Abstract
Background: Conventional colonoscopy (CC) allows access for colonic investigation and intervention; in the small group in whom CC is unsuccessful alternative imaging is often sufficient. There remains a subset, however, requiring full colonic visualisation or intervention. Balloon-assisted colonoscopy (BAC) gives a further option when access is difficult. Aims: This study aims to present the experience with BAC of two European tertiary referral centres. Methods: Procedures were carried out under local protocol over 15-years (2006–2020). Markers of procedural quality such as caecal intubation, complications and comfort were retrospectively compiled and analysed. Published evidence was summarised for comparison. Results: 122 procedures were undertaken, with polyps the most frequent indication and 90.2% having at least one previously incomplete CC. Features associated with difficult colonoscopy were common, including intraabdominal surgery (32.0%). 92.6% reached the caecum; completion was higher (96.3%) in those failing CC due to discomfort and lower in those failing due to anatomical difficulties (90.7%) or previous surgery (84.6%). Mean time to the caecum was 20.9 minutes and mean midazolam and fentanyl doses were 2.6 mg and 49.9 µg with low discomfort scores. Conclusion(s): Balloon-assisted colonoscopy is successful in >90% of patients, is well-tolerated, and is safe.
Keywords: balloon-assisted endoscopy, colonoscopy, caecal intubation, intervention
1. Introduction
The flexible endoscope has been in evolution since the 1950s and today is established as the principal mode for investigation and intervention of the colonic and terminal ileal mucosa [1,2]. Despite ongoing development in colonoscope design and improvements in endoscopic technique(s), there remains a subset of patients in whom complete colonoscopy proves challenging. A prerequisite for independent colonoscopy practice across the globe is that an endoscopist’s caecal intubation rate should be at least 90% [3,4]. In expert hands, the expectation would be that the number of incomplete procedures is reduced to a very small subset of difficult cases [5]. To complete the examination of the ileocolonic area, when therapy is not required, either computed tomography colonoscopy (CTC) or colon capsule endoscopy (CCE) is often adequate [6,7].
Nevertheless, there will always be a small group of patients with challenging colons in whom complete colonoscopy is necessary for visualisation or therapy. In this subgroup, balloon-assisted colonoscopy (BAC) is an option. This technique allows the colon to be gripped by inflatable balloons and the colon shortened for ease of navigation and tip control stability, Figure 1. The technique follows the principles of double-balloon enteroscopy (DBE), which was developed to allow deep exploration of the small bowel by Yamamoto et al. [8], with simplification to a single-balloon (SBE) system following [9]. The utility of these systems for completion of long and difficult colonoscopies was quickly realised [10] with a couple of studies [11,12] also presenting a comprehensive review of the literature, which shows BAC to be safe and effective. In these centres, the first line of investigation following failed colonoscopy is CT colonography (CTC) and CCE. When it is felt likely that therapy is likely to be required however BAC becomes the preferred option.
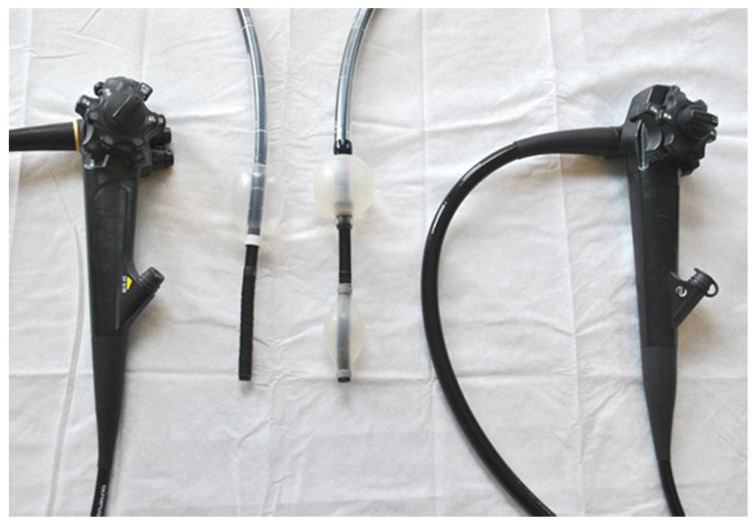
Figure 1.
A single balloon endoscope (left) and double balloon endoscope (right).
This manuscript aims to present the practice of using BAC in two European tertiary referral centres when conventional colonoscopy has either been incomplete, or unable to provide a stable platform for therapy, and present a summary of the evidence available internationally to support our findings.
2. Materials and Methods
Balloon-assisted colonoscopies performed in Edinburgh (Scotland) and Malmö (Sweden) between March 2006 and March 2020 were retrospectively reviewed. Procedures during this time were carried out as per departmental protocol(s). Double-balloon procedures were performed with Fujinon (Tokyo, Japan) endoscopes EC450-B15, EC450-LP5, EN450-T5, EC530-A131, EN580-T, EC600WL and single-balloon procedures with Olympus Optical Co. (Tokyo, Japan) endoscope SIF-Q180. Data regarding procedure details and outcomes were retrieved from endoscopy reporting systems on patients undergoing BAC. Patient records were retrospectively reviewed for demographics, medical history, indication(s) for colonoscopy, reason for failed conventional colonoscopy, indication for BAC, the type of endoscope, caecal intubation, findings, intervention(s) performed, sedation used, complications, and finally patient comfort during the procedure. These data were anonymised and securely stored for analysis.
2.1. Statistics
Data were collated, analysed and graphed through Microsoft Excel (Microsoft Corporation, WA, USA). Results are descriptive with values expressed as mean (±SD) or median (range). Student’s t-test was used to compare means with the level of statistical significance p < 0.05.
2.2. Ethics
This study used routinely collated data and conducted as a service evaluation. Anonymised data were stored securely, with methodology in compliance with the Declaration of Helsinki.
3. Results
3.1. Cohort Demographics
A total of 122 procedures (66 in female patients) between March 2006 and March 2020 were included and reviewed. Of those, 110 used a double-balloon endoscope (DBC), with 12 using single-balloon (SBC). All SBCs were performed at Skane University Hospital in Malmö. All procedures were performed by senior endoscopists, this included five individuals in Malmö and three in Edinburgh. The endoscopists were all certified as independent in colonoscopy with life experience of >1000 procedures. The median age of patients at the time of procedure was 66.5 (20–89) years. Indications for the procedures are listed in Table 1.
Table 1.
Indications for balloon-assisted colonoscopy.
| Indication | Cases (% of total) |
|---|---|
| Polyp(s) | 53 (43.4) |
| IBD Surveillance | 18 (14.8) |
| Iron Deficiency Anaemia | 16 (13.1) |
| OGIB/PR Bleeding | 14 (11.5) |
| Suspected Cancer | 7 (5.7) |
| Abnormal Imaging | 6 (4.9) |
| Abdominal Pain | 3 (2.5) |
| Control of Post-Operative Bleeding | 2 (1.6) |
| Diarrhoea | 2 (1.6) |
| Treatment of Angioectasia(s) | 1 (0.8) |
IBD, Inflammatory bowel disease; OGIB, obscure/occult GI bleeding; PR, per rectum.
3.2. Previous Abdominal Surgery and Other Comorbidities
Of the patients, 32.0% (39/122) had had previous abdominal surgery; these are listed in Table 2. Furthermore, the presence of significant medical comorbidity was common, Table 2.
Table 2.
Previous abdominal surgery and comorbidities in patients undergoing balloon-assisted colonoscopy.
| Previous Abdominal Surgery | Number (%) | Comorbidities | Number (%) |
|---|---|---|---|
| Hysterectomy (±BSO) | 13 (10.7) | Hypertension | 32 (26.2) |
| Gastric Surgery | 5 (4.1) | Respiratory | 28 (23.0) |
| Pelvic Floor Repair | 4 (3.3) | Cardiac | 27 (22.1) |
| Right Hemicolectomy | 4 (3.3) | Diabetes | 25 (20.5) |
| Renal/Adrenal | 3 (2.5) | Rheumatology | 21 (17.2) |
| Perforation | 3 (2.5) | Functional | 13 (10.7) |
| Appendicectomy | 2 (1.6) | Endocrine | 12 (9.8) |
| Meckel’s Diverticulectomy | 2 (1.6) | IBD | 12 (9.8) |
| Cystectomy | 2 (1.6) | Psychiatric | 11 (9.0) |
| Sigmoid Resection | 2 (1.6) | Neurological | 11 (9.0) |
| Splenectomy | 1 (0.8) | Other Malignancy | 10 (8.2) |
| Caesarean Section | 1 (0.8) | Obesity | 10 (8.2) |
| Prostatectomy | 1 (0.8) | Hepato-Pancreatic | 9 (7.4) |
| No Documented Surgery | 83 (68.0) | Renal | 8 (6.6) |
| Vascular | 6 (4.9) | ||
| No Major Comorbidity Listed | 22 (18.0) |
BSO, Bilateral salpingo-oophorectomy; IBD, inflammatory bowel disease.
3.3. Reason for Failure of Conventional Colonoscopy
Incomplete conventional colonoscopy prior to BAC was recorded in 90.2% (110/122). In 12 (9.8%) cases, although the caecum was reached, polypectomy was not possible due to unstable position, thus requiring the procedure to be repeated. Overall, 63.1% (77/122) had only one previous incomplete procedure, 15.6% (19/122) had two, and 11.5% (14/122) had more than two incomplete procedures prior to BAC. In individuals with previous failed procedures (n = 110) the reasons included anatomical (long/looping or redundant/capacious colon n = 63, diverticula n = 2, fixed/angulated area n = 10), patient discomfort (n = 27), unclear (n = 6) or small-bowel pathology (n = 2).
3.4. Success Rate of BAC and Reasons for BAC Failure
BAC had a caecal intubation rate of 92.6%. Nine BACs were incomplete due to poor bowel preparation, significant pathology encountered or anatomy. In total, 8.3% (1/12) of the SBC and 7.3% (8/110) of the DBC procedures were failed. None were due to complications or severe discomfort to the patient. Six of the failed BACs were in patients with previous abdominal surgery. As such, the caecal intubation rate of BAC in those with previous abdominal surgery was lower at 84.6% (33/39). The operations and comorbidities of those having failed BAC were varied. For patients who had an incomplete initial colonoscopy due to discomfort caecal intubation with BAC was achieved in 96.3% (26/27). Caecal intubation was 90.7% (68/75) in those failing initial colonoscopy because of angulation, diverticula or long colon (six BAC failures had been in those labelled initially as long capacious colon and one angulation). Characteristics of those with incomplete BAC (n = 9) are shown in Table 3.
Table 3.
Characteristics of those failing BAC.
| Characteristic | Number (%) |
|---|---|
| Age | Median 66.0 (44–86) years |
| Female | 4 (44.4) |
| Midazolam | Mean 3.4 (±1.5) mg Excluding One Having GA |
| Fentanyl | Mean 39.3 (±37.8) ug Excluding One Having GA |
| Unable to Proceed Due to Preparation | 2 (22.2) |
| Obstructing Tumour | 1 (11.1) |
| Previous Surgery | 6 (66.7) |
| Reason for Failed Colonoscopy | Long/Looping/Redundant Colon (7); Discomfort (1- Note Repeated With GA); Fixed Sigmoid (1) |
| Indication | PR Bleeding (2), Polyps (2), Abdominal Pain (2), IBD (1), Post Op Bleeding (1), Diarrhoea (1) |
BAC, balloon-assisted colonoscopy; GA, general anaesthesia; PR, per rectum; IBD, inflammatory bowel disease.
3.5. Findings and Therapies Given
The largest group requiring BAC were for investigation and treatment of polyps or to improve stability to safely enable polypectomy and this was the most common finding in this cohort (n = 67). In this group, 89.6% (60/67) had polypectomy ± argon plasma coagulation (APC), tattoo or clips during BAC procedure. Other primary findings are shown in Table 4.
Table 4.
Common, non-polyp findings. APC, argon plasma coagulation.
| Primary Finding of BAC | Procedures (n =) | Therapy Required |
|---|---|---|
| Colitis/Ileitis | 13 | Biopsies Only |
| Diverticulosis | 11 | Polypectomy for Incidental Polyps (n = 5) |
| Angioectasia | 5 | APC (n = 3), Clip and APC (n = 1) and Polypectomy (n = 1) |
| Tumour | 4 | Biopsies Only |
| Normal | 29 | n/a |
3.6. Time to Caecum, Comfort and Complications
The time taken to reach the caecum was recorded in 31 procedures with a mean of 20.9 (±13.5) and median of 19 (4–60) minutes. Five individuals required propofol or general anaesthetic (GA) for their BAC procedure (117 had conscious sedation ± analgesia or neither). Those having conscious sedation with midazolam (n = 96) had a mean dose of 2.6 mg (±1.9 mg). A total of 77 patients had received fentanyl for their procedure at mean dose of 49.9 µg (±45.0 µg). There was no significant difference between the dose of midazolam given between those having SBC or DBC (p = 0.34), although none of the SBC patients had fentanyl.
Discomfort scores were subjectively reported by the endoscopist and recorded for 82 procedures. No discomfort reported in 36.6% (30/82), mild in 47.6% (39/82), moderate in 14.6% (12/82), significant in 1.2% (1/82) and none for severe. The only complication reported was a vasovagal attack during polypectomy.
4. Discussion
Even the best endoscopists will inevitably encounter a colon which they cannot fully traverse with conventional colonoscopy, irrespective of the tips and tricks of the trade [5]. In such cases, there are several options available, and the decision should be tailored to the individual patient. In procedures with diagnostic intention less invasive complimentary imaging techniques such as CTC and/or CCE can be considered [6]. For those who require intervention, however, an invasive procedure is still required.
We present herein the experience of using BAC, in two European tertiary referral centres, to address this issue, which represents the largest single study published so far. The most frequent indication (43%) in this cohort was providing access and stable instrument tip position for accurate polyp assessment and safe polypectomy in difficult colons. Previous studies have frequently sited polypectomy as the most common indication for DBC, see Table 5. In this study, most patients successfully underwent polypectomy of often large or difficult lesions. The reasons for no polypectomy taking place included the polyp being isolated and unresectable or post inflammatory. Others had colitis or incomplete procedure (due to obstructing pathology, poor prep) or no polyp being found. In this cohort several patients had caecal intubation on initial colonoscopy. Although the caecum had been reached, these procedures were still not adequate to provide the required intervention and so repeat with BAC allowed a safer, more stable position from which polypectomy could be achieved. This in our opinion is a strength and strong indication for BAC. An informative tabulated summary of published evidence on the use BAC is also presented, Table 5.
Table 5.
Summary of available literature. DY, diagnostic yield; n/s, not specified.
| Authors, Year | Country | Type of Study | No. Of Patients (M/F) | Age: Mean ±SD Or Median (Range in Years) |
Type of Endoscope | Caecal Intubation Rate, n (%) |
Time to Caecum: Mean ±SD Or Median (Range in Min) |
DY Of BAC (n) | Interventions Performed (n) | Adverse Events, (n) |
|---|---|---|---|---|---|---|---|---|---|---|
| May et al., 2006 [13] | Germany | Prospective, Single Centre |
14 (6/8) | 62 ± 15 | Single Balloon | 14/14 (100) | n/s | Polyps (6) IBD (3) Cancer (2) |
Polypectomy (6) Biopsy (5) |
Polypectomy Bleeding (1) |
| Kaltenbach et al., 2006 [14] | USA | Prospective, Single Centre |
20 (16/4) |
66 ± 12 | Single Balloon | 19/20 (95) | 28 ± 20 | Significant (7) (Polyps (5) Ibd (2)) |
Polypectomy (5) Biopsy (1) |
None |
| Das 2007 [15] | USA |
n/s, Single Centre |
16 (n/s) | n/s | Double Balloon | 14/16 (87.5) | 27 ± 9.5 | n/s | Polypectomy (6) Haemostasis (1) |
None |
| Gay & Delvaux, 2007 [16] | France | Retrospective, Single Centre |
29 (5/24) | 54±17 | Double Balloon | 28/29 (96.6) | 18 ± 14 | Diverticulosis (7) Polyps (4) IBD (2) |
Biopsy (8) APC (2) Polypectomy (2) |
None |
| Moönkemuüller et al., 2007 [17] | Germany |
n/s, Single Centre |
7 (3/4) | 64(50–75) | Double Balloon | 7/7 (100) |
15 (9–25) | Diverticulosis (2) Polyps (2) Stenosis (2) |
n/s | n/s |
| Pasha et al., 2007 [18] | USA | Retrospective, Single Centre |
16 (5/11) | 69 ± 12 | Double Balloon | 14/16 (87.5) | 27 ± 9.5 | n/S | Polypectomy (6) APC (1) |
n/s |
| Moreels & Pelckmans, 2008 [19] | Belgium | Retrospective, Single Centre |
26 (n/s) | n/s | Double Balloon | 23/26 (89) | n/s | n/S | n/s | n/s |
| Moreels et al. 2010 [20] | Belgium | Prospective, Single Centre |
45 (28/17) | 63 ± 2 | Double Balloon | 42/45 (93.3) | n/s | Polyps (18) | Polypectomy (18) APC (3), Biopsy (2) |
None |
| Teshima et al., 2010 [10] | Netherlands | Prospective, Single Centre |
23 (14/8) | 53(19–75) | Single Balloon | 22/23 (96) | 30 (20–60) | Polyps (6) IBD (5) Diverticulosis (2) |
Polypectomy (6) Dilation (1) |
None |
| Matsushita et al., 2011 [21] | Japan | Retrospective, Single Centre |
24 (n/s) | n/s | Double Balloon | 24/24 (100) | 17 | n/S | 17 Interventions (n/s) | n/s |
| Keswani et al., 2011 [22] | USA | Prospective, Single Centre |
14 (4/10) | 58.5 ± 12.5 (35–74) | Single Balloon | 13/14 (92.9) | 22 ± 18 (10–81) | Polyps (7) | n/s | None |
| Dzeletovic et al., 2012 [23] | USA | Retrospective, Single Centre |
53 (12/41) | 71(43–83) | Single Balloon& Double Balloon | 51/53 (96) (26/26 SBC, 25/27 DBC) | 19 (7–58) | Polyps (32) Diverticulosis (21) |
Polypectomy (37) | None |
| Goómez et al., 2012 [24] | USA | Retrospective, Single Centre |
45 (21/24) | 67(21–84) | Double Balloon | 46/51 (90) | n/s | Polyps (28) Angiectasia (5) |
Polypectomy (28) | None |
| Hotta et al., 2012 [25] | Japan | Prospective, Multicentre |
110 (62/48) | 66.5(27–79) | Double Balloon | 110/110 (100) | 12 (4–47) | Polyps (55) Cancer (5) |
Polypectomy (45) Biopsy (8) |
Mild Mucosal Injury (1) |
| Suzuki et al., 2012 [26] | Japan | Prospective, Single Centre |
47 (22/25) | 63.4 ± 10.9 | Double Balloon | 47/47 (100) | 13.0 ± 5.3 | Polyps (21) C ancer (1) |
Polypectomy/Resection (6) Further Surgery (1) |
None |
| Kobayashi et al., 2013 [27] | Japan | n/sSingle Centre | 15 (8/7) | 65.7 ± 8.7 (38–81) | Single Balloon | 15/15 (100) | 22.9 ± 8.9 (9–40) | Polyps Radiation Colitis (3) Diverticulosis (3) |
Polypectomy (N/S) Biopsy (N/S) |
None |
| Yamada et al., 2013 [28] | Japan | Prospective, Single Centre |
21 (n/s) | 71.5 ± 7.8 | Single Balloon& Double Balloon | 20/21 (95) | 12.8 (9.5–42) | Polyps (8) Diverticulosis (7) Cancer (1) |
Polypectomy (8) Biopsy (1) |
None |
| Becx & Al-Toma, 2014 [29] | Netherlands | Retrospective, Single Centre |
114 (45/69) | 64.8(31–91) | Double Balloon | 101/114 (88.6) | n/s | New Diagnoses (55) | Polypectomy (51) Further Surgery (7) |
Bleeding with Spontaneous Resolution (2) |
| Nemoto et al., 2014 [30] | Japan | Prospective, Single Centre |
28 (14/14) | 74(35–88) | Double Balloon | 28/28 (100) | 16 (6–66) | n/S | n/s | None |
| Yung et al., 2016 [11] | UK | Retrospective, Single Centre |
57 (26/31) | 62.9(20–89) | Double Balloon | 55/57 (96.5) | n/s | 29 | Polypectomy/APC (22) | None |
| Sulz et al., 2016 [31] | Switzerland | Retrospective, Single Centre |
100 (46/54) | 70(38–87) | Single Balloon | 98/100 (98) | 27.5 (4–92) | Diverticulosis (54) Polyps (47), Colitis (4) Cancer (1) |
Polypectomy (45) APC (1) |
Mucosal Defect After Polypectomy (1) Haematochezia (1) |
| Despott et al., 2017 [32] | UK | Prospective, Single Centre |
22 (7/15) | 68 ± 10 | Double Balloon | 22/22 (100) | 17.5 (16.0–23.7) | n/S | n/s | n/s |
| Hermans et al., 2018 [33] | Netherlands | Retrospective, Single Centre |
61 (34/27) | 65(29–82) | Double Balloon | 60/63 (95) | n/s | Polyps (34) Cancer (3) |
Polypectomy (34) Biopsy (3) |
Bleeding at Polypectomy (1) |
| Robertson et al., 2020 | UK/Sweden | Retrospective, Multicentre |
122 (56/66) | 64.4 ± 12.3 | Single Balloon& Double Balloon | 113/122 (92.6) | 20.9 ± 13.5 | Polyps (67) , Cancer (4) Colitis (13), Diverticulosis (11) Angiectasia (5) |
Polypectomy (60) APC (4) Biopsy |
Vasovagal Reaction During Polypectomy (1) |
The relatively low number of procedures (122 procedures between 2006 and 2020) indicates that BAC is reserved for a small percentage of patients. In our centres, BAC is primarily reserved for those who are likely to require therapy, as CT colonography and CCE provide adequate diagnostic information in most. Despite this, there were 29 patients who did not have pathology seen on their BAC. When an invasive procedure is required, other options such as axis-shortening techniques including underwater/water immersion colonoscopy for longer, looping colons, or deep sedation (propofol)/general anaesthesia for anxiety or tenderness are more frequently employed. Over the course of a long study period, there were relatively few patients requiring BAC, but this included assessment of IBD or abnormal imaging, who were deemed likely to require biopsies or requiring haemostatic treatment, which was most frequently APC. In our study, there was no difference in the completion rate of DBC and SBC, which is in accordance to the previous publications, showing that the outcomes are similar using double and single-balloon colonoscopy in patients with previously failed or difficult colonoscopy. [10,11]. This suggesting that the choice of instrument would depend on local availability or expertise.
The patients seen were elderly and frequently female, with a high incidence of cardiorespiratory comorbidity. They were also frequently observed to have had previous abdominal surgery (in roughly a third). These being features associated with a more difficult colonoscopy and initial procedures were failed in most due to either long capacious colons or angulation. BAC in these patients had a completion rate of 90.7%, with failure of BAC most often associated with previous abdominal surgery. Tolerance was good following previous experience of discomfort during initial colonoscopy, with 70.6% (12/17 of those with recorded discomfort scores) undergoing conscious sedation with discomfort score of ‘mild’ or ‘no discomfort’. The caecal intubation rate was high, at 96.3% in those previously failing due to discomfort. Sedation practice during this time has also changed. Although none of the cases in Edinburgh used propofol or GA, it was introduced in Malmö in 2012. Five patients required propofol or GA for their procedure and these patients were spread over the course of the study period, both pre and post 2012. Many patients managed BAC without any analgesia or sedation and those given IV medication tolerated the procedure with a mean dose of midazolam of 2.6 mg and fentanyl of 49.9 mg.
There are several limitations of this study. It is retrospective in design and without a comparison group, making the significance of the percentages difficult to extrapolate. There is also a prolonged study period across two northern European centres, during which time, equipment and training have improved. Although the addition of propofol as an option in Malmö may have also reduced the failure of conventional colonoscopy, half of those requiring BAC following procedures failed due to discomfort were after 2012. The patients also varied, but as older, comorbid patients they are usually excluded from trials. As such, this study, which includes these complicated patients with failed and difficult colonoscopies who require intervention, has strengths. It represents a difficult real-world situation which is frequently encountered in clinical practice and shows that in the vast majority BAC provides a solution. A recent meta-analysis of balloon-assisted colonoscopy in patients with difficult or incomplete procedures included 667 patients across 18 studies [12]. This paper represents the largest study of which we are aware at the time of writing and we would agree with the meta-analysis’ conclusion that major centres should have balloon assisted colonoscopy available as a rescue technique.
In patients requiring a complete diagnostic or therapeutic procedure balloon-assisted colonoscopy can provide an option after failure of conventional colonoscopy. Based on our results and review of the literature, it is successful in >90% of even very difficult cases, and it is safe and well tolerated in a predominantly elderly and comorbid population. When a complete procedure is required in difficult colons for therapy, BAC is an option to consider.
Author Contributions
Conceptualization, T.E., K.A. and W.J.G..; methodology, R.A.R.; data collection, W.J.G.; N.A.; Y.D.E., and R.A.R; validation, T.E., W.J.G. and R.A.R; formal analysis, all coauthors..; investigation, T.K., P.J.N., F.C., R.A.R., T.E., N.A. and W.J.G.; data curation, W.J.G., Y.D.E., and R.A.R.; writing—original draft preparation, R.A.R. and W.J.G.; writing—review and editing, all coauthors; visualization, R.A.R.; supervision, T.E., K.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
A.K. has received travel support from Aquilant Endoscopy, the rest of the coauthors have not COI to declare.
References
- 1.Hirschowitz B.I., Curtiss L.E., Peters C.W., Pollard H. Demonstration of a new gastroscope, the fiberscope. Gastroenterology. 1958;35:50–53. doi: 10.1016/S0016-5085(19)35579-9. [DOI] [PubMed] [Google Scholar]
- 2.Overholt B.F. Colonoscopy: A Review. Gastroenterology. 1975;68:1308–1320. doi: 10.1016/S0016-5085(75)80250-2. [DOI] [PubMed] [Google Scholar]
- 3.Rees C.J., Gibson S.T., Rutter M.D., Baragwanath P., Pullan R., Feeney M., Haslam N. UK key performance indicators and quality assurance standards for colonoscopy. Gut. 2016;65:1923–1929. doi: 10.1136/gutjnl-2016-312044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaminski M., Thomas-Gibson S., Bugajski M., Bretthauer M., Rees C., Dekker E., Hoff G., Jover R., Suchanek S., Ferlitsch M., et al. Performance measures for lower gastrointestinal endoscopy: A European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2017;49:378–397. doi: 10.1055/s-0043-103411. [DOI] [PubMed] [Google Scholar]
- 5.Rex D.K. Response: Gastrointest. Endoscopy. 2016;84:882. doi: 10.1016/j.gie.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Spada C., Hassan C., Barbaro B., Iafrate F., Cesaro P., Petruzziello L., Grazioli L.M., Senore C., Brizi G., Costamagna I., et al. Colon capsule endoscopy vs. CT-colonography in the evaluation of patients with incomplete colonoscopy. J. Gastroenterol. Hepatol. 2013;28:31–32. [Google Scholar]
- 7.Toth E., Yung D.E., Nemeth A., Johansson G.W., Thorlacius H., Koulaouzidis A. Video capsule colonoscopy in routine clinical practice. Ann. Transl. Med. 2017;5:195. doi: 10.21037/atm.2017.03.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yamamoto H., Sekine Y., Sato Y., Higashizawa T., Miyata T., Iino S., Ido K., Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216–220. doi: 10.1067/mge.2001.112181. [DOI] [PubMed] [Google Scholar]
- 9.Tsujikawa T., Saitoh Y., Andoh A., Imaeda H., Hata K., Minematsu H., Senoh K., Hayafuji K., Ogawa A., Nakahara T., et al. Novel single-balloon enteroscopy for diagnosis and treatment of the small intestine: Preliminary experiences. Endoscopy. 2008;40:11–15. doi: 10.1055/s-2007-966976. [DOI] [PubMed] [Google Scholar]
- 10.Teshima C., Aktas H., Haringsma J., Kuipers E.J., Mensink P.B.F. Single-balloon-assisted colonoscopy in patients with previously failed colonoscopy. Gastrointest. Endosc. 2010;71:1319–1323. doi: 10.1016/j.gie.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Yung D.E., Koulaouzidis A., Fraser C., Trimble K.C., Plevris J.N. Double-balloon colonoscopy for failed conventional colonoscopy: The Edinburgh experience and systematic review of existing data. Gastrointest. Endosc. 2016;84:878–881. doi: 10.1016/j.gie.2016.06.024. [DOI] [PubMed] [Google Scholar]
- 12.Tan M., Lahiff C., Bassett P., Bailey A., East J.E. Efficacy of balloon overtube-assisted colonoscopy in patients with incomplete or previous difficult colonoscopies: A meta-analysis. Clin. Gastroenterol. Hepatol. 2017;15:1628–1630. doi: 10.1016/j.cgh.2017.04.023. [DOI] [PubMed] [Google Scholar]
- 13.May A., Nachbar I., Ell C. Push-and-pull enteroscopy using a single-ballon technique for difficult colonoscopy. Endoscopy. 2006;38:395–398. doi: 10.1055/s-2006-925063. [DOI] [PubMed] [Google Scholar]
- 14.Kaltenbach T., Soetikno R., Friedland S. Use of a double balloon enteroscope facilitates caecal intubation after incomplete colonoscopy with a standard colonoscope. Dig Liver Dis. 2006;38:921–925. doi: 10.1016/j.dld.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Das A. Future perspective of double balloon endoscopy: Newer indications. Gastrointest. Endosc. 2007;66:S51–S53. doi: 10.1016/j.gie.2007.02.066. [DOI] [PubMed] [Google Scholar]
- 16.Gay G., Delvaux M. Double-balloon colonoscopy after failed conventional colonoscopy: A pilot series with a new instrument. Endoscopy. 2007;39:788–792. doi: 10.1055/s-2007-966753. [DOI] [PubMed] [Google Scholar]
- 17.Mönkemüller K., Knippig C., Rickes S., Fry L.C., Schulze A., Malfertheiner P. Usefulness of the double-balloon enteroscope in colonoscopies performed in patients with previously failed colonoscopy. Scand. J. Gastroenterol. 2007;42:277–278. doi: 10.1080/00365520600802785. [DOI] [PubMed] [Google Scholar]
- 18.Pasha S.F., Harrison M.E., Das A., Corrado C.M., Arnell K.N., Leighton J.A. Utility of double-balloon colonoscopy for completion of colon examination after incomplete colonoscopy with conventional colonoscope. Gastrointest. Endosc. 2007;65:848–853. doi: 10.1016/j.gie.2006.08.046. [DOI] [PubMed] [Google Scholar]
- 19.Moreels T.G., Pelckmans P.A. Double-balloon endoscope for failed conventional colonoscopy. Clin. Gastroenterol. Hepatol. 2008;6:259. doi: 10.1016/j.cgh.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 20.Moreels T.G., Macken E.J., Roth B., Van Outryve M.J., Pelckmans P.A. Cecal intubation rate with the double-balloon endoscope after incomplete conventional colonoscopy: A study in 45 patients. J. Gastroenterol. Hepatol. 2010;25:80–83. doi: 10.1111/j.1440-1746.2009.05942.x. [DOI] [PubMed] [Google Scholar]
- 21.Matsushita M., Shimatani M., Tanaka T., Fukata N., Kawamata S., Okazaki K. Short double-balloon enteroscope for previously failed colonoscopy. Gastrointest. Endosc. 2011;73:854–855. doi: 10.1016/j.gie.2010.09.045. [DOI] [PubMed] [Google Scholar]
- 22.Keswani R.N. Single-balloon colonoscopy versus repeat standard colonoscopy for previous incomplete colonoscopy: A randomized, controlled trial. Gastrointest. Endosc. 2011;73:507–512. doi: 10.1016/j.gie.2010.09.047. [DOI] [PubMed] [Google Scholar]
- 23.Dzeletovic I., Harrison M.E., Pasha S.F., Crowell M.D., Decker G.A., Gurudu S.R., Leighton J.A. Comparison of single- Versus double-balloon assisted-colonoscopy for colon examination after previous incomplete standard colonoscopy. Dig. Dis. Sci. 2012;57:2680–2686. doi: 10.1007/s10620-012-2227-z. [DOI] [PubMed] [Google Scholar]
- 24.Gómez V., Patel M.K., Stark M.E., Lukens F. Double-balloon enteroscopy in patients with previous incomplete colonoscopy: Should we perform them more often? J. Clin. Gastroenterol. 2012;46:887–888. doi: 10.1097/MCG.0b013e31825f2d05. [DOI] [PubMed] [Google Scholar]
- 25.Hotta K., Katsuki S., Ohata K., Abe T., Endo M., Shimatani M., Nagaya T., Kusaka T., Matsuda T., Uraoka T., et al. A multicenter, prospective trial of total colonoscopy using a short double-balloon endoscope in patients with previous incomplete colonoscopy. Gastrointest. Endosc. 2012;75:813–818. doi: 10.1016/j.gie.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 26.Suzuki T., Matsushima M., Tsukune Y., Fujisawa M., Yazaki T., Uchida T., Gocyo S., Okita I., Shirakura K., Sasao K., et al. Double-balloon endoscopy versus magnet-imaging enhanced colonoscopy for difficult colonoscopies, a randomized study. Endoscopy. 2012;44:38–42. doi: 10.1055/s-0030-1256875. [DOI] [PubMed] [Google Scholar]
- 27.Kobayashi K., Mukae M., Ogawa T., Yokoyama K., Sada M., Koizumi W. Clinical usefulness of single-balloon endoscopy in patients with previously incomplete colonoscopy. World J. Gastrointest. Endosc. 2013;5:117. doi: 10.4253/wjge.v5.i3.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yamada A., Watabe H., Takano N., Togo G., Yamaji Y., Yoshida H., Kawabe T., Omata M., Koike K. Utility of single and double balloon endoscopy in patients with difficult colonoscopy: A randomized controlled trial. World J. Gastroenterol. 2013;19:4732. doi: 10.3748/wjg.v19.i29.4732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Becx M.C., Al-Toma A. Double-balloon endoscopy: An effective rescue procedure after incomplete conventional colonoscopy. Eur. J. Gastroenterol. Hepatol. 2014;26:519–522. doi: 10.1097/MEG.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 30.Nemoto D., Isohata N., Utano K.-I., Hewett D.G., Togashi K. Double-balloon colonoscopy carried out by a trainee after incomplete conventional colonoscopy. Dig. Endosc. 2014;26:392–395. doi: 10.1111/den.12195. [DOI] [PubMed] [Google Scholar]
- 31.Sulz M.C., Frei R., Semadeni G.-M., Sawatzki M., Borovicka J., Meyenberger C. The role of single-balloon colonoscopy for patients with previous incomplete standard colonoscopy: Is it worth doing it? Surg. Endosc. 2016;30:1876–1882. doi: 10.1007/s00464-015-4405-5. [DOI] [PubMed] [Google Scholar]
- 32.Despott E.J., Murino A., Nakamura M., Bourikas L., Fraser C. A prospective randomised study comparing double-balloon colonoscopy and conventional colonoscopy in pre-defined technically difficult cases. Dig. Liver Dis. 2017;49:507–513. doi: 10.1016/j.dld.2017.01.139. [DOI] [PubMed] [Google Scholar]
- 33.Hermans C., Van Der Zee D., Gilissen L. Double-balloon endoscopy after incomplete colonoscopy and its comparison with computed tomography colonography. Clin. Endosc. 2018;51:66. doi: 10.5946/ce.2017.011. [DOI] [PMC free article] [PubMed] [Google Scholar]