HIGHLIGHTS
-
•
Can PEARLS, a brief, home-based intervention focused on problem solving treatment and behavioral activation for low-income older adults living with depression, improve social connectedness for underserved older populations?
-
•
PEARLS participants significantly improved on all three social connectedness constructs (social interactions and satisfaction with social support; perceived isolation; loneliness) 6-months after PEARLS enrollment. Though most improvements persisted during early COVID-19 pandemic, additional supports may be needed for older persons with complex health and social needs.
-
•
PEARLS is a promising intervention for increasing social connectedness among underserved older adults living with depression.
Key Words: Social isolation, loneliness, depression care management, underserved, community
Abstract
Objective
To evaluate PEARLS effectiveness for increasing social connectedness among underserved older adults with depression.
Design
Multisite, pre-post single-group evaluation.
Setting
Community-based social service organizations (N = 16) in five U.S. states, purposively sampled for maximum variation of participants and providers.
Participants
A total of 320 homebound older adults (mean(SD) age 72.9(9.6), 79% female, 44% people of color, 81% low-income, 61% living alone, average four chronic conditions) with clinically significant depression (PHQ-9 mean(SD) 12.7(4.6)).
Intervention
Four to 6 month home-based depression care management model delivered by trained front-line providers.
Measurements
Brief validated social connectedness scales: Duke Social Support Index 10-item (DSSI-10), PROMIS-Social Isolation (6-item), UCLA-Loneliness (3-item); sociodemographic and health measures.
Results
At baseline, PEARLS participants overall and with ≥1 of the following characteristics were less socially connected: younger (50–64), white, LGBTQ+, not partnered, not caregiving, living alone, financial limitations, chronic conditions, and/or recently hospitalized. Six-months post-PEARLS enrollment, participants significantly increased social interactions and satisfaction with social support (DSSI-10 t[312] = 5.2, p <0.001); and reduced perceived isolation (PROMIS t[310] = 6.3, p <0.001); and loneliness (UCLA t[301] = 3.7, p =0.002), with small to moderate effect sizes (Cohen's d DSSI-10: 0.28, PROMIS-SI: 0.35, UCLA: 0.21). Increased social connectedness was associated with reduced depression. Improvements in social connectedness (except social interactions) persisted during early COVID-19. Being Latino and/or having difficulty paying for basic needs was associated with less improvement in post-PEARLS social connectedness.
Conclusion
PEARLS has potential to improve social connectedness among underserved older adults, though additional supports may be needed for persons facing multiple social determinants of health. Further research is needed to establish causality.
OBJECTIVE
Social isolation and loneliness have emerged as significant health concerns for older adults, increasing their risk of early death, cognitive decline, poor health and well-being,1 and costs of health care.2 While often conflated, these are distinct health concerns: Social isolation is an objective measure of social ties and activities, while loneliness is a subjective assessment of the disconnect between perceived and ideal social connections.3 , 4 The overarching term “social connectedness” is now used to encompass the “structural, functional, and qualitative aspects of social relationships,” including social isolation and loneliness.5
Late-life depression is another pressing public health concern that impacts quality of life, function, management of other chronic conditions, and risk of death.6 Depression and low social connectedness are distinct yet related issues, with each being a risk factor and a consequence of the other.7 Qualitative aspects of relationships (e.g., lack of social support, absence of confidants) have been significantly associated with depression, whereas quantitative aspects (e.g., living alone, size of social network) show less consistent associations.8 Isolation and loneliness stemming from role changes in later life—retirement, job loss, full-time caregiving, limited mobility and function—are key risk factors for depression.9 A recent review10 found “social isolation/loneliness” was the most common depression symptom not in the Diagnostic Statistical Manual (DSM-V).11
Low social connectedness among older adults is often described as an emerging public health epidemic, yet little is known about how to effectively treat it. What is known is that older adults who are underserved by healthcare and other institutions —including Black, Indigenous, and other people of color (BIPOC); those living in poverty, homebound, and/or in rural communities—are at increased risk for both low social connectedness12 and depression.13 Therefore, it is essential that interventions be designed and delivered to effectively reach these underserved communities.14
PEARLS (Program to Encourage Active, Rewarding Lives) is an evidence-based intervention designed to reduce depression among homebound older adults who receive social services and are often underserved by healthcare systems.15 Many PEARLS participants report causes of social disconnect common among older adults, including poor health and well-being; life transitions, loss, role changes; and social determinants of health such as ageism, racism, and poor access to resources. Brief, person-centered, home-based, behavioral interventions like PEARLS could improve social connectedness for underserved older adults by enhancing participants’ sense of purpose and control, and could be tailored to address different causes for disconnect (e.g., lack of social support or meaningful social interactions).16 , 17
This study evaluates whether PEARLS participants improve social connectedness over time. Specifically:
-
1.
What is the magnitude of low social connectedness among older adults living with depression who participate in PEARLS?
-
2.
Do PEARLS participants improve their social connectedness after program participation? What sociodemographic and health factors are associated with improvements in social connectedness?
-
3.
Are improvements in social connectedness related to improvements in depression?
This research helps fill current evidence gaps about interventions to improve social connectedness among older adults. Our focus on older adults receiving social services aligns with public health's call to prioritize underserved populations to achieve health for all.18
METHODS
Design
We used a single group, multisite, pre-post evaluation design. We applied PRECIS (Pragmatic-Explanatory Continuum Indicator Summary Model)19 to gather pragmatic evidence on PEARLS as a social connectedness intervention. This study was determined exempt from UW Institutional Review Board review as activities fell under quality improvement and program evaluation.
Participants and Setting
PEARLS is offered by community-based social service organizations (Area Agencies on Aging, community centers, organizations representing specific cultural groups) to support aging in place among older adults with financial or other limitations. We used maximum variation purposive sampling20 to select a variety of organizations and providers (e.g., social workers, counselors, and community health workers) offering PEARLS in urban and rural contexts to older adults from diverse racial and ethnic backgrounds, with a preference for speaking English or Spanish. We partnered with 16 PEARLS organizations in five U.S. states (WA, TX, NY, MD, FL). Within each organization, all who enrolled in PEARLS during our study period were invited to participate. PEARLS participants are primarily low-income older adults (age >/= 50) with clinically significant depressive symptoms (Patient Health Questionnaire 9-item depression measure (PHQ-9)21 who meet DSM criteria for minor or major depression or persistent depressive disorder.11 Adults with significant cognitive impairment, functionally impairing substance use disorder, or severe mental illness are ineligible for PEARLS.
Intervention
PEARLS was co-created and tested in a community-academic partnership to reach underserved homebound older adults.15 PEARLS trains front-line providers (e.g., case managers, community health workers) from social service safety-net organizations engaging communities with poor access to traditional clinical care. In eight 1-hour home-visits over a 4-to-6-month period, PEARLS providers (“coaches” or “counselors”) meet one-on-one with participants. They help participants build problem-solving skills to gain a sense of control over overwhelming issues in their lives (Problem Solving Treatment [PST]),22 and plan meaningful and accessible physical, social, and pleasant activities (Behavioral Activation).23 Providers also offer psychoeducation (information and support to better understand and cope with depression) and linkages to social and health services when needed. A clinical supervisor (e.g., psychiatrist or other clinician) provides regular oversight and consultation for older adults with complex health needs. Regular clinical supervision provides built-in fidelity assessment, and previous research found consistent fidelity among different provider types.24
Data Collection
Our recruitment of PEARLS organizations and their recruitment of PEARLS participants occurred on a rolling basis. Organizations collected baseline social connectedness data from participants between January 2018 and September 2019. Our study team collected follow-up data by phone 6 months after PEARLS enrollment (timed to align with program completion) between June 2018 and May 2020. While not optimal to collect data using two modalities (in-person versus phone; provider versus researcher), this protocol was designed to collect real-time quality data from underserved communities.
The same multiscale assessment of social connectedness was used at baseline and follow-up. At follow-up our study team also collected sociodemographic, health, and program satisfaction items, and participants received a $20 incentive. Bilingual, bicultural PEARLS providers collected baseline surveys in Spanish when appropriate, and bilingual/bicultural study staff collected Spanish-language follow-up surveys. PEARLS organizations and study staff had a protocol for immediately supporting distressed or suicidal participants, and a geriatric psychiatrist available for consultation.
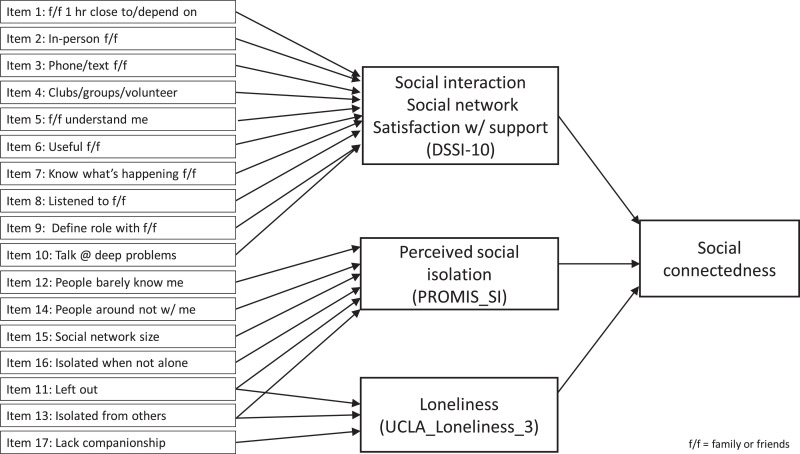
Social connectedness measures
We selected instruments that measure different constructs of social connectedness (Fig. 1 ) and are valid and reliable with older adults.25, 26, 27 Lower scores indicate lower social connectedness; we recoded PROMIS-SI and UCLA-Loneliness for interpretability across scales.
Duke Social Support Index (DSSI-10) 25: 10-item measure (range 10–30) derived from DSSI-35.28 Consists of two subscales: social interactions (DSSI-SI; 4 items) and satisfaction with social support (DSSI-SS; 6-items); we used the latter for sensitivity analysis as the SI subscale is unreliable. While the validation paper25 reported mean(SD) of 24.4 (3.3), no cut-off has been established for social isolation.
Patient-Reported Outcomes Measurement Information System Social Isolation (PROMIS-SI) 29: 6-item scale for perceived isolation (being avoided, excluded, detached, disconnected from, or unknown by others) (range 6–30). A raw score of 13 is average for U.S. adults with chronic conditions.
UCLA-Loneliness 26: 3-item scale (range 3–9) of relational connectedness, social connectedness, and self-perceived isolation; derived from UCLA-20.30 Recoded scores </= 6 suggest being “lonely.”31
FIGURE 1.
Diagram of the conceptual framework for social connectedness measures.
We piloted these measures with 20 PEARLS participants in Fall 2017, afterwards modifying the DSSI-10 (with permission from Dr. George, personal communication, November 2017) to add texting, Facebook and other social media to phone contacts, and changing “family and friends” to “family or friends.”
Other measures
We collected sociodemographic and health data to characterize our sample and understand which factors were associated with changes in social connectedness. These were identified from recent literature on risk factors and consequences of social disconnectedness among older adults.1 , 3 , 5 , 8 , 32 We also asked participants why they would/would not recommend PEARLS to family or friends in an open-ended survey question. During analysis, we created a variable to indicate whether follow-up surveys were collected before/after COVID-19 onset (March 1, 2020) given physical distancing and shelter-at-home guidelines may act as an exogenous covariate.
Analysis
Our three social connectedness scales had good reliability (internal consistency) with Cronbach's alphas 0.76, 0.88, 0.77 for DSSI-10, PROMIS-SI, and UCLA-Loneliness, respectively. Construct validity was established through moderate-strong item and scale pairwise correlations, and convergent validity was demonstrated by statistically significant correlations with age, chronic conditions, and the PHQ-9. Participants with >1 missing item on the baseline or follow-up DSSI-10 (7:320, 2.2%) and PROMIS-SI (10:320, 3.2%), and >/=1 missing item on the UCLA-Loneliness (19:320, 5.9%) were recoded as missing and not included in analyses using that scale. We did not conduct imputation, given the small proportion of missingness.
We used REDCap33 for data management and Stata 15.1 for analysis. We ran descriptive statistics to summarize sample characteristics including social connectedness. We used paired t tests to statistically test whether there was a change in social connectedness pre-post PEARLS, and Cohen's d effect sizes to evaluate the magnitude of change. We used unadjusted and adjusted regression models to identify factors associated with improvements in social connectedness. Regression results are reported using unstandardized slope estimates (B coefficients and their 95% confidence intervals [CI]), the t-statistic (t), and p-value. Our p-value threshold is 0.05 for statistical significance, recognizing tests of statistical significance should be interpreted cautiously due to potential problems with multiple testing. We used Bonferroni correction to adjust p-values (0.05/3 = 0.017) for the three paired t tests and three adjusted regression models. We conducted thematic analyses34 of open-ended survey items about reasons for recommending PEARLS to describe possible mechanisms by which PEARLS participants improved their social connectedness.
RESULTS
Participation
Baseline surveys were completed by 854 of 1,149 (74.3%) PEARLS participants in study partner organizations. Over the course of PEARLS, 44.7% (382:854) of study participants dropped out of PEARLS: 202 (53%) for lack of interest, 63 (16%) due to illness, 19 (5%) moved out of area, and 98 (26%) for reasons not specified. Of the 472 baseline survey participants who completed PEARLS, 320 (68%) completed post-PEARLS surveys. Of those who completed PEARLS and did not complete a post-PEARLS survey, 40% (61:152) declined to complete the survey and 60% (91:152) were unreachable after multiple contact attempts. We conducted an attrition analysis to examine the magnitude of differences between pre- and post-PEARLS survey participants (Appendix Table 1). Both groups had similar levels of social connectedness, depression, self-rated health, and past/current mental health treatment at baseline. More post-PEARLS nonrespondents had recent hospitalizations and were sedentary at baseline, and fewer non-respondents found it hard to pay for basic needs or were providing caregiving. We did not conduct statistical testing, which is only appropriate for testing hypotheses about group differences.
Our final study sample (N = 320) includes older populations who are underserved in terms of race/ethnicity, poverty, living alone, caregiving, and health (Table 1 ).
TABLE 1.
Participant Demographics for PEARLS Pre-Post Social Connectedness Evaluation (N = 320)
| % | n | % | n | ||
|---|---|---|---|---|---|
| Age (Mean SD) (range 50–96) | 72.6 | 9.6 | < 250% Federal Poverty Level | 80.9 | 229 |
| Female | 79.1 | 253 | Basic needs (food, housing, heating) | ||
| Somewhat hard to pay for basics | 35.0 | 112 | |||
| Race and Ethnicity | Very hard to pay for basics | 35.6 | 114 | ||
| White | 56.0 | 179 | |||
| Black | 20.6 | 66 | Occupation - % not working/retiredd | 95.3 | 301 |
| Latino a | 18.9 | 60 | |||
| Other b | 3.8 | 12 | Caregiving in last 12 months | 31.4 | 100 |
| Care for adults with dementia | 45.6 | 41 | |||
| LGBTQ | 6.1% | 19 | Live with care partner | 44.4 | 44 |
| Was paid for caregiving | 7.0 | 7 | |||
| Rural (RUCA zip) | 7.2 | 23 | Mean (SD) caregiving hours/week | 69.9 | 67.4 |
| Relationship status | Poor/fair self-rated health | 64.6 | 203 | ||
| Married/Partnered | 19.4 | 62 | |||
| Widowed | 28.4 | 91 | Chronic conditions (CC) | ||
| Divorced | 5.0 | 16 | Mean (SD) chronic conditions | 4.2 | 2.0 |
| Separated | 27.2 | 87 | >/=2 chronic conditions (“multiple”) | 93.2 | 298 |
| Single (Never Married/Partnered) | 20.0 | 64 | 5 or more chronic conditions | 42.5 | 136 |
| Living status | Lung disease (e.g., asthma) | 29.4 | 94 | ||
| Live alone | 60.8 | 194 | Joint problems (e.g., arthritis) | 70.3 | 225 |
| Live with spouse/partner | 13.5 | 43 | Cancer | 13.4 | 43 |
| Live with other family | 22.6 | 72 | Diabetes | 36.1 | 115 |
| Live with friends/other people | 3.2 | 10 | Digestive problems (e.g., ulcer) | 34.7 | 111 |
| Heart problems (e.g. angina, CHF) | 40 | 128 | |||
| Live with pets | 40.1 | 127 | Hypertension | 61.8 | 197 |
| HIV/AIDS | 1.3 | 4 | |||
| Education | Kidney disease | 18.8 | 60 | ||
| Less than high school/GED | 17.5 | 56 | Liver problems (e.g. cirrhosis) | 5.4 | 17 |
| High school graduate / GED | 23.4 | 75 | Neurological (e.g. Parkinson's) | 13.8 | 44 |
| Some college | 29.4 | 94 | Stroke | 20.0 | 64 |
| College graduate | 18.1 | 58 | Mental health conditions e | 76.0 | 241 |
| Graduate school | 11.6 | 37 | |||
| Mean (SD) PHQ-9 depression score | 12.6 | 4.9 | |||
| Income c | PHQ-9 >/= 10 | 73.8 | 236 | ||
| < $30,000 (household size = 1) | 80.3 | 155 | |||
| < $40,000 (household size = 2) | 61.8 | 47 | Access to health care | ||
| < $51,000 (household size = 3) | 70.4 | 19 | Hospitalized in the last 3 months | 21.6 | 69 |
| < $61,000 (household size = 4) | 40.0 | 4 | Did not see PCP in the last 3 mo. | 20.9 | 67 |
| < $71,000 (household size = 5) | 40.0 | 2 | Mean (SD) doctor visits last 3 mo. | 2 | 3.8 |
| < $82,000 (household size = 6) | 50 | 2 |
Notes:N (%) unless otherwise noted. Mean (SD) is in italics. AIDS: acquired immunodeficiency syndrome; CC: chronic conditions; CHF: congestive heart failure; GED: general educational development; HIV: human-immunodeficiency virus; LGBTQ+: Lesbian, Gay, Bisexual, Transgender, Queer or Questioning, and other sexual identities. PCP: primary care provider; PHQ-9: Patient Health Questionnaire 9-item; RUCA: rural urban commuting area; SD: standard deviation.
Latino includes 36.7% Puerto Rican, 18.3% Dominican, 30% Other Latino countries in North, Central, and South America, 15% country of origin not specified.
Other Race/Ethnicity includes participants who identified as Asian or American Indian/Alaskan Native.
The denominator is different for each income question as participants were only asked one income question based on their household size.
Includes persons not working due to disabilities and/or retired.
While all PEARLS participants have clinically significant depressive symptoms, some do not have an official depression diagnosis.
Baseline Magnitude of Low Social Connectedness and Associated Factors
PEARLS participants’ baseline social connectedness is reported in Table 2 . Overall, mean(SD) scale scores suggest lower social interaction and satisfaction with social support (DSSI-10) and higher perceived isolation (PROMIS-SI) than population averages referenced above. The mean(SD) score on the UCLA-Loneliness scale (6.1(2.2)) falls right at the cut off (</=6) for being lonely. Older adults who were younger (50–64), white, LGBTQ+, not married/partnered, not caregivers, living alone, living in poverty, or having difficulty paying for basic needs were less socially connected across all three scales. PEARLS participants who were recently hospitalized and/or had more chronic conditions were less socially connected across all three scales. Lower social connectedness was most pronounced for those living with higher depression severity (PHQ-9 scores). These magnitudes of difference are reported descriptively due to concerns about Type 1 errors from multiple testing.
TABLE 2.
Baseline Social Connectedness by Sociodemographic Items for Older Adults With Clinically Significant Depression (N = 320)
| DSSI-10 |
PROMIS-SI |
UCLA-Loneliness |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | N | 95% CI | Mean (SD) | N | 95% CI | Mean (SD) | N | 95% CI | |
| Age | |||||||||
| 50–64 | 20.3 (3.8) | 63 | 19.4–21.2 | 17.8 (6.0) | 62 | 16.3–19.3 | 5.4 (2.1) | 61 | 4.9–6.0 |
| 65–79 | 21.3 (4.3) | 173 | 20.6–21.9 | 20.6 (6.4) | 170 | 19.7–21.6 | 6.2 (2.3) | 165 | 5.9–6.6 |
| 80–96 | 21.9 (3.9) | 76 | 21.0–22.8 | 22.0 (6.4) | 76 | 20.5–23.4 | 6.5 (2.1) | 75 | 6.0–7.0 |
| Gender | |||||||||
| Female | 21.3 (4.1) | 247 | 20.8–21.8 | 20.1 (6.7) | 244 | 19.3–21.0 | 6.0 (2.2) | 238 | 5.7–6.3 |
| Male | 21.0 (4.1) | 64 | 20.0–22.0 | 21.1 (5.6) | 63 | 19.8–22.6 | 6.5 (2.1) | 62 | 6.0–7.1 |
| Race and Ethnicity | |||||||||
| White | 21.0 (4.2) | 165 | 20.3–21.6 | 19.5 (6.3) | 162 | 18.6–20.5 | 5.8 (2.2) | 157 | 5.4–6.1 |
| Black | 21.8 (3.6) | 64 | 20.9–22.6 | 21.2 (6.0) | 62 | 19.7–22.7 | 6.5 (2.0) | 62 | 6.0–7.0 |
| Latino a | 21.3 (4.7 | 46 | 20.0–22.7 | 21.7 (7.5) | 48 | 19.6–23.8 | 6.6 (2.3) | 47 | 6.0–7.3 |
| Other b | 21.0 (3.7) | 30 | 19.7–22.4 | 20.9 (6.9) | 30 | 18.4–23.4 | 6.1 (2.4) | 28 | 5.3–7.0 |
| Sexual Orientation | |||||||||
| LGBTQ | 19.1 (4.2) | 19 | 17.2–21.0 | 18.7 (5.8) | 19 | 16.1–21.4 | 5.0 (2.0) | 18 | 4.1–5.9 |
| Straight | 21.4 (4.1) | 288 | 20.9–21.9 | 20.5 (6.5) | 284 | 19.8–21.3 | 6.2 (2.2) | 278 | 5.9–6.5 |
| Relationship status | |||||||||
| Married/Partnered | 22.5 (3.9) | 60 | 21.5–23.5 | 22.7 (5.7) | 60 | 21.3–24.2 | 7.1 (1.9) | 59 | 6.6–7.6 |
| Widowed | 20.7 (4.3) | 89 | 19.8–21.6 | 20.1 (6.8) | 86 | 18.7–21.5 | 6.0 (2.3) | 85 | 5.5–6.5 |
| Separated | 21.1 (3.8) | 16 | 19.2–22.9 | 17.5 (6.1) | 15 | 14.4–20.6 | 5.8 (2.5) | 13 | 4.5–7.2 |
| Divorced | 21.5 (4.1) | 85 | 20.6–22.3 | 19.7 (6.5) | 84 | 18.3–21.1 | 5.7 (2.2) | 83 | 5.2–6.2 |
| Single (Never Married/Partnered) | 20.5 (4.0) | 63 | 19.5–21.5 | 20.3 (6.5) | 64 | 18.7–21.9 | 6.0 (2.1) | 62 | 5.5–6.5 |
| Living status | |||||||||
| Live alone | 21.0 (4.2) | 189 | 20.4–21.6 | 20.0 (6.6) | 185 | 19.1–21.0 | 5.9 (2.2) | 182 | 5.6–6.2 |
| Live with spouse/partner | 22.3 (3.9) | 41 | 21.1–23.5 | 21.5 (6.1) | 41 | 19.6–23.4 | 6.7 (2.1) | 41 | 6.0–7.3 |
| Live with other family | 21.5 (3.8) | 71 | 20.6–22.4 | 20.8 (6.5) | 72 | 19.2–22.3 | 6.3 (2.2) | 69 | 5.8–6.8 |
| Live with friends | 21.8 (4.4) | 6 | 18.3–25.3 | 18.7 (7.2) | 6 | 12.9–24.4 | 5.2 (2.6) | 5 | 2.9–7.5 |
| Live with other people | 16.5 (5.3) | 4 | 11.3–21.7 | 21.3 (6.5) | 3 | 13.9–28.7 | 5.7 (1.2) | 3 | 4.4–7.0 |
| Lives with Pets | |||||||||
| No | 21.2 (4.1) | 187 | 20.6–21.8 | 20.4 (6.5) | 185 | 19.4–21.3 | 6.0 (2.2) | 184 | 5.7–6.3 |
| Yes | 21.3 (4.2) | 123 | 20.6–22.1 | 20.46.6) | 121 | 19.2–21.6 | 6.2 (2.3) | 116 | 5.8–6.7 |
| Education | |||||||||
| Less than high school/GED | 21.5 (3.5) | 29 | 20.2–22.8 | 20.1 (7.5) | 29 | 17.4–22.9 | 6.4 (2.3) | 30 | 5.5–7.2 |
| Some high school/GED | 20.8 (4.4) | 24 | 19.1–22.6 | 19.6 (6.6) | 24 | 17.0–22.3 | 6.3 (2.0) | 23 | 5.5–7.1 |
| High school graduate/GED | 20.9 (3.9) | 75 | 20.0–21.8 | 20.1 (6.1) | 72 | 18.7–21.5 | 6.0 (2.2) | 71 | 5.5–6.5 |
| Some college | 21.0 (4.5) | 94 | 20.1–21.9 | 20.4 (6.5) | 94 | 19.1–21.8 | 6.2 (2.3) | 89 | 5.7–6.7 |
| College graduate | 21.8 (3.9) | 57 | 20.8–22.8 | 21.1 (7.1) | 56 | 19.2–22.9 | 5.9 (2.3) | 56 | 5.3–6.6 |
| Post-college | 21.8 (4.3) | 34 | 20.3–23.2 | 20.5 (5.5) | 34 | 18.7–22.4 | 6.1 (2.1) | 33 | 5.3–6.8 |
| Low-income | |||||||||
| No | 22.4 (4.2) | 53 | 21.2–23.5 | 21.4 (6.3) | 52 | 19.7-23.1 | 6.2 (2.3) | 51 | 5.5–6.8 |
| Yes | 21.0 (4.1) | 225 | 20.5–21.5 | 20.1 (6.6) | 220 | 19.3–21.0 | 6.1 (2.2) | 216 | 5.8–6.4 |
| Ability to pay for basic needs | |||||||||
| Not hard at all | 22.2 (3.9) | 90 | 21.4–23.0 | 22.1 (6.3) | 91 | 20.8–23.4 | 6.6 (2.1) | 87 | 6.2–7.0 |
| Somewhat hard | 21.5 (4.2) | 109 | 20.7–22.2 | 21.1 (6.0) | 107 | 20.0–22.3 | 6.4 (2.1) | 105 | 6.0–6.8 |
| Very hard | 20.2 (4.1) | 113 | 19.5–21.0 | 18.3 (6.6) | 110 | 19.5 | 5.5 (2.3) | 109 | 5.1–5.9 |
| Caregiving in last 12 months | |||||||||
| No | 20.8 (4.1) | 213 | 20.2–21.3 | 20.3 (6.5) | 209 | 19.4–21.1 | 6.1 (2.2) | 204 | 5.7–6.4 |
| Yes | 22.3 (3.9) | 99 | 21.5–23.1 | 20.8 (6.5) | 99 | 19.5–22.0 | 6.3 (2.2) | 97 | 5.9–6.7 |
| Care for persons with dementia | |||||||||
| No | 21.7 (3.7) | 48 | 20.6–22.8 | 21.1 (6.5) | 48 | 19.3–23.0 | 6.5 (2.1) | 48 | 6.0–7.1 |
| Yes | 22.5 (4.2) | 41 | 21.2–23.8 | 20 (6.7) | 41 | 17.9–22.1 | 5.9 (2.3) | 39 | 5.1–6.6 |
| Live with care partner | |||||||||
| No | 22.2 (3.8) | 54 | 21.2–23.2 | 21.3 (6.9) | 54 | 19.4–23.1 | 6.5 (2.2) | 54 | 5.9–7.1 |
| Yes | 22.3 (4.1) | 44 | 21.1–23.6 | 20.0 (5.9) | 44 | 18.2–21.7 | 6.0 (2.1) | 42 | 5.3–6.6 |
| DSSI-10 | PROMIS-SI | UCLA-Loneliness | |||||||
| Mean (SD) | N | 95% CI | Mean (SD) | N | 95% CI | Mean (SD) | N | 95% CI | |
| Chronic conditions | |||||||||
| No chronic conditions (CC) | 23.5 (2.9) | 4 | 20.7–26.3 | 22.0 (8.4) | 4 | 13.8–30.2 | 7.3 (2.1) | 4 | 5.2–-9.3 |
| 1 CC | 22.4 (4.7) | 28 | 20.3–24.6 | 22.8 (6.4) | 17 | 19.8–25.9 | 7.2 (2.0) | 16 | 6.2–8.2 |
| 2 CC | 22.6 (3.5) | 47 | 21.5–23.6 | 22.5 (5.7) | 44 | 20.8–24.1 | 6.6 (2.2) | 43 | 6.0–7.3 |
| 3 CC | 21.5 (3.9) | 51 | 20.4–22.5 | 19.8 (6.6) | 51 | 18.0–21.7 | 6.0 (2.3) | 48 | 5.4–6.7 |
| 4 CC | 21.3 (3.7) | 61 | 20.4–22.3 | 21.5 (6.3) | 63 | 20.0–23.1 | 6.5 (2.1) | 62 | 6.0–7.0 |
| 5 CC or more | 20.4 (4.4) | 132 | 19.7–21.1 | 19.0 (6.5) | 130 | 17.9–20.1 | 5.6 (2.2) | 129 | 5.2–6.0 |
CC: chronic conditions; CI: confidence interval; GED: general educational development; LGBTQ+: Lesbian, Gay, Bisexual, Transgender, Queer or Questioning, and other sexual identities; SD: standard deviation.
DSSI-10: Duke Social Support Index (10-item) (range 10-30, higher scores = more social connectedness); PROMIS-SI: PROMIS Social Isolation scale (range 6–30, higher scores = less isolated); UCLA: UCLA Loneliness 3-Item Scale (range 3-9; higher scores = less lonely).
Latino includes 36.7% Puerto Rican, 18.3% Dominican, 30% Other Latino countries in North, Central, and South America, 15% country of origin not specified.
Other Race/Ethnicity includes participants who identified as Asian or American Indian/Alaskan Native.
Women were more connected than men according to measures of social interactions and satisfaction with social support, yet they also reported greater perceived isolation and loneliness. Similarly, participants caring for someone with dementia or living with their care partner had greater social interactions and/or satisfaction with social support, yet more perceived isolation and loneliness. There was no clear pattern to social connectedness by level of education, living with a pet, or having visited a primary care provider (PCP) in the last 3 months.
Changes in Social Connectedness After PEARLS
PEARLS participants were more socially connected at 6-month follow-up than at baseline (Table 3 ). The mean(SD) change in social connectedness was 1.2(3.9) for DSSI-10, 2.2(6.2) for PROMIS-SI, and 0.5(2.2) for UCLA-Loneliness, with all three scales showing statistically significant (p <0.001) changes at follow-up using paired t-tests (DSSI-10: t = 5.2, df = 312, p <0.001; PROMIS: t = 6.3, df = 310, p <0.001; UCLA: t = 3.7, df = 301,p <0.002). Sensitivity analysis of the DSSI-10 subscales using paired t-tests suggests most of the DSSI-10 change was driven by increased satisfaction with social support. Effect sizes were small to moderate for the DSSI-10 (−0.28), PROMIS-SI (−0.35), and UCLA-Loneliness (−0.21).
TABLE 3.
Magnitude (Mean (SD)) of Social Connectedness and Depression at PEARLS Baseline, Follow-Up and Change Over Time (N = 320)
| Mean (SD) |
||||||
|---|---|---|---|---|---|---|
| Outcome | Baseline | 6-Month Follow-Up | Pre-post Change | t | df | p a |
| Social interaction and satisfaction with social support (DSSI-10) | 21.2 (4.1) | 22.4 (4.2) | 1.2 (3.9) | 5.2 | 312 | <0.001 |
| Perceived social isolation (PROMIS-SI) | 20.4 (6.5) | 22.6 (6.2) | 2.2 (6.2) | 6.3 | 310 | <0.001 |
| Loneliness (UCLA) | 6.1 (2.2) | 6.6 (2.1) | 0.5 (2.2) | 3.7 | 301 | 0.002 |
| Depressive symptom severity (PHQ-9) | 12.7 (4.6) | 7.5 (5.4) | -5.1 (5.8) | -15.2 | 301 | 0.002 |
DSSI-10: Duke Social Support Index (10-item) (range 10–30, higher scores = more social connectedness); PROMIS-SI: PROMIS Social Isolation scale (range 6–30, higher scores = less isolated); UCLA: UCLA Loneliness 3-Item Scale (range 3-9; higher scores = less lonely). PHQ-9: Patient Health Questionnaire 9-item): range 0–27, higher scores = more depressive symptom severity. PHQ-9 >/= 10 suggest clinically significant depressive symptoms. SD: standard deviation.
Probability values for differences between pre- and post-measures were calculated using paired t tests.
Some PEARLS participants showed smaller improvements in social connectedness after program completion. In unadjusted linear regression models, participants who identified as Latino (B = −1.34, 95% CI: 2.64–0.05, t = −2.14, df = 1, p = 0.042), had not seen a doctor in the past three-months (B = 1.31, 95% CI: 0.24–2.38, t = 2.40, df = 1, p = 0.017), and/or without stroke history (B = 1.35, 95% CI: 0.24–2.45, t = 2.40, p = 0.017) had smaller average improvements in their DSSI-10 (p <0.05). Black older adults had smaller improvements in social connectedness (DSSI-10, PROMIS, UCLA) compared to white participants (p = NS). Being a widow/er was associated with more social connectedness (as indicated by increased DSSI-10) post-PEARLS (B = 1.31, 95% CI: −1.42–0.12, t = 0.047, df = 4, p = 0.021) compared to being married/partnered. Participants who lived with more people or who provided more caregiving hours were less likely to improve perceived isolation (PROMIS-SI) after PEARLS (B = −0.77, 95% CI: 2.64–0.05, t = −2.32, df = 1, p = 0.042 and B = −.02, 95% CI: −0.04–0.01, t = −2.28, df = 1, p = 0.025). Lastly, participants without a recent PCP visit (B = 0.65, 95% CI: 0.05–1.25, t = 2.13, df = 1, p = 0.034) and/or with a pet (B = 0.51, 95% CI: 0.01–1.01, t = 1.99, df = 1, p = 0.047) had significantly smaller improvements in loneliness (UCLA) post-PEARLS.
We ran adjusted regression models with covariates from the literature on social connectedness, including age, gender, race/ethnicity, sexual orientation, living alone, marital status, difficulty meeting basic needs, multiple chronic conditions, depression severity, and baseline social connectedness score. Across all three measures, the level of social connectedness at baseline was significantly associated with improvement in social connectedness at follow-up (p <0.001 when all other covariates were held constant. For the DSSI-10, being Latino (B = −1.27, 95% CI: 2.47 to −0.65, t = −2.07, df = 11, p = 0.039) remained significantly associated with smaller improvements in social connectedness post-PEARLS. Difficulty paying for basic needs (B = −1.02, 95% CI −1.98 to −0.06, t = −2.09, df = 11, p = 0.037) was associated with lower social connectedness in the adjusted (but not unadjusted) model, suggesting one or more covariates in the model are not independent of change in social connectedness over time. No other factors remained associated with changes in the PROMIS-SI and UCLA-Loneliness from pre- to post-PEARLS.
Improvements in social connectedness remained consistent after the onset of the COVID-19 pandemic, with participants reporting similar improvements in perceived isolation (PROMIS-SI mean(SD) change 2.2(6.1) pre-COVID versus 2.4(6.5) during-COVID) and loneliness (UCLA mean(SD) change 0.43(2.2) pre-COVID versus 0.57(2.1) during-COVID). Participants showed smaller overall improvements in the DSSI-10 during COVID-19 (mean(SD) change 1.3(3.8) pre-COVID versus 0.78(4.2) during-COVID). Sensitivity analysis suggests that while statistically significant improvements in satisfaction with social support remained steady, there were decreases in social interaction. This is not surprising given shelter-at-home and physical distancing guidelines during the pandemic.
Improvements in Social Connectedness and Depression
Participants reduced their depression after PEARLS: the mean(SD) change in depression (PHQ-9) was −5.4(5.3) pre-post PEARLS (Table 4 ). At baseline, PEARLS participants with more severe depressive symptoms reported less social connectedness. Paired t tests showed significant improvements in PHQ-9 scores after PEARLS. Reduction in depression severity was moderately negatively correlated with the three social connectedness measures (Pearson's r = −.35, −0.46, −0.42, for DSSI-10, PROMIS-SI, UCLA-Loneliness; p <0.0001 for all three correlations), suggesting that participants’ improvement in social connectedness was related to reduced depression severity (PHQ-9). After PEARLS, participants with a depression response (≥50% decrease between pre-post PHQ-9) and remission (post-PHQ-9 <5) reported greater average improvements in social connectedness (Table 5 ).
TABLE 4.
Mean (SD) DSSI-10, PROMIS-SI, UCLA-Loneliness by Depression Severity at PEARLS Baseline
| Scale | Mild (PHQ-9 5–9) N = 67 | Moderate (PHQ-9 10-14) N 1 17 | Mod-Severe (PHQ-9 15-19) N = 84 | Severe (PHQ-9 >/= 20) N = 27 |
|---|---|---|---|---|
| DSSI-10 | 23.3 (3.9) | 21.0 (4.2) | 20.2 (3.6) | 19.0 (3.6) |
| PROMIS-SI | 23.8 (5.0) | 19.8 (6.3) | 17.8 (6.1) | 18.8 (7.0) |
| UCLA-Loneliness | 7.1 (2.0) | 6.0 (2.2) | 5.3 (2.2) | 5.4 (2.3) |
DSSI-10, PROMIS-SI, and UCLA-Loneliness scores were SS different across depression severity categories (p < .05). For DSSI-10, PROMIS, and UCLA higher scores = more social connectedness. DSSI-10 range 6-30, PROMIS-SI range 6-30; UCLA-Loneliness range 3 – 9; PHQ-9 range 0 – 27. SS: Statistically Significant.
TABLE 5.
Mean (SD) Change in Social Connectedness by Depression Response and Remission
| Response | No Response | Remission | No Remission | |
|---|---|---|---|---|
| Social interaction and satisfaction with social support (DSSI-10) | 2.6 (3.2) N = 133 | −0.1 (4.1) N = 162 | 2.2 (3.4) N = 102 | 0.6 (4.1) N = 194 |
| Perceived social isolation (PROMIS-SI) | 4.4 (5.7) N = 132 | 0.4 (6.1) N = 158 | 3.8 (5.8) N = 101 | 1.5 (6.4) N = 190 |
| Loneliness (UCLA) | 1.3 (2.0) N = 130 | −0.2 (2.1) N = 153 | 1.2 (2.2) N = 99 | 0.14 (2.1) N = 185 |
DSSI-10: Duke Social Support Index (10-item) (range 10-30, higher scores = more social connectedness); PROMIS-SI: PROMIS Social Isolation scale (range 6–30, higher scores = less isolated); UCLA: UCLA Loneliness 3-Item Scale (range 3–9; higher scores = less lonely). M: Mean; PHQ-9 : Patient Health Questionnaire 9-item; SD: Standard Deviation. Response = >/= 50% change between pre-post PHQ-9. Remission = post-PEARLS PHQ-9 < 5.
Participant Perspectives on How PEARLS May Have Improved Social Connectedness
PEARLS participants reported receiving encouragement and social support from their PEARLS providers, and appreciated having someone to talk to about issues they were experiencing. Their provider also connected them to additional services to address food and housing insecurity and to better manage their health. As one participant shared: “The one-on-one personal connection and the feeling that I was an important aspect of her work, that I mattered. We dealt with issues that were current at the time and she shared suggestions that have a continuing impact. She provided support and insight that will last longer than that particular moment.” (NY530)
PEARLS also helped participants identify and address problems in their lives, providing accountability and motivation to achieve their goals. They appreciated learning skills to overcome challenges they were experiencing, including changing both their approach to social interactions and their feelings about these interactions. For example, one Black caregiver described: “I learned to look within myself to recognize things to change. There was an emphasis on taking care of myself so that I can be a better caregiver for my husband and my daughter. I learned to ask for what I needed from others. That was very difficult for me to ask for help from family and friends.” (WA030). Some participants wished the PEARLS program would last longer or sessions would occur more frequently, given the valuable support they received from their provider.
CONCLUSION
This study engaged underserved older adults with depressive symptoms. As a whole, our participants at baseline reported being less socially connected than the general older population. When they started PEARLS, older adults who were younger, white, LGBTQ+, not partnered, living alone, experiencing financial limitations, recently hospitalized, and/or living with chronic conditions were less socially connected than persons who were older, BIPOC, straight, married/partnered, living with others, and/or without financial hardships, recent hospitalizations, or chronic conditions. Many of these less connected older adult groups have been identified by recent literature3 , 12 , 16 as priority populations for interventions to improve social connectedness and reduce the negative health impacts of isolation and loneliness. One unexpected finding was caregivers reported being more socially connected at baseline. The burden and stress often experienced by caregivers may be counteracted to some degree by enabling an older adult to tap into a sense of purpose, a supportive caregiving community, and positive cultural values.35
Overall, PEARLS participants significantly improved on all three social connectedness constructs (social interactions and satisfaction with social support; perceived isolation; loneliness) six months after enrollment, although effect sizes were small to moderate (0.21 – 0.35). Participants with lower baseline social connectedness showed smaller improvements post-PEARLS, and participants who improved their depression after PEARLS were also more socially connected after PEARLS.
Our findings align with previous research showing associations between social isolation, loneliness, and depression.7 , 8 , 36 Our findings are similar to Choi and colleagues’26 recent RCT that found similar improvements in social connectedness (DSSI-10, PROMIS-SI) among low-income, homebound older adults participating in BA via video-conferencing. Our lower effect sizes may be because we did not use isolation or loneliness as an eligibility criteria for our study, though our baseline measures suggest our study participants are on average more disconnected than the general older population. Maintaining (not worsening) social connectedness is also an appropriate outcome for older social service recipients so they can independently age in place. However, given the small effect sizes, further research should test adaptations to improve PEARLS performance, such as increasing the program frequency and/or duration, and including social connectedness as one of the prompts when generating the problem list with the participant.
After controlling for sociodemographics, health, and baseline social connectedness, participants who identified as Latino and/or who had difficulty paying for basic needs had smaller overall improvements in social connectedness after PEARLS. Existing literature offers possible reasons for these findings. Older Latinos cultural value of familismo may make it harder to be or feel connected if they are away from family social networks.37 For older persons experiencing poverty, it can be hard to access or prioritize meaningful social connections, or reciprocate social support, when having difficulty meeting housing, food and other basic needs.38
Our study highlights the importance of assessing multiple constructs of social connectedness. At baseline, while female participants reported more social activities and satisfaction with support than male participants, they also felt more isolated and lonely than males. In other words, being more connected was not the same as feeling more connected. Thus, it is essential that research and practice assess structure, function, and quality of social connections, and tailor interventions accordingly. This study combined the DSSI-10, PROMIS, and UCLA into a 17-item measure; future research will determine whether fewer items can accurately capture social connectedness. There are limitations to these measures, as they do not capture sources of social support which may differ depending on cultural and social norms and values.39 , 40 Future studies should also measure “perceived age,” given that loneliness among older adults during COVID-19 is associated with feeling older rather than chronological age.41
Participants’ comments about recommending PEARLS suggest the program can increase social connectedness through known mechanisms for change—improving social skills, enhancing social support, increasing opportunities for social interactions, and addressing maladaptive social cognition.4 , 42 PEARLS also aligns with literature on effective interventions to increase social connectedness among older adults: the program is a) theory-driven, b) designed to reach isolated and/or lonely persons, and engages older adults as c) active participants in understanding the nature of their disconnection, co-creating a personalized approach, and connecting to supports and services.3 , 16
While much of our evaluation was conducted pre-COVID-19, one-quarter of study participants completed post-PEARLS surveys between March and May 2020. Though many PEARLS programs pivoted to provide remote PEARLS delivery (phone or video-conferencing) when the pandemic began,43 most study participants had already received all of their in-person PEARLS sessions. Those who completed their follow-up survey in April or May 2020 had received up to two remote PEARLS sessions. Shelter-at-home and physical distancing requirements during the pandemic have reduced social cohesion,44 and increased mental health risks.45 Aging in general, and during COVID-19 in particular, presents challenges for older adults to manage collective and individual losses and to create a “new normal”—a sense of purpose, meaning and connection despite these obstacles. That PEARLS participants improved their social connectedness despite COVID-19 suggests the ongoing benefits of learning PST and BA skills with support from front-line providers. However, additional supports may be needed for older adults facing multiple, ongoing challenges, such as living in poverty with multiple chronic conditions. One PEARLS partner organization has created support groups for PEARLS graduates to maintain health and well-being including social connectedness, and link to services to address social needs and risk factors. While these in-person groups have moved to video-conferencing in COVID-19 times, it is important we improve access and support to technology given wide disparities faced by underserved older adults' populations.46
This study has several limitations. As a single group evaluation with no comparison group or randomization, we cannot attribute improvements in social connectedness to PEARLS specifically. We do not have social connectedness data for PEARLS participants who did not complete study surveys, so cannot describe the representativeness of our sample or assess potential selection bias. Pre-post survey analysis does not indicate whether improvements in social connectedness after PEARLS were due to PST and BA skill building or due to interactions with the PEARLS provider. With only a post-test, we are unable to evaluate whether social connectedness is maintained after visits from the PEARLS provider have ceased. As a second phase of this study we have conducted participant interviews and a second follow-up wave of surveys (12 months after PEARLS enrollment). We are currently analyzing this data to better understand mechanisms for change and whether changes in social connectedness are sustained. Second, we used different data collectors and modalities for pre- and post-data collection. We assessed accuracy at both time points to ensure scales were performing similarly–while there were slightly more missing items at baseline, other metrics were the same. In addition, PEARLS providers reported that baseline social connectedness data collection assisted them in building rapport with participants, and in partnering with them to create a more tailored and meaningful problem-solving and activity plan.
Engaging resource-constrained yet resilient settings such as our social service community partners that reach underserved older communities offers important “reverse innovations” for improving social connectedness; that is, centering our learning about interventions in organizations that innovate to make programs work efficiently and sustainably despite limited resources.47 While we aimed to conduct a pragmatic study with underserved populations, we acknowledge older adults connected to social services/PEARLS are less disadvantaged than those not connected to services. Further research is needed in partnership with older rural and/or LGBTQ+ communities (only 7% of our study participants identified with each)—both groups are at risk for social disconnectedness and depression. We also recognize the limitations of evaluating an individual-level intervention to address upstream social determinants of health (fundamental causes of health inequities)48 that create and perpetuate social disconnections for marginalized older adults. Embedding PEARLS within social services that address social needs and risk factors offers one avenue, but multi-level and -sector interventions that impact institutions, environments, policies and culture are also sorely needed for lasting structural and systemic change. Community-clinical linkages between health care systems and social service agencies also offer a continuum of care for older adults and sustainability for PEARLS organizations.
In conclusion, PEARLS is a promising program to improve social connectedness among underserved older populations. In collaboration with community-based social service organizations around the United States, we gathered important early evidence about one model for helping older adults be and feel more socially connected in ways that are meaningful and accessible to them. The COVID-19 pandemic and recent reports on the negative health effects of social isolation and loneliness have brought social connectedness into focus for policymakers and health systems. The network of aging and social service providers that engage underserved older adults is well poised to deliver and scale promising interventions like PEARLS to meet this call to action.
AUTHOR CONTRIBUTIONS
Study concept and design: Steinman, Parrish, Mayotte, Snowden; Acquisition of data: Parrish, Mayotte, Bravo, Torres, Markova, Boddie, Lachenmayr, Montoya, Parker, Conton-Pelaez; Analysis and interpretation of data: All authors; Drafting of the manuscript: Steinman, Parrish; Critical revision of the manuscript for important intellectual content: All authors; Accountability for the work: All authors
Acknowledgments
DISCLOSURE
We are grateful to PEARLS participants, providers, and our partner organizations for sharing their time and wisdom. We appreciate the support from the AARP Foundation who has prioritized their grant making on improving social connectedness among older adults living in poverty. Many thanks to Kai Zhang for data collection support, Yael Yanich for manuscript preparation, and Dr. Brian Leroux for statistical consultation and oversight.
The Health Promotion Research Center (LS, AP, CMa, PB, ET, MM, MS) is currently receiving a grant from the AARP Foundation to support this research. The Health Promotion Research Center is one of 26 CDC Prevention Research Centers across the U.S. J. Silsby is the evaluation director at AARP Foundation. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of AARP Foundation. For the remaining authors, no conflicts of interest are declared.
Footnotes
Supplementary material associated with this article can be found, in the online version, at https://doi.org/10.1016/j.jagp.2020.10.005.
Appendix. SUPPLEMENTARY MATERIALS
References
- 1.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7 doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flowers L, Houser A, Noel-Miller C, et al: Medicare Spends More on Socially Isolated Older Adults. Insight on the Issues (#125). AARP Public Policy Institute. Available at:https://www.aarp.org/content/dam/aarp/ppi/2017/10/medicare-spends-more-on-socially-isolated-older-adults.pdf. Accessed July 30, 2020.
- 3.National Academies of Sciences, Engineering, and Medicine . The National Academies Press; Washington, DC: 2020. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Available at: Accessed July 30, 2020. [DOI] [PubMed] [Google Scholar]
- 4.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2021;172:1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holt-Lunstad J, Robles TF, Sbarra DA. Advancing social connection as a public health priority in the United States. Am Psychol. 2017;72:517–530. doi: 10.1037/amp0000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aziz R, Steffens DC. What are the causes of late-life depression? Psychiatr Clin North Am. 2013;36:497–516. doi: 10.1016/j.psc.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blazer D. Depression and social support in late life: a clear but not obvious relationship. Aging Ment Health. 2005;9:497–499. doi: 10.1080/13607860500294266. [DOI] [PubMed] [Google Scholar]
- 8.Schwarzbach M, Luppa M, Forstmeier S. Social relations and depression in late life—a systematic review. Int J Geriatr Psychiatry. 2014;10:1–21. doi: 10.1002/gps.3971. [DOI] [PubMed] [Google Scholar]
- 9.Freedman VA, Spillman BC. Disability and care needs among older Americans. Milbank Q. 2014;92:509–541. doi: 10.1111/1468-0009.12076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haroz EE, Ritchey M, Bass JK. How is depression experienced around the world? A systematic review of qualitative literature. Soc Sci Med. 2017;183:151–162. doi: 10.1016/j.socscimed.2016.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Psychiatric Association . 4th edition. American Psychiatric Association; Washington, DC: 2000. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 12.Anderson O, Thayer CE. AARP Foundation; Washington, DC: 2018. Loneliness and Social Connections: A National Survey of Adults 45 and Older.https://www.aarp.org/content/dam/aarp/research/surveys_statistics/life-leisure/2018/loneliness-social-connections-2018.doi.10.26419-2Fres.00246.001.pdf Available at: Accessed July 30, 2020. [Google Scholar]
- 13.Crystal S, Sambamoorthi U, Walkup JT. Diagnosis and treatment of depression in the elderly Medicare population: predictors, disparities, and trends. J Am Geriatr Soc. 2003;51:1718–1728. doi: 10.1046/j.1532-5415.2003.51555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baumann AA, Cabassa LJ. Reframing implementation science to address inequities in healthcare delivery. BMC Health Services Res. 2020;20:1–9. doi: 10.1186/s12913-020-4975-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ciechanowski P, Wagner E, Schmaling K. Community-integrated home-based depression treatment in older adults: a randomized controlled trial. JAMA. 2004;291:1569–1577. doi: 10.1001/jama.291.13.1569. [DOI] [PubMed] [Google Scholar]
- 16.Fakoya OA, McCorry NK, Donnelly M. Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health. 2020;20:129. doi: 10.1186/s12889-020-8251-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klinenberg E. Social isolation, loneliness, and living alone: identifying the risks for public health. Am J Public Health. 2016;106:786. doi: 10.2105/AJPH.2016.303166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frohlich KL, Potvin L. Transcending the known in public health practice. Am J Public Health. 2008;98:216–221. doi: 10.2105/AJPH.2007.114777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thorpe KE, Zwarenstein M, Oxman A.D. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J Clin Epidemiol. 2009;62:464–475. doi: 10.1016/j.jclinepi.2008.12.011. doi.org/10.1016/j.jclinepi.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 20.Palinkas LA, Horwitz SM, Green CA. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm Policy Ment Health. 2015;42:533–544. doi: 10.1007/s10488-013-0528-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mynors-Wallis LM, Gath DH, Lloyd-Thomas A. Randomised controlled trial comparing problem solving treatment with amitriptyline and placebo for major depression in primary care. BMJ. 1995;310:441–445. doi: 10.1136/bmj.310.6977.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacobson NS, Dobson KS, Truax PA. A component analysis of cognitive-behavioral treatment for depression. J Consult Clin Psychol. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- 24.Farren L, Snowden M, Steinman L. Development and evaluation of a fidelity instrument for PEARLS. Front Public Health. 2015;2:200. doi: 10.3389/fpubh.2014.00200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wardian J, Robbins D, Wolfersteig W. Validation of the DSSI-10 to measure social support in a general population. Res Soc Work Pract. 2013;23:100–106. [Google Scholar]
- 26.Hughes ME, Waite LJ, Hawkley LH. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choi NG, Pepin R, Marti CN. Improving social connectedness for homebound older adults: randomized controlled trial of tele-delivered behavioral activation versus tele-delivered friendly visits. Am J Geriatr Psychiatry. 2020 doi: 10.1016/j.jagp.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Landerman R, George LK, Campbell RT. Alternative models of the stress buffering hypothesis. Am J Community Psychol. 1989;17:625–642. doi: 10.1007/BF00922639. [DOI] [PubMed] [Google Scholar]
- 29.Hahn EA, DeWalt DA, Bode RK. New English and Spanish social health measures will facilitate evaluating health determinants. Health Psychol. 2014;33:490–499. doi: 10.1037/hea0000055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Russell D, Peplau LA, Cutrona CE. The Revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39:472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- 31.Steptoe A, Shankar A, Demakakos P. Social isolation, loneliness, and all-cause mortality in older men and women. PNAS. 2013;110:5797–5801. doi: 10.1073/pnas.1219686110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nicholson NR. A review of social isolation: an important but underassessed condition in older adults. J Prim Prev. 2012;33:137–152. doi: 10.1007/s10935-012-0271-2. [DOI] [PubMed] [Google Scholar]
- 33.Harris PA, Taylor R, Thielke R. Research electronic data capture (REDCap)––a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2009;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 35.Clay OJ, Roth DL, Wadley VG. Changes in social support and their impact on psychosocial outcome over a 5-year period for African American and White dementia caregivers. Int J of Geriatr Psychiatry. 2008;23:857–862. doi: 10.1002/gps.1996. [DOI] [PubMed] [Google Scholar]
- 36.Barg FK, Huss-Ashmore R, Wittink MN. A mixed-methods approach to understanding loneliness and depression in older adults. J Gerontol B Psychol Sci Soc Sci. 2006;61:S329–S339. doi: 10.1093/geronb/61.6.s329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ortiz DV, Cole SA. Culture, place of origin, and service delivery for latino older adult immigrants: the case of Puerto Rican older adults. J Gerontol Soc Work. 2008;51:3–4. doi: 10.1080/01634370802039627. 300-314. [DOI] [PubMed] [Google Scholar]
- 38.Portacolone E. Structural factors of elders’ isolation in a high-crime neighborhood: an in-depth perspective. Public Policy Aging Report. 2017;27:152–155. doi: 10.1093/ppar/prx025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bélanger E, Ahmed T, Vafaei A. Sources of social support associated with health and quality of life: a cross-sectional study among Canadian and Latin American older adults. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2016-011503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pachana NA, Smith N, Watson M. Responsiveness of the duke social support sub-scales in older women. Age Ageing. 2008;37:666–672. doi: 10.1093/ageing/afn205. [DOI] [PubMed] [Google Scholar]
- 41.Shrira A, Hoffman Y, Bodner E. COVID-19 related loneliness and psychiatric symptoms among older adults: the buffering role of subjective age. Am J Geriatr Psychiatry. 2020 doi: 10.1016/j.jagp.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Umberson D, Karas Montez J. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. 2010;51(1_suppl):S54–S66. doi: 10.1177/0022146510383501. doi.org/10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith ML, Steinman LE, Casey EA. Combatting social isolation among older adults in a time of physical distancing: the COVID-19 social connectivity paradox. Front Public Health. 2020;8:403. doi: 10.3389/fpubh.2020.00403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Brenner MH. Will there be an epidemic of corollary illnesses linked to a COVID-19-related recession? Am J Public Health. 2020;110:974–975. doi: 10.2105/AJPH.2020.305724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- 46.Roberts ET, Mehrotra A. Assessment of disparities in digital access among medicare beneficiaries and implications for telemedicine. JAMA Intern Med. 2020;3 doi: 10.1001/jamainternmed.2020.2666. Published online August 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yapa HM, Bärnighausen T. Implementation science in resource-poor countries and communities. Implement Sci. 2018;13:154. doi: 10.1186/s13012-018-0847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(Suppl):S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.