Abstract
Therapy of hormone receptor positive breast cancer (BCa) generally targets estrogen receptor (ER) function and signaling by reducing estrogen production or by blocking its interaction with the ER. Despite good long-term responses, resistance to treatment remains a significant issue, with approximately 40% of BCa patients developing resistance to ET. Mutations in the gene encoding ERα, ESR1, have been identified in BCa patients and are implicated as drivers of resistance and disease recurrence. Understanding the molecular consequences of these mutations on ER protein levels and its activity, which is tightly regulated, is vital. ER activity is in part controlled via its short protein half-life and therefore changes to its stability, either through mutations or alterations in pathways involved in protein stability, may play a role in therapy resistance. Understanding these connections and how ESR1 alterations could affect protein stability may identify novel biomarkers of resistance. This review explores the current reported data regarding posttranslational modifications (PTMs) of the ER and the potential impact of known resistance associated ESR1 mutations on ER regulation by affecting these PTMs in the context of ET resistance.
Keywords: breast cancer, ESR1, proteasome, posttranslational modifications, endocrine therapy
1. Introduction
The estrogen receptor (ER) is the main downstream effector of its ligand estrogen and has functions connected to the menstrual cycle, pregnancy, and lactation in females and in maintaining cardiovascular, nervous, musculoskeletal, and immune system functioning [1]. There are two subtypes of ER, namely ERα and ERβ, encoded by ESR1 and ESR2, respectively. These genes are located on separate chromosomes, ESR1 at position 6q24-27 and ESR2 at 14q22-24 [2,3,4]. Whilst highly similar, their ligand binding domains (LBD) differ, enabling specific physiological functions [1,5,6].
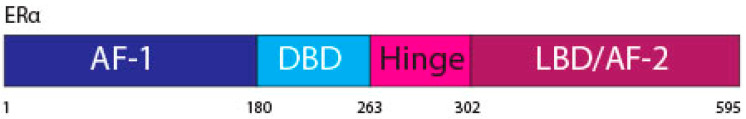
The ERα, a 66 kDa protein, is comprised of four domains, namely activation function 1 (AF-1), DNA binding domain (DBD), the hinge region, and the LBD also known as AF-2 [1,7] (Figure 1).
Figure 1.
ERα functional domains. The ERα functional domains include; Activation Function 1 (AF-1) (purple), DNA Binding Domain (DBD) (blue), hinge (pink), Ligand Binding Domain (LBD) and AF-2 (plum).
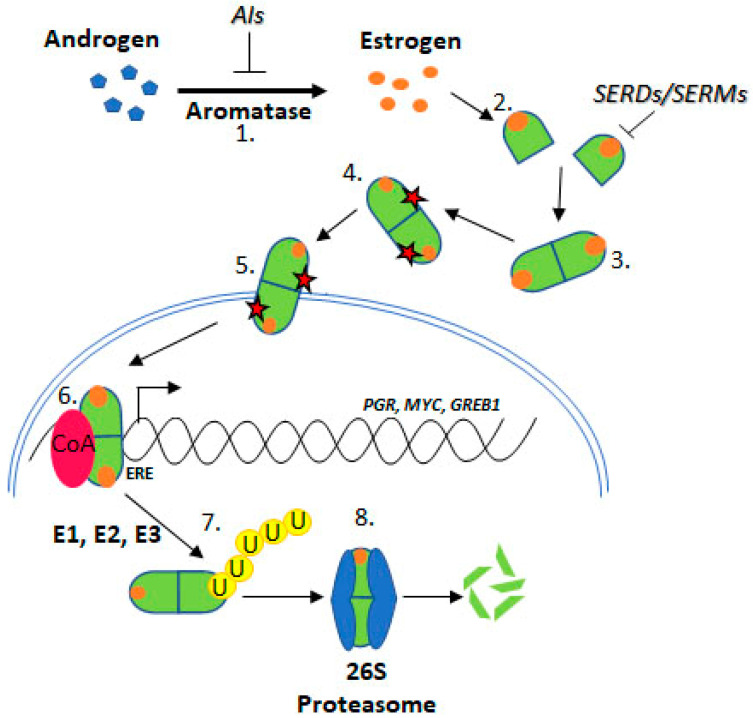
Upon estrogen binding, ER forms homodimers (ERα/ERα or ERβ/ERβ) and heterodimers (ERα/ERβ) [8,9]. This review focuses on ESR1 encoding ERα, referred to as ER henceforth. Following dimerisation, ER translocates to the nucleus and regulates transcription through estrogen response element (ERE) binding within target gene promoters (Figure 2, “genomic function”).
Figure 2.
Estrogen Receptor Signalling and ER Targeting Treatment. Aromatase converts androgens to estrogens, Estrogen receptor binds estrogen, Dimerisation, Post translational modification, Nuclear localisation, Coactivator binding and target gene (PGR, c-Myc, GREB1) transcription, Addition of ubiquitin by E1, E2 & E3 ligases, Degradation by the 26S proteasome. Aromatase Inhibitors (AIs) inhibit the enzyme aromatase, Selective Estrogen Receptor Degraders (SERDs) and Selective Estrogen Receptor Modifiers (SERMs) prevent estrogen binding.
Alternatively, ER may crosstalk with the PI3K-AKT-mTOR or MAPK pathways, in a “non-genomic” manner (see below), in both scenarios promoting cell proliferation and suppressing apoptosis [10].
Approximately 75% of BCa express ER, which promotes oncogenesis. As such, the ER is a common target for BCa treatment using endocrine therapies (ETs) including tamoxifen, fulvestrant, and aromatase inhibitors (AIs) [11] (Figure 2). Tamoxifen is known as a selective ER modifier (SERM) and fulvestrant as a selective ER degrader (SERD) [12]. SERMs competitively bind ER forming an inactive complex, by preventing coactivator interactions [12,13,14,15]. SERDs also competitively bind ER; however, their binding targets the receptor for proteasomal degradation [16,17,18]. AIs are a group of drugs that prevent the synthesis of the estrogen, through inhibition of aromatase [19,20,21]. AIs include letrozole, anastrozole, and exemestane. Whilst these treatments are initially effective for many ER positive BCa patients, resistance remains a significant issue.
Resistance to ET is common, approximately 30% of BCa patients acquire resistance [22,23]. ESR1 mutations have been identified in ET resistant BCa tumours. Several ESR1 mutations have been functionally characterised and confer key attributes associated with ET resistance, indicating mechanistic roles in resistance such as estrogen independence, increased transcription of ER target genes like PGR (progesterone receptor), GREB1 (growth regulation by estrogen in breast cancer 1), and MYC (c-myc), and increased proliferation and altered ER conformation [24,25] (Figure 2).
Since a major control of ER activity is through regulation of its half-life, changes to ER stability may influence sensitivity to ET. For example, posttranslational modifications (PTMs) and ESR1 mutations causing amino acid substitutions at PTM sites may influence ER stability, and ultimately activity. This review explores the link between ER PTMs and turnover, with a focus on ET resistance associated ESR1 mutations and their effects.
2. Estrogen Receptor Signaling
The estrogen/ER complex can result in activation of two distinct types of signaling pathways, the genomic and non-genomic. In the genomic pathway, the ER regulates gene transcription through direct binding of its DBD to promotors containing an ERE, or through interactions with other transcription factors at promoter regions [9,26]. The non-genomic pathway, however, enables rapid signaling through bidirectional crosstalk with PI3K-AKT-mTOR and MAPK pathways. These pathways are frequently upregulated in BCa and enable signaling in an estrogen independent manner [27,28,29]. Several kinases from these pathways phosphorylate the ER at various sites, mediating ER stability, localization, and transactivational capacity, discussed in detail below [30,31]. Further, these pathways may contribute to ET resistance through phosphorylation at key sites, even in the absence of estrogen [32,33,34,35,36,37]. Additionally, crosstalk between ER and PI3K-AKT-mTOR and MAPK pathways is bidirectional. The ER may activate these pathways through interaction with modulator of non-genomic action of estrogen receptor (MNAR) scaffold protein and subsequent SRC activation [38,39]. Ultimately, these pathways promote cell cycle progression through increased expression of cyclin D1, and suppress apoptosis [38,40]. Understanding these interactions is important as the PI3K and MAPK pathways are frequently active in ET resistant BCa and contribute to ET resistance [27,28,29].
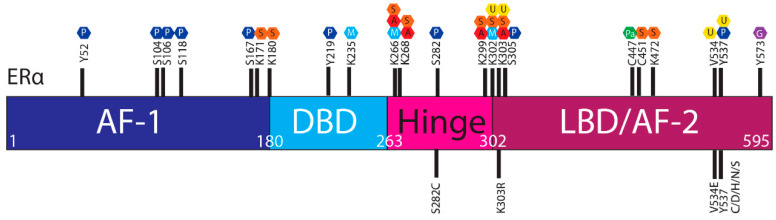
The ER is regulated by a range of PTMs including ubiquitylation, SUMOylation, phosphorylation, palmitoylation, acetylation, methylation and glycosylation [41,42,43,44]. These modifications are proposed to regulate the activity, stability, and interactions of ER with other proteins or DNA, and ESR1 mutations may influence PTMs and hence ER stability and function (Figure 3).
Figure 3.
Post translational modifications of ERα. The ERα functional domains include: Activation Function 1 (AF-1) (purple), DNA Binding Domain (DBD) (blue), hinge (pink), Ligand Binding Domain (LBD) and AF-2 (plum). At the top of the schematic are known sites PTMs of ERα; phosphorylation (P, dark blue), SUMOylation (S, orange), methylation (M, light blue), acetylation (A, red), ubiquitylation (U, yellow), pamiltoylation (Pa, green) and gycosylation (G, purple). At the bottom are PTM sites affected by ESR1 mutations.
2.1. Estrogen Receptor Turnover
Whilst ER is produced through transcription and protein synthesis, changes to ER degradation kinetics is the major factor determining ER levels. In BCa, there is an imbalance between the rate of transcription, synthesis and degradation of the ER leading to increased ER stability and thus activity [45]. The half-life of the ER differs significantly depending on estrogen exposure. Generally, the ER half-life is 3–5 h [46] and estrogen presence can reduce the half-life to just 1 h [47]. However, persistent estrogen exposure causes relative ER stability. In fact, in MCF-7 cells exposed to estrogen for 72 h, ER half-life was increased to 6 h, due to the decreased rate of proteolysis associated with p-S118 [48].
2.2. Degradation by the Ubiquitin Proteasome Pathway
Several studies have shown increased ER stability in the presence of the proteasome inhibitor, MG132, indicating that degradation by the ubiquitin–proteasome system (UPS) regulates ER stability [47,49,50,51]. Degradation of the ER occurs predominantly through the UPS, which relies on ER ubiquitylation by ubiquitin activating enzymes (E1) and ubiquitin conjugating enzymes (E2). Conversely, the ER may be protected from degradation through the activity of ubiquitin ligases (E3), which remove ubiquitin from the ER.
Ubiquitin conjugation or removal occurs on lysine residues, and mutations resulting in an exchange, either of such lysines or of amino acids affecting the accessibility of important lysines, may therefore alter the protein’s stability. Additionally, some UPS proteins act as coactivators of nuclear receptors and promote downstream gene transcription [16,44,52,53]. For example, ubiquitin ligase E3A (E6-AP) acts as an ER coactivator and increases gene transcription [16,53].
3. Post Translational Modifications
3.1. Ubiquitylation
The ER is regulated by both monoubiquitylation and polyubiquitylation and these serve distinct functions. Monoubiquitylation increases the stability and transcriptional activity of the receptor, whilst further addition of ubiquitin, polyubiquitylation, targets the protein for degradation by the UPS [53]. Some proteins have an inhibitory effect on ubiquitylation which leads to increased stability of the ER associated with ET resistance, broadly classified as coactivators, E3 ligases, kinases and scaffold proteins [45].
The K303 site is affected by an ESR1 mutation, K303R, and is a reported ubiquitination target. K302 and K303 have been implicated in ER stability and its nuclear localisation [52] (Table 1).
Table 1.
ER Posttranscriptional Modification Sites and Effects of Mutations.
| Site | Posttranslational Modification (Mediator) | Effect | ESR1 Mutations # | ET Resistant | Frequency | Functionally Tested |
|---|---|---|---|---|---|---|
| Y52 | Phosphorylation (c-Abl) |
Increased gene transactivation, increased DNA binding and dimerisation, rapid cell growth and increased invasive capacity [54] | None | N/A | N/A | N/A |
| S104 | Phosphorylation (Cyclin A/CDK2, MAPK ERK1/2, GSK3β) |
Increased gene transactivation, tamoxifen sensitivity, ER stability in absence of E2 [31,55] | None | N/A | N/A | N/A |
| S106 | Phosphorylation (MAPK ERK1/2, GSK3β) |
Increased gene transactivation, tamoxifen sensitivity, ER stability in absence of E2 [31,55] | None | N/A | N/A | N/A |
| S118 | Phosphorylation (CDK7, ERK1/2, IKKα, GSK3β, ILK, EGFR, IGF1R, DNA-PK, RET) |
Increased stability [48] | None | N/A | N/A | N/A |
| S167 | Phosphorylation (p90, RSK1, S6 K1, Akt, IKKƐ, CK2) |
Inhibits proteasomal degradation [30] | None | N/A | N/A | N/A |
| K171 | SUMOylation (SUMO3) |
Repressed gene transactivation, antiestrogen sensitivity [56] | None | N/A | N/A | N/A |
| K180 | SUMOylation (SUMO3) |
Repressed gene transactivation, antiestrogen sensitivity [56] | None | N/A | N/A | N/A |
| Y219 | Phosphorylation (c-Abl) |
Enhanced gene transactivation, increased DNA binding and dimerisation, rapid cell growth and increased invasive capacity [54] | None | N/A | N/A | N/A |
| K235 | Methylation (SMYND2) |
Repressed gene transactivation [44] | None | N/A | N/A | N/A |
| K266 | SUMOylation (SUMO-1) |
Repressed gene transactivation [57] | None | N/A | N/A | N/A |
| Acetylation (p300) |
Promotes DNA binding and transactivation capacity [58] | |||||
| Methylation (SET7, SMYND2) |
Repressed gene transactivation [44] | |||||
| K268 | SUMOylation (SUMO-1) |
Repressed gene transactivation [59] | None | N/A | N/A | N/A |
| Acetylation (p300) |
Enhances DNA binding and gene transactivation [60] | |||||
| S282 | Phosphorylation (CK2) |
Tamoxifen sensitivity, suppression of gene transactivation, ER stability [37,61] | S282C | Unknown | 0.3% (1/292) [62] | N/A |
| K299 | SUMOylation (SUMO1, SUMO2/3) |
Repressed gene transactivation, antiestrogen sensitivity [56,57] | None | N/A | N/A | N/A |
| Acetylation (p300) |
Not major target of acetylation, hinge lysines are preferentially acetylated [60,63] | |||||
| K302 | Ubiquitylation (BRCA1/BARD1) |
ER degradation, induced by estrogen or fulvestrant [52,64] | None | N/A | N/A | N/A |
| SUMOylation (SUMO-1) |
Repressed gene transactivation [59] | |||||
| Methylation (SET7/9, SMYD2) |
ER stability, recruitment to promoter [59] | |||||
| K303 | Ubiquitylation (BRCA1/BARD1?) | ER degradation, induced by estrogen or fulvestrant [52,64] | K303R | Yes, resistant to AIs and tamoxifen [33,65] | 49.81% (133/267) of invasive BCa [66] | In combination with S305, promotes crosstalk with growth factor pathways, and confers resistance to AIs and tamoxifen [32,33,65] |
| SUMOylation (SUMO-1) |
Enhances estrogen induced DNA binding and transcription [52] Repressed gene transactivation [57] |
|||||
| Acetylation (p300) |
Represses ER transactivation activity [63] | |||||
| S305 | Phosphorylation (PAK1, PKA) |
Tamoxifen resistance In the presence of the K303R mutation, enhances crosstalk with IGF-1/IRS/Akt pathway and aromatase inhibitor resistance [33,34,35,61,67] |
None | N/A | N/A | N/A |
| C447 | Palmitoylation (DHHC-7, DHHC-21) |
Membrane localisation [68] | None | N/A | N/A | N/A |
| C451 | SUMOylation (SUMO3) |
Sensitivity to fulvestrant and tamoxifen, through gene repression [69] | None | N/A | N/A | N/A |
| K472 | SUMOylation (SUMO3) |
Repressed gene transactivation, antiestrogen sensitivity [56] | None | N/A | N/A | N/A |
| V534 | Ubiquitylation (E6-AP ligase) |
ER degradation, induced by estrogen Subcellular localisation, gene transactivation and the degradation of the ER [70] |
V534E | Unlikely | 1/616 (0.16%) metastatic BCa [25] | No effect, neither constitutively active nor inactivating [25] |
| Y537 | Ubiquitylation (E6-AP ligase) |
ER degradation, induced by estrogen Subcellular localisation, gene transactivation and the degradation of the ER [70] |
Y537C | Yes | 6/616 (0.97%) metastatic BCa [25] | Ligand independent, somewhat resistant to tamoxifen, fulvestrant and estrogen deprivation [25,71] |
| Phosphorylation (SRC) |
Regulation of subcellular localisation, transcriptional activity and degradation of the ER [25,45] | Y537D | Unknown | 1/616 (0.16%) metastatic BCa [25] | Estrogen independent, increased activation of progesterone receptor [25] | |
| Y537H | Unknown | 1/56 (1.79%) cfDNA [72] | N/A | |||
| Y537N | Yes | 5/616 (0.81%) metastatic BCa [25] | Ligand independent, relatively resistant to tamoxifen, fulvestrant and estrogen deprivation [25,71] | |||
| Y537S | Yes | 13/616 (2.11%) metastatic BCa [25] | Constitutively active, adopts conformation that enhances coactivator binding, requires much higher concentrations of fulvestrant for inhibition of ER activities than WT [25] | |||
| S573 | Glycosylation (GALNT6) |
Nuclear localisation, gene transactivation [41] | None | N/A | N/A | N/A |
# reported mutations in breast cancer.
The wildtype (WT) K302/K303 ER sites stabilise ligand-free ER and estrogen-mediated ubiquitylation and increase ER transactivational capacity through nuclear translocation. Within the hinge region of the ER, between amino acids K299 and K303, is the nuclear localisation sequence. This sequence is also essential for polyubiquitination and degradation induced by fulvestrant. Mutagenesis of K302 and K303 to alanine (K302R and K303R) result in a disruption to the nuclear localisation sequence [16]. Additionally, lysines central to ubiquitin binding are removed, which causes reduced ER degradation thus, confirming their role in regulating ER stability and antiestrogen resistance [52]. The K302R and K303R mutants are resistant to ubiquitylation by breast cancer type 1 susceptibility protein (BRCA1), hence promoting ER stability [73] and opposing fulvestrant induced degradation [52]. However, some data suggest that BRCA1/BRCA1 associated RING domain 1 ubiquitylates K302/K303 mutant ER at alternative, nearby lysines instead lead to a reduced rate of degradation compared to WT [64].
The Y537 site, although not a lysine, is also important in ubiquitylation and subsequent degradation. In response to estrogen binding, ER associates with the proto-oncogene tyrosine-protein kinase Src (SRC). SRC phosphorylates the ER at various sites, including Y537 [70]. Y537 phosphorylation favours interaction of ER with E6-AP ligase, enhancing ER binding to target promoters [70]. Following ER driven gene transcription, the E6-AP ligase polyubiquitylates the ER targeting it for degradation [70]. Mutagenesis to Y537F results in reduced interaction with the E6-AP ligase, reduced transactivation of ER target genes, including GREB1 and pS2, and increased stability [70]
3.2. SUMOylation
Small ubiquitin-related modifier 1 (SUMO-1), shares structural similarities with ubiquitin and has a similar mechanistic pathway, involving activating, conjugating and ligase enzymes. Despite this, SUMO-1 has distinct functions to ubiquitin. The SUMO pathway regulates transcription, nuclear transport, cell growth, proliferation, apoptosis, and protein stability and activity, which are important cellular processes in carcinogenesis [57]. The SUMOylation pathway relies on the actions of activating (SUMO Activating Enzyme), conjugating (ubiquitin-conjugating enzyme E2) and ligase enzymes (protein inhibitor of activated STAT) [57]. Whilst the ER lacks the classical ΨKXE SUMOylation site, SUMOylation at lysines K171, K180, K266, K268, K299, K302, K303, and K472, within the hinge region, has been reported [56,57] (Table 1).
ER SUMOylation regulates the transcriptional activity of the receptor in response to estrogen and tamoxifen. Treatment with estrogen and with tamoxifen enhances SUMOylation required for transcriptional activity. In a study by Sentis et al. mutation of ER lysine to arginine mutations at several positions (K266, K268, K299, K302, and K303) significantly reduced SUMOylation and gene transactivation. However, in that study, several mutations were investigated simultaneously, which explains why the effects of individual lysine to arginine mutations were not assessed [57].
SUMOylation is required for fulvestrant induced transcriptional repression, and is associated with recruitment of corepressors and reduced chromatin accessibility [56,69]. In the presence of fulvestrant, SUMOylation may only allow transient DNA binding of the receptor, reducing overall transcription [69]. However, another study suggested that fulvestrant induces SUMOylation at K171, K180, K99, K472 sites. Furthermore, mutagenesis of L539A or L540A reduces this SUMOylation and hence promotes gene transcription in the presence of antiestrogens [56]. This notion is supported by the fact that the ET-resistance ER mutation V534E, which prevents SUMOylation, also enhances ER dependent gene transcription in the presence of fulvestrant [69]. Therefore, SUMOylation may be required for the effect of antiestrogens, and can be influenced by mutations in the LBD of the ER.
3.3. Phosphorylation
Phosphorylation is a common PTM regulating the activity of the ER, with various kinases phosphorylating approximately 20 ER sites. ER phosphorylation affects ligand binding, DNA binding, dimerisation, transcription, coactivator binding, protein stability, subcellular localisation, interactions with other PTM effectors, and cell growth and invasion [74]. Here, we focus on those involved in ER stability and ET resistance or occurring at sites of ESR1 mutations: Y52, S104, S106, S118, S167, Y219, S282, K303, S305, and Y537 (Table 1). Many studies have investigated the effects of ER phosphorylation, using mutagenesis to change amino acids at serine or tyrosine phosphorylation sites to either prevent (mutagenesis to alanine or phenylalanine, respectively) or mimic (serine to glutamic acid) phosphorylation. The data support the premise that S104, S106, and S118 phosphorylation is essential for ER transactivational activity. Moreover, alanine substitution inhibits, whilst a change with glutamic acid enhances, ER target gene transcription, compared to WT [31]. At ER S167 and S118 sites, phosphorylation loss results in increased growth and migration/invasive capacity, distinct gene expression patterns, and a reduction in apoptosis, in MCF-7 cells [75]. S167 phosphorylation, however, stabilises ER. In the presence of the protein synthesis inhibitor, cycloheximide, in 293T cells ectopically expressing ER S167A, its levels were reduced compared to ectopic WT ER. MG132 restored ER levels in S167A mutant expressing cells, demonstrating regulation of stability by the UPS [30].
ER S118A and S118E mutants on the other hand were more stable than WT ER, and S118E displayed higher transcriptional activation capacity, whilst S118A reduced gene transcription, compared to WT. This suggests that the S118 site has mechanistically distinct roles in regulating ER degradation and ER transcriptional activity [76]. Following estrogen exposure and subsequent gene transcription, a portion of the total receptor pool are ubiquitylated leading to degradation; this response is rapid, occurring within the first 24 h [48]. Meanwhile, another portion of ER is phosphorylated at S118, effectively preventing ubiquitination and thus degradation. Thus, over time, 24–72 h post estrogen addition, the rate of proteolysis decreases [48]. Thus, the S118 site of ER maybe central to controlling the tight balance of activity and protein turnover.
Phosphorylation at Y52 and Y219 ER sites by c-Abl individually enhances gene transcription and ER stability [54]. Y219 phosphorylation also promotes DNA binding and dimerisation [54]. Mutagenesis of these sites (Y52F and Y219F) causes a reduction in cell number and invasive capacity [54]. Interestingly, c-Abl also inhibits the proteasome, through phosphorylation of a subunit known as PSMA7, and thus may reduce ER degradation [54]. c-Abl extends the half-life of the ER from 6 h (c-Abl inhibited) to 12 h (c-Abl active), with no observable change in the mRNA levels of ER [54]. Likewise, inhibition of the 26S proteasome by MG132 extends the half-life of ER, even after c-Abl inhibition [54].
Phosphorylation also regulates tamoxifen response. The effect of tamoxifen on the ER is context dependent in that it can either block ER (antagonist) in breast tissue and it can promote ER activity (agonist) in other tissues through activation of AF-1 [77]. For instance, phosphorylation of S104, S106 and S118 promotes tamoxifen agonist activity in the breast [31]. COS-1 cells expressing S106E, mimicking phosphorylation, had greatest activity followed by S104E and S118E, in the presence of tamoxifen [31]. Meanwhile, phosphorylation of the S282 site is thought to contribute to tamoxifen sensitivity. Patients treated with tamoxifen with phosphorylated S282 ER had longer progression free survival (PFS) and overall survival (OS) than patients lacking phosphorylation at this site [37]. The phosphorylation at S282 also plays an important role in ER stability. COS-1 cells ectopically expressing ER S282A mutant displayed reduced mutant ER levels at 24 h, but not as early as 3 h, of estrogen exposure, compared to WT ER expressing cells [61].
The S305 ER site is phosphorylated by protein kinase A (PKA) and p21-activated kinase 1 (PAK1), and, in some cases, by Aurora Kinase A and AKT [33,67,78,79]. Phosphorylation of S305 in K303R ER mutants enhances interaction with insulin-like growth factor 1 (IGF-1) and is associated with constitutive phosphorylation of IGF-1 and insulin receptor substrate (IRS); promoting cell growth [33]. This cell growth is reduced by inhibiting IGF-1 receptor (IGF-1R) with the tyrosine kinase inhibitor, Tyrphostin AGTreatment with both the AI substrate androstenedione and IGF-1 resulted in greater growth of K303R mutant cells, than with either of these ligands independently [33]. These data provides further evidence of the crosstalk between K303R ER and the IGF-1/IRS/AKT pathway and suggest that phosphorylation of S305 plays critical roles in ER protein interactions and in AI resistance [33].
ER S305 phosphorylation by PKA and PAK1 is associated with tamoxifen resistance and is a potential predictive marker of tamoxifen treatment response [34,35,80]. S305 phosphorylation causes tamoxifen bound ER to remain in its active conformation, thereby promoting resistance [35]. Indeed, BCa patients with tumours that had nuclear PAK1 expression and phosphorylated ER S305, had significantly reduced responses to tamoxifen; nuclear expression of phosphorylated ER S305 was observed in 36% of patients and showed a trend towards reduced tamoxifen response [80]. However as less than 10% of tumours had both phosphorylated ER S305 and nuclear PAK1 expression, this suggests some redundancy and other kinases, such as PKA, may also be involved in the phosphorylation of ER S305 [80]. It was proposed that PKA phosphorylates tamoxifen bound ER at the S305 site, and this alters its conformation such that the coactivator SRC can facilitate transcription factor complex assembly and localisation to target promoters, to enable gene transcription in the presence of tamoxifen [67]. Indeed, activation of PKA through the down regulation of a negative regulator of PKA, known as PKA-Riα, was predictive of tamoxifen resistance and resulted in a growth stimulatory effect in the presence of tamoxifen, interestingly not observed when treated with fulvestrant [35]. These studies suggest that phosphorylation of ER S305, by either PKA or PAK1, is linked with resistance to tamoxifen and AIs.
The Y537 site is phosphorylated by SRC, following ER ligand binding. As outlined above, p-Y537 attracts E6-AP ubiquitin ligase, promoting transactivational activity and ultimately degradation, linking these PTMs functionally [70]. ER Y537 phosphorylation promotes cytoplasmic localisation, however, is associated with increased proliferation [81]. While it remains counterintuitive that cytoplasmic p-Y537 ER increases proliferation, it was speculated that proliferation occurs as a result of growth signaling pathway interactions which promote cell cycle progression [81]. Indeed, there is evidence that p-Y537, while less transcriptionally active, cooperates with phosphorylated SRC to drive proliferation via the AKT pathway and downstream cyclin D1 upregulation [81]. In MDA-MB-231 cells ectopically expressing ER Y537F, ER is retained in the nucleus, preventing its extranuclear activities [70]. There, ER Y537F is stabilised likely due to a lack of E6-AP interaction needed for proteasomal degradation within the nucleus [70] These data highlight the importance of Y537 in ER regulation and may help explain its frequency as AI resistance associated ER mutations. Further study is needed to fully elucidate the effects of p-Y537 and the effects of loss of this functional PTM via amino acid substitutions.
One resistance associated change is Y537S, and the substituted serine may be a target of phosphorylation but that has not been investigated to-date. One study, however, observed increased S118 phosphorylation for ER Y537S mutants [82], associated with increased ER stability [48].
It is evident that a large proportion of ER phosphorylation is mediated by kinases belonging to the PI3K-AKT-mTOR and MAPK pathways, mentioned earlier in the context of non-genomic ER signaling. Signaling through these pathways abrogates the necessity for ER binding and contributes to ET resistance. For example, phosphorylation of S167 on K303R mutated ER by AKT, leading to aromatase inhibitor resistance [30,32]. Phosphorylation of ER at S167 by AKT has also been shown to promote ER stability and activate ER mediated transcription in an estrogen independent manner [30,32,83]. Furthermore, ER Y537 phosphorylation by SRC promotes promoter occupancy and gene transcription [70]. These studies demonstrate estrogen independent ER signaling through crosstalk mediated by kinases. Later, potential therapeutics targeting these resistance mechanisms are discussed.
3.4. Palmitoylation
Palmitoylation of the ER is important for its stabilisation and localisation. Palmitoylation at C447 drives the association of ER with caveolin-1, which results in membrane localisation and favours non-genomic ER actions (see above) [84]. ER-estrogen interaction promotes removal of palmitoyl groups, the dissociation of caveolin-1, and hence nuclear localisation and ultimately degradation [43,84]. Inhibition of palmitoylation, with 2-bromo-hexadecanoic acid or by C447A mutation, increased ER degradation at all time points investigated, up to 8 h post estrogen treatment [43]. Interestingly, this resulted in reduced ER stabilising S118 phosphorylation, further highlighting relationships between different PTMs at various ER sites [43,48].
3.5. Acetylation
Acetylation of the ER occurs within the hinge and LBD region, by the actions of p300/CREB-binding protein at the sites K266, K268, K299, K302, and K303 (Table 1) [60,63]. The effect of acetylation varies dependent on the site. Acetylation at K266 and K268 promotes DNA binding and transactivation capacity [60]. Conversely, acetylation at K302 and K303 represses ER transactivation activity [63]. Phosphorylation at S305 site prevents the acetylation at K303 [33] in turn hypersensitising the ER to estrogen [85]. The ER K303R change, identified in both breast hyperplasia and BCa tissue [66,86] therefore confers estrogen hypersensitivity and prolongs ER stability.
3.6. Methylation
Methylation occurs on lysine residues and is catalysed by the histone lysine methyltransferases SET7 and SET and MYND domain containing 2 (SMYND2). SET7 methylates ER at K302 and thereby enhances ER stability, mediates target promoter recruitment and directly competes with ubiquitination, which increases ER stability [59]. ER lysine methylation may also promote interaction with proteins, such as calmodulin, indirectly preventing ubiquitylation mediated by E6-AP also increasing ER stability [59].
The ER hinge region enables the coordination of multiple PTMs in response to the presence/absence of estrogen. For example, K266 methylation and acetylation is dependent on estrogen levels. K266 methylation by either SET7 or SMYND2 represses transactivation activity by preventing ER chromatin recruitment in the estrogen deprived setting [44]. Upon estrogen binding, K266 is demethylated by histone H3K4 demethylase lysine-specific demethylase 1 [44]. Subsequently, p300/CBP acetylates the ER, permitting chromatin recruitment and gene transcription [44]. K235 is also methylated by SMYND2, in the absence of estrogen, acting to repress gene transcription. Crosstalk between methylation and acetylation at this site is mediated by the transcriptional coactivator euchromatin histone methyltransferase 2, which recognises demethylated K235 [87]. This results in recruitment of the ‘PHD finger protein’/’males absent on the first’ complex, which is responsible for the acetylation of the ER and results in transcriptional activity [87].
3.7. Glycosylation
Glycosylation of S573, facilitated by a polypeptide known as N-acetylgalactosaminyltransferase 6 (GALNT6), promotes nuclear localisation, transcriptional activity and stability of the ER (Table 1). In T47D and MCF-7 cells, siRNA knockdown of GLANT6, results in reduced ER nuclear localisation and expression of ER target genes (MYC, CCND1 and CTSD) and this was generally irrespective of estrogen presence [41]. Hence, S573 glycosylation by GLANT6 is an important regulator of ER localisation and transcriptional activity [41].
4. Clinical Relevance
ER signaling remains central to the treatment of ER positive BCa, and PTMs play a significant role in determining responses to ET, alongside ESR1/ER mutations. Table 1, outlines the functions of common ER PTMs, including phosphorylation, acetylation, ubiquitylation and SUMOylation, and known ESR1/ER mutations at these sites. Resistance mechanisms to ET are complex, and likely involve changes to number of pathways with ER at a central hub. While ER PTMs and their dysregulation due to mutations would affect the interactions of ER with several signaling pathways, including growth signaling and proteasomal degradation pathways, this presents an opportunity whereby combination therapies with drugs targeting these pathways may help to re-sensitise tumours to ET.
4.1. Estrogen Receptor Mutations and Resistance
Several ESR1 mutations have been identified. The general consensus is that these mutations may cause conformational changes that affect drug binding and/or ER activity. For this review it is important to emphasise that four key mutation sites are also sites of PTMs, namely S282C, V534E, K303R and Y537C/N/S, described below (Table 1).
4.1.1. S282C
The S282C ESR1 mutation was identified in a single BCa tumour [62]. Functionally, the effect of this mutation has not been tested, but p-S282 has been proposed to inhibit ligand dependent activation of the ER. The S282A ER mutation prevents phosphorylation and increases ligand independent transcriptional activity compared to WT [61]. The S282C mutation detected in a patient’s tumour tissue would likely also prevent phosphorylation and increase ligand independent ER transactivation activity. Due to its rarity, the clinical relevance of this mutant, however, may be minimal.
4.1.2. K303R
The K303R ESR1 mutation was first identified in breast typical hyperplasia patients, with a frequency of 34% in (20/59) of ET resistant BCa patients [86]. In invasive BCa, K303R was detected in 50% (133/267) of patients and was associated with reduced 10-year recurrence free survival, larger tumour size and lymph node involvement [66]. Functional testing showed that ER K303R is hypersensitive to estrogen, binds to PI3K to promote growth and survival via the PI3K/pathway, and in combination with p-S305, promotes signaling through the IGF-1R/IRS-1/AKT pathway. It is through these pathways that the K303R mutation may promote resistance to tamoxifen and anastrozole [32,33,65]. The effect of K303 is mediated by PTMs and connected to other posttranslational events as the phosphorylation of S305 inhibits acetylation of K303 resulting in ER inhibition [85]. Some of these functional changes may be based on the K303 site being a common PTM site for ubiquitylation, SUMOylation and acetylation, dependent on the context. Thus, a substitution from lysine to arginine at position 303 likely has important implications for ER activity.
4.1.3. Y537C/S/N
There are number of mutations identified at Y537, including Y537C, Y537D, Y537H, Y537N, and Y537S [25,45]. P-Y537 is critical to control ligand binding, DNA binding, dimerisation, transcription, coactivator binding, protein stability, subcellular localisation, interactions with other PTMs, and cell growth and invasion [58]. Y537N and Y537S were detected in 13.89% of biopsies from patients with hormone resistant tumours and accounted for over half of all detected ESR1 mutations [24]. Y537S confers resistance to fulvestrant treatment, and is associated with reduced PFS, and occurs at a higher frequency following fulvestrant treatment 8.7% (17/195) compared to 1.5% (3/196) in advanced BCa patients [88]. In another study, ESR1 mutations were detected in CTCs exclusively from patients treated with estrogen deprivation therapy, and of the 13 patients with ESR1 mutations detected in CTCs, 23% (3/13) had Y537C/N mutations [89]. The outlined importance of PTMs at the Y537 site suggests that ESR1 Y537 mutations may at least in part cause resistance by affecting ubiquitylation and phosphorylation and the connected molecular outcomes of these PTMs.
4.2. Other PTM Sites and Resistance
S167 and S118
Several studies have investigated the effect of phosphorylation at S167 and S118 and the resulting sensitivity to tamoxifen. Reports with regard to p-S167 are conflicting with some studies observing no association, some reporting trends of association and others showing correlation, between phosphorylation loss and tamoxifen resistance [90,91,92,93]. The effect p-S118 site is also controversial. In patients with primary tumours expressing p-S118, it was reported that tamoxifen treatment assured longer disease-free survival (DFS) and a trend towards better OS [94]. Conversely, another study demonstrated that patients whose primary tumours were positive for p-S118 had significantly shorter DFS and OS after treatment with tamoxifen [91]. Low phosphorylation levels at S118 was associated with improved DFS and OS [63] and elevated p-S118 levels were associated with relapse following tamoxifen treatment [95]. Interestingly, another study investigated the effect of the S118P variant on endocrine response and found no significant difference in response to either tamoxifen or fulvestrant [96]. Whilst these studies may differ in patient cohorts and methods, it is possible that the effect of the phosphorylation is context dependent and may relate to other PTMs and pathways. A number of studies have observed tamoxifen resistance in association with p-S305 in both in vitro studies and in patient cohorts [97,98].
4.3. Treatments
Treatment of metastatic ER positive BCa is challenging with 30 of patients developing resistance to ET [22,23]. Therapy options for these patients can be broadly categorised into one of three groups, based on their targets: (i) those specifically targeting the ER, (ii) those targeting ER signaling pathways, and (iii) those targeting alternative pathways [99]. Treatment can be a monotherapy or a combination of drugs from these different categories, targeting mutated ER, degradation (proteasome inhibitors), or kinase pathways (Table 2).
Table 2.
Current and Potential Therapeutic Targets in Breast Cancer.
| Treatment | Target | Experimental/Clinical Trial/Current Treatment | Outcome/Conclusion |
|---|---|---|---|
| Aromatase Inhibitors (Anastrozole, Exemestane, Letrozole) | Aromatase | Current | The proliferation marker, Ki67, was significantly suppressed by anastrozole (76%) after 2 weeks of treatment compared to tamoxifen (62%) and the combination (64%) [12] |
| Tamoxifen | ER (SERD) | Current | 5-yr adjuvant tamoxifen use results 47% reduction in recurrence [12] |
| Fulvestrant | ER (SERM | Current | Greater suppression of ER, PgR and Ki-67 was observed in the higher dose fulvestrant [12] |
| Cyclin-dependent kinase 4/6 inhibitors (CDKIs) | Cyclin-dependent kinase 4/6 | Current | CDKI treatment in combination with ET extends PFS by a median of 8.8 months [100] |
| H3B-5942 | ER (SERCA) | Experimental | Greater antiproliferative effect than fulvestrant. Has synergistic effect when combined with CDK4/6 and mTOR inhibitors [101] |
| AZD9496 | ER | Trial | Disease stabilisation [25,102,103,104] |
| Bortezomib | Proteasome inhibitor | Experimental | Inhibit cell growth of both ER+ and ER- cells [49,50,51] |
| FK228 | Histone deacetylase inhibitor | Trial | Combined with vorinostat and tamoxifen results in tumour regression [105,106] |
| Vorinostat | Histone deacetylase inhibitor | Trial | Show tumour regression with FK228 [106] |
| Capivasertib | AKT inhibitor | Trial | Patients who received capivasertib plus fulvestrant had a median PFS of 10.3 months compared to 4.8 months in patients who received a placebo plus fulvestrant, warranting further investigation, in a phase III trial [107] |
| Alisertib | Aurora Kinase A inhibitor | Trial | In combination with fulvestrant demonstrated anti-tumour activity [108] |
| FRAX1036 | PAK1 inhibitor | Experimental | Acts synergistically with alisertib with greater efficacy [109] |
| Dasatinib | SRC and AbI inhibitor | Experimental | In combination with letrozole was promising in 71% of patients [110] |
| Saracatinib (AZD0530) | SRC inhibitor | Experimental | In combination with fulvestrant had a greater effect at reducing proliferation than alone [111,112] |
| Bosutinib | SRC inhibitor | Experimental | Had an unfavourable risk-benefit ratio [113,114] |
4.3.1. Targeting ESR1 Mutants
Currently, drugs targeting the ER are categorised as either SERDs or SERMs. Many patients treated with monotherapies of fulvestrant or tamoxifen, for example, develop resistance, in part due to acquired ESR1 mutations. Novel therapy options for these patients are arising including a novel drug, H3B-5942, which falls into a new ER target category coined “Selective Estrogen Receptor Covalent Antagonists” [101]. H3B-5942 covalently binds to the ER cysteine at position 530, which is located within helix 11 in the ligand binding pocket. ER mutations, at Y537 and D538, are known to stabilise the agonist conformation of the ER [101]. However, upon binding of H3B-5942 an antagonist conformation is adopted, regardless of the presence or absence of the Y537S or D538G ESR1 mutation [101]. Compared with fulvestrant, H3B-5942 has a greater antiproliferative effect and increased the suppression of ER target genes [101]. Additionally, CDK4/6 inhibitors and mTOR inhibitors, have a synergistic effect when combined with H3B-5942, resulting in greater antiproliferative effects than monotherapy alone [101].
A novel SERD, known as AZD9496, showed anti-tumour activity of AZD9496 in the ESR1 Y537S mutant in in vitro models, with greater potency than fulvestrant [25,104]. It was also effective in a CTC-174 ER positive BCa patient derived xenograft (PDX) model with the D538G ESR1 mutation [104]. In a phase I clinical trial for the treatment of ER+/HER- BCa with AZD9496 patients, there was evidence of prolonged disease stabilisation, with good drug tolerability by patients [102]. These data suggest, that AZD9496 may be an effective treatment option for BCa patients with Y537S and D538G mutations. However, in a window-of-opportunity presurgical study, treatment with AZD9496 for two weeks was not superior to fulvestrant at the dose tested [103].
4.3.2. Clinical Proteasomal Inhibition
Proteasome subunits are frequently upregulated and exhibit increased activity in a variety of cancers including BCa [115]. A proteasome inhibitor, bortezomib, has been FDA approved for the treatment of multiple myeloma [116] and several studies are currently investigating its therapeutic potential of in ER positive BCa.
Short-term exposure to bortezomib has been shown to increase ER stability. However, chronic exposure to proteasome inhibition results in reduced transcription of ESR1 [49,50,51]. Bortezomib is thought to cause chromatin changes of a distal enhancer region of ESR1 reducing its transcription and consequently ER accumulation [50]. Another study observed a downregulation of ER, Erb-B2 Receptor Tyrosine Kinase 2 (HER2), and epidermal growth factor receptor (EGFR) expression that led to a reduction in PI3K-Akt, mTOR, and MAPK signaling [117].
Bortezomib also inhibits cell growth in ER BCa positive cell lines, by increasing mRNA levels of the cyclin dependent kinase inhibitor (CDKI), p21, causing cell cycle arrest [118]. Interestingly, silencing of the ER prevented the effects of bortezomib, suggesting that ER is required for this p21 regulation [118]. In MCF-7 cells, the combination of bortezomib and tamoxifen inhibited cell growth by 70% [118].
As a proteasome inhibitor, bortezomib has the potential to affect many protein types, and how this contributes to treatment response or toxicity is largely ill defined. The drug was well tolerated in a single agent clinical trial in metastatic BCa patients but had little beneficial effect [119]. Multiple studies have demonstrated that combination therapy of bortezomib and SERDs are effective in the treatment of BCa, including in the ET resistant setting. A randomised phase II trial with the combination of fulvestrant and bortezomib for the treatment of AI resistant metastatic BCa found significantly improved PFS (28.1%), compared to fulvestrant alone (13.6%), despite the median PFS remaining similar. Patients who progressed on fulvestrant alone, were able to change to the combination arm, and in this group PFS was at 18% for a minimum of 24 weeks [120].
Fulvestrant causes the accumulation of newly synthesised ER aggregates in the cytoplasm. In the presence of bortezomib, these aggregates are not degraded and hence build up within the cytoplasm, leading to the initiation of what is described as the “proapoptotic unfolded protein response”, leading to cell death [121]. For any treatment, identification of patient groups that are likely responders is essential; one study identified a proteasome signature which was associated with poorer patient outcomes and demonstrated that MCF10A cells expressing this signature were susceptible to Bortezomib treatment [116].
4.3.3. Targeting Kinases
ER p-S305 is strongly associated with ET resistance. This site is phosphorylated by PAK1, PKA, Aurora Kinase A or AKT [33,78] and overexpression of PAK1 and PKA is associated with poorer patient outcomes in BCa. Additionally, both PAK1 and PKA induced S305 phosphorylation are strongly correlated with reduced time to progression. Patients with p-S305 progressed in nine months, compared with 18 months seen in patients without PAK1/PKA associated S305 phosphorylation [97]. The ESR1 K303R mutation, which is associated with tamoxifen and AI resistance, increases the efficiency of S305 phosphorylation [32,33,78]. As this site may be phosphorylated by three different kinases, targeted therapy could be challenging, but may also provide the opportunity to target based on context. Several studies have demonstrated that inhibiting S305 phosphorylation, in in vitro and in xenograft models, may re-sensitise ET-resistant tumour cells to ET and cause increased apoptosis.
A clinical trial has investigated the combination of alisertib with fulvestrant as a therapeutic option for BCa patients [108]. Alisertib is a drug which targets Aurora Kinase A, which is another kinase associated with ET resistance and which phosphorylates the ER at S305 [79]. In a phase I study, the combination of alisertib and fulvestrant had a positive anti-tumour activity, in ET resistant patients, which had been previously treated with tamoxifen and AIs. A six-month clinical benefit rate was achieved in 77.8% of patients [108].
FRAX1036 is PAK1 inhibitor and has been combined with Alisertib with promising results in a range of BCa cell lines, and in BT474 xenograft models. The combination acts synergistically, to inhibit growth and ER signaling and reduces cell survival and its greatest efficacy was observed in hormone receptor positive/HER2 positive BCa cell lines [109]. Furthermore, it was observed that this combination inhibits phosphorylation of ER S305 and S118 in BT447 and T47D cell lines, and prevents PAK1 and ER signaling in BT474 xenograft models [109].
PAK1 activation can be blocked by the histone deacetylase inhibitor, FK228, which suppresses estrogen dependent growth in MCF-7 cells, and blocks growth in tamoxifen sensitive and resistant xenograft models [105]. Other histone deacetylase inhibitors have shown promising results in treating ET resistant BCa including a phase II study where 40% of patients resistant to AIs achieved tumour regression or disease stabilisation in response to the combined treatment with histone deacetylase inhibitor, vorinostat, and tamoxifen [106].
As mentioned previously, AKT can phosphorylate S305, in the presence of K303R. Given the significant crosstalk between the PI3K/AKT pathway and the ER, it could be a potential therapeutic target. In a phase II study, an AKT inhibitor, capivasertib, was tested in combination with fulvestrant in patients who had progressed on AIs. Patients who received capivasertib plus fulvestrant had a median PFS of 10.3 months compared to 4.8 months in patients who received a placebo plus fulvestrant, warranting further investigation in a phase III trial [107].
4.3.4. Targeting Coactivators
Another approach to the treatment of ET resistant BCa is to identify druggable targets in the resistance pathways. ER Y537S and D538G expressing BCa cells are reliant on SRC activity. Unlike WT, these ER mutants can bind the coactivator SRC, even in the absence of estrogen [96,122]. As such, SRC inhibition may be an effective therapeutic option. The combined treatment with a SRC inhibitor, SI-1, and the SERD AZD9496 resulted in a significant reduction in tumour volume compared with monotherapy and controls, in a PDX ER Y537S expressing mouse model [122].
Several studies have also investigated SRC inhibitor potential in ET resistant BCa, particularly combination with AIs or SERDs. The combination of the AI, letrozole, and the SRC inhibitor dasatinib resulted in a clinical benefit rate (the percentage of patients with complete response, partial response or stable disease ≥6 months) of 71% for patients treated with the combination, 66% for those treated with letrozole alone and 23% for those that progressed on letrozole alone and crossed over to the dasatinib/letrozole combination [110]. It was proposed that the addition of dasatinib may delay resistance to letrozole [110].
Saracatinib (AZD0530), another SRC inhibitor, may also be effective in combination with ET, such as fulvestrant or AIs. The combination of saracatinib with fulvestrant reduced proliferation and to a greater extent than either drug alone in both MCF-7Arom5 cells, which express aromatase, and xenograft mouse models, suggesting a synergistic effect [111]. The combination of saracatinib and anastrazole achieved greater cell cycle arrest than either drug alone, and in xenograft models had greater antitumour activity, supporting further clinical investigation [112].
5. Conclusions
The ER and its signaling remain central to BCa treatment and ET resistance poses significant challenges. Since PTMs significantly modify ER functions, including protein interactions, subcellular localisation, estrogen sensitivity, transactivation capacity, and stability, amino acid substitution mutations altering PTM sites may dramatically change ER effects and responses to ET. The S282, K303, and Y537 sites play key roles in ER regulation and are sites of ESR1 mutations associated with ET resistance. Mutations at these sites will prevent ubiquitination (K303 and Y537), SUMOylation (K303), phosphorylation directly (S282, Y537, and indirectly at S305), and acetylation (K303). Here, we reviewed ample evidence that these changes affect ER function and half-life and ultimately change the response to ET. This review has highlighted the factors contributing to ET resistance and promising therapeutic options for the treatment of ET resistant BCa, particularly in patients with ESR1 mutations.
Author Contributions
Conceptualization, S.A.J. and T.M.B.; literature search and review, S.A.J.; figures/tables, S.A.J. and B.P.; drafting, S.A.J., B.P. and T.M.B.; critical review of work, B.P., B.B., K.M., P.S., A.F., H.N., P.d.S. and T.M.B. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a grant (13/TRC/1-01) from the Cancer Institute NSW through the CONCERT Translational Cancer Research Centre, S.A.J. is a recipient of an Ingham Institute PhD Scholarship, generated by the Liverpool Catholic Club. B.P. is funded through a Clinical Academic Group Seed Grant from the Sydney Partnership for Health, Education, Research and Enterprise (SPHERE). A.F. received funding through the German Academic Exchange Service (DAAD; project-ID 57390343).
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Yaşar P., Ayaz G., User S.D., Güpür G., Muyan M. Molecular mechanism of estrogen-estrogen receptor signaling. Reprod. Med. Boil. 2016;16:4–20. doi: 10.1002/rmb2.12006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Menasce L., White G., Harrison C.J., Boyle J. Localization of the Estrogen Receptor Locus (ESR) to Chromosome 6q25.1 by FISH and a Simple Post-FISH Banding Technique. Genomics. 1993;17:263–265. doi: 10.1006/geno.1993.1320. [DOI] [PubMed] [Google Scholar]
- 3.Enmark E., Pelto-Huikko M., Grandien K., Lagercrantz S., Lagercrantz J., Fried G., Nordenskjöld M., Gustafsson J.-A. Human Estrogen Receptor β-Gene Structure, Chromosomal Localization, and Expression Pattern. J. Clin. Endocr. Metab. 1997;82:4258–4265. doi: 10.1210/jc.82.12.4258. [DOI] [PubMed] [Google Scholar]
- 4.Gosden J., Middleton P., Rout D. Localization of the human oestrogen receptor gene to chromosome 6q24→q27 by in situ hybridization. Cytogenet. Genome Res. 1986;43:218–220. doi: 10.1159/000132325. [DOI] [PubMed] [Google Scholar]
- 5.Mosselman S., Polman J., Dijkema R. ERβ: Identification and characterization of a novel human estrogen receptor. FEBS Lett. 1996;392:49–53. doi: 10.1016/0014-5793(96)00782-X. [DOI] [PubMed] [Google Scholar]
- 6.Paech K., Webb P., Kuiper G.G.J.M., Nilsson S., Gustafsson J.-Å., Kushner P.J., Scanlan T.S. Differential Ligand Activation of Estrogen Receptors ER and ER at AP1 Sites. Science. 1997;277:1508–1510. doi: 10.1126/science.277.5331.1508. [DOI] [PubMed] [Google Scholar]
- 7.Kumar V., Green S., Stack G., Berry M., Jin J.-R., Chambon P. Functional domains of the human estrogen receptor. Cell. 1987;51:941–951. doi: 10.1016/0092-8674(87)90581-2. [DOI] [PubMed] [Google Scholar]
- 8.Cowley S.M., Hoare S., Mosselman S., Parker M.G. Estrogen Receptors α and β Form Heterodimers on DNA. J. Boil. Chem. 1997;272:19858–19862. doi: 10.1074/jbc.272.32.19858. [DOI] [PubMed] [Google Scholar]
- 9.Kumar V., Chambon P. The estrogen receptor binds tightly to its responsive element as a ligand-induced homodimer. Cell. 1988;55:145–156. doi: 10.1016/0092-8674(88)90017-7. [DOI] [PubMed] [Google Scholar]
- 10.Brown K.K., Toker A. The phosphoinositide 3-kinase pathway and therapy resistance in cancer. F1000Prime Rep. 2015;7:13. doi: 10.12703/P7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allred D.C., Brown P., Medina D. The origins of estrogen receptor alpha-positive and estrogen receptor alpha-negative human breast cancer. Breast Cancer Res. 2004;6:240–245. doi: 10.1186/bcr938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel H.K., Bihani T. Selective estrogen receptor modulators (SERMs) and selective estrogen receptor degraders (SERDs) in cancer treatment. Pharmacol. Ther. 2018;186:1–24. doi: 10.1016/j.pharmthera.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Jordan V. Antitumour activity of the antiestrogen ICI 46,474 (Tamoxifen) in the dimethylbenzanthracene (DMBA)—Induced rat mammary carcinoma model. J. Steroid Biochem. 1974;5:354. doi: 10.1016/0022-4731(74)90388-4. [DOI] [Google Scholar]
- 14.Jordan V.C. Biochemical pharmacology of antiestrogen action. Pharmacol. Rev. 1984;36:245–276. [PubMed] [Google Scholar]
- 15.Shiau A.K., Barstad D., Loria P.M., Cheng L., Kushner P.J., Agard D.A., Greene G.L. The Structural Basis of Estrogen Receptor/Coactivator Recognition and the Antagonism of This Interaction by Tamoxifen. Cell. 1998;95:927–937. doi: 10.1016/S0092-8674(00)81717-1. [DOI] [PubMed] [Google Scholar]
- 16.Casa A.J., Hochbaum D., Sreekumar S., Oesterreich S., Lee A.V. The estrogen receptor alpha nuclear localization sequence is critical for fulvestrant-induced degradation of the receptor. Mol. Cell. Endocrinol. 2015;415:76–86. doi: 10.1016/j.mce.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Dauvois S., Danielian P.S., White R., Parker M.G. Antiestrogen ICI 164,384 reduces cellular estrogen receptor content by increasing its turnover. Proc. Natl. Acad. Sci. USA. 1992;89:4037–4041. doi: 10.1073/pnas.89.9.4037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dauvois S., White R., Parker M.G. The antiestrogen ICI 182780 disrupts estrogen receptor nucleocytoplasmic shuttling. J. Cell Sci. 1993;106:1377–1388. doi: 10.1242/jcs.106.4.1377. [DOI] [PubMed] [Google Scholar]
- 19.Dowsett M., Jones A., Johnston S.R., Jacobs S., Trunet P., Smith I. In vivo measurement of aromatase inhibition by letrozole (CGS 20267) in postmenopausal patients with breast cancer. Clin. Cancer Res. 1995;1:1511–1515. [PubMed] [Google Scholar]
- 20.Geisler J., King N., Anker G., Ornati G., Di Salle E., Lønning P.E., Dowsett M. In vivo inhibition of aromatization by exemestane, a novel irreversible aromatase inhibitor, in postmenopausal breast cancer patients. Clin. Cancer Res. 1998;4:2089–2093. [PubMed] [Google Scholar]
- 21.Geisler J., King N., Dowsett M., Ottestad L., Lundgren S., Walton P., Kormeset P., Lonning P.E. Influence of anastrozole (Arimidex), a selective, non-steroidal aromatase inhibitor, on in vivo aromatisation and plasma oestrogen levels in postmenopausal women with breast cancer. Br. J. Cancer. 1996;74:1286–1291. doi: 10.1038/bjc.1996.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dowsett M. Endocrine Resistance in Advanced Breast Cancer. Acta Oncol. 1996;35:91–95. doi: 10.3109/02841869609083979. [DOI] [PubMed] [Google Scholar]
- 23.Haque M., Desai K.V. Pathways to Endocrine Therapy Resistance in Breast Cancer. Front. Endocrinol. 2019;10 doi: 10.3389/fendo.2019.00573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Toy W., Shen Y., Won H., Green B., Sakr R.A., Will M., Li Z., Gala K., Fanning S.W., King T.A., et al. ESR1 ligand-binding domain mutations in hormone-resistant breast cancer. Nat. Genet. 2013;45:1439–1445. doi: 10.1038/ng.2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Toy W., Weir H., Razavi P., Lawson M., Goeppert A.U., Mazzola A.M., Smith A., Wilson J., Morrow C., Wong W.L., et al. Activating ESR1 Mutations Differentially Affect the Efficacy of ER Antagonists. Cancer Discov. 2016;7:277–287. doi: 10.1158/2159-8290.CD-15-1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fuentes N., Silveyra P. Estrogen receptor signaling mechanisms. Adv. Protein Chem. Struct. Biol. 2019;116:135–170. doi: 10.1016/bs.apcsb.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Martin L.-A., Farmer I., Johnston S.R.D., Ali S., Marshall C., Dowsett M. Enhanced Estrogen Receptor (ER) α, ERBB2, and MAPK Signal Transduction Pathways Operate during the Adaptation of MCF-7 Cells to Long Term Estrogen Deprivation. J. Boil. Chem. 2003;278:30458–30468. doi: 10.1074/jbc.M305226200. [DOI] [PubMed] [Google Scholar]
- 28.Miller T.W., Rexer B.N., Garrett J.T., Arteaga C.L. Mutations in the phosphatidylinositol 3-kinase pathway: Role in tumor progression and therapeutic implications in breast cancer. Breast Cancer Res. 2011;13:224. doi: 10.1186/bcr3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sanchez C.G., Ma C., Crowder R.J., Guintoli T., Phommaly C., Gao F., Lin L., Ellis M.J. Preclinical modeling of combined phosphatidylinositol-3-kinase inhibition with endocrine therapy for estrogen receptor-positive breast cancer. Breast Cancer Res. 2011;13:R21. doi: 10.1186/bcr2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park S., Song J., Joe C.O., Shin I. Akt stabilizes estrogen receptor α with the concomitant reduction in its transcriptional activity. Cell. Signal. 2008;20:1368–1374. doi: 10.1016/j.cellsig.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 31.Thomas R.S., Sarwar N., Phoenix F., Coombes R.C., Ali S. Phosphorylation at serines 104 and 106 by Erk1/2 MAPK is important for estrogen receptor-alpha activity. J. Mol. Endocrinol. 2008;40:173–184. doi: 10.1677/JME-07-0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barone I., Cui Y., Herynk M.H., Rodriguez C.-A., Giordano C., Selever J., Beyer A., Andò S., Fuqua A.W.S. Expression of the K303R estrogen receptor-α breast cancer mutation induces resistance to an aromatase inhibitor via addiction to the PI3K/Akt kinase pathway. Cancer Res. 2009;69:4724–4732. doi: 10.1158/0008-5472.CAN-08-4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barone I., Iacopetta D., Covington K.R., Cui Y., Tsimelzon A., Beyer A., Andò S., Fuqua S.A., Anna T. Phosphorylation of the mutant K303R estrogen receptor α at serine 305 affects aromatase inhibitor sensitivity. Oncogene. 2010;29:2404–2414. doi: 10.1038/onc.2009.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holm C., Kok M., Michalides R., Fles R., Koornstra R., Wesseling J., Hauptmann M., Neefjes J., Peterse J., Stål O., et al. Phosphorylation of the oestrogen receptor α at serine 305 and prediction of tamoxifen resistance in breast cancer. J. Pathol. 2009;217:372–379. doi: 10.1002/path.2455. [DOI] [PubMed] [Google Scholar]
- 35.Michalides R., Griekspoor A.C., Balkenende A., Verwoerd D., Janssen L., Jalink K., Floore A., Velds A., Veer L.V., Neefjes J. Tamoxifen resistance by a conformational arrest of the estrogen receptor α after PKA activation in breast cancer. Cancer Cell. 2004;5:597–605. doi: 10.1016/j.ccr.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 36.Skliris G.P., Nugent Z., Watson P.H., Murphy L.C. Estrogen Receptor Alpha Phosphorylated at Tyrosine 537 is Associated with Poor Clinical Outcome in Breast Cancer Patients Treated with Tamoxifen. Horm. Cancer. 2010;1:215–221. doi: 10.1007/s12672-010-0049-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Skliris G.P., Nugent Z.J., Rowan B.G., Penner C.R., Watson P.H., Murphy L.C. A phosphorylation code for oestrogen receptor-α predicts clinical outcome to endocrine therapy in breast cancer. Endocr. Relat. Cancer. 2010;17:589–597. doi: 10.1677/ERC-10-0030. [DOI] [PubMed] [Google Scholar]
- 38.Cheskis B., Greger J., Cooch N., McNally C., McLarney S., Lam H., Rutledge S., Mekonnen B., Hauze D., Nagpal S. MNAR plays an important role in ERa activation of Src/MAPK and PI3K/Akt signaling pathways. Steroids. 2008;73:901–905. doi: 10.1016/j.steroids.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 39.Zheng F.F., Wu R.-C., Smith C.L., O’Malley B.W. Rapid Estrogen-Induced Phosphorylation of the SRC-3 Coactivator Occurs in an Extranuclear Complex Containing Estrogen Receptor. Mol. Cell. Boil. 2005;25:8273–8284. doi: 10.1128/MCB.25.18.8273-8284.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Castoria G., Migliaccio A., Bilancio A., Di Domenico M., De Falco A., Lombardi M., Fiorentino R., Varricchio L., Barone M.V., Auricchio F. PI3-kinase in concert with Src promotes the S-phase entry of oestradiol-stimulated MCF-7 cells. EMBO J. 2001;20:6050–6059. doi: 10.1093/emboj/20.21.6050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deng B., Tarhan Y.E., Ueda K., Ren L., Katagiri T., Park J.-H., Nakamura Y. Critical Role of Estrogen Receptor Alpha O-Glycosylation by N-Acetylgalactosaminyltransferase 6 (GALNT6) in Its Nuclear Localization in Breast Cancer Cells. Neoplasia. 2018;20:1038–1044. doi: 10.1016/j.neo.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Faus H., Haendler B. Post-translational modifications of steroid receptors. Biomed. Pharmacother. 2006;60:520–528. doi: 10.1016/j.biopha.2006.07.082. [DOI] [PubMed] [Google Scholar]
- 43.La Rosa P., Pesiri V., Leclercq G., Marino M., Acconcia F. Palmitoylation Regulates 17β-Estradiol-Induced Estrogen Receptor-α Degradation and Transcriptional Activity. Mol. Endocrinol. 2012;26:762–774. doi: 10.1210/me.2011-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang X., Tanaka K., Yan J., Li J., Peng D., Jiang Y., Yang Z., Barton M.C., Wen H., Shi X. Regulation of estrogen receptor α by histone methyltransferase SMYD2-mediated protein methylation. Proc. Natl. Acad. Sci. USA. 2013;110:17284–17289. doi: 10.1073/pnas.1307959110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tecalco-Cruz A.C., Ramírez-Jarquín J.O. Polyubiquitination inhibition of estrogen receptor alpha and its implications in breast cancer. World J. Clin. Oncol. 2018;9:60–70. doi: 10.5306/wjco.v9.i4.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kisselev A.F., Goldberg A.L. Proteasome inhibitors: From research tools to drug candidates. Chem. Boil. 2001;8:739–758. doi: 10.1016/S1074-5521(01)00056-4. [DOI] [PubMed] [Google Scholar]
- 47.Fan M., Nakshatri H., Nephew K.P. Inhibiting Proteasomal Proteolysis Sustains Estrogen Receptor-α Activation. Mol. Endocrinol. 2004;18:2603–2615. doi: 10.1210/me.2004-0164. [DOI] [PubMed] [Google Scholar]
- 48.Valley C.C., Solodin N.M., Powers G.L., Ellison S.J., Alarid E.T. Temporal variation in estrogen receptor-α protein turnover in the presence of estrogen. J. Mol. Endocrinol. 2007;40:23–34. doi: 10.1677/JME-07-0067. [DOI] [PubMed] [Google Scholar]
- 49.Kinyamu H.K., Collins J.B., Grissom S.F., Hebbar P.B., Archer T.K. Genome wide transcriptional profiling in breast cancer cells reveals distinct changes in hormone receptor target genes and chromatin modifying enzymes after proteasome inhibition. Mol. Carcinog. 2008;47:845–885. doi: 10.1002/mc.20440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Powers G.L., Ellison-Zelski S.J., Casa A.J., Lee A.V., Alarid E.T. Proteasome inhibition represses ERα gene expression in ER+ cells: A new link between proteasome activity and estrogen signaling in breast cancer. Oncogene. 2009;29:1509–1518. doi: 10.1038/onc.2009.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Powers G.L., Rajbhandari P., Solodin N.M., Bickford B., Alarid E.T. The Proteasome Inhibitor Bortezomib Induces an Inhibitory Chromatin Environment at a Distal Enhancer of the Estrogen Receptor-α Gene. PLoS ONE. 2013;8:e81110. doi: 10.1371/journal.pone.0081110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berry N.B., Fan M., Nephew K.P. Estrogen receptor-alpha hinge-region lysines 302 and 303 regulate receptor degradation by the proteasome. Mol. Endocrinol. 2008;22:1535–1551. doi: 10.1210/me.2007-0449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tecalco-Cruz A.C., Ramirez-Jarquin J.O., Cruz-Ramos E. Estrogen Receptor Alpha and its Ubiquitination in Breast Cancer Cells. Curr. Drug Targets. 2019;20:690–704. doi: 10.2174/1389450119666181015114041. [DOI] [PubMed] [Google Scholar]
- 54.He X., Zheng Z., Song T., Wei C., Ma H., Ma Q., Zhang Y., Xu Y., Shi W., Ye Q., et al. c-Abl regulates estrogen receptor α transcription activity through its stabilization by phosphorylation. Oncogene. 2010;29:2238–2251. doi: 10.1038/onc.2009.513. [DOI] [PubMed] [Google Scholar]
- 55.Medunjanin S., Hermani A., De Servi B., Grisouard J., Rincke G., Mayer D. Glycogen Synthase Kinase-3 Interacts with and Phosphorylates Estrogen Receptor α and Is Involved in the Regulation of Receptor Activity. J. Boil. Chem. 2005;280:33006–33014. doi: 10.1074/jbc.M506758200. [DOI] [PubMed] [Google Scholar]
- 56.Hilmi K., Hussein N., Mendoza-Sanchez R., El-Ezzy M., Ismail H., Durette C., Bail M., Rozendaal M.J., Bouvier M., Thibault P., et al. Role of SUMOylation in Full Antiestrogenicity. Mol. Cell. Boil. 2012;32:3823–3837. doi: 10.1128/MCB.00290-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sentis S., Le Romancer M., Bianchin C., Rostan M.-C., Corbo L. Sumoylation of the Estrogen Receptor α Hinge Region Regulates Its Transcriptional Activity. Mol. Endocrinol. 2005;19:2671–2684. doi: 10.1210/me.2005-0042. [DOI] [PubMed] [Google Scholar]
- 58.Murphy L.C., Seekallu S.V., Watson P.H. Clinical significance of estrogen receptor phosphorylation. Endocr. Relat. Cancer. 2010;18:R1–R14. doi: 10.1677/ERC-10-0070. [DOI] [PubMed] [Google Scholar]
- 59.Subramanian K., Jia D., Kapoor-Vazirani P., Powell D.R., Collins R.E., Sharma D., Peng J., Cheng X., Vertino P.M. Regulation of Estrogen Receptor α by the SET7 Lysine Methyltransferase. Mol. Cell. 2008;30:336–347. doi: 10.1016/j.molcel.2008.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim M.Y., Woo E.M., Chong Y.T.E., Homenko D.R., Kraus W.L. Acetylation of Estrogen Receptor α by p300 at Lysines 266 and 268 Enhances the Deoxyribonucleic Acid Binding and Transactivation Activities of the Receptor. Mol. Endocrinol. 2006;20:1479–1493. doi: 10.1210/me.2005-0531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Williams C.C., Basu A., El-Gharbawy A., Carrier L., Smith C.L., Rowan B.G. Identification of four novel phosphorylation sites in estrogen receptor α: Impact on receptor-dependent gene expression and phosphorylation by protein kinase CK2. BMC Biochem. 2009;10:36. doi: 10.1186/1471-2091-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xie Y., Li G., Chen M., Guo X., Tang L., Luo X., Wang S., Yi W., Dai L., Wang J. Mutation screening of 10 cancer susceptibility genes in unselected breast cancer patients. Clin. Genet. 2017;93:41–51. doi: 10.1111/cge.13063. [DOI] [PubMed] [Google Scholar]
- 63.Wang C., Fu M., Angeletti R.H., Siconolfi-Baez L., Reutens A.T., Albanese C., Lisanti M.P., Katzenellenbogen B.S., Kato S., Hopp T., et al. Direct Acetylation of the Estrogen Receptor α Hinge Region by p300 Regulates Transactivation and Hormone Sensitivity. J. Boil. Chem. 2001;276:18375–18383. doi: 10.1074/jbc.M100800200. [DOI] [PubMed] [Google Scholar]
- 64.Eakin C.M., MacCoss M.J., Finney G.L., Klevit R.E. Estrogen receptor α is a putative substrate for the BRCA1 ubiquitin ligase. Proc. Nat. Acad. Sci. USA. 2007;104:5794–5799. doi: 10.1073/pnas.0610887104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Giordano C., Cui Y., Barone I., Ando S., Mancini M.A., Berno V., Fuqua S.A.W. Growth factor-induced resistance to tamoxifen is associated with a mutation of estrogen receptor α and its phosphorylation at serine. Brea. Canc. Res. Treat. 2010;119:71–85. doi: 10.1007/s10549-009-0334-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Herynk M.H., Parra I., Cui Y., Beyer A., Wu M.-F., Hilsenbeck S.G., Fuqua S.A. Association between the estrogen receptor alpha A908G mutation and outcomes in invasive breast cancer. Clin. Cancer Res. 2007;13:3235–3243. doi: 10.1158/1078-0432.CCR-06-2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zwart W., Griekspoor A.C., Berno V., Lakeman K., Jalink K., Mancini M., Neefjes J., Michalides R. PKA-induced resistance to tamoxifen is associated with an altered orientation of ERα towards co-activator SRC-1. EMBO J. 2007;26:3534–3544. doi: 10.1038/sj.emboj.7601791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pedram A., Razandi M., Deschenes R.J., Levin E.R. DHHC-7 and -21 are palmitoylacyltransferases for sex steroid receptors. Mol. Boil. Cell. 2012;23:188–199. doi: 10.1091/mbc.e11-07-0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Traboulsi T., El Ezzy M., Dumeaux V., Audemard E., Mader S. Role of SUMOylation in differential ERα transcriptional repression by tamoxifen and fulvestrant in breast cancer cells. Oncogene. 2018;38:1019–1037. doi: 10.1038/s41388-018-0468-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sun J., Zhou W., Kaliappan K., Nawaz Z., Slingerland J. ERα phosphorylation at Y537 by Src triggers E6-AP-ERα binding, ERα ubiquitylation, promoter occupancy, and target gene expression. Mol. Endocrinol. 2012;26:1567–1577. doi: 10.1210/me.2012-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jeselsohn R., Yelensky R., Buchwalter G., Frampton G.M., Meric-Bernstam F., Gonzalez-Angulo A.M., Ferrer J., Perez-Fidalgo J.A., Cristofanilli M., Gomez H., et al. Emergence of constitutively active estrogen receptor-α mutations in pretreated advanced estrogen receptor-positive breast cancer. Clin. Cancer Res. 2014;20:1757–1767. doi: 10.1158/1078-0432.CCR-13-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lupini L., Moretti A., Bassi C., Schirone A., Pedriali M., Querzoli P., Roncarati R., Frassoldati A., Negrini M. High-sensitivity assay for monitoring ESR1 mutations in circulating cell-free DNA of breast cancer patients receiving endocrine therapy. Sci. Rep. 2018;8:4371. doi: 10.1038/s41598-018-22312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ma Y., Fan S., Hu C., Meng Q., Fuqua S.A., Pestell R.G., Tomita Y.A., Rosen E.M. BRCA1 Regulates Acetylation and Ubiquitination of Estrogen Receptor-α. Molec. Endocr. 2010;24:76–90. doi: 10.1210/me.2009-0218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Murphy L.C., Skliris G.P., Rowan B.G., Al-Dhaheri M., Williams C., Penner C., Troup S., Begic S., Parisien M., Watson P.H. The relevance of phosphorylated forms of estrogen receptor in human breast cancer in vivo. J. Steroid Biochem. Mol. Boil. 2009;114:90–95. doi: 10.1016/j.jsbmb.2009.01.017. [DOI] [PubMed] [Google Scholar]
- 75.Huderson B.P., Duplessis T.T., Williams C.C., Seger H.C., Marsden C.G., Pouey K.J., Hill S.M., Rowan B.G. Stable inhibition of specific estrogen receptor α (ERα) phosphorylation confers increased growth, migration/invasion, and disruption of estradiol signaling in MCF-7 breast cancer cells. Endocrinology. 2012;153:4144–4159. doi: 10.1210/en.2011-2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Valley C.C., Métivier R., Solodin N.M., Fowler A.M., Mashek M.T., Hill L., Alarid E.T. Differential Regulation of Estrogen-Inducible Proteolysis and Transcription by the Estrogen Receptor α N Terminus. Mol. Cell. Boil. 2005;25:5417–5428. doi: 10.1128/MCB.25.13.5417-5428.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Arnott J.A., Martinkovich S., Planey S.L., Shah D. Selective estrogen receptor modulators: Tissue specificity and clinical utility. Clin. Interv. Aging. 2014;9:1437–1452. doi: 10.2147/CIA.S66690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Rayala S.K., Talukder A.H., Balasenthil S., Tharakan R., Barnes C.J., Wang R.-A., Aldaz C.M., Khan S.A., Kumar R. P21-Activated Kinase 1 Regulation of Estrogen Receptor- Activation Involves Serine 305 Activation Linked with Serine 118 Phosphorylation. Cancer Res. 2006;66:1694–1701. doi: 10.1158/0008-5472.CAN-05-2922. [DOI] [PubMed] [Google Scholar]
- 79.Zheng X.Q., Guo J.P., Yang H., Kanai M., He L.L., Li Y.Y., Koomen J.M., Minton S., Gao M., Ren X.B., et al. Aurora-A is a determinant of tamoxifen sensitivity through phosphorylation of ERα in breast cancer. Oncogene. 2013;33:4985–4996. doi: 10.1038/onc.2013.444. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 80.Bostner J., Skoog L., Fornander T., Nordenskjold B., Stål O. Estrogen Receptor- Phosphorylation at Serine 305, Nuclear p21-Activated Kinase 1 Expression, and Response to Tamoxifen in Postmenopausal Breast Cancer. Clin. Cancer Res. 2010;16:1624–1633. doi: 10.1158/1078-0432.CCR-09-1733. [DOI] [PubMed] [Google Scholar]
- 81.Castoria G., Giovannelli P., Lombardi M., De Rosa C., Giraldi T., De Falco A., Barone M.V., Abbondanza C., Migliaccio A., Auricchio F. Tyrosine phosphorylation of estradiol receptor by Src regulates its hormone-dependent nuclear export and cell cycle progression in breast cancer cells. Oncogene. 2012;31:4868–4877. doi: 10.1038/onc.2011.642. [DOI] [PubMed] [Google Scholar]
- 82.Jia S., Miedel M.T., Ngo M., Hessenius R., Chen N., Wang P., Bahreini A., Li Z., Ding Z., Shun T.Y., et al. Clinically Observed Estrogen Receptor Alpha Mutations within the Ligand-Binding Domain Confer Distinguishable Phenotypes. Oncology. 2018;94:176–189. doi: 10.1159/000485510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sun M., Paciga J.E., Feldman R.I., Yuan Z.-Q., Coppola D., Lu Y.Y., Shelley S.A., Nicosia S.V., Cheng J.Q. Phosphatidylinositol-3-OH kinase (PI3K)/AKT2, activated in breast cancer, regulates and is induced by estrogen receptor α (ERα) via interaction between ERα and PI3K. Cancer Res. 2001;61:5985–5991. [PubMed] [Google Scholar]
- 84.Acconcia F., Ascenzi P., Bocedi A., Spisni E., Tomasi V., Trentalance A., Visca P., Marino M. Palmitoylation-dependent Estrogen Receptor α Membrane Localization: Regulation by 17β-Estradiol. Mol. Boil. Cell. 2005;16:231–237. doi: 10.1091/mbc.e04-07-0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cui Y., Zhang M., Pestell R., Curran E.M., Welshons W.V., Fuqua S.A. Phosphorylation of Estrogen Receptor α Blocks Its Acetylation and Regulates Estrogen Sensitivity. Cancer Res. 2004;64:9199–9208. doi: 10.1158/0008-5472.CAN-04-2126. [DOI] [PubMed] [Google Scholar]
- 86.Fuqua S.A., Wiltschke C., Zhang Q.X., Borg Å., Castles C.G., Friedrichs W.E., Hopp T., Hilsenbeck S., Mohsin S., O’Connell P., et al. A hypersensitive estrogen receptor-α mutation in premalignant breast lesions. Cancer Res. 2000;60:4026–4029. [PubMed] [Google Scholar]
- 87.Zhang X., Peng D., Xi Y., Yuan C., Sagum C.A., Klein B.J., Tanaka K., Wen H., Kutateladze T.G., Li L., et al. G9a-mediated methylation of ERα links the PHF20/MOF histone acetyltransferase complex to hormonal gene expression. Nat. Comm. 2016;7:10810. doi: 10.1038/ncomms10810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.O’Leary B., Cutts R.J., Liu Y., Hrebien S., Huang X., Fenwick K., Andre F., Loibl S., Loi S.M., Garcia-Murillas I., et al. The Genetic Landscape and Clonal Evolution of Breast Cancer Resistance to Palbociclib plus Fulvestrant in the PALOMA-3 Trial. Cancer Discov. 2018;8:1390–1403. doi: 10.1158/2159-8290.CD-18-0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Franken A., Honisch E., Reinhardt F., Meier-Stiegen F., Yang L., Jaschinski S., Esposito I., Alberter B., Polzer B., Huebner H., et al. Detection of ESR1 Mutations in Single Circulating Tumor Cells on Estrogen Deprivation Therapy but Not in Primary Tumors from Metastatic Luminal Breast Cancer Patients. J. Mol. Diagn. 2019;22:111–121. doi: 10.1016/j.jmoldx.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 90.Bostner J., Karlsson E., Pandiyan M.J., Westman H., Skoog L., Fornander T., Nordenskjöld B., Stål O. Activation of Akt, mTOR, and the estrogen receptor as a signature to predict tamoxifen treatment benefit. Breast Cancer Res. Treat. 2012;137:397–406. doi: 10.1007/s10549-012-2376-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen M., Cui Y.-K., Huang W.-H., Man K., Zhang G.-J. Phosphorylation of estrogen receptor α at serine 118 is correlated with breast cancer resistance to tamoxifen. Oncol. Lett. 2013;6:118–124. doi: 10.3892/ol.2013.1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jiang J., Sarwar N., Peston D., Kulinskaya E., Shousha S., Coombes R.C., Ali S. Phosphorylation of Estrogen Receptor- at Ser167 Is Indicative of Longer Disease-Free and Overall Survival in Breast Cancer Patients. Clin. Cancer Res. 2007;13:5769–5776. doi: 10.1158/1078-0432.CCR-07-0822. [DOI] [PubMed] [Google Scholar]
- 93.Yamashita H., Nishio M., Toyama T., Sugiura H., Kondo N., Kobayashi S., Fujii Y., Iwase H. Low phosphorylation of estrogen receptor α (ERα) serine 118 and high phosphorylation of ERα serine 167 improve survival in ER-positive breast cancer. Endocr. Rel. Canc. 2008;15:755–763. doi: 10.1677/ERC-08-0078. [DOI] [PubMed] [Google Scholar]
- 94.Murphy L.C., Niu Y., Snell L., Watson P. Phospho-Serine-118 Estrogen Receptor- Expression Is Associated with Better Disease Outcome in Women Treated with Tamoxifen. Clin. Cancer Res. 2004;10:5902–5906. doi: 10.1158/1078-0432.CCR-04-0191. [DOI] [PubMed] [Google Scholar]
- 95.Sarwar N., Kim J., Jiang J., Peston D., Sinnett H., Madden P., Gee J.M., Nicholson R.I., Lykkesfeldt A.E., Shousha S., et al. Phosphorylation of ERalpha at serine 118 in primary breast cancer and in tamoxifen-resistant tumours is indicative of a complex role for ERalpha phosphorylation in breast cancer progression. Endoc. Relat. Cancer. 2006;13:851–861. doi: 10.1677/erc.1.01123. [DOI] [PubMed] [Google Scholar]
- 96.Button B., Croessmann S., Chu D., Rosen D.M., Zabransky D.J., Dalton W.B., Cravero K., Kyker-Snowman K., Waters I., Karthikeyan S., et al. The estrogen receptor-alpha S118P variant does not affect breast cancer incidence or response to endocrine therapies. Breast Cancer Res. Treat. 2018;174:401–412. doi: 10.1007/s10549-018-05087-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kok M., Zwart W., Holm C., Fles R., Hauptmann M., Veer L.J.V., Wessels L.F.A., Neefjes J., Stål O., Linn S.C., et al. PKA-induced phosphorylation of ERα at serine 305 and high PAK1 levels is associated with sensitivity to tamoxifen in ER-positive breast cancer. Breast Cancer Res. Treat. 2010;125:1–12. doi: 10.1007/s10549-010-0798-y. [DOI] [PubMed] [Google Scholar]
- 98.Toaldo C.B., Alexi X., Beelen K., Kok M., Hauptmann M., Jansen M.P.H.M., Berns P.M.J.J., Neefjes J., Linn S., Michalides R., et al. Protein Kinase A-induced tamoxifen resistance is mediated by anchoring protein AKAP13. BMC Cancer. 2015;15:588. doi: 10.1186/s12885-015-1591-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Busonero C., Leone S., Bartoloni S., Acconcia F. Strategies to degrade estrogen receptor α in primary and ESR1 mutant-expressing metastatic breast cancer. Mol. Cell. Endocrinol. 2019;480:107–121. doi: 10.1016/j.mce.2018.10.020. [DOI] [PubMed] [Google Scholar]
- 100.Gao J.J., Cheng J., Bloomquist E., Sanchez J., Wedam S.B., Singh H., Amiri-Kordestani L., Ibrahim A., Sridhara R., Goldberg K.B., et al. CDK4/6 inhibitor treatment for patients with hormone receptor-positive, HER2-negative, advanced or metastatic breast cancer: A US Food and Drug Administration pooled analysis. Lancet Oncol. 2020;21:250–260. doi: 10.1016/S1470-2045(19)30804-6. [DOI] [PubMed] [Google Scholar]
- 101.Puyang X., Furman C., Zheng G.Z., Wu Z.J., Banka D., Aithal K., Agoulnik S., Bolduc D.M., Buonamici S., Caleb B., et al. Discovery of selective estrogen receptor covalent antagonists for the treatment of ERαWT and ERαMUT breast cancer. Cancer Discov. 2018;8:1176–1193. doi: 10.1158/2159-8290.CD-17-1229. [DOI] [PubMed] [Google Scholar]
- 102.Hamilton E.P., Patel M.R., Armstrong A.C., Baird R.D., Jhaveri K., Hoch M., Klinowska T., Lindemann J.P.O., Morgan S.R., Schiavon G., et al. A first-in-human study of the new oral selective estrogen receptor degrader AZD9496 for ER+/HER2− advanced breast cancer. Clin. Cancer Res. 2018;24:3510–3518. doi: 10.1158/1078-0432.CCR-17-3102. [DOI] [PubMed] [Google Scholar]
- 103.Robertson J.F.R., Evans A., Henschen S., Kirwan C.C., Jahan A., Kenny L.M., Dixon J.M., Schmid P., Kothari A., Mohamed O., et al. A randomized, open-label, pre-surgical, window of opportunity study comparing the pharmacodynamic effects of the novel oral SERD AZD9496 with fulvestrant in patients with newly diagnosed ER+ HER2-primary breast cancer. Clin. Cancer Res. 2020;26:4242–4249. doi: 10.1158/1078-0432.CCR-19-3387. [DOI] [PubMed] [Google Scholar]
- 104.Weir H.M., Bradbury R.H., Lawson M., Rabow A.A., Buttar D., Callis R.J., Curwen J.O., de Almeida C., Ballard P., Hulse M., et al. AZD9496: An oral estrogen receptor inhibitor that blocks the growth of ER-positive and ESR1-mutant breast tumors in preclinical models. Cancer Res. 2016;76:3307–3318. doi: 10.1158/0008-5472.CAN-15-2357. [DOI] [PubMed] [Google Scholar]
- 105.Hirokawa Y., Arnold M., Nakajima H., Zalcberg J., Maruta H. Signal therapy of breast cancers by the HDAC inhibitor FK228 that blocks the activation of PAK1 and abrogates the tamoxifen-resistance. Cancer Boil. Ther. 2005;4:956–960. doi: 10.4161/cbt.4.9.1911. [DOI] [PubMed] [Google Scholar]
- 106.Munster P.N., Thurn K.T., Thomas S., Raha P., Lacevic M., Miller A., Melisko M., Ismail-Khan R., Rugo H., Moasser M., et al. A phase II study of the histone deacetylase inhibitor vorinostat combined with tamoxifen for the treatment of patients with hormone therapy-resistant breast cancer. Br. J. Cancer. 2011;104:1828–1835. doi: 10.1038/bjc.2011.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jones R.H., Casbard A., Carucci M., Cox C., Butler R., Alchami F., Madden T.-A., Bale C., Bezecny P., Joffe J., et al. Fulvestrant plus capivasertib versus placebo after relapse or progression on an aromatase inhibitor in metastatic, oestrogen receptor-positive breast cancer (FAKTION): A multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2020;21:345–357. doi: 10.1016/S1470-2045(19)30817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Haddad T.C., D’Assoro A., Suman V., Opyrchal M., Peethambaram P., Liu M.C., Goetz M.P., Ingle J.N. Phase I trial to evaluate the addition of alisertib to fulvestrant in women with endocrine-resistant, ER+ metastatic breast cancer. Breast Cancer Res. Treat. 2017;168:639–647. doi: 10.1007/s10549-017-4616-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Korobeynikov V.A., Borakove M., Feng Y., Wuest W.M., Koval A.B., Nikonova A.S., Serebriiskii I., Chernoff J., Borges V.F., Golemis E.A., et al. Combined inhibition of Aurora A and p21-activated kinase 1 as a new treatment strategy in breast cancer. Breast Cancer Res. Treat. 2019;177:369–382. doi: 10.1007/s10549-019-05329-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Paul D., Vukelja S.J., Holmes F.A., Blum J.L., McIntyre K.J., Lindquist D.L., Osborne C.R., Sanchez I.J., Goldschmidt J.H., Wang Y., et al. Randomized phase-II evaluation of letrozole plus dasatinib in hormone receptor positive metastatic breast cancer patients. NPJ Breast Cancer. 2019;5:36–37. doi: 10.1038/s41523-019-0132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chen Y., Alvarez E.A., Azzam D.J., Wander S.A., Guggisberg N., Jorda M., Ju Z., Hennessy B.T., Slingerland J. Combined Src and ER blockade impairs human breast cancer proliferation in vitro and in vivo. Breast Cancer Res. Treat. 2010;128:69–78. doi: 10.1007/s10549-010-1024-7. [DOI] [PubMed] [Google Scholar]
- 112.Chen Y., Guggisberg N., Jorda M., Gonzalez-Angulo A., Hennessy B., Mills G.B., Tan C.-K., Slingerland J.M. Combined Src and Aromatase Inhibition Impairs Human Breast Cancer Growth In vivo and Bypass Pathways Are Activated in AZD0530-Resistant Tumors. Clin. Cancer Res. 2009;15:3396–3405. doi: 10.1158/1078-0432.CCR-08-3127. [DOI] [PubMed] [Google Scholar]
- 113.Moy B., Neven P., Lebrun F., Bellet M., Xu B., Sarosiek T., Chow L., Goss P., Zacharchuk C., Leip E., et al. Bosutinib in Combination With the Aromatase Inhibitor Exemestane: A Phase II Trial in Postmenopausal Women With Previously Treated Locally Advanced or Metastatic Hormone Receptor-Positive/HER2-Negative Breast Cancer. Oncology. 2014;19:346–347. doi: 10.1634/theoncologist.2014-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Moy B., Neven P., Lebrun F., Bellet M., Xu B., Sarosiek T., Chow L., Goss P., Zacharchuk C., Leip E., et al. Bosutinib in Combination With the Aromatase Inhibitor Letrozole: A Phase II Trial in Postmenopausal Women Evaluating First-Line Endocrine Therapy in Locally Advanced or Metastatic Hormone Receptor-Positive/HER2-Negative Breast Cancer. Oncology. 2014;19:348–349. doi: 10.1634/theoncologist.2014-0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tsvetkov P., Adler J., Myers N., Biran A., Reuven N., Shaul Y. Oncogenic addiction to high 26S proteasome level. Cell Death Dis. 2018;9:773. doi: 10.1038/s41419-018-0806-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wong D.J., Nuyten D.S.A., Regev A., Lin M., Adler A.S., Segal E., Van De Vijver M.J., Chang H.Y. Revealing Targeted Therapy for Human Cancer by Gene Module Maps. Cancer Res. 2008;68:369–378. doi: 10.1158/0008-5472.CAN-07-0382. [DOI] [PubMed] [Google Scholar]
- 117.Thaler S., Thiede G., Hengstler J.G., Schad A., Schmidt M., Sleeman J.P. The proteasome inhibitor Bortezomib (Velcade) as potential inhibitor of estrogen receptor-positive breast cancer. Int. J. Cancer. 2015;137:686–697. doi: 10.1002/ijc.29404. [DOI] [PubMed] [Google Scholar]
- 118.Maynadier M., Basile I., Gallud A., Gary-Bobo M., Garcia M. Combination treatment with proteasome inhibitors and antiestrogens has a synergistic effect mediated by p21WAF1 in estrogen receptor-positive breast cancer. Oncol. Rep. 2016;36:1127–1134. doi: 10.3892/or.2016.4873. [DOI] [PubMed] [Google Scholar]
- 119.Yang C.H., Gonzalez-Angulo A.M., Reuben J.M., Booser D.J., Pusztai L., Krishnamurthy S., Esseltine D., Stec J., Broglio K.R., Islam R., et al. Bortezomib (VELCADE®) in metastatic breast cancer: Pharmacodynamics, biological effects, and prediction of clinical benefits. Ann. Oncol. 2006;17:813–817. doi: 10.1093/annonc/mdj131. [DOI] [PubMed] [Google Scholar]
- 120.Adelson K., Ramaswamy B., Sparano J.A., Christos P.J., Wright J.J., Raptis G., Han G., Villalona-Calero M., Ma C.X., Hershman D., et al. Randomized phase II trial of fulvestrant alone or in combination with bortezomib in hormone receptor-positive metastatic breast cancer resistant to aromatase inhibitors: A New York Cancer Consortium trial. NPJ Breast Cancer. 2016;2:16037. doi: 10.1038/npjbcancer.2016.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Ishii Y., Papa L., Bahadur U., Yue Z., Aguirre-Ghiso J., Shioda T., Waxman S., Germain D. Bortezomib enhances the efficacy of fulvestrant by amplifying the aggregation of the estrogen receptor, which leads to a proapoptotic unfolded protein response. Clin. Cancer Res. 2011;17:2292–2300. doi: 10.1158/1078-0432.CCR-10-1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gates L.A., Gu G., Chen Y., Rohira A.D., Lei J.T., Hamilton R.A., Yu Y., Lonard D.M., Wang J., Wang S.-P., et al. Proteomic profiling identifies key coactivators utilized by mutant ERα proteins as potential new therapeutic targets. Oncogene. 2018;37:4581–4598. doi: 10.1038/s41388-018-0284-2. [DOI] [PMC free article] [PubMed] [Google Scholar]