Abstract
Chronic obstructive pulmonary disease (COPD) is a respiratory illness characterized by airflow limitation and chronic respiratory symptoms with a global prevalence estimated to be more than 10% in 2010 and still on the rise. Furthermore, hypercapnic subject COPD leads to an increased risk of mortality, morbidity, and poor QoL (quality of life) than normocapnic subjects. Series of studies showed the usefulness of the forced oscillation technique (FOT) to measure small airway closure. Traditional findings suggested that hypercapnia may not be the main treating targets, but recent findings suggested that blood stream CO2 may lead to a worse outcome. This study aimed to seek the relationship between CO2 and small airway closure by using FOT. Subjects with COPD (n = 124; hypercapnia 22 and normocapnia 102) were analyzed for all pulmonary function values, FOT values, and arterial blood gas analysis. Student’s t-test, Spearman rank correlation, and multi linear regression analysis were used to analyze the data. COPD subjects with hypercapnia showed a significant increase in R5, R20, Fres, and ALX values, and a greater decrease in X5 value than normocapnic patients. Also, multiple linear regression analysis showed R5 was associated with hypercapnia. Hypercapnia may account for airway closure among subjects with COPD and this result suggests treating hypercapnia may lead to better outcomes for such a subject group.
Keywords: CO2, hypercapnia, FOT
1. Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogenous condition with clinical presentation, mainly dyspnea, cough, sputum, and importantly, airflow limitation [1,2]. Briefly, the disease severity is defined by the degree of functional impairment of pulmonary function and (activity by) frequency of exacerbations. There is a link between disease severity and activity which forms a vicious circle that (finally) impacts patient’s quality of life (QoL) and may lead to frailty status with abnormal gas exchange, hypoxia, and hypercapnia [3,4,5].
Gaseous molecules such as oxygen (O2) and CO2 are sensed by lung cells eliciting specific responses via intracellular signaling pathways [6,7,8,9,10,11,12,13,14]. Hypercapnia, an elevation in the arterial CO2 tension, is generally well tolerated in mechanically ventilated patients with acute respiratory distress syndrome (ARDS), but recent studies suggest that a high concentration of CO2, independently of hypoxia, can act a gaso-signaling molecule resulting in adverse consequences via the alteration of transcription factor activity and microRNA (miR) expression in the lung [6,7,8,9,13,15,16,17,18,19]. Specifically, our recent study showed that high CO2 levels increased airway smooth muscle contractility via activation of the caspase-7-mediated miR-133a-RhoA signaling [9]. We also reported that in a small cohort of severe COPD, airway obstruction was worsened in hypercapnic patients [9]. These lines of evidence raised the possibility that elevated levels of CO2 within the lung (may result in an impact on) attenuated pulmonary function and lead to worse QoL in COPD [4,8,9,16].
The forced oscillation technique (FOT) is a noninvasive method and measures respiratory impedance of the airway which was first described by Dubois in 1956 [20,21,22,23,24]. FOT was able to measure and calculate the airway resistance (Rrs) and reactance (Xrs). Recent findings showed the clinical utility among asthma, cystic fibrosis, interstitial lung disease, and COPD [20,25,26,27,28,29]. Among COPD patients, previous reports showed the relationship between the early detection of acute exacerbation and physiological activity, and used this to distinguish between asthma [25,26,27,28], but the relationship between FOT and CO2 has not been fully investigated.
In this study, we hypothesized that elevated levels of CO2 could possibly influence the respiratory function values including FOT values and investigated which specific respiratory function value correlates with the level of CO2 levels in arterial blood. Our final aim for this study was to see the correlation between PCO2 and FOT values among subjects with COPD.
2. Methods
2.1. Participating COPD Subjects
Patients with chronic stable COPD with or without hypercapnia presented at Showa University Hospital meeting all the inclusion criterion: pulmonary function criteria of the global initiative for chronic obstructive lung disease guidelines, age above 40 years old, and current or ex-smoker with a smoking history of >10 pack-years. Hypercapnia was defined as PCO2 of more than 45 mmHg [9,30]. Clinician-based asthma diagnosed subjects were excluded. The study population, gender, age, body mass index (BMI), arterial blood gas results, and pulmonary function tests results were obtained from medical records. This study was carried out in accordance with the guidelines of the Helsinki Declaration. Study approval was granted by the ethics committee of Showa University School of Medicine (approval number, 2360) and newly enrolled patients were added to our previous study [9].
2.2. Arterial Blood Gas Analysis
Femoral arterial blood (1.0 mL; 3 units of heparin per syringe) was drawn with a 22-gauge needle attached to a heparinized syringe. Samples were immediately analyzed with a blood gas analyzer (Rapidlab 1200; Siemens Healthcare Diagnostics, Sudbury, United Kingdom).
2.3. Pulmonary Function Test and FOT
On the same examination day of arterial blood gas was taken, pulmonary function test and FOT were performed. Pulmonary function test was determined using computerized equipment (model CHESTAC-8800; Chest M.I. Co. Ltd., Tokyo, Japan) according to the recommendations of the American Thoracic Society [31]. Forced vital capacity (FVC) is the expiratory air volume after the maximum inspiration, forced expiratory volume in 1 s (FEV1) is the volume of FVC in the first 1 s, and peak expiratory flow (PEF) is the maximal flow achieved during measurement of FVC at full inspiration. Furthermore, V50 and V25 are the velocity of expiratory airflow at 50% or 25% of FVC, respectively. Finally, %FVC, %FEV1, %PEF, %V50, and %V25 stands for comparative value in (%) to normal value of each subjects.
FOT was performed with available commercial-based equipment (MostGraph-01, CHEST M.I.). The FOT procedure was performed according to major recommendations published by several authors [9,22,25,26]. On the day of the procedure, subjects were asked to wear a nose clip and were seated during tidal breathing [32]. All subjects were asked to seal their lips tightly around the mouthpiece and firmly supporting their cheeks with their hands. A minimum of three trials, each lasting 30 s, were performed. Mouth pressure and flow signals were measured and calculated for Rrs and Xrs properties against oscillatory frequency ranging from 4 to 36 Hz. We used Rrs at 5 and 20 Hz (R5 and R20, respectively), Xrs at 5 Hz (X5) for values that reflect elastic properties, resonant frequency (Fres) where Xrs crosses zero and the elastic and inertial forces are equal in magnitude and opposite, and a low-frequency reactance area (ALX), which is the integral of Xrs at 5 Hz to the Fres as previously described by other groups [22,25,26]. Briefly, R5, R20, and R5–R20 indicate the respiratory system resistance of total, central, and peripheral portions, respectively. The reactance at 5 Hz (X5) reflects the combined effect of tissue elastance and inertance. Both inspiratory and expiratory phases of oscillatory index were measured.
2.4. Statistical Analysis
Data are expressed as mean ± 25% of range unless specified otherwise. Values of pulmonary function test, FOT, and arterial blood gas were assessed using Student’s t-test, Spearman rank correlation, and multi linear regression analysis. All statistical analyses were performed using GraphPad Prism 5.0 (GraphPad Software, La Jolla, CA, USA) software.
3. Results
3.1. Characteristics of COPD Subjects
In total, 124 subjects were enrolled and analyzed (Table 1). Subjects’ median age was 76.5 years-old, female dominant with the median PCO2 value of 46.60 mmHg in the group of subjects with hypercapnic COPD. Whereas, median age of 73 years-old, male dominant, and median PCO2 value of 36.55 mmHg in the subjects with normocapnic COPD group. Arterial blood gas values were distinct for each other group, whereas background characteristics were not significantly different.
Table 1.
Background characteristics of enrolled subjects with COPD.
| Hypercapnia | Normocapnia | p Value | |
|---|---|---|---|
| (n = 22) | (n = 102) | ||
| Age, years-old | 76.5 (68.25–80.75) | 73 (67.25–77.75) | 0.245 |
| Gender, male/female, n | 9/13 | 74/28 | 0.303 |
| Smoking history, pack-years | 55 (32.5–105.12) | 54 (39–91.87) | 0.816 |
| Hight, cm | 157.35 (151.72–168) | 161 (154.37–167.22) | 0.786 |
| Body weight, kg | 52.85 (48.17–67.25) | 57.9 (50.15–68.8) | 0.252 |
| BMI, kg/m2 | 20.88 (18.66–25.60) | 23.36 (20.11–25.74) | 0.18 |
| Body surface area, m2/kg2 | 1.53 (1.45–1.69) | 1.58 (1.47–1.75) | 0.308 |
| Arterial blood gas | |||
| pH | 7.42 (7.39–7.42) | 7.44 (7.43–7.46) | <0.001 |
| pCO2, mmHg | 46.60 (45.7–53.2) | 36.55 (35–39.7) | <0.001 |
| pO2, mmHg | 71.2 (67.8–84.52) | 84.55 (75.62–90.45) | <0.003 |
| HCO3-, mmol/L | 30 (27.97–32.52) | 24.9 (23.32–26.37) | <0.001 |
| BE, mmol/L | 4.1 (2.95–7.5) | 0.9 (−0.3–2.2) | <0.001 |
| tCO2, mmHg | 26 (24–27.7) | 30.75 (29.2–33.82) | <0.001 |
3.2. Pulmonary Function Test and FOT Values of Enrolled Subjects with COPD
Most of the pulmonary function test values were significantly lower in the subjects with hypercapnic COPD group than normocapnic COPD group; FVC, %FVC, FEV1, %FEV1, %PEF, V25, and %V25 (Table 2). Only R5 and R5-20 values showed a consistent difference in all phases (whole breath, inspiratory, and expiratory) when both groups were compared (Table 3). The whole breath of R5, R5–R20, Fres, and ALX values showed higher subjects with hypercapnia. Meanwhile, X5 value showed higher in subjects with non-hypercapnia.
Table 2.
Pulmonary function test values of enrolled subjects with COPD.
| Hypercapnia | Normocapnia | p Value | |
|---|---|---|---|
| (n = 22) | (n = 102) | ||
| FVC, L | 1.97 (1.40–2.57) | 2.89 (2.33–3.47) | <0.001 |
| %FVC, % | 65.85 (51.40–82) | 97.3 (84.85–110.07) | <0.001 |
| FEV1, L | 0.8 (0.66–1.31) | 1.73 (1.32–2.19) | <0.001 |
| %FEV1, % | 36.82 (29.1–62.95) | 74.7 (55.12–84.45) | <0.001 |
| FEV1%, % | 53.71 (31.88–68.94) | 63.15 (50.84–71.19) | 0.228 |
| PEF, L | 2.98 (2.54–4.18) | 5.11 (3.76–6.69) | 0.781 |
| %PEF, % | 39.20 (29.55–39.20) | 69.35 (48.02–81.15) | <0.001 |
| V50, L | 0.58 (0.21–1.43) | 1.15 (0.65–1.89) | 0.044 |
| %V50, % | 18.35 (7.15–67.75) | 35.05 (19.27–61.4) | 0.101 |
| V25, L | 0.14 (0.12–0.34) | 0.26 (0.16–0.42) | 0.006 |
| %V25, % | 18.1 (10.72–29.27) | 27.2 (16.22–39.57) | 0.015 |
Table 3.
FOT values of enrolled subjects with COPD.
| Hypercapnia | Normocapnia | p Value | |
|---|---|---|---|
| (n = 22) | (n = 102) | ||
| R5, cmH2O/L/s | |||
| Whole breath | 5.05 (3.58–6.43) | 3.50 (2.72–4.32) | 0.001 |
| Inspiratory | 5.56 (3.62–7.75) | 3.91 (3.00–5.02) | 0.004 |
| Exspiratory | 4.32 (3.28–5.07) | 3.09 (2.34–3.83) | 0.005 |
| delta R5 | 1.17 (0.25–2.07) | 0.77 (0.47–1.29) | 0.001 |
| R20, cmH2O/L/s | |||
| Whole breath | 2.78 (2.01–3.77) | 2.56 (2.21–3.31) | 0.891 |
| Inspiratory | −1.47 (−3.45–0.22) | 2.87 (2.33–3.62) | <0.001 |
| Exspiratory | 3.94 (1.87–7.51) | 2.34 (1.90–3.06) | 0.009 |
| delta R20 | −5.46 (−11.25–−0.21) | 0.41 (0.22–0.75) | <0.001 |
| R5–R20, cmH2O/L/s | |||
| Whole breath | 9.29 (2.54–18.76) | 0.80 (0.53–1.19) | <0.001 |
| Inspiratory | −14.75 (−30.01–−1.01) | 1.00 (0.66–1.47) | <0.001 |
| Exspiratory | 24.04 (3.71–48.77) | 0.57 (0.34–0.89) | <0.001 |
| delta (R5-R20) | −38.78 (−78.77–−2.98) | 0.38 (0.18–0.58) | <0.001 |
| X5, cmH2O/L/s | |||
| Whole breath | −2.66 (−4.51–−1.12) | −0.74 (−1.90–−0.37) | <0.001 |
| Inspiratory | −3.34 (−5.26–−1.09) | −0.78 (−2.41–−0.35) | <0.001 |
| Exspiratory | −1.96 (−3.01–−1.16) | −0.74 (−1.34–−0.39) | <0.001 |
| delta X5 | −0.79 (−2.29–0.09) | −0.09 (−0.96–0.18) | 0.108 |
| Fres, Hz | |||
| Whole breath | 19.03 (11.99–22.57) | 9.90 (7.44–15.05) | <0.001 |
| Inspiratory | 20.87 (12.16–23.89) | 10.47 (7.46–16.73) | <0.001 |
| Exspiratory | 16.76 (11.66–22.18) | 9.81 (7.34–13.04) | <0.001 |
| delta Fres | 2.34 (0.89–4.35) | 1.18 (−0.62–4.14) | 0.431 |
| ALX, cmH2O/L/s Hz | |||
| Whole breath | 22.70 (5.17–36.94) | 2.91 (1.24–12.16) | <0.001 |
| Inspiratory | 29.53 (5.20–47.61) | 2.98 (1.12–16.00) | <0.001 |
| Exspiratory | 14.31 (5.75–23.49) | 2.92 (1.28–7.25) | <0.001 |
| delta ALX | 7.76 (0.81–18.79) | 0.74 (−0.47–7.24) | 0.059 |
3.3. Correlation of PCO2 and Pulmonary Function Test and FOT Values
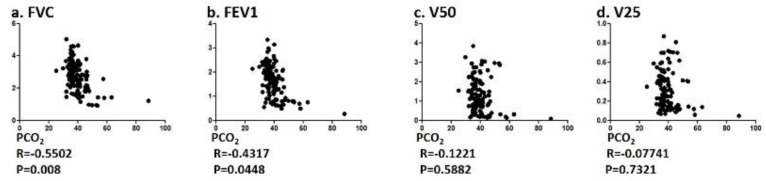
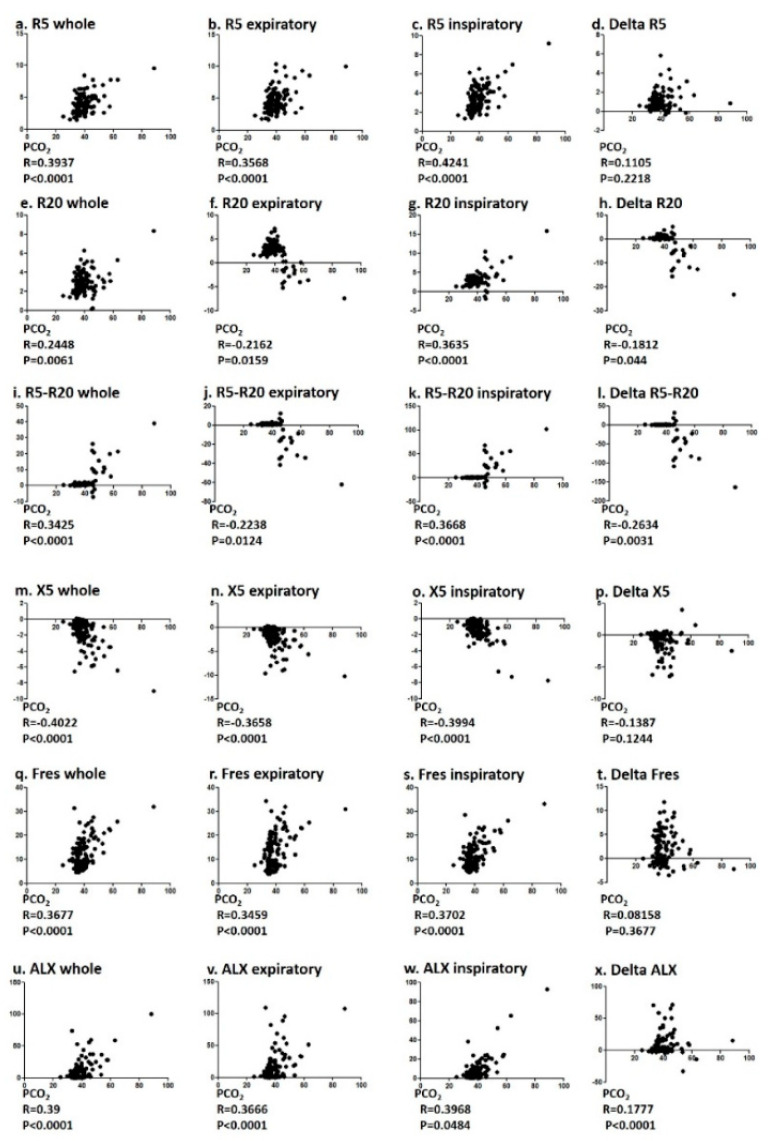
The correlation between PCO2 and pulmonary function values (FVC and FEV1) were correlated with significance, but both V50 and V25 did not (Figure 1). R5, R20, R5–R20, X5, Fres, and the ALX in whole breath phase showed a significant correlation with PCO2 (Figure 2). Among FOT values, R5 in the inspiratory phase and X5 in the whole breath phase showed a significant correlation with relatively strong R values of 0.4241 and −0.422, respectively.
Figure 1.
Correlation between PCO2 and pulmonary function test values. Specifically, correlation between PCO2 and (a) FVC, (b) FEV1, (c) V50, and (d) V25 were analyzed using Spearman rank correlation test.
Figure 2.
Correlation between PCO2 and FOT values. Specifically, correlation between PCO2 (a–d) R5, (e–h) R20, (i–l) R5-R20, (m–p) X5, (q–t) Fres, and (u–x) ALX were analyzed using Spearman rank correlation test.
3.4. Multiple Linear Regression Analysis of Clinical Variables Associated with Hypercapnia
Multiple linear regression analysis of hypercapnia-positivity was performed using eight variables (Table 4). The hypercapnia-positivity was independently predicted by the whole breath of R5 values.
Table 4.
Multiple linear regression analysis of clinical variables associated with hypercapnia.
| Coefficient | SE | 95%CI | p Value | |
|---|---|---|---|---|
| Age | −0.101 | 0.064 | −0.229 to 0.026 | 0.118 |
| Gender | 2.127 | 1.292 | −0.431 to 4.687 | 0.102 |
| BMI | −0.214 | 0.269 | −0.474 to 0.046 | 0.105 |
| R5 whole breath | 1.46 | 0.679 | 0.114 to 2.805 | 0.033 |
| R20 whole breath | −1.138 | 0.693 | −2.5116 to 0.234 | 0.103 |
| Fres whole breath | −0.414 | 0.269 | −0.948 to 0.118 | 0.126 |
| X5 whole breath | −1.482 | 2.231 | −5.903 to 2.938 | 0.507 |
| ALX whole breath | 0.21 | 0.179 | −0.145 to 0.566 | 0.244 |
4. Discussion
In this current study, we assessed the correlation between each FOT values and PCO2 among COPD subjects. We found that FOT values largely differ between COPD subjects with or without hypercapnia. Although the values of pulmonary function test also correlated significantly with PCO2, the correlation was also significant using the values of FOT, which were easier to obtain than conventional pulmonary function tests.
Current COPD guideline diagnosis process relies on using spirometry to assess airflow limitation with symptoms and exacerbation history [33]. Spirometry involves a forced expiratory operation to measure each value such as FEV1 [24]. This procedure cannot be found in real life and often gives stress to low and high-aged population. It is true that the forced expiratory flow between 25 and 75% of FVC is one of the represented values of small airway closure, but the repeated process can make a large difference. To solve these problems, FOT was developed in subjects with asthma and COPD, and for pediatrics subjects [34]. The current study showed the correlation of arterial CO2 and small airway closure, suggesting measuring FOT maybe useful for monitoring arterial CO2, since obtaining arterial blood gas sample is time taking and invasive in some degree. Further studies will be needed to assess the usefulness of FOT in subjects with hypercapnia.
The correlation between respiratory impedance and pulmonary function has been reported [35,36,37,38,39]. Lower FEV1 /FVC and altered peripheral FOT measures (X5 and Fres) were associated with uncontrolled asthma [36]. Previous studies showed that correlations between Rrs and Xrs values and FEV1 and FEV1/FVC, while Matsumoto et al. found the correlations between alveolar NO levels and R5–R20, X5, and ALX [37,38]. Williamson et al. also found weak correlations between fractions of exhaled NO and FOT values, R5–R20, and Fres in patients with asthma or COPD [39]. Additionally, in a cohort of 215 patients GOLD stages 1 to 4, values for ALX was related to the ratio of residual volume to total lung capacity (RV/TLC), leading to inferring the degree of air trapping is related to reduced lung compliance [24,40]. Other studies demonstrated the relationship between increased value of ALX and the exacerbation rate of COPD [40,41]. Multiple regression analysis of 75 patients with moderate COPD found that R5–R20 was more related to health status and symptoms than either FEV1 or HRCT low attenuation [42]. Even in the early stage of subjects with COPD, among 124 subjects who had positive spirometry criteria, the presence of self-reported symptoms was associated with higher values of R5–R20 and ALX [43]. Our current study showed positive correlation between PCO2 and R5, R20, R5–R20, Fres, and ALX. X5 was the only factor that negatively correlated and showed a relatively high value of correlation. X5 is thought to reflect the combined effect of tissue elastance and inertance, therefore not only caused of COPD, mainly tobacco smoke, but CO2 may affect the tissue remodeling. Since there was correlation between PCO2 and conventional pulmonary function test or FOT from our current study, it is fair to say that airway closure is evident in some degree. Also, our previous findings showed that this action is partly due to caspase-7-mediated miR-133a-RhoA signaling [6,9].
Our study showed the degree of significant hypoxia was greater in subjects with hypercapnia as compared to normoxia than without hypercapnia. Two trials undertaken in the 1970s showed a decrease in mortality in patients with COPD and severe resting hypoxemia when receiving long-term oxygen therapy (LTOT) compared to nocturnal oxygen therapy or control [44,45]. In a more recent study from the Long-Term Oxygen Treatment Trial Research Group, patients with stable COPD and resting or exercise-induced moderate desaturation had no benefit of LTOT versus the no supplemental oxygen group in terms of mortality, exacerbations or functional status, suggesting PO2 level is not the only factor that regulate those outcomes in severe COPD [46]. The widely discussed study by Köhnlein et al. showed a dramatic improvement of 1-year mortality (12% versus 33%) in patients with hypercapnic, stable COPD when home mechanical ventilation was targeted to reduce hypercapnia, suggesting the importance of PCO2 level in treating COPD patients [47]. A recent report by Suh et al. investigated whether FOT-based auto-titration of end-expiratory pressure (EPAP) would abolish or minimize tidal-breathing expiratory flow limitation among subjects with COPD and chronic respiratory failure [48]. Although participated patients were small, what they found was that FOT-based algorithm abolished tidal-breathing expiratory flow limitation followed by minimizing transdiaphragmatic pressure swing and neural respiratory drive (NRD) in the study. It was also reported that NRD is related to PCO2 and removal of PCO2 may further reduce the mortality rate in the acute settings [17]. From our own and previous studies, an FOT-based and decreasing PCO2 approach may improve parameters of both acute and chronic settings.
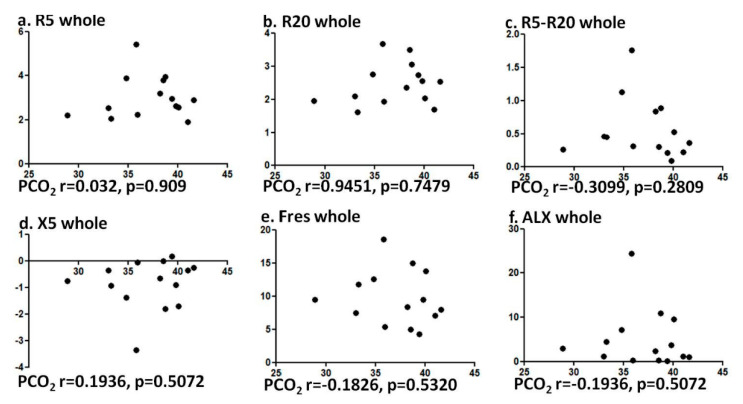
The current study has some limitations. The number of subjects enrolled in the study was not large, but large enough when compared to past studies. Although subjects’ current medication was not accounted for this study, there is not much of the study pointing out that inhaled agents, such as inhaled corticosteroids, long-acting beta-agonists, and long-acting anticholinergics, could alter the gas exchange. We cannot deny the possibility that hypoxia may affect the pulmonary function values in our subjects. Our prior study showed the role of elevated CO2 for airway contractility, independently of hypoxia [9]. This study showed that the relation between PCO2 level and FOT values in healthy volunteers was not evident (Figure 3), suggesting that changes in CO2 levels at normal PCO2 range may not affect pulmonary functions.
Figure 3.
Correlation was not observed between PCO2 and FOT values among healthy patients. Specifically, correlation between PCO2 and (a) R5, (b) R20, (c) R5-R20, (d) X5, (e) Fres, and (f) ALX were analyzed using Spearman rank correlation test.
The term ‘permissive hypercapnia’ has been proposed for a while and the strategy is currently accepted in treating patients [18,19,49]. It has been increasingly evident that elevated CO2 acts as a signaling molecule with unwanted effects on the local lung and whole body [15,47,49,50,51,52,53,54]. Further preclinical (basic) and clinical studies are warranted to define who should benefit from treating or leaving hypercapnia (for subjects with acute to chronic) in lung diseases. Since one of the targets to treat subjects with COPD is to evaluate the narrowed small airways, the current study supports targeting to correct PCO2 level as the new strategy [48] to treat subjects with COPD and hypercapnia.
Acknowledgments
Corresponding author would like to thank Sznajder JI (Northwestern University, USA) for great support for the series of studies.
Author Contributions
Conceptualization, T.U., T.H., M.S., Y.F., and H.S. (Hironori Sagara); Data curation, T.U., T.H., T.K. (Tomoyuki Kimura), C.O., and H.S. (Hiroki Sato); Formal analysis, T.U., T.H., T.K. (Tomoko Kawahara), H.S. (Hiroki Sato), K.A. (Koichi Ando), S.Y., T.E., T.M., A.K. and H.S. (Hiromitsu Suganuma); Funding acquisition, T.H., H.I. (Hideki Inoue), M.Y., and H.S. (Hironori Sagara); Investigation, T.U., T.H., K.K., H.M., H.S. (Haruna Sato), Y.U., A.F., N.K., H.I.(Hitomi Ida), R.M., K.H., Y.M., M.J., S.O., Y.K., Y.W., S.K., K.A.(Kaho Akimoto), S.S., A.T., T.O., and H.S. (Hironori Sagara); Original writing, T.U., T.H., M.S., Y.F., and H.S. (Hironori Sagara); Revision, T.U., T.H., M.S., Y.F., and H.S. (Hironori Sagara). All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported in part by JSPS KAKENHI (grant number: 18K10654 to T. Homma, 18K16160 to H. Inoue, 19K24240 to M. Yamamoto, and 20K03161 to S. Suzuki) and by the Environment Research and Technology Development Fund (year 2019 to 2021) of the Environmental Restoration and Conservation Agency of Japan.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Calverley P.M., Celli B.R., Coxson H., Edwards L., Lomas D.A., MacNee W., Miller B.E., Rennard S.I., Silverman E.C., Agustí A. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir. Res. 2010;11:122. doi: 10.1186/1465-9921-11-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Terry P.D., Dhand R. Inhalation therapy for stable COPD: 20 Years of GOLD reports. Adv. Ther. 2020;37:1812–1828. doi: 10.1007/s12325-020-01289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agustí A., Gea J., Faner R. Biomarkers, the control panel and personalized COPD medicine. Respirology. 2015;21:24–33. doi: 10.1111/resp.12585. [DOI] [PubMed] [Google Scholar]
- 4.Hirai K., Tanaka A., Homma T., Kaneko K., Uno T., Sato H., Manabe R., Ohta S., Kusumoto S., Yamaguchi F., et al. Comparison of three frailty models and a sarcopenia model in elderly patients with chronic obstructive pulmonary disease. Geriatr. Gerontol. Int. 2019;19:896–901. doi: 10.1111/ggi.13740. [DOI] [PubMed] [Google Scholar]
- 5.Singh D., Criner G.J., Naya I., Jones P.W., Tombs L., Lipson D.A., Han M.K. Measuring disease activity in COPD: Is clinically important deterioration the answer? Respir. Res. 2020;21:134. doi: 10.1186/s12931-020-01387-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shigemura M., Lecuona E., Sznajder J.I. Effects of hypercapnia on the lung. J. Physiol. 2017;595:2431–2437. doi: 10.1113/JP273781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vadász I., Hubmayr R.D., Nin N., Sporn P.H.S., Sznajder J.I. Hypercapnia: A nonpermissive environment for the lung. Am. J. Respir. Cell Mol. Boil. 2012;46:417–421. doi: 10.1165/rcmb.2011-0395PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shigemura M., Lecuona E., Angulo M., Dada L.A., Edwards M.B., Welch L.C., Casalino-Matsuda S.M., Sporn P.H.S., Vadász I., Helenius I.T., et al. Elevated CO2 regulates the Wnt signaling pathway in mammals, Drosophila melanogaster and Caenorhabditis elegans. Sci. Rep. 2019;9:1–8. doi: 10.1038/s41598-019-54683-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shigemura M., Lecuona E., Angulo M., Homma T., Rodríguez D.A., Gonzalez-Gonzalez F.J., Welch L.C., Amarelle L., Kim S.-J., Kaminski N., et al. Hypercapnia increases airway smooth muscle contractility via caspase-7-mediated miR-133a-RhoA signaling. Sci. Transl. Med. 2018;10:eaat1662. doi: 10.1126/scitranslmed.aat1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casey J.R., Grinstein S., Orlowski J. Sensors and regulators of intracellular pH. Nat. Rev. Mol. Cell Boil. 2009;11:50–61. doi: 10.1038/nrm2820. [DOI] [PubMed] [Google Scholar]
- 11.Kamenetsky M., Middelhaufe S., Bank E.M., Levin L.R., Buck J., Steegborn C. Molecular details of cAMP generation in mammalian cells: A tale of two systems. J. Mol. Boil. 2006;362:623–639. doi: 10.1016/j.jmb.2006.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamamoto M., Tochino Y., Chibana K., Trudeau J.B., Holguin F., Wenzel S. Nitric oxide and related enzymes in asthma: Relation to severity, enzyme function and inflammation. Clin. Exp. Allergy. 2011;42:760–768. doi: 10.1111/j.1365-2222.2011.03860.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weir E.K., López-Barneo J., Buckler K.J., Archer S.L. Acute oxygen-sensing mechanisms. N. Engl. J. Med. 2005;353:2042–2055. doi: 10.1056/NEJMra050002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holmes A.P., Nunes A.R., Cann M., Kumar P. Ecto-5′-nucleotidase, adenosine and transmembrane adenylyl cyclase signalling regulate basal carotid body chemoafferent outflow and establish the sensitivity to hypercapnia. Adv. Exp. Med. Biol. 2015;860:279–289. doi: 10.1007/978-3-319-18440-1_32. [DOI] [PubMed] [Google Scholar]
- 15.Vohwinkel C.U., Lecuona E., Sun H., Sommer N., Vadász I., Chandel N.S., Sznajder J.I. Elevated CO2 levels cause mitochondrial dysfunction and impair cell proliferation. J. Boil. Chem. 2011;286:37067–37076. doi: 10.1074/jbc.M111.290056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Vu G., Ha G.H., Nguyen C.T., Vu G.T., Pham H.Q., Latkin C.A., Tran B.X., Ho R., Ho C.S.H. Interventions to improve the quality of life of patients with chronic obstructive pulmonary disease: A global mapping during 1990–2018. Int. J. Environ. Res. Public Heal. 2020;17:3089. doi: 10.3390/ijerph17093089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karagiannidis C., Strassmann S., Schwarz S.B., Merten M., Fan E., Beck J., Sinderby C., Windisch W. Control of respiratory drive by extracorporeal CO2 removal in acute exacerbation of COPD breathing on non-invasive NAVA. Crit. Care. 2019;23:135. doi: 10.1186/s13054-019-2404-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hickling K.G., Walsh J., Henderson S., Jackson R. Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: A prospective study. Crit. Care Med. 1994;22:1568–1578. doi: 10.1097/00003246-199422100-00011. [DOI] [PubMed] [Google Scholar]
- 19.Amato M.B.P., Barbas C.S.V., Medeiros D.M., Magaldi R.B., Schettino G.P., Lorenzi-Filho G., Kairalla R.A., Deheinzelin D., Muñoz C., Oliveira R., et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N. Engl. J. Med. 1998;338:347–354. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 20.Hitomi Y., Tanaka A., Yasunari K., Mikuni H., Tomoko K., Ohta S., Yamamoto M., Suzuki S., Ohnishi T., Sagara H., et al. Association between respiratory impedance measured by forced oscillation technique and exacerbations in patients with COPD. Int. J. Chronic Obstr. Pulm. Dis. 2017;13:79–89. doi: 10.2147/COPD.S146669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oostveen E., Macleod D., Lorino H., Farré R., Hantos Z., Desager K., Marchal F. The forced oscillation technique in clinical practice: Methodology, recommendations and future developments. Eur. Respir. J. 2003;22:1026–1041. doi: 10.1183/09031936.03.00089403. [DOI] [PubMed] [Google Scholar]
- 22.Mori K., Shirai T., Mikamo M., Shishido Y., Akita T., Morita S., Asada K., Fujii M., Hozumi H., Suda T., et al. Respiratory mechanics measured by forced oscillation technique in combined pulmonary fibrosis and emphysema. Respir. Physiol. Neurobiol. 2013;185:235–240. doi: 10.1016/j.resp.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 23.Dubois A.B., Brody A.W., Lewis D.H., Burgess B.F. Oscillation mechanics of lungs and chest in man. J. Appl. Physiol. 1956;8:587–594. doi: 10.1152/jappl.1956.8.6.587. [DOI] [PubMed] [Google Scholar]
- 24.Lipworth B.J., Jabbal S. What can we learn about COPD from impulse oscillometry? Respir. Med. 2018;139:106–109. doi: 10.1016/j.rmed.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Shirai T., Mori K., Mikamo M., Shishido Y., Akita T., Morita S., Asada K., Fujii M., Suda T., Chida K. Respiratory mechanics and peripheral airway inflammation and dysfunction in asthma. Clin. Exp. Allergy. 2013;43:521–526. doi: 10.1111/cea.12083. [DOI] [PubMed] [Google Scholar]
- 26.Fujii M., Shirai T., Mori K., Mikamo M., Shishido Y., Akita T., Morita S., Asada K., Suda T. Inspiratory resonant frequency of forced oscillation technique as a predictor of the composite physiologic index in interstitial lung disease. Respir. Physiol. Neurobiol. 2015;207:22–27. doi: 10.1016/j.resp.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 27.Paredi P., Goldman M., Alamen A., Ausin P., Usmani O.S., Pride N.B., Barnes P.J. Comparison of inspiratory and expiratory resistance and reactance in patients with asthma and chronic obstructive pulmonary disease. Thorax. 2010;65:263–267. doi: 10.1136/thx.2009.120790. [DOI] [PubMed] [Google Scholar]
- 28.Zimmermann S.C., Huvanandana J., Nguyen C.D., Bertolin A., Watts J.C., Gobbi A., Farah C.S., Peters M.J., Dellaca R.L., King G.G., et al. Day-to-day variability of forced oscillatory mechanics for early detection of acute exacerbations in COPD. Eur. Respir. J. 2020:1901739. doi: 10.1183/13993003.01739-2019. [DOI] [PubMed] [Google Scholar]
- 29.Zannin E., Nyilas S., Ramsey K., Latzin P., Dellaca R.L. Within-breath changes in respiratory system impedance in children with cystic fibrosis. Pediatr. Pulmonol. 2019;54:737–742. doi: 10.1002/ppul.24281. [DOI] [PubMed] [Google Scholar]
- 30.Kregenow D.A., Rubenfeld G.D., Hudson L.D., Swenson E.R. Hypercapnic acidosis and mortality in acute lung injury. Crit. Care Med. 2006;34:1–7. doi: 10.1097/01.CCM.0000194533.75481.03. [DOI] [PubMed] [Google Scholar]
- 31.American Thoracic Society Standardization of spirometry, 1994. Am. J. Respir. Crit. Care Med. 1995;152:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 32.Brashier B., Salvi S. Measuring lung function using sound waves: Role of the forced oscillation technique and impulse oscillometry system. Breathe. 2015;11:57–65. doi: 10.1183/20734735.020514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vogelmeier C.F., Criner G.J., Martinez F.J., Anzueto A., Barnes P.J., Bourbeau J., Celli B.R., Chen R., Decramer M., Fabbri L.M., et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am. J. Respir. Crit. Care Med. 2017;195:557–582. doi: 10.1164/rccm.201701-0218PP. [DOI] [PubMed] [Google Scholar]
- 34.Galant S.P., Komarow H.D., Shin H.-W., Siddiqui S., Lipworth B.J., Hye-Won S. The case for impulse oscillometry in the management of asthma in children and adults. Ann. Allergy Asthma Immunol. 2017;118:664–671. doi: 10.1016/j.anai.2017.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nair A., Ward J., Lipworth B.J. Comparison of bronchodilator response in patients with asthma and healthy subjects using spirometry and oscillometry. Ann. Allergy Asthma Immunol. 2011;107:317–322. doi: 10.1016/j.anai.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 36.Rentzhog C.H., Janson C., Berglund L., Borres M.P., Nordvall L., Alving K., Malinovschi A. Overall and peripheral lung function assessment by spirometry and forced oscillation technique in relation to asthma diagnosis and control. Clin. Exp. Allergy. 2017;47:1546–1554. doi: 10.1111/cea.13035. [DOI] [PubMed] [Google Scholar]
- 37.Mori K., Shirai T., Mikamo M., Shishido Y., Akita T., Morita S., Asada K., Fujii M., Suda T., Chida K. Colored 3-dimensional analyses of respiratory resistance and reactance in COPD and asthma. COPD J. Chronic Obstr. Pulm. Dis. 2011;8:456–463. doi: 10.3109/15412555.2011.626818. [DOI] [PubMed] [Google Scholar]
- 38.Matsumoto H., Niimi A., Jinnai M., Nakaji H., Takeda T., Oguma T., Otsuka K., Inoue H., Yamaguchi M., Matsuoka H., et al. Association of alveolar nitric oxide levels with pulmonary function and its reversibility in stable asthma. Respiration. 2011;81:311–317. doi: 10.1159/000319566. [DOI] [PubMed] [Google Scholar]
- 39.Williamson P.A., Clearie K., Menzies D., Vaidyanathan S., Lipworth B.J. Assessment of small-airways disease using alveolar nitric oxide and impulse oscillometry in asthma and COPD. Lung. 2010;189:121–129. doi: 10.1007/s00408-010-9275-y. [DOI] [PubMed] [Google Scholar]
- 40.Wei X., Shi Z., Cui Y., Mi J., Ma Z., Ren J., Li J., Xu S., Guo Y.-M. Impulse oscillometry system as an alternative diagnostic method for chronic obstructive pulmonary disease. Medicine. 2017;96:e8543. doi: 10.1097/MD.0000000000008543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Crim C., Celli B.R., Edwards L., Wouters E., Coxson H.O., Tal-Singer R., Calverley P.M. Respiratory system impedance with impulse oscillometry in healthy and COPD subjects: ECLIPSE baseline results. Respir. Med. 2011;105:1069–1078. doi: 10.1016/j.rmed.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 42.Haruna A., Oga T., Muro S., Ohara T., Sato S., Marumo S., Kinose D., Terada K., Nishioka M., Ogawa E., et al. Relationship between peripheral airway function and patient-reported outcomes in COPD: A cross-sectional study. BMC Pulm. Med. 2010;10:10. doi: 10.1186/1471-2466-10-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frantz S., Nihlen U., Dencker M., Engstrom G., Lofdahl C.G., Wollmer P. Impulseoscillometry may be of value in detecting early manifestations of COPD. Respir. Med. 2012;106:1116–1123. doi: 10.1016/j.rmed.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 44.Nocturnal Oxygen Therapy Trial Group Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: A clinical trial. Ann. Intern. Med. 1980;93:391–398. doi: 10.7326/0003-4819-93-3-391. [DOI] [PubMed] [Google Scholar]
- 45.Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Report of the Medical Research Council Working Part. Lancet. 1981;317:681–686. doi: 10.1016/s0140-6736(81)91970-x. [DOI] [PubMed] [Google Scholar]
- 46.Long-Term Oxygen Treatment Trial Research Group. Albert R.K., Au D.H., Blackford A.L., Casaburi R., Cooper J.A., Criner G.J., Diaz P., Fuhlbrigge A.L., Gay S.E., et al. A randomized trial of long-term oxygen for COPD with moderate desaturation. N. Engl. J. Med. 2016;375:1617–1627. doi: 10.1056/nejmoa1604344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Köhnlein T., Windisch W., Köhler D., Drabik A., Geiseler J., Hartl S., Karg O., Laier-Groeneveld G., Nava S., Schönhofer B., et al. Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: A prospective, multicentre, randomised, controlled clinical trial. Lancet Respir. Med. 2014;2:698–705. doi: 10.1016/S2213-2600(14)70153-5. [DOI] [PubMed] [Google Scholar]
- 48.Suh E.S., Pompilio P., Mandal S., Hill P., Kaltsakas G., Murphy P.B., Romano R., Moxham J., Dellaca R., Hart N. Auto-titrating external positive end-expiratory airway pressure to abolish expiratory flow limitation during tidal breathing in patients with severe chronic obstructive pulmonary disease: A physiological study. Eur. Respir. J. 2020 doi: 10.1183/13993003.02234-2019. [DOI] [PubMed] [Google Scholar]
- 49.Contreras M., Masterson C., Laffey J. Permissive hypercapnia. Curr. Opin. Anaesthesiol. 2015;28:26–37. doi: 10.1097/ACO.0000000000000151. [DOI] [PubMed] [Google Scholar]
- 50.Vadász I., Dada L.A., Briva A., Trejo H.E., Welch L.C., Chen J., Toth P.T., Lecuona E., Witters L.A., Schumacker P.T., et al. AMP-activated protein kinase regulates CO2-induced alveolar epithelial dysfunction in rats and human cells by promoting Na,K-ATPase endocytosis. J. Clin. Investig. 2008;118:752–762. doi: 10.1172/JCI29723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gates K.L., Howell H.A., Nair A., Vohwinkel C.U., Welch L.C., Beitel G.J., Hauser A.R., Sznajder J.I., Sporn P.H.S. Hypercapnia impairs lung neutrophil function and increases mortality in murine pseudomonas pneumonia. Am. J. Respir. Cell Mol. Boil. 2013;49:821–828. doi: 10.1165/rcmb.2012-0487OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Casalino-Matsuda S.M., Nair A., Beitel G.J., Gates K.L., Sporn P.H.S. Hypercapnia inhibits autophagy and bacterial killing in human macrophages by increasing expression of Bcl-2 and Bcl-xL. J. Immunol. 2015;194:5388–5396. doi: 10.4049/jimmunol.1500150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dada L.A., Bittar H.E.T., Welch L.C., Vagin O., Deiss-Yehiely N., Kelly A.M., Baker M.R., Capri J., Cohn W., Whitelegge J.P., et al. High CO2Leads to Na,K-ATPase endocytosis via c-Jun amino-terminal kinase-induced LMO7b phosphorylation. Mol. Cell. Boil. 2015;35:3962–3973. doi: 10.1128/MCB.00813-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bharat A., Graf N., Mullen A., Kanter J., Andrei A.-C., Sporn P.H.S., DeCamp M.M., Sznajder J.I. Pleural hypercarbia after lung surgery is associated with persistent alveolopleural fistulae. Chest. 2016;149:220–227. doi: 10.1378/chest.15-1591. [DOI] [PMC free article] [PubMed] [Google Scholar]