Abstract
Background
The novel coronavirus (COVID-19) pandemic has defined 2020 thus far. Businesses, social and religious gatherings, travel, and almost all forms of transportation shut down to halt the spread of COVID-19. People were ordered to quarantine in place, and the world appears to go into a standstill. In the midst of being quarantined people with acute and chronic conditions still require medical care and treatment. An alternative way for people to receive needed health care was necessary. Hence, we saw an unprecedented surge in telehealth. With this unprecedented surge in use of telehealth, there is matter of delivering quality care.
Objective
Guided by the Donabedian Model, the purpose of this integrative review was to examine current evidence on patient and healthcare provider's satisfaction with the use of telehealth during the COVID-19 pandemic.
Design
An integrative review of the literature
Data sources
The literature review was conducted utilizing PubMED, CINAHL, Google Scholar and Cochrane Library databases. Inclusion criteria were studies published from January 2020 to July 11, 2020, published and translated in English language, and studies that evaluated patients and providers satisfaction with the use of telehealth or telemedicine during COVID-19. Eighteen articles were included in this review.
Review methods
An evaluation matrix was developed to collect data from the included articles. The articles were appraised using Fineout-Overholt & Gallagher-Ford Rapid Critical Appraisal Checklist for Descriptive Studies and Rapid Critical Appraisal of Evidence-Based Practice Implementation or Quality Improvement Projects (Melnyk & Fineout-Overholt, 2015). Authors independently appraised each article using the appropriate appraisal tools.
Results
Ten of the articles (53%) included were studies conducted in the United States. Sixteen out of 18 studies evaluated patient satisfaction and five studies examined healthcare providers’ satisfaction with the use of telehealth. The majority of telehealth services offered were by subspecialists. Overall, patients and healthcare providers have high level of satisfaction with the use of telehealth during COVID-19 pandemic. Many patients and healthcare providers reported willingness to continue using telehealth after the pandemic.
Conclusion
This integrative review provided additional evidence on patient and healthcare provider's satisfaction with the use of telehealth. Findings in this review may not be surprising as individuals, healthcare providers, and health systems needed to adopt the use telehealth due to necessity. However, the results for telehealth are promising.
Keywords: Telehealth, Telemedicine, Satisfaction, COVID-19 pandemic
Contribution to the paper
What is already known about the topic?
-
1.
Telehealth is not a new approach in health care.
-
2.
There is evidence that showed telehealth can improve a patient's overall health and lifestyle.
-
3.
Telehealth adoption was very slow before the COVID-19 pandemic.
What this paper adds
-
1.
Coronavirus (COVID-19) pandemic has propelled the surge in the use of telehealth.
-
2.
Patients have high level of satisfaction with the use of telehealth during COVID-19 pandemic.
-
3.
Healthcare providers in subspecialty areas are satisfied with the use of telehealth during a pandemic
1. Background
The novel coronavirus, or COVID-19, has defined 2020 thus far. This viral illness has become a dictator of economies, societies, and medicine worldwide. COVID-19 first appeared in Wuhan, China, which quickly spread worldwide; so much so that in early 2020 the World Health Organization (WHO) declared a pandemic (Centers for Disease Control and Prevention [CDC], 2020). By July 2020, there were almost 14 million people infected with COVID-19 worldwide, with nearly 3.5 million cases in the United States (U.S.) alone (Johns Hopkins University and Medicine, 2020). Furthermore, there have been over 550,000 deaths worldwide, and 136,000 in the US (CDC, 2020). Almost all countries shut down businesses, social and religious gatherings, travel, and almost all forms of transportation to halt the spread of COVID-19. Worldwide, people were ordered to quarantine in place and the world went into a standstill. Unfortunately, while people were quarantined those with acute and chronic conditions still require medical care and treatment. An alternative way for these individuals to receive health care was necessary. The government has promoted the use of telehealth and made provisions to address some of the earlier known barriers, including reimbursement; hence an upsurge in the adoption of telehealth (Annis et al., 2020; Peden et al., 2020). Telehealth is the use of information and communication technologies (ICT), including computers and mobile devices, to access care remotely and to manage health (Mayo Clinic, n.d). Born out of necessity, many health care systems have expeditiously adopted or switched their current platform from face-to-face visits to telehealth in order to continue or sustain delivery of care to patients during the pandemic. However, with this unprecedented upsurge in the use of telehealth, there is matter of delivering quality care or service to the patients. Therefore, guided by the Donabedian (2005) Model, the purpose of this systematic review was to examine current evidence on patient and provider satisfaction regarding the use of telehealth during the COVID-19 pandemic.
2. PICOT question
The clinical question for this systematic review was, among patients and providers (P), what is their satisfaction (O) with the use of telehealth or telemedicine (I) during COVID-19 pandemic (T)?
3. Method
3.1. Design
This is an integrative research review of the literature. The steps used by the authors in conducting this integrative review were 1) identify the clinical topic of interest, 2) develop a PICOT question, 3) search strategy/inclusion and exclusion criteria, 4) conduct quality assessments of the articles, 4) extract and analyze data, 5) synthesize the results, and 6) identify implications to nursing.
3.2. Search strategy
Electronic databases searched included PubMED, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Google Scholar, and Cochrane Library. Articles included in the review were those published from January 1, 2020 to July 11, 2020, articles published and translated in the English language, and studies that evaluated patients and providers satisfaction in the use of telehealth or telemedicine. Abstracts, protocols, commentaries, non-English, usability assessment of an app only, studies evaluating student training, and satisfaction studies on the use of telehealth prior to the COVID-19 pandemic were excluded. Keywords used in the search were COVID-19 AND telehealth AND satisfaction; telemedicine AND satisfaction AND COVID-19; teleconsultation AND COVID-19 AND satisfaction; tele* AND satisfaction AND COVID-19.
3.3. Quality assessment
The articles were appraised using Fineout-Overholt & Gallagher-Ford Rapid Critical Appraisal Checklist for Descriptive Studies and Rapid Critical Appraisal of Evidence-Based Practice Implementation or Quality Improvement Projects (Melnyk and Fineout-Overholt, 2015). Authors independently appraised each article using the appropriate appraisal tools. All articles that fit the inclusion and exclusion criteria in this integrative review were included regardless of the appraisal results.
3.4. Data abstraction and data analysis
An evaluation matrix was developed to collect data from the included articles. The articles were organized and evaluated in an evaluation matrix that included the following: authors and date of publication, design method, sample settings, variables and measurements, study findings, and level of evidence. The Rating System for the Hierarchy of Evidence for Intervention and Treatment Questions by Melnyk and Fineout-Overholt (2015) was used to determine the level of evidence (LOE) for each study.
4. Results
4.1. Article/Sample characteristics
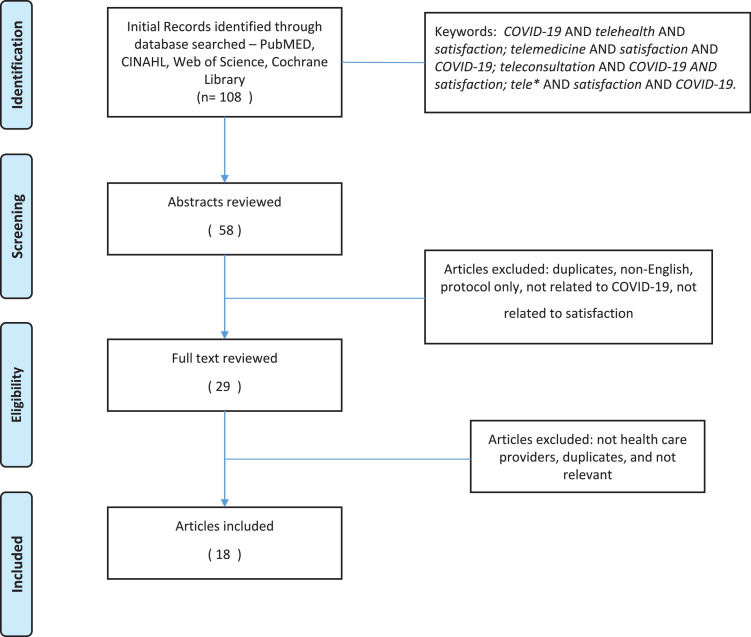
Initial search for articles generated 108 articles, of which 18 articles fit the inclusion and exclusion criteria set in this integrative review (See Table 1). The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram was used to demonstrate the search strategy (see Fig. 1). All of the articles reviewed have level of evidence VI. Five of the 18 articles were quality improvement (QI) projects. Ten of the articles (56%) were studies conducted in the US, two were from the United Kingdom, and one study each from Italy, France, Slovenia, Hong Kong, China, and India. All studies captured data during COVID-19 pandemic. The duration of the studies ranged from a minimum of 4 days to maximum of 119 days. The overall sample for all the articles included was 15,539 (14,767 for patients and 772 healthcare providers). The sample size for each reviewed article ranged from 41 to 4589 with patients and range from 13 to 503 with healthcare providers.
Table 1.
Included Articles Characteristics.
| Primary author (yr.) Country of Publication | Design | Service Area offered/Data range collection | Sample, sample size and setting | Method/instruments used | Level of Evidence (LOE) |
|---|---|---|---|---|---|
| Ambrosini et al. (2020) Italy |
Descriptive | GU cancer (Uro-oncology) From Mar. 9, 2020 |
41 out of 60 patients who were scheduled for virtual consultation responded to the survey. Response rate – 68.3% | Survey | LOE VI |
|
Dobrussin et al. (2020) USA |
Descriptive | GI March- May 2020 |
1492 patients and 503 providers responded to the survey; 65% females Michigan and Washington DC |
Online survey | LOE VI |
|
Fieux et al. (2020) France |
Quantitative, Prospective Survey | ENT April 6–10, 2020 |
100 of the 125 patients in the ENT tele-consultation over the 7-day inclusion period completed the survey Mean age= 51; 2:3 M/F ratio Lyon, France |
Questionnaire | LOE VI |
|
Gilbert et al. (2020) UK |
qi | orthopedic march 16-april 20, 2020 |
215 patients; 103 clinicians RNOC |
Survey | LOE VI |
|
Holcomb et al. (2020) USA |
Descriptive cross-sectional | Prenatal visit March 17-May 31, 2020 |
283 out of 421 pregnant women who participated in at least one visit agreed to participate (65% response rate); 89% females; 84% Whites; 66.8% with college degrees Texas |
Telephone survey | LOE VI |
|
Holtz (2020) USA |
Descriptive cross-sectional |
Not identified March 31-April 20, 2020 |
1011 participated the survey but data from 434 participants who had used telemedicine were included in their analysis; 89% females | Survey | LOE VI |
|
Itamura et al. (2020) USA |
Descriptive | Otolaryngo-logy clinic January 1-May 1, 20,202 |
195 virtual visits and 4013 in-person visits California |
Survey | LOE VI |
|
Kanc et al. (2020) Slovenia |
Descriptive Pilot study |
DM April – May 2020 |
98, 60% women, with mean age of 52 (SD=15.1), recent A1C level 7.1% | Telephone Survey | LOE VI |
|
Layfield et al. (2020) USA |
Descriptive | Head and Neck March 25-April 24, 2020 |
100 patients who had video-based telemedicine visits only (FaceTime= 22; BluJeans = 58; Doximity =20). Mean age 62.6 (SD=13.9) years; 59% males; 94% were return patients; 66% had some college or had college degree; 55% had private insurance; Pennsylvania |
Survey | LOE VI |
|
Li et al. (2020) Hong Kong |
Descriptive Pilot study |
Vascular Feb 19- March 16, 2020 |
114 patient. Mean age = 60 (SD 15.2) years old; 65% men; 81% were post-op patients. China |
Questionnaire | LOE VI |
|
Liu et al. (2020) China |
Descriptive Retrospective review |
Adults and Paediatrics Health, and Psychological counselling Jan. 24 to Feb. 17, 2020 |
4589 patients; 58% females and 42% males; Age range - 78 days old to 85 years old. 81% were aged 20–39 age group |
Electronic Questionnaire | LOE VI |
|
Mann et al. (2020) USA |
Descriptive |
Urgent and non-urgent ambulatory care visits January 1 to April 14, 2020 |
1693 participants; Highest age group aged 20–44, particularly for urgent care. NYU Langone |
text message survey | LOE VI |
| Mostafa et al. (2020) USA |
Descriptive | Allergy & Immunology Apr. 13-May 8, 2020 |
177 out of 290 who received telemedicine completed satisfaction survey; 65% females Median age – 33 years old; 65% females; 41% were new patient (NP) encounters Rochester, NY |
Survey | LOE VI |
|
Rametta et al. (2020) USA |
QI | Pediatric Oct. 1 to Mar. 15, 2020 (in – person) and Mar. 16- Apr. 24, 2020 (telemed-icine) |
2589 telehealth encounters Most common diagnosis: epilepsy and migraine Philadelphia |
Survey | LOE VI |
|
Shenoy et al. (2020) India |
QI Audit | Rheumatology Mar. 12–20, 2020 |
100 completed satisfaction survey Median age 54, 87% females |
Survey | LOE VI |
|
Smrke et al. (2020) UK |
Descriptive Retrospective case series |
Rare Cancer Mar. 23 to April 24, 2020 |
108 patients completed survey (70 telemedicine and 34 face-to-face); median age 58 years old; 56% females 18 clinicians: (4 consultants, 4 clinical research fellows, 4 residents, 2 nurse specialists, 4 research nurses Royal Mardsen Hospital Sarcoma Unit, UK |
Patient and provider experience with telemedicine - Questionnaire | LOE VI |
|
Svider et al. (2020) USA |
Descriptive survey-based study | Rhinology April 2020 |
135 respondents from four practice regions New Jersey |
Degree of use; Satisfaction with service – Anonymous Survey |
LOE VI |
|
Tenforde et al. (2020) USA |
QI | Sports & Musculoskeletal Most common duration 15–29 min April 6–17, 2020 |
Surveys completed by 119 patients and 13 physiatrists. Majority of patients were female and age range was 34–64. |
# of telemedicine visits, types, duration of encounter, quality and satisfaction - Survey Physician experiences performing telemedicine - Survey |
LOE VI |
Fig. 1.
Search Strategy and Selection of Paper
Telehealth Platforms and Services Offered.
Telehealth platforms used varied among studies. Table 2 presents the different telehealth platforms. No single technology platform was used consistently. The telehealth platform used in each of the studies was dependent on the technology available in the country where the study was conducted. Services offered by the healthcare system or providers varied by study, but the majority of services offered were in sub-specialty areas, such as allergy and immunology, pediatricians, head, eyes, ears, nose and throat (HEENT), oncologist, otolarhygologist, gastroenterologist, vascular surgeons, rheumatology, musculoskeletal and sport medicine, and orthopedics.
Table 2.
Telehealth platform.
| Study | Platform |
|---|---|
| AMBROSINI ET AL. (2020) | Patients were told via email with phone call by urologist; F2F only if disease progression, metastasis or clinical troubles. Providers met via Zoom (Zoom Video Communication, Inc. San Jose, California, 2011) |
| DOBRUSSIN ET AL. (2020) | Desktop/laptop; smartphones/tablets; phones |
| FEIUX ET AL. (2020) | Teleconsultation used SARA platform accessible via computer, smartphones, Apple or Android. |
| GILBERT ET AL. (2020) | Virtual Consultation platform Attend Anywhere |
| HOLCOMB ET AL. (2020) | Audio-only virtual visit |
| HOLTZ ET AL (2020) | Various devices such as laptop, smart watch, smart phones, tablets, etc. |
| ITAMURA ET AL. (2020) | Providers have used Doximity Dialer videoconferencing software for most visits, with FaceTime as an alternative |
| KANC ET AL. (2020) | Patients chose telephone (90%), WhatsApp (6%) and Skype (2%) to discuss results |
| LAYFIELD ET AL. (2020) | Earliest remote communication was conducted via Apple FaceTime Institution-licensed platform: Blue Jeans, Doximity |
| LI ET AL. (2020) | Video calls using WeChat software |
| LIU ET AL. (2020) | In order to consult with a clinician, patients can scan the official QR (Quick Response) code or follow the WeChat public account HNFYSY1904, which directs them to the expert consultation |
| MANN ET AL. (2020) | Video-based telemedicine |
| MUSTAFA ET AL. (2020) | Telemedicine encounters were completed using the following third-party vendors: Epic Warp (Epic Systems Corp, Verona, Wisconsin); Skype (Skype Communications, Palo Alto, California); FaceTime (Apple Inc, Cupertino, California); and Doximity (Doximity, San Francisco, California), depending on the patient preference. |
| RAMETTA ET AL. (2020) | Audio-video telemedicine |
| SHENOY ET AL. (2020) | Teleconsultation using WhatsAPP app. |
| SMRKE ET AL. (2020) | Phone |
| SVIDER ET AL. (2020) | Various video platforms including Doxy.me, Zoom, Google Hangouts, Apple Facetime, Skype, Upfox, VSee, Others |
| TENFORDE ET AL. (2020) | Synchronous audiovisual telemedicine platforms and included both InTouch and Zoom |
Legends: F2F – face-to-face.
4.2. Satisfaction
Sixteen out of 18 studies evaluated patient satisfaction and five studies examined healthcare providers’ satisfaction with the use of telehealth (see Table 3). The majority (14/16) of the studies showed high level of patient satisfaction with the use of telehealth during the COVID-19 pandemic. The study by Itamura et al. (2020) reported that patients were more satisfied with inpatient (93%) rather than virtual consultation (93% vs. 74%, respectively). One study did not report any score on patient satisfaction but reported high level based on caregiver's positive comments with use of telehealth (Kanc et al., 2020).
Table 3.
Satisfaction Results.
| Article | Patient satisfaction | Provider satisfaction |
|---|---|---|
| Ambrosini et al. (2020) | Most patients had high level of satisfaction - (M = 4.7/5). | |
| Dobrussin et al. (2020) | Overall, patients were highly satisfied (greater than 80%) with their telehealth visits. | High level of satisfaction (greater than 90%) with telehealth services among providers |
| Fieux et al. (2020) | Overall satisfaction was 87%. | |
| Gilbert et al. (2020) | Satisfaction scores were high for phone and virtual consultations (90 and 85%, respectively) | Clinicians rated virtual consultation as 78/100 for clinicians |
| Holcomb et al. (2020) | 99% participants rated their visit “good” or “very good | |
| Holtz et al. (2020) | People were overall satisfied with their telemedicine experience(s), (mean = 1.67, SD = 0.61). [lower score represents higher satisfaction] | |
| itamura et al. (2020) | inpatient visit satisfaction survey – 93% virtual visit satisfaction survey – 74% |
|
| Kanc et al. (2020) | Almost all had positive comments about telemedicine appointment and 72% would consider after Covid-19 | |
| Layfield et al. (2020) | Satisfaction score with telehealth (6.29/7), [higher score represents higher satisfaction] Average score across all questions was 6.01 on a scale from 1 to 7, where 7 indicated the highest level of patient agreement. |
|
| Li et al. (2020) | Overall experience of the video consultation, all of the patients were ‘‘satisfied’’ or ‘‘highly satisfied’’ with the video calls | |
| Liu et al. (2020) | 98.1% (n = 966) of respondents were satisfied (rated as 4 stars or above/5 star) with the service they received. | |
| Mann et al. (2020) | Satisfaction score was 4.73/5 | |
| Mostafa et al. (2020) | Overall satisfaction with telemedicine encounter was rated as agree and strongly agree – 96.7%; telemedicine was as satisfactory as in-person – 77.4% | |
| Rametta et al. (2020) | Caregivers indicated an interest in telemedicine as part of future care for 86% of encounters | Overall provider satisfaction with telemedicine in 93% of the encounters; 60% were very satisfied; 89% would use telemedicine components for follow-up |
| Shenoy et al. (2020) | Overall median satisfaction was 9 (IQR 8–1) on the Numeric Rating Scale. | |
| Smrki et al. (2020) | Mean satisfaction with telephone consultation was higher than face-to-face consultation (rating 8.99/10 vs. 8.35/10, respectively). | |
| Svider et al. (2020) | 82.0% noted feeling some level of satisfaction ranging from absolutely satisfied to satisfied, while 18.0% reported dissatisfaction or total failure. Telemedicine satisfaction levels did not differ by region (MW, NE, S, W satisfaction at 86.2%, 84.1%, 78.8, 76.0%, respectively, p = 0.73). |
|
| Tenforde et al. (2020) | Patient rated telemedicine visit as excellent or very good across measures (91.6–95%) | 92.3% of physicians reported excellent or very good overall satisfaction |
Of the five studies that evaluated clinician satisfaction with the use of telehealth, four studies reported high level of satisfaction based on scores of 80% and above (Dobrussion et al., 2020; Rametta et al., 2020; Svider et al., 2020; Telforde et al., 2020), whereas one study reported healthcare provider's satisfaction score of 78 out of 100 (Gilbert et al., 2020). Several studies noted that patients and healthcare providers were willing to continue to use telehealth as part of their follow-up visits even after the COVID-19 pandemic (Dobrussin et al., 2020; Holtz et al., 2020; Li et al., 2020; Rametta et al., 2020).
5. Discussion
Findings from this integrative review showed high level of satisfaction with the use of telehealth by patients and healthcare providers during the COVID-19 pandemic. The finding of high patient satisfaction with use of telehealth was supported by several studies prior to the pandemic (Kruse et al., 2017; Moore et al., 2020; Orlando et al., 2019; Polinski et al., 2016). This result may not be too surprising, as one of the main reasons for increased use of telehealth services is driven by necessity. Telehealth presented an avenue for the patients to have continuity of care during this unprecedented time. The use of telehealth and telemedicine are not new. Telehealth, a subset of E-Health, is the umbrella term for clinical and non-clinical services provided remotely, whereas telemedicine is a subset of telehealth, which involves delivery of clinical services to patients with the use of electronic communications and software (Cranford, 2020). Prior to COVID-19, the adoption to telehealth had been very slow, but the presence of a pandemic has seen a surged in its use to the frontline of care. Telehealth is bridging the gap between people, providers, and healthcare systems during a pandemic, enabling people to communicate with providers through virtual channels while staying at home Siwicki (2020). There are four types of telehealth platforms that are currently available - live video-conferencing (synchronous), asynchronous meetings, remote patient monitoring, and mobile health monitoring (CDC, 2020; Rossow, 2018). Telehealth has three distinct roles during the COVID-19 pandemic (Siwicki, 2020). First is to triage or screen patients remotely, so that clinically stable patients stay home, decreasing transmission and contraction rates. The second role is to provide continuous routine care for patients with chronic disease and those at high-risk to decrease potential exposure to the virus. The last identified role is for healthcare providers to provide uninterrupted care to their patients remotely in the event that the healthcare provider themselves contract the virus Siwicki (2020).
Another finding in this review is that healthcare providers also reported high satisfaction with the use of telehealth. The healthcare providers evaluated in the five studies were subspecialists. This result is inconsistent with finding prior to COVID-19 that showed subspecialists were the least users of telemedicine (American College of Physicians [ACP], 2020). The ACP survey found that hospitalists (52%) and internist (45%) were more likely to use e-consult than the subspecialists (30%). The increase use in telehealth among subspecialists during a pandemic is again not surprising as patients who require specialty care are expected to still receive treatments. However, it is imperative to note that it may not always be possible for subspecialists to treat patients using telehealth. Referrals to subspecialists oftentimes require face-to-face encounters for accurate diagnosis and treatment. Most of the encounters in the included studies were follow-up and post-op follow-up visits hence there was an established relationship between the patient and healthcare providers, making the use of telehealth more feasible.
This integrative review has significant implications to nursing practice, research and policy. The use of telehealth or telemedicine is here to stay. The profession of nursing will continue to be impacted by telehealth. Nurses, including advanced practice nurses, are at the frontline in patient care, hence, must become familiar with the various technological advances. They should be open and willing to adjust their own practice based on the ever-changing technology and patient need. From an educational perspective, current nurses may need to be trained or re-trained to the various telehealth platforms. Additionally, it is imperative for nurses to continue to partake in research and evidence-based projects to increase nursing knowledge. Nurse should also participate in developing guidelines for best practice in telehealth nursing. Lastly, results from this integrative review may have implication in the future of health care. Findings provided additional support for the use of telehealth in the ambulatory care settings. More importantly, satisfaction among providers in subspecialty areas were also noted in this review. This could lead to integrating more telehealth into some components of clinic visits by both the patient and health care providers. From institutional perspectives, health care systems should continue to restructure their current systems to include telehealth. Thus, the future of telehealth in health care is promising.
This review acknowledges several limitations. A major limitation is that all the studies have level of evidence VI. Several of the articles were published pre-proof by the journals. The duration of each study was very short. Surveys used to measure satisfaction were mostly researcher developed. The validity and reliability of instruments were not addressed. Potential for election bias is high since most of the participants who were surveyed had no choice but to choose telehealth because of the pandemic. Participants who may have chosen to use telehealth may be more familiar with technology and that studies only evaluated patients from their health system. The recommendation is to repeat the study after the pandemic with a larger sample size from multiple settings or comparing multiple setting and samples using more rigorous study design.
6. Conclusion
This integrative review presented additional support on satisfaction with the use of telehealth. The findings in this review may not be surprising as individuals, healthcare providers, and health systems had to transform their way receiving and delivering health care out of necessity. It showed the adaptability of healthcare systems and providers in developing an alternative way of delivering care to patients during a crisis as well as resilience of individuals in quickly adapting to the new system.
COVID-19 has changed our way of living as well as how we manage our health. As the number of cases of COVID-19 continues to rise, people with acute and chronic conditions need to be cared for in the safest manner possible. Telehealth will continue to evolve regardless of the presence of a pandemic and the future of telehealth in delivering care is promising.
Funding source
No funding received for this paper.
Declaration Competing Interest
None.
References
- Ambrossini F., Di Stacio A., Mantica G., Cavallone B., Searao A. COVID-19 pandemic and uro-oncology follow-up: a “virtual” multidisciplinary team strategy and patients’ satisfaction assessment. Archivio Italiano di Urologia e Andrologia. 2020;92(2):78–79. doi: 10.4081/aiua.2020.2.78. [DOI] [PubMed] [Google Scholar]
- American College of Physicians [ACP] (2020). 2020 ACP member survey about telehealth implementation. https://www.acponline.org/system/files/documents/practice-resources/health-information-technology/telehealth/acp-telehealth-survey-results-2020-march.pdf
- Annis T., Pleasants S., Hultman G., Lindemann B., Thompson J., Billecke S., Badlani S., Melton G. Rapid implementation of a COVID-19 remote patient monitoring program. J. Am. Med. Inform. Assoc. 2020;0(0):1–5. doi: 10.1093/jamia/ocaa097. https://doi:10.1093/jamia/ocaa097 ocaa097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC]. (2020, July 16). Cases in the US. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- Cranford L. Chiron; 2020, May 1. Telemedicine Vs telehealth: What's the Difference.https://chironhealth.com/blog/telemedicine-vs-telehealth-whats-the-difference/ [Google Scholar]
- Dobrussin A., Hawa F., Gladshteyn M., Corsello M., Harlen K., Walsh C., Alparthi L., Weinstein M., Baig N., Sousa A., Gunaratnam N.T. Gastroenterologists and patients report high satisfaction rates with telehealth services during the novel coronavirus 2019 (COVID-19) pandemic. Clin. Gastroenterol. Hepatol. 2020:1–17. doi: 10.1016/j.cgh.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donabedian A. Evaluating the quality of medical care. Milbank Q. 2005;83(4):691–729. doi: 10.1111/j.1468-0009.2005.00397.x. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2690293/pdf/milq0083-0397.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fieux M., Duret S., Bawazeer N., Denoix L., Zaouche S., Tringali S. Telemedicine for ENT: effects of quality of care during COVID-19 pandemic. Eur Ann Otorhinolaryngol Head Neck Dis. 2020:1–5. doi: 10.1016/j.anorl.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert A., Billany J., Adam R., Martin L., Tobin R., Bagdai S., Galvin N., Farr I., Allain A., Davies L., Bateson J. Rapid implementation of virtual clinics due to COVID-19: report and early evaluation of a quality improvement initiative. BMJ Open Quality. 2020;9(2) doi: 10.1136/bmjoq-2020-000985. https://doi:10.1136/bmjoq-2020-000985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holcomb D., Faucher M.A., Bouzid J., Quint-Bouzid M., Nelson D.B., Duryea E. Patient perspectives on audio-only virtual prenatal visits amidst the severe acute respiratory syndrome coronavirus 2 (SARS –CoV-2) pandemic. Obstet Gynecol. 2020;136(2):317–322. doi: 10.1097/AOG.0000000000004026. [DOI] [PubMed] [Google Scholar]
- Holtz B.E. Patients perceptions on telemedicine visits before and after the coronavirus disease 2019 pandemic. Telemed. eHealth. 2020 doi: 10.1089/tmj.2020.0168. [Ahead of print] [DOI] [PubMed] [Google Scholar]
- Itamura K., Rimmel K.L., Illing E.A., Higgins T.S., Ting J.Y., Lee M.K., Wu A.W. Assessment of patient experiences in otolaryngology virtual visits during the COVID-19 pandemic. OPO Open. 2020;4(2) doi: 10.1177/2473974X20933573. 2473974X20933573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John Hopkins University & Medicine . Coronavirus Research Center, John Hopkins University & Medicine; 2020. COVID-19 Dashboard by the Center for Systems Science and Engineering at Johns Hopkins University.https://coronavirus.jhu.edu/map.html [Google Scholar]
- Kanc K., Komel J., Khos M., Wagner J. H(ome)bA1c testing and telemedicine: high satisfaction of people with diabetes for diabetes management during COVID-19 lockdown. Diabetes Res. Clin. Pract. 2020:1–3. doi: 10.1016/j.diabres.2020.108285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruse C.S., Krowski N., Rodriguez B., Tran L., Vela J., Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8) doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layfield E., Triantafillou V., Prasad A., Newman J., Rajasekaran K. Telemedicine for head and neck ambulatory visits during COVID-19: evaluating usability and patient satisfaction. Head Neck. 2020;42(7):1681–1689. doi: 10.1002/hed.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H.-.L., Chen Y.C., Huang J.-.X., Cheng S.W. Pilot study using telemedicine video consultation for vascular patients’ care during the COVID-19 period. Ann Vasc Surg. 2020:1–7. doi: 10.1016/j.avsg.2020.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Gu J., Shao F., Liang X., Yue L., Cheng Q., Zhang Z. Application and preliminary outcomes of remote diagnosis and treatment during COVID-19 outbreak: retrospective cohort study. JMIR Mhealth Uhealth. 2020;8(7):e19417. doi: 10.2196/19417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann D.M., Chen J., Chunara R., Testa P.A., Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J. Am. Med. Inform. Ass. 2020;27(7):1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo Clinic (n.d.). Telehealth: Technology meets health care. https://www.mayoclinic.org/healthy-lifestyle/consumerhealth/in-depth/telehealth/art-20044878.
- Melnyk B., Fineout-Overholt E. 3rd ed. Wolters Kluwer; 2015. Evidence-based Practice in Nursing & healthcare: A guide to Best Practice. [Google Scholar]
- Moore S.L., Santodomingo M., Elsberrnd K., McHale M., Massone J. Using telehealth for hospice reauthorization visits: results of a quality improvement analysis. J Pain Symptom Manage. 2020 doi: 10.1016/j.jpainsymman.2020.06.002. https://www.jpsmjournal.com/article/S0885-3924(20)30434-6/pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustafa S.S., Yang L., Mortezavi M., Vadamalai K., Ramsey A. Patient satisfaction with telemedicine encounters in an allergy and immunology practice during coronavirus disease 2019 pandemic. Ann. Allergy, Asthma Immunol. 2020:1–2. doi: 10.1016/j.anai.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orlando J.F., Beard M., Kumar S. Systematic review of patients and caregivers'satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients' health. PLOS One. 2019;14(8) doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peden C.J., Mohan S., Pagán V. Telemedicine and COVID-19: an observational study of rapid scale up in a US academic medical system. J Gen Intern Med. 2020:1–3. doi: 10.1007/s11606-020-05917-9. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polinski J.M., Barker T., Gagliano N., Sussman A., Brennan T.A., Shrank M. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med. 2016;31(3):269–275. doi: 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rametta S.C., Fridinger S.E., Gonzales A.K., Xian J., Galer P.D., Kaufman M., Prelack M.S., Shariff U., Fitxgerald M.P., Melamed S.E., Malcolm M.P., Kessler S.K., Stephenson D.J., Banwell B.L., Abend N.S., Helbig I. Analyzing 2,589 child neurology telehealth encounters necessitated by the COVID-19 pandemic. Neurology. 2020 doi: 10.1212/WNL.0000000000010010. https://n.neurology.org/content/early/2020/06/09/WNL.0000000000010010 Published ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossow R. iSalus; 2018, August 15. The Different Types of Telehealth.https://isalushealthcare.com/blog/the-different-types-of-telehealth/ [Google Scholar]
- Shenoy P., Ahmed S., Paul A., Skaria T.G., Joby J., Alias B. Switching to teleconsultation for rheumatology in the wake of the COVID-19 pandemic: feasibility and patient response in India. Clin. Rheumatol. 2020:1–6. doi: 10.1007/s10067-020-05200-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siwicki B. Healthcare IT News; 2020, March 19. Telemedicine During COVID-19: Benefits, limitations, burdens, Adaptation.https://www.healthcareitnews.com/news/telemedicine-during-covid-19-benefits-limitations-burdens-adaptation [Google Scholar]
- Smrke A., Younger E., Wilson R., Husson O., Farag S., Merry E., Macklin-Doherty A., Cojocaru E., Arthur A., Benson C., Miah A.B., Zaidi S., Gannata S., Jones R.L. Telemedicine during COVID-19 pandemic: impact on care for rare cancers. JCO Global Oncology. 2020;6 doi: 10.1200/GO.20.00220. 10-46-1051https://doi.org/10. 1200/GO.20.00220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svider P., Setzen M., Ow R., Folbe A.J., Eloy J.A., Johnson A.P. Incorporation of telemedicine by rhinologists: the COVID-19 pandemic and beyond. Am. J. Otolaryngol.-Head and Neck Med. Surg. 2020:1–18. doi: 10.1016/j.amjoto.2020.102567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenforde A.S., Iaccarino M.A., Borgstrom H., Hefner J.E., Silver J., Ahmed M., Babu A.N., Blauwet C.A., Elson L., Eng C., Kotler D., Homer S., Makovitch S., McInnis C., Vora A., Borg-Stein J. Telemedicine during COVID-19 for outpatient sports and musculoskeletal medicine physicians. PM&R. 2020 doi: 10.1002/pmrj.12422. https://doi:10.1002/pmrj.12422 [DOI] [PMC free article] [PubMed] [Google Scholar]