Abstract
Maternal mortality and severe maternal morbidity are urgent issues in the United States. It is important to establish priority areas to address these public health crises. On April 8, 2019, and May 2 to 3, 2019, the Eunice Kennedy Shriver National Institute of Child Health and Human Development organized and invited experts with varied perspectives to 2 meetings, a community engagement forum and a scientific workshop, to discuss underlying themes involved in the rising incidence of maternal mortality in the United States. Experts from diverse disciplines reviewed current data, ongoing activities, and identified research gaps focused on data measurement and reporting, obstetrical and health system factors, social determinants and disparities, and the community perspective and engagement. Key scientific opportunities to reduce maternal mortality and severe maternal morbidity include improved data quality and measurement, understanding the populations affected as well as the numerous etiologies, clinical research to confirm preventive and interventional strategies, and engagement of community participation in research that will lead to the reduction of maternal mortality in the United States. This article provides a summary of the workshop presentations and discussions.
Keywords: alliance for innovation, community engagement, epidemiology, health disparities, levels of maternal care, maternal morbidity, maternal mortality, measurement, perinatal collaborative, postpartum care, pregnancy-related mortality surveillance, race and ethnicity, social determinants of health, surveillance, vital statistics
Remarkable advances in perinatal care over the last 25 years in the United States have led to notable improvements in neonatal morbidity and mortality. In contrast, between 1987 and 2016, pregnancy-related mortality in the United States increased from 7.2 to 16.9 maternal deaths per 100,000 live births.1 Moreover, racial disparities in maternal mortality in the United States are staggering, with a >3-fold higher maternal mortality rate of 41 deaths per 100,000 live births for non-Hispanic black women compared with 13 deaths per 100,000 live births for non-Hispanic white women.2–4 Of the approximately 700 pregnancy-related deaths occurring in the United States yearly, more than half are attributable to preventable causes.5
Research is an essential component of understanding the reasons and finding solutions to the rising maternal mortality rates.6 Research forms the evidence base for future policies and interventions. In 2019, the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) convened 2 workshops that examined the current state of the science, identified research gaps, and focused on the priorities for maternal mortality and morbidity research. The first workshop, Community Engagement Forum on Improving Maternal Health, held on April 8, 2019, brought together members of community-based and healthcare provider groups for panel discussions about maternal morbidity and mortality. The second workshop, Maternal Mortality in the United States: Future Research Directions Workshop, held on May 2 to 3, 2019, convened scientific experts from diverse disciplines to inform a research agenda designed to address the high rate of maternal mortality in the United States. Experts at both workshops reviewed current data, ongoing activities, and discussed research gaps focused on data measurement and reporting, obstetrical and health system factors, social determinants and disparities, and the community perspective and engagement.
Moreover, through these venues, NICHD connected scientific experts, members of healthcare and community organizations, patient advocates, and practitioners. Research needs, gaps, challenges, and opportunities for research to improve maternal health were identified during these 2 workshops.
Maternal Mortality in the United States: Future Research Directions Workshopa
Collaboration among patients, providers, and healthcare systems is crucial to better understand and prevent maternal morbidity and mortality.7–9 Challenges include the complexity of using different measures of maternal mortality, incomplete data, and lack of standardized definitions. Unintended consequences of health policies and medical insurance reimbursements include the closure of maternity units and limited access to critical care resources in both urban neighborhoods and remote geographic areas. Data from 2011 to 2015 indicate that 31% of maternal deaths occur during pregnancy, 36% at or within 1 week after delivery, and 33% from 1 week to 1 year after delivery.10 Of note, most publicly insured women lose their medical insurance 42 days after delivery. Multidimensional factors contribute to disparities in maternal outcomes. The traditional medical model is inadequate.11,12 Future efforts must bring together diverse perspectives and address the social determinants of health, including structural racism, implicit bias, disparities in different geographic and birth settings,13,14 and the need for social support and respectful care.
Data and demographyb
Between 2008–2009 and 2013–2014, maternal mortality in the United States increased for women of all ages. Strikingly, the maternal mortality rate attributable to unspecified causes was 20 times higher inwomen at the age of 40 years and older than it was in younger women (Figure 1).15,16 Even when analyses are limited to women younger than 40 years or with specific causes of death, mortality rates are 3 to 4 times higher in the United States than in manycountries inEurope.17 Despite the inherent risks of childbirth, the disparities in the populations experiencing these maternal deaths and the large percentage of maternal deaths that could be prevented are most concerning. For example, the Texas state maternal mortality review committee (MMRC) found that 70% of maternal deaths occurred in women insured by Medicaid at the time of delivery and that 80% of all maternal deaths were preventable.18
FIGURE 1. Comparison of maternal mortality rates by age for specific and nonspecific causes in 27 states and DC for 2008 and 2009 (green bars) and for 2013 and 2014 (blue bars).
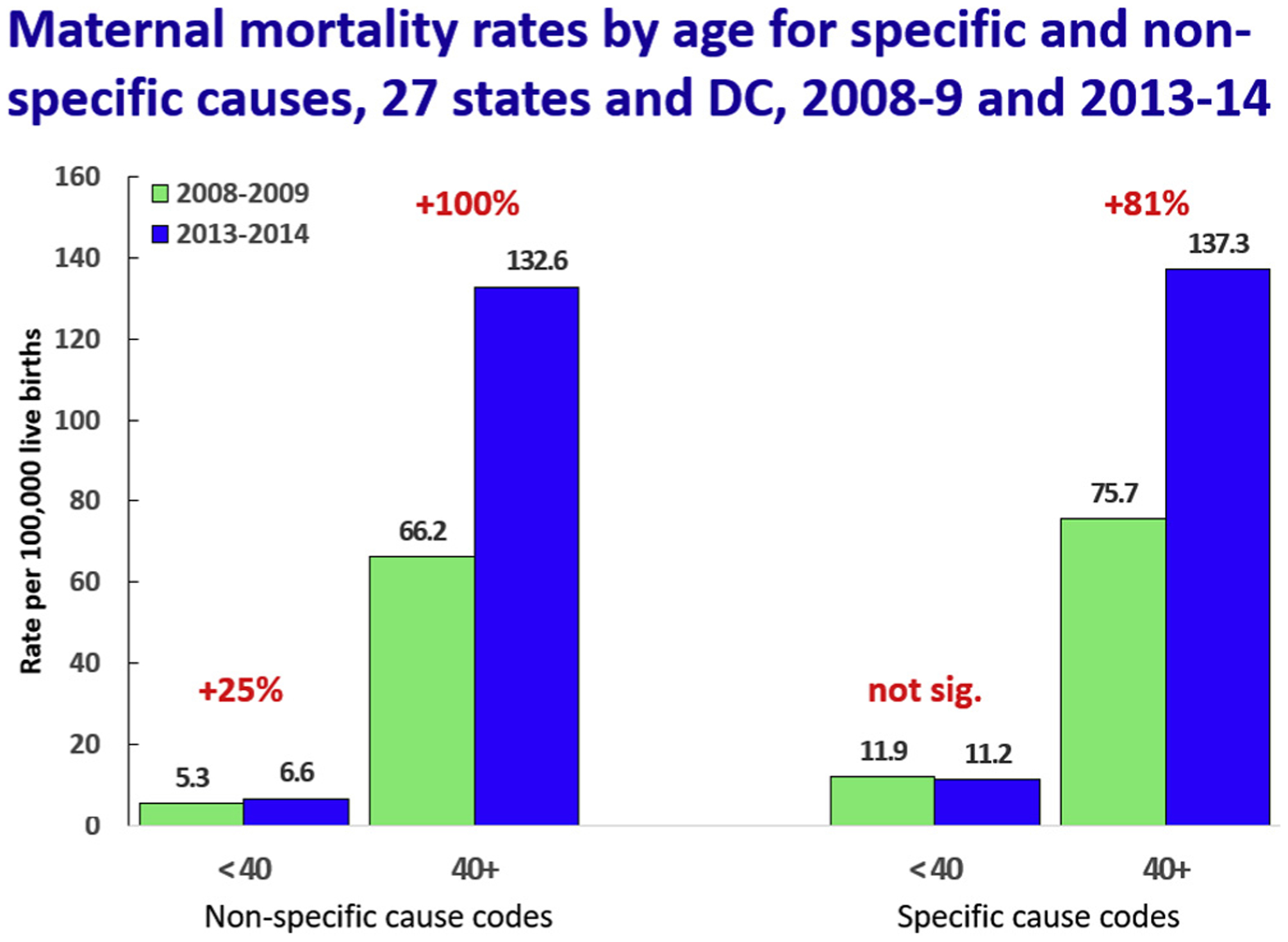
Percentage increase between the 2 time periods is highlighted in red for each age group by specific and nonspecific causes. Nonspecific causes of death include other specified pregnancy-related conditions, unknown cause, and other specified diseases and conditions complicating pregnancy, childbirth, and the puerperium. As presented by MacDorman et al.15,16
Chinn. US maternal mortality: research gaps, opportunities, and priorities. Am J Obstet Gynecol 2020.
The United States relies on the following 3 primary sources for national data on maternal mortality: the National Vital Statistics System, the Pregnancy Mortality Surveillance System (PMSS), and state-based MMRCs. The collection of vital records data occurs at the state level and these data are transmitted to the National Center for Health Statistics of the Centers for Disease Control and Prevention. A federal-state contract provides for federal funding, standards, and coordination of these data. Until January 2020, the United States had not reported an official maternal mortality statistic since 2007 because of the phased process for adding a pregnancy checkbox to the death certificate that was implemented over a decade. After its implementation, the accuracy of measurement of maternal mortality has been negatively impacted by both over- and undercounting of maternal deaths and miscoding of the International Cause of Death chapter 15 (O) codes. Most errors in the reporting of maternal death information occur in the data for women older than 40 years; the reason is currently unknown. Since the workshop was conducted, the National Center for Health Statistics has implemented several measures to improve the accuracy of maternal mortality estimates,19 including new coding procedures.20
In addition, the United States has relied on the World Health Organization’s definition of maternal mortality, which excludes “incidental” deaths without defining “incidental.” By not defining incidental, the current definition may be incomplete and insufficient. Considerable variability occurs among hospitals and geographic areas regarding who is assigned to record death data. Inconsistencies are also present in how maternal deaths are coded. This lack of standardization poses a challenge for MMRCs and researchers alike.
The PMSS is a national surveillance of pregnancy-related deaths. It was started in 1986 to collect the clinical information needed to fill data gaps about causes of maternal death.c
The in-depth examination of individual maternal mortality cases is conducted by state-based MMRCs. These reviews reveal the complex story of each decedent. Challenges for the MMRC process include lack of training of MMRC members, limited diversity in the MMRC composition, time and cost to process the records, lack of information on key drivers of inequitable outcomes, missing information, correct identification of maternal deaths in medical records, and the adjudication of cause of death.21,22 Even with this detailed information on cause of death, some answers to the question “If she had not been pregnant, would she have died?” are clear for pregnancy-specific conditions such as preeclampsia; however, some are not so clear in cases, such as with suicide or fatal injury that occurs during a custody-related altercation while pregnant or within a year after delivery.
Maternal mortality, obstetrical, and health system factorsd
Approximately 3 of 5 pregnancy-related deaths are preventable; this does not differ substantially when analyzed by race or ethnicity or timing of death.23 Severe maternal morbidity (SMM), the life-threatening complications of labor and delivery, may serve as a window into maternal mortality.24 The reduction of maternal deaths requires the elimination of preventable SMM. Rates of SMM more than doubled from 1998 to 2011, increasing from 60 to 160 per 10,000 delivery hospitalizations.25 Increases in twin births,26 rising rates of cesarean delivery,27 elective cesarean delivery for first delivery, delivery at a gestational age of <34 weeks, and increasing obesity may each contribute to the rising rates of SMM. The continuum of obstetrical risk factors is compounded by health system factors including lack of access to adequate health insurance coverage, hospitals with low resources or low delivery volume, and closures of obstetrical units in rural areas. All these factors converge to create the conditions that lead to a high risk of SMM and mortality.
The risk of maternal mortality is associated with maternal health and comorbidities (cardiovascular disease, sepsis, obstetrical hemorrhage,28 preeclampsia/eclampsia/hypertensive disorders,29 venous thromboembolism, amniotic fluid embolism).30 The topic of clinical obstetrical and comorbid conditions was outside the scope of these workshops and was closely examined at a subsequent workshop in May 2020, that is, the Pregnancy and Maternal Conditions that Increase Risk of Morbidity and Mortality workshop. Furthermore, SMM and maternal mortality are increased by the intersection of pregnancy-related contributors and health systems factors such as inadequate knowledge, services, equipment, facilities, and lack of coordinated care. Preexisting chronic conditions disproportionately burden non-Hispanic black women, women living in rural and low-income communities,31 and women who have Medicaid insurance coverage for childbirth. In addition, high rates of insurance coverage at the time of delivery mask the considerable proportion of women who experience gaps and transitions in health insurance in the prenatal and postpartum periods.32
Approaches occurring at the population level include collaborations among governmental, professional, and clinical organizations, such as the Alliance for Innovation on Maternal Health, MMRC, and Perinatal Quality Collaboratives. These collaborations identify critical issues, create action steps, disseminate knowledge, and implement changes with the hope of improving maternal health outcomes and reducing maternal mortality.33,34 Maternal safety bundles are resources for hospitals and practitioners to improve safety for all women during childbirth.35 For example, California used a multipronged approach, including safety bundles, to substantially reduce its maternal mortality rate from a high rate of 16.9 in 2007 to 7.3 in 2014.36
Maternal mortality is inversely proportional to the delivery volume of the hospital and population density of maternal-fetal medicine specialists available. Pregnant women with high comorbidity risk profiles fare worse at low-resource hospitals than at high-resource hospitals.37 The categorization of hospitals by levels of maternal care, to mirror the categorization of neonatal units in hospitals, may facilitate addressing the complexities of current obstetrical practice. Furthermore, matching the acuity of the patient with the acuity of the hospital has the potential to reduce SMM and mortality. Additional opportunities for improvement include simple measures that are amassed into action bundles, education on the classical obstetrical causes of maternal mortality, standardized algorithms and protocols, and training of caregivers and research to develop an evidence base for management of pregnancy-related and obstetrical complications. Well-conducted epidemiologic studies and large-scale randomized clinical trials addressing obstetrical and health system issues are critical to obtain the answers to important clinical questions directed at improving obstetrical practice and reducing SMM and mortality.
Disparities and social determinants of maternal mortalitye
The social determinants of health are “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”38 Disparities in maternal mortality are particular types of maternal mortality differences that are “closely linked with social, economic, and/or environmental disadvantage.”39 Maternal deaths are inseparable from the context in which they occur. In the United States, black women at all levels of income and education are more likely to experience a maternal death than white women. Clinical complications do not fully account for the disparity in maternal mortality rates.40
The foundation of institutional policies and practices that create and reinforce inequalities began in the 1800s during the development of gynecology as a medical specialty. The lack of regulations for the protection of human subjects in research allowed for the acceptability of unethical experimentation on black women. These women received discriminatory treatment and unequal access to care.
Structural racism is a fundamental cause of maternal health inequities. Through its influence on factors such as the quality of the built environment and the infliction of chronic stress, structural racism results in black and American Indian or Alaskan Native women entering pregnancy with less than optimal health. This disadvantage is compounded by poor treatment and negative experiences within the healthcare system.41 Women from racial and ethnic minority groups give birth in lower-quality hospitals and hospitals with higher rates of SMM.42,43 Qualitative research reveals that many black and Latina women giving birth in low-performing hospitals experience poor patient-provider communication, trauma, and difficulties in obtaining appropriate prenatal and postpartum care.44
States have become the battleground for an array of public policies shaping access to healthcare and social services that affect women’s health and maternal mortality. Some states have maternal mortality rates (Figure 2) that are comparable with developing nations, whereas other states resemble more developed European countries. Changes in federal and state policies as well as decreased state investments in their populations come at the detriment of women, the less educated, and minority populations. Disparities in maternal morbidity and mortality need to be addressed at the state and local levels.
FIGURE 2. Maternal mortality rates (MMR) in the United States compared with MMR in other countries.

Graphic depicting maternal mortality rate (number of deaths per 100,000 live births), as calculated by America’s Health Rankings, on the basis of the CDC WONDER data, a 5-year estimate from 2013 to 2017. To demonstrate the variability among states, numbers are depicted as approximate mortality rates in different countries around the world, as presented by the CIA World Factbook. Maternal mortality rate by state: https://www.americashealthrankings.org/explore/health-of-women-and-children/measure/maternal_mortality_a/state/ALL. Maternal mortality rate by country: https://www.cia.gov/library/publications/the-world-factbook/fields/353rank.html.
Note: America’s Health Rankings defines number of deaths as the number of deaths from any cause related to or aggravated by pregnancy or its management (excluding accidental or incidental causes) during pregnancy and childbirth or within 1 year of termination of pregnancy, irrespective of the duration and site of the pregnancy, per 100,000 live births (5-year estimate). CIA World Factbook defines number of deaths as follows: the maternal mortality rate (MMR) is the annual number of female deaths per 100,000 live births from any cause related to or aggravated by pregnancy or its management (excluding accidental or incidental causes).
CDC, Centers for Disease Control and Prevention; CIA, Central Intelligence Agency.
Chinn. US maternal mortality: research gaps, opportunities, and priorities. Am J Obstet Gynecol 2020.
Community Engagement Forum on Improving Maternal Healthf,g
Community engagement is a valuable tool to inform research discussions.45 In Washington, DC, maternal mortality research has been enriched by holding community-level focus groups, involving community representatives on maternal-child health committees and coalitions, and the District of Columbia Department of Health’s efforts to improve maternal outcomes.
Intersecting roles of patient advocates and healthcare providersh
Notably, 3 overarching themes emerged as opportunities to improve maternal outcomes: provider and patient education, healthcare infrastructure, and research. Education aimed at providers and other healthcare workers that addresses respectful care, especially for minority women and those with disabilities, is needed. Patient educational materials that describe the range of “normal” pregnancy experiences and efforts to increase awareness of existing resources are also needed. Evidence acquired from collecting qualitative data on women’s experiences and developing measures of respectful maternity care could inform the development of healthcare provider training and education modules. It is important to build and sustain healthcare infrastructure in local communities that improves healthcare quality and coordination among providers. In particular, providers may collaborate with community advocates and healthcare navigators who are aware of individual patient and community needs, partner with doulas and other birth paraprofessionals, and use telemedicine to enhance partnership with the community. Supporting research led by community-based organizations, as well as black and Native Americanwomen and women with disabilities, is a way in which academic and clinical researchers can partner with the community. The community expressed the desire for researchers to actively recognize and partner with the populations most adversely affected by SMM and mortality.
Local and state initiativesi
Initiatives to mitigate maternal morbidity and mortality require participation at the local and state levels. These include creating culturally acceptable approaches and support systems for women, and holistically addressing their physical and mental health needs. Examples of strategies designed to improve maternal outcomes include community and academic partnerships that address transportation, housing, and food challenges and working with community partners and neighborhood groups to identify health education topics of interest and institutional barriers faced by community members. Another approach to increase the involvement of minority women in research is to enlist church members to serve as ambassadors and to train ministers to explain the value of research to their community. Holding activities within community settings, such as churches and community centers, may increase awareness and comfort and strengthen relationships within minority communities. Collaborations among state perinatal collaboratives, hospitals, and providers are important for the implementation of obstetrical bundles. Furthermore, engagement of MMRCs with these groups contributes a better understanding of the leading causes of maternal death at the community level. Development of infrastructure to engage patients and nonclinicians in rural settings is also imperative to improving maternal health outcomes. There are opportunities for academic researchers to partner with the community to conduct qualitative research to hear the voices of women and understand their needs. Community partnership is a resource in the research enterprise. Community-based and national organizations serve a pivotal role in the pursuit to reduce SMM and mortality in the United States.
Research gaps, challenges, and opportunities
Focused discussions to highlight research gaps, challenges, and opportunities occurred during each workshop as well as in structured breakout sessions. Specific topics included the intersections of data, health systems, and racial disparities; capturing obstetrical events in large-scale data systems; geographic and health systems data collections; and measurement of maternal mortality and maternal adverse events at the population, community, and individual levels. The inclusion of groups underrepresented in biomedical research (racial and ethnic minorities, low socioeconomic status and rural populations, and women at higher risk of maternal mortality and other adverse maternal events) in MMRCs and in research was stressed as a research need and challenge. Other needs included ways to measure healthcare provider access and availability, healthcare provider knowledge and ability to handle acute events, and healthcare delivery factors, as well as approaches to address culture mistrust and implicit bias. The inability to link maternal and infant health records was cited as a challenge to fully understand the risks associated with SMM and maternal mortality. Participants identified technology, such as telehealth and the use of wearable devices, as research opportunities. A more complete list of research gaps, challenges, and opportunities is presented in the Supplementary Tables in Appendix 1.
Conclusion
Maternal mortality is a serious outcome of pregnancy and childbirth. Despite a global decline, maternal mortality has been on the rise in the United States. The causes of maternal mortality are complex and multidimensional, including data measurement and quality issues, obstetrical and health system factors, structural racism, and health disparities, among others. Importantly, a variety of solutions are needed on various levels to address the underlying issues in different communities. Some inroads have been made through collaborations and partnerships, and more are needed. These 2 workshops highlighted the complexity of the problem of maternal mortality; identified scientific gaps, needs, and opportunities; and pointed out that research is an important component of a multipronged approach to reduce SMM and maternal mortality. A summary of the highest priorities for future research to reduce SMM and maternal mortality is given here. Of note, after these workshops in November 2019, a trans-NIH Task Force was formed to address implementation of a research agenda. The resulting initiative will be known as IMPROVE (Implementing a Maternal health and Pregnancy Outcomes Vision for Everyone).
ACKNOWLEDGMENTS
The Maternal Mortality in the United States: Future Research Directions workshop was sponsored by the Eunice Kennedy Shriver NICHD, with generous cofunding provided by the National Institutes of Health, Office of Disease Prevention and the National Institutes of Health, Office of Behavioral and Social Science Research. The authors thank the workshops’ speakers (Appendix 2, Appendix 3) and participants, both online and in person. Their scientific contributions were a vital part of the workshops’ success.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institutes of Health.
All authors are United States federal government staff of National Institute of Child Health and Human Development of the National Institutes of Health and report no conflict of interest.
K.L.G. was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (HD008794-13).
Appendix 1
SUPPLEMENTAL TABLE 1.
Research gaps, challenges, and opportunities highlighted by the research and community engagement meetings
| Topic | Considerations |
|---|---|
| Data quality | Standardize the definition of SMM. |
| Add additional data quality checks within the vital statistics data system to validate maternal deaths. | |
| Improve the assessment of “incidental causes” of maternal deaths. | |
| Create quality assurance procedures with an emphasis on maternal deaths in persons at the age of >40 years or who died of nonspecific causes. | |
| Health services | Understand the risks and benefits of different birth settings. |
| Study the use of social media or apps in maternal care. | |
| Study the feasibility and efficacy of telehealth as applied to pregnancy care. | |
| Institutional policies and structural barriers | Explore current payment systems to determine effective use of resources to improve pregnancy planning, women’s health during pregnancy, and management of care for pregnant women with chronic conditions. |
| Conduct research to understand persistent disparities in maternal mortality. | |
| Review federal- and state-level policies regarding equitable access to care for all women that are rooted in evidence-based epidemiologic and accurate demographic data. | |
| Conduct research that is inclusive of quantitative, qualitative, and mixed-methods research approaches and data to capture the voice of women at risk of adverse maternal health outcomes. | |
| Study the hospital factors and clinical practices associated with lower rates of maternal morbidity and mortality. | |
| Methodology | Fund research that includes community partnerships. |
| Train researchers on the appropriate use of data. | |
| Increase the use of mixed-methods research to identify effective interventions including those that reduce disparities. | |
| Research the role of social support and pregnancy outcomes. | |
| Add pregnancy questions to existing large-scale data collections. | |
| Link mother and infant electronic health records to provide for timely prospective analyses of SMM and mortality. | |
| Racism | Support and cite black and American Indian or Alaskan Native scholarship related to maternal morbidity and mortality. |
| Create an evidence base on the impact of culturally centered and equitable models of maternity care. | |
| Conduct research to determine effectiveness of implicit bias training. | |
| Technology | Use of wearable devices and biomarkers in maternal mortality research. |
| Use artificial intelligence to identify potential morbidities. | |
| Underlying biologic mechanisms of disease | Understand the basic biology and pathophysiology of SMM and maternal mortality. |
| Use translational approaches to study new interventions. |
Some considerations are a combination of research, clinical, and policy gaps, challenges, and opportunities highlighted at the research and community engagement meetings. These lists of considerations are not exhaustive and do not imply the consideration is within the purview of NICHD.
NICHD, National Institute of Child Health and Human Development; SMM, severe maternal morbidity.
Chinn. US maternal mortality: research gaps, opportunities, and priorities. Am J Obstet Gynecol 2020.
SUPPLEMENTAL TABLE 2.
Clinical gaps, challenges, and opportunities highlighted by the research and community engagement meetings
| Topic | Considerations |
|---|---|
| Education | Diversify the medical workforce. |
| Educate patients regarding ante-, intra-, and postpartum expectations. | |
| Understand that health inequalities in women’s health do not begin at pregnancy. | |
| Health services | Explore the impact of earlier postpartum office visits on maternal outcomes. |
| Explore the impact of postnatal and infant care in same office visit on maternal outcomes. | |
| Support interdisciplinary health teams (gynecologist, obstetrician, pediatrician, primary care physician) to support maternal health at any engagement with healthcare system. | |
| MMRC composition | Expand the MMRC review process to include information related to chain of events before mortality, family, and social, demographic, and environmental data. |
| Racism | Improve customer service provided to marginalized populations in a healthcare setting. |
| Technology | Telemedicine in rural and areas with low access to quality care. |
| Use drones to assist with maternal care as needed. | |
| Create simulation videos for provider training. |
Some considerations are a combination of research, clinical, and policy gaps, challenges, and opportunities highlighted at the research and community engagement meetings. These lists of considerations are not exhaustive and do not imply the consideration is within the purview of NICHD.
MMRC, Maternal Mortality Review Committee; NICHD, National Institute of Child Health and Human Development.
Chinn. US maternal mortality: research gaps, opportunities, and priorities. Am J Obstet Gynecol 2020.
SUPPLEMENTAL TABLE 3.
Policy gaps, challenges, and opportunities highlighted by the research and community engagement meetings
| Topic | Considerations |
|---|---|
| Health services | Consider the impact of payment models on maternal outcomes. |
| Institutional policies and structural barriers | Support reasonable accommodations for pregnant women and policies that encourage paid family leave. |
| Expand Medicaid to include the fourth trimester. | |
| MMRC composition | Include women from demographic groups disproportionately affected by maternal mortality on MMRCs to help mitigate bias in the review process. |
Some considerations are a combination of research, clinical, and policy gaps, challenges, and opportunities highlighted at the research and community engagement meetings. These lists of considerations are not exhaustive and do not imply the consideration is within the purview of NICHD.
MMRC, Maternal Mortality Review Committee; NICHD, National Institute of Child Health and Human Development.
Chinn. US maternal mortality: research gaps, opportunities, and priorities. Am J Obstet Gynecol 2020.
Appendix 2
Speaker list and affiliations (at time of the workshop)
Keynote speakers
Elizabeth Howell, MD, MPP
Vice Chair for Research
Department of Obstetrics, Gynecology, and Reproductive Science
Icahn School of Medicine at Mount Sinai, New York, NY
M. Kathryn Menard, MD, MPH
Director, Division of Maternal-Fetal Medicine
University of North Carolina at Chapel Hill, Chapel Hill, NC
Opening address
Diana Bianchi, MD
Director
National Institute of Child Health and Human Development
Panelists
Lindsay Admon, MD, MSc
Institute for Healthcare Policy and Innovation
University of Michigan, Ann Arbor, MI
Robert N. Anderson, PhD
Chief, Mortality Statistics Branch
National Center for Health Statistics
Rachel Hardeman, PhD, MPH
Assistant Professor, Division of Health Policy and Management, School of Public Health
University of Minnesota, Minneapolis, MN
Mark D. Hayward, PhD
Professor of Sociology
Population Research Center, The University of Texas at Austin, Austin, TX
Sarah Kilpatrick, MD, PhD
Department of Obstetrics and Gynecology
Cedar Sinai Medical Center, Los Angeles, CA
Marian MacDorman, PhD
Research Professor, Maryland Population Research Center
University of Maryland, College Park, MD
Luis D. Pacheco, MD
Department of Obstetrics and Gynecology and Anesthesiology
University of Texas Medical Branch
Amy Raines-Milenkov, DrPH
Assistant Professor
University of North Texas Health Science Center
Maeve Wallace, PhD
Assistant Professor, School of Public Health and Tropical Medicine
Tulane University, New Orleans, LA
Moderators
Wanda Barfield, MD, MP
Director, Division of Reproductive Health
Centers for Disease Control and Prevention
Stephen Gilman, ScD
Chief, Social and Behavioral Sciences Branch
National Institute of Child Health and Human Development
Elliott Main, MD
Medical Director
California Maternal Quality Care Collaborative, Stanford, CA
Other speaking roles
Nahida Chakhtoura, MD, MsGH
Medical Officer,
Maternal and Pediatric Infectious Disease Branch
National Institute of Child Health and Human Development
Juanita J. Chinn, PhD
Program Director
Population Dynamics Branch
National Institute of Child Health and Human Development
Esther Eisenberg, MD, MPH
Medical Officer
Fertility Infertility Branch
National Institute of Child Health and Human Development
Della Hann, PhD
Director
Division of Extramural Research
National Institute of Child Health and
Human Development
Charisee Lamar, PhD, MPH, RRT
Director
Office of Health Equity National Institute of Child Health and
Human Development
Constantine Stratakis, MD, DSc
Director
Division of Intramural Research
National Institute of Child Health and
Human Development

NICHD leadership, scientists, program officials, presenters, and grantees at the Maternal Mortality in the United States: Future Research Directions Workshop
Appendix 3
Opening remarks
Diana W. Bianchi, MD
Director
National Institute of Child Health and Human Development
Keynote speaker
LaQuandra Nesbitt, MD, MPH
Director
District of Columbia Department of Health
Voice of the participant
Mavis Stephens
Volunteer
Preeclampsia Foundation
Panelists
Haywood Brown, MD
Vice President
Office of Diversity, Inclusion and Equal Opportunity
University of South Florida
Immediate Past President
American College of Obstetricians and Gynecologists
Angela Doyinsola Aina, MPH
Codirector
Black Mamas Matter Alliancez,
Sonia Hassan, MD
Associate Dean, Maternal, Perinatal, and Child Health
Wayne State University School of Medicine
Melissa Kottke, MD, MPH, MBA
Maternal Chair
Georgia Perinatal Quality Collaborative
Jennifer Senda
Advisory Board Member
National Research Center for Parents with Disabilities
Moderators
Shavon Artis Dickerson, DrPH, MPH
Senior Advisor for Health Equity Research and Analysis
Office of Health Equity
National Institute of Child Health and Human Development
Charisee Lamar, PhD, MPH, RRT
Director
Office of Health Equity
National Institute of Child Health and Human Development
Robyn D’Oria, MA, RNC, APN
Executive Director
Central Jersey Family Health Consortium
Representative
Association of Women’s Health, Obstetric and Neonatal Nurses
Peggy Gautreau, RN, CNM
Administrator
Total Family Medical
Representative
National Association of Rural Health Clinics
Tesheia Johnson, MBA, MHS
Deputy Director and Chief Operating Officer
Yale Center for Clinical Investigation
Yale School of Medicine
Kay Matthews, LCSW
Founder, Shades of Blue Project
Executive Council Member
MoMMA’s Voices

NICHD leadership, Office of Health Equity team, and presenters at the Community Engagement Forum on Improving Maternal Health.
Footnotes
An overview of maternal mortality in the United States was presented by Dr Kathryn Menard.
A panel comprised of speakers Drs Robert N. Anderson, Marian MacDorman, and Amy Raines-Milenkov, moderated by Rear Admiral Dr Wanda Barfield, discussed the quality of the data used to measure trends in maternal mortality. The panel also described improvements to the data that are possible or currently underway.
The PMSS was not discussed in depth during the meeting.
The second session, moderated by Dr Elliott Main, included remarks and discussion by panelists Drs Sarah J Kilpatrick, Luis D. Pacheco, and Lindsay Admon.
Dr Elizabeth Howell delivered the keynote address on this topic. A panel that comprised the speakers Drs. Rachel Hardeman, Mark D. Hayward, and Maeve Wallace, and the moderator Stephen Gilman discussed a timeline of institutional policies that create and reinforce inequalities.
The NICHD Office of Health Equity held a Community Engagement Forum on Improving Maternal Health, in which attendees participated in a 3-hour dialogue with NICHD leadership to inform broader future research discussions. The forum opened with a keynote address by Dr LaQuandra Nesbitt.
Ms Mavis Stephens recounted her experience with pregnancy-related preeclampsia complications and subsequent pregnancy loss.
Panelists, Angela Doyinsola Aina,Robyn D’Oria, Peggy Gautreau, Kay Matthews, Jennifer Senda, and Dr Haywood Brown, addressed questions submitted from the audience and via Facebook Live.
Tesheia Johnson and Drs Sonia Hassan and Melissa Kottke discussed local and state initiatives focused on maternal health.
REFERENCES
- 1.Centers for Disease Control and Prevention. Pregnancy mortality surveillance system. 2016. Available at: https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm. Accessed July 1, 2020.
- 2.Creanga AA, Berg CJ, Ko JY, et al. Maternal mortality and morbidity in the United States: where are we now? J Womens Health (Larchmt) 2014;23:3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011–2013. Obstet Gynecol 2017;130:366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen EE, Davis NL, Goodman D, et al. Racial/ethnic disparities in pregnancy-related deaths—United States, 2007–2016. MMWR Morb Mortal Wkly Rep 2019;68:762–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Public Radio. For every woman who dies in childbirth in the U.S., 70 more come close. 2018. Available at: https://www.npr.org/2018/05/10/607782992/for-every-woman-who-dies-in-childbirth-in-the-u-s-70-more-come-close. Accessed July 1, 2020.
- 6.Chakhtoura N, Chinn JJ, Grantz KL, et al. Importance of research in reducing maternal morbidity and mortality rates. Am J Obstet Gynecol 2019;221:179–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Institutes of Health VideoCasting. Maternal mortality in the United States: future research directions (day 1). May 2, 2019. Available at: https://videocast.nih.gov/summary.asp?Live=31709&bhcp=1. Accessed July 1, 2020.
- 8.National Institutes of Health VideoCasting. Maternal mortality in the United States: future research directions (day 2). May 3, 2019. Available at: https://videocast.nih.gov/summary.asp?Live=31715&bhcp=1. Accessed July 1, 2020.
- 9.Council on Patient Safety in Women’s Health Care. Alliance for Innovation on Maternal Health Program. Available at: https://safehealthcareforeverywoman.org/aim-program/. Accessed January 24, 2020.
- 10.Centers for Disease Control and Prevention. Pregnancy-related deaths: saving women’s lives before, during and after delivery. 2019. Available at: https://www.cdc.gov/vitalsigns/maternal-deaths 2019. Accessed July 1, 2020.
- 11.Main EK, Menard MK. Maternal mortality: time for national action. Obstet Gynecol 2013;122:735–6. [DOI] [PubMed] [Google Scholar]
- 12.Mann S, Hollier LM, McKay K, Brown H. What we can do about maternal mortality—and how to do it quickly. N Engl J Med 2018;379: 1689–91. [DOI] [PubMed] [Google Scholar]
- 13.Zahn CM, Remick A, Catalano A, Goodman D, Kilpatrick SJ, Menard MK. Levels of maternal care verification pilot: translating guidance into practice. Obstet Gynecol 2018;132:1401–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burgess A, Clark S, Dongarwar D, Salihu H. 5: Hospital maternal mortality rates are falling, overall maternal mortality still rises: implications for forward movement. Am J Obstet Gynecol 2020;222(Suppl5). [Google Scholar]
- 15.MacDorman MF, Declercq E, Thoma ME. Trends in maternal mortality by sociodemo-graphic characteristics and cause of death in 27 states and the District of Columbia. Obstet Gynecol 2017;129:811–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacDorman MF, Declercq E, Thoma ME. US maternal mortality data—strengths and pitfalls. Lecture presented at: Maternal mortality in the United States: future research directions workshop; May 2, 2019; Rockville, MD. [Google Scholar]
- 17.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384:980–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raines-Milenkov A. The promise and challenges of maternal mortality review committees: reflections on the Texas experience. Lecture presented at: Maternal mortality in the United States: future research directions workshop; May 2, 2019; Rockville, MD. [Google Scholar]
- 19.Centers for Disease Control and Prevention. Maternal mortality. 2019. Available at: https://www.cdc.gov/nchs/maternal-mortality/index.htm 2019. Accessed July 1, 2020.
- 20.Centers for Disease Control and Prevention. Implementation of new coding methods. 2019. Available at: https://www.cdc.gov/nchs/maternal-mortality/implementation.htm 2019. Accessed July 1, 2020.
- 21.Anderson RN. Maternal deaths in the National Vital Statistics System. Lecture presented at: Maternal mortality in the United States: future research directions workshop; May 2, 2019; Rockville, MD. [Google Scholar]
- 22.Baeva S, Saxton DL, Ruggiero K, et al. Identifying maternal deaths in Texas using an enhanced method, 2012. Obstet Gynecol 2018;131:762–9. [DOI] [PubMed] [Google Scholar]
- 23.Petersen EE, Davis NL, Goodman D, et al. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR Morb Mortal Wkly Rep 2019;68:423–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American College of Obstetricians and Gynecologists. Obstetric Care Consensus No. 5. Severe maternal morbidity: screening and review. Obstet Gynecol 2016;128:e54–60. [DOI] [PubMed] [Google Scholar]
- 25.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol 2012;120:1029–36. [DOI] [PubMed] [Google Scholar]
- 26.Madar H, Goffinet F, Seco A, Rozenberg P, Dupont C, Deneux-Tharaux C. Severe acute maternal morbidity in twin compared with singleton pregnancies. Obstet Gynecol 2019;133:1141–50. [DOI] [PubMed] [Google Scholar]
- 27.Korb D, Goffinet F, Seco A, Chevret S, Deneux-Tharaux C; EPIMOMS Study Group. Risk of severe maternal morbidity associated with cesarean delivery and the role of maternal age: a population-based propensity score analysis. CMAJ 2019;191:E352–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pacheco LD, Saade GR, Hankins GDV. Medical management of postpartum hemorrhage: an update. Semin Perinatol 2019;43: 22–6. [DOI] [PubMed] [Google Scholar]
- 29.Judy AE, McCain CL, Lawton ES, Morton CH, Main EK, Druzin ML. Systolic hypertension, preeclampsia-related mortality, and stroke in California. Obstet Gynecol 2019;133: 1151–9. [DOI] [PubMed] [Google Scholar]
- 30.Pacheco LD, Clark SL, Klassen M, Hankins GDV. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol 2020;222:48–52. [DOI] [PubMed] [Google Scholar]
- 31.Kozhimannil KB, Interrante JD, Tofte AN, Admon LK. Severe maternal morbidity and mortality among indigenous women in the United States. Obstet Gynecol 2020;135: 294–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Taylor YJ, Liu TL, Howell EA. Insurance differences in preventive care use and adverse birth outcomes among pregnant women in a Medicaid nonexpansion state: a retrospective cohort study. J Womens Health (Larchmt) 2020;29:29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Main EK, Cape V, Abreo A, et al. Reduction of severe maternal morbidity from hemorrhage using a state perinatal quality collaborative. Am J Obstet Gynecol 2017;216:298.e1–11. [DOI] [PubMed] [Google Scholar]
- 34.D’Alton ME, Friedman AM, Bernstein PS, et al. Putting the “M” back in maternal-fetal medicine: a 5-year report card on a collaborative effort to address maternal morbidity and mortality in the United States. Am J Obstet Gynecol 2019;221:311–7.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Council on Patient Safety in Women’s Health Care. Safe health care for every woman. 2020. Available at: safehealthcareforevery-woman.org. Accessed July 1, 2020.
- 36.Markow C, Main EK. Creating change at scale: quality improvement strategies used by the California Maternal Quality Care Collaborative. Obstet Gynecol Clin North Am 2019;46: 317–28. [DOI] [PubMed] [Google Scholar]
- 37.Clapp MA, James KE, Kaimal AJ. The effect of hospital acuity on severe maternal morbidity in high-risk patients. Am J Obstet Gynecol 2018;219:111.e1–7. [DOI] [PubMed] [Google Scholar]
- 38.United States Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Social determinants of health. HealthyPeople.gov. 2019. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed September 6, 2019.
- 39.United States Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Disparities. HealthyPeople.gov. 2019. Available at: https://www.healthypeople.gov/2020/about/foundation-health-measures/Disparities#6. Accessed September 6, 2019.
- 40.Leonard SA, Main EK, Carmichael SL. The contribution of maternal characteristics and cesarean delivery to an increasing trend of severe maternal morbidity. BMC Pregnancy Childbirth 2019;19:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hardeman RR. Disparities and social determinants of maternal mortality. Lecture presented at: Maternal mortality in the United States: future research directions workshop; May 3, 2019; Rockville, MD. [Google Scholar]
- 42.Howell EA, Zeitlin J. Improving hospital quality to reduce disparities in severe maternal morbidity and mortality. Semin Perinatol 2017;41:266–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Howell EA, Egorova NN, Janevic T, et al. Race and ethnicity, medical insurance, and within-hospital severe maternal morbidity disparities. Obstet Gynecol 2020;135:285–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Howell EA. Maternal Mortality: disparities and health inequities. Lecture presented at: Maternal mortality in the United States: future research directions workshop; May 3, 2019; Rockville, MD. [Google Scholar]
- 45.National Institutes of Health VideoCasting. Community engagement forum on improving maternal health. April 8, 2019. Available at: https://videocast.nih.gov/summary.asp?live=31665&bhcp=1. Accessed July 1, 2020.


