Abstract
The novel 2019 coronavirus disease (COVID-19) pandemic is a global public health emergency. To date, physical distancing and good personal hygiene have been the only effective measures to limit spread. The pandemic has altered routine cancer care, including allied health and supportive care interventions. Clinicians must adapt and find ways to continue to deliver optimal patient care at this time. The prescription of exercise to people with cancer has been demonstrated to have meaningful benefits for both physical and mental health and quality of life, and may even enhance survival. Such exercise interventions provide the largest benefit to patients when delivered in a supervised, group, clinic-based setting. In the age of COVID-19, group-based exercise in communal facilities presents risks for both aerosol and surface transmission of the virus among people exercising, necessitating a pivot from the usual methods of exercise delivery to home-based exercise programs. In this article, we discuss the challenges that need to be overcome in moving to a home-based program for patients with cancer while maintaining the benefits of targeted and high-fidelity exercise medicine. We provide practical recommendations for how home-based exercise can be supported and nurtured by qualified exercise professionals who treat people living with cancer, as well as pointing to resources that are available online to assist practitioners. Despite the challenges faced during this pandemic, we believe that it is important for people to continue to benefit from exercise in a safe environment with the support of exercise specialists.
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing the novel 2019 coronavirus disease (COVID-19) is recognized by the WHO as a public health emergency of international proportions, the overall scale and impact of which has been described elsewhere.1-3 The pandemic has caused considerable disruption to routine supportive care for patients with cancer and survivors. Clinicians and patients must adjust to the many evolving external constraints confronting them. Various groups have prepared guidance documents to assist oncologists and hematologists with this adjustment of their clinical practice to best facilitate patient-centered cancer care in this new environment.4,5 It is important that the delivery of allied health and psychosocial services also continue with adaptations in place to minimize the risk of transmission of COVID-19 infection.
Exercise for patients with cancer and survivors has benefits across the cancer spectrum, including as neoadjuvant or adjuvant therapy; as a preventive, preparatory, and rehabilitative tool for surgery (presurgical and postsurgical); and as symptom control during and after primary treatments, including radiotherapy, chemotherapy, and hormone therapy postdiagnosis and in advanced disease states.6,7 Specifically, exercise oncology (ie, exercise medicine in the management of cancer) serves to improve patient quality and quantity of life. It achieves these patient outcomes through the reduction, prevention, or reversal of treatment-related toxicities; mitigation of cancer-related fatigue; and restoration of physical function and exercise capacity, most notably in response to treatment-driven changes in body composition. Furthermore, exercise has synergistic potential with primary cancer therapies that may help patients with cancer better tolerate their treatments (thus fewer dose limitations) and could increase the potency or effectiveness of these therapies (such as chemotherapy or radiation therapy through changes in tumor vasculature and perfusion).8,9 Accordingly, exercise oncology remains an integral component of cancer treatment and survivorship programs.
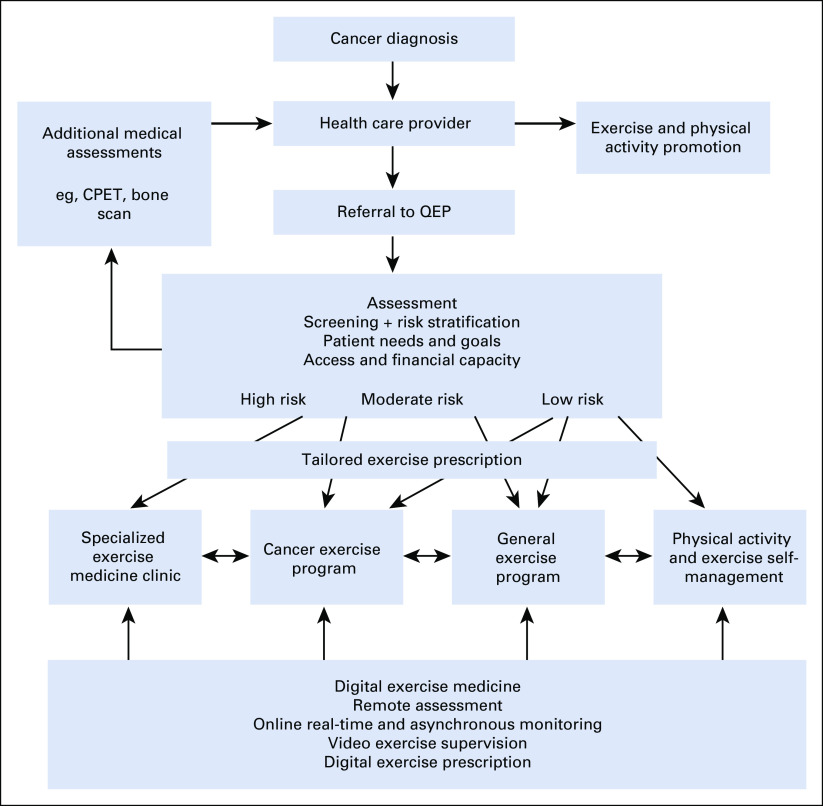
Patients with cancer and survivors must commence or continue to exercise frequently to maintain their psychological well-being, physical health, and functional capacity; manage treatment adverse effects; and limit or reverse progression of other chronic diseases.6,7 The term exercise describes a suite of prescribed interventions using specific modalities tailored to the individual needs of patients with cancer and survivors,6 with exercise prescriptions able to effectively improve immune function and patient resistance to communicable diseases.10-12 Current recommendations direct high-risk individuals to isolate themselves, usually at home, during the COVID-19 pandemic. As such, exercise programs for patients with cancer and survivors must pivot from their usual clinic-based and community-based models to programs that can be safely and reliably delivered in the home environment, preferably with telehealth exercise oncology support and monitoring (Fig 1).
Fig 1.
Triage pathway of patients with cancer and survivors from diagnosis to referral to a qualified exercise professional (QEP), risk stratification, and prescription of a tailored exercise program. Setting of exercise program depends on patient risk profile, with digital exercise medicine providing support in each environment, as appropriate. Patients may migrate between settings as health and risk profile change. Modified from Santa Mina et al31 CPET, cardiopulmonary exercise test.
TRIAGING PATIENTS WITH CANCER TO ENGAGE IN EXERCISE
Oncology and hematology clinicians form a critical contact point to increase patient participation in exercise medicine. Clinicians act as trusted sources of information and education—they can introduce the importance of exercise and proactively encourage patients to exercise at a time when they are more likely to engage in new health behaviors. Relatively healthy and fit patients without major comorbidities or treatment adverse effects may continue under self-management (Fig 1), with assurance from the physician that exercise will not have a negative impact on their cancer or treatment. However, most patients will be older and have health issues that require a more targeted approach as well as assessment of risk of adverse effects of some exercise modes and dosages. Referral to an appropriately qualified exercise professional (QEP) is recommended (Fig 1). In most countries, this would be an accredited exercise physiologist, clinical exercise physiologist, or physiotherapist or physical therapist. Professionals with such qualifications undertake, at a minimum, a 4-year university program, and many will have additional qualifications and clinical experience in exercise oncology.
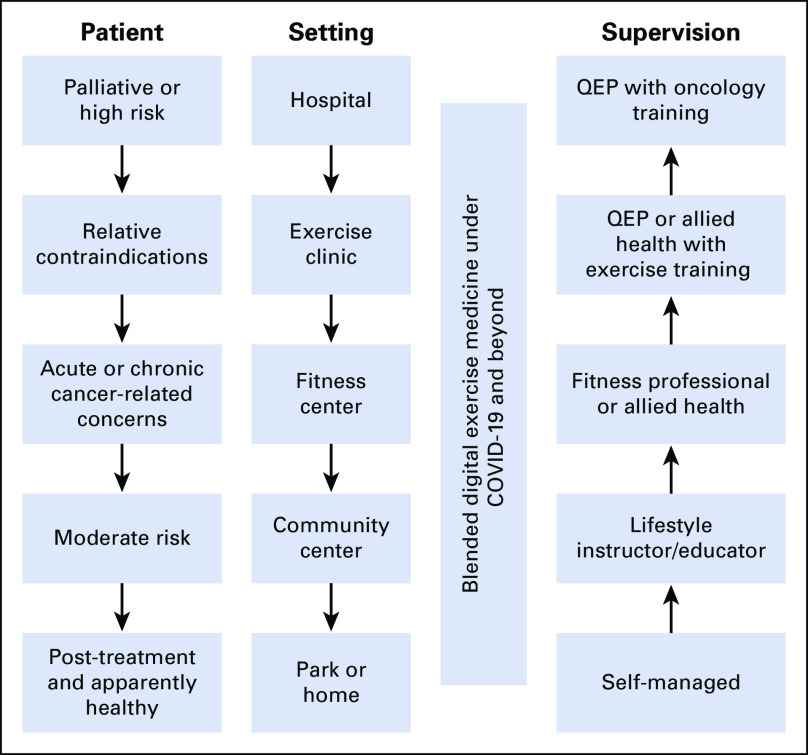
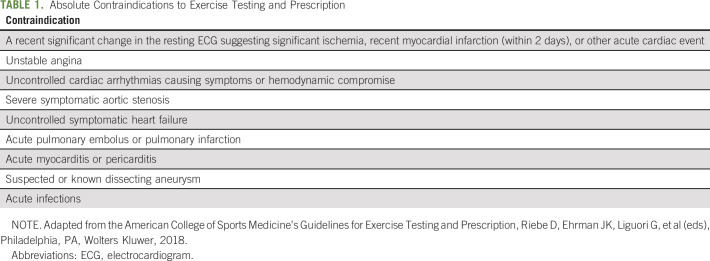
The QEP will use health and medical information from the referring physician and perform additional health and fitness assessments, as well as collate patient-reported outcome measures, such as cancer- and treatment-specific concerns, exercise preferences and experiences, access to facilities, equipment and expertise, and financial capacity, as well as patient goals and needs.6 Triage at this stage involves 2 key processes. First, patient risk of exercise-induced adverse events (eg, risk of skeletal fracture or cardiovascular event) must be assessed to determine contraindicated exercise modes and dosages and the required level of supervision and acceptable settings (Fig 2). Second, the patient’s health issues are prioritized, and the exercise prescription is designed to address in order of emphasis those morbidities causing greatest concern, functional impairment, mortality risk, and preparation for subsequent cancer treatments (eg, surgery). There are absolute contraindications to exercise testing and training (Table 1); however, most patients with cancer will only exhibit relative contraindications,6 meaning that they can exercise provided the prescription, setting, and supervision is appropriate.6
Fig 2.
Appropriate setting and supervision intersect with patient risk and relative contraindications as well as cancer-specific complexities, for example, bone metastases. Because of COVID-19, setting may be limited to park or home, requiring much higher fidelity telehealth support to manage risk and optimize effectiveness. QEP, qualified exercise professional.
TABLE 1.
Absolute Contraindications to Exercise Testing and Prescription
COVID-19, PATIENTS WITH CANCER AND EXERCISE SETTINGS
Exercise clinics, fitness centers, and other community spaces are typically preferred environments for patients with cancer and survivors to receive exercise medicine in a supervised and socially supportive setting. Beyond high-fidelity exercise programs, these environments encourage critically important levels of peer support and camaraderie inherent in any group of cancer survivors exercising together. Group exercise is one of the primary reasons for patient exercise adoption, adherence, compliance, and, ultimately, success.13 However, patients with cancer and survivors are at increased risk of developing COVID-19, often because of the presence of comorbidities, advancing age (for some), immunosuppressive effects of malignancy,14 immunologic effects of cancer therapies,15 disruption of mucosal barriers, and the use of potent immunosuppression to manage some treatment toxicities.16 The National Comprehensive Cancer Network has released guidelines with regard to the risk of infections in patients with cancer based on various therapeutic interventions in the management of patients with hematologic and solid organ malignancy.17
SARS-CoV-2 surface and aerosol viability may render exercise clinics, fitness centers, and community facilities as unacceptable risks for people living with cancer, particularly in group exercise or shared facility situations.18 Given that intense exercise increases respiration and the generation of aerosols,19 significant ventilation would be required to enhance the removal of aerosolized pathogens that may pose an infection risk to patients with cancer.19 Furthermore, these facilities contain surfaces exposed to body fluids that are stable for SARS-CoV-2 (such as stainless steel) and thus require frequent cleaning20 and the application of appropriate disinfectants before and after their use.
In Australia, a prohibition on exercise facilities has existed since March 25, 2020,21 which is not dissimilar to most other nations worldwide. This creates a conundrum that requires transitioning to home-based exercise for the whole population, but especially patients with cancer and survivors in the supportive care setting. During COVID-19, physical distancing, self-isolation, and stay-at-home orders have proven effective in contagion control when implemented.22,23 As such, patients with cancer and survivors may be separated from their usual venues for exercise, whereby clinical oncologists and hematologists, QEPs, and patients with cancer worldwide must adapt to engage in exercise programs for the maintenance or betterment of their health.
TRANSITIONING PATIENTS WITH CANCER TO HOME-BASED EXERCISE
Patients with cancer should exercise on most days, if not every day, to maintain their psychological and physical health, and combat the deleterious effects of cancer and its associated treatments, in the absence of absolute contraindications (Table 1). Strikingly, there are numerous large studies reporting reduced all-cause mortality and cancer-related mortality for patients with cancer who are more physically active, further emphasizing the imperative to exercise.24,25 During COVID-19 restrictions, patients with cancer and survivors risk regressing to a sedentary lifestyle, which will result in declining health and quality of life, particularly for patients undergoing treatment or suffering adverse effects of treatment.
Transitioning a high-fidelity exercise program from an exercise clinic, fitness center, or community center into the home-based environment is challenging. Using the terms “cancer AND exercise AND home-based” in PubMed returns approximately 383 results, which provide potentially safe and effective exercise that cancer survivors can pursue in their own home environment. This is of high interest to researchers, clinicians, and the patient with cancer or survivor. However, there have been mixed experiences of adherence and effectiveness of home-based exercise programs relative to supervised programs overseen by qualified exercise professionals conducted in exercise clinics.26
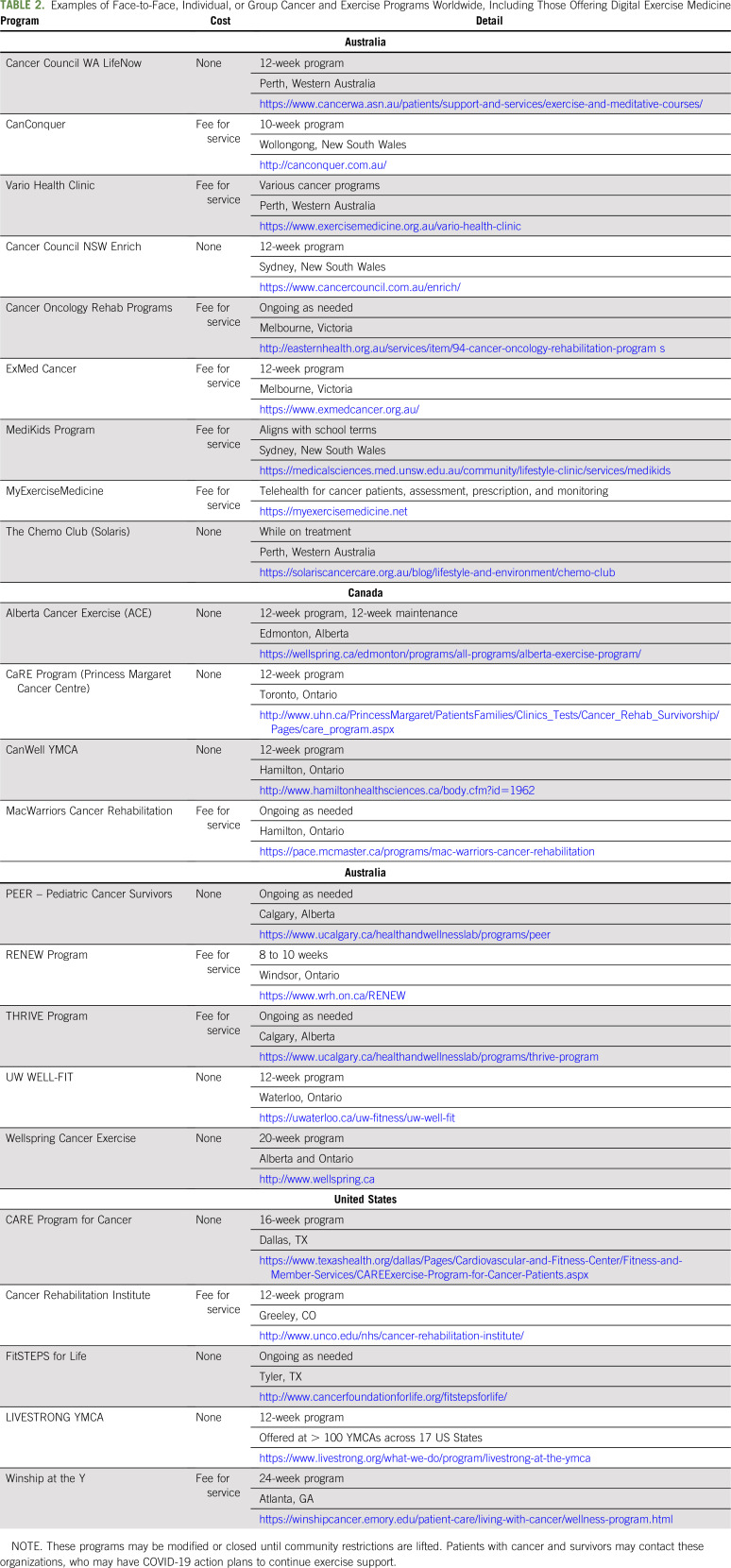
Where possible, patients considered at high risk for undertaking an exercise program (eg, deconditioned, poor performance status, significant comorbidities, or poor physical literacy [history of exercise]) should ideally continue to receive their exercise interventions face to face. Options for remotely supervised exercise programs (telehealth with video chat, online monitoring, and digital exercise programs) with a QEP are available and are developing rapidly driven by the imperative of COVID-19. This is particularly helpful for patients who are at moderate to advanced risk, because high-fidelity virtual supervision is necessary to ensure exercise safety and effectiveness. Although those at low risk can still receive the online support of a QEP, they are also suitable for self-managed exercise platforms where the patient has independence and/or can partake in peer-support exercise programs online. Face-to-face, remote, and independent exercise programs and options for patients with cancer and survivors worldwide are provided in Tables 2 and 3. These are not exhaustive; however, they may reflect options that can be accessible locally or globally.
TABLE 2.
Examples of Face-to-Face, Individual, or Group Cancer and Exercise Programs Worldwide, Including Those Offering Digital Exercise Medicine
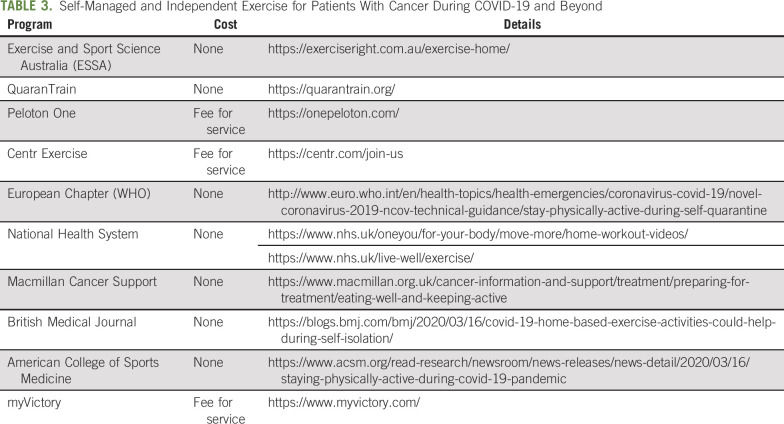
TABLE 3.
Self-Managed and Independent Exercise for Patients With Cancer During COVID-19 and Beyond
ADAPTING EXERCISE FOR PEOPLE WITH CANCER DURING COVID-19
A new age is upon us with COVID-19, and exercise oncology programs must adapt to the changing environment. Fortunately, information technology is rapidly evolving to facilitate this change. Social media and other Internet-based solutions, including reliable and high-quality video communication (video chat) applications are increasingly easy to set up and use.27 There are many examples available for smartphones, laptops, and personal computing devices (eg, Microsoft Teams, Zoom, Skype, Viber, WhatsApp, FaceTime, Facebook Messenger, Instagram). Most are free of charge beyond the cost of Internet or mobile connection, providing direct one-to-one communication for QEPs and their patients or between 2 individuals wishing to interact and provide peer support while exercising, regardless of geographic location. Peer-to-peer communication is also ubiquitous now via the Internet with full sound, video, and chat such that groups of patients can freely communicate with or without an exercise professional also participating in the session. To a large extent, this can overcome one of the major deficits of home-based exercise. In prior research, the peer support and camaraderie inherent in groups of cancer survivors exercising together is one of the main reasons home-based exercise programs have inferior adherence and reduced effectiveness.28
The second key component is to be able to provide quality and engaging exercise instruction and guidance to the patient. Although this could be done in a group format and a virtual environment led by an exercise professional, it is appealing to have the capacity for the patient or group of patients to schedule their exercise at a time most convenient for them. Here again, information technology provides the solution with a considerable range of well-developed exercise prescription platforms (eg, TechnoGym MyWellness, PhysiTrack, Salaso) in which the exercise professional can design the exercise program and patients can receive this on their smartphones or tablets as an app or on their computers through a Web browser. These platforms lead the patient through the exercise program accompanied by video demonstrations of the exercises and provide timing of the exercise sets and recovery periods. If patients are wearing activity and/or heart rate monitors that are Internet connected, their exercise performance can be uploaded to the cloud to provide them with feedback as well as a tool for the QEP to monitor the patient.
Our facility at Edith Cowan University in Western Australia (Vario Health Clinic and the Exercise Medicine Research Institute) delivers exercise oncology programs to > 500 active patients each week through health practitioner referral, patient self-referral, and ongoing clinical trials, running > 2,000 one-on-one and group exercise sessions for adult patients with cancer and survivors across all stages of disease over 6 exercise clinic sites each year. Owing to the COVID-19 pandemic, we have transitioned all patients from in-clinic supervision, rapidly supporting them to exercise while in self-isolation through employing these latest “digital exercise medicine” methodologies to maintain routine supportive care. Critically, we have several large exercise medicine clinical trials ongoing involving dozens of patients with cancer from local to advanced disease, and these studies have been dependent on face-to-face interactions with high-fidelity supervision.29 To salvage our research programs, we have ensured that participants can continue with safe, high-quality, and effective exercise medicine within their home. We also operate several exercise clinics across the city, supporting patients with a range of chronic diseases and other health issues, as well as healthy older people. For those who are willing, we are offering our digital exercise medicine and telehealth services as a subsidized service to keep them active, support their health behavior change, and reduce the risk of their health declining during what might be an extended period of limited time outside their own home.
PRACTICAL RECOMMENDATIONS
Patients should approach home exercise sessions as they would any other (Data Supplement) by scheduling the session, dressing in exercise apparel, and attempting to coordinate with a buddy to join in virtually. They should set up a safe and conducive environment to exercise with space, an exercise mat, equipment, music, and preferably a television, computer monitor, tablet, or smartphone to view the exercise program and video chat with buddies and the exercise professional.
An effective and enjoyable exercise program can be completed with a minimum of equipment. In fact, quality aerobic and resistance training can be prescribed just using body weight. For example, walking or jogging on the spot, interval sprints up and down a corridor, walking up and down stairs, or jogging around the house or apartment make for an excellent aerobic (cardiorespiratory) workout. Resistance training can also be achieved using body weight, with exercises such as squats, split squats, lunges, push-ups, and tricep dips (in the absence of equipment). Adding basic equipment increases the range of exercises available, and in priority order, this could include dumbbells, steps or stairs, stretch bands, a skipping rope, medicine ball, and an aerobic ergometer such as a treadmill, cycle, or rower, but these items are far from essential. However, in the home environment, there will be household objects that have weight and can be used for a range of resistance training activities. Shopping bags filled with rice or various items, plastic bottles of water, sandbags, and so on can be used to increase load during aerobic, interval training, and resistance exercise. Being inventive can help overcome equipment shortages.
Exercise oncology prescriptions should be tailored to each individual patient specific to their priority health issues, while managing risks on an individual basis, such as the presence of hypertension or bone metastases.6,30 Each patient should exercise on most days, if not every day, for at least 20 minutes; the volume of exercise may be less for severely deconditioned or unwell individuals. In general, the program should be a combination of aerobic and resistance exercise, progressively overloaded (increasing intensity as the patient becomes fitter), and vary across 1-week, 4-week, and 12-week cycles through “periodization” to increase effectiveness, reduce staleness of the intervention, and lessen injury risk.29 Variety of exercise is also important, with the combination of moderate-intensity continuous training, high-intensity interval training, and different forms of resistance training, including high-intensity resistance training, recommended for most patients.6 Last, programs should be autoregulated to accommodate changes and fluctuations in each patient's well-being throughout treatment, where lowering intensity or volume can occur if the patient is fatigued or unwell, or raising intensity or volume can occur if the patient is energetic and motivated.
Ideally, assessments of patients with cancer and survivors transitioning to a home-based setting during self-isolation during the COVID-19 pandemic, along with their individually tailored exercise prescription, should be conducted by a QEP with a minimum of 4 years of university training (such as Accredited or Certified Exercise Physiologists) and preferably with additional postgraduate training in exercise oncology. As acknowledged, access to QEPs may be strained by this pandemic; therefore, it is important that those at low risk still engage in exercise if a QEP is not available to assist them. Those at increased risk should be given telehealth exercise medicine options.
SUMMARY
The COVID-19 pandemic and associated measures for pandemic control have had far-reaching effects on society. For people living with cancer, it has essentially put a stop to exercising in any public space. Maintaining an exercise regimen is important for general well-being, mitigation of treatment toxicities, amelioration of other chronic conditions, and the improvement of important clinical outcomes, such as reducing the risk of recurrence and improving all-cause and cancer-specific mortality regardless of disease stage. The challenge for clinicians caring for these patients is to provide safe and effective exercise medicine that patients will adhere to in the longer term. Internet technologies and adaptations in patient management may well achieve this much of what has been rapidly advanced because of COVID-19.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Collection and assembly of data: All authors
Data analysis and interpretation: All authors
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Keeping Patients With Cancer Exercising in the Age of COVID-19
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Robert U. Newton
Honoraria: GenesisCare
Research Funding: Ipsen
Travel, Accommodations, Expenses: Genesis Cancer Care
Nicolas H. Hart
Research Funding: Ipsen Pty (Inst)
Timothy Clay
Honoraria: Novartis, Roche, AstraZeneca
Speakers' Bureau: AstraZeneca, Novartis
Research Funding: Exelixis (Inst), Immutep (Inst), Clovis Oncology (Inst), Merck Sharp & Dohme (Inst), BeyondSpring Pharmaceuticals (Inst), Bayer (Inst)
Travel, Accommodations, Expenses: Genentech, Bristol Myers Squibb, Astra Zeneca, Foundation Medicine, Astellas Pharma
No other potential conflicts of interest were reported.
REFERENCES
- 1. Ghebreyesus T. WHO Director-General’s opening remarks at the media briefing on COVID-19 - March 11, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2. van der Velden WJ, Herbers AH, Netea MG, et al. Mucosal barrier injury, fever and infection in neutropenic patients with cancer: Introducing the paradigm febrile mucositis. Br J Haematol. 2014;167:441–452. doi: 10.1111/bjh.13113. [DOI] [PubMed] [Google Scholar]
- 3. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Weinkove R, McQuilten ZK, Adler J, et al. Managing haematology and oncology patients during the COVID-19 pandemic: Interim consensus guidance. Med J Aust. 2020;212:481–489. doi: 10.5694/mja2.50607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Segelov E, Underhill C, Prenen H, et al. Practical considerations for treating cancer patients in the COVID-19 pandemic. JCO Oncol Pract. 2020;16:467–482. doi: 10.1200/OP.20.00229. [DOI] [PubMed] [Google Scholar]
- 6. Hayes SC, Newton RU, Spence RR, et al. The Exercise and Sports Science Australia position statement: Exercise medicine in cancer management. J Sci Med Sport. 2019;22:1175–1199. doi: 10.1016/j.jsams.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 7. Hart NH, Galvão DA, Newton RU. Exercise medicine for advanced prostate cancer. Curr Opin Support Palliat Care. 2017;11:247–257. doi: 10.1097/SPC.0000000000000276. [DOI] [PubMed] [Google Scholar]
- 8. Iyengar NM, Jones LW. Development of exercise as interception therapy for cancer: A review. JAMA Oncol. 2019;5:1620–1627. doi: 10.1001/jamaoncol.2019.2585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Koelwyn GJ, Jones LW. Exercise as a candidate antitumor strategy: A window into the future. Clin Cancer Res. 2019;25:5179–5181. doi: 10.1158/1078-0432.CCR-19-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Martin SA, Pence BD, Woods JA. Exercise and respiratory tract viral infections. Exerc Sport Sci Rev. 2009;37:157–164. doi: 10.1097/JES.0b013e3181b7b57b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fondell E, Lagerros YT, Sundberg CJ, et al. Physical activity, stress, and self-reported upper respiratory tract infection. Med Sci Sports Exerc. 2011;43:272–279. doi: 10.1249/MSS.0b013e3181edf108. [DOI] [PubMed] [Google Scholar]
- 12. Mondal A, Chatterjee S. Exercise and immunity: A correlated mechanism. Int J Health Sci Res. 2018;8:284–294. [Google Scholar]
- 13. Lund LW, Ammitzbøll G, Hansen DG, et al. Adherence to a long-term progressive resistance training program, combining supervised and home-based exercise for breast cancer patients during adjuvant treatment. Acta Oncol. 2019;58:650–657. doi: 10.1080/0284186X.2018.1560497. [DOI] [PubMed] [Google Scholar]
- 14. Mittal D, Gubin MM, Schreiber RD, et al. New insights into cancer immunoediting and its three component phases--Elimination, equilibrium and escape. Curr Opin Immunol. 2014;27:16–25. doi: 10.1016/j.coi.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Galluzzi L, Buqué A, Kepp O, et al. Immunological effects of conventional chemotherapy and targeted anticancer agents. Cancer Cell. 2015;28:690–714. doi: 10.1016/j.ccell.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 16. Puzanov I, Diab A, Abdallah K, et al. Managing toxicities associated with immune checkpoint inhibitors: Consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer. 2017;5:95. doi: 10.1186/s40425-017-0300-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. National Cancer Comprehensive Network: Prevention and treatment of cancer related infections. https://www.nccn.org/professionals/physician_gls/pdf/infections.pdf.
- 18. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Andrade A, Dominski FH, Pereira ML, et al. Infection risk in gyms during physical exercise. Environ Sci Pollut Res Int. 2018;25:19675–19686. doi: 10.1007/s11356-018-1822-8. [DOI] [PubMed] [Google Scholar]
- 20.Gola M, Gaviraghi L, Capasso LM, et al. Design and hygiene issues in sports facilities. A pilot study which investigates fitness centres by using a multidisciplinary tool. Ann 1st Super Sanita 55:224-2322019. [DOI] [PubMed]
- 21.Morrison S.Update on coronavirus measures. Prime Minister’s Media Statement 8th May 2020. https://www.pm.gov.au/media/update-coronavirus-measures-08may20.
- 22. Bedford J, Enria D, Giesecke J, et al. COVID-19: Towards controlling of a pandemic. Lancet. 2020;395:1015–1018. doi: 10.1016/S0140-6736(20)30673-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ng Y, Li Z, Chua YX, et al. Evaluation of the effectiveness of surveillance and containment measures for the first 100 patients with COVID-19 in Singapore – January 2-February 29, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:307–311. doi: 10.15585/mmwr.mm6911e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kenfield SA, Stampfer MJ, Giovannucci E, et al. Physical activity and survival after prostate cancer diagnosis in the health professionals follow-up study. J Clin Oncol. 2011;29:726–732. doi: 10.1200/JCO.2010.31.5226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lee I-M, Shiroma EJ, Kamada M, et al. Association of step volume and intensity with all-cause mortality in older women. JAMA Intern Med. 2019;179:1105–1112. doi: 10.1001/jamainternmed.2019.0899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Galvão DA, Newton RU, Girgis A, et al. Randomized controlled trial of a peer led multimodal intervention for men with prostate cancer to increase exercise participation. Psychooncology. 2018;27:199–207. doi: 10.1002/pon.4495. [DOI] [PubMed] [Google Scholar]
- 27. Chan JM, Newton RU, Culos-Reed SN, et al. An international, population-level initiative to promote healthy lifestyle practices among prostate cancer survivors. J Clin Oncol. 2016;34 (suppl; abstr e287) [Google Scholar]
- 28. Fox L, Wiseman T, Cahill D, et al. Barriers and facilitators to physical activity in men with prostate cancer: A qualitative and quantitative systematic review. Psychooncology. 2019;28:2270–2285. doi: 10.1002/pon.5240. [DOI] [PubMed] [Google Scholar]
- 29. Newton RU, Kenfield SA, Hart NH, et al. Intense Exercise for Survival Among Men With Metastatic Castrate-Resistant Prostate Cancer (INTERVAL-GAP4): A multicentre, randomised, controlled phase III study protocol. BMJ Open. 2018;8:e022899. doi: 10.1136/bmjopen-2018-022899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Galvão DA, Taaffe DR, Spry N, et al. Exercise preserves physical function in prostate cancer patients with bone metastases. Med Sci Sports Exerc. 2018;50:393–399. doi: 10.1249/MSS.0000000000001454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Santa Mina D, Sabiston CM, Au D, et al. Connecting people with cancer to physical activity and exercise programs: A pathway to create accessibility and engagement. Curr Oncol. 2018;25:149–162. doi: 10.3747/co.25.3977. [DOI] [PMC free article] [PubMed] [Google Scholar]