Abstract
Background
Gay, bisexual and other men who have sex with men (GBMSM) are at increased risk of mental health disorders and drug use. In GBMSM taking pre-exposure prophylaxis (PrEP) for HIV, the proportion engaging in risk behaviors could increase due to decreased perception in HIV risk. In turn, this could leave them further susceptible to mental health disorders.
Methods
The AMsterdam PrEP study (AMPrEP) is a demonstration project offering a choice of daily PrEP or event-driven PrEP regimen at the STI clinic of the Public Health Service of Amsterdam. Eligible participants were HIV-negative GBMSM and transgender people at risk of HIV, aged ≥18 years. We assessed anxiety and depressive mood disorders (Mental Health Inventory 5), sexual compulsivity (Sexual Compulsivity Scale), alcohol use disorder (Alcohol Use Disorder Identification Test), and drug use disorder (Drug Use Disorder Identification Test) using yearly self-administered assessments (August 2015–September 2018). The proportion of mental health problems were analyzed and changes over time and between regimen were assessed using a logistic regression model. Variables associated with the development or recovery of disorders were assessed using a multistate Markov model.
Outcomes
Of 376 enrolled, we analyzed 341 participants with data at baseline and at least one follow-up visit. During a median follow-up of 2.5 years (IQR=2.3–2.7), the proportion assessed with sexual compulsivity decreased from 23% at baseline to 10% at the last visit (p<0.001) and drug use disorder decreased from 38% at baseline to 31% at the last visit (p = 0.004). No changes occurred in proportion assessed with anxiety/depressive mood disorders (20% at baseline, 18% at last visit, p = 0.358) or alcohol use disorder (28% at baseline, 22% at the last visit, p = 0.106). During follow-up, participants reported significant less use of alcohol (p<0.001), nitrites (p<0.001) and ecstasy (p<0.001). We found no differences between daily and event-driven PrEP users. The development and recovery of disorders during follow-up were highly interrelated.
Interpretation
Mental health disorders are prevalent among those initiating PrEP. We did not find increases in mental health disorders during PrEP use, but rather a decrease in sexual compulsivity and drug use disorders. The initial prevalence of mental health disorders in our study point at the continuous need to address mental health disorders within PrEP programs.
Funding
ZonMw, H-TEAM, Internal GGD research funds, Aidsfonds, Stichting AmsterdamDiner Foundation, Gilead Sciences, Janssen Pharmaceutica, M A C AIDS Fund, and ViiV Healthcare.
Keywords: Homosexuality male, Pre-exposure prophylaxis, HIV, Mental health, Substance use, Risk behavior, Syndemics, Transgender persons
Research in context.
Evidence before this study
Gay, bisexual and other men who have sex with men (GBMSM) are at increased risk of synergistically interacting afflictions (syndemics), including mental health problems, drug use and sexual risk behaviour. Pre-exposure prophylaxis is an effective tool to prevent HIV infections. Concerns have been raised regarding an increase in mental health problems among PrEP users, including alcohol/drug use and sexual compulsivity. We searched MEDLINE on August 26, 2019, for articles or abstracts and found several studies describing high levels of mental health problems and drug use among sexual minorities initiating PrEP. Two studies, both within a randomized controlled trials(RCT), used longitudinal data; one RCT on PrEP effectiveness (PROUD) described intimate partner violence and another RCT on PrEP adherence aimed to investigate the association between substance/alcohol use and adherence to PrEP.
Added value of this study
To our knowledge, we are the first to report longitudinally on mental health issues among PrEP users, including detailed information on drug use. The Amsterdam Pre-Exposure Prophylaxis (AMPrEP) demonstration project uniquely offers participants a choice of daily and event-driven PrEP regimens. We were able to show that both daily and event-driven users are equally affected by mental health problems at inclusion and over time we found a decrease in participants assessed with sexual compulsivity and drug use disorder. The comprehensive battery of mental health problems assessed by validated questionnaires in this study allowed us to show that the development and recovery from certain mental health disorders were related to one another. Lastly, we also measured help-seeking behaviour for mental health issues, which gives an indication of mental health needs among this at-risk population.
Implications of all the available evidence
GBMSM initiating PrEP show high levels of mental health problems, including drug use and sexual compulsivity. Concerns regarding a rise in mental health problems, particular sexual compulsivity and drug-use disorder, associated with PrEP-use are not supported by our evidence. PrEP offers ample opportunity to incorporate sexual health, mental health and drug use within one program, which seems vital considering mutually reinforcing syndemics and the clustering of diseases among GBMSM at-risk for sexually transmitted infections and HIV.
Alt-text: Unlabelled box
1. Introduction
Tenofovir/emtricitabine is highly effective as pre-exposure prophylaxis (PrEP) to prevent HIV infection in gay, bisexual and other men who have sex with men (GBMSM) [1]. Qualitative research has shown that PrEP minimizes HIV-related fear and could trigger problematic increases in preoccupation with sex and recreational drug use, influencing sexual at-risk behavior [i.e. condomless anal sex (CAS), increased number of sexual partners] and sexually transmitted infections (STI) and affecting general health [2]. While the relation between PrEP use, CAS and consequently STI-incidence has been extensively studied in GBMSM [1,3], the effect on mental health problems, such as sexual compulsivity, drug use and general well-being are less known.
In this context, it is important to mention that GBMSM have poorer mental health outcomes, and are more likely to use recreational drugs compared to the general population [4,5]. This could be explained by the unique stressors experienced by sexual minorities (i.e. prejudice, victimization and discrimination) that lead to harmful effects on mental health, as described in Meyer's minority model [6]. These mental health problems (such as depression, sexual compulsivity, drug use and intimate partner violence (IPV)) are associated with both increased sexual at-risk behavior, HIV and STI among GBMSM [7,8]. These afflictions can interact with one another to increase and or maintain each other, which is the heart of the syndemic theory. The syndemic theory implies that two or more afflictions – be it social, biological or mental - can reinforce each other synergistically and contribute to an excess burden of disease [9]. Studying these interactions, such as depression, drug use and sexual compulsivity, requires assessment of a broad range of mental health disorders within the same context.
To date, only a handful of studies have addressed mental health and substance use among GBMSM at PrEP initiation, finding high prevalence of drug use, depression and sexual compulsivity [10], [11], [12], [13]; none of these studies have assessed these outcomes longitudinally.
We conducted a large, prospective cohort study of GBMSM using PrEP who were administered four standardized questionnaires on (1) anxiety and depressive mood disorder, (2) sexual compulsivity, (3) alcohol use and (4) drug use disorders at yearly intervals. We aimed to describe changes in these mental health disorders and drug use during the first years of PrEP use. We also aimed to identify factors associated with the development of, and recovery from these four mental health disorders, and to assess which participants are vulnerable to any of these mental health disorders, and might therefor benefit from extra guidance during follow-up of PrEP.
2. Methods
2.1. Study design and population
The Amsterdam PrEP (AMPrEP) study is a prospective, longitudinal, demonstration project offering choice of daily or event-driven PrEP. This study was conducted at the Public Health Service of Amsterdam, housing the largest STI clinic in the Netherlands, with approximately 50,000 consultations annually. Study design and procedures have been previously described [11]. Eligible individuals were HIV-negative GBMSM and transgender persons who had sex with men, were ≥18 years old and met one or more of the following criteria in the six months preceding inclusion: condomless anal sex (CAS) with casual partners, at least one bacterial STI, use of post-exposure prophylaxis after a sexual incident, or an HIV-positive sexual partner with a detectable viral load. Inclusion took place from August 2015 through June 2016. After written informed consent was obtained, participants had a follow-up visit every three months. The study was originally planned until June 2018 (phase-1), but was later extended for two years (phase-2). For this analysis, we used data from phase-1, including the end of phase-1 visit. Data collection occurred between August 2015 through September 2018.
``The study was approved by the ethics board of the Amsterdam University Medical Centers, location Academic Medical Center, the Netherlands (NL49504.018.14) and is registered at the Dutch trial registry (registration number NL5302; protocol available online) [14]. AMPrEP is part of the HIV Transmission Elimination AMsterdam (H-TEAM) initiative, a multidisciplinary and integrative approach to stop the urban epidemic (Hteam.nl). Data of this study is not publicly available due to informed consent. Individual researchers can contact the AMPrEP research team and submit a request for datasets.
2.2. Procedures
We offered participants a choice of daily (one tablet per day) or event-driven PrEP (two tablets taken between 24 and two hours before sexual intercourse, followed by one tablet every 24 h up to 48 h after the last sexual intercourse). Participants were allowed to switch PrEP regimens at each trimonthly study visit.
At each trimonthly study visit, participants received sexual health counseling based on motivational interviewing, were tested for STI according to routine procedures, and completed computer-assisted self-administered questionnaires on sexual behavior in the preceding 3 months.
2.3. Primary outcome measurements
Extended questionnaires including various mental health assessments were administered at baseline, 12-months, 24-months, and at the end of phase-1. We evaluated four outcomes: anxiety or depressive mood disorder using the Mental health inventory-5 (MHI5) [15], sexual compulsivity using the sexual compulsivity scale (SCS) [16], alcohol use disorder using the Alcohol Use Disorder Identification Test (AUDIT) [17], and drug use disorder using the Drug Use Disorder Identification Test (DUDIT) [18]. Presence of anxiety or depressive mood disorder was defined as an MHI-5 <60, sexual compulsivity as an SCS ≥24, alcohol use disorder as an AUDIT ≥8, and drug use disorder as a DUDIT ≥8. The recall period for the MHI5 was four weeks and for the AUDIT and DUDIT 1 year, while the SCS did not specify a recall period.
2.4. Secondary outcome measurements
We measured concern about acquiring HIV using a 7-point Likert scale (1=“very concerned” to 7=“not concerned at all”). Substance use in the previous 3 months was recorded, including type of substance [alcohol, cannabis, cocaine, erectile dysfunction drugs (EDD), gamma-hydroxybutyrate (GHB)/gamma-butyrolactone (GBL), methamphetamine, mephedrone, nitrites and 3,4-methylenedioxy-N-methylamphetamine (XTC/MDMA), or other], the frequency of use (once per month or less, 2–4 times a month, 2–3 times a week, 4 times a week or more) and injecting drug use.
At the end of phase-1, participants were asked additional questions on whether they experienced sexual abuse, intimate partner violence, or a drug-induced blackout (i.e. unconsciousness) and whether they sought help for mental health problems during the past year.
2.5. Statistical analysis
Baseline characteristics of participants with follow-up data on MHI5, SCS, AUDIT or DUDIT questionnaires were compared to participants without follow-up data.
We considered PrEP regimens as time-updated for all longitudinal analysis (i.e. PrEP regimen at the according time point). To describe trends in proportion of mental health problems over time, we used a logistic regression model including study visit (baseline, month-12, month-24, and end phase-1), PrEP regimen and the interaction between the two with a random-intercept for each participant accounting for baseline differences in MHI5, SCS, AUDIT and DUDIT. We modeled changes in concern about HIV as a continuous variable, to ensure no loss of information, using a linear regression model including study visit, PrEP regimen and the interaction between the two with a random-intercept for each participant. To describe changes in frequency of drug use, we used an interval regression model estimating the frequency of use within intervals of lower and upper bounds of all possible responses. We kept the time-frame consistent (per month), which required transforming responses as follows: 0, >0–1; ≥2-<6; ≥6-<14 and ≥14–30 times per month. This model included study visit, PrEP regimen and the interaction between the two with a random-intercept. For all models, we tested for changes over study visits with a Wald test on marginal linear predictions, first simultaneously as single tests within PrEP regimens and as a joint test across PrEP regimens, and second as an interaction between PrEP regimens, using the ‘contrast’ command in STATA. Missing data were not imputed. No further adjustments were made on these models.
Since mental health problems may fluctuate over time, we modeled outcomes each mental health problem separately as a Markov process between states of problems going from absent to present (defined as “developing” a problem) and going from present to absent (defined as “recovering” from a problem). These transitions were modeled using a two-state, time-homogenous Markov model during continuous time, allowing instantaneous rates of transitioning, or transition intensities (TI), to and from states to be estimated. To identify determinants for transitions between states, the TI over time between levels of factors can be modeled as a proportional hazards using maximum likelihood methods. From this model, we calculated hazard ratios (HR) and their 95% confidence intervals (CI) comparing average TIs over time between levels of factors. Univariable and multivariable HRs were calculated for time-fixed variables [age at inclusion, self-declared ethnicity, education level, being in a steady relationship at inclusion, employment at inclusion and residence (Amsterdam vs not Amsterdam)] and time-varying co-variables (natural logarithm of number of anal sex partners and CAS acts and PrEP regimen). Covariates whose 95%CI did not cross 1 were selected in a forward stepwise fashion to create a multivariable model.
Statistical analyses were performed with STATA (v13.1, STATA Corporation, College Station, TX, USA) and R (v3.5.2, Vienna, Austria). Significance was defined as a p-value <0.05.
2.6. Role of the funding source
The study funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The authors had full access to all data and were responsible for the decision to submit for publication.
3. Results
3.1. Description of the study population
Of 376 participants included, seven participants had an incomplete mental health assessment at baseline and 28 did not have any assessment during follow-up. The remaining 341 participants were included in analysis (Table 1). We found no differences in baseline characteristics between participants with and without follow-up data. The majority were white (85%), held a university degree (77%), and chose daily PrEP (74%). Two participants identified as transgender women. In the 3 months preceding enrolment, participants reported a median of 15 [IQR 8–31] sexual partners and 125/341 (37%) used ≥5 types of drugs.
Table 1.
Baseline characteristics of 369 participants using Pre-Exposure prophylaxis to prevent HIV (PrEP) who did and did not have data on mental health assessments during follow-up. The AMPrEP study, Amsterdam, The Netherlands, 2015–2018.
| At least 1 assessment during follow up n = 341 | Not any assessment during follow up n = 28 | p-value | |
|---|---|---|---|
| Demographic characteristics | |||
| Age in years (median, [IQR]) | 40 [33–48] | 36 [30–44] | 0.105 |
| White ethnicity a | 290 (85%) | 25 (89%) | 0.542 |
| Transgender women a | 2 (1%) | 0 (0%) | 0.684 |
| University degree | 261 (77%) | 20 (71%) | 0.542 |
| Steady relationship | 149 (44%) | 11 (39%) | 0.614 |
| Unemployed | 76 (23%) | 5 (18%) | 0.566 |
| Living in Amsterdam | 211 (62%) | 13 (46%) | 0.108 |
| Validated assessments on mental healthb | |||
| Depressive or anxiety disorder | 69 (20%) | 7 (25%) | 0.549 |
| Sexual compulsivity | 78 (23%) | 6 (21%) | 0.861 |
| Alcohol use disorder | 94 (28%) | 10 (36%) | 0.357 |
| Drug use disorder | 128 (38%) | 8 (29%) | 0.344 |
| Presence of at least one disorder | 218 (64%) | 18 (64%) | 0.970 |
| Substance usec | |||
| Alcohol | 302 (90%) | 26 (93%) | 0.585 |
| Amphetamine | 74 (22%) | 6 (21%) | 0.942 |
| Cannabis | 118 (35%) | 10 (36%) | 0.958 |
| Cocaine | 101 (30%) | 12 (43%) | 0.160 |
| Erectile dysfunction drugs | 243 (73%) | 17 (63%) | 0.287 |
| GHB/GBL | 140 (42%) | 7 (25%) | 0.084 |
| Ketamine | 72 (21%) | 9 (33%) | 0.156 |
| Methamphetamine | 32 (10%) | 2 (7%) | 0.677 |
| Nitrites | 242 (72%) | 19 (68%) | 0.638 |
| XTC/MDMA | 177 (53%) | 18 (64%) | 0.243 |
| Injected | 13 (4%) | 2 (7%) | 0.372 |
| Sexual characteristics | |||
| Number of sex partners (median, [IQR]) c | 15 [8–31] | 10.5 [5.5–20] | 0.565 |
| Number of condomless anal sex acts (median, [IQR])c | 11 [4–23] | 7.5 [2–18.5] | 0.453 |
| Daily PrEP | 251 (74%) | 16 (57%) | 0.061 |
| Any bacterial STI | 66 (19%) | 7 (25%) | 0.481 |
| Chlamydia | 34 (10%) | 1 (4%) | 0.253 |
| Gonorrhoea | 32 (10%) | 5 (18%) | 0.167 |
| Syphilis | 4 (1%) | 1 (4%) | 0.399 |
Abbreviations: AMPrEP, Amsterdam Pre-Exposure Prophylaxis for HIV study; IQR, Interquartile range; GHB, gamma-hydroxybutyrate; GBL, gamma-butyrolacton; XTC, 3,4-methyleendioxymethamfetamine; STI, sexually transmitted infection; PrEP, Pre-exposure Prophylaxis.
Self-identified.
According to mental health inventory 5 (MHI5, score<60), sexual compulsivity scale (SCS, score ≥24), alcohol use disorder identification test (AUDIT, score ≥ 8) and drug use disorder identification test (DUDIT, score ≥8).
In the preceding 3 months.
3.2. Mental health problems during PrEP use
We obtained data on 334 participants at 12 months, 299 participants at 24 months, and 289 participants at the end of phase-1 (eFig. 1). For the 11 individuals whose end of phase-1 visit was also their month 24-visit, their data were considered as a month-24 visit. Median follow-up was 2.5 years (IQR 2.3–2.7), totaling 831.6 person-years. The majority (n = 239) continued their initial PrEP regimen, while 59 switched regimens once, and 43 switched more than once. Of all 153 switches, 85 (51·8%) were from daily to event-driven and 79 (48·2%) from event-driven to daily.
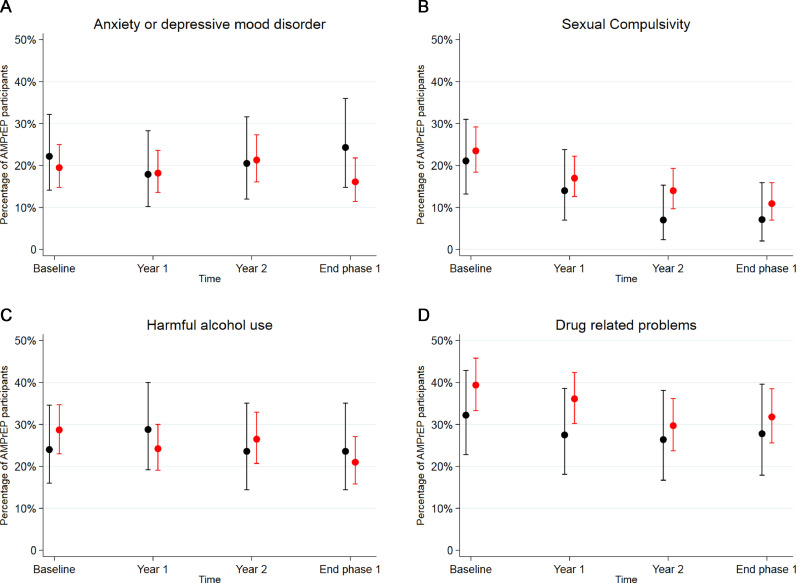
We found no significant change over time across both regimens in proportion of individuals assessed with anxiety or depressive mood disorders (20% at baseline to 18% at the end phase-1, p = 0.358, Fig. 1 and supplementary Table 1 for exact numbers per regimen, per year). We observed a significant decrease over time in proportion of individuals assessed with sexual compulsivity (23% at baseline to 10% at the end phase-1, p<0.001). The proportion of individuals assessed with alcohol use disorder did not change over time (28% at baseline to 22% at the end of phase-1, p = 0.106), yet the proportion with drug use disorder significantly decreased (38% at baseline to 31% at the end of phase-1, p = 0.026). None of the changes in mental health problems over time were significantly different between event-driven and daily PrEP regimens (p for interaction): anxiety or depressive mood disorder (p = 0.155), sexual compulsivity (p = 0.526), drug use disorder (p = 0.801), and alcohol use disorder (p = 0.561).
Fig. 1.
Mental and sexual health over time among 341 event-driven(ED, black whisker plots) and daily (red whisker plots) Pre-exposure prophylaxis users in the AMPrEP study using a logistic regression model with a random intercept for study participants, Amsterdam, the Netherlands, 2015–2018.
A Anxiety or depressive mood disorder. Decrease over time (p = 0.385).
B Sexual compulsivity. Decrease over time (p<0.001).
C Alcohol use disorder. Decrease over time (p = 0.106).
D Drug use disorder. Decrease over time (p = 0.026).
X-axis: time. Y-axis: percentage of AMPrEP participants. Abbreviations: AMPrEP, Amsterdam Pre-Exposure Prophylaxis for HIV study; according to mental health inventory 5 (MHI5, score<60), sexual compulsivity scale (SCS, score ≥24), alcohol use disorder identification test (AUDIT, score ≥ 8) and drug use disorder identification test (DUDIT, score ≥8). For exact numbers see eTable1.
In addition, participants became significantly less concerned about acquiring HIV over time (median concern 3 (IQR 2–4) at baseline to 5 (IQR 2–6) at the end phase-1, p<0.001, eFig. 2). Participants reported significantly less frequent use of alcohol (p<0.001), nitrites (p<0.001) and XTC (p = 0.005) over follow-up visits (Fig. 2), whereas no significant changes were reported in use of cannabis (p = 0.943), cocaine (p = 0.472), erectile dysfunction drugs (p = 0.104), GHB/GBL (p = 0.793), crystal meth (p = 0.096) or injecting drug use (p = 0.258). Again, none of the changes over time were significantly different between PrEP regimens.
Fig. 2.
Drug use over time among 341 pre-exposure prophylaxis users, The AmPrEP study, Amsterdam, The Netherlands, 2015–2018.
A Alcohol (decrease, p<0.001).
B Cannabis (p = 0.943).
C Cocaine (p = 0.472).
D Erectile dysfunction drugs (p = 0.104).
E GHB/GBL (p = 0.793).
F Methamphetamine (p = 0.096).
G Nitrites (decrease, p<0.001).
H XTC (decrease, p = 0.005).
X-axis: time. Y-axis: Percentage of AMPrEP participants. Abbreviations: AMPrEP, Amsterdam Pre-Exposure Prophylaxis for HIV study; GHB, gamma-hydroxybutyrate; GBL, gamma-butyrolacton,; XTC, 3,4-methyleendioxymethamfetamine.
dark red: ≥4 weekly, red: 2-4 weekly, orange: 2-4 monthly, yellow: ≤1 montlhy, green: no use.
At the last study visit, 26/147 (18%) participants assessed with a mental health problem reported visiting a health professional due to issues related to mental health, drug use, or sex (overall 49/290, 13%). Moreover, 78/290 (27%) reported ever having experienced a drug-induced blackout, of which 28/78 (36%) occurred in the past year; 16/287 (6%) reported intimate partner violence within the past 5 years; 41/287 (14%) reported ever having a non-consensual sexual experience, of which 15/41 (37%) occurred before the age of 18.
3.3. Developing and recovering from mental health problems during follow-up
From the multi-state Markov model, we showed univariable associations with developing or recovering from anxiety or depressive mood disorder (eTable 2), sexual compulsivity (eTable 3), alcohol use (eTable 4) or drug use disorders (eTable 5). In multivariable analysis (Table 2), there were several instances when the presence of one mental health problem was associated with the development or recovery from another mental health problem. Those assessed with anxiety or depressive mood disorder were less likely to recover from sexual compulsivity (aHR 0.3, 95%CI 0.2–0.6) and more likely to develop drug use disorder (aHR 2.3, 95%CI 1.2–4.6); those with sexual compulsivity were less likely to recover from anxiety or depressive mood disorder (aHR 0.5, 95%CI 0.3–1.0); and those with drug use disorder were more likely to develop sexual compulsivity (aHR 2.2, 95%CI 1.0–4.6) and alcohol use disorder (aHR 2.4, 95%CI 1.3–4.4). We found no associations with PrEP regimen or switching between regimens.
Table 2.
Characteristics associated with developing and recovering an anxiety or depressive mood disorder, sexual compulsivity, alcohol use or drug use disorder in multivariable Markov model among 341 AMPrEP participants, Amsterdam, The Netherlands, 2015–2018.a
| Anxiety or depressive mood disorder |
Sexual compulsivity |
Alcohol use disorder |
Drug use disorder |
|||||
|---|---|---|---|---|---|---|---|---|
| Developing | Recovering | Developing | Recovering | Developing | Recovering | Developing | Recovering | |
| aHR [95% CI] | aHR [95% CI] | aHR [95% CI] | aHR [95% CI] | aHR [95% CI] | aHR [95% CI] | aHR [95% CI] | aHR [95% CI] | |
| Age (years)b | ||||||||
| <35 | Ref | Ref | ||||||
| 35–44 | 1.3 [0.6–2.5] | 0.8 [0.5–1.6] | ||||||
| ≥45 | 2.2 [1.1–4.4] | 0.7 [0.4–1.2] | ||||||
| Education levelb | ||||||||
| Low and middle | Ref | Ref | ||||||
| University or higher | 0.3 [0.1–0.8] | 0.2 [0.1–0.7] | ||||||
| Employmentb | ||||||||
| Employed | Ref | Ref | ||||||
| Unemployed | 0.5 [0.2–1.0]c | 0.4 [0.2–0.8] | ||||||
| Residenceb | ||||||||
| Amsterdam | Ref | Ref | ||||||
| Other | 1.1 [0.6–2.1] | 1.7 [1.1–2.2] | ||||||
| Anxiety or depressive mood disorder | ||||||||
| Absent | / | / | Ref | Ref | Ref | Ref | ||
| Present | / | / | 1.1 [0.5–2.6] | 0.3 [0.2–0.6] | 2.3 [1.2–4.6] | 1.3 [0.7–2.4] | ||
| Sexual compulsivity | ||||||||
| Absent | Ref | Ref | / | / | Ref | Ref | ||
| Present | 0.9 [0.5–1.9] | 0.5 [0.3–1.0] | / | / | 1.0 [0.5–2.3] | 0.5 [0.2–0.9] | ||
| Alcohol use disorder | ||||||||
| Absent | / | / | ||||||
| Present | / | / | ||||||
| Drug use disorder | ||||||||
| Absent | Ref | Ref | Ref | Ref | / | / | ||
| Present | 2.2 [1.0–4.6] | 1.0 [0.6–1.8] | 2.4 [1.3–4.4] | 1.3 [0.8–2.2] | / | / | ||
Abbreviations: AMPrEP, Amsterdam Pre-Exposure Prophylaxis for HIV study; aHR, adjusted Hazard Ratio; CI, Confidence Interval.
According to mental health inventory 5 (MHI5, score<60), sexual compulsivity scale (SCS, score ≥24), alcohol use disorder identification test (AUDIT, score ≥ 8) and drug use disorder identification test (DUDIT, score ≥8).
Measurement at baseline.
95% CI crosses 1, not significant.
4. Discussion
In this prospective demonstration project, we described that more than half of GBMSM initiating PrEP were assessed with a mental health problem. At the end of follow-up, we observed a 13% reduction in the proportion with sexual compulsivity and 7% reduction with drug use disorder, but no significant difference in the proportion with anxiety or depressive mood disorders or alcohol use disorder. These findings provide important clinical insight on the extent of mental health problems and their changes among both daily and event-driven PrEP users.
The simultaneous decrease in drug use disorder and sexual compulsivity was unexpected. Explanations of how PrEP might influence drug-related problems and sexual compulsivity are speculative. Some individuals engage in sex-related drug use as means of losing sexual inhibition or increasing sexual arousal and confidence [19]. PrEP use, through the diminished fear of acquiring HIV, could buoy loss of sexual inhibition and confidence and replace the perceived need for drug use. The diminishing preoccupation in failure to use condoms and concern around HIV might give way to a decrease in sexual compulsivity [2,20]. An additional explanation could be tri-monthly counseling and motivational interviewing by medical staff. However, given the decreasing trend in sexual compulsivity amid stable number of anal sex acts previously observed in this cohort [3], more studies would be needed to disentangle the relationship between sexual behavior and compulsivity within the context of PrEP.
Unlike drug use disorders, we observed no decrease in the proportion of participants assessed with alcohol use disorder. A possible explanation could be that excessive drug use may be more strongly motivated by sex among GBMSM than alcohol use [20]. We also observed no decrease in the proportion with anxiety and depressive disorders. Previous studies have shown associations between internalizing disorders, such as depression, and drug use in GBMSM [21]. Nevertheless, it is unclear why the proportion of those with drug-use disorder was declining while that of anxiety or depression did not change during PrEP use. These diverging trends need to be confirmed in other studies.
One of the most striking features of these data is the comprehensive amount of mental health problems assessed by validated questionnaires, which is important given their potential for synergistic interaction [4,5,9]. The development and inability to recover from certain mental health disorders could be linked to the presence of others. Indeed, being assessed with anxiety or depressive mood disorder made it less likely to recover from sexual compulsivity and vice versa. This finding illustrates that the syndemic nature and complexity of individual mental health problems cannot be fully captured in population estimates.
There are marked differences between daily and event-driven PrEP users. In AMPrEP, individuals choosing daily PrEP at baseline had more sexual partners, were more likely to be diagnosed with a prevalent STI, and were less likely to be in a steady relationship than event-driven users [11]. While on PrEP, daily users have a higher incidence in STIs and higher numbers of total sexual partners and condomless anal sex acts compared to event-driven users [3,11]. On the contrary, we demonstrate that there is no difference between daily and event-driven PrEP in the proportion with mental health disorders across visits and thus mental health problems appear to affect all PrEP users irrespective of PrEP regimen.
It remains debatable to what extent mental health problems in GBMSM PrEP users are different than their overall source population. National data from Statistics Netherlands reported that 10.5% of Dutch men within the age of 35 to 45 were assessed with an anxiety or depressive mood disorder using the MHI5 [22], compared to 20.5% among AMPrEP participants. A study using a national sample among 1033 HIV-negative GBMSM in the United States observed a prevalence of depression (as measured by the 20-item Centre for Epidemiological Studies Depression scale) at 26.7%, sexual compulsivity at 13.8%, and polydrug use at 8% [7]. From our study and others, the prevalence of depression among PrEP using GBMSM could be considered comparable to the general U.S. GBMSM population (11–40%), while prevalence of sexual compulsivity (31%), alcohol use disorder (28–40%), and drug use disorder (36–37%) were all higher [12,13,23]. Notwithstanding the differences in mental health assessments and demographic composition between studies, the relatively higher prevalence of these disorders emphasizes the importance of addressing mental health in GBMSM who initiate PrEP.
High levels of drug use among GBMSM PrEP users have been reported previously [10,12,13]. In our study, participants reported using most of their drugs 2–4 times a month or less. This could indicate that some individuals can effectively manage drug use in a positive, recreational manner [24]. However, with 28/290 (10%) experiencing a blackout due to drug use in the past year, problems like hospitalization, and neurological damage should not be underestimated [25].
The extent of mental health disorders found here does provide a sense of the psychological needs for this population. Of the 52% reporting a mental health problem at the last follow-up visit, only 26/147 (18%) of them sought help. This proportion is remarkably lower compared to the general Dutch population, wherein 34% with a mental health problem sought professional help [26]. Barriers to help seeking behavior need to be addressed in future studies [27]. Currently, standard screening or referral for mental health problems is not recommended in PrEP guidelines. Given their overall prevalence, and the entanglement of disorders, PrEP services offer a unique opportunity to integrate mental health care using a syndemic-based approach.
Our study has some limitations. First, the mental health assessments used in our study are meant for screening and not diagnostic purposes. The true prevalence of assessed mental disorders could be in fact lower, while other mental disorders could have gone unnoticed. Second, our project was the first to offer access to free-of-charge PrEP in the Netherlands. The study population likely represented early adopters, most of whom were white, older and highly educated. Included participants are unlikely to represent others who could benefit from PrEP. Considering that people with lower education or non-Western migration background have a higher prevalences of mental health problems compared to the general population [22], it is unlikely that including these individuals would lower the prevalence of mental health problems. Third, individuals with depressive symptoms could be more likely to discontinue PrEP or become lost to follow-up. We did not observe a significant difference in median follow-up time between those with and without baseline mental health disorders, yet this does not preclude the potential bias of decreasing proportions with mental health disorders due to attrition. Finally, causality between PrEP use and decrease in mental health problems cannot be inferred from this study. Participants received – apart from PrEP – trimonthly motivational-based counseling regarding sexual health and assessments about sexual, drug- and alcohol-use behavior. Motivational interviewing on sexual behavior has previously shown to lead to a decrease in depression, anxiety and stress among HIV-positive adults [28]. The questionnaires on sexual health and drug use could have influenced respondents, leading them to rethink behavioral choices [29]. As motivational interviewing might not be standard of care and assessments on sexual health and drug use are not likely to be implemented in real-life settings, we urge caution in the generalizability of our findings to clinical settings.
Similar decreasing trends in sexual compulsivity and drug use disorder were observed in a prospective study among MSM performed by our public health service [30]. In that study, we aimed to increase help-seeking behaviour by screening for psychosocial problems in addition to personalized feedback. Similarly in AMPrEP, we also offered trimonthly motivational-based counseling regarding sexual health with comprehensive assessments of mental health, substance use and sexual behaviour. The impact of supportive assessments, motivational interviewing and the role of a long-term patient – healthcare provider relationship within a sexual health context warrants further research.
Although mental health problems were prevalent, with decreases over time in sexual compulsivity and drug use disorder, we observed no evidence to suggest that risk compensation involving drug use or the development or worsening of mental health problems occurred with time on PrEP. Based on our findings, PrEP guidelines should address mental health and drug use problems in GBMSM both at PrEP initiation and during PrEP follow-up. Given the interrelatedness of disorders, PrEP services should consider integrating mental health and addiction services.
Author contributions
Study concept and design: RA, EH, UD, MSvdL, MP, HdV; data acquisition: EH, RA; analysis and/or interpretation of data: RA, LC, SM, AB, MvR and HdV; drafting of the article: RA, AB and HdV; critical revision of the article: all authors.
Data sharing
The AMPrEP data are owned by the Public Health Service of Amsterdam. Original data can be requested by submitting a study proposal to the steering committee of AMPrEP. The proposal format can be obtained from the corresponding author (h.j.devries@amsterdamumc.nl or amprep@ggd.amsterdam.nl). Requests for further information can also be submitted via the same email addresses. The AMPrEP steering committee will check each proposal for compatibility with general objectives, ethical approvals, and informed consent forms of the AMPrEP study, and potential overlap with ongoing work. There are no other restrictions to obtaining the data and all data requests will be processed in the same manner.
Declaration of Competing Interest
Dr. Achterbergh and Dr. Hoornenborg reports grants and non-financial support (study medication) from Gilead Sciences all provided to their institution. Dr. Boyd, L. Coyer, Dr. van Rooijen and Dr. de Vries report grants from ZonMW, grants from National Institute for Public Health and the Environment and GGD research funds, non-financial support and grants from Gilead Sciences, grants from Aidsfonds Netherlands, grants from Stichting Amsterdam Dinner Foundation, grants from Gilead Sciences Europe Ltd, grants from Janssen Pharmaceuticals, grants from M.A.C. AIDS Fund and grants from ViiV Healthcare provided to their institution during the conduct of the study. Dr. Davidovich reports non-financial support and unconditioned grants for conduction of AMPrEP study and speaker fees, all provided/paid to his institution. Dr. Prins reports unrestricted research grants and speaker fees from Gilead Sciences, Roche, Abbvie and MSD, all of which were paid to her institute, during the conduct of the study. The other authors reported no conflicts of interests.
Acknowledgments
Acknowledgements
The authors thank the following persons for their invaluable support to this study: Kees de Jong, Ilya Peters, Princella Felipa, Paul Oostvogel, Sylvia Bruisten, Wendy van der Veldt, Homeyra Amir, Marjo Broeren, Michelle Kroone, Myra van Leeuwen, Adriaan Tempert, Dominique Loomans, Ertan Ersan and Gerben Rienk Visser as well as the teams of the STI outpatient clinic and research department of the department of infectious diseases of Public Health Service of Amsterdam.
AMPrEP is part of the HIV Transmission Elimination Amsterdam (H-team) Consortium (www.hteam.nl)
We thank all AMPrEP participants.
Funding
The AMPrEP study received funding as part of the H-team initiative from ZonMw (grant number: 522002003), the National Institute for Public Health and the Environment and GGD research funds. The study drug was provided by Gilead Sciences. The H-TEAM initiative is supported by the Aidsfonds Netherlands (grant number: 2013169), Stichting Amsterdam Dinner Foundation, Gilead Sciences Europe Ltd (grant number: PA-HIV-PREP-16–0024), Gilead Sciences (protocol numbers: CO-NL-276-4222, CO-US-276-1712), Janssen Pharmaceuticals (reference number: PHNL/JAN/0714/0005b/1912fde), M.A.C. AIDS Fund, and ViiV Healthcare (PO numbers: 3000268822, 3000747780).
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2020.100505.
Appendix. Supplementary materials
References
- 1.Fonner V.A., Dalglish S.L., Kennedy C.E., Baggaley R., O'Reilly K.R., Koechlin F.M. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS. 2016;30(12):1973–1983. doi: 10.1097/QAD.0000000000001145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zimmerman H., Postma L., Eekman S., Achterbergh R., Prins M., MSvd L.o.e.f.f. ARPH Annual Conference. 2019. The impact of PrEP use on the sexual well-being of men who have sex with men (MSM). Oral presentation. [Google Scholar]
- 3.Hoornenborg E., Coyer L., Achterbergh R.C.A., Matser A., Schim van der Loeff M.F., Boyd A. Sexual behaviour and incidence of HIV and sexually transmitted infections among men who have sex with men using daily and event-driven pre-exposure prophylaxis in AMPrEP: 2 year results from a demonstration study. Lancet HIV. 2019;6(7):e447–ee55. doi: 10.1016/S2352-3018(19)30136-5. [DOI] [PubMed] [Google Scholar]
- 4.Mercer C.H., Prah P., Field N., Tanton C., Macdowall W., Clifton S. The health and well-being of men who have sex with men (MSM) in Britain: evidence from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3) BMC Public Health. 2016;16:525. doi: 10.1186/s12889-016-3149-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.King M., Semlyen J., Tai S.S., Killaspy H., Osborn D., Popelyuk D. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8:70. doi: 10.1186/1471-244X-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meyer I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parsons J.T., Millar B.M., Moody R.L., Starks T.J., Rendina H.J., Grov C. Syndemic conditions and HIV transmission risk behavior among HIV-negative gay and bisexual men in a U.S. national sample. Health Psychol. 2017;36(7):695–703. doi: 10.1037/hea0000509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferlatte O., Salway T., Samji H., Dove N., Gesink D., Gilbert M. An application of syndemic theory to identify drivers of the syphilis epidemic among gay, bisexual, and other men who have sex with men. Sex Transm Dis. 2018;45(3):163–168. doi: 10.1097/OLQ.0000000000000713. [DOI] [PubMed] [Google Scholar]
- 9.Singer M., Bulled N., Ostrach B., Mendenhall E. Syndemics and the biosocial conception of health. Lancet. 2017;389(10072):941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- 10.McCormack S., Dunn D.T., Desai M., Dolling D.I., Gafos M., Gilson R. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387(10013):53–60. doi: 10.1016/S0140-6736(15)00056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoornenborg E., Achterbergh R.C., van der Loeff M.F.S., Davidovich U., van der Helm J.J., Hogewoning A. Men who have sex with men more often chose daily than event-driven use of pre-exposure prophylaxis: baseline analysis of a demonstration study in Amsterdam. J Int AIDS Soc. 2018;21(3):e25105. doi: 10.1002/jia2.25105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu A.Y., Cohen S.E., Vittinghoff E., Anderson P.L., Doblecki-Lewis S., Bacon O. Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Intern Med. 2016;176(1):75–84. doi: 10.1001/jamainternmed.2015.4683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilton J., Noor S.W., Schnubb A., Lawless J., Hart T.A., Grennan T. High HIV risk and syndemic burden regardless of referral source among MSM screening for a PrEP demonstration project in Toronto, Canada. BMC Public Health. 2018;18(1):292. doi: 10.1186/s12889-018-5180-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.AMPrEP study group. Study protocol AMPrEP. 2015. available athttps://www.trialregister.nl/trial/5302. Accessed 1 September 2019.
- 15.Kelly M.J., Dunstan F.D., Lloyd K., Fone D.L. Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: a comparison of five different methods. BMC Psychiatry. 2008;8:10. doi: 10.1186/1471-244X-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalichman S.C., Rompa D. Sexual sensation seeking and Sexual Compulsivity Scales: reliability, validity, and predicting HIV risk behavior. J Pers Assess. 1995;65(3):586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- 17.Babor T.F., Higgins-Biddle J.C., Saunders J.B., Monteiro M.G. World Health Organization; Geneva: 2001. The alcohol use disorders identification test: guideline for use in primary care; p. 2001. [Google Scholar]
- 18.Voluse A.C., Gioia C.J., Sobell L.C., Dum M., Sobell M.B., Simco E.R. Psychometric properties of the drug use disorders identification test (DUDIT) with substance abusers in outpatient and residential treatment. Addict Behav. 2012;37(1):36–41. doi: 10.1016/j.addbeh.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 19.Bourne A., Reid D., Hickson F., Torres-Rueda S., Weatherburn P. Illicit drug use in sexual settings ('chemsex') and HIV/STI transmission risk behaviour among gay men in South London: findings from a qualitative study. Sex Transm Infect. 2015;91(8):564–568. doi: 10.1136/sextrans-2015-052052. [DOI] [PubMed] [Google Scholar]
- 20.Rooney B.M., Tulloch T.G., Blashill A.J. Psychosocial syndemic correlates of sexual compulsivity among men who have sex with men: a meta-analysis. Arch Sex Behav. 2018;47(1):75–93. doi: 10.1007/s10508-017-1032-3. [DOI] [PubMed] [Google Scholar]
- 21.Lachowsky N.J., Dulai J.J., Cui Z., Sereda P., Rich A., Patterson T.L. Lifetime doctor-diagnosed mental health conditions and current substance use among gay and bisexual men living in Vancouver, Canada. Subst Use Misuse. 2017;52(6):785–797. doi: 10.1080/10826084.2016.1264965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.SN. MD. Geestelijke ongezondheid in Kaart gebracht (in Dutch). 2011. available athttps://wwwcbsnl/-/media/imported/documents/2011/03/2011-geestelijke-ongezondheid-in-nederland-in-kaart-gebracht-art-v3pdf. Accessed at 1 September 2019.
- 23.Hoenigl M., Jain S., Moore D., Collins D., Sun X., Anderson P.L. Substance use and adherence to HIV preexposure prophylaxis for men who have sex with men(1) Emerg Infect Dis. 2018;24(12) doi: 10.3201/eid2412.180400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holt M. Sex, drugs, and HIV: let's avoid panic. The Lancet HIV. 2014;1(1):e4–e5. doi: 10.1016/S2352-3018(14)70007-4. [DOI] [PubMed] [Google Scholar]
- 25.Raposo Pereira F., McMaster M.T.B., Polderman N., de Vries Y., van den Brink W., van Wingen G.A. Adverse effects of GHB-induced coma on long-term memory and related brain function. Drug Alcohol Depend. 2018;190:29–36. doi: 10.1016/j.drugalcdep.2018.05.019. [DOI] [PubMed] [Google Scholar]
- 26.Graaf Rd hM., Dorsselaer Sv. De psychische gezondheid van de Nederlandse bevolking (in Dutch) Trimbos. 2010 https://wwwtrimbosnl/?act=winkeldldownload&prod=295) available at. Accessed at 1 September 2019. [Google Scholar]
- 27.Salway T., Ferlatte O., Shoveller J., Purdie A., Grennan T., Tan D.H.S. The need and desire for mental health and substance use-related services among clients of publicly funded sexually transmitted infection clinics in Vancouver, Canada. J Public Health Manag Pract. 2018 doi: 10.1097/PHH.0000000000000904. [DOI] [PubMed] [Google Scholar]
- 28.Lovejoy T.I. Telephone-delivered motivational interviewing targeting sexual risk behavior reduces depression, anxiety, and stress in HIV-positive older adults. Ann Behav Med. 2012;44(3):416–421. doi: 10.1007/s12160-012-9401-6. [DOI] [PubMed] [Google Scholar]
- 29.Kurtz S.P., Surratt H.L., Buttram M.E., Levi-Minzi M.A., Chen M. Interview as intervention: the case of young adult multidrug users in the club scene. J Subst Abuse Treat. 2013;44(3):301–308. doi: 10.1016/j.jsat.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Achterbergh R.C.A, Van Rooijen M.S., Van den Brink W., Boyd A., de Vries H.J.C. Enhancing help-seeking behaviour among men who have sex with men at risk for sexually transmitted infections: the syn.bas.in randomised controlled trial. Sex Transm Infect. 2020 doi: 10.1136/sextrans-2020-054438. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.