apply in daily life. The second method uses a goniometer built into a smartphone.7,22 In this method, equipment such as grips or tape, which hold the smartphone firmly to the body, are required during measurement. Moreover, detailed user instructions require careful explanation. The third method uses a photograph taken using a smartphone camera.9 In this method, instructions are simple regarding how to take the pictures. However, the angles are calculated manually in photo editing software, which requires more time than a practical measurement.
In this study, a system was built that allowed for semiautomatic measurement of angles using a smartphone, and there was no need to print out the photographs. Considering that most patients do not own goniometers, this digital solution may be helpful for patients who need to measure joint ROM at home. In addition to enabling remote consultation, this system is expected to contribute to a reduction in consultation time.23 The system will also allow for the measurement of ROM without direct contact, which is currently important owing to the spread of the novel coronavirus infection.5
Although generally good results were obtained using this method, there were some measurements with relatively large errors. These errors likely resulted from cases in which the hand was thick or the dorsum of the hand was curved. Based on the angle calculation, if the shooting angle of camera, which was same as the elevation angle, was within 32°, the estimated ROM decreased by 5°; however, when the shooting angle was more than 45°, the estimated ROM decreased by 30° (data not shown). To avoid larger errors caused by the increased shooting angle, the implementation of an alert system may be helpful. In addition, collecting cases with large errors for analysis may help us introduce a prediction system using machine learning to improve accuracy. Larger differences were observed in wrist flexion than in extension. This discrepancy could be the result of differences in the shape of the dorsal side of hand during wrist extension and flexion. The dorsal side of the hand tends to curve when it is in flexion, which probably resulted in increased variance of the drawn lines. In contrast, the dorsal side of the hand tends to be flat in extension and might reduce variance.
Several limitations of this study should be considered. First, it is impossible to extract the area of the forearm and hand completely from the image using only automatic methods; a rough area needs to be specified. However, it is relatively easy to designate the area, and even if a layperson designates it, a high ICC can be yielded. For a more complete automation, a system is being built that uses image recognition. Second, it is necessary to explain precautions that should be taken when taking pictures with a smartphone. The main precaution which should be conveyed is to avoid placing the wrist joint in more than 32° radial or ulnar deviation, because this may result in large errors during measurement. Third, in this study, we focused only on active ROM or the extension and flexion angles of the wrist. Moreover, this system could not be applied to one-armed patients. To apply this method to clinical evaluation, other movements in various joints should be measured. This study may serve as the basis for developing methods similarly to obtain measurements of radioulnar deviation and pronosupination in video format for more comprehensive video evaluations. Our dataset was obtained from healthy people. However, because there was no significant difference in absolute error between the larger (≥50°) and smaller (<50°) ROM groups., we assume that ROM can be measured with the same accuracy in patients with smaller arcs of motion.
Acknowledgments
This work was supported by Japan Science and Technology Agency (JST) AIP-PRISM (Center for Advanced Intelligence Project—Public/Private R&D Investment Strategic Expansion PrograM) (Grant No. JPMJCR18Y2). We would like to thank Editage (www.editage.jp) for English language editing.
Footnotes
N.I. and K.F. contributed equally to this article.
Declaration of interests: No benefits in any form have been received or will be received by the authors related directly or indirectly to the subject of this article.
References
- 1.Schuind F.A., Mouraux D., Robert C., et al. Functional and outcome evaluation of the hand and wrist. Hand Clin. 2003;19(3):361–369. doi: 10.1016/s0749-0712(03)00026-x. [DOI] [PubMed] [Google Scholar]
- 2.Slutsky D.J. Outcomes assessment in wrist surgery. J Wrist Surg. 2013;2(1):1–4. doi: 10.1055/s-0033-1333892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horger M.M. The reliability of goniometric measurements of active and passive wrist motions. Am J Occup Ther. 1990;44(4):342–348. doi: 10.5014/ajot.44.4.342. [DOI] [PubMed] [Google Scholar]
- 4.van de Pol R.J., van Trijffel E., Lucas C. Inter-rater reliability for measurement of passive physiological range of motion of upper extremity joints is better if instruments are used: a systematic review. J Physiother. 2010;56(1):7–17. doi: 10.1016/s1836-9553(10)70049-7. [DOI] [PubMed] [Google Scholar]
- 5.Vannabouathong C., Devji T., Ekhtiari S., et al. Novel coronavirus COVID-19: current evidence and evolving strategies. J Bone Joint Surg Am. 2020;102(9):734–744. doi: 10.2106/JBJS.20.00396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cai LS, Ma Y, Xiong S, Zhang YX. Validity and reliability of upper limb functional assessment using the Microsoft Kinect V2 sensor. Appl Bionics Biomech. 201911;2019:7175240. [DOI] [PMC free article] [PubMed]
- 7.Kim T.S., Park D.D.H., Lee Y.B., et al. A Study on the measurement of wrist motion range using the iPhone 4 gyroscope application. Ann Plas Surg. 2014;73(2):215–218. doi: 10.1097/SAP.0b013e31826eabfe. [DOI] [PubMed] [Google Scholar]
- 8.Mejia-Hernandez K., Chang A., Eardley-Harris N., Jaarsma R., Gill T.K., McLean J.M. Smartphone applications for the evaluation of pathologic shoulder range of motion and shoulder scores—a comparative study. JSES Open Access. 2018;2(1):109–114. doi: 10.1016/j.jses.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wagner E.R., Mica M.C., Shin A.Y. Smartphone photography utilized to measure wrist range of motion. J Hand Surg Eur Vol. 2018;43(2):187–192. doi: 10.1177/1753193417729140. [DOI] [PubMed] [Google Scholar]
- 10.Yang Z., Lim P.P.H., Teo S.H., Chen H., Qiu H., Pua Y.H. Association of wrist and forearm range of motion measures with self-reported functional scores amongst patients with distal radius fractures: a longitudinal study. BMC Musculoskelet Disord. 2018;19(1):142. doi: 10.1186/s12891-018-2065-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Otsu N. A threshold selection method from gray-level histograms. IEEE Trans Syst. 1979;9(1):62–66. [Google Scholar]
- 12.Rother C., Kolmogorov V., Blake A. “GrabCut”—Interactive foreground extraction using iterated graph cuts. ACM Trans Graph. 2004;23(3):309–314. [Google Scholar]
- 13.Giavarina D. Understanding Bland Altman analysis. Biochem Med (Zagreb) 2015;25(2):141–151. doi: 10.11613/BM.2015.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saghaei M. An overview of randomization and minimization programs for randomized clinical trials. J Med Signals Sens. 2011;1(1):55–61. [PMC free article] [PubMed] [Google Scholar]
- 15.Koo T.K., Li M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McHugh M.L. Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- 17.Reissner L., Fischer G., List R., Taylor W.R., Giovanoli P., Calcagni M. Minimal detectable difference of the finger and wrist range of motion: comparison of goniometry and 3D motion analysis. J Orthop Surg Res. 2019;14(1):173. doi: 10.1186/s13018-019-1177-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fujita K., Kaburagi H., Nimura A., et al. Lower grip strength and dynamic body balance in women with distal radial fractures. Osteoporos Int. 2019;30(5):949–956. doi: 10.1007/s00198-018-04816-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uttley J. Power analysis, sample size, and assessment of statistical assumptions improving the evidential value of lighting research. Leukos. 2019;15(2-3):143–162. [Google Scholar]
- 20.Kumar Y., Yen S.C., Tay A., et al. Wireless wearable range-of-motion sensor system for upper and lower extremity joints: a validation study. Healthc Technol Lett. 2015;2(1):12–17. doi: 10.1049/htl.2014.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Teufl W., Miezal M., Taetz B., Frohlich M., Bleser G. Validity of inertial sensor based 3D joint kinematics of static and dynamic sport and physiotherapy specific movements. PloS One. 2019;14(2) doi: 10.1371/journal.pone.0213064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keogh J.W.L., Cox A., Anderson S., et al. Reliability and validity of clinically accessible smartphone applications to measure joint range of motion: a systematic review. PloS One. 2019;14(5) doi: 10.1371/journal.pone.0215806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buvik A., Bugge E., Knutsen G., Smabrekke A., Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16(1):483. doi: 10.1186/s12913-016-1717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]