Abstract
Bone morphogenetic proteins (BMPs) are members of the transforming growth factor-beta (TGFβ) superfamily of cytokines. While some ligand members are potent inducers of angiogenesis, others promote vascular homeostasis. However, the precise understanding of the molecular mechanisms underlying these functions is still a growing research field. In bone, the tissue in which BMPs were first discovered, crosstalk of TGFβ/BMP signaling with mechanobiology is well understood. Likewise, the endothelium represents a tissue that is constantly exposed to multiple mechanical triggers, such as wall shear stress, elicited by blood flow or strain, and tension from the surrounding cells and to the extracellular matrix. To integrate mechanical stimuli, the cytoskeleton plays a pivotal role in the transduction of these forces in endothelial cells. Importantly, mechanical forces integrate on several levels of the TGFβ/BMP pathway, such as receptors and SMADs, but also global cell-architecture and nuclear chromatin re-organization. Here, we summarize the current literature on crosstalk mechanisms between biochemical cues elicited by TGFβ/BMP growth factors and mechanical cues, as shear stress or matrix stiffness that collectively orchestrate endothelial function. We focus on the different subcellular compartments in which the forces are sensed and integrated into the TGFβ/BMP growth factor signaling.
Keywords: BMP, TGFβ, mechanobiology, endothelial-cell, shear stress
1. Introduction
Since their discovery as cytokines extractable from bone matrix, data on pleiotropic activities by bone morphogenetic proteins (BMPs) belonging to the ligand superfamily of transforming growth factors beta (TGFβs) are vastly expanding. There are more than 30 known TGFβ/BMP ligands, which bind to the heteromeric receptor complexes, comprising two type I (R1) and two type II (R2) serine/threonine kinase receptors. Numerous co-receptors fine-tune signaling of these receptors [1,2,3,4]. Activated TGFβ/BMP receptor complexes signal via mothers against decapentaplegic homologs (SMADs) transcription factors or induce a number of non-canonical responses, including activation of mitogen-activated protein kinases (MAPKs), phosphoinositide-3-kinase (PI3K), as well as Rho homologous (Rho) GTPase signaling amongst others [5].
Both TGFβs and BMPs regulate important functions of the vasculature. This is underlined by several vascular phenotypes of the TGFβ/BMP-related knock-outs, which is subject to excellent reviews [6,7,8,9]. The pivotal role of these proteins for endothelial cells (ECs) forming the most inner layer of blood vessels, is further highlighted by a number of human diseases, where perturbed TGFβ/BMP signaling impedes blood vessel formation or maintenance of vascular integrity. Of note here are pulmonary arterial hypertension (PAH), Osler-Weber Rendu syndrome/hereditary hemorrhagic telangiectasia (HHT), and Loeys-Dietz-syndrome (reviewed in [9,10,11,12]).
In addition to biochemical signals, mechanical signals are equally required to orchestrate blood vessel formation, patterning, branching, pruning, and to maintain their integrity. Crosstalk of TGFβ/BMP signaling with cellular mechanobiology is a growing research field and contribution thereof to the above-mentioned vascular pathologies is little understood. In this review, we focus on the current efforts to understand how biochemical TGFβ/BMP signals in conjunction with mechanical signals, are received and integrated by the endothelium. A special focus is given to the different subcellular compartments in which we and others propose crosstalk to occur.
2. Activating Versus Homeostatic TGFβ/BMP Signaling in Endothelial Cells
To put endothelial mechanobiology into context, it helps to briefly introduce the different known actions of TGFβ/BMP signaling in the endothelium. ECs can transit between an activated and homeostasis state, regulated by an intricate balance between the activating and homeostatic TGFβ/BMP ligands, in addition to other potent extracellular factors [13,14,15]; Figure 1a. BMP 2, 6, and 7, all referred to as EC activating BMPs’, induce EC migration and angiogenesis [16,17,18,19,20]; Figure 1a, top. They signal mainly via R1s ALK2, ALK3, and ALK6, in conjunction with either R2s BMPR2 or ACVRIIs (Figure 1b). Sprouting angiogenesis is the formation of new blood vessels out of pre-existing ones [21]. During sprouting angiogenesis, activated tip-cells adopt a fibroblast-like front-to-rear end polarity over the course of migration. The single migratory tip-cell at sprout’s distal end is followed by multiple adjacent stalk-cells that proliferate (Figure 1a, upper) and dynamically compete with the tip-cell for its position [22]. A hallmark of tip-cell phenotype are long actin-driven filopodia at the leading edge. These protrusions are rich in integrins and form focal adhesions (FAs), connecting the extracellular matrix (ECM) with the cellular cytoskeleton, enabling the cell to sense ECM rigidity [23,24] and its nanotopography [25]. Tip-cell filopodia promote sprouting [26,27] by projecting cytokine-gradient sensing receptors to their most distal ends. Several groups have shown in vitro that different ECs, including ECs of arterial and venous origin, as well as microvascular and macrovascular ECs but also EC progenitors, respond to BMP2, 6, and 7 amongst others, by migration, sprouting, or tube-formation [17,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44]. We could recently show that BMP6 promotes the expression of stalk-cell-associated genes, while BMP2 induced delta-like ligand 4 (DLL4) [17], a known tip-cell marker [45]. Application of BMP6 in a gradient-like fashion is sufficient to induce EC filopodia formation, alignment along, and chemotaxis within this gradient [17,30]. Whether EC activating BMP2, 6, 7 gradients exist in-vivo is still debatable. While BMP gradients are well-described in early developmental tissue patterning of invertebrates and vertebrates [46], their existence and contribution for sprouting angiogenesis in vivo is still not clearly shown. Mouse data on BMP-induced tumor vascularization, however suggest, that BMPs induce tumor angiogenesis, similar to vascular endothelial growth factor (VEGF)-like gradients [39,40]. Interestingly, interfering with BMP signaling in zebrafish caudal vein plexus reduces the number of tip-cells and their filopodia, by a process requiring CDC42 Rho GTPase activity [47]. Interfering with endothelial SMAD1/5 signaling in mice results in less functional tip-cells during retinal angiogenesis [48]. Taken together, EC activating BMPs 2, 6, and 7 facilitate in-vitro angiogenic sprouting through regulation of tip- and stalk-cell identities in a gradient-like fashion, and it remains to be proven if this phenomenon also occurs in vivo (Figure 1a).
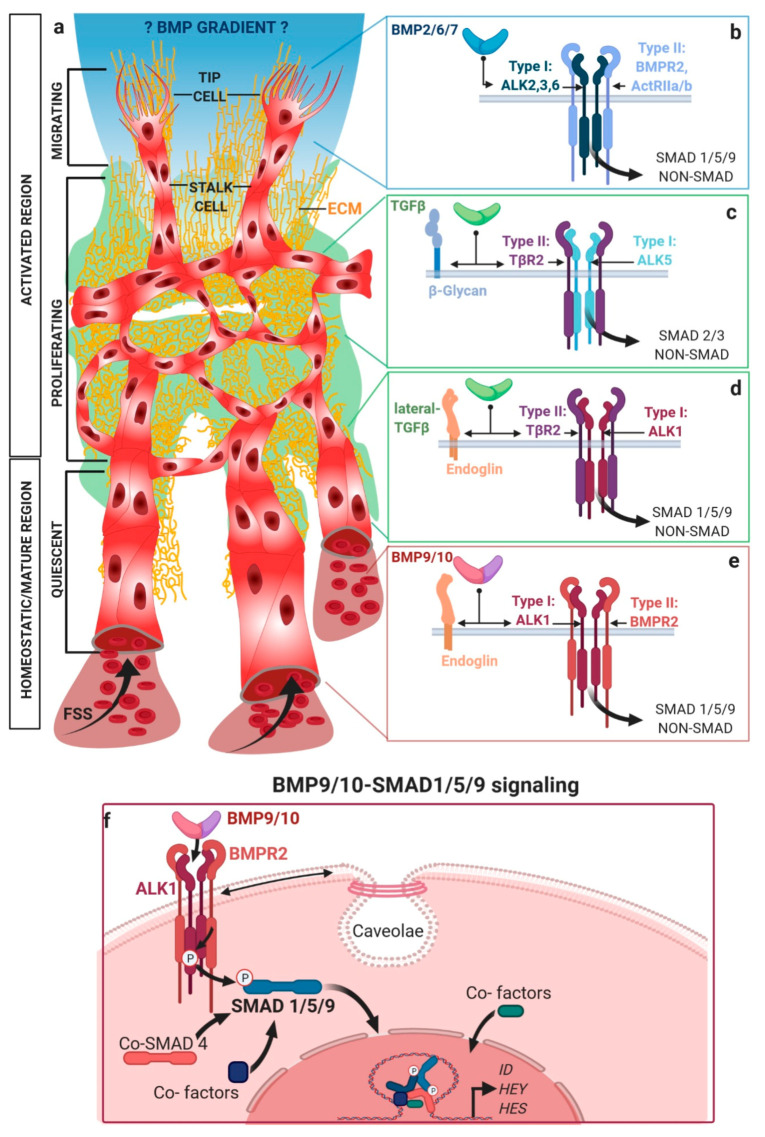
Figure 1.
Different BMPs/TGFβ ligands induce activating or quiescent/homeostatic functions on endothelial cells (ECs). Depicted is the outgrowth (upper), pruning (middle), and maturation (lower) of a developing vascular network, (a) with an activated region (upper/middle) and a more quiescent, homeostatic region (lower). Characteristic at the active angiogenic front (upper) is the induction of sprouting angiogenesis, with distinct tip-cells at the leading front that utilize filopodia to sense- and pull- the extracellular matrix (ECM), followed by the proliferating stalk cells. Angiogenic gradients of activating BMP2, 6, or 7 (blue) are proposed based on in vitro data. TGFβ (green) bio-availability is tightly controlled through the interactions of the latent TGFβ complexes, with the underlying ECM (yellow). Intraluminal blood flow (lower) internally provides systemic BMPs (such as BMP9/10 (purple)) to ECs, inducing their maturation and ultimately maintaining a quiescent endothelial phenotype. Hemodynamics of blood flow exert concomitantly mechanical inputs through generation of fluid shear stress (FSS). The corresponding TGFβ/BMP receptor complexes and signaling branches proposed to be involved in these processes are shown on the right. Activating BMP2, 6, or 7 (blue) signal via R1s ALK 2, 3, and 6, together with R2 BMPR2 or ActRIIa/b to induce SMAD1/5/9 signaling or non-canonical responses (b). TGFβ (green) signals via ALK5 and TβR2 to activate SMAD2/3, (c) while it can also signal via ALK1 and TβR2, to activate SMAD1/5/9 signaling (lateral signaling) (d). Co-receptors like Endoglin and beta-glycan help presenting ligands to the receptors on the surface of ECs. BMP9/10 signaling via ALK1 and BMPR2 provides quiescence signals (e). Nuclear SMAD translocation and co-factor incorporation is shown in (f) at the example of BMP9/10-mediated SMAD1/5/9 signaling, inducing the transcription of EC genes. Among them are the inhibitor-of-differentiation (ID), HES, and HEY genes. ALK1 is located in caveolae, membrane structures that are mechanically regulated by FSS, for example.
TGFβ adopts a bipartite role for EC activation vs. homeostasis, dependent on its concentration and engagement of different receptor complexes. TGFβ signals via R1s ALK4 and ALK5. At early stages in the blood vessel development preceding angiogenesis, TGFβ1 mediates vasculogenesis via ALK5 (Figure 1c). Later, sprouting angiogenesis is inhibited by TGFβ1/3-ALK1/5 signaling [49,50]. Here, TGFβ signals in a so-called ‘lateral’ fashion, to activate SMAD 1/5/9 engaging ALK1 (Figure 1d). While treatment with low levels of TGFβ3 was found to inhibit proliferation and migration in mouse embryonic ECs, the opposite effect was apparent at higher concentrations [51]. This could be explained by a lateral signaling switch (Figure 1c). At higher TGFβ concentrations, ALK1-TGFβR2 complexes are activated, which transduce signals via SMAD 1/5/9, while at low levels of TGFβ, binding to the high affinity receptor complex ALK5-TβR2 is limited, which signals via SMAD 2/3 (Figure 1d). This switch in receptor recognition is reminiscent to the concentration-dependent activities of TGFβ in cancer [52]. Moreover, the EC origin/vascular bed [53] and their maturation state [49] are decisive for differential R1 expression, which might explain the bipartite pro- or anti-angiogenic activities reported for some TGFβ/BMP ligands with receptor promiscuity. Interestingly, TGFβ is stored within the extracellular matrix (ECM) (Figure 1a, middle) in a latent form, requiring integrin-dependent mechanical forces to act on its pro-domain, to be released and to activate signaling (see Section 3.1).
In sharp contrast, BMP9 and BMP10, also synthesized as large pro-domain associated precursors, freely circulate in the blood stream [54,55], while they are still associated with their pro-domains [56]. This association does not influence receptor binding [57,58,59,60]. BMP9/10 signaling provides the endothelium systemically with homeostasis/quiescent signals (reviewed in [9,19]), when angiogenic vessels become transfused with blood, e.g., after successful anastomosis [61,62]. BMP9/10 inhibit sprouting [54], promote maturation, and preserve the quiescence of ECs. In the adult lumen, the average EC divides approximately only twice in a lifetime [63]. BMP9/10 induces signaling via ALK1 (Figure 1e), the most abundant R1 expressed in ECs [59,64]. In zebrafish, it was shown that BMP9/10-Alk1 signaling limits the EC numbers and, thereby, stabilizes the caliber of nascent arteries [65]. Additionally, Alk1 expression depends on fluid shear stress (FSS) exerted by blood flow in the zebrafish [66] and some flow-responsive genes are dysregulated in Alk1 mutant arterial ECs, suggesting Alk1 to be the main BMP type I receptor integrating endothelial FSS into biochemical signaling responses [66]. Furthermore, deletion of ALK1 in mice leads to exuberated sprouting in the mouse retina [16], and addition of BMP9 normalized aberrant tumor vasculature, by decreasing permeability in Lewis lung carcinoma (mice) [67]. Studies using human cells revealed that BMP9 induces expression and secretion of stromal cell-derived factor 1 (SDF1/CXCL12), which promotes vessel maturation by regulating mural cell coverage [68], and counteracts VEGF-induced angiogenesis [59]. However, comparison of different model systems for Bmp10-Alk1 signaling should be done with care, due to the very different nature of vascular beds, flow regimes, and paralog expression [69].
While several studies report on the anti-angiogenic properties of BMP9, recent studies in human-induced pluripotent stem-cell derived ECs suggest that BMP9 also induces sprouting angiogenesis [70], which could recapitulate the above-mentioned bipartite role of TGFβ. Dependent on BMP9 concentration, receptor expression levels and the respective SMAD branches are activated.
Receptor regulated (R) SMADs consist of two domains—the MAD homology (MH) 1 domain at the amino-terminus of SMADs is important for their nuclear import and DNA binding. The C-terminal MH2 domain defines R1 binding, SMAD oligomerization, and interaction with cytosolic adaptors and transcriptional co-factors (Figure 1f, lower; exemplary canonical signaling scheme). Since R-SMADs have a low DNA binding affinity, they require the common mediator SMAD4 (co-SMAD4) and other co-factors. These co-factors integrate into SMAD complexes to regulate shuttling dynamics [71], and to make SMAD complexes competent in DNA binding and specify target gene recognition [72]. Phosphorylation of the SMAD-linker was previously shown to induce a crosstalk with the mechanical co-activator, yes-associated protein 1 (YAP1)/transcriptional co-activator with PDZ-binding motif (TAZ) signaling (see Chapter 6.3), which fine-tunes SMAD stability [73]. Additionally, SMADs compete with inhibitory SMADs (I-SMADs) for receptor and co-SMAD4 binding.
EC BMP9-SMAD 1/5 signaling upregulates about 100 genes and downregulates around 40 genes more than 2-fold [74], collectively giving rise to inhibition of ECs mitogenic response [75], while maintaining the vascular phenotype. This includes JAG1 activation and crosstalk to the NOTCH pathway by regulation of Jagged1, Dll4, Hairy/Enhancer of Split related with the YRPW motif (HEY) and Hairy/Enhancer of Split (HES) genes [76]. Additionally, BMP9 mediates EC quiescence by regulating cell-cycle-related proteins, such as c-myc and p21/waf1, and downregulates the FA complex-related genes, such as beta-actin, paxillin, and zyxin [77], suggesting BMP9 to balance EC–ECM adhesion.
Although the co-receptor Endoglin is not required for BMP9/10 activation of ALK1, it enhances its signaling output [78,79,80,81]. Endoglin binds BMP9 and potentiates BMP9-ALK1 signaling, however, it interferes with TGFβ-ALK5 signaling [82], (Figure 1c–e), thereby pushing the TGFβ/BMP balance towards BMP9 and SMAD1/5. Endoglin binds to TGFβ1,3 but not TGFβ2 [78], as well as the receptor complexes mediating signaling of Activins, BMP2, and BMP7 [79]. It also interacts with VEGF receptor 2 (VEGFR2) [83], zyxin [2], and integrins. Endoglin cooperates with FSS to potentiate BMP-induced Alk1 signaling [84], which is later explained in details. Moreover, Endoglin loss-of-function mutations mediate arterio-venous malformations found in HHT or in lung pulmonary vasculature in PAH [85]. Taken together, TGFβ/BMPs induce different functions in the activated and quiescent endothelium, which sets the base to better understand the crosstalk to mechanical cues that is introduced in the next section.
2.1. Mechanical Regulation of Endocytosis Suggests Modulation of TGFβ/BMP-SMAD Signaling
BMP-SMAD1/5/9 signaling, in particular its turn-over rate, is regulated by endocytosis (Figure 1f), which in turn depends on the physical properties of the plasma membrane [86,87,88]. Two major endocytic routes were described for membrane-bound BMP-receptor complexes (1) clathrin-mediated endocytosis (CME) involving clathrin-coated pits (CCPs), and (2) caveolin-dependent endocytosis [89,90]. CME facilitates SMAD signaling, as the SMAD anchor protein SARA recruits SMADs to the receptors in endosomes derived from CCPs [91,92]. Caveolin-dependent endocytosis originating from lipid rafts is involved in the regulation of non-canonical responses, including activation of MAPK [93]. The caveolae-based internalization pathway contains ubiquitin ligase Smurf2 bound receptors and was proposed to shut down the BMP/TGFβ-SMAD signaling [91], while others showed that BMP-SMAD signaling could be initiated from receptors residing within caveolae [94,95]. Importantly, physical stimuli, such as substrate stiffness sensed by ECs, were sufficient to induce caveolin-dependent endocytosis of membrane receptors [96,97,98]. Mechanistically, ALK1 and BMPR2 localize within caveolae, while Alk1 physically interacts with caveolin-1 (cav-1) through cav-1′s scaffolding domain, suggesting a joint contribution of ALK1, BMPR2, and cav-1, as the key mediators of BMP9/10 signaling [99,100,101] (Figure 1f). This is further highlighted by cav-1 mutations leading to PAH [102], similar to BMPR2 and ALK1 mutations [103]. Caveolae act as membrane reservoirs to compensate for the increased membrane tension induced by flow, emphasizing their role in mechanosensing [104] (reviewed in [105]). Consequently, the caveolae flatten and disassemble [104]. Strikingly, the number of caveolae was reported to increase in response to physiological FSS in ECs [106,107]. This seemingly contradictory finding could provide an explanation to the dual role of caveolae in integrating FSS into the TGFβ/BMP signaling. First, an overall increase in FSS-induced caveolar endocytic turnover-rate might affect the TGFβ/BMP receptor degradation, recycling, or cytosolic retention. Second, flattening and disassembly of caveolae in response to FSS could impact on receptor oligomerization and SMAD activation. The particular shape of caveolae suggests that these structures prevent over-exposure of mechanosensors to shear stress, as already shown for VEGFR2. Since caveolae are found at the apical but moreover at the basal side of ECs, they provide islands for cooperative signaling between BMP receptors and integrins. Interestingly, it was reported that activation of integrin α5 by flow, requires its translocation to membrane lipid rafts [108], and that integrin mechano-transduction promotes cav-1 phosphorylation [109]. Furthermore, integrins seem to cluster in caveolae upon FSS [110], and caveolae-mediated integrin endocytosis regulates ECM remodeling [111]. Since integrin-BMP receptor interaction was suggested to participate in EC FSS sensation [112], caveolae could provide membrane environments for cooperative clustering. Interestingly, whereas cav-1 patches redistribute to the upstream edge facing the direction of flow, there is no change in the distribution of AP-1/2, which is indicative of CME [113]. As micropinocytosis, a process involving heavy cortical actin remodeling mediated by the small GTPase CDC42 [114], was described as the prevalent internalization route for VEGFR2, in the presence of ligand, this route could also be suggested for the TGFβ/BMP receptors in ECs. As with other analogies of TβRs/BMPRs to VEGFRs, one might raise the question whether these receptors are similarly affected by endocytosis. In addition to endocytosis, other cellular mechanisms were described to integrate mechanical forces into the endothelial TGFβ/BMP signaling. These mechanisms were associated with discrete subcellular compartments, which is discussed hereafter.
2.2. TGFβ/BMP-SMAD Signaling Crosstalk to Mechanobiology at Distinct Subcellular Compartments
In the following chapters, we walk through the distinct EC subcellular compartments proposed to incorporate cellular mechanics into the TGFβ/BMP signaling and vice versa (Figure 2). Given is an example of a muscularized artery (Figure 2a), with its different cell and ECM layers forming the vessel wall (Figure 2b). ECs interact with the ECM of the inner elastic membrane (IEM) and adjacent cells through FAs. These adjacent cells are collectively referred to as mural cells (e.g., pericytes and smooth muscle cells (SMCs)). Interaction of ECs to ECM (Figure 2b, I) allows for integrin-mediated ´outside-in´ or ´inside-out signaling´ [115]. Binding of ECM ligands to cell surface integrins stimulates conformational changes that induce intracellular signaling through integrin-associated proteins [116]. ´Inside-out signaling´ strengthens adhesive EC contacts and the appropriate force necessary for integrin-mediated cell migration, invasion, ECM remodeling, and traction force. Inside-out integrin-signaling allows cells to generate traction forces that participate in liberating latent ECM-bound TGFβ, for example. Since TGFβ/BMP signaling regulates the expression of a diverse set of integrins and ECM molecules, it directly modulates the availability of proteins required for such integrin-dependent cellular mechanics in a feed-forward fashion. We give examples of how FAs participate in the liberation of latent TGFβ and the localization of receptors, and how TGFβ/BMP signaling acts upstream of actin, ECM, and integrin regulation.
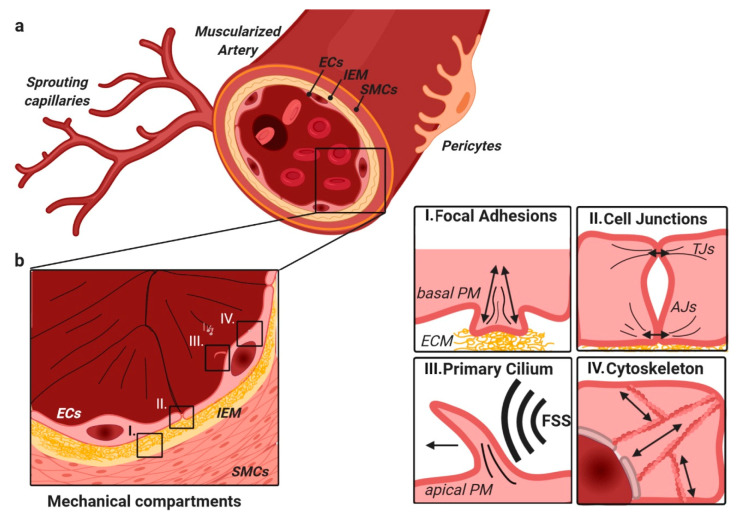
Figure 2.
Muscularized arteries are composed of different layers of cells and interconnective ECM (a); from inside to outside—ECs, the IEM, SMCs, and pericytes (b). In ECs, mechanical signaling is found at four major hubs (enlarged on the right): I. Focal adhesion-ECM contact sites, important in cellular migration, and adhesion. II. Cell–cell junctions that are highly important in the regulation of EC barrier function and cell–cell communication. This includes AJs, TJs, and gap junctions that contribute differently. III. The primary cilium, which is apically located in ECs and initiates signaling upon deflection by FSS, for example. IV. The cytoskeleton that links the plasma membrane with the nucleus, thereby allowing direct force transmission. Abbreviations: ECs—endothelial cells, IEM—inner elastic membrane, SMCs—smooth muscle cells, FSS—fluid shear stress, AJs—adherens junctions, TJs—tight junctions, and PM—plasma membrane.
EC junctions (Figure 2b, II) resemble another subcellular compartment where crosstalk occurs. In a mature/quiescent blood vessel, ECs provide barrier function through tight lateral connectivity and a well-balanced equilibrium between cell-to-cell tension and cell-to-ECM traction. The equilibrium between these basolateral forces is important to maintain the barrier quality. We give examples of how TGFβ/BMP signaling is involved in regulation of this junctional force equilibrium.
One main mechanical force coupling to biochemical signals in ECs is the blood-flow generated FSS, which is sensed by the deflection of the primary cilium, for example (Figure 2b, III). Early reports on FSS-induced BMP-signaling suggest that FSS can activate TGFβ/BMP signaling, i.e., through receptor activation, which included integrin-mediated signaling [117] in the absence of TGFβ/BMP ligands. Such ligand-independent but FSS dependent activation was reported for VEGFR2, for example [118]. Recent work showed a requirement for at least a low concentration of endothelial BMP ligands for the effects of FFS on SMAD signaling, through careful titration and sequestration of BMP ligands from the tissue culture media [84,119]. The mode through which the primary cilium allowed for FSS-dependent TGFβ/BMP-signaling regulation is still not entirely understood. We give examples of FSS and cilia-related TGFβ/BMP research, and emphasize the role of TGFβ/BMP signaling as an upstream regulator of cilium formation.
Finally, we conclude our review by placing the EC nucleus into focus, together with the cell’s cytoskeleton as a mechanosensor (Figure 2b, IV). The nuclear compartment is linked via the cytoskeleton to the above-mentioned mechanisms, directing nuclear import of TGFβ/BMP signaling factors and changes in global chromatin architecture, conferring gene accessibility.
3. TGFβ/BMP Signaling Crosstalk at Focal Adhesions with Extracellular Matrix and Stiffness
There is a wealth of evidence that actin driven filopodia allow chemotactic and mechanical responses in ECs. The latter include durotaxis, the sensing of stiffness gradients at the tip of the cell, as well as tip-cell pulling forces (Figure 3a) that support the outgrowth of a new sprout (Figure 3b) [120,121]. Interestingly, VEGFR2 and its co-receptor neuropilin-1 accumulate at the distal filopodia tips [26,122,123]. Cytoskeletal rearrangements in proximity to BMP receptors are induced via ligand-induced non-SMAD pathways and rely on LIM kinase-cofilin [124], PI3K [125], and Rho GTPases [47] signaling. Additionally, we found that non-SMAD responses such as MAPK-p38-HSP27 signaling can induce EC migration [17] (Figure 3c).
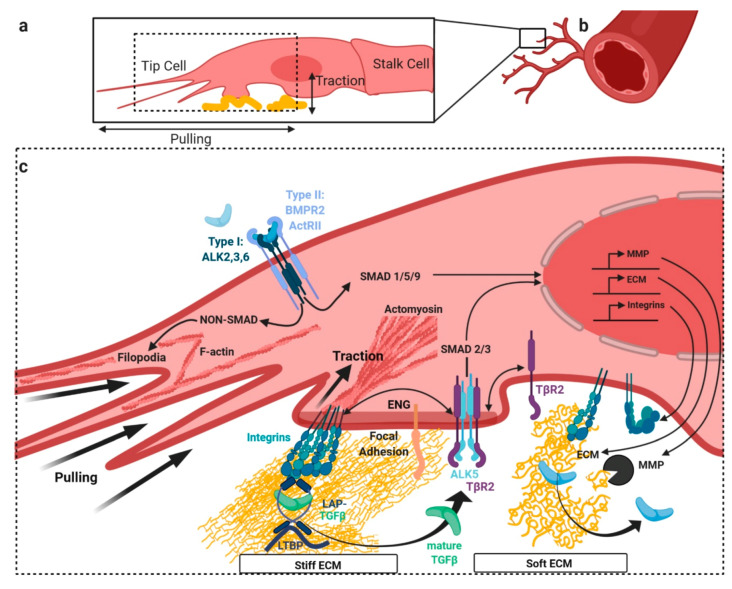
Figure 3.
Crosstalk with the TGFβ/BMP SMAD pathway at focal adhesions (FA). In angiogenesis tip-cells at the sprouting front (a) emerging from pre-existing blood vessels (b) display enhanced FA-ECM contacts and filamentous (F-) actin driven filopodia (c). Exemplified at the sprouting front (lower caption), actin reorganization is in part orchestrated by non-SMAD signaling. FAs influence mechanical properties of the ECM, including stiffness. These contacts are mainly mediated by integrins, providing the cell with inside-out signaling properties. Integrins can directly bind ECM molecules outside the cell and are indirectly bound to the intracellular contractile actomyosin cytoskeleton. Endoglin (ENG) interacts with both, integrins and signaling receptors. TGFβ in its latent form (LAP-TGFβ) is bound to ECM filaments via LTBP. Viscoelastic properties of ECM directly influence integrin-mediated TGFβ retrieval from LAP-TGFβ-LTBP complexes. Integrins release mature TGFβ from the latent complex by exerting pulling forces, through the contraction of the actomyosin cytoskeleton. Stiff ECM allows more efficient release of mature ligand than soft ECM. In a feedback-loop, SMAD signaling in turn regulates the expression of ECM genes, integrins, and MMPs, which support the softening and the release of ligands by degrading the ECM. Abbreviations: ENG—endoglin, LAP—latency associated peptide, ECM—extracellular matrix, LTBP—latent TGFβ- binding protein, and MMPs—matrix metalloproteinases.
ECM stiffness is beneficial for efficient sprouting angiogenesis in development and disease [126,127,128], and incorporates into the fate determination of different vascular beds [129,130]. As such, it was found that ECM stiffness controls lymphatic vessel formation through the regulation of GATA2, and subsequent downregulation of TGFβ2 on soft matrix [131]. Moreover, ECM stiffness is required for capillary maintenance and is related to vascular pathology [132]. Data on blood vessel stiffness largely differ depending on the method used, and can vary by several orders of magnitude [133,134,135], also depending on whether the whole vessel or only the subendothelial layers were analyzed [136,137]. It clearly differs between arterial and venous ECs, between species and between material of different age [138,139]. However, significant stiffness increase is found consistently in diseased endothelium, such as in atherosclerotic ApoE-null mice [140] or the fibrous cap in human carotid atherosclerotic plaques [141] and TGFβ-induced endothelial-to-mesenchymal transition (EndMT) of aortic valves [142], and it also occurs under higher matrix stiffness [143,144]. In arteries, increase in stiffness correlates positively with expression of BMP2 [145], as was reported for TGFβ2 in human umbilical vein ECs (HUVECs) [136].
Mechanical forces involved in sprouting angiogenesis include pulling by the tip-cell and possibly some pushing by the stalk-cells. It was observed through three-dimensional (3D) traction force microscopy that matrix deformations induced by tip-cells were dependent on actin-mediated force generation and correlated with sprout morphological dynamics. Furthermore, sprout tips were found to exert radial pulling forces on the ECM, possibly involving FAs [146]. Interestingly, high ECM stiffness increased the endocytosis rate of VEGFR2 and was involved in VEGFR2 clustering at the plasma membrane [147]. Cells in sparse culture exhibit less cell–cell contractility but the forces concentrate towards their substrate adhesion sites. A similar phenomenon for the TGFβ signaling was observed in fibroblasts. Here, ALK5 clustered to a higher degree with TGFβR2 at FAs, when cellular tension was reduced, which also increased the SMAD2/3 signaling. The same study suggested that FAs provide subcellular signaling hubs, in which the oligomerization and clustering of TGFβ receptors is regulated in a force-dependent manner [148] (Figure 3c).
3.1. Release of Latent TGFβ from Extracellular Depots by Mechanical Forces
Additionally to the regulation of receptor oligomerization, FAs provide a second layer of regulation, through which the mechanics are integrated into endothelial TGFβ/BMP signaling. Integrin-dependent traction forces emerging from FAs directly participate in liberating TGFβ as a biologically active growth factor, from its latent form (i.e., biologically inactive) (Figure 3c). In detail, TGFβ1/3 remains associated with a latency associated peptide (LAP) after secretion [149,150], which shields receptor-binding epitopes and preserves the inactive growth factor as part of an extracellular depot (Figure 3). Deposition of this latent TGFβ complex to ECM is facilitated via tethering to fibrillin fibers [151,152], through the adaptor protein latent TGFβ binding protein (LTBP) [153,154]. LTBP covalently links the latent TGFβ to the ECM, through an iso-peptide bond between LTBP and fibrillin [155]. Interestingly, it was found that activation of TGFβ ligands requires binding and pulling of specific integrins, such as αvβ1, αvβ6, and αvβ8 [156] on LAP RGD motif, to release the active forms of TGFβ1/3 [150,156,157] (Figure 3c). For this mechanism, it is important that the ECM, to which the latent complex is tethered, provides a certain degree of mechanical elasticity and thus provides resistance against the pulling forces applied by the cells. In fact, it was shown that ECM remodeling, preceding the activation step, mechanically primes latent TGFβ1, akin to loading a mechanical spring [158]. Hinz and co-workers found that stiff ECM allows a more efficient integrin-mediated TGFβ retrieval from the latent depot, compared to soft ECM [150] (Figure 3c). A soft matrix with an elastic modulus (E) ≤ 5 kPa preferentially deforms under the stresses applied by cells, leaving the latent complex intact and the TGFβ extracellularly sequestered. Whereas a stiff matrix with E >> 10 kPa resists deformation, resulting in distortion of the latent complex and the release of active TGFβ. The crucial role for ECM elasticity and integrin-mediated traction forces is underlined by the finding that absence of integrin-mediated TGFβ1 activation in vivo recapitulates the phenotype of TGFβ1-null mice [157]. Mechanistically, integrin binding to LAP allows conformational changes of the latent complex through actomyosin-generated tensile force, which act through the integrin β-subunit [158,159,160]. Structural analysis of latent TGFβ by the Springer group showed that this resembles the opening of a “straitjacket” [161]. Interestingly, TGFβ released by such mechano-dependent mechanism signals in close vicinity to the cell pulling [162], creating a local niche environment enriched in TGFβ. Forces required to induce a conformational change in LAP were measured to be in the tens of piconewton range [160]. It is to be noted that this level of force can be sustained by individual integrins and produced by few myosin motors, and it is a thousand times lower than the forces transmitted by one single FA [163]. Mature BMPs were also shown to bind to ECM, including tenascin-c, heparins, and laminins [164,165,166], creating an extracellular BMP growth factor depot. In contrast to integrin-mediated pulling forces, their bioavailability might be dependent on mechanisms including secretion of matrix metalloproteinases (MMPs), leading to ECM degradation and subsequent BMP release (Figure 3c). Here, MMP expression in ECs was shown to be dependent on cyclic stretch and strain [167,168,169]. TGFβ also acts upstream of integrin and ECM expression (Figure 3c), highlighted by findings that TGFβ2 stimulation of ECs can directly enhance cell-matrix traction stresses [136]. TGFβ induces expression of integrins α2, α5, αv, β1, and β3 in both microvascular [170] and macrovascular ECs [171,172]. Moreover, TGFβ induces expression of ECM proteins, including fibronectin and collagens I, IV, V (Figure 3c). We showed previously that depletion of endothelial BMPR2 shifts signaling responses from BMP towards TGFβ through increased mechanical retrieval of active TGFβ from the ECM. BMPR2 deficiency led to enhanced contractile forces and stiffness of ECs [173]. This suggests that unbalancing BMP and TGFβ signaling is sufficient to induce major mechanical alterations on the level of cell adhesion and composition of the ECM. Moreover, TGFβ/BMP receptors might directly cooperate with integrins. It was shown before that endoglin mediates fibronectin/α5β1 integrin and TGFβ pathway crosstalk in ECs [174]. Fibronectin and its cellular receptor α5β1 integrin specifically increase TGFβ1- and BMP9-induced Smad1/5/8 phosphorylation, via endoglin and ALK1. Endoglin controls cell migration and composition of FAs by interacting with the FA-related protein zyxin [2]. Upon BMP9 stimulation, endoglin regulates subcellular localization of zyxin in FAs [175]. Latent TGFβ becomes biologically active, not only by cell-mediated integrin pulling, but also by the shear forces acting on the latent complex [176,177]. More recently, it was found that oscillatory shear stress (OSS) potentiates latent TGFβ1 activation, more than laminar FSS. Abrupt changes in rotation direction seem sufficient to recruit mature TGFβ from the latent complex [178]. These findings highlight the role of excessive TGFβ signaling for vascular pathologies that involve dysregulated integrin expression on one hand, and disturbed flow regimes on the other. Together, at the FA compartment, integrin-mediated traction/pulling forces on the ECM or latent TGFβ provides a delicate mechanism of how ECs mechanically interact with the environment. Interfering with such mechanisms or the TGFβ/BMP-signaling dependent upregulation of integrins or ECM proteins could be a promising strategy to target vascular pathologies.
4. BMP/TGFβ Signaling and Integration of Basolateral Forces
Mature ECs are mechanically coupled both to the ECM and via cell junctions to neighboring cells (Figure 4). However, the balance, coordination, and interdependency of these forces are poorly understood. Junctional resolution is a hallmark of EndMT, characterized by loss of EC junctional proteins such as vascular endothelial (VE)-cadherin and Platelet and Endothelial Cell Adhesion Molecule (PECAM)-1, both essential to maintain cell barrier integrity. EndMT is favored under perturbed BMP and TGFβ signaling in disease, but also in normal development, such as formation of the endocardial cushions in the atrioventricular canal [62,179], and is characterized by the expression of Snail, Slug, and Twist genes [179,180,181].
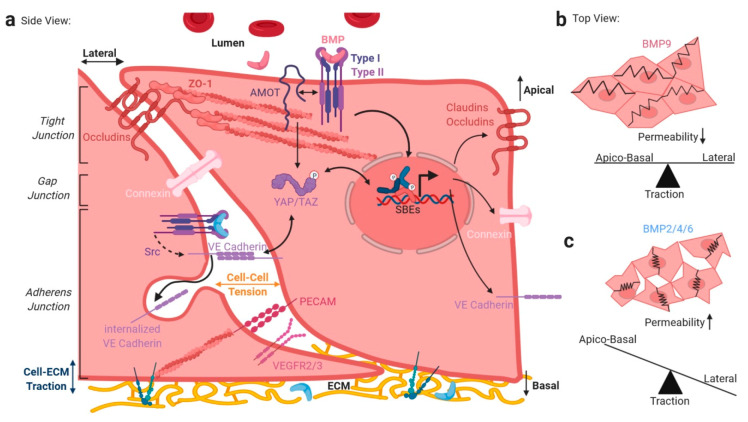
Figure 4.
Crosstalk of mechanical and TGFβ/BMP signaling at endothelial cell junctions. EC junctions are crucial for cell–to-cell communications and barrier function (a). Apical TJs, composed mainly of claudins and occludins connect to the cytoskeleton via zona occludens (ZO) proteins, regulating trans-endothelial macromolecule transport by narrowing the inter-endothelial junction size. AJ-related protein AMOT regulates the apical BMP signaling by interaction with BMP receptors. Gap junctions allow communication between neighboring ECs via pore-forming proteins like connexins. Basal AJs constitute connection points of cell–ECM and cell–cell interactions. The main components are the trans-interacting proteins VE-Cadherin and PECAM-1, together with VEGFR2/3, which form a mechanosensory complex, necessary for FSS sensation. VE-Cadherin internalization and thus AJ resolution is regulated by BMP signaling via Src. Additionally, VE-Cadherin associated β-Catenin complex interacts with YAP/TAZ in the cytoplasm, and YAP/TAZ interacts with SMADs proposed to influence SMAD stability, shuttling, and transcriptional competence. SMAD gene transcription regulates the expression of several junctional proteins like claudins, occludins, connexins, or VE-Cadherin. Here, distinct BMP ligands exhibit different potentials of junction regulation and thus cell–cell and cell–ECM traction (a). As proposed on the right, homeostatic BMP9 might decrease EC permeability by keeping a balance of apical–basal and lateral traction (b). In contrast, BMP2/4/6 might increase EC permeability by shifting towards apico-basal traction (c). Abbreviations: SBE-—MAD binding elements, TJs—Tight junctions, AJs—Adherens junctions.
It was recently found that force sustained at the cell–cell contact between epithelial cells is approximately 100 nN, directed perpendicular to the cell–cell interface and concentrated at the contact edges [182]. Intriguingly, a direct relationship between the total cellular traction force on the ECM and the endogenous cell–cell force exists, indicating that cell–cell tension is a constant fraction of cell–ECM traction (Figure 4a) [182]. Mechanisms disrupting this balance, e.g., up-regulation of cell-substrate adhesion-related proteins such as integrins, directly imbalance EC cell–cell connectivity and thus the EC barrier function. While cell–ECM traction is facilitated via ECM-bound integrin clusters at FAs, cell–cell tension is mediated via cell junction proteins like VE-cadherin and PECAM-1, providing mechanical stability by zipper-like trans-intermolecular interactions (Figure 4). If seen as force vectors, force distribution is thus balanced between apico-basal traction forces and tensile forces in the lateral plane, or in other words, cell adhesion forces influence junctional forces (see Figure 4b,c). EC junctions can be subdivided into tight (TJs), gap (GJ), and adherens junctions (AJs) [183]. TGFβ/BMP signaling integrates into balancing junctional forces twofold. First, TGFβ/BMP signaling regulates integrin expression and ECM deposition, as mentioned earlier, impacting the cell–ECM traction, and second, lateral cell–cell tension is affected by the TGFβ/BMP-dependent regulation of junctional protein localization, expression, and their turnover/endocytosis (Figure 4).
We recently showed that angiomotin (AMOT), a TJ-associated membrane protein, drives BMP-SMAD signaling at the apical membrane in polarized cells. In HUVECs, AMOT interacts with BMPR2 and knockdown of AMOT reduces SMAD signaling, only from the apical side of polarized cells, while basolateral BMP-SMAD signaling remained unaffected [4] (Figure 4a, upper). For example, microvascular beds specifically rely on TJs, as part of the blood–brain barrier (BBB) [184]. TGFβ1 was shown to promote barrier function upon maturation of corneal ECs [185] and to upregulate tight junction- and P-glyco-proteins in brain microvascular ECs [186]. Further, depletion of TGFβ1 in vivo and in vitro leads to a breakdown of the microvascular blood–retinal-barrier. This was characterized by decreased association between the TJ proteins ZO-1 and occludin [187]. Second, concerning GJs, it was demonstrated that Cx37 (Connexin37) is a differentially regulated target of ligand-induced and mechano-transduced SMAD1/5 signaling, and that the Cx37-loss enables pathological vessel enlargement and shunting [119]. Moreover, the ALK1 signaling axis was found to regulate endothelial Cx40 expression [188]. AJs contribute significantly to the EC barrier function and are prone to regulation by FSS, which reorganizes junction-associated proteins [189]. We recently reported that BMP6 leads to Src-dependent phosphorylation of VE-Cadherin and subsequent internalization (Figure 4a, depicted in center), ultimately leading to EC hyperpermeability [29]. Concordantly, BMP4 was reported to regulate leukocyte diapedesis and promote EC inflammation, while BMP4 KO leads to increased VE-Cadherin expression [190]. Both BMP2 [191] and BMP4 increased vascular permeability [192]. These results in summary showed that BMP2/4/6 induce EC permeability, likely resulting in reduced cell–cell tension. In contrast, BMP9/ALK1 signaling prevents vascular permeability and was recently shown to prevent the leakiness of the inflamed lung microvasculature [193]. BMP9-ALK1 signaling facilitates cell–cell contacts and balances the interdependency between apico-basal and lateral forces [194]; Figure 4b,c. This is further supported by the finding that BMP9/ALK1 signaling prevents VEGF-induced phosphorylation of VE-cadherin, and induces the expression of occludin, thus, strengthening the vascular barrier functions [194]. Third, the VE–cadherin–catenin complex forms the molecular basis of AJs and cooperates with actin filaments, controlled by the Arp2/3 complex. While fully mature EC monolayers have long and tight junctions, activated ECs display more transient and lesser stable cell-to-cell interactions. The junctional dynamics through which ECs form these highly dynamic interactions were studied in detail in the presence of FSS [195], and were termed junction-associated intermittent lamellipodia (JAILs) [196]. JAILs allow for subcellular organization of junctional forces homing clusters of VE-Cadherins [196]. Dynamic JAIL remodeling of confluent EC monolayers exposed to FSS is important to maintain barrier integrity or allow for cell migration and angiogenesis [197]. AJs are rich in a FSS mechanosensitive super-complex, composed of VE-Cadherin, VEGFR2/3, and PECAM1 [198,199]; Figure 4a, center. However, it is not clear whether this complex acts in cooperation with or independent of FSS-sensitive mechano-complexes, comprising integrins and BMP receptors [112]. In support of such cooperation is that VE-cadherin was reported to co-immunoprecipitate with all components of the TGFβ receptor complex—TGFβRII, ALK1, ALK5, and endoglin. Accordingly, ECs lacking VE-cadherin are less responsive to TGFβ/ALK1- and TGFβ/ALK5-induced SMAD phosphorylation and target gene transcription [200]. Interestingly, AMOT can retain YAP/TAZ in the cytosol and VE-Cadherin tethers it to stable junctions [201,202,203]; Figure 4a. In line with this, excluding endothelial YAP/TAZ from the nucleus by tethering it to junctions, i.e., through mechanical regulation, such as reduced junctional tension, could limit nuclear SMAD signaling, as shown for fibroblasts, for example [73]. However, Gerhardt et al. recently found that YAP/TAZ act upstream of junctional VE-cadherin turnover and that nuclear YAP and TAZ also decreases endothelial BMP signaling, possibly by increasing the expression of BMP inhibitors [204]. Together, it could be concluded that EC junctions build a discrete subcellular compartment, where TGFβ/BMP signaling integrates into mechanobiology, and that in healthy blood vessels, a balanced equilibrium of basolateral forces is tightly coupled to a similarly balanced TGFβ/BMP signaling. Targeting this in the context of pathological changes in vascular barrier functionality would be an interesting opportunity.
5. Shear-Stress-Induced TGFβ/BMP Signaling at the Primary Cilium
EC phenotype and homeostasis are maintained by a unidirectional, laminar blood flow, ranging approximately from 1 to 5 Pa (Pa; equals 10–50 dyn/cm2) in human vessels [205]. This laminar fluid shear stress (FSS) is typically vaso/aterio-protective. The vessel architecture at bifurcations, curvatures, and rough luminal topographies, could create inhomogeneous flow dynamics, such as at venous and lymphatic valves, termed oscillatory shear stress (OSS) or disturbed shear stress (DSS). OSS and DSS are characteristic of low shear stress, flow reversal, and in the latter case, chaotic turbulent flow regimes. Regions of OSS/DSS blood flow perturbation, together with hyperlipidemia, could show signs of inflammation, including low nitric oxide production, reduced barrier function, and increased pro-adhesive, pro-coagulant, and pro-proliferative properties. Shear stress is sensed mainly by cells, through the primary cilium (Figure 5a), a single microtubule-driven membrane protrusion on the apical side. However, according to the decentralized model of endothelial mechano-transduction [206], FSS integrates into all compartments mentioned in this review and a single shear stress mechano-transducer is unlikely to exist.
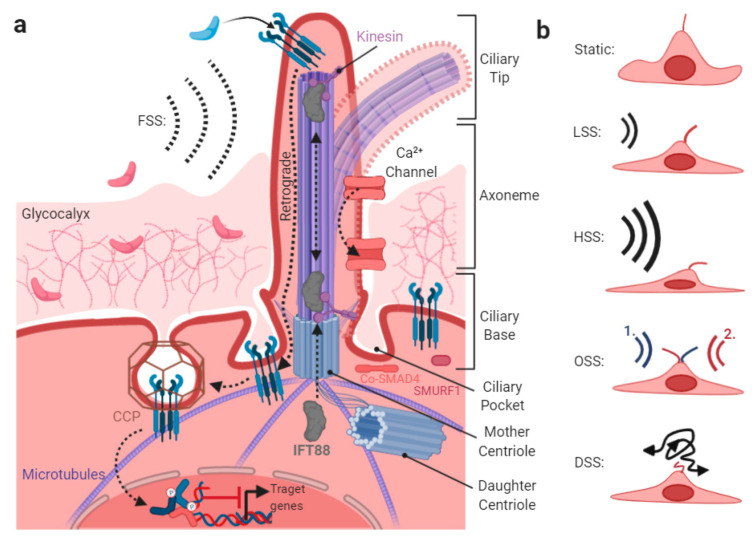
Figure 5.
Crosstalk of fluid shear stress and TGFβ/BMP signaling at the primary cilium. The primary cilium is composed of a mother and a daughter centriole connected to other cellular compartments (like the Golgi apparatus), through extended microtubules. The axoneme, consisting of 9 pairs of microtubules, extends from the mother centriole in the vascular lumen, protrudes the PM, and exceeds the surrounding glycocalyx. Build up and maintenance of the axoneme is regulated by the shuttling proteins, e.g., IFT88 connected to motor proteins like kinesin. BMP/TGFβ receptors are mainly found at the ciliary tip, the most distal part of the axoneme. Upon ligand binding, retrograde shuttling of receptors towards the ciliary base, the part proximal to the mother centriole, is initiated. The ciliary base is a hotspot for clathrin-mediated endocytosis, which might be crucial for tuning cellular sensitivity to TGFβ, by regulating receptor endocytosis. Additionally, SMAD4 and SMURF1 are found at the ciliary base (a). Deflection properties of cilia in response to different FSS regimes are indicated on the right (b). Abbreviations: CCP—clathrin-coated pit, FSS—fluid shear stress, LSS—low shear stress, HSS—high shear stress, OSS—oscillatory shear stress, and DSS—disturbed shear stress.
The main flow-induced force acting on the ciliary membrane is bending vs. relaxation [207] (Figure 5a). Cilia deflect sideward, in response to unidirectional low shear stress (LSS) or high shear stress (HSS) [208], whereas they deflect in alternate directions at OSS or DSS, according to a heavy elastic model [209] (Figure 5b). Consequently, a direct activation of ciliary-membrane-located receptors involves conformational changes induced by cilia mechanical bending [209,210], as best studied for calcium channels [211], depicted in Figure 5. Interestingly, depletion of osmolarity and cell volume regulating calcium channel TRPV4 in mice, completely abolishes shear stress induced vasodilation [212]. TRPV4 localizes to mesenchymal stem cell cilia [213] and it was shown that the differentiation process of cardiac fibroblasts to myofibroblasts is dependent on TRPV4, which integrates mechanical (i.e., ECM stiffness) and TGFβ signals [214]. Moreover, interfering with TRPV4 signaling blocks TGFβ-induced epithelial-to-mesenchymal transition (EMT) in normal mouse primary epidermal keratinocytes (NMEKs) [215]. It is thus tempting to speculate that TRPV4 might also be a regulator of mechano-TGFβ crosstalk in the endothelium.
Receptors located at the tip of the cilium are activated upon ciliary deflection [213]. TGFβ/BMP signaling was shown to regulate the formation and length of primary cilia [216,217], including regulation of IFT88 expression [218], a major ciliary structural protein. In ECs, a lack of primary cilia primes shear-induced EndMT via the TGFβ-ALK5-SMAD2/3 axis [219] and ECs lacking primary cilia are sensitized to undergo TGFβ/BMP-induced EndMT (reviewed in [181]). This is in line with the finding that Slug is expressed in ECs lacking primary cilia, promoting EndMT and cellular calcification [220]. Furthermore, TGF-β receptors were shown to be endocytosed at the pocket region of the primary cilium (Figure 5), while TGFβ stimulation increased receptor localization and activation of SMAD2/3 and ERK1/2 at the ciliary base, along with SMAD4 accumulation [221] (Figure 5a).
With regards to endothelial ALK1-BMP9 signaling, primary cilia sensitize ECs to BMP9 ligands and prevent excessive vascular regression [222]. Here, it was proposed that BMP9 signaling positively cooperates with the primary cilia at low flow, to keep the immature vessels open before high–shear-stress-mediated remodeling [222]. The finding that the ALK1-BMP9-SMAD1/5/9 signaling axis is specifically enriched at the primary cilia, is in line with the observation that ALK1 appears enriched around the cilium. Moreover, prominent phosphorylation of SMAD1/5/9 was found at the basal body and along the cilium. Furthermore, FSS increases the physical interaction between ALK1 and endoglin, and thereby lowers the effective concentration of BMP9 required for ALK1 activation [84]. FSS-enhanced association of Alk1 and endoglin, showed that Alk1 is required for BMP9 and flow responses, whereas endoglin is only required to enhance the effects of flow [84]. Finally, both TGFβ and BMP signaling is fine-tuned in a ciliary-compartment-specific manner through several PTMs at the receptor- and SMAD-levels. For example, it was found that the E3 ubiquitin ligase SMURF1 localizes to the cilium and controls local BMP signaling [223] (Figure 5a).
The Endothelial Glycocalyx
A significant portion of the apically applied FSS is absorbed by the glycocalyx, a thick coat of glycoproteins and proteoglycans that is negatively charged, forming a brush-like cushion on the surface of ECs (Figure 5a, upper). The glycocalyx varies in its viscoelastic properties, due to the degree of crosslinked side chains [224] and has a thickness reaching up to 0.5–3 μm into the lumen of vessels. This relatively large glycocalyx exceeds the thickness of the endothelium and the length of several apically localized transmembrane receptors, including leucocyte adhesion molecules [225] and TGFβ/BMP receptors, if not localized to ciliary tips surpassing the glycocalyx. The glycocalyx was found to be thinner in atherosclerotic risk regions, where OSS/DSS can be expected [226], while it is thickened under protective FSS [227]. Moreover, proteases involved in ECM degradation, and consequently releasing ECM-bound growth factors, are expressed upon FSS [228,229], as well as furin, a pro-TGFβ processing protease [230]. Since both TGFβs and BMPs are positively charged and were found to bind to negatively charged heparins [231,232], it was proposed that the glycocalyx could provide a superb reservoir for TGFβ/BMP growth factors, as well as their antagonists, including Noggin [233,234].
Together, the primary cilium acts as a small but important center for integrating FSS into TGFβ/BMP signaling. Current advances in super resolution microscopy and development of in vitro flow devices will add further knowledge on how TGFβ/BMP receptors and their signaling are regulated at the primary cilium. The modes of how FSS and the glycocalyx regulate TGFβ/BMP signaling and bioavailability are important to understand vascular diseases, e.g., arteriosclerosis.
6. Integrating Forces into Nuclear TGFβ/BMP Signaling
The term shear stress response element (SSRE) was first proposed after the identification of the sequence GAGACC, within the shear stress responsive gene promoters [235], and was later extended to a number of other shear stress responsive elements. Among several cis-acting elements that were implicated in mediating shear modulation of gene expression, one example of a factor that binds to the GAGACC promoter region, is the transcription factor nuclear factor κ-B (NF-κB) p50–p65 heterodimers. Another factor found to bind SSRE is myocyte enhancer factor 2 (MEF2), downstream of MAPK or PI3K signals, which regulates the well-studied shear–stress-induced expression of Krüppel-like factors (KLFs) [236]. One mechanism making shear–stress-sensitive genes competent for transcription, is the regulation of the nuclear architecture itself. Here, the EC nucleus is appreciated as a direct sensor of blood flow direction [237] and possesses its own mechanosensitive apparatus [238]. Global EC responses to FSS include nuclear elongation, position adaptation of nuclear-envelope-associated organelles against the direction of flow [239] and a ´streamlined´ cell morphology [240]. When ECs adapt to shear stress, forming an upstream edge, the centrosome positions relative to the nucleus, driven by the actin and microtubule networks in a ´string puppet´-like fashion (Figure 6a,b). Indeed, the centrosome is an ideal integrator of extracellular and intracellular mechanical signals [241]. Interestingly, ECs with depletion of SMAD4 fail to migrate against the direction of FSS [16].
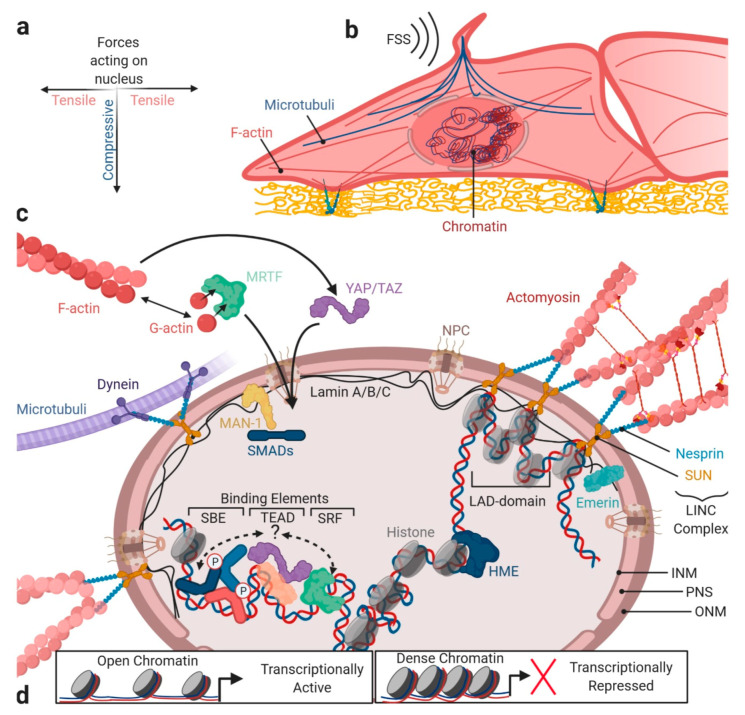
Figure 6.
TGFβ/BMP signaling crosstalk and nuclear mechanics. The nucleus is connected to the PM, including the primary cilium, junctions, and cell–ECM contacts via the F-actin fibers and microtubules. Thereby, the nucleus is indirectly exposed to external mechanical forces acting in a tensile (via F-actin) and compressive (via microtubules) fashion (a), e.g., induced by FSS (b). In particular, the filaments are connected to the inner and outer nuclear membrane (INM/ONM) via LINC complexes, composed of the nesprin and SUN proteins (c). For microtubule, connection to LINC complexes is mediated via dynein. By transmission of external forces, opening of NPCs might be regulated, allowing a more efficient influx of TFs, like SMADs or F/G-actin-ratio-sensing MRTF, or co-factors like YAP/TAZ. TFs can regulate the transcription of target genes in regions of “open” heterochromatin. SMADs can direct HMEs to target gene sequences, thereby allowing epigenetic modification and thus the activation or repression of genes (d). Chromatin compartments of inactive euchromatin are merely found to be proximal to the INM in lamin-associated LADs. Additional to lamins, integral proteins like MAN-1 sit in the NM. MAN-1 confers a further layer of BMP signaling regulation, by binding SMADs and competing with the co-factor binding. Abbreviations: NPC—nuclear pore complex, ONM—outer nuclear membrane, PNS—perinuclear space, INM—inner nuclear membrane, LAD—lamina-associated domain, HME—histone modifying enzyme, and SBE—SMAD binding element.
6.1. Forces Acting at the Nuclear Envelope
Nuclear import of several transcription factors is altered upon the application of FSS, including YAP [242]. One mode of how forces promote nuclear import of transcription factors is direct force transmission towards stretching and widening of nuclear pore complexes (NPCs), as shown for YAP shuttling [243]. Impressively, mechano-transduction bypasses the kinetics of biochemical signaling, as shown for Src (<0.3 s of mechanical Src activation vs. >12 s by soluble epidermal growth factor stimulation) [244]. Recent reports indicate that forces are directly transmitted from the ECM to the nucleus, via the cytoskeleton (reviewed in [238,245]). Physically, forces are coupled to the nucleus via a mechanical hardwiring established between the junctional cadherins and integrins within FAs that enable bridging of cytoskeletal filaments, which reach out to the linker proteins attached to the nuclear envelope [246]; Figure 6b,c. The actin and microtubule cytoskeletons exert differential control on nuclear morphology [247]. While the actin and actomyosin fibers provide tensile forces to the nucleus in a lateral plane, mechanical loading of the nucleus is facilitated by compression through microtubules on top of the nucleus [247,248,249,250] (Figure 6a,b). Furthermore, cells can protect their nucleus from deformation through an actin cap, shielding the nucleus from mechanical stress from the top [251]. A proper positioning of the actin cap is dependent on basal zyxin FAs, with perinuclear localization [252,253]. Concerning the nuclear structure, the nuclear envelope is composed of the outer nuclear membrane (ONM), and the inner nuclear membrane (INM), separated by the perinuclear space (PNS) (Figure 6c). A key feature of the nuclear envelope is the nuclear lamina (NL), a polymer mesh lining the inner surface of the INM, formed by lamins. These levels of lamin A/C determine the nuclear envelope stiffness and deformability [254,255,256]. Supporting this, lamin A/C-deficient cells exhibited increased numbers of misshaped nuclei and severely reduced nuclear stiffness [255,257]. Interestingly, ECM stiffness directly influences lamin A expression [258], and LSS (5 dyn/cm2) leads to decreased lamin A/C expression in ECs [259]. However, this differs between the young and aged ECs [260]. Regarding TGFβ signaling, a deficiency in A-type lamins correlates with the hyperactivation of TGFβ signaling [261,262]. In epithelial cells, TGFβ-induced EMT leads to downregulation of lamin A/C, lamin B, the nuclear envelope membrane protein emerin, and multiple nucleoporins forming the NPC [263,264]. Further crucial nuclear envelope proteins are integral inner nuclear membrane proteins, such as MAN-1. MAN-1 binds R-SMADs but not co- and I-SMADs, thereby competing with the transcriptional co-factors for binding to SMADs (Figure 6c). Additionally, MAN-1 facilitates SMAD dephosphorylation through phosphatase PPM1, which represses signaling by both TGFβ and BMPs [265,266,267,268,269]. Mechanical force transduction acting from outside of the cell towards the nuclear envelope requires tethering of cytoskeletal elements to the Linker of Nucleoskeleton and Cytoskeleton (LINC) complex, formed by the interaction of nuclear envelope spectrin-repeat proteins (nesprins) and Sad1p, UNC-84 (SUN) proteins [245,270,271]. Both nesprin and SUN proteins are downregulated in ECs, when exposed to LSS, providing a relevance for altered nuclear mechano-sensation via LINC, during vascular dysfunction [272]. Different nesprin isoforms orchestrate coupling of the SUN complex to either actin fibers, microtubules, or intermediate filaments (Figure 6c). Importantly, there is strong evidence that nesprins also influence SMAD nuclear shuttling, as depletion of nesprin-2 in HaCaT cells lead to slower TGFβ-induced nuclear translocation of SMAD2/3. Here, nesprin, based on its ability to interact with emerin and lamin, was suggested to affect TGFβ/SMAD signaling, as emerin is directly involved in this signaling pathway through its interaction with MAN-1 [273].
6.2. Forces Acting on the Chromosomal Architecture
Cytoskeletal forces acting on the LINC complex influence heterochromatin localization and core histone protein mobility, and thereby, directly alter gene transcription and induce epigenetic changes (Figure 6d). Transcriptionally inactive heterochromatin, which is marked by a distinct pattern of histone trimethylation and acetylation, tends to localize to the NL, creating the so-called lamina associated domains (LADs) [274,275] (Figure 6d). Interestingly, mature ECs with a quiescent phenotype have a high dependency on epigenetic regulators that maintain this phenotype. Transcriptomic and epigenetic mapping of quiescent lung endothelium revealed that inhibitory SMAD6 and SMAD7 are particularly epigenetically regulated in quiescent ECs, to control TGFβ signaling [276]. SMADs also co-immunoprecipitate with histone-modifying enzymes (HME, Figure 6c) such as histone deacetylases (HDACs), homeodomain protein TG-interacting factor (TGIF), and histone methyltransferases. This provides a mechanism through which SMAD binding to the DNA influences the epigenetic landscape in vascular development and homeostasis [277,278], and provides a mechanism that allows SMADs to become transcriptional repressors [279,280].
6.3. Forces and SMAD Transcriptional Co-Factors
A third way through which mechanics integrate into nuclear TGFβ/BMP signaling is through the SMAD dependency on transcriptional co-factors that act in cis or trans to recruit additional enhancers to the SMAD-binding elements. Thus, they increase SMADs transcriptional activity and direct the SMAD complex to particular target genes (Figure 6). Two mechanically regulated pathways were shown to integrate into SMAD signaling in ECs—YAP/TAZ and myocardin-related transcription factor-A (MRTF-A) signaling. TGFβ was shown to induce formation of YAP/TAZ–Smad2/3-4 complexes [71,281] and BMPs were shown to induce YAP/TAZ-Smad1/5-4 complexes [282,283], however, there is evidence that SMADs 2/3 and SMADs 1/5/9 react differently to YAP/TAZ incorporation, with respect to their transcriptional activity. YAP/TAZ are incapable of directly binding DNA, but instead they interact with the TEA domain transcription factors (TEADs) [284]. Mechanistically, YAP/TAZ in complex with TGFβ-SMADs (SMAD2/3) and co-Smad4, require concomitant binding to SMAD binding elements (SBEs) and TEAD promoter elements, such as that found in promoters of cysteine-rich angiogenic inducer 61 (CYR61) [285,286] and connective tissue growth factor (CTGF) [287]. For BMP SMADs, it was found that Smad1/5/Smad4 binding with YAP/TAZ competed with YAP for the TEAD interaction and inhibited YAP’s co-transcriptional activity [283]. However, data also showed that BMP-SMAD1/5 interaction with YAP/TAZ increased transcriptional activity, which might depend on a stabilizing role of YAP binding for SMAD protein [282,288].
A delicate mechanism through which MRTF-A transcription factor integrates into the mechano-dependency of TGFβ/BMP SMAD signaling, is the ability of MRTF-A to directly sense the status of actin remodeling, by binding to globular actin (G-actin) (Figure 6c). MRTF-A is required for TGF-β2-induced α-SMA expression [289] and regulates Slug expression in synergy with TGFβ [290]. MRTFs are co-activators of serum response factor (SRF)-dependent transcription [291] and MRTF-A was shown to interact with TGFβ-SMAD3 [290] and BMP-Smad1 [292], to co-activate the expression of SMAD target genes (Figure 6). In the repressed state of MRTF-A, monomeric G-actin binds in a 5:1 complex to MRTF-A. Transcriptionally inactive G-actin:MRTF-A complexes are found both outside and inside the nucleus, and either inhibit the nuclear import or foster the nuclear export of MRTF-A [293]. Importantly, MRTF nuclear translocation and transcriptional activation depends on competition with actin regulatory proteins, such as the Wiskott–Aldrich syndrome protein (WASP) for G-actin binding [294]. In TGFβ-induced EMT, nuclear localization of MRTF-A correlates directly with mechanical stress, tissue geometry, and the resultant variability in cytoskeleton dynamics of epithelial cells [295]. Mechanistically, the same scenario is likely to occur during TGFβ-induced EndMT. Furthermore, the SMAD-MRTF-A complex could form an interesting Ménage-à-trois relationship with the aforementioned YAP/TAZ transcription factors. While functional relationship between YAP/TAZ and MRTF-A in ECs was suggested before [296], it could be speculated that cooperation of this complex exists together with SMADs [5,297] (Figure 6c).
7. Perspective and Concluding Remarks
As summarized here, crosstalk of endothelial mechanobiology and TGFβ/BMP signaling has a pivotal role for endothelial physiology and pathology. The various mechanisms through which mechanobiology integrate into this delicate signaling network create another layer of regulation that participates in fine-tuning and diversifying TGFβ/BMP signaling. We and others aim to understand the precise molecular mechanisms behind this signaling crosstalk. Such basic molecular investigations remain challenging in an in vivo setting. While previous data gained under static EC culture are a first approximation, technical developments for in vitro tissue culture now allow us to study ECs signaling under biochemical and mechanical conditions, which make these data more relevant to the human system.
We have cited examples of how TGFβ/BMP signaling integrates into mechano-transduction in a compartment-specific manner. With crosstalks at discrete membrane domains, the cytoskeleton, the primary cilium, and the nucleus listed, show some of the most crucial compartments integrating EC mechanics into TGFβ/BMP signaling and vice versa. Since investigating endothelial TGFβ/BMP mechano-crosstalk is a relatively young research field, we cited a number of research articles on non-endothelial cells, where we considered as a wealth of evidence that in ECs it might be mechanistically similarly relevant. However, it remains to be proven whether all of the mentioned crosstalk mechanisms were conserved between other cell types and ECs. Further research will help answer these questions and to better understand crosstalk mechanisms of TGFβ/BMP signaling with mechanobiology that underlie human vascular pathologies.
Acknowledgments
The authors would like to thank Carolina DaSilva Madaleno and Susanne Hildebrandt for commenting on the manuscript. We thank Boris Hinz, Hans Schnittler, and Maike Frye for valuable discussions.
Author Contributions
Conceptualization, C.H. and P.-L.M.; Writing and editing C.H., P.-L.M., and P.K.; Figures preparation, C.H.; Supervision, P.K.; Funding acquisition and resources P.K. All authors have read and agreed to the published version of the manuscript.
Funding
P.K. was supported by the Deutsche Forschungsgemeinschaft (DFG), FOR2165, P.-L.M. is funded by the international Max-Planck Research School for Biology and Computation. All figures were created by using BioRender.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Miller D.S.J., Schmierer B., Hill C.S. Tgf-β family ligands exhibit distinct signalling dynamics that are driven by receptor localisation. J. Cell Sci. 2019;132 doi: 10.1242/jcs.234039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Conley B.A., Koleva R., Smith J.D., Kacer D., Zhang D., Bernabéu C., Vary C.P. Endoglin controls cell migration and composition of focal adhesions: Function of the cytosolic domain. J. Biol. Chem. 2004;279:27440–27449. doi: 10.1074/jbc.M312561200. [DOI] [PubMed] [Google Scholar]
- 3.López-Casillas F., Payne H.M., Andres J.L., Massagué J. Betaglycan can act as a dual modulator of tgf-beta access to signaling receptors: Mapping of ligand binding and gag attachment sites. J. Cell Biol. 1994;124:557–568. doi: 10.1083/jcb.124.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brunner P., Hastar N., Kaehler C., Burdzinski W., Jatzlau J., Knaus P. Amot130 drives bmp-smad signaling at the apical membrane in polarized cells. Mol. Biol. Cell. 2020;31:118–130. doi: 10.1091/mbc.E19-03-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miranda M.Z., Bialik J.F., Speight P., Dan Q., Yeung T., Szászi K., Pedersen S.F., Kapus A. Tgf-β1 regulates the expression and transcriptional activity of taz protein via a smad3-independent, myocardin-related transcription factor-mediated mechanism. J. Biol. Chem. 2017;292:14902–14920. doi: 10.1074/jbc.M117.780502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.García de Vinuesa A., Abdelilah-Seyfried S., Knaus P., Zwijsen A., Bailly S. Bmp signaling in vascular biology and dysfunction. Cytokine Growth Factor Rev. 2016;27:65–79. doi: 10.1016/j.cytogfr.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 7.David L., Feige J.J., Bailly S. Emerging role of bone morphogenetic proteins in angiogenesis. Cytokine Growth Factor Rev. 2009;20:203–212. doi: 10.1016/j.cytogfr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Beets K., Huylebroeck D., Moya I.M., Umans L., Zwijsen A. Robustness in angiogenesis: Notch and bmp shaping waves. Trends Genet. 2013;29:140–149. doi: 10.1016/j.tig.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Goumans M.J., Zwijsen A., Ten Dijke P., Bailly S. Bone morphogenetic proteins in vascular homeostasis and disease. Cold Spring Harb. Perspect. Biol. 2018;10:a031989. doi: 10.1101/cshperspect.a031989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cai J., Pardali E., Sánchez-Duffhues G., ten Dijke P. Bmp signaling in vascular diseases. FEBS Lett. 2012;586:1993–2002. doi: 10.1016/j.febslet.2012.04.030. [DOI] [PubMed] [Google Scholar]
- 11.Cunha S.I., Magnusson P.U., Dejana E., Lampugnani M.G. Deregulated tgf-β/bmp signaling in vascular malformations. Circ. Res. 2017;121:981–999. doi: 10.1161/CIRCRESAHA.117.309930. [DOI] [PubMed] [Google Scholar]
- 12.MacCarrick G., Black J.H., 3rd, Bowdin S., El-Hamamsy I., Frischmeyer-Guerrerio P.A., Guerrerio A.L., Sponseller P.D., Loeys B., Dietz H.C., 3rd Loeys-dietz syndrome: A primer for diagnosis and management. Genet. Med. Off. J. Am. Coll. Med. Genet. 2014;16:576–587. doi: 10.1038/gim.2014.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang X., Liaw L., Prudovsky I., Brooks P.C., Vary C., Oxburgh L., Friesel R. Fibroblast growth factor signaling in the vasculature. Curr. Atheroscler. Rep. 2015;17:509. doi: 10.1007/s11883-015-0509-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adams R.H., Alitalo K. Molecular regulation of angiogenesis and lymphangiogenesis. Nat. Rev. Mol. Cell Biol. 2007;8:464–478. doi: 10.1038/nrm2183. [DOI] [PubMed] [Google Scholar]
- 15.Augustin H.G., Koh G.Y., Thurston G., Alitalo K. Control of vascular morphogenesis and homeostasis through the angiopoietin-tie system. Nat. Rev. Mol. Cell Biol. 2009;10:165–177. doi: 10.1038/nrm2639. [DOI] [PubMed] [Google Scholar]
- 16.Lee H.W., Chong D.C., Ola R., Dunworth W.P., Meadows S., Ka J., Kaartinen V.M., Qyang Y., Cleaver O., Bautch V.L., et al. Alk2/acvr1 and alk3/bmpr1a provide essential function for bone morphogenetic protein-induced retinal angiogenesis. Arterioscler. Thromb. Vasc. Biol. 2017;37:657–663. doi: 10.1161/ATVBAHA.116.308422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benn A., Hiepen C., Osterland M., Schutte C., Zwijsen A., Knaus P. Role of bone morphogenetic proteins in sprouting angiogenesis: Differential bmp receptor-dependent signaling pathways balance stalk vs. Tip cell competence. FASEB J. 2017;31:4720–4733. doi: 10.1096/fj.201700193RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamashita H., Shimizu A., Kato M., Nishitoh H., Ichijo H., Hanyu A., Morita I., Kimura M., Makishima F., Miyazono K. Growth/differentiation factor-5 induces angiogenesis in vivo. Exp. Cell Res. 1997;235:218–226. doi: 10.1006/excr.1997.3664. [DOI] [PubMed] [Google Scholar]
- 19.Glienke J., Schmitt A.O., Pilarsky C., Hinzmann B., Weiss B., Rosenthal A., Thierauch K.H. Differential gene expression by endothelial cells in distinct angiogenic states. Eur. J. Biochem. 2000;267:2820–2830. doi: 10.1046/j.1432-1327.2000.01325.x. [DOI] [PubMed] [Google Scholar]
- 20.Moreno-Miralles I., Schisler J.C., Patterson C. New insights into bone morphogenetic protein signaling: Focus on angiogenesis. Curr. Opin. Hematol. 2009;16:195–201. doi: 10.1097/MOH.0b013e32832a07d6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Risau W. Mechanisms of angiogenesis. Nature. 1997;386:671–674. doi: 10.1038/386671a0. [DOI] [PubMed] [Google Scholar]
- 22.Phng L.K., Gerhardt H. Angiogenesis: A team effort coordinated by notch. Dev. Cell. 2009;16:196–208. doi: 10.1016/j.devcel.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 23.Kim M.C., Silberberg Y.R., Abeyaratne R., Kamm R.D., Asada H.H. Computational modeling of three-dimensional ecm-rigidity sensing to guide directed cell migration. Proc. Natl. Acad. Sci. USA. 2018;115:E390–E399. doi: 10.1073/pnas.1717230115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacquemet G., Stubb A., Saup R., Miihkinen M., Kremneva E., Hamidi H., Ivaska J. Filopodome mapping identifies p130cas as a mechanosensitive regulator of filopodia stability. Curr. Biol. CB. 2019;29:202–216.e207. doi: 10.1016/j.cub.2018.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Albuschies J., Vogel V. The role of filopodia in the recognition of nanotopographies. Sci. Rep. 2013;3:1658. doi: 10.1038/srep01658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gerhardt H., Golding M., Fruttiger M., Ruhrberg C., Lundkvist A., Abramsson A., Jeltsch M., Mitchell C., Alitalo K., Shima D., et al. Vegf guides angiogenic sprouting utilizing endothelial tip cell filopodia. J. Cell Biol. 2003;161:1163–1177. doi: 10.1083/jcb.200302047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Phng L.K., Stanchi F., Gerhardt H. Filopodia are dispensable for endothelial tip cell guidance. Development (Camb. Engl.) 2013;140:4031–4040. doi: 10.1242/dev.097352. [DOI] [PubMed] [Google Scholar]
- 28.Mouillesseaux K.P., Wiley D.S., Saunders L.M., Wylie L.A., Kushner E.J., Chong D.C., Citrin K.M., Barber A.T., Park Y., Kim J.D., et al. Notch regulates bmp responsiveness and lateral branching in vessel networks via smad6. Nat. Commun. 2016;7:13247. doi: 10.1038/ncomms13247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benn A., Bredow C., Casanova I., Vukičević S., Knaus P. Ve-cadherin facilitates bmp-induced endothelial cell permeability and signaling. J. Cell Sci. 2016;129:206–218. doi: 10.1242/jcs.179960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pi X., Ren R., Kelley R., Zhang C., Moser M., Bohil A.B., Divito M., Cheney R.E., Patterson C. Sequential roles for myosin-x in bmp6-dependent filopodial extension, migration, and activation of bmp receptors. J. Cell Biol. 2007;179:1569–1582. doi: 10.1083/jcb.200704010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ren R., Charles P.C., Zhang C., Wu Y., Wang H., Patterson C. Gene expression profiles identify a role for cyclooxygenase 2-dependent prostanoid generation in bmp6-induced angiogenic responses. Blood. 2007;109:2847–2853. doi: 10.1182/blood-2006-08-039743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Valdimarsdottir G., Goumans M.J., Rosendahl A., Brugman M., Itoh S., Lebrin F., Sideras P., ten Dijke P. Stimulation of id1 expression by bone morphogenetic protein is sufficient and necessary for bone morphogenetic protein-induced activation of endothelial cells. Circulation. 2002;106:2263–2270. doi: 10.1161/01.CIR.0000033830.36431.46. [DOI] [PubMed] [Google Scholar]
- 33.Heinke J., Wehofsits L., Zhou Q., Zoeller C., Baar K.M., Helbing T., Laib A., Augustin H., Bode C., Patterson C., et al. Bmper is an endothelial cell regulator and controls bone morphogenetic protein-4-dependent angiogenesis. Circ. Res. 2008;103:804–812. doi: 10.1161/CIRCRESAHA.108.178434. [DOI] [PubMed] [Google Scholar]
- 34.Gangopahyay A., Oran M., Bauer E.M., Wertz J.W., Comhair S.A., Erzurum S.C., Bauer P.M. Bone morphogenetic protein receptor ii is a novel mediator of endothelial nitric-oxide synthase activation. J. Biol. Chem. 2011;286:33134–33140. doi: 10.1074/jbc.M111.274100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rothhammer T., Bataille F., Spruss T., Eissner G., Bosserhoff A.K. Functional implication of bmp4 expression on angiogenesis in malignant melanoma. Oncogene. 2007;26:4158–4170. doi: 10.1038/sj.onc.1210182. [DOI] [PubMed] [Google Scholar]
- 36.Akiyama I., Yoshino O., Osuga Y., Shi J., Harada M., Koga K., Hirota Y., Hirata T., Fujii T., Saito S., et al. Bone morphogenetic protein 7 increased vascular endothelial growth factor (vegf)-a expression in human granulosa cells and vegf receptor expression in endothelial cells. Reprod. Sci. (Thousand OaksCalif.) 2014;21:477–482. doi: 10.1177/1933719113503411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen W.C., Chung C.H., Lu Y.C., Wu M.H., Chou P.H., Yen J.Y., Lai Y.W., Wang G.S., Liu S.C., Cheng J.K., et al. Bmp-2 induces angiogenesis by provoking integrin alpha6 expression in human endothelial progenitor cells. Biochem. Pharmacol. 2018;150:256–266. doi: 10.1016/j.bcp.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 38.Finkenzeller G., Hager S., Stark G.B. Effects of bone morphogenetic protein 2 on human umbilical vein endothelial cells. Microvasc. Res. 2012;84:81–85. doi: 10.1016/j.mvr.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 39.Langenfeld E.M., Langenfeld J. Bone morphogenetic protein-2 stimulates angiogenesis in developing tumors. Mol. Cancer Res. Mcr. 2004;2:141–149. [PubMed] [Google Scholar]
- 40.Raida M., Clement J.H., Leek R.D., Ameri K., Bicknell R., Niederwieser D., Harris A.L. Bone morphogenetic protein 2 (bmp-2) and induction of tumor angiogenesis. J. Cancer Res. Clin. Oncol. 2005;131:741–750. doi: 10.1007/s00432-005-0024-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suzuki Y., Ohga N., Morishita Y., Hida K., Miyazono K., Watabe T. Bmp-9 induces proliferation of multiple types of endothelial cells in vitro and in vivo. J. Cell Sci. 2010;123:1684–1692. doi: 10.1242/jcs.061556. [DOI] [PubMed] [Google Scholar]
- 42.Zhou Q., Heinke J., Vargas A., Winnik S., Krauss T., Bode C., Patterson C., Moser M. Erk signaling is a central regulator for bmp-4 dependent capillary sprouting. Cardiovasc. Res. 2007;76:390–399. doi: 10.1016/j.cardiores.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 43.Kane R., Godson C., O’Brien C. Chordin-like 1, a bone morphogenetic protein-4 antagonist, is upregulated by hypoxia in human retinal pericytes and plays a role in regulating angiogenesis. Mol. Vis. 2008;14:1138–1148. [PMC free article] [PubMed] [Google Scholar]
- 44.Tate C.M., Mc Entire J., Pallini R., Vakana E., Wyss L., Blosser W., Ricci-Vitiani L., D’Alessandris Q.G., Morgante L., Giannetti S., et al. A bmp7 variant inhibits tumor angiogenesis in vitro and in vivo through direct modulation of endothelial cell biology. PLoS ONE. 2015;10:e0125697. doi: 10.1371/journal.pone.0125697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Del Toro R., Prahst C., Mathivet T., Siegfried G., Kaminker J.S., Larrivee B., Breant C., Duarte A., Takakura N., Fukamizu A., et al. Identification and functional analysis of endothelial tip cell-enriched genes. Blood. 2010;116:4025–4033. doi: 10.1182/blood-2010-02-270819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bier E., De Robertis E.M. Embryo development. Bmp gradients: A paradigm for morphogen-mediated developmental patterning. Science. 2015;348:aaa5838. doi: 10.1126/science.aaa5838. [DOI] [PubMed] [Google Scholar]
- 47.Wakayama Y., Fukuhara S., Ando K., Matsuda M., Mochizuki N. Cdc42 mediates bmp-induced sprouting angiogenesis through fmnl3-driven assembly of endothelial filopodia in zebrafish. Dev. Cell. 2015;32:109–122. doi: 10.1016/j.devcel.2014.11.024. [DOI] [PubMed] [Google Scholar]
- 48.Benn A., Alonso F., Mangelschots J., Génot E., Lox M., Zwijsen A. Bmp-smad1/5 signaling regulates retinal vascular development. Biomolecules. 2020;10:488. doi: 10.3390/biom10030488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mallet C., Vittet D., Feige J.J., Bailly S. Tgfbeta1 induces vasculogenesis and inhibits angiogenic sprouting in an embryonic stem cell differentiation model: Respective contribution of alk1 and alk5. Stem Cells. 2006;24:2420–2427. doi: 10.1634/stemcells.2005-0494. [DOI] [PubMed] [Google Scholar]
- 50.Ito C., Akimoto T., Ioka T., Kobayashi T., Kusano E. Tgf-beta inhibits vascular sprouting through tgf-beta type i receptor in the mouse embryonic aorta. Tohoku J. Exp. Med. 2009;218:63–71. doi: 10.1620/tjem.218.63. [DOI] [PubMed] [Google Scholar]
- 51.Goumans M.J., Valdimarsdottir G., Itoh S., Rosendahl A., Sideras P., ten Dijke P. Balancing the activation state of the endothelium via two distinct tgf-beta type i receptors. EMBO J. 2002;21:1743–1753. doi: 10.1093/emboj/21.7.1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Seoane J., Gomis R.R. Tgf-beta family signaling in tumor suppression and cancer progression. Cold Spring Harb. Perspect. Biol. 2017;9 doi: 10.1101/cshperspect.a022277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Neal A., Nornes S., Payne S., Wallace M.D., Fritzsche M., Louphrasitthiphol P., Wilkinson R.N., Chouliaras K.M., Liu K., Plant K., et al. Venous identity requires bmp signalling through alk3. Nat. Commun. 2019;10:453. doi: 10.1038/s41467-019-08315-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.David L., Mallet C., Keramidas M., Lamande N., Gasc J.M., Dupuis-Girod S., Plauchu H., Feige J.J., Bailly S. Bone morphogenetic protein-9 is a circulating vascular quiescence factor. Circ. Res. 2008;102:914–922. doi: 10.1161/CIRCRESAHA.107.165530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rostama B., Turner J.E., Seavey G.T., Norton C.R., Gridley T., Vary C.P., Liaw L. Dll4/notch1 and bmp9 interdependent signaling induces human endothelial cell quiescence via p27kip1 and thrombospondin-1. Arterioscler. Thromb. Vasc. Biol. 2015;35:2626–2637. doi: 10.1161/ATVBAHA.115.306541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sengle G., Charbonneau N.L., Ono R.N., Sasaki T., Alvarez J., Keene D.R., Bächinger H.P., Sakai L.Y. Targeting of bone morphogenetic protein growth factor complexes to fibrillin. J. Biol. Chem. 2008;283:13874–13888. doi: 10.1074/jbc.M707820200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kienast Y., Jucknischke U., Scheiblich S., Thier M., de Wouters M., Haas A., Lehmann C., Brand V., Bernicke D., Honold K., et al. Rapid activation of bone morphogenic protein 9 by receptor-mediated displacement of pro-domains. J. Biol. Chem. 2016;291:3395–3410. doi: 10.1074/jbc.M115.680009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.David L., Mallet C., Mazerbourg S., Feige J.J., Bailly S. Identification of bmp9 and bmp10 as functional activators of the orphan activin receptor-like kinase 1 (alk1) in endothelial cells. Blood. 2007;109:1953–1961. doi: 10.1182/blood-2006-07-034124. [DOI] [PubMed] [Google Scholar]
- 59.Scharpfenecker M., van Dinther M., Liu Z., van Bezooijen R.L., Zhao Q., Pukac L., Lowik C.W., ten Dijke P. Bmp-9 signals via alk1 and inhibits bfgf-induced endothelial cell proliferation and vegf-stimulated angiogenesis. J. Cell Sci. 2007;120:964–972. doi: 10.1242/jcs.002949. [DOI] [PubMed] [Google Scholar]
- 60.Townson S.A., Martinez-Hackert E., Greppi C., Lowden P., Sako D., Liu J., Ucran J.A., Liharska K., Underwood K.W., Seehra J., et al. Specificity and structure of a high affinity activin receptor-like kinase 1 (alk1) signaling complex. J. Biol. Chem. 2012;287:27313–27325. doi: 10.1074/jbc.M112.377960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ostrowski M.A., Huang N.F., Walker T.W., Verwijlen T., Poplawski C., Khoo A.S., Cooke J.P., Fuller G.G., Dunn A.R. Microvascular endothelial cells migrate upstream and align against the shear stress field created by impinging flow. Biophys. J. 2014;106:366–374. doi: 10.1016/j.bpj.2013.11.4502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wang C., Baker B.M., Chen C.S., Schwartz M.A. Endothelial cell sensing of flow direction. Arterioscler. Thromb. Vasc. Biol. 2013;33:2130–2136. doi: 10.1161/ATVBAHA.113.301826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bicknell R. Endothelial Cell Culture. Roy Bicknell; Cambridge, UK: 1996. p. 152. [Google Scholar]
- 64.Luo J., Tang M., Huang J., He B.C., Gao J.L., Chen L., Zuo G.W., Zhang W., Luo Q., Shi Q., et al. Tgfbeta/bmp type i receptors alk1 and alk2 are essential for bmp9-induced osteogenic signaling in mesenchymal stem cells. J. Biol. Chem. 2010;285:29588–29598. doi: 10.1074/jbc.M110.130518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Laux D.W., Young S., Donovan J.P., Mansfield C.J., Upton P.D., Roman B.L. Circulating bmp10 acts through endothelial alk1 to mediate flow-dependent arterial quiescence. Development (Camb. Engl.) 2013;140:3403–3412. doi: 10.1242/dev.095307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Corti P., Young S., Chen C.Y., Patrick M.J., Rochon E.R., Pekkan K., Roman B.L. Interaction between alk1 and blood flow in the development of arteriovenous malformations. Development (Camb. Engl.) 2011;138:1573–1582. doi: 10.1242/dev.060467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Viallard C., Audiger C., Popovic N., Akla N., Lanthier K., Legault-Navarrete I., Melichar H., Costantino S., Lesage S., Larrivée B. Bmp9 signaling promotes the normalization of tumor blood vessels. Oncogene. 2020;39:2996–3014. doi: 10.1038/s41388-020-1200-0. [DOI] [PubMed] [Google Scholar]
- 68.Young K., Conley B., Romero D., Tweedie E., O’Neill C., Pinz I., Brogan L., Lindner V., Liaw L., Vary C.P. Bmp9 regulates endoglin-dependent chemokine responses in endothelial cells. Blood. 2012;120:4263–4273. doi: 10.1182/blood-2012-07-440784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Capasso T.L., Li B., Volek H.J., Khalid W., Rochon E.R., Anbalagan A., Herdman C., Yost H.J., Villanueva F.S., Kim K., et al. Bmp10-mediated alk1 signaling is continuously required for vascular development and maintenance. Angiogenesis. 2020;23:203–220. doi: 10.1007/s10456-019-09701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Richter A., Alexdottir M.S., Magnus S.H., Richter T.R., Morikawa M., Zwijsen A., Valdimarsdottir G. Egfl7 mediates bmp9-induced sprouting angiogenesis of endothelial cells derived from human embryonic stem cells. Stem Cell Rep. 2019;12:1250–1259. doi: 10.1016/j.stemcr.2019.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Varelas X., Sakuma R., Samavarchi-Tehrani P., Peerani R., Rao B.M., Dembowy J., Yaffe M.B., Zandstra P.W., Wrana J.L. Taz controls smad nucleocytoplasmic shuttling and regulates human embryonic stem-cell self-renewal. Nat. Cell Biol. 2008;10:837–848. doi: 10.1038/ncb1748. [DOI] [PubMed] [Google Scholar]
- 72.Hill C.S. Transcriptional control by the smads. Cold Spring Harb. Perspect. Biol. 2016;8 doi: 10.1101/cshperspect.a022079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Szeto S.G., Narimatsu M., Lu M., He X., Sidiqi A.M., Tolosa M.F., Chan L., De Freitas K., Bialik J.F., Majumder S., et al. Yap/taz are mechanoregulators of tgf-β-smad signaling and renal fibrogenesis. J. Am. Soc. Nephrol. JASN. 2016;27:3117–3128. doi: 10.1681/ASN.2015050499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Morikawa M., Koinuma D., Tsutsumi S., Vasilaki E., Kanki Y., Heldin C.H., Aburatani H., Miyazono K. Chip-seq reveals cell type-specific binding patterns of bmp-specific smads and a novel binding motif. Nucleic Acids Res. 2011;39:8712–8727. doi: 10.1093/nar/gkr572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Upton P.D., Davies R.J., Trembath R.C., Morrell N.W. Bone morphogenetic protein (bmp) and activin type ii receptors balance bmp9 signals mediated by activin receptor-like kinase-1 in human pulmonary artery endothelial cells. J. Biol. Chem. 2009;284:15794–15804. doi: 10.1074/jbc.M109.002881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ricard N., Ciais D., Levet S., Subileau M., Mallet C., Zimmers T.A., Lee S.J., Bidart M., Feige J.J., Bailly S. Bmp9 and bmp10 are critical for postnatal retinal vascular remodeling. Blood. 2012;119:6162–6171. doi: 10.1182/blood-2012-01-407593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lamouille S., Mallet C., Feige J.J., Bailly S. Activin receptor-like kinase 1 is implicated in the maturation phase of angiogenesis. Blood. 2002;100:4495–4501. doi: 10.1182/blood.V100.13.4495. [DOI] [PubMed] [Google Scholar]
- 78.Cheifetz S., Bellón T., Calés C., Vera S., Bernabeu C., Massagué J., Letarte M. Endoglin is a component of the transforming growth factor-beta receptor system in human endothelial cells. J. Biol. Chem. 1992;267:19027–19030. [PubMed] [Google Scholar]
- 79.Barbara N.P., Wrana J.L., Letarte M. Endoglin is an accessory protein that interacts with the signaling receptor complex of multiple members of the transforming growth factor-beta superfamily. J. Biol. Chem. 1999;274:584–594. doi: 10.1074/jbc.274.2.584. [DOI] [PubMed] [Google Scholar]
- 80.Castonguay R., Werner E.D., Matthews R.G., Presman E., Mulivor A.W., Solban N., Sako D., Pearsall R.S., Underwood K.W., Seehra J., et al. Soluble endoglin specifically binds bone morphogenetic proteins 9 and 10 via its orphan domain, inhibits blood vessel formation, and suppresses tumor growth. J. Biol. Chem. 2011;286:30034–30046. doi: 10.1074/jbc.M111.260133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Saito T., Bokhove M., Croci R., Zamora-Caballero S., Han L., Letarte M., de Sanctis D., Jovine L. Structural basis of the human endoglin-bmp9 interaction: Insights into bmp signaling and hht1. Cell Rep. 2017;19:1917–1928. doi: 10.1016/j.celrep.2017.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Blanco F.J., Santibanez J.F., Guerrero-Esteo M., Langa C., Vary C.P., Bernabeu C. Interaction and functional interplay between endoglin and alk-1, two components of the endothelial transforming growth factor-beta receptor complex. J. Cell. Physiol. 2005;204:574–584. doi: 10.1002/jcp.20311. [DOI] [PubMed] [Google Scholar]
- 83.Tian H., Huang J.J., Golzio C., Gao X., Hector-Greene M., Katsanis N., Blobe G.C. Endoglin interacts with vegfr2 to promote angiogenesis. FASEB J. 2018;32:2934–2949. doi: 10.1096/fj.201700867RR. [DOI] [PubMed] [Google Scholar]
- 84.Baeyens N., Larrivée B., Ola R., Hayward-Piatkowskyi B., Dubrac A., Huang B., Ross T.D., Coon B.G., Min E., Tsarfati M., et al. Defective fluid shear stress mechanotransduction mediates hereditary hemorrhagic telangiectasia. J. Cell Biol. 2016;214:807–816. doi: 10.1083/jcb.201603106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chaouat A., Coulet F., Favre C., Simonneau G., Weitzenblum E., Soubrier F., Humbert M. Endoglin germline mutation in a patient with hereditary haemorrhagic telangiectasia and dexfenfluramine associated pulmonary arterial hypertension. Thorax. 2004;59:446–448. doi: 10.1136/thx.2003.11890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Iyer K.V., Piscitello-Gómez R., Paijmans J., Jülicher F., Eaton S. Epithelial viscoelasticity is regulated by mechanosensitive e-cadherin turnover. Curr. Biol. CB. 2019;29:578–591. doi: 10.1016/j.cub.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 87.Yoshida A., Sakai N., Uekusa Y., Imaoka Y., Itagaki Y., Suzuki Y., Yoshimura S.H. Morphological changes of plasma membrane and protein assembly during clathrin-mediated endocytosis. PLoS Biol. 2018;16:e2004786. doi: 10.1371/journal.pbio.2004786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wu X.S., Elias S., Liu H., Heureaux J., Wen P.J., Liu A.P., Kozlov M.M., Wu L.G. Membrane tension inhibits rapid and slow endocytosis in secretory cells. Biophys. J. 2017;113:2406–2414. doi: 10.1016/j.bpj.2017.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ehrlich M. Endocytosis and trafficking of bmp receptors: Regulatory mechanisms for fine-tuning the signaling response in different cellular contexts. Cytokine Growth Factor Rev. 2016;27:35–42. doi: 10.1016/j.cytogfr.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 90.Zuo W., Chen Y.G. Specific activation of mitogen-activated protein kinase by transforming growth factor-beta receptors in lipid rafts is required for epithelial cell plasticity. Mol. Biol. Cell. 2009;20:1020–1029. doi: 10.1091/mbc.e08-09-0898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Di Guglielmo G.M., Le Roy C., Goodfellow A.F., Wrana J.L. Distinct endocytic pathways regulate tgf-beta receptor signalling and turnover. Nat. Cell Biol. 2003;5:410–421. doi: 10.1038/ncb975. [DOI] [PubMed] [Google Scholar]
- 92.Hayes S., Chawla A., Corvera S. Tgf beta receptor internalization into eea1-enriched early endosomes: Role in signaling to smad2. J. Cell Biol. 2002;158:1239–1249. doi: 10.1083/jcb.200204088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hartung A., Bitton-Worms K., Rechtman M.M., Wenzel V., Boergermann J.H., Hassel S., Henis Y.I., Knaus P. Different routes of bone morphogenic protein (bmp) receptor endocytosis influence bmp signaling. Mol. Cell. Biol. 2006;26:7791–7805. doi: 10.1128/MCB.00022-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bonor J., Adams E.L., Bragdon B., Moseychuk O., Czymmek K.J., Nohe A. Initiation of bmp2 signaling in domains on the plasma membrane. J. Cell. Physiol. 2012;227:2880–2888. doi: 10.1002/jcp.23032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Saldanha S., Bragdon B., Moseychuk O., Bonor J., Dhurjati P., Nohe A. Caveolae regulate smad signaling as verified by novel imaging and system biology approaches. J. Cell. Physiol. 2013;228:1060–1069. doi: 10.1002/jcp.24253. [DOI] [PubMed] [Google Scholar]
- 96.He Z., Zhang W., Mao S., Li N., Li H., Lin J.M. Shear stress-enhanced internalization of cell membrane proteins indicated by a hairpin-type DNA probe. Anal. Chem. 2018;90:5540–5545. doi: 10.1021/acs.analchem.8b00755. [DOI] [PubMed] [Google Scholar]
- 97.Urbano R.L., Furia C., Basehore S., Clyne A.M. Stiff substrates increase inflammation-induced endothelial monolayer tension and permeability. Biophys. J. 2017;113:645–655. doi: 10.1016/j.bpj.2017.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Albinsson S., Nordström I., Swärd K., Hellstrand P. Differential dependence of stretch and shear stress signaling on caveolin-1 in the vascular wall. Am. J. Physiol. Cell Physiol. 2008;294:C271–C279. doi: 10.1152/ajpcell.00297.2007. [DOI] [PubMed] [Google Scholar]
- 99.Santibanez J.F., Blanco F.J., Garrido-Martin E.M., Sanz-Rodriguez F., del Pozo M.A., Bernabeu C. Caveolin-1 interacts and cooperates with the transforming growth factor-beta type i receptor alk1 in endothelial caveolae. Cardiovasc. Res. 2008;77:791–799. doi: 10.1093/cvr/cvm097. [DOI] [PubMed] [Google Scholar]
- 100.Schwartz E.A., Reaven E., Topper J.N., Tsao P.S. Transforming growth factor-beta receptors localize to caveolae and regulate endothelial nitric oxide synthase in normal human endothelial cells. Biochem. J. 2005;390:199–206. doi: 10.1042/BJ20041182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nohe A., Keating E., Underhill T.M., Knaus P., Petersen N.O. Dynamics and interaction of caveolin-1 isoforms with bmp-receptors. J. Cell Sci. 2005;118:643–650. doi: 10.1242/jcs.01402. [DOI] [PubMed] [Google Scholar]
- 102.Mathew R. Pathogenesis of pulmonary hypertension: A case for caveolin-1 and cell membrane integrity. Am. J. Physiol. Heart Circ. Physiol. 2014;306:H15–H25. doi: 10.1152/ajpheart.00266.2013. [DOI] [PubMed] [Google Scholar]
- 103.Harrison R.E., Flanagan J.A., Sankelo M., Abdalla S.A., Rowell J., Machado R.D., Elliott C.G., Robbins I.M., Olschewski H., McLaughlin V., et al. Molecular and functional analysis identifies alk-1 as the predominant cause of pulmonary hypertension related to hereditary haemorrhagic telangiectasia. J. Med. Genet. 2003;40:865–871. doi: 10.1136/jmg.40.12.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sinha B., Köster D., Ruez R., Gonnord P., Bastiani M., Abankwa D., Stan R.V., Butler-Browne G., Vedie B., Johannes L., et al. Cells respond to mechanical stress by rapid disassembly of caveolae. Cell. 2011;144:402–413. doi: 10.1016/j.cell.2010.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Parton R.G., del Pozo M.A. Caveolae as plasma membrane sensors, protectors and organizers. Nat. Rev. Mol. Cell Biol. 2013;14:98–112. doi: 10.1038/nrm3512. [DOI] [PubMed] [Google Scholar]
- 106.Park H., Go Y.M., St John P.L., Maland M.C., Lisanti M.P., Abrahamson D.R., Jo H. Plasma membrane cholesterol is a key molecule in shear stress-dependent activation of extracellular signal-regulated kinase. J. Biol. Chem. 1998;273:32304–32311. doi: 10.1074/jbc.273.48.32304. [DOI] [PubMed] [Google Scholar]
- 107.Boyd N.L., Park H., Yi H., Boo Y.C., Sorescu G.P., Sykes M., Jo H. Chronic shear induces caveolae formation and alters erk and akt responses in endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 2003;285:H1113–H1122. doi: 10.1152/ajpheart.00302.2003. [DOI] [PubMed] [Google Scholar]
- 108.Sun X., Fu Y., Gu M., Zhang L., Li D., Li H., Chien S., Shyy J.Y., Zhu Y. Activation of integrin α5 mediated by flow requires its translocation to membrane lipid rafts in vascular endothelial cells. Proc. Natl. Acad. Sci. USA. 2016;113:769–774. doi: 10.1073/pnas.1524523113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Radel C., Rizzo V. Integrin mechanotransduction stimulates caveolin-1 phosphorylation and recruitment of csk to mediate actin reorganization. Am. J. Physiol. Heart Circ. Physiol. 2005;288:H936–H945. doi: 10.1152/ajpheart.00519.2004. [DOI] [PubMed] [Google Scholar]
- 110.Radel C., Carlile-Klusacek M., Rizzo V. Participation of caveolae in beta1 integrin-mediated mechanotransduction. Biochem. Biophys. Res. Commun. 2007;358:626–631. doi: 10.1016/j.bbrc.2007.04.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shi F., Sottile J. Caveolin-1-dependent beta1 integrin endocytosis is a critical regulator of fibronectin turnover. J. Cell Sci. 2008;121:2360–2371. doi: 10.1242/jcs.014977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhou J., Lee P.L., Lee C.I., Wei S.Y., Lim S.H., Lin T.E., Chien S., Chiu J.J. Bmp receptor-integrin interaction mediates responses of vascular endothelial smad1/5 and proliferation to disturbed flow. J. Thromb. Haemost. JTH. 2013;11:741–755. doi: 10.1111/jth.12159. [DOI] [PubMed] [Google Scholar]
- 113.Isshiki M., Ando J., Yamamoto K., Fujita T., Ying Y., Anderson R.G. Sites of ca(2+) wave initiation move with caveolae to the trailing edge of migrating cells. J. Cell Sci. 2002;115:475–484. doi: 10.1242/jcs.115.3.475. [DOI] [PubMed] [Google Scholar]
- 114.Basagiannis D., Zografou S., Murphy C., Fotsis T., Morbidelli L., Ziche M., Bleck C., Mercer J., Christoforidis S. Vegf induces signalling and angiogenesis by directing vegfr2 internalisation through macropinocytosis. J. Cell Sci. 2016;129:4091–4104. doi: 10.1242/dev.146456. [DOI] [PubMed] [Google Scholar]
- 115.Munger J.S., Sheppard D. Cross talk among tgf-β signaling pathways, integrins, and the extracellular matrix. Cold Spring Harb. Perspect. Biol. 2011;3:a005017. doi: 10.1101/cshperspect.a005017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Luo B.H., Carman C.V., Springer T.A. Structural basis of integrin regulation and signaling. Annu. Rev. Immunol. 2007;25:619–647. doi: 10.1146/annurev.immunol.25.022106.141618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhou J., Lee P.L., Tsai C.S., Lee C.I., Yang T.L., Chuang H.S., Lin W.W., Lin T.E., Lim S.H., Wei S.Y., et al. Force-specific activation of smad1/5 regulates vascular endothelial cell cycle progression in response to disturbed flow. Proc. Natl. Acad. Sci. USA. 2012;109:7770–7775. doi: 10.1073/pnas.1205476109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Jin Z.G., Ueba H., Tanimoto T., Lungu A.O., Frame M.D., Berk B.C. Ligand-independent activation of vascular endothelial growth factor receptor 2 by fluid shear stress regulates activation of endothelial nitric oxide synthase. Circ. Res. 2003;93:354–363. doi: 10.1161/01.RES.0000089257.94002.96. [DOI] [PubMed] [Google Scholar]
- 119.Peacock H.M., Tabibian A., Criem N., Caolo V., Hamard L., Deryckere A., Haefliger J.A., Kwak B.R., Zwijsen A., Jones E.A.V. Impaired smad1/5 mechanotransduction and cx37 (connexin37) expression enable pathological vessel enlargement and shunting. Arterioscler. Thromb. Vasc. Biol. 2020;40:e87–e104. doi: 10.1161/ATVBAHA.119.313122. [DOI] [PubMed] [Google Scholar]
- 120.Santos-Oliveira P., Correia A., Rodrigues T., Ribeiro-Rodrigues T.M., Matafome P., Rodríguez-Manzaneque J.C., Seiça R., Girão H., Travasso R.D. The force at the tip--modelling tension and proliferation in sprouting angiogenesis. PLoS Comput. Biol. 2015;11:e1004436. doi: 10.1371/journal.pcbi.1004436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Bibi H., Armoni M., Ohali M., Pollak S. tuberculosis in early childhood. Harefuah. 1996;131:166–215. (In Hebrew) [PubMed] [Google Scholar]
- 122.Fantin A., Lampropoulou A., Gestri G., Raimondi C., Senatore V., Zachary I., Ruhrberg C. Nrp1 regulates cdc42 activation to promote filopodia formation in endothelial tip cells. Cell Rep. 2015;11:1577–1590. doi: 10.1016/j.celrep.2015.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Gerhardt H., Ruhrberg C., Abramsson A., Fujisawa H., Shima D., Betsholtz C. Neuropilin-1 is required for endothelial tip cell guidance in the developing central nervous system. Dev. Dyn. 2004;231:503–509. doi: 10.1002/dvdy.20148. [DOI] [PubMed] [Google Scholar]
- 124.Lee-Hoeflich S.T., Causing C.G., Podkowa M., Zhao X., Wrana J.L., Attisano L. Activation of limk1 by binding to the bmp receptor, bmprii, regulates bmp-dependent dendritogenesis. EMBO J. 2004;23:4792–4801. doi: 10.1038/sj.emboj.7600418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hiepen C., Benn A., Denkis A., Lukonin I., Weise C., Boergermann J.H., Knaus P. Bmp2-induced chemotaxis requires pi3k p55γ/p110α-dependent phosphatidylinositol (3,4,5)-triphosphate production and ll5β recruitment at the cytocortex. BMC Biol. 2014;12:43. doi: 10.1186/1741-7007-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Sieminski A.L., Hebbel R.P., Gooch K.J. The relative magnitudes of endothelial force generation and matrix stiffness modulate capillary morphogenesis in vitro. Exp. Cell Res. 2004;297:574–584. doi: 10.1016/j.yexcr.2004.03.035. [DOI] [PubMed] [Google Scholar]
- 127.Mason B.N., Starchenko A., Williams R.M., Bonassar L.J., Reinhart-King C.A. Tuning three-dimensional collagen matrix stiffness independently of collagen concentration modulates endothelial cell behavior. Acta Biomater. 2013;9:4635–4644. doi: 10.1016/j.actbio.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bordeleau F., Mason B.N., Lollis E.M., Mazzola M., Zanotelli M.R., Somasegar S., Califano J.P., Montague C., LaValley D.J., Huynh J., et al. Matrix stiffening promotes a tumor vasculature phenotype. Proc. Natl. Acad. Sci. USA. 2017;114:492–497. doi: 10.1073/pnas.1613855114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wong L., Kumar A., Gabela-Zuniga B., Chua J., Singh G., Happe C.L., Engler A.J., Fan Y., McCloskey K.E. Substrate stiffness directs diverging vascular fates. Acta Biomater. 2019;96:321–329. doi: 10.1016/j.actbio.2019.07.030. [DOI] [PubMed] [Google Scholar]
- 130.Xue C., Zhang T., Xie X., Zhang Q., Zhang S., Zhu B., Lin Y., Cai X. Substrate stiffness regulates arterial-venous differentiation of endothelial progenitor cells via the ras/mek pathway. Biochim. Biophys. Acta. Mol. Cell Res. 2017;1864:1799–1808. doi: 10.1016/j.bbamcr.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 131.Frye M., Taddei A., Dierkes C., Martinez-Corral I., Fielden M., Ortsäter H., Kazenwadel J., Calado D.P., Ostergaard P., Salminen M., et al. Matrix stiffness controls lymphatic vessel formation through regulation of a gata2-dependent transcriptional program. Nat. Commun. 2018;9:1511. doi: 10.1038/s41467-018-03959-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kniazeva E., Putnam A.J. Endothelial cell traction and ecm density influence both capillary morphogenesis and maintenance in 3-d. Am. J. Physiol. Cell Physiol. 2009;297:C179–C187. doi: 10.1152/ajpcell.00018.2009. [DOI] [PubMed] [Google Scholar]
- 133.Bae Y.H., Liu S.L., Byfield F.J., Janmey P.A., Assoian R.K. Measuring the stiffness of ex vivo mouse aortas using atomic force microscopy. J. Vis. Exp. Jove. 2016;116 doi: 10.3791/54630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Spronck B., Humphrey J. Arterial stiffness: Different metrics, different meanings. J. Biomech. Eng. 2019;141:0910041–09100412. doi: 10.1115/1.4043486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Woodrum D.A., Romano A.J., Lerman A., Pandya U.H., Brosh D., Rossman P.J., Lerman L.O., Ehman R.L. Vascular wall elasticity measurement by magnetic resonance imaging. Magn. Reson. Med. 2006;56:593–600. doi: 10.1002/mrm.20991. [DOI] [PubMed] [Google Scholar]
- 136.Bastounis E.E., Yeh Y.T., Theriot J.A. Subendothelial stiffness alters endothelial cell traction force generation while exerting a minimal effect on the transcriptome. Sci. Rep. 2019;9:18209. doi: 10.1038/s41598-019-54336-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Peloquin J., Huynh J., Williams R.M., Reinhart-King C.A. Indentation measurements of the subendothelial matrix in bovine carotid arteries. J. Biomech. 2011;44:815–821. doi: 10.1016/j.jbiomech.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 138.Huynh J., Nishimura N., Rana K., Peloquin J.M., Califano J.P., Montague C.R., King M.R., Schaffer C.B., Reinhart-King C.A. Age-related intimal stiffening enhances endothelial permeability and leukocyte transmigration. Sci. Transl. Med. 2011;3:112ra122. doi: 10.1126/scitranslmed.3002761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.De Beaufort H.W.L., Ferrara A., Conti M., Moll F.L., van Herwaarden J.A., Figueroa C.A., Bismuth J., Auricchio F., Trimarchi S. Comparative analysis of porcine and human thoracic aortic stiffness. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2018;55:560–566. doi: 10.1016/j.ejvs.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 140.Kothapalli D., Liu S.L., Bae Y.H., Monslow J., Xu T., Hawthorne E.A., Byfield F.J., Castagnino P., Rao S., Rader D.J., et al. Cardiovascular protection by apoe and apoe-hdl linked to suppression of ecm gene expression and arterial stiffening. Cell Rep. 2012;2:1259–1271. doi: 10.1016/j.celrep.2012.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Teng Z., Zhang Y., Huang Y., Feng J., Yuan J., Lu Q., Sutcliffe M.P.F., Brown A.J., Jing Z., Gillard J.H. Material properties of components in human carotid atherosclerotic plaques: A uniaxial extension study. Acta Biomater. 2014;10:5055–5063. doi: 10.1016/j.actbio.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhong A., Mirzaei Z., Simmons C.A. The roles of matrix stiffness and ß-catenin signaling in endothelial-to-mesenchymal transition of aortic valve endothelial cells. Cardiovasc. Eng. Technol. 2018;9:158–167. doi: 10.1007/s13239-018-0363-0. [DOI] [PubMed] [Google Scholar]
- 143.Chen J.H., Chen W.L., Sider K.L., Yip C.Y., Simmons C.A. Β-catenin mediates mechanically regulated, transforming growth factor-β1-induced myofibroblast differentiation of aortic valve interstitial cells. Arterioscler. Thromb. Vasc. Biol. 2011;31:590–597. doi: 10.1161/ATVBAHA.110.220061. [DOI] [PubMed] [Google Scholar]
- 144.Zhang H., Chang H., Wang L.M., Ren K.F., Martins M.C., Barbosa M.A., Ji J. Effect of polyelectrolyte film stiffness on endothelial cells during endothelial-to-mesenchymal transition. Biomacromolecules. 2015;16:3584–3593. doi: 10.1021/acs.biomac.5b01057. [DOI] [PubMed] [Google Scholar]
- 145.Dalfino G., Simone S., Porreca S., Cosola C., Balestra C., Manno C., Schena F.P., Grandaliano G., Pertosa G. Bone morphogenetic protein-2 may represent the molecular link between oxidative stress and vascular stiffness in chronic kidney disease. Atherosclerosis. 2010;211:418–423. doi: 10.1016/j.atherosclerosis.2010.04.023. [DOI] [PubMed] [Google Scholar]
- 146.Vaeyens M.M., Jorge-Peñas A., Barrasa-Fano J., Steuwe C., Heck T., Carmeliet P., Roeffaers M., Van Oosterwyck H. Matrix deformations around angiogenic sprouts correlate to sprout dynamics and suggest pulling activity. Angiogenesis. 2020;23:315–324. doi: 10.1007/s10456-020-09708-y. [DOI] [PubMed] [Google Scholar]
- 147.LaValley D.J., Zanotelli M.R., Bordeleau F., Wang W., Schwager S.C., Reinhart-King C.A. Matrix stiffness enhances vegfr-2 internalization, signaling, and proliferation in endothelial cells. Converg. Sci. Phys. Oncol. 2017;3:044001. doi: 10.1088/2057-1739/aa9263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Rys J.P., DuFort C.C., Monteiro D.A., Baird M.A., Oses-Prieto J.A., Chand S., Burlingame A.L., Davidson M.W., Alliston T.N. Discrete spatial organization of tgfβ receptors couples receptor multimerization and signaling to cellular tension. eLife. 2015;4:e09300. doi: 10.7554/eLife.09300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yadin D., Knaus P., Mueller T.D. Structural insights into bmp receptors: Specificity, activation and inhibition. Cytokine Growth Factor Rev. 2016;27:13–34. doi: 10.1016/j.cytogfr.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 150.Hinz B. The extracellular matrix and transforming growth factor-β1: Tale of a strained relationship. Matrix Biol. J. Int. Soc. Matrix Biol. 2015;47:54–65. doi: 10.1016/j.matbio.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 151.Isogai Z., Ono R.N., Ushiro S., Keene D.R., Chen Y., Mazzieri R., Charbonneau N.L., Reinhardt D.P., Rifkin D.B., Sakai L.Y. Latent transforming growth factor beta-binding protein 1 interacts with fibrillin and is a microfibril-associated protein. J. Biol. Chem. 2003;278:2750–2757. doi: 10.1074/jbc.M209256200. [DOI] [PubMed] [Google Scholar]
- 152.Chaudhry S.S., Cain S.A., Morgan A., Dallas S.L., Shuttleworth C.A., Kielty C.M. Fibrillin-1 regulates the bioavailability of tgfbeta1. J. Cell Biol. 2007;176:355–367. doi: 10.1083/jcb.200608167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Saharinen J., Taipale J., Keski-Oja J. Association of the small latent transforming growth factor-beta with an eight cysteine repeat of its binding protein ltbp-1. EMBO J. 1996;15:245–253. doi: 10.1002/j.1460-2075.1996.tb00355.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Saharinen J., Keski-Oja J. Specific sequence motif of 8-cys repeats of tgf-beta binding proteins, ltbps, creates a hydrophobic interaction surface for binding of small latent tgf-beta. Mol. Biol. Cell. 2000;11:2691–2704. doi: 10.1091/mbc.11.8.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Hirani R., Hanssen E., Gibson M.A. Ltbp-2 specifically interacts with the amino-terminal region of fibrillin-1 and competes with ltbp-1 for binding to this microfibrillar protein. Matrix Biol. J. Int. Soc. Matrix Biol. 2007;26:213–223. doi: 10.1016/j.matbio.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 156.Sheppard D. Integrin-mediated activation of latent transforming growth factor beta. Cancer Metastasis Rev. 2005;24:395–402. doi: 10.1007/s10555-005-5131-6. [DOI] [PubMed] [Google Scholar]
- 157.Yang Z., Mu Z., Dabovic B., Jurukovski V., Yu D., Sung J., Xiong X., Munger J.S. Absence of integrin-mediated tgfbeta1 activation in vivo recapitulates the phenotype of tgfbeta1-null mice. J. Cell Biol. 2007;176:787–793. doi: 10.1083/jcb.200611044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Klingberg F., Chow M.L., Koehler A., Boo S., Buscemi L., Quinn T.M., Costell M., Alman B.A., Genot E., Hinz B. Prestress in the extracellular matrix sensitizes latent tgf-β1 for activation. J. Cell Biol. 2014;207:283–297. doi: 10.1083/jcb.201402006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Dong X., Zhao B., Iacob R.E., Zhu J., Koksal A.C., Lu C., Engen J.R., Springer T.A. Force interacts with macromolecular structure in activation of tgf-β. Nature. 2017;542:55–59. doi: 10.1038/nature21035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Buscemi L., Ramonet D., Klingberg F., Formey A., Smith-Clerc J., Meister J.J., Hinz B. The single-molecule mechanics of the latent tgf-β1 complex. Curr. Biol. CB. 2011;21:2046–2054. doi: 10.1016/j.cub.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 161.Shi M., Zhu J., Wang R., Chen X., Mi L., Walz T., Springer T.A. Latent tgf-β structure and activation. Nature. 2011;474:343–349. doi: 10.1038/nature10152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Qin Y., Garrison B.S., Ma W., Wang R., Jiang A., Li J., Mistry M., Bronson R.T., Santoro D., Franco C., et al. A milieu molecule for tgf-β required for microglia function in the nervous system. Cell. 2018;174:156–171.e116. doi: 10.1016/j.cell.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Roca-Cusachs P., Iskratsch T., Sheetz M.P. Finding the weakest link: Exploring integrin-mediated mechanical molecular pathways. J. Cell Sci. 2012;125:3025–3038. doi: 10.1242/jcs.095794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.De Laporte L., Rice J.J., Tortelli F., Hubbell J.A. Tenascin c promiscuously binds growth factors via its fifth fibronectin type iii-like domain. PLoS ONE. 2013;8:e62076. doi: 10.1371/journal.pone.0062076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ruppert R., Hoffmann E., Sebald W. Human bone morphogenetic protein 2 contains a heparin-binding site which modifies its biological activity. Eur. J. Biochem. 1996;237:295–302. doi: 10.1111/j.1432-1033.1996.0295n.x. [DOI] [PubMed] [Google Scholar]
- 166.Ishihara J., Ishihara A., Fukunaga K., Sasaki K., White M.J.V., Briquez P.S., Hubbell J.A. Laminin heparin-binding peptides bind to several growth factors and enhance diabetic wound healing. Nat. Commun. 2018;9:2163. doi: 10.1038/s41467-018-04525-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Von Offenberg Sweeney N., Cummins P.M., Birney Y.A., Cullen J.P., Redmond E.M., Cahill P.A. Cyclic strain-mediated regulation of endothelial matrix metalloproteinase-2 expression and activity. Cardiovasc. Res. 2004;63:625–634. doi: 10.1016/j.cardiores.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 168.Wang B.W., Chang H., Lin S., Kuan P., Shyu K.G. Induction of matrix metalloproteinases-14 and -2 by cyclical mechanical stretch is mediated by tumor necrosis factor-alpha in cultured human umbilical vein endothelial cells. Cardiovasc. Res. 2003;59:460–469. doi: 10.1016/S0008-6363(03)00428-0. [DOI] [PubMed] [Google Scholar]
- 169.Von Offenberg Sweeney N., Cummins P.M., Cotter E.J., Fitzpatrick P.A., Birney Y.A., Redmond E.M., Cahill P.A. Cyclic strain-mediated regulation of vascular endothelial cell migration and tube formation. Biochem. Biophys. Res. Commun. 2005;329:573–582. doi: 10.1016/j.bbrc.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 170.Enenstein J., Waleh N.S., Kramer R.H. Basic fgf and tgf-beta differentially modulate integrin expression of human microvascular endothelial cells. Exp. Cell Res. 1992;203:499–503. doi: 10.1016/0014-4827(92)90028-7. [DOI] [PubMed] [Google Scholar]
- 171.Pepper M.S. Transforming growth factor-beta: Vasculogenesis, angiogenesis, and vessel wall integrity. Cytokine Growth Factor Rev. 1997;8:21–43. doi: 10.1016/S1359-6101(96)00048-2. [DOI] [PubMed] [Google Scholar]
- 172.Baranska P., Jerczynska H., Pawlowska Z., Koziolkiewicz W., Cierniewski C.S. Expression of integrins and adhesive properties of human endothelial cell line ea.Hy 926. Cancer Genom. Proteom. 2005;2:265–269. [PubMed] [Google Scholar]
- 173.Hiepen C., Jatzlau J., Hildebrandt S., Kampfrath B., Goktas M., Murgai A., Cuellar Camacho J.L., Haag R., Ruppert C., Sengle G., et al. Bmpr2 acts as a gatekeeper to protect endothelial cells from increased tgfβ responses and altered cell mechanics. PLoS Biol. 2019;17:e3000557. doi: 10.1371/journal.pbio.3000557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Tian H., Mythreye K., Golzio C., Katsanis N., Blobe G.C. Endoglin mediates fibronectin/α5β1 integrin and tgf-β pathway crosstalk in endothelial cells. EMBO J. 2012;31:3885–3900. doi: 10.1038/emboj.2012.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Young K., Tweedie E., Conley B., Ames J., FitzSimons M., Brooks P., Liaw L., Vary C.P. Bmp9 crosstalk with the hippo pathway regulates endothelial cell matricellular and chemokine responses. PLoS ONE. 2015;10:e0122892. doi: 10.1371/journal.pone.0122892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ahamed J., Burg N., Yoshinaga K., Janczak C.A., Rifkin D.B., Coller B.S. In vitro and in vivo evidence for shear-induced activation of latent transforming growth factor-beta1. Blood. 2008;112:3650–3660. doi: 10.1182/blood-2008-04-151753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Baker A.B., Ettenson D.S., Jonas M., Nugent M.A., Iozzo R.V., Edelman E.R. Endothelial cells provide feedback control for vascular remodeling through a mechanosensitive autocrine tgf-beta signaling pathway. Circ. Res. 2008;103:289–297. doi: 10.1161/CIRCRESAHA.108.179465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Kouzbari K., Hossan M.R., Arrizabalaga J.H., Varshney R., Simmons A.D., Gostynska S., Nollert M.U., Ahamed J. Oscillatory shear potentiates latent tgf-β1 activation more than steady shear as demonstrated by a novel force generator. Sci. Rep. 2019;9:6065. doi: 10.1038/s41598-019-42302-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kokudo T., Suzuki Y., Yoshimatsu Y., Yamazaki T., Watabe T., Miyazono K. Snail is required for tgfbeta-induced endothelial-mesenchymal transition of embryonic stem cell-derived endothelial cells. J. Cell Sci. 2008;121:3317–3324. doi: 10.1242/jcs.028282. [DOI] [PubMed] [Google Scholar]
- 180.Medici D., Potenta S., Kalluri R. Transforming growth factor-β2 promotes snail-mediated endothelial-mesenchymal transition through convergence of smad-dependent and smad-independent signalling. Biochem. J. 2011;437:515–520. doi: 10.1042/BJ20101500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sánchez-Duffhues G., García de Vinuesa A., Ten Dijke P. Endothelial-to-mesenchymal transition in cardiovascular diseases: Developmental signaling pathways gone awry. Dev. Dyn. 2018;247:492–508. doi: 10.1002/dvdy.24589. [DOI] [PubMed] [Google Scholar]
- 182.Maruthamuthu V., Sabass B., Schwarz U.S., Gardel M.L. Cell-ecm traction force modulates endogenous tension at cell-cell contacts. Proc. Natl. Acad. Sci. USA. 2011;108:4708–4713. doi: 10.1073/pnas.1011123108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lampugnani M.G. Endothelial cell-to-cell junctions: Adhesion and signaling in physiology and pathology. Cold Spring Harb. Perspect. Med. 2012;2 doi: 10.1101/cshperspect.a006528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Rüffer C., Strey A., Janning A., Kim K.S., Gerke V. Cell-cell junctions of dermal microvascular endothelial cells contain tight and adherens junction proteins in spatial proximity. Biochemistry. 2004;43:5360–5369. doi: 10.1021/bi035517c. [DOI] [PubMed] [Google Scholar]
- 185.Beaulieu Leclerc V., Roy O., Santerre K., Proulx S. Tgf-β1 promotes cell barrier function upon maturation of corneal endothelial cells. Sci. Rep. 2018;8:4438. doi: 10.1038/s41598-018-22821-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Dohgu S., Yamauchi A., Takata F., Naito M., Tsuruo T., Higuchi S., Sawada Y., Kataoka Y. Transforming growth factor-beta1 upregulates the tight junction and p-glycoprotein of brain microvascular endothelial cells. Cell. Mol. Neurobiol. 2004;24:491–497. doi: 10.1023/B:CEMN.0000022776.47302.ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Walshe T.E., Saint-Geniez M., Maharaj A.S., Sekiyama E., Maldonado A.E., D’Amore P.A. Tgf-beta is required for vascular barrier function, endothelial survival and homeostasis of the adult microvasculature. PLoS ONE. 2009;4:e5149. doi: 10.1371/journal.pone.0005149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Gkatzis K., Thalgott J., Dos-Santos-Luis D., Martin S., Lamandé N., Carette M.F., Disch F., Snijder R.J., Westermann C.J., Mager J.J., et al. Interaction between alk1 signaling and connexin40 in the development of arteriovenous malformations. Arterioscler. Thromb. Vasc. Biol. 2016;36:707–717. doi: 10.1161/ATVBAHA.115.306719. [DOI] [PubMed] [Google Scholar]
- 189.Seebach J., Dieterich P., Luo F., Schillers H., Vestweber D., Oberleithner H., Galla H.J., Schnittler H.J. Endothelial barrier function under laminar fluid shear stress. Lab. Investig. A J. Tech. Methods Pathol. 2000;80:1819–1831. doi: 10.1038/labinvest.3780193. [DOI] [PubMed] [Google Scholar]
- 190.Helbing T., Arnold L., Wiltgen G., Hirschbihl E., Gabelmann V., Hornstein A., Esser J.S., Diehl P., Grundmann S., Busch H.J., et al. Endothelial bmp4 regulates leukocyte diapedesis and promotes inflammation. Inflammation. 2017;40:1862–1874. doi: 10.1007/s10753-017-0627-0. [DOI] [PubMed] [Google Scholar]
- 191.Hussein K.A., Choksi K., Akeel S., Ahmad S., Megyerdi S., El-Sherbiny M., Nawaz M., Abu El-Asrar A., Al-Shabrawey M. Bone morphogenetic protein 2: A potential new player in the pathogenesis of diabetic retinopathy. Exp. Eye Res. 2014;125:79–88. doi: 10.1016/j.exer.2014.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Helbing T., Wiltgen G., Hornstein A., Brauers E.Z., Arnold L., Bauer A., Esser J.S., Diehl P., Grundmann S., Fink K., et al. Bone morphogenetic protein-modulator bmper regulates endothelial barrier function. Inflammation. 2017;40:442–453. doi: 10.1007/s10753-016-0490-4. [DOI] [PubMed] [Google Scholar]
- 193.Li W., Long L., Yang X., Tong Z., Southwood M., Caruso P., Upton P.D., Yang P., Bocobo G.A., Nikolic I., et al. Circulating bmp9 protects the pulmonary endothelium during inflammation-induced lung injury in mice. bioRxiv. 2020 doi: 10.1101/2020.05.12.088880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Akla N., Viallard C., Popovic N., Lora Gil C., Sapieha P., Larrivée B. Bmp9 (bone morphogenetic protein-9)/alk1 (activin-like kinase receptor type i) signaling prevents hyperglycemia-induced vascular permeability. Arterioscler. Thromb. Vasc. Biol. 2018;38:1821–1836. doi: 10.1161/ATVBAHA.118.310733. [DOI] [PubMed] [Google Scholar]
- 195.Abu Taha A., Taha M., Seebach J., Schnittler H.J. Arp2/3-mediated junction-associated lamellipodia control ve-cadherin-based cell junction dynamics and maintain monolayer integrity. Mol. Biol. Cell. 2014;25:245–256. doi: 10.1091/mbc.e13-07-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Cao J., Ehling M., März S., Seebach J., Tarbashevich K., Sixta T., Pitulescu M.E., Werner A.C., Flach B., Montanez E., et al. Polarized actin and ve-cadherin dynamics regulate junctional remodelling and cell migration during sprouting angiogenesis. Nat. Commun. 2017;8:2210. doi: 10.1038/s41467-017-02373-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Cao J., Schnittler H. Putting ve-cadherin into jail for junction remodeling. J. Cell Sci. 2019;132 doi: 10.1242/jcs.222893. [DOI] [PubMed] [Google Scholar]
- 198.Tzima E., Irani-Tehrani M., Kiosses W.B., Dejana E., Schultz D.A., Engelhardt B., Cao G., DeLisser H., Schwartz M.A. A mechanosensory complex that mediates the endothelial cell response to fluid shear stress. Nature. 2005;437:426–431. doi: 10.1038/nature03952. [DOI] [PubMed] [Google Scholar]
- 199.Coon B.G., Baeyens N., Han J., Budatha M., Ross T.D., Fang J.S., Yun S., Thomas J.L., Schwartz M.A. Intramembrane binding of ve-cadherin to vegfr2 and vegfr3 assembles the endothelial mechanosensory complex. J. Cell Biol. 2015;208:975–986. doi: 10.1083/jcb.201408103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Rudini N., Felici A., Giampietro C., Lampugnani M., Corada M., Swirsding K., Garrè M., Liebner S., Letarte M., ten Dijke P., et al. Ve-cadherin is a critical endothelial regulator of tgf-beta signalling. EMBO J. 2008;27:993–1004. doi: 10.1038/emboj.2008.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hirate Y., Sasaki H. The role of angiomotin phosphorylation in the hippo pathway during preimplantation mouse development. Tissue Barriers. 2014;2:e28127. doi: 10.4161/tisb.28127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zhao B., Li L., Lu Q., Wang L.H., Liu C.Y., Lei Q., Guan K.L. Angiomotin is a novel hippo pathway component that inhibits yap oncoprotein. Genes Dev. 2011;25:51–63. doi: 10.1101/gad.2000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Giampietro C., Disanza A., Bravi L., Barrios-Rodiles M., Corada M., Frittoli E., Savorani C., Lampugnani M.G., Boggetti B., Niessen C., et al. The actin-binding protein eps8 binds ve-cadherin and modulates yap localization and signaling. J. Cell Biol. 2015;211:1177–1192. doi: 10.1083/jcb.201501089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Neto F., Klaus-Bergmann A., Ong Y.T., Alt S., Vion A.C., Szymborska A., Carvalho J.R., Hollfinger I., Bartels-Klein E., Franco C.A., et al. Yap and taz regulate adherens junction dynamics and endothelial cell distribution during vascular development. eLife. 2018;7 doi: 10.7554/eLife.31037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Zhou J., Li Y.S., Chien S. Shear stress-initiated signaling and its regulation of endothelial function. Arterioscler. Thromb. Vasc. Biol. 2014;34:2191–2198. doi: 10.1161/ATVBAHA.114.303422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Davies P.F. Hemodynamic shear stress and the endothelium in cardiovascular pathophysiology. Nat. Clin. Pract. Cardiovasc. Med. 2009;6:16–26. doi: 10.1038/ncpcardio1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Young Y.N., Downs M., Jacobs C.R. Dynamics of the primary cilium in shear flow. Biophys. J. 2012;103:629–639. doi: 10.1016/j.bpj.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Goetz J.G., Steed E., Ferreira R.R., Roth S., Ramspacher C., Boselli F., Charvin G., Liebling M., Wyart C., Schwab Y., et al. Endothelial cilia mediate low flow sensing during zebrafish vascular development. Cell Rep. 2014;6:799–808. doi: 10.1016/j.celrep.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 209.Schwartz E.A., Leonard M.L., Bizios R., Bowser S.S. Analysis and modeling of the primary cilium bending response to fluid shear. Am. J. Physiol. 1997;272:F132–F138. doi: 10.1152/ajprenal.1997.272.1.F132. [DOI] [PubMed] [Google Scholar]
- 210.Hoey D.A., Downs M.E., Jacobs C.R. The mechanics of the primary cilium: An intricate structure with complex function. J. Biomech. 2012;45:17–26. doi: 10.1016/j.jbiomech.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Masyuk A.I., Gradilone S.A., LaRusso N.F. Calcium signaling in cilia and ciliary-mediated intracellular calcium signaling: Are they independent or coordinated molecular events? Hepatology (Baltim. Md.) 2014;60:1783–1785. doi: 10.1002/hep.27331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Hartmannsgruber V., Heyken W.T., Kacik M., Kaistha A., Grgic I., Harteneck C., Liedtke W., Hoyer J., Köhler R. Arterial response to shear stress critically depends on endothelial trpv4 expression. PLoS ONE. 2007;2:e827. doi: 10.1371/journal.pone.0000827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Corrigan M.A., Johnson G.P., Stavenschi E., Riffault M., Labour M.N., Hoey D.A. Trpv4-mediates oscillatory fluid shear mechanotransduction in mesenchymal stem cells in part via the primary cilium. Sci. Rep. 2018;8:3824. doi: 10.1038/s41598-018-22174-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Adapala R.K., Thoppil R.J., Luther D.J., Paruchuri S., Meszaros J.G., Chilian W.M., Thodeti C.K. Trpv4 channels mediate cardiac fibroblast differentiation by integrating mechanical and soluble signals. J. Mol. Cell. Cardiol. 2013;54:45–52. doi: 10.1016/j.yjmcc.2012.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Sharma S., Goswami R., Zhang D.X., Rahaman S.O. Trpv4 regulates matrix stiffness and tgfβ1-induced epithelial-mesenchymal transition. J. Cell. Mol. Med. 2019;23:761–774. doi: 10.1111/jcmm.13972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Ehnert S., Sreekumar V., Aspera-Werz R.H., Sajadian S.O., Wintermeyer E., Sandmann G.H., Bahrs C., Hengstler J.G., Godoy P., Nussler A.K. Tgf-β(1) impairs mechanosensation of human osteoblasts via hdac6-mediated shortening and distortion of primary cilia. J. Mol. Med. (Berl. Ger.) 2017;95:653–663. doi: 10.1007/s00109-017-1526-4. [DOI] [PubMed] [Google Scholar]
- 217.Han S.J., Jung J.K., Im S.S., Lee S.R., Jang B.C., Park K.M., Kim J.I. Deficiency of primary cilia in kidney epithelial cells induces epithelial to mesenchymal transition. Biochem. Biophys. Res. Commun. 2018;496:450–454. doi: 10.1016/j.bbrc.2018.01.079. [DOI] [PubMed] [Google Scholar]
- 218.Kawasaki M., Ezura Y., Hayata T., Notomi T., Izu Y., Noda M. Tgf-β suppresses ift88 expression in chondrocytic atdc5 cells. J. Cell. Physiol. 2015;230:2788–2795. doi: 10.1002/jcp.25005. [DOI] [PubMed] [Google Scholar]
- 219.Egorova A.D., Khedoe P.P., Goumans M.J., Yoder B.K., Nauli S.M., ten Dijke P., Poelmann R.E., Hierck B.P. Lack of primary cilia primes shear-induced endothelial-to-mesenchymal transition. Circ. Res. 2011;108:1093–1101. doi: 10.1161/CIRCRESAHA.110.231860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Sánchez-Duffhues G., de Vinuesa A.G., Lindeman J.H., Mulder-Stapel A., DeRuiter M.C., Van Munsteren C., Goumans M.J., Hierck B.P., Ten Dijke P. Slug is expressed in endothelial cells lacking primary cilia to promote cellular calcification. Arterioscler. Thromb. Vasc. Biol. 2015;35:616–627. doi: 10.1161/ATVBAHA.115.305268. [DOI] [PubMed] [Google Scholar]
- 221.Clement C.A., Ajbro K.D., Koefoed K., Vestergaard M.L., Veland I.R., Henriques de Jesus M.P., Pedersen L.B., Benmerah A., Andersen C.Y., Larsen L.A., et al. Tgf-β signaling is associated with endocytosis at the pocket region of the primary cilium. Cell Rep. 2013;3:1806–1814. doi: 10.1016/j.celrep.2013.05.020. [DOI] [PubMed] [Google Scholar]
- 222.Vion A.C., Alt S., Klaus-Bergmann A., Szymborska A., Zheng T., Perovic T., Hammoutene A., Oliveira M.B., Bartels-Klein E., Hollfinger I., et al. Primary cilia sensitize endothelial cells to bmp and prevent excessive vascular regression. J. Cell Biol. 2018;217:1651–1665. doi: 10.1083/jcb.201706151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Koefoed K., Skat-Rørdam J., Andersen P., Warzecha C.B., Pye M., Andersen T.A., Ajbro K.D., Bendsen E., Narimatsu M., Vilhardt F., et al. The e3 ubiquitin ligase smurf1 regulates cell-fate specification and outflow tract septation during mammalian heart development. Sci. Rep. 2018;8:9542. doi: 10.1038/s41598-018-27854-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Gandhi J.G., Koch D.L., Paszek M.J. Equilibrium modeling of the mechanics and structure of the cancer glycocalyx. Biophys. J. 2019;116:694–708. doi: 10.1016/j.bpj.2018.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Gouverneur M., Berg B., Nieuwdorp M., Stroes E., Vink H. Vasculoprotective properties of the endothelial glycocalyx: Effects of fluid shear stress. J. Intern. Med. 2006;259:393–400. doi: 10.1111/j.1365-2796.2006.01625.x. [DOI] [PubMed] [Google Scholar]
- 226.Van den Berg B.M., Spaan J.A., Rolf T.M., Vink H. Atherogenic region and diet diminish glycocalyx dimension and increase intima-to-media ratios at murine carotid artery bifurcation. Am. J. Physiol. Heart Circ. Physiol. 2006;290:H915–H920. doi: 10.1152/ajpheart.00051.2005. [DOI] [PubMed] [Google Scholar]
- 227.Ueda A., Shimomura M., Ikeda M., Yamaguchi R., Tanishita K. Effect of glycocalyx on shear-dependent albumin uptake in endothelial cells. Am. J. Physiol. Heart Circ. Physiol. 2004;287:H2287–H2294. doi: 10.1152/ajpheart.00808.2003. [DOI] [PubMed] [Google Scholar]
- 228.Galie P.A., Nguyen D.H., Choi C.K., Cohen D.M., Janmey P.A., Chen C.S. Fluid shear stress threshold regulates angiogenic sprouting. Proc. Natl. Acad. Sci. USA. 2014;111:7968–7973. doi: 10.1073/pnas.1310842111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Uchida C., Haas T.L. Endothelial cell timp-1 is upregulated by shear stress via sp-1 and the tgfβ1 signaling pathways. Biochem. Cell Biol. Biochim. Et Biol. Cell. 2014;92:77–83. doi: 10.1139/bcb-2013-0086. [DOI] [PubMed] [Google Scholar]
- 230.Negishi M., Lu D., Zhang Y.Q., Sawada Y., Sasaki T., Kayo T., Ando J., Izumi T., Kurabayashi M., Kojima I., et al. Upregulatory expression of furin and transforming growth factor-beta by fluid shear stress in vascular endothelial cells. Arterioscler. Thromb. Vasc. Biol. 2001;21:785–790. doi: 10.1161/01.ATV.21.5.785. [DOI] [PubMed] [Google Scholar]
- 231.McCaffrey T.A., Falcone D.J., Du B. Transforming growth factor-beta 1 is a heparin-binding protein: Identification of putative heparin-binding regions and isolation of heparins with varying affinity for tgf-beta 1. J. Cell. Physiol. 1992;152:430–440. doi: 10.1002/jcp.1041520226. [DOI] [PubMed] [Google Scholar]
- 232.Rider C.C., Mulloy B. Heparin, heparan sulphate and the tgf-β cytokine superfamily. Molecules. 2017;22:713. doi: 10.3390/molecules22050713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Murphy N., Gaynor K.U., Rowan S.C., Walsh S.M., Fabre A., Boylan J., Keane M.P., McLoughlin P. Altered expression of bone morphogenetic protein accessory proteins in murine and human pulmonary fibrosis. Am. J. Pathol. 2016;186:600–615. doi: 10.1016/j.ajpath.2015.10.032. [DOI] [PubMed] [Google Scholar]
- 234.Paine-Saunders S., Viviano B.L., Economides A.N., Saunders S. Heparan sulfate proteoglycans retain noggin at the cell surface: A potential mechanism for shaping bone morphogenetic protein gradients. J. Biol. Chem. 2002;277:2089–2096. doi: 10.1074/jbc.M109151200. [DOI] [PubMed] [Google Scholar]
- 235.Resnick N., Collins T., Atkinson W., Bonthron D.T., Dewey C.F., Jr., Gimbrone M.A., Jr. Platelet-derived growth factor b chain promoter contains a cis-acting fluid shear-stress-responsive element. Proc. Natl. Acad. Sci. USA. 1993;90:4591–4595. doi: 10.1073/pnas.90.10.4591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Nayak L., Lin Z., Jain M.K. “Go with the flow”: How krüppel-like factor 2 regulates the vasoprotective effects of shear stress. Antioxid. Redox Signal. 2011;15:1449–1461. doi: 10.1089/ars.2010.3647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Tkachenko E., Gutierrez E., Saikin S.K., Fogelstrand P., Kim C., Groisman A., Ginsberg M.H. The nucleus of endothelial cell as a sensor of blood flow direction. Biol. Open. 2013;2:1007–1012. doi: 10.1242/bio.20134622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Wang N., Tytell J.D., Ingber D.E. Mechanotransduction at a distance: Mechanically coupling the extracellular matrix with the nucleus. Nat. Rev. Mol. Cell Biol. 2009;10:75–82. doi: 10.1038/nrm2594. [DOI] [PubMed] [Google Scholar]
- 239.Coan D.E., Wechezak A.R., Viggers R.F., Sauvage L.R. Effect of shear stress upon localization of the golgi apparatus and microtubule organizing center in isolated cultured endothelial cells. J. Cell Sci. 1993;104:1145–1153. doi: 10.1242/jcs.104.4.1145. [DOI] [PubMed] [Google Scholar]
- 240.Cucina A., Sterpetti A.V., Pupelis G., Fragale A., Lepidi S., Cavallaro A., Giustiniani Q., Santoro D’Angelo L. Shear stress induces changes in the morphology and cytoskeleton organisation of arterial endothelial cells. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 1995;9:86–92. doi: 10.1016/S1078-5884(05)80230-8. [DOI] [PubMed] [Google Scholar]
- 241.Joukov V., De Nicolo A. The Centrosome and the Primary Cilium: The Yin and Yang of a Hybrid Organelle. Cells. 2019;8:701. doi: 10.3390/cells8070701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Lai J.K., Stainier D.Y. Pushing yap into the nucleus with shear force. Dev. Cell. 2017;40:517–518. doi: 10.1016/j.devcel.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 243.Elosegui-Artola A., Andreu I., Beedle A.E.M., Lezamiz A., Uroz M., Kosmalska A.J., Oria R., Kechagia J.Z., Rico-Lastres P., Le Roux A.L., et al. Force triggers yap nuclear entry by regulating transport across nuclear pores. Cell. 2017;171:1397–1410. doi: 10.1016/j.cell.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 244.Na S., Collin O., Chowdhury F., Tay B., Ouyang M., Wang Y., Wang N. Rapid signal transduction in living cells is a unique feature of mechanotransduction. Proc. Natl. Acad. Sci. USA. 2008;105:6626–6631. doi: 10.1073/pnas.0711704105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Isermann P., Lammerding J. Nuclear mechanics and mechanotransduction in health and disease. Curr. Biol. CB. 2013;23:R1113–R1121. doi: 10.1016/j.cub.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Maniotis A.J., Chen C.S., Ingber D.E. Demonstration of mechanical connections between integrins, cytoskeletal filaments, and nucleoplasm that stabilize nuclear structure. Proc. Natl. Acad. Sci. USA. 1997;94:849–854. doi: 10.1073/pnas.94.3.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Ramdas N.M., Shivashankar G.V. Cytoskeletal control of nuclear morphology and chromatin organization. J. Mol. Biol. 2015;427:695–706. doi: 10.1016/j.jmb.2014.09.008. [DOI] [PubMed] [Google Scholar]
- 248.Martin M., Veloso A., Wu J., Katrukha E.A., Akhmanova A. Control of endothelial cell polarity and sprouting angiogenesis by non-centrosomal microtubules. eLife. 2018;7 doi: 10.7554/eLife.33864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Kushner E.J., Ferro L.S., Yu Z., Bautch V.L. Excess centrosomes perturb dynamic endothelial cell repolarization during blood vessel formation. Mol. Biol. Cell. 2016;27:1911–1920. doi: 10.1091/mbc.e15-09-0645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Wu J., Misra G., Russell R.J., Ladd A.J., Lele T.P., Dickinson R.B. Effects of dynein on microtubule mechanics and centrosome positioning. Mol. Biol. Cell. 2011;22:4834–4841. doi: 10.1091/mbc.e11-07-0611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Kim J.K., Louhghalam A., Lee G., Schafer B.W., Wirtz D., Kim D.H. Nuclear lamin a/c harnesses the perinuclear apical actin cables to protect nuclear morphology. Nat. Commun. 2017;8:2123. doi: 10.1038/s41467-017-02217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Yoshigi M., Hoffman L.M., Jensen C.C., Yost H.J., Beckerle M.C. Mechanical force mobilizes zyxin from focal adhesions to actin filaments and regulates cytoskeletal reinforcement. J. Cell Biol. 2005;171:209–215. doi: 10.1083/jcb.200505018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Shiu J.Y., Aires L., Lin Z., Vogel V. Nanopillar force measurements reveal actin-cap-mediated yap mechanotransduction. Nat. Cell Biol. 2018;20:262–271. doi: 10.1038/s41556-017-0030-y. [DOI] [PubMed] [Google Scholar]
- 254.Schirmer E.C., Foisner R. Proteins that associate with lamins: Many faces, many functions. Exp. Cell Res. 2007;313:2167–2179. doi: 10.1016/j.yexcr.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 255.Lammerding J., Fong L.G., Ji J.Y., Reue K., Stewart C.L., Young S.G., Lee R.T. Lamins a and c but not lamin b1 regulate nuclear mechanics. J. Biol. Chem. 2006;281:25768–25780. doi: 10.1074/jbc.M513511200. [DOI] [PubMed] [Google Scholar]
- 256.Ihalainen T.O., Aires L., Herzog F.A., Schwartlander R., Moeller J., Vogel V. Differential basal-to-apical accessibility of lamin a/c epitopes in the nuclear lamina regulated by changes in cytoskeletal tension. Nat. Mater. 2015;14:1252–1261. doi: 10.1038/nmat4389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Sullivan T., Escalante-Alcalde D., Bhatt H., Anver M., Bhat N., Nagashima K., Stewart C.L., Burke B. Loss of a-type lamin expression compromises nuclear envelope integrity leading to muscular dystrophy. J. Cell Biol. 1999;147:913–920. doi: 10.1083/jcb.147.5.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Swift J., Ivanovska I.L., Buxboim A., Harada T., Dingal P.C., Pinter J., Pajerowski J.D., Spinler K.R., Shin J.W., Tewari M., et al. Nuclear lamin-a scales with tissue stiffness and enhances matrix-directed differentiation. Science. 2013;341:1240104. doi: 10.1126/science.1240104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Qi Y.X., Jiang J., Jiang X.H., Wang X.D., Ji S.Y., Han Y., Long D.K., Shen B.R., Yan Z.Q., Chien S., et al. Pdgf-bb and tgf-{beta}1 on cross-talk between endothelial and smooth muscle cells in vascular remodeling induced by low shear stress. Proc. Natl. Acad. Sci. USA. 2011;108:1908–1913. doi: 10.1073/pnas.1019219108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Jiang Y., Ji J.Y. Expression of nuclear lamin proteins in endothelial cells is sensitive to cell passage and fluid shear stress. Cell. Mol. Bioeng. 2018;11:53–64. doi: 10.1007/s12195-017-0513-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Chatzifrangkeskou M., Le Dour C., Wu W., Morrow J.P., Joseph L.C., Beuvin M., Sera F., Homma S., Vignier N., Mougenot N., et al. Erk1/2 directly acts on ctgf/ccn2 expression to mediate myocardial fibrosis in cardiomyopathy caused by mutations in the lamin a/c gene. Hum. Mol. Genet. 2016;25:2220–2233. doi: 10.1093/hmg/ddw090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Hata A., Lagna G., Massagué J., Hemmati-Brivanlou A. Smad6 inhibits bmp/smad1 signaling by specifically competing with the smad4 tumor suppressor. Genes Dev. 1998;12:186–197. doi: 10.1101/gad.12.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Altraja S., Jaama J., Valk E., Altraja A. Changes in the proteome of human bronchial epithelial cells following stimulation with leucotriene e4 and transforming growth factor-beta1. Respirology. 2009;14:39–45. doi: 10.1111/j.1440-1843.2008.01414.x. [DOI] [PubMed] [Google Scholar]
- 264.Comaills V., Kabeche L., Morris R., Buisson R., Yu M., Madden M.W., LiCausi J.A., Boukhali M., Tajima K., Pan S., et al. Genomic instability is induced by persistent proliferation of cells undergoing epithelial-to-mesenchymal transition. Cell Rep. 2016;17:2632–2647. doi: 10.1016/j.celrep.2016.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Pan D., Estévez-Salmerón L.D., Stroschein S.L., Zhu X., He J., Zhou S., Luo K. The integral inner nuclear membrane protein man1 physically interacts with the r-smad proteins to repress signaling by the transforming growth factor-{beta} superfamily of cytokines. J. Biol. Chem. 2005;280:15992–16001. doi: 10.1074/jbc.M411234200. [DOI] [PubMed] [Google Scholar]
- 266.Lin F., Morrison J.M., Wu W., Worman H.J. Man1, an integral protein of the inner nuclear membrane, binds smad2 and smad3 and antagonizes transforming growth factor-beta signaling. Hum. Mol. Genet. 2005;14:437–445. doi: 10.1093/hmg/ddi040. [DOI] [PubMed] [Google Scholar]
- 267.Raju G.P., Dimova N., Klein P.S., Huang H.C. Sane, a novel lem domain protein, regulates bone morphogenetic protein signaling through interaction with smad1. J. Biol. Chem. 2003;278:428–437. doi: 10.1074/jbc.M210505200. [DOI] [PubMed] [Google Scholar]
- 268.Osada S., Ohmori S.Y., Taira M. Xman1, an inner nuclear membrane protein, antagonizes bmp signaling by interacting with smad1 in xenopus embryos. Development (Camb. Engl.) 2003;130:1783–1794. doi: 10.1242/dev.00401. [DOI] [PubMed] [Google Scholar]
- 269.Bourgeois B., Gilquin B., Tellier-Lebègue C., Östlund C., Wu W., Pérez J., El Hage P., Lallemand F., Worman H.J., Zinn-Justin S. Inhibition of tgf-β signaling at the nuclear envelope: Characterization of interactions between man1, smad2 and smad3, and ppm1a. Sci. Signal. 2013;6:ra49. doi: 10.1126/scisignal.2003411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Lombardi M.L., Jaalouk D.E., Shanahan C.M., Burke B., Roux K.J., Lammerding J. The interaction between nesprins and sun proteins at the nuclear envelope is critical for force transmission between the nucleus and cytoskeleton. J. Biol. Chem. 2011;286:26743–26753. doi: 10.1074/jbc.M111.233700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Cain N.E., Jahed Z., Schoenhofen A., Valdez V.A., Elkin B., Hao H., Harris N.J., Herrera L.A., Woolums B.M., Mofrad M.R.K., et al. Conserved sun-kash interfaces mediate linc complex-dependent nuclear movement and positioning. Curr. Biol. CB. 2018;28:3086–3097. doi: 10.1016/j.cub.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Han Y., Wang L., Yao Q.P., Zhang P., Liu B., Wang G.L., Shen B.R., Cheng B., Wang Y., Jiang Z.L., et al. Nuclear envelope proteins nesprin2 and lamina regulate proliferation and apoptosis of vascular endothelial cells in response to shear stress. Biochim. Biophys. Acta. 2015;1853:1165–1173. doi: 10.1016/j.bbamcr.2015.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Rashmi R.N., Eckes B., Glöckner G., Groth M., Neumann S., Gloy J., Sellin L., Walz G., Schneider M., Karakesisoglou I., et al. The nuclear envelope protein nesprin-2 has roles in cell proliferation and differentiation during wound healing. Nucleus (AustinTex.) 2012;3:172–186. doi: 10.4161/nucl.19090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Van Steensel B., Belmont A.S. Lamina-associated domains: Links with chromosome architecture, heterochromatin, and gene repression. Cell. 2017;169:780–791. doi: 10.1016/j.cell.2017.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Uhler C., Shivashankar G.V. Regulation of genome organization and gene expression by nuclear mechanotransduction. Nat. Rev. Mol. Cell Biol. 2017;18:717–727. doi: 10.1038/nrm.2017.101. [DOI] [PubMed] [Google Scholar]
- 276.Schlereth K., Weichenhan D., Bauer T., Heumann T., Giannakouri E., Lipka D., Jaeger S., Schlesner M., Aloy P., Eils R., et al. The transcriptomic and epigenetic map of vascular quiescence in the continuous lung endothelium. eLife. 2018;7 doi: 10.7554/eLife.34423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Hayashi M., Nimura K., Kashiwagi K., Harada T., Takaoka K., Kato H., Tamai K., Kaneda Y. Comparative roles of twist-1 and id1 in transcriptional regulation by bmp signaling. J. Cell Sci. 2007;120:1350–1357. doi: 10.1242/jcs.000067. [DOI] [PubMed] [Google Scholar]
- 278.Kim D.W., Lassar A.B. Smad-dependent recruitment of a histone deacetylase/sin3a complex modulates the bone morphogenetic protein-dependent transcriptional repressor activity of nkx3.2. Mol. Cell. Biol. 2003;23:8704–8717. doi: 10.1128/MCB.23.23.8704-8717.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Wotton D., Lo R.S., Lee S., Massagué J. A smad transcriptional corepressor. Cell. 1999;97:29–39. doi: 10.1016/S0092-8674(00)80712-6. [DOI] [PubMed] [Google Scholar]
- 280.Frontelo P., Leader J.E., Yoo N., Potocki A.C., Crawford M., Kulik M., Lechleider R.J. Suv39h histone methyltransferases interact with smads and cooperate in bmp-induced repression. Oncogene. 2004;23:5242–5251. doi: 10.1038/sj.onc.1207660. [DOI] [PubMed] [Google Scholar]
- 281.Grannas K., Arngården L., Lönn P., Mazurkiewicz M., Blokzijl A., Zieba A., Söderberg O. Crosstalk between hippo and tgfβ: Subcellular localization of yap/taz/smad complexes. J. Mol. Biol. 2015;427:3407–3415. doi: 10.1016/j.jmb.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 282.Alarcón C., Zaromytidou A.I., Xi Q., Gao S., Yu J., Fujisawa S., Barlas A., Miller A.N., Manova-Todorova K., Macias M.J., et al. Nuclear cdks drive smad transcriptional activation and turnover in bmp and tgf-beta pathways. Cell. 2009;139:757–769. doi: 10.1016/j.cell.2009.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Yao M., Wang Y., Zhang P., Chen H., Xu Z., Jiao J., Yuan Z. Bmp2-smad signaling represses the proliferation of embryonic neural stem cells through yap. J. Neurosci. 2014;34:12039–12048. doi: 10.1523/JNEUROSCI.0486-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Zhao B., Ye X., Yu J., Li L., Li W., Li S., Yu J., Lin J.D., Wang C.Y., Chinnaiyan A.M., et al. Tead mediates yap-dependent gene induction and growth control. Genes Dev. 2008;22:1962–1971. doi: 10.1101/gad.1664408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Bartholin L., Wessner L.L., Chirgwin J.M., Guise T.A. The human cyr61 gene is a transcriptional target of transforming growth factor beta in cancer cells. Cancer Lett. 2007;246:230–236. doi: 10.1016/j.canlet.2006.02.019. [DOI] [PubMed] [Google Scholar]
- 286.Zhou Y., Huang T., Cheng A.S., Yu J., Kang W., To K.F. The tead family and its oncogenic role in promoting tumorigenesis. Int. J. Mol. Sci. 2016;17:138. doi: 10.3390/ijms17010138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Fujii M., Toyoda T., Nakanishi H., Yatabe Y., Sato A., Matsudaira Y., Ito H., Murakami H., Kondo Y., Kondo E., et al. Tgf-β synergizes with defects in the hippo pathway to stimulate human malignant mesothelioma growth. J. Exp. Med. 2012;209:479–494. doi: 10.1084/jem.20111653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Huang Z., Hu J., Pan J., Wang Y., Hu G., Zhou J., Mei L., Xiong W.C. Yap stabilizes smad1 and promotes bmp2-induced neocortical astrocytic differentiation. Development (Camb. Engl.) 2016;143:2398–2409. doi: 10.1242/dev.130658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Mihira H., Suzuki H.I., Akatsu Y., Yoshimatsu Y., Igarashi T., Miyazono K., Watabe T. Tgf-β-induced mesenchymal transition of ms-1 endothelial cells requires smad-dependent cooperative activation of rho signals and mrtf-a. J. Biochem. 2012;151:145–156. doi: 10.1093/jb/mvr121. [DOI] [PubMed] [Google Scholar]
- 290.Morita T., Mayanagi T., Sobue K. Dual roles of myocardin-related transcription factors in epithelial mesenchymal transition via slug induction and actin remodeling. J. Cell Biol. 2007;179:1027–1042. doi: 10.1083/jcb.200708174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Wang D.Z., Li S., Hockemeyer D., Sutherland L., Wang Z., Schratt G., Richardson J.A., Nordheim A., Olson E.N. Potentiation of serum response factor activity by a family of myocardin-related transcription factors. Proc. Natl. Acad. Sci. USA. 2002;99:14855–14860. doi: 10.1073/pnas.222561499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Iwasaki K., Hayashi K., Fujioka T., Sobue K. Rho/rho-associated kinase signal regulates myogenic differentiation via myocardin-related transcription factor-a/smad-dependent transcription of the id3 gene. J. Biol. Chem. 2008;283:21230–21241. doi: 10.1074/jbc.M710525200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Vartiainen M.K., Guettler S., Larijani B., Treisman R. Nuclear actin regulates dynamic subcellular localization and activity of the srf cofactor mal. Science. 2007;316:1749–1752. doi: 10.1126/science.1141084. [DOI] [PubMed] [Google Scholar]
- 294.Weissbach J., Schikora F., Weber A., Kessels M., Posern G. Myocardin-related transcription factor a activation by competition with wh2 domain proteins for actin binding. Mol. Cell. Biol. 2016;36:1526–1539. doi: 10.1128/MCB.01097-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Finch-Edmondson M., Sudol M. Framework to function: Mechanosensitive regulators of gene transcription. Cell. Mol. Biol. Lett. 2016;21:28. doi: 10.1186/s11658-016-0028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Kim J., Kim Y.H., Kim J., Park D.Y., Bae H., Lee D.H., Kim K.H., Hong S.P., Jang S.P., Kubota Y., et al. Yap/taz regulates sprouting angiogenesis and vascular barrier maturation. J. Clin. Investig. 2017;127:3441–3461. doi: 10.1172/JCI93825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Speight P., Kofler M., Szászi K., Kapus A. Context-dependent switch in chemo/mechanotransduction via multilevel crosstalk among cytoskeleton-regulated mrtf and taz and tgfβ-regulated smad3. Nat. Commun. 2016;7:11642. doi: 10.1038/ncomms11642. [DOI] [PMC free article] [PubMed] [Google Scholar]