Abstract
Usually, miRNAs function post-transcriptionally, by base-pairing with the 3′UTR of target mRNAs, repressing protein synthesis in the cytoplasm. Furthermore, other regions including gene promoters, as well as coding and 5′UTR regions of mRNAs are able to interact with miRNAs. In recent years, miRNAs have emerged as important regulators of both translational and transcriptional programs. The expression of miRNA genes, similar to protein-coding genes, can be epigenetically regulated, in turn miRNA molecules (named epi-miRs) are able to regulate epigenetic enzymatic machinery. The most recent line of evidence indicates that miRNAs can influence physiological processes, such as embryonic development, cell proliferation, differentiation, and apoptosis as well as pathological processes (e.g., tumorigenesis) through epigenetic mechanisms. Some tumor types show repression of tumor-suppressor epi-miRs resulting in cancer progression and metastasis, hence these molecules have become novel therapeutic targets in the last few years. This review provides information about miRNAs involvement in the various levels of transcription and translation regulation, as well as discusses therapeutic potential of tumor-suppressor epi-miRs used in in vitro and in vivo anti-cancer therapy.
Keywords: Ago, DNMT inhibitor, epi-miRs, HDAC, lncRNA, virial vector
1. Introduction
Although research into RNA biology has been ongoing for more than two decades, almost each year brings new discoveries. Until recently, it was thought that microRNAs (miRNAs) act mainly in the cytoplasm at the post-transcriptional level. Interestingly, miRNAs can exert regulatory effect both in the cell (i.e., cytoplasm and nucleus) in which they are produced and in neighboring cells. The latter intracellular transfer of miRNA is mediated by gap junction channels or exosomes [1]. Interestingly, mature miRNAs can regulate one or more mRNA targets, but also a single mRNA transcript can be bound and regulated by many different miRNAs. It is estimated that each miRNA can recognize ~100–200 target sites of the transcriptome and the inhibitory effect on expression can be achieved at 1000 copies per cell [1,2]. miRNAs can recognize and bind to 3′UTR, 5′UTR and coding sequence of their targets’ mRNA, as well as to promoter regions. Considering miRNAs variety and localization, cell type and cell state, their possibilities to regulate gene expression are limitless.
2. Inhibition or Activation of Translation
Mature miRNAs (mainly guide strands) form a complex with Argonaut (AGO) proteins called miRNA-induced silencing complex (miRISC) which interact with other proteins including DICER, TRBP, PACT and GW182. The miRNA specific region called ‘seed sequence’ (which includes nucleotides between 2 and 8, counting from the 5′ end of the miRNA) base-pairs with miRNA recognition elements (MREs) located on mRNA targets. miRISC complex binding to 3′UTR leads to mRNA cleavage or mRNA decay and finally translation inhibition. For example, full complementarity of the seed region to MRE induces AGO-2 endonuclease activity resulting in mRNA cleavage and destabilization of AGO2-miRNA interaction that ultimately promotes miRNA degradation [3,4]. In contrast, incomplete complementarity prevents AGO-2 endonuclease activity but initiates the recruitment of GW182 protein family leading to mRNA decay. GW182 interacts with PABPC (polyadenylate-binding protein) that promotes efficient mRNA deadenylation by recruiting poly(A)-deadenylase complexes (PAN2-PAN3 and CCR4-NOT). Subsequently, mRNA-decapping enzymes (DCP1-DCP2) recognize and remove the 5′-cap from mRNA transcripts making mRNA susceptible to degradation by 5′-3′ exoribonuclease 1 (XRN1) [5,6]. A recent study has revealed that mRNA decay is responsible for a large majority (66–90%) of miRNA-mediated translation repression [7]. Moreover, miRISC can inhibit translation at the initiation step probably through dissociation of eukaryotic initiation factors 4A (eIFA4-I and eIFA4-II) making it difficult for ribosome scanning and assembly of the eIF4F translation initiation complex [8,9].
In addition, miRNAs can also bind to target sites in the coding region and inhibit translation. Probably, target sequences in the coding regions are used when the 3′UTR are too short or adjust to protein abundance of alternative splice variants [10]. For example, Cardinali et al. have identified that the AHNAK gene contains a miR-222 target sequence within the coding region hence miR-222 can directly down-regulate its expression [11]. Additionally, a study by Splengler et al. has revealed an abundance of miRNA target sites in gene coding regions [12].
Surprisingly, some studies have reported that miRNAs binding to 3′UTR or 5′UTR regions can up-regulate gene expression by increasing translation rates of proteins.
It was demonstrated that translation activation can depend on the cell cycle state and proteins that are bound to the AGO2-miRNA complex within the 3′UTR. Indeed, in serum starved cells Fragile-X-mental retardation related protein 1 (FXR1) was recruited by the AGO2-miRNA complex associated with AU-rich elements (AREs) at the 3′UTR and activated translation [13]. The miRNA-mediated activation of transcription has been observed also in other quiescent cells, such as immature oocytes of the Xenopus (e.g., Myt1 mRNA via AGO-miR16-FXR1 complex) [14].
Furthermore, it was revealed that miRNAs that bind to the 5′UTR can enhance translation through various mechanisms. For example, liver specific miR-122 binding to RNA of hepatitis C virus protects the single-stranded 5′ end from cytosolic exonuclease activities (increasing RNA stability against Xrn1) and enhances the recruitment of ribosomes as well as possibly providing a scaffold for binding of other essential factors for translation [15,16,17,18]. Another example is miR-10a that interacts with the 5′ terminal oligopyrimidine (5′TOP) motif of ribosomal protein mRNAs and enhance their translation during amino acid starvation [19]. Moreover, miR-346, produced mostly in brain tissues, binds to 5′UTR of the receptor interacting protein 140 (RIP140) mRNA facilitating its association with the polysomes and finally activating translation via an AGO2-independent manner [20].
3. Suppression or Enhancement of Transcription
Surprisingly, studies have shown bidirectional transport of the core components of miRNA silencing machinery. It was demonstrated that several proteins including Importin-8, Importin α/β (Impα/Impβ) and Exportin-1 (XPO1) mediate shuttling of key RISC components from the cytoplasm to the nucleus, moreover, XPO1 is able to transport the nuclear RISC (miRNA-Ago-TNRC6A complex) to the cytoplasm [21,22].
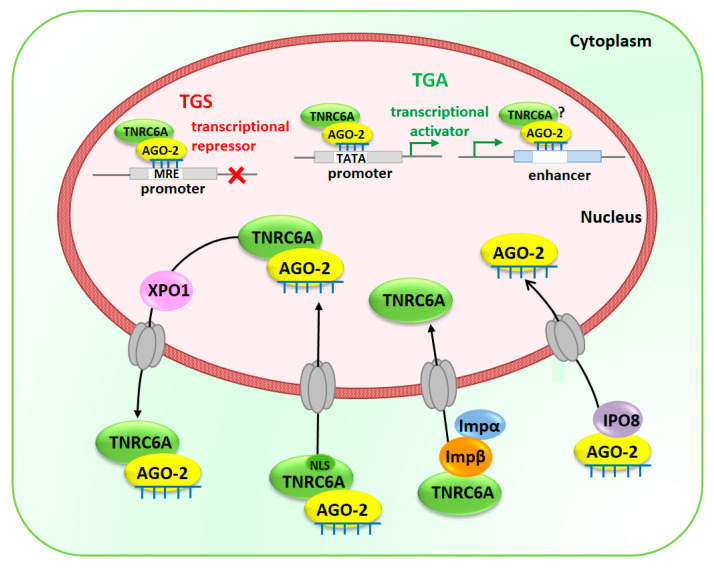
On the one hand, TNRC6A protein, also known as GW182, can be independently transported into the nucleus binding directly to Impβ and interacting with Impα [23,24]. On the other hand, TNRC6A facilitates the shuttling of miRNA containing AGO-2 into the nucleus via its own nuclear localization signal sequence [25]. Besides, AGO-2 can be imported into the nucleus via IPO8 only when it loads mature miRNA [26]. Figure 1 illustrates the different ways of delivering RISC proteins and miRNAs from the cytoplasm into the nucleus.
Figure 1.
Transport of mature miRNAs and components of RISC (RNA-induced silencing complex) into the nucleus. TNRC6A is shuttled from the cytoplasm into the nucleus either via its own NLS sequence when it interacts with miRNA-AGO complex or independently via its interaction with Importin β (Imp β) and Importin α (Impα). While mature miRNAs loaded into AGO-2 are translocated into the nucleus by Importin 8 (IPO8) miRNA-AGO-TNRC6A complex can be exported back to the cytoplasm by Exportin 1 (XPO1). In the nucleus, miRISC will interact with promoters or enhancers leading to transcriptional gene silencing (TGS) or transcriptional gene activation (TGA). The putative miRNA recognition elements (MREs) could be recognized by miRNAs that mediate chromatin silencing complex assembly or de novo DNA methylation at the promoter region resulting in compact, silent heterochromatin and TGS. Unlike, when miRISC interacts with TATA-box motifs enhancing promoter activities leading to TGA through enrichment of chromatin-remodeling factors and active chromatin marks. Moreover, miRNAs interaction with enhancers result in TGA through chromatin remodeling and the enrichment of active marks at enhancer regions. NLS—nuclear localization signal sequence.
Moreover, it is proposed that miRNA nuclear localization can also be controlled by nuclear localization signal sequences in miRNA molecules or full processing of pre-miRNAs in the nucleus. Several studies show that various motifs, including AGUGUU-motif, 5′-UUGCAUAGU-3′ and 5′-AGGUUGKSUG-3′ motifs (where K is a uridine or a guanine) as well as the consensus ASUS sequence (where S is a cytosine or a guanidine) are presented in many miRNAs and are engaged in the nuclear translocation [27,28,29]. It is supposed that miRNAs translocation is controlled by RNA-binding proteins (RBPs), however, molecular pathways are now recognized. Regarding processing of pre-miRNA molecules and their loading into nuclear RISC complex, there are many uncertainties that need to be investigated.
Although the functions of nuclear miRNAs have not been fully elucidated, it is suggested that they can regulate both transcriptional rates and post-transcriptional levels of mRNAs. miRNA-promoter interaction mediated by AGO proteins may either suppress or activate transcription depending on the location of their target region and epigenetic status of the promoter [22,30]. Genome-wide analysis revealed that human promoters contain miRNA-seed matching sites, suggesting that miRNA-mediated transcription regulation is likely to be a common phenomenon [31]. On the one hand, Benhamed et al. demonstrated that AGO-2 and let-7f are involved in the transcriptional repression of proliferation-promoting genes regulated by the retinoblastoma (Rb)/E2F repressor complex in senescence [32]. The putative MREs for the let-7f have been localized in the promoters of two E2F-target genes CDC2 and CDCA8. Similarly, nuclear miR-522 suppresses transcription of CYP2E1 gene by interacting with its promoter forming a DNA:RNA hybrid which probably prevents binding of Pol II and transcription factor [33]. On the other hand, Zhang et al. revealed that several miRNAs, such as let-7i, miR-138, miR-92a and miR-181d bind to the TATA-box motifs and enhance the promoter activities of interleukin-2, insulin, calcitonin or c-Myc, respectively [34]. Also, Cyclin B gene has a sequence located in its promoter that interacts with miR-744-5p and miR-466d-3p leading to transcriptional upregulation [35]. A recent study has revealed, that miRNAs (miR-26a-1, miR-339, miR-3179, miR-24-1 and miR-24-2) are able to induce expression of neighboring genes and function as enhancer (cis-acting DNA elements) regulators [36]. Moreover, this study has also shown that miR-24-1 (located in the enhancer region) increases expression of FBP1 and FANCC genes and triggers direct chromatin state alteration of the FBP1 enhancer that activate transcription. Another notable fact is that transcriptional gene silencing (TGS) and transcriptional gene activation (TGA) can be achieved by miRNA-mediated epigenetic regulation. Indeed, miRNA directs the RNA-induced transcriptional silencing complex (RITS), which consists of chromatin remodeling enzymes (e.g., HDAC1, EHMT2 and EZH2) and DNA methyltransferase (DNMT3A), to promoter leading to the transition of active chromatin structure to silent heterochromatin [31]. According to the study carried out by Kim and co-workers miR-320 directs to the promoter region AGO-1 that acts as the effector protein for transcriptional silencing of POLR3D gene [37]. Furthermore, simultaneous enrichment of tri-methyl histone H3 lysine 27 (H3K27me3, a repressive chromatin mark) and EZH2, a histone methyltransferase that mediates H3K27me3, has been observed at the POLR3D promoter [37]. Another study has revealed that miR17-5p and miR20a, encoded within a poly-miRNA cluster miR-17-92, are involved in the acquisition of heterochromatin marks at the promoters through seed-paring manner [38]. miRNA-mediated TGS is involved in cell differentiation processes. For example, during granulopoiesis miR-223-RISC interaction with the promoter of nuclear factor I-A (NFI-A) results in the recruitment of Polycomb group complex and histone-modifying enzymes that repress transcription of NFI-A, an important step for granulocytic differentiation [39]. It is postulated that specific miRNA can initiate TGS through de novo DNA methylation or chromatin modification in human cancer cells. In fact, miR-10a with AGO-1 and AGO-3 reduces HOX4 expression in human breast cells mediating in de novo DNA methylation and accumulation of repressive chromatin marks (H3K27me3 and H3K9me2, di-methyl histone H3 lysine 9) at its promoter [40].
In contrast, AGO-miRNA complex may activate the expression of target loci by either disruption of the recruitment of silencing proteins (e.g., PRC2) to lncRNAs (long non-coding RNAs) or recruitment of protein complex containing transcriptional activators (e.g., transcription factors) [31,41]. In the nucleus, lncRNAs regulate epigenetic silencing of adjacent genes through recruiting chromatin-remodeling factors in close proximity of their promoters [42]. In case of miR-744 and Ccnb1 gene, miRNA-mediated TGA rely on the recruitment of AGO proteins and RNA Pol II enrichment as well as active chromatin marks (such as H3K4me3, tri-methyl histone H3 lysine 4) at the regulated gene promoters [35]. Moreover, miR-373 activates transcription of E-cadherin and CSDC2 genes only via enrichment of RNA Pol II at their promoters [43], while miR-205 induces the expression of IL24 and IL32 tumor suppressor genes by targeting specific sites in their promoters as well enrichment of RNA Pol II and active chromatin modifications [44].
Similar to cytoplasmic miRNAs, nuclear miRNAs can also mediate post-transcriptional gene silencing (PTGS) inducing degradation of target mRNAs. Several studies suggest that miRNAs contribute to the regulation of miRNA precursors and lncRNA transcripts [31]. For instance, mouse nuclear miR-709 is involved in the post-transcriptional regulation of the pri-miR-15a/miR-16-1, binding to a 19-nt recognition element and preventing processing of primary transcripts, thus, nuclear miRNAs can influence the biogenesis of other miRNAs suggesting hierarchical structures among miRNAs [45]. Furthermore, some nuclear-retained lncRNAs are also regulated by AGO-miRNA complexes that interact with miRNA-complementary sequences located in lncRNAs, thus impairing their stability and function [42]. Indeed, the highly abundant lncRNA, metastasis associated lung adenocarcinoma transcript 1 (MALAT1), has two MRE’s which are recognized and bound by miR-9 [46]. Subsequently, putative miR-675-5p binding site within H19 RNA transcripts has been identified and the overexpression of miR-675-5p significantly downregulated the level of the H19 transcript [47]. So far, several other non-coding RNAs directly targeted by miRNAs have been identified. Interestingly, a long non-protein coding RNA involved in mammalian X-chromosome inactivation, X (inactive)-specific transcript (XIST), has seed-paring sites for miR-210 which modulates its RNA level [48]. Additionally, miR-671 directs AGO2-mediated cleavage of a circular antisense transcript of the CDR1 gene and negatively regulates this non-coding antisense transcript [49].
Regulation of Alternative Splicing
miRNAs are able to indirectly modulate alternative splicing by regulating translation of various splicing factors. However, mounting evidence suggests that AGO-miRNA complexes can affect the regulation of alternative splicing directly in the nucleus by epigenetic and non-epigenetic mechanisms. A co-immunoprecipitation study has identified multiple AGO-associated splicing factors, moreover, AGO-1, AGO-2 and DICER1 knockdown and overexpression experiments confirmed their involvement in splicing decisions at alternatively spliced exons [50,51]. Advanced molecular analyses were able to identify miRNA binding sites within intronic sequences in mouse and human brain as well as in human myocardial cells [12,52,53]. It is proposed that miRNAs-mediated compaction of chromatin structure at specific exon-intron junctions slows the rate of RNA Pol II elongation, which favors exon inclusion [54]. Surprisingly, exon skipping can be achieved by single-stranded oligonucleotides (ss-siRNA), ss-siRNA is incorporated by AGO-2 in the cytoplasm, then is transported into the nucleus where AGO2-ss-siRNA complex binds to the target mRNA and disrupts association with the splicing machinery [55].
Taken together, the above considerations illustrate the complex regulatory mechanisms of miRNA-mediated gene expression in the cytoplasm and the nucleus. It should be emphasized, that miRNAs are involved in many crucial cellular regulatory processes and may activate or inhibit gene expression at both transcriptional and post-transcriptional level. Thus, deregulation of miRNAs biogenesis and function can disrupt these processes and finally lead to a wide range of human diseases. Hence, miRNAs are valuable as diagnostic and prognostic biomarkers for many diseases, including cancer, diabetes mellitus, cardiovascular pathologies and neurological disorders. Moreover, miRNAs are considered as molecular targets of novel therapies and treatment strategies.
4. miRNAs As Potential Cancer Epi-Therapeutics
Over the past few decades growing evidence has linked epigenetic mechanisms with the regulation of gene expression. Epigenetic markers such as DNA methylation and post-translational modifications of histone tails can rearrange the structure of chromatin leading either to activation or repression of transcription activity (for details see reviews [56,57]). It is interesting that not only nucleotide sequences determine the level of gene expression but also epigenetic modifications are involved in this process. Epigenetic processes are orchestrated by multiple proteins (e.g., DNA methyltransferases, DNA demethylases and histone modifying enzymes), non-coding RNAs (e.g., miRNAs and lncRNAs) and environmental factors. Typically, loss of DNA methylation (hypomethylation) turns on gene transcription by altering the structure of chromatin. In turn, too much DNA methylation (hypermethylation) induces chromatin compaction and hinders the expression of genes. Therefore, disruption of epigenetic regulation can lead to inappropriate gene expression that impairs crucial biological processes resulting in the development of “epigenetic diseases”. The first “epigenetic disease” was cancer and it was established that patients with colorectal cancer had less DNA methylation levels in cancer tissues than from their normal tissue [58]. Growing evidence suggests that epigenetic changes, unlike DNA sequence mutations, are reversible, so it seems that these changes can be an ideal target for epigenetic treatments.
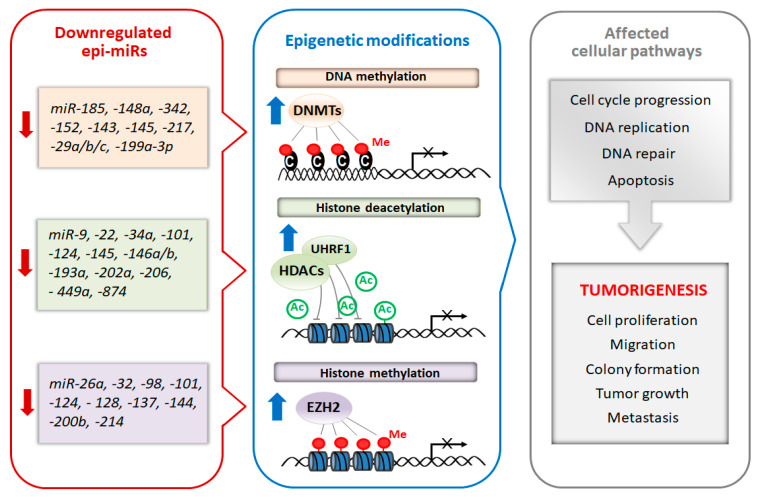
Recently, a subclass of miRNAs, referred to as epi-miRNAs, that influence the expression of genes encoding epigenetic effector and reader proteins, has been identified [59]. Due to the important role of epi-miRs in the modulation of the epigenome, they are currently considered as potential therapeutic targets, especially in cancer. Manipulation of epi-miRs can affect the expression of epigenetically-regulated genes, such as oncogenes and/or tumor suppressor genes, involved in important cellular pathways including DNA replication, cell cycle progression and apoptosis [60,61]. The two types of miRs, oncomiRs and tumor-suppressor miRs, can be distinguished regarding their role in carcinogenesis. Generally, oncomiRs are up-regulated thereby increasing cancer cell proliferation and metastasis, in contrast the expression of tumor-suppressor miRs are down-regulated leading to enhanced tumorigenesis [62]. In this review, we focus on the therapeutic potential of tumor-suppressor epi-miRs that are downregulated in various types of cancer (casi el tinc. Emerging studies found that the decreased levels of epi-miRs promote cell proliferation, colony formation, tumor growth and metastasis [62,63,64]. Moreover, the suppression of some epi-miRs are responsible for the drug resistance of cancer cells [64,65]. Schematic relationship between downregulated tumor-suppressor epi-miRs, chromatin-modifying enzymes and cellular processes is shown in Figure 2.
Figure 2.
Schematic diagram of epi-miRs involved in the regulation of epigenetic modifiers and tumorigenesis. Suppression of miRNAs that regulate chromatin-remodeling enzymes lead to their overexpression. In turn epigenetic dysregulation resulting in improper regulation of genes responsible for different cell processes including cell proliferation, DNA repair and apoptosis thus triggering tumorigenesis.
To date, several causes have been found that influence the activity of miRNAs, their down-regulation is coupled with epigenetic silencing or genomic abnormalities, such as gene amplification, deletions and microdeletions (e.g., at miR-101-1 loci) as well as mutations and chromosomal rearrangements [66,67]. Considering, the drug resistance of cancer chemotherapy (i.e., doxorubicin, cisplatin, paclitaxel), which are related to down-regulation of epi-miRs, their enforced expression appears to be an interesting approach to restore drug sensitivity (Table 1). Fabbri and co-workers revealed that the miR-29 family (29a, -b, and -c) act as tumor suppressor miRs in lung cancer and regulate transcript levels of DNMT3A and DNMT3B [68]. Moreover, it has been established that synthetic epi-miR, miR-29b oligonucleotides, potentiates a hypomethylating effect of DNMT1 inhibitors (decitabine or azacitidine) resulting in better AML response for treatment probably due to the inhibition of other DNMT isoforms that are not efficiently suppressed by these agents [69]. Another study showed that synthetic miR-29b mimics inhibit HDAC4 expression in multiple myeloma cell lines, reduce migration potential and increase apoptosis, therefore, this approach could offer a novel targeted therapy [70]. In addition, a recent study has shown that miR-148a combination therapy with either cisplatin or doxorubicin significantly enhanced apoptosis in urothelial cell carcinoma of the bladder cell lines [71]. Importantly, cancer stem cells (CSCs) are characterized by their ability to self-renew and resistance to standard chemotherapy, during remission can regenerate a tumor identical to the original one. An elegant study by Iliopoulos and colleagues uncovered that the combinatorial therapy of doxorubicin with epi-miR (miR-200b) was more effective than doxorubicin alone, blocking tumor growth and preventing relapse [72]. Interestingly, many natural agents, such as resveratrol, curcumin and glabridin used for epigenetic therapy, among others, exert their potent anti-tumor effects by enhancing expression of epi miRs. For instance, resveratrol causes up-regulation of miR-137 in neuroblastoma tumors [73], curcumin increases levels of miR-29a and miR-185 in hepatocellular cancer cells [74], in turn glabridin potentiates expression of miR-148a in breast cancer cells [75].
Table 1.
Epi-miRs as potential cancer therapeutics.
| Epi-miRNA | mRNA Target | Cell Lines | Methods | Animal Study | Results | References |
|---|---|---|---|---|---|---|
| Breast cancer | ||||||
| miR-34a |
HDAC1
HDAC7 |
MCF-7, MDA-MB-231, BT-20, T47-D, PC3, DU-145, LNCaP, NIH:OVCAR, SK-OV-3, HeLa and non-transformed mammary MCF-10A cells | miR-34a mimics; luciferase reporter assay (in MCF-7, PC3, and MDA-MB-231 cells) | ND | miR-34a expression negatively correlates with tumor grades; transfection of miR-34a mimic reduces cell survival and increases the cytotoxicity of chemotherapy drugs; re-expression of miR-34a inhibits the tumorigenic activity of cancer stem cells (CSCs). | [82] |
| miR-101 | EZH2 | SKBR3 | pre-miR-101; luciferase reporter assay (in SKBr3 cells) | ND | miR-101 overexpression in SKBr3 attenuates cell proliferation, migration and inhibits the invasive potential. | [83] |
| miR-128 | BMI1 | SK-3rd, MCF-7 and SKBR3 | lentivirus vector miR-128; luciferase reporter assay (in SK-3rd and MCF-7 cells) | ND | Ectopic expression of miR-128 decreases cell viability and increases apoptosis and DNA damage in the presence of doxorubicin; ectopic miR-128 expression sensitizes BT-ICs (breast tumor–initiating cells) to doxorubicin enhancing the DNA damage and pro-apoptotic effects. | [84] |
| miR-148a | SMAD2 | MDA-MB-231 and Hs-578T | miR-148a mimics; luciferase reporter assay (in MDA-MB-231 cells) | BALB/c nude mice; MDA-MB-231 cells were injected s.c.; glabridin (GLA) was administered intragastrically each day. | GLA enhances the expression of miR-148a; GLA-treated tumors have increased expression of miR-148a and decreased expressions of SMAD2. | [75] |
| miR-185 | DNMT1 | MDA-MB-231, MDA-MB-361, MDA-MB-435, MDA-MB-468, MCF-7, T47D, BT-474, BT-20 and BT-483; normal mammary epithelial cell lines (HBL-100, 184A1 and MCF-10A) | miR-185 mimics | Nude mice; MDA-MB-231 cells were injected s.c.; intratumoral injection of miR-185 mimics. | Ectopic expression of miR-185 inhibits cell proliferation and induces apoptosis; inhibits tumor growth in vivo. | [85] |
| miR200b | SUZ12 | MCF-10A cells containing the ER-Src fusion gene, MCF7, SKBR3, MDAMB-231, MDA-MB-435, NSCCs (non-stem cancer cells) | miR-200b; luciferase reporter assay (in ER-Src cells) | Athymic nude mice; CSCs were pretreated with miR-200b and injected s.c.; ER-Src (treated and untreated with tamoxifen) were injected s.c. and then doxorubicin or combination doxorubicin and miR-200b was administered i.p. | miR-200b overexpression affects CSCs growth and reduces cell invasiveness; pretreatment of CSCs with miR-200b blocked tumor formation in vivo; combinatorial therapy (doxorubicin with miR-200b) causes regression of tumor growth and prevents relapse of the disease. | [72] |
| Bladder cancer | ||||||
| miR-101 | EZH2 | T24, UM-UC-3 and TCCSUP | vector pcDNA3.1 with pre-miR-101; luciferase reporter assay (in UM-UC-3 cells) | ND | Restored miR-101 expression inhibits cell proliferation, suppresses colony formation and hinders EZH2-mediated neoplastic progression. | [86] |
| miR-124 | UHRF1 | J82, T24, HEK 293 and SV-HUC-1 | miR-124 mimics; luciferase reporter assay (in HEK-293cells) | Male BALB/C-A mice; T24 cells were injected s.c. and then intratumoral injection was performed with miR-124 mimics. | miR-124 overexpression attenuates cell proliferation, migration, invasion and vasculogenic mimicry; inhibits tumor growth in vivo. | [87] |
| miR-144 | EZH2 | T24 | vector pcDNA–miR-144; luciferase reporter assay (in HEK293 cells) | ND | miR-144 overexpression inhibits cell proliferation; decreases EZH2 protein levels. | [88] |
|
miR-145-5p
miR-145-3p |
UHRF1 | T24 and BOY | pre-miR-145-5p and pre-miR-145-3p; luciferase reporter assay (in T24 and BOY cells) | ND | Ectopic expression of either miR-145-5p or miR-145-3p suppresses cancer cell growth, migration and invasion and induces apoptosis. | [89] |
| miR-148a | DNMT1 | SV-HUC-1, T24, TCCSUP, J82 and UM-UC-3 | miR-148a mimics; cisplatin or doxorubicin treatment | ND | miR-148a overexpression reduces cell viability by promoting apoptosis; combinatorial therapy (miR-148a/cisplatin or miR-148a/doxorubicin) enhanced apoptosis. | [71] |
| Colorectal cancer | ||||||
| miR-9 | UHRF1 | HCT116 and HT29 | miR-9 oligonucleotides; lentivirus vector miR-9; luciferase reporter assay (in HCT116 and HT29 cells) | ND | miR-9 overexpression attenuates CRC cell proliferation and promotes cell apoptosis; reduces UHRF1 expression. | [90] |
| miR-143 | DNMT3A | 228, CaCO2, Clone A, HCT116, HT-29, MIP101 and SW480 | pre-miR-143; luciferase reporter assay (in 228 and SW480 cells) | ND | Ectopic expression of miR-143 inhibits cell growth, reduces clone formation; restored miR-143 expression decreases tumor cell growth and soft-agar colony formation, and downregulates DNMT3A expression. | [91] |
| miR-342 | DNMT1 | SW480, HT29, HCT116 and HEK293T | miR-342 oligonucleotides; lentivirus vector miR-342; luciferase reporter assay (in SW480 cells) | Female athymic BABL/c nude mice; cell lines stably expressing miR-342 were injected s.c. | Enhanced miR-342 expression inhibits cell proliferation and invasion; miR-342 overexpression leads to demethylation and induction of tumor suppressor genes through blocking DNMT1 expression; miR-342 overexpression inhibits tumor growth and lung metastasis in vivo. | [92] |
| Endometrial cancer | ||||||
| miR-101 | EZH2 | SPAC-1-L and SPAC-1-S; HEC-50 and HOUA-I cell lines were derived from poorly-differentiated endometrioid EC (endometrial carcinoma) | vector with pre-miR-101-3p; luciferase reporter assay (in SPAC-1-L and HOUA-I cells) | ND | Ectopic overexpression of miR-101 suppresses cell proliferation, attenuates the epithelial-mesenchymal transition associated cancer cell migration and invasion, abrogates the sphere-forming capacity and enhances chemosensitivity to paclitaxel. | [93] |
| Esophageal cancer | ||||||
| miR-203 | BMI1 | EC9706 and KYSE150 | lentivirus vector miR-203; luciferase reporter assay (in EC9706 cells) | Female nude mice and nonobese diabetic/severe combined immunodeficient mice; freshly prepared cells were injected s.c. | miR-203 overexpression reduces colony formation, tumorigenicity ability and self-renewal of esophageal cancer stem-like cells; increases sensitivity to cisplatin. | [94] |
| Gastric cancer | ||||||
| miR-29b/c | DNMT3A | AGS and BGC-823 | miR-29b/c mimics; luciferase reporter assay (in BGC-823 cells) | ND | miR-29b/c overexpression decreases migration and reduces invasive ability; miR-29b/c suppresses the expression of DNMT3A. | [95] |
|
miR-146a
miR-146b |
UHRF1 | GC9811, GC9811-P, MKN28NM and MKN28M | pre-miR-146a/b; lentivirus vector miR-146a/b; luciferase reporter assay (in HEK293T and GC9811 cells) | Nude mice; metastasis assay: GC9811-P cells infected with miR-146a/b were injected into the tail vein. | Restored expression of miR-146a/b reduces the expression of UHRF1; upregulation of miR-146a/b suppresses metastasis. | [96] |
| miR-148a | DNMT1 | SGC-7901, BGC-823 and GES-1 (human gastric epithelium-immortalized cell line) | miR-148a mimics | ND | miR-148a mimics suppresses cell proliferation; miR-148a overexpression decreases DNMT1 expression and induces the overexpression of MEG3 (lncRNA). | [97] |
| miR-206 | HDAC4 | SGC-7901, BGC-823, AGS, non-malignant gastric cell line GES-1 and HEK293T | miR-206 mimics; vector with miR-206 | Nude mice; SGC-7901 cells carrying P2GM-miR-206 was injected s.c. | Ectopic expression of miR-206 represses cell proliferation, colony formation, invasion and migration; miR-206 promotes myogenic differentiation and blocks tumor growth in vivo. | [98] |
| Glioblastoma | ||||||
| miR-128 | Bim-1 | U87MG, U251MG and U373MG | pre-miR-128 mimics; lentivirus vector pri-miR-128-1; luciferase reporter assay (in U87, U251, and U373 cells) | Athymic mice; U87 cells stably expressing miR-128 were implanted s.c. | miR-128 expression reduces glioma cell proliferation, self-renewal in vitro and glioma xenograft growth in vivo. | [99] |
| miR-128 |
SUZ12
BMI1 |
U87 malignant glioma (MG) and U251MG glioblastoma cells | pre-miR-128; lentivirus vector miR-128; luciferase reporter assay (in HEK293 cells) | Mut3 mice (hGFAP-cre; Nf1flox/+; Trp532/+). | miR-128 overexpression reduces proliferative potential and colony formation; reestablishment of miR-128 expression impairs glioma stem-like cells self-renewal and increases their radiosensitivity. | [100] |
| Head and neck squamous cell carcinoma | ||||||
| miR-874 | HDAC1 | SAS, FaDu, HSC3, IMC-3, human fibroblast and MRC-5 | mature miR-874; luciferase reporter assay (in SAS cells) | ND | Restoration of miR-874 inhibits cell proliferation, induces cell cycle arrest and apoptosis. | [101] |
| Hepatobiliary cancer | ||||||
|
miR-152
miR-148a |
DNMT1 | KMCH-1, Mz-ChA-1, TFK-1 and H69; Mz-IL-6 (KMCH-1 stably transfected with IL-6) | pre-miR-152 and pre-miR-148a; luciferase reporter assay (in Mz-ChA-1 cells) | Male athymic nu/nu mice; Mz-IL-6 cells were injected s.c. | pre-miR-148a and pre-miR-152 decreases DNMT-1 protein expression and reduces cell proliferation; miR-148a and miR-152 expression was reduced in tumor cell xenografts in vivo. | [102] |
| Hepatocellular carcinoma | ||||||
| miR-22 | HDAC4 | Hep3B and SMMC7721 | miR-22 mimics; luciferase reporter assay (in Hep3B cells) | Male BALB/c athymic nude mice; miR-22 mimics transfected Hep3B or SMMC7721 cells were injected s.c. | Restoration of miR-22 expression suppresses cell proliferation and endogenous expression of HDAC4 protein; miR-22 transfection delays tumor formation and reduces tumor size in vivo. | [103] |
|
miR-29a
miR-185 |
DNMT3A
DNMT3B |
HepG2 and HuH-7 | dendrosomal curcumin (DNC) treatment | ND | Overexpression of miR-29a and miR-185 after dendrosomal curcumin (DNC) treatment, down-regulates the expression of DNMT1, 3A and 3B. | [74] |
| miR-145 | HDAC2 | Hep3B, HepG2, SNU-182, SNU-449 and PLC/PRF/5 | miR-145 mimics; vector with miR-145; luciferase reporter assay (in SNU-449 cells) | Male athymic nude mice; Hep3B cells transfected with miR-145 were injected s.c. | Ectopic expression of miR-145 inhibits cell growth and HDAC2 expression; inhibits tumor growth in vivo. | [104] |
| miR-200a | HDAC4 | SMMC-7721 and HepG2 | miR-200a mimics; lentivirus vector miR-200a; luciferase reporter assay (in SMMC-7721 cells) | Nude mice; HepG2 cells stably transfected with miR-200a were implanted s.c. | miR-200a inhibits cell proliferation and migration both in vivo and in vitro; miR-200a overexpression induces up-regulation of global acetyl-histone H3. | [105] |
| Acute myeloid leukemia | ||||||
| miR-29b |
DNMT3A
DNMT3B |
AML cell lines, Kasumi-1, MV4-11 and K562 | pre-miR-29b; lentivirus vector miR-29b; luciferase reporter assays (in K562 cells) | ND | Enforced expression of miR-29b in AML cells reduces of the expression of DNMT1, DNMT3A, and DNMT3B; pre-miR-29b overexpression induces partial differentiation of AML blasts. | [79] |
| miR-29b | DNMT3B | primary AML blasts, K562 and Kasumi-1 | synthetic miR-29b | Female nude mice; synthetic miR-29b oligonucleotides were injected directly into the tumors. | Restoring miR-29b expression, induces apoptosis and dampens cell growth in AML cells. | [106] |
| miR-193a-3p |
DNMT3A
HDAC3 |
HL60, U937, U937-A/E-HA, Kasumi-1, SKNO-1, SKNO-1-siA/E-RNA and KG1 | miR-193a mimics; lentivirus vector miR-193a; luciferase reporter assay (in 293T cells) | Nude mice; SKNO-1 cells were injected s.c.; intratumor injection of miR-193a. | Enhanced miR-193a levels induce G1 arrest, apoptosis, and restores leukemic cell differentiation; decreases tumor size in vivo. | [107] |
| Chronic myeloid leukemia | ||||||
| miR-217 | DNMT3A | Bcr/Abl-expressing K562 cells | lentivirus vector miR-217; luciferase reporter assay (in K562DR cells) | Female immune deficient BALB/c nude mice; K562 cells were injected s.c.; drug administration: dasatinib or 5-AzadC or a combination of both dasatinib and 5-AzadC. | Forced expression of miR-217 inhibits expression of DNMT3A and sensitizes cells to growth inhibition mediated by the tyrosine kinase inhibitors (prevents drug resistance). | [108] |
| Multiple myeloma | ||||||
| miR-29b |
DNMT3A
DNMT3B |
MM cell lines | pre-miR-29b mimics (formulated with a Neutral Lipid Emulsion (NLE) delivery system); lentivirus vector miR-29b; luciferase reporter assay (in INA-6 cells) | Male CB-17 severe combined immunodeficient (SCID) mice; MM cells were inoculated s.c.; miR-29b mimics were administered intratumorally and systemically via tail vein. | miR-29b mimics impair cell cycle progression and potentiate the growth-inhibitory effects induced by the demethylating agent 5-azacitidine; miR-29b mimics induce anti-tumor effects in vivo. | [70] |
| Leukemia | ||||||
| miR-143 | DNMT3A | AML (HL-60, NB4 and U937), CML (K562), acute erythroleukemia (HEL), T lymphocytic leukemia (Jurkat and CEM), B-cell lymphoma (CA46, Raji cells of Burkitt’s lymphoma) and multiple myeloma (U266) | lentivirus vector miR-143 | ND | miR-143 overexpression decreases DNMT3A mRNA and protein expression, reduces cell proliferation, colony formation and cell cycle progression as well as induces apoptosis. | [109] |
| Lung cancer | ||||||
| miR-29a, -b, -c |
DNMT3A
DNMT3B |
A549 and H1299 | pre-miR-29a, -29b-1, -29c oligonucleotides; luciferase reporter assay (in A549 cells) | Female nude mice; A549 cells transfected with pre-miR-29a, -29b, or -29c, were injected s.c. | Enforced expression of miR-29s restores normal patterns of DNA methylation, induces re-expression of methylation-silenced tumor suppressor genes and inhibits tumorigenicity in vitro and in vivo. | [68] |
|
miR-193a-3p
miR-193a-5p |
UHRF1 | SPC-A-1, SPC-A-1sci, A549, H1299, LC-21, H358 and HEK-293T | miR-193a-3p/5p mimics; lentivirus vector miR-193a-3p/5p; luciferase reporter assay (in HEK293T cells) | BALB/C-nu/nu nude male mice; metastasis assays: SPC-A-1sci cells stably expressing the miR-193a-3p/5p-mimic were injected into the tail vein. | miR-193a-3p/5p overexpression inhibits cell proliferation, migration, invasion and epithelial–mesenchymal transition (EMT); lung metastasis formation in vivo. | [110] |
| Lymphoma | ||||||
| miR-26a | EZH2 | human BL cell lines; murine MYC-induced lymphoma cell lines | vectors with mature miR-26a; luciferase reporter assay (in HEK-293 cells) | ND | miR-26a overexpression reduces cell numbers and results in an anti-proliferative effect. | [111] |
| Melanoma | ||||||
| miR-200c | BMI1 | WM35, WM793, WM115A, M3523A, 1205Lu and 293T | lentivirus vector miR-200c; vector pEZX-miR-200c | Male athymic nu/nu mice; miR-200c–WM115A cells were injected s.c. | miR-200c overexpression decreases cell proliferation, colony formation and migratory capacity as well as drug resistance and increases sensitivity to various chemotherapeutic agents (including cisplatin); inhibits melanoma xenograft growth and metastasis in vivo. | [112] |
| Neuroblastoma | ||||||
| miR-137 | EZH2 | Mouse Neuro-2a (N-2a); human SH-SY5Y | miR-137 mimics; resveratrol (RSV) treatment; luciferase reporter assay (in HEK293 cells) | ND | miR-137 expression is up-regulated after RSV treatment; miR-137 inhibits EZH2 expression after RSV treatment; miR-137 regulates the EZH2-mediated apoptosis after RSV treatment. | [73] |
| miR-124 | EZH2 | Neural Stem Cells (NSCs) and HEK293T | mature miR-124 | ND | miR-124 overexpression down-regulates expression of Ezh2 and up-regulates neuron-specific Ezh2 target genes; promotes neuronal differentiation. | [113] |
| miR-137 | KDM1A | IMR-32, SHEP, SKN-BE and HEK-293 | pre-miR-137; luciferase reporter assay (in SHEP and HEK293 cells) | ND | Re-expression of miR-137 increases apoptosis, decreases cell viability and proliferation, induces neuronal differentiation; downregulates KDM1A. | [114] |
| miR-152 | DNMT1 | SK-N-BE, SH-SY5Y, SK-N-AS and Kelly | pre-miR-152; luciferase reporter assay (in Kelly cells) | ND | Ectopic upregulation of miR-152 declines cell invasiveness and anchorage-independent cell growth, contributing to the differentiated phenotype. | [115] |
| Oral squamous cell carcinoma | ||||||
| miR-32 | EZH2 | SCC-4, SCC-9, SCC-25 and Tca8113; normal oral keratinocyte cell line (hNOK) | mature miR-32 mimics; luciferase reporter assay (in Tca8113 cells) | ND | miR-32 overexpression reduces cell proliferation, migration and invasion, promotes cell apoptosis; miR-32 down-regulates the expression of EZH2. | [116] |
| Ovarian cancer | ||||||
|
miR-15a
miR-16 |
BMI1 | OVCAR-5, OV-167, OV-202, CP-70, A2780 and OSE (ovarian surface epithelial cell) | pre-miR-15a, pre-miR-16; luciferase reporter assay (in OV-202 and CP-70 cells) | ND | miR-15a or miR-16 overexpression decreases cell proliferation and clonal growth; downregulates BMI1 protein levels. | [117] |
|
miR-152
miR-185 |
DNMT1 | SKOV3, A2780, A2780/DDP (cisplatin-resistant), A549 and HepG2 | miR-152 and miR-185 mimics; luciferase reporter assay (in SKOV3/DDP cells) | CD-1/CD-1 nude mice; SKOV3/DDP cells transfected with miR-152 that were injected i.p. | miR-152 or miR-185 overexpression increases cisplatin sensitivity by inhibiting proliferation and promoting apoptosis; promotes sensitivity to cisplatin through targeting DNMT1 directly. | [118] |
| Pancreatic cancer | ||||||
|
miR-148a
miR152 |
DNMT1 | MIA PaCa-2 and AsPC-1 | pre-miR-148b, pre-miR-152; luciferase reporter assay (in MIA PaCa-2 and AsPC-1 cells) | ND | miR-148b and miR-152 overexpression inhibits cell proliferation and induces apoptosis; decreases DNMT1 expression, returns DNA methylation to normal patterns and induces re-expression of tumor suppressor genes. | [119] |
| Prostate cancer | ||||||
| miR-101 | EZH2 | DU145 | pre-miR-101; luciferase reporter assay (in SKBr3 cells) | Male nude athymic BALB/c nu/nu mice, DU145 stable cells overexpressing miR-101 were injected s.c. | miR-101 overexpression attenuates cell proliferation, migration and invasive potential; reduces colony formation; reduces tumor growth in vivo. | [83] |
| miR-145 | DNMT3B | PC3 | miR-145 mimics; luciferase reporter assay (in PC3 cells) | ND | miR-145 overexpression downregulates the expression of DNMT3B; sensitizes prostate cancer cells to X-ray radiation. | [120] |
| miR-449a | HDAC1 | PC-3, DU-145, BPH-1 and LNCaP | mature miR-449a mimics; a longer, dicer-dependent pre-miR-449a; luciferase reporter assays (in PC-3 cells) | ND | miR-449 expression arrests cell cycle, apoptosis; regulates cell growth and viability in part by repressing the expression of HDAC-1. | [121] |
| Renal cell carcinoma | ||||||
| miR-101 | UHRF1 | 786-O and Caki-1 | pre-miR-101-3p; luciferase reporter assay (in 786-O cells) | ND | Restoration of miR-101 inhibits cell proliferation, migration and decreases invasion activity; suppresses UHRF1 expression. | [122] |
| Rhabdomyosarcoma | ||||||
| miR-29 | Yin Yang 1 (YY1) | C2C12 myoblasts, RH30 and RD2 | pre-miR-29; lentivirus vector miR-29; luciferase reporter assays (in MB cells) | Athymic nu/nu female mice; RH30 cells were injected s.c.; intratumoral injection of lentivirus with miR-29. | miR-29 overexpression reduces cell growth and increases levels of the differentiation markers; intratumoral addition of miR-29 stimulates myogenic differentiation; inhibits tumor growth in vivo. | [123] |
| Testicular cancer | ||||||
| miR-199a-3p | DNMT3A (especially DNMT3A2) | Ntera 2 (NT2) | miR-199a-3p mimics; luciferase reporter assay (in NT2 cells) | ND | miR-199a-3p overexpression restores the expression of tumor-suppressor genes by affecting DNA methylation of their promoter regions. | [124] |
| Waldenström macroglobulinemia | ||||||
| miRNA-9 * |
HDAC4
HDAC5 |
BCWM.1, WM-WSU, MEC-1 and RL | pre-miRNA-9 * | ND | Restoring miRNA-9 * levels induces toxicity, apoptosis and autophagy; supports down-modulation of HDAC4 and HDAC5 and up-regulation of acetyl-histone-H3 and -H4 | [125] |
ND—no data; s.c.—subcutaneous; i.p.—intraperitoneal injection. * miR-9-3p.
Epi-miRs-targeted cancer therapy seems to be a promising approach since it is able to influence not only a single gene, but multiple pathways. It is possible to re-establish expression of epi-miRs by delivering synthetic miR mimics (double stranded RNA oligonucleotides directly loaded into RISC) or chemically modified poly(nucleic acids), however, cellular uptake of free synthetic miRs are limited because of the ease in which they a degraded in biofluids [76]. In order to overcome poor in vivo stability and improve efficient and specific-site delivery of miRs to the tumor, innovative delivery systems are required. Currently, both viral and non-viral systems are used to increase stability of miRNA oligonucleotides and enhance their therapeutic effect. Administration of epi-miRs via viral vectors (e.g., adenoviruses, adeno-associated viruses (AAV) or lentiviruses) is very effective, as shown by systemic intravenous injection of epi-miR, miR-26a, packaged into AAV vector, which inhibited progression of hepatocellular carcinoma in a mouse model [77]. However, due to the viral vectors possible toxicity and immunogenicity their use in clinical practice is limited. In this context, non-viral systems seem to be more promising, because of the control of their molecular composition, ease in manufacturing and relatively low immunogenicity. Different delivery systems including, lipid-based delivery system, synthetic polymers (e.g, polyethyleneimine (PEI)) and naturally occurring polymers (e.g., chitosan, protamine and atelocollagen) are applied to protect miRs from degradation (for details see the review [78]). For example, a novel transferrin-conjugated nanoparticle delivery system for synthetic epi-miR, miR-29b, was injected intravenously and significantly prolonged leukemic mice survival [79]. Despite significant advances made in delivery systems of miRs, substantial improvements will be necessary for achieving site-specific delivery.
The discovery of therapeutic epi-miRs potential in cancer therapy makes them attractive candidates for next-generation cancer treatment. It therefore seems likely that profiling of miRs expression and then using appropriate epi-miR-based therapeutics may revolutionize cancer treatment by enabling the reversal of the epigenetic program of tumor cells to a more normal state.
However, we realize that turning epi-miR-based therapy into clinical practice faces challenges. Indeed, some clinical trials with miRNA drugs have not always produced satisfactory results. For example, the FDA (Food and Drug Administration) halted phase I clinical trial of miR-34a mimic (drug: MRX34) used in patients with different types of cancer. Double-stranded miR-34a was encapsulated into a liposome-formulated nanoparticle and administered intravenously [80]. Although, preclinical studies were promising, immune-related serious adverse events (SAEs) appeared during phase I. Due to SAEs this clinical trial was terminated and future phase II trials of MRX34 for melanoma were withdrawn. In contrast human trial of miR-16 mimic (drug: MesomiR-1) exhibited hopeful results in patients with pleural mesothelioma and non-small cell lung cancer. Double-stranded miR-16 was delivered by non-living bacterial minicells with a targeting moiety (i.e., an anti-EGFR bispecific antibody that recognizes EGFR-expressing cancer cells) [81]. This is a new targeted therapy known as TargomiRs. The successful completion of phase I trial confirmed safety and early signs of antitumor activity of TargomiRs so phase II of the trial is expected to begin soon.
5. Conclusions
Knowledge in the miRNA field is steadily increasing and recent information about the mechanisms of action, especially their involvement in epigenetic regulation has shed new light on cellular regulatory networks.
Interestingly, mature miRNAs are present in both the nucleus and the cytoplasm, therefore they can be involved in the regulation of transcription and translation processes. Nuclear miRNAs can influence gene expression via transcriptional activation or transcriptional gene silencing and shaping alternative splicing, Cytoplasmic miRNAs mainly mediated translation inhibition, however, some miRNAs are capable of activating translation of their target mRNA. A growing body of evidence suggests that miRNAs can act as regulators of the cell epigenome through translation inhibition of proteins engaged in epigenetic control and/or interaction with lncRNA. Considering the pervasive role of miRNAs in numerous biological processes, especially tumorigenesis, better understanding of their role in epigenetic regulation will aid the development of new therapeutic strategies.
Currently, miRNA-based treatment approaches for cancer, including tumor-suppressor epi-miRs, are tested in in vitro and in vivo experiments. Although results seem promising further studies will be needed to clarify the safety and effectiveness of epi-miR therapy in clinical practice. We strongly believe that re-introduction of tumor-suppressor epi-miRs will allow for more effective, personalized therapies in the near future.
Acknowledgments
The author thanks Monika Chojnacka for assistance in language and text editing.
Funding
No external funding was used in the preparation of this article.
Conflicts of Interest
The author declares no conflict of interest.
References
- 1.Lemcke H., David R. Potential mechanisms of microRNA mobility. Traffic. 2018;19:910–917. doi: 10.1111/tra.12606. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Lopez J., Brieno-Enriquez M.A., Del Mazo J. MicroRNA biogenesis and variability. Biomol. Concepts. 2013;4:367–380. doi: 10.1515/bmc-2013-0015. [DOI] [PubMed] [Google Scholar]
- 3.Jo M.H., Shin S., Jung S.R., Kim E., Song J.J., Hohng S. Human Argonaute 2 Has Diverse Reaction Pathways on Target RNAs. Mol. Cell. 2015;59:117–124. doi: 10.1016/j.molcel.2015.04.027. [DOI] [PubMed] [Google Scholar]
- 4.O’Brien J., Hayder H., Zayed Y., Peng C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018;9:402. doi: 10.3389/fendo.2018.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Behm-Ansmant I., Rehwinkel J., Doerks T., Stark A., Bork P., Izaurralde E. mRNA degradation by miRNAs and GW182 requires both CCR4:NOT deadenylase and DCP1:DCP2 decapping complexes. Genes Dev. 2006;20:1885–1898. doi: 10.1101/gad.1424106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braun J.E., Truffault V., Boland A., Huntzinger E., Chang C.T., Haas G., Weichenrieder O., Coles M., Izaurralde E. A direct interaction between DCP1 and XRN1 couples mRNA decapping to 5’ exonucleolytic degradation. Nat. Struct. Mol. Biol. 2012;19:1324–1331. doi: 10.1038/nsmb.2413. [DOI] [PubMed] [Google Scholar]
- 7.Eichhorn S.W., Guo H., McGeary S.E., Rodriguez-Mias R.A., Shin C., Baek D., Hsu S.H., Ghoshal K., Villen J., Bartel D.P. mRNA destabilization is the dominant effect of mammalian microRNAs by the time substantial repression ensues. Mol. Cell. 2014;56:104–115. doi: 10.1016/j.molcel.2014.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fukao A., Mishima Y., Takizawa N., Oka S., Imataka H., Pelletier J., Sonenberg N., Thoma C., Fujiwara T. MicroRNAs trigger dissociation of eIF4AI and eIF4AII from target mRNAs in humans. Mol. Cell. 2014;56:79–89. doi: 10.1016/j.molcel.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Gebert L.F.R., MacRae I.J. Regulation of microRNA function in animals. Nat. Rev. Mol. Cell Biol. 2019;20:21–37. doi: 10.1038/s41580-018-0045-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brummer A., Hausser J. MicroRNA binding sites in the coding region of mRNAs: Extending the repertoire of post-transcriptional gene regulation. Bioessays. 2014;36:617–626. doi: 10.1002/bies.201300104. [DOI] [PubMed] [Google Scholar]
- 11.Cardinali B., Cappella M., Provenzano C., Garcia-Manteiga J.M., Lazarevic D., Cittaro D., Martelli F., Falcone G. MicroRNA-222 regulates muscle alternative splicing through Rbm24 during differentiation of skeletal muscle cells. Cell Death Dis. 2016;7:e2086. doi: 10.1038/cddis.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spengler R.M., Zhang X., Cheng C., McLendon J.M., Skeie J.M., Johnson F.L., Davidson B.L., Boudreau R.L. Elucidation of transcriptome-wide microRNA binding sites in human cardiac tissues by Ago2 HITS-CLIP. Nucleic Acids Res. 2016;44:7120–7131. doi: 10.1093/nar/gkw640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vasudevan S., Steitz J.A. AU-rich-element-mediated upregulation of translation by FXR1 and Argonaute 2. Cell. 2007;128:1105–1118. doi: 10.1016/j.cell.2007.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Truesdell S.S., Mortensen R.D., Seo M., Schroeder J.C., Lee J.H., LeTonqueze O., Vasudevan S. MicroRNA-mediated mRNA Translation Activation in Quiescent Cells and Oocytes Involves Recruitment of a Nuclear microRNP. Sci. Rep. 2012;2:1–12. doi: 10.1038/srep00842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henke J.I., Goergen D., Zheng J., Song Y., Schuttler C.G., Fehr C., Junemann C., Niepmann M. microRNA-122 stimulates translation of hepatitis C virus RNA. Embo J. 2008;27:3300–3310. doi: 10.1038/emboj.2008.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Machlin E.S., Sarnow P., Sagan S.M. Masking the 5′ terminal nucleotides of the hepatitis C virus genome by an unconventional microRNA-target RNA complex. Proc. Natl. Acad. Sci. USA. 2011;108:3193–3198. doi: 10.1073/pnas.1012464108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shimakami T., Yamane D., Jangra R.K., Kempf B.J., Spaniel C., Barton D.J., Lemon S.M. Stabilization of hepatitis C virus RNA by an Ago2-miR-122 complex. Proc. Natl. Acad. Sci. USA. 2012;109:941–946. doi: 10.1073/pnas.1112263109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valinezhad Orang A., Safaralizadeh R., Kazemzadeh-Bavili M. Mechanisms of miRNA-Mediated Gene Regulation from Common Downregulation to mRNA-Specific Upregulation. Int. J. Genom. 2014;2014:970607. doi: 10.1155/2014/970607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orom U.A., Nielsen F.C., Lund A.H. MicroRNA-10a binds the 5’UTR of ribosomal protein mRNAs and enhances their translation. Mol. Cell. 2008;30:460–471. doi: 10.1016/j.molcel.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 20.Tsai N.P., Lin Y.L., Wei L.N. MicroRNA mir-346 targets the 5’-untranslated region of receptor-interacting protein 140 (RIP140) mRNA and up-regulates its protein expression. Biochem. J. 2009;424:411–418. doi: 10.1042/BJ20090915. [DOI] [PubMed] [Google Scholar]
- 21.Schraivogel D., Meister G. Import routes and nuclear functions of Argonaute and other small RNA-silencing proteins. Trends Biochem. Sci. 2014;39:420–431. doi: 10.1016/j.tibs.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Liu H., Lei C., He Q., Pan Z., Xiao D., Tao Y. Nuclear functions of mammalian MicroRNAs in gene regulation, immunity and cancer. Mol. Cancer. 2018;17:64. doi: 10.1186/s12943-018-0765-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schraivogel D., Schindler S.G., Danner J., Kremmer E., Pfaff J., Hannus S., Depping R., Meister G. Importin-β facilitates nuclear import of human GW proteins and balances cytoplasmic gene silencing protein levels. Nucleic Acids Res. 2015;43:7447–7461. doi: 10.1093/nar/gkv705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chaston J.J., Stewart A.G., Christie M. Structural characterisation of TNRC6A nuclear localisation signal in complex with importin-alpha. PLoS ONE. 2017;12:e0183587. doi: 10.1371/journal.pone.0183587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nishi K., Nishi A., Nagasawa T., Ui-Tei K. Human TNRC6A is an Argonaute-navigator protein for microRNA-mediated gene silencing in the nucleus. RNA. 2013;19:17–35. doi: 10.1261/rna.034769.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei Y., Li L., Wang D., Zhang C.Y., Zen K. Importin 8 regulates the transport of mature microRNAs into the cell nucleus. J. Biol. Chem. 2014;289:10270–10275. doi: 10.1074/jbc.C113.541417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hwang H., Wentzel E., Mendell J. A hexanucleotide element directs microRNA nuclear import. Science. 2007;315 doi: 10.1126/science.1136235. [DOI] [PubMed] [Google Scholar]
- 28.Jeffries C.D., Fried H.M., Perkins D.O. Nuclear and cytoplasmic localization of neural stem cell microRNAs. RNA. 2011;17:675–686. doi: 10.1261/rna.2006511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turunen T.A., Roberts T.C., Laitinen P., Väänänen M.-A., Korhonen P., Malm T., Ylä-Herttuala S., Turunen M.P. Changes in nuclear and cytoplasmic microRNA distribution in response to hypoxic stress. Sci. Rep. 2019;9:1–12. doi: 10.1038/s41598-019-46841-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li L.C. Small RNA-Guided Transcriptional Gene Activation (RNAa) in Mammalian Cells. Adv. Exp. Med. Biol. 2017;983:1–20. doi: 10.1007/978-981-10-4310-9_1. [DOI] [PubMed] [Google Scholar]
- 31.Roberts T.C. The MicroRNA Biology of the Mammalian Nucleus. Mol. Ther. Nucleic Acids. 2014;3:e188. doi: 10.1038/mtna.2014.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benhamed M., Herbig U., Ye T., Dejean A., Bischof O. Senescence is an endogenous trigger for microRNA-directed transcriptional gene silencing in human cells. Nat. Cell Biol. 2012;14:266–275. doi: 10.1038/ncb2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miao L., Yao H., Li C., Pu M., Yao X., Yang H., Qi X., Ren J., Wang Y. A dual inhibition: microRNA-552 suppresses both transcription and translation of cytochrome P450 2E1. Biochim. Biophys. Acta. 2016;1859:650–662. doi: 10.1016/j.bbagrm.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 34.Zhang Y., Fan M., Zhang X., Huang F., Wu K., Zhang J., Liu J., Huang Z., Luo H., Tao L., et al. Cellular microRNAs up-regulate transcription via interaction with promoter TATA-box motifs. RNA. 2014;20:1878–1889. doi: 10.1261/rna.045633.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang V., Place R.F., Portnoy V., Wang J., Qi Z., Jia Z., Yu A., Shuman M., Yu J., Li L.C. Upregulation of Cyclin B1 by miRNA and its implications in cancer. Nucleic Acids Res. 2012;40:1695–1707. doi: 10.1093/nar/gkr934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xiao M., Li J., Li W., Wang Y., Wu F., Xi Y., Zhang L., Ding C., Luo H., Li Y., et al. MicroRNAs activate gene transcription epigenetically as an enhancer trigger. RNA Biol. 2017;14:1326–1334. doi: 10.1080/15476286.2015.1112487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim D.H., Saetrom P., Snove O., Jr., Rossi J.J. MicroRNA-directed transcriptional gene silencing in mammalian cells. Proc. Natl. Acad. Sci. USA. 2008;105:16230–16235. doi: 10.1073/pnas.0808830105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gonzalez S., Pisano D.G., Serrano M. Mechanistic principles of chromatin remodeling guided by siRNAs and miRNAs. Cell Cycle. 2008;7:2601–2608. doi: 10.4161/cc.7.16.6541. [DOI] [PubMed] [Google Scholar]
- 39.Zardo G., Ciolfi A., Vian L., Starnes L., Billi M., Racanicchi S., Maresca C., Fazi F., Travaglini L., Noguera N., et al. Polycombs and microRNA-223 regulate human granulopoiesis by transcriptional control of target gene expression. Blood. 2012;119 doi: 10.1182/blood-2011-08-371344. [DOI] [PubMed] [Google Scholar]
- 40.Tan Y., Zhang B., Wu T., Skogerbø G., Zhu X., Guo X., He S., Chen R. Transcriptional inhibiton of Hoxd4 expression by miRNA-10a in human breast cancer cells. BMC Mol. Biol. 2009;10:1–9. doi: 10.1186/1471-2199-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ramchandran R., Chaluvally-Raghavan P. miRNA-Mediated RNA Activation in Mammalian Cells. Adv. Exp. Med. Biol. 2017;983:81–89. doi: 10.1007/978-981-10-4310-9_6. [DOI] [PubMed] [Google Scholar]
- 42.Catalanotto C., Cogoni C., Zardo G. MicroRNA in Control of Gene Expression: An Overview of Nuclear Functions. Int. J. Mol. Sci. 2016;17:1712. doi: 10.3390/ijms17101712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Place R.F., Li L.C., Pookot D., Noonan E.J., Dahiya R. MicroRNA-373 induces expression of genes with complementary promoter sequences. Proc. Natl. Acad. Sci. USA. 2008;105:1608–1613. doi: 10.1073/pnas.0707594105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Majid S., Dar A.A., Saini S., Yamamura S., Hirata H., Tanaka Y., Deng G., Dahiya R. MicroRNA-205-directed transcriptional activation of tumor suppressor genes in prostate cancer. Cancer. 2010;116:5637–5649. doi: 10.1002/cncr.25488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tang R., Li L., Zhu D., Hou D., Cao T., Gu H., Zhang J., Chen J., Zhang C.Y., Zen K. Mouse miRNA-709 directly regulates miRNA-15a/16-1 biogenesis at the posttranscriptional level in the nucleus: Evidence for a microRNA hierarchy system. Cell Res. 2012;22:504–515. doi: 10.1038/cr.2011.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leucci E., Patella F., Waage J., Holmstrom K., Lindow M., Porse B., Kauppinen S., Lund A.H. microRNA-9 targets the long non-coding RNA MALAT1 for degradation in the nucleus. Sci. Rep. 2013;3:2535. doi: 10.1038/srep02535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liang W.C., Fu W.M., Wang Y.B., Sun Y.X., Xu L.L., Wong C.W., Chan K.M., Li G., Waye M.M., Zhang J.F. H19 activates Wnt signaling and promotes osteoblast differentiation by functioning as a competing endogenous RNA. Sci. Rep. 2016;6:20121. doi: 10.1038/srep20121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fasanaro P., Greco S., Lorenzi M., Pescatori M., Brioschi M., Kulshreshtha R., Banfi C., Stubbs A., Calin G.A., Ivan M., et al. An integrated approach for experimental target identification of hypoxia-induced miR-210. J. Biol. Chem. 2009;284:35134–35143. doi: 10.1074/jbc.M109.052779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hansen T.B., Wiklund E.D., Bramsen J.B., Villadsen S.B., Statham A.L., Clark S.J., Kjems J. miRNA-dependent gene silencing involving Ago2-mediated cleavage of a circular antisense RNA. Embo J. 2011;30:4414–4422. doi: 10.1038/emboj.2011.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Allo M., Buggiano V., Fededa J.P., Petrillo E., Schor I., de la Mata M., Agirre E., Plass M., Eyras E., Elela S.A., et al. Control of alternative splicing through siRNA-mediated transcriptional gene silencing. Nat. Struct. Mol. Biol. 2009;16:717–724. doi: 10.1038/nsmb.1620. [DOI] [PubMed] [Google Scholar]
- 51.Ameyar-Zazoua M., Rachez C., Souidi M., Robin P., Fritsch L., Young R., Morozova N., Fenouil R., Descostes N., Andrau J.C., et al. Argonaute proteins couple chromatin silencing to alternative splicing. Nat. Struct. Mol. Biol. 2012;19:998–1004. doi: 10.1038/nsmb.2373. [DOI] [PubMed] [Google Scholar]
- 52.Chi S.W., Zang J.B., Mele A., Darnell R.B. Argonaute HITS-CLIP decodes microRNA-mRNA interaction maps. Nature. 2009;460:479–486. doi: 10.1038/nature08170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Boudreau R.L., Jiang P., Gilmore B.L., Spengler R.M., Tirabassi R., Nelson J.A., Ross C.A., Xing Y., Davidson B.L. Transcriptome-wide discovery of microRNA binding sites in human brain. Neuron. 2014;81:294–305. doi: 10.1016/j.neuron.2013.10.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Castel S.E., Martienssen R.A. RNA interference in the nucleus: Roles for small RNAs in transcription, epigenetics and beyond. Nat. Rev. Genet. 2013;14:100–112. doi: 10.1038/nrg3355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu J., Hu J., Hicks J.A., Prakash T.P., Corey D.R. Modulation of Splicing by Single-Stranded Silencing RNAs. Nucleic Acid Ther. 2015;25:113–120. doi: 10.1089/nat.2014.0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sadakierska-Chudy A., Kostrzewa R.M., Filip M. A comprehensive view of the epigenetic landscape part I: DNA methylation, passive and active DNA demethylation pathways and histone variants. Neurotox. Res. 2015;27:84–97. doi: 10.1007/s12640-014-9497-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sadakierska-Chudy A., Filip M. A comprehensive view of the epigenetic landscape. Part II: Histone post-translational modification, nucleosome level, and chromatin regulation by ncRNAs. Neurotox. Res. 2015;27:172–197. doi: 10.1007/s12640-014-9508-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Feinberg A.P., Vogelstein B. Hypomethylation distinguishes genes of some human cancers from their normal counterparts. Nature. 2020;301:89–92. doi: 10.1038/301089a0. [DOI] [PubMed] [Google Scholar]
- 59.Dai E., Yu X., Zhang Y., Meng F., Wang S., Liu X., Liu D., Wang J., Li X., Jiang W. EpimiR: A database of curated mutual regulation between miRNAs and epigenetic modifications. Database. 2014;2014:bau023. doi: 10.1093/database/bau023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Malumbres M. miRNAs and cancer: An epigenetics view. Mol. Asp. Med. 2013;34:863–874. doi: 10.1016/j.mam.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Memari F., Joneidi Z., Taheri B., Aval S.F., Roointan A., Zarghami N. Epigenetics and Epi-miRNAs: Potential markers/therapeutics in leukemia. Biomed. Pharmacother. 2018;106:1668–1677. doi: 10.1016/j.biopha.2018.07.133. [DOI] [PubMed] [Google Scholar]
- 62.Svoronos A.A., Engelman D.M., Slack F.J. OncomiR or Tumor Suppressor? The Duplicity of MicroRNAs in Cancer. Cancer Res. 2016;76:3666–3670. doi: 10.1158/0008-5472.CAN-16-0359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Oliveto S., Mancino M., Manfrini N., Biffo S. Role of microRNAs in translation regulation and cancer. World J. Biol. Chem. 2017;8:45–56. doi: 10.4331/wjbc.v8.i1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Humphries B., Wang Z., Yang C. MicroRNA Regulation of Epigenetic Modifiers in Breast Cancer. Cancers. 2019;11:897. doi: 10.3390/cancers11070897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Corra F., Agnoletto C., Minotti L., Baldassari F., Volinia S. The Network of Non-coding RNAs in Cancer Drug Resistance. Front. Oncol. 2018;8:327. doi: 10.3389/fonc.2018.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Calin G.A., Croce C.M. MicroRNA signatures in human cancers. Nat. Rev. Cancer. 2006;6:857–866. doi: 10.1038/nrc1997. [DOI] [PubMed] [Google Scholar]
- 67.Carvalho J., van Grieken N.C., Pereira P.M., Sousa S., Tijssen M., Buffart T.E., Diosdado B., Grabsch H., Santos M.A., Meijer G., et al. Lack of microRNA-101 causes E-cadherin functional deregulation through EZH2 up-regulation in intestinal gastric cancer. J. Pathol. 2012;228:31–44. doi: 10.1002/path.4032. [DOI] [PubMed] [Google Scholar]
- 68.Fabbri M., Garzon R., Cimmino A., Liu Z., Zanesi N., Callegari E., Liu S., Alder H., Costinean S., Fernandez-Cymering C., et al. MicroRNA-29 family reverts aberrant methylation in lung cancer by targeting DNA methyltransferases 3A and 3B. Proc. Natl. Acad. Sci. USA. 2007;104:15805–15810. doi: 10.1073/pnas.0707628104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Garzon R., Liu S., Fabbri M., Liu Z., Heaphy C.E., Callegari E., Schwind S., Pang J., Yu J., Muthusamy N., et al. MicroRNA-29b induces global DNA hypomethylation and tumor suppressor gene reexpression in acute myeloid leukemia by targeting directly DNMT3A and 3B and indirectly DNMT1. Blood. 2009;113:6411–6418. doi: 10.1182/blood-2008-07-170589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Amodio N., Rossi M., Raimondi L., Pitari M.R., Botta C., Tagliaferri P., Tassone P. miR-29s: A family of epi-miRNAs with therapeutic implications in hematologic malignancies. Oncotarget. 2015;6:12837–12861. doi: 10.18632/oncotarget.3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lombard A.P., Mooso B.A., Libertini S.J., Lim R.M., Nakagawa R.M., Vidallo K.D., Costanzo N.C., Ghosh P.M., Mudryj M. miR-148a dependent apoptosis of bladder cancer cells is mediated in part by the epigenetic modifier DNMT1. Mol. Carcinog. 2016;55:757–767. doi: 10.1002/mc.22319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Iliopoulos D., Lindahl-Allen M., Polytarchou C., Hirsch H.A., Tsichlis P.N., Struhl K. Loss of miR-200 inhibition of Suz12 leads to polycomb-mediated repression required for the formation and maintenance of cancer stem cells. Mol. Cell. 2010;39:761–772. doi: 10.1016/j.molcel.2010.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ren X., Bai X., Zhang X., Li Z., Tang L., Zhao X., Ren Y., Wei S., Wang Q., Liu C., et al. Quantitative nuclear proteomics identifies that miR-137-mediated EZH2 reduction regulates resveratrol-induced apoptosis of neuroblastoma cells. Mol. Cell Proteom. 2015;14:316–328. doi: 10.1074/mcp.M114.041905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zamani M., Sadeghizadeh M., Behmanesh M., Najafi F. Dendrosomal curcumin increases expression of the long non-coding RNA gene MEG3 via up-regulation of epi-miRs in hepatocellular cancer. Phytomedicine. 2015;22:961–967. doi: 10.1016/j.phymed.2015.05.071. [DOI] [PubMed] [Google Scholar]
- 75.Jiang F., Li Y., Mu J., Hu C., Zhou M., Wang X., Si L., Ning S., Li Z. Glabridin inhibits cancer stem cell-like properties of human breast cancer cells: An epigenetic regulation of miR-148a/SMAd2 signaling. Mol. Carcinog. 2016;55:929–940. doi: 10.1002/mc.22333. [DOI] [PubMed] [Google Scholar]
- 76.Baumann V., Winkler J. miRNA-based therapies: Strategies and delivery platforms for oligonucleotide and non-oligonucleotide agents. Future Med. Chem. 2014;6:1967–1984. doi: 10.4155/fmc.14.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kota J., Chivukula R.R., O’Donnell K.A., Wentzel E.A., Montgomery C.L., Hwang H.W., Chang T.C., Vivekanandan P., Torbenson M., Clark K.R., et al. Therapeutic microRNA delivery suppresses tumorigenesis in a murine liver cancer model. Cell. 2009;137:1005–1017. doi: 10.1016/j.cell.2009.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang Y., Wang Z., Gemeinhart R.A. Progress in MicroRNA Delivery. J. Control. Release. 2013;172:962–974. doi: 10.1016/j.jconrel.2013.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Huang X., Schwind S., Yu B., Santhanam R., Wang H., Hoellerbauer P., Mims A., Klisovic R., Walker A.R., Chan K.K., et al. Targeted delivery of microRNA-29b by transferrin-conjugated anionic lipopolyplex nanoparticles: A novel therapeutic strategy in acute myeloid leukemia. Clin. Cancer Res. 2013;19:2355–2367. doi: 10.1158/1078-0432.CCR-12-3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Beg M.S., Brenner A.J., Sachdev J., Borad M., Kang Y.K., Stoudemire J., Smith S., Bader A.G., Kim S., Hong D.S. Phase I study of MRX34, a liposomal miR-34a mimic, administered twice weekly in patients with advanced solid tumors. Investig. New Drugs. 2017;35:180–188. doi: 10.1007/s10637-016-0407-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Reid G., Kao S., Pavlakis N., Brahmbhatt H., MacDiarmid J., Clarke S., Boyer M., van Zandwijk N. Clinical development of TargomiRs, a miRNA mimic-based treatment for patients with recurrent thoracic cancer. Epigenomics. 2016;8:1079–1085. doi: 10.2217/epi-2016-0035. [DOI] [PubMed] [Google Scholar]
- 82.Wu M.Y., Fu J., Xiao X., Wu J., Wu R.C. MiR-34a regulates therapy resistance by targeting HDAC1 and HDAC7 in breast cancer. Cancer Lett. 2014;354:311–319. doi: 10.1016/j.canlet.2014.08.031. [DOI] [PubMed] [Google Scholar]
- 83.Varambally S., Cao Q., Mani R.S., Shankar S., Wang X., Ateeq B., Laxman B., Cao X., Jing X., Ramnarayanan K., et al. Genomic loss of microRNA-101 leads to overexpression of histone methyltransferase EZH2 in cancer. Science. 2008;322:1695–1699. doi: 10.1126/science.1165395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhu Y., Yu F., Jiao Y., Feng J., Tang W., Yao H., Gong C., Chen J., Su F., Zhang Y., et al. Reduced miR-128 in breast tumor-initiating cells induces chemotherapeutic resistance via Bmi-1 and ABCC5. Clin. Cancer Res. 2011;17:7105–7115. doi: 10.1158/1078-0432.CCR-11-0071. [DOI] [PubMed] [Google Scholar]
- 85.Tang H., Liu P., Yang L., Xie X., Ye F., Wu M., Liu X., Chen B., Zhang L. miR-185 suppresses tumor proliferation by directly targeting E2F6 and DNMT1 and indirectly upregulating BRCA1 in triple-negative breast cancer. Mol. Cancer Ther. 2014;13:3185–3197. doi: 10.1158/1535-7163.MCT-14-0243. [DOI] [PubMed] [Google Scholar]
- 86.Friedman J.M., Liang G., Liu C.C., Wolff E.M., Tsai Y.C., Ye W., Zhou X., Jones P.A. The putative tumor suppressor microRNA-101 modulates the cancer epigenome by repressing the polycomb group protein EZH2. Cancer Res. 2009;69:2623–2629. doi: 10.1158/0008-5472.CAN-08-3114. [DOI] [PubMed] [Google Scholar]
- 87.Wang X., Wu Q., Xu B., Wang P., Fan W., Cai Y., Gu X., Meng F. MiR-124 exerts tumor suppressive functions on the cell proliferation, motility and angiogenesis of bladder cancer by fine-tuning UHRF1. FEBS J. 2015;282:4376–4388. doi: 10.1111/febs.13502. [DOI] [PubMed] [Google Scholar]
- 88.Guo Y., Ying L., Tian Y., Yang P., Zhu Y., Wang Z., Qiu F., Lin J. miR-144 downregulation increases bladder cancer cell proliferation by targeting EZH2 and regulating Wnt signaling. FEBS J. 2013;280:4531–4538. doi: 10.1111/febs.12417. [DOI] [PubMed] [Google Scholar]
- 89.Matsushita R., Yoshino H., Enokida H., Goto Y., Miyamoto K., Yonemori M., Inoguchi S., Nakagawa M., Seki N. Regulation of UHRF1 by dual-strand tumor-suppressor microRNA-145 (miR-145-5p and miR-145-3p): Inhibition of bladder cancer cell aggressiveness. Oncotarget. 2016;7:28460–28487. doi: 10.18632/oncotarget.8668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhu M., Xu Y., Ge M., Gui Z., Yan F. Regulation of UHRF1 by microRNA-9 modulates colorectal cancer cell proliferation and apoptosis. Cancer Sci. 2015;106:833–839. doi: 10.1111/cas.12689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ng E.K., Tsang W.P., Ng S.S., Jin H.C., Yu J., Li J.J., Rocken C., Ebert M.P., Kwok T.T., Sung J.J. MicroRNA-143 targets DNA methyltransferases 3A in colorectal cancer. Br. J. Cancer. 2009;101:699–706. doi: 10.1038/sj.bjc.6605195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang H., Wu J., Meng X., Ying X., Zuo Y., Liu R., Pan Z., Kang T., Huang W. MicroRNA-342 inhibits colorectal cancer cell proliferation and invasion by directly targeting DNA methyltransferase 1. Carcinogenesis. 2011;32:1033–1042. doi: 10.1093/carcin/bgr081. [DOI] [PubMed] [Google Scholar]
- 93.Konno Y., Dong P., Xiong Y., Suzuki F., Lu J., Cai M., Watari H., Mitamura T., Hosaka M., Hanley S.J., et al. MicroRNA-101 targets EZH2, MCL-1 and FOS to suppress proliferation, invasion and stem cell-like phenotype of aggressive endometrial cancer cells. Oncotarget. 2014;5:6049–6062. doi: 10.18632/oncotarget.2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yu X., Jiang X., Li H., Guo L., Jiang W., Lu S.H. miR-203 inhibits the proliferation and self-renewal of esophageal cancer stem-like cells by suppressing stem renewal factor Bmi-1. Stem Cells Dev. 2014;23:576–585. doi: 10.1089/scd.2013.0308. [DOI] [PubMed] [Google Scholar]
- 95.Cui H., Wang L., Gong P., Zhao C., Zhang S., Zhang K., Zhou R., Zhao Z., Fan H. Deregulation between miR-29b/c and DNMT3A is associated with epigenetic silencing of the CDH1 gene, affecting cell migration and invasion in gastric cancer. PLoS ONE. 2015;10:e0123926. doi: 10.1371/journal.pone.0123926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhou L., Zhao X., Han Y., Lu Y., Shang Y., Liu C., Li T., Jin Z., Fan D., Wu K. Regulation of UHRF1 by miR-146a/b modulates gastric cancer invasion and metastasis. FASEB J. 2013;27:4929–4939. doi: 10.1096/fj.13-233387. [DOI] [PubMed] [Google Scholar]
- 97.Yan J., Guo X., Xia J., Shan T., Gu C., Liang Z., Zhao W., Jin S. MiR-148a regulates MEG3 in gastric cancer by targeting DNA methyltransferase 1. Med. Oncol. 2014;31:879. doi: 10.1007/s12032-014-0879-6. [DOI] [PubMed] [Google Scholar]
- 98.Ren J., Huang H.J., Gong Y., Yue S., Tang L.M., Cheng S.Y. MicroRNA-206 suppresses gastric cancer cell growth and metastasis. Cell Biosci. 2014;4:26. doi: 10.1186/2045-3701-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Godlewski J., Nowicki M.O., Bronisz A., Williams S., Otsuki A., Nuovo G., Raychaudhury A., Newton H.B., Chiocca E.A., Lawler S. Targeting of the Bmi-1 oncogene/stem cell renewal factor by microRNA-128 inhibits glioma proliferation and self-renewal. Cancer Res. 2008;68:9125–9130. doi: 10.1158/0008-5472.CAN-08-2629. [DOI] [PubMed] [Google Scholar]
- 100.Peruzzi P., Bronisz A., Nowicki M.O., Wang Y., Ogawa D., Price R., Nakano I., Kwon C.H., Hayes J., Lawler S.E., et al. MicroRNA-128 coordinately targets Polycomb Repressor Complexes in glioma stem cells. Neuro Oncol. 2013;15:1212–1224. doi: 10.1093/neuonc/not055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nohata N., Hanazawa T., Kinoshita T., Inamine A., Kikkawa N., Itesako T., Yoshino H., Enokida H., Nakagawa M., Okamoto Y., et al. Tumour-suppressive microRNA-874 contributes to cell proliferation through targeting of histone deacetylase 1 in head and neck squamous cell carcinoma. Br. J. Cancer. 2013;108:1648–1658. doi: 10.1038/bjc.2013.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Braconi C., Huang N., Patel T. MicroRNA-dependent regulation of DNA methyltransferase-1 and tumor suppressor gene expression by interleukin-6 in human malignant cholangiocytes. Hepatology. 2010;51:881–890. doi: 10.1002/hep.23381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhang J., Yang Y., Yang T., Liu Y., Li A., Fu S., Wu M., Pan Z., Zhou W. microRNA-22, downregulated in hepatocellular carcinoma and correlated with prognosis, suppresses cell proliferation and tumourigenicity. Br. J. Cancer. 2010;103:1215–1220. doi: 10.1038/sj.bjc.6605895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Noh J.H., Chang Y.G., Kim M.G., Jung K.H., Kim J.K., Bae H.J., Eun J.W., Shen Q., Kim S.J., Kwon S.H., et al. MiR-145 functions as a tumor suppressor by directly targeting histone deacetylase 2 in liver cancer. Cancer Lett. 2013;335:455–462. doi: 10.1016/j.canlet.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 105.Yuan J.H., Yang F., Chen B.F., Lu Z., Huo X.S., Zhou W.P., Wang F., Sun S.H. The histone deacetylase 4/SP1/microrna-200a regulatory network contributes to aberrant histone acetylation in hepatocellular carcinoma. Hepatology. 2011;54:2025–2035. doi: 10.1002/hep.24606. [DOI] [PubMed] [Google Scholar]
- 106.Garzon R., Heaphy C.E., Havelange V., Fabbri M., Volinia S., Tsao T., Zanesi N., Kornblau S.M., Marcucci G., Calin G.A., et al. MicroRNA 29b functions in acute myeloid leukemia. Blood. 2009;114:5331–5341. doi: 10.1182/blood-2009-03-211938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Li Y., Gao L., Luo X., Wang L., Gao X., Wang W., Sun J., Dou L., Li J., Xu C., et al. Epigenetic silencing of microRNA-193a contributes to leukemogenesis in t(8;21) acute myeloid leukemia by activating the PTEN/PI3K signal pathway. Blood. 2013;121:499–509. doi: 10.1182/blood-2012-07-444729. [DOI] [PubMed] [Google Scholar]
- 108.Nishioka C., Ikezoe T., Yang J., Nobumoto A., Tsuda M., Yokoyama A. Downregulation of miR-217 correlates with resistance of Ph(+) leukemia cells to ABL tyrosine kinase inhibitors. Cancer Sci. 2014;105:297–307. doi: 10.1111/cas.12339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Shen J.Z., Zhang Y.Y., Fu H.Y., Wu D.S., Zhou H.R. Overexpression of microRNA-143 inhibits growth and induces apoptosis in human leukemia cells. Oncol. Rep. 2014;31:2035–2042. doi: 10.3892/or.2014.3078. [DOI] [PubMed] [Google Scholar]
- 110.Yu T., Li J., Yan M., Liu L., Lin H., Zhao F., Sun L., Zhang Y., Cui Y., Zhang F., et al. MicroRNA-193a-3p and -5p suppress the metastasis of human non-small-cell lung cancer by downregulating the ERBB4/PIK3R3/mTOR/S6K2 signaling pathway. Oncogene. 2015;34:413–423. doi: 10.1038/onc.2013.574. [DOI] [PubMed] [Google Scholar]
- 111.Sander S., Bullinger L., Klapproth K., Fiedler K., Kestler H.A., Barth T.F., Moller P., Stilgenbauer S., Pollack J.R., Wirth T. MYC stimulates EZH2 expression by repression of its negative regulator miR-26a. Blood. 2008;112:4202–4212. doi: 10.1182/blood-2008-03-147645. [DOI] [PubMed] [Google Scholar]
- 112.Liu S., Tetzlaff M.T., Cui R., Xu X. miR-200c inhibits melanoma progression and drug resistance through down-regulation of BMI-1. Am. J. Pathol. 2012;181:1823–1835. doi: 10.1016/j.ajpath.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Neo W.H., Yap K., Lee S.H., Looi L.S., Khandelia P., Neo S.X., Makeyev E.V., Su I.H. MicroRNA miR-124 controls the choice between neuronal and astrocyte differentiation by fine-tuning Ezh2 expression. J. Biol. Chem. 2014;289:20788–20801. doi: 10.1074/jbc.M113.525493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Althoff K., Beckers A., Odersky A., Mestdagh P., Koster J., Bray I.M., Bryan K., Vandesompele J., Speleman F., Stallings R.L., et al. MiR-137 functions as a tumor suppressor in neuroblastoma by downregulating KDM1A. Int. J. Cancer. 2013;133:1064–1073. doi: 10.1002/ijc.28091. [DOI] [PubMed] [Google Scholar]
- 115.Das S., Foley N., Bryan K., Watters K.M., Bray I., Murphy D.M., Buckley P.G., Stallings R.L. MicroRNA mediates DNA demethylation events triggered by retinoic acid during neuroblastoma cell differentiation. Cancer Res. 2010;70:7874–7881. doi: 10.1158/0008-5472.CAN-10-1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zhang D., Ni Z., Xu X., Xiao J. MiR-32 functions as a tumor suppressor and directly targets EZH2 in human oral squamous cell carcinoma. Med. Sci. Monit. 2014;20:2527–2535. doi: 10.12659/msm.892636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bhattacharya R., Nicoloso M., Arvizo R., Wang E., Cortez A., Rossi S., Calin G.A., Mukherjee P. MiR-15a and MiR-16 control Bmi-1 expression in ovarian cancer. Cancer Res. 2009;69:9090–9095. doi: 10.1158/0008-5472.CAN-09-2552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xiang Y., Ma N., Wang D., Zhang Y., Zhou J., Wu G., Zhao R., Huang H., Wang X., Qiao Y., et al. MiR-152 and miR-185 co-contribute to ovarian cancer cells cisplatin sensitivity by targeting DNMT1 directly: A novel epigenetic therapy independent of decitabine. Oncogene. 2014;33:378–386. doi: 10.1038/onc.2012.575. [DOI] [PubMed] [Google Scholar]
- 119.Azizi M., Teimoori-Toolabi L., Arzanani M.K., Azadmanesh K., Fard-Esfahani P., Zeinali S. MicroRNA-148b and microRNA-152 reactivate tumor suppressor genes through suppression of DNA methyltransferase-1 gene in pancreatic cancer cell lines. Cancer Biol. Ther. 2014;15:419–427. doi: 10.4161/cbt.27630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Xue G., Ren Z., Chen Y., Zhu J., Du Y., Pan D., Li X., Hu B. A feedback regulation between miR-145 and DNA methyltransferase 3b in prostate cancer cell and their responses to irradiation. Cancer Lett. 2015;361:121–127. doi: 10.1016/j.canlet.2015.02.046. [DOI] [PubMed] [Google Scholar]
- 121.Noonan E.J., Place R.F., Pookot D., Basak S., Whitson J.M., Hirata H., Giardina C., Dahiya R. miR-449a targets HDAC-1 and induces growth arrest in prostate cancer. Oncogene. 2009;28:1714–1724. doi: 10.1038/onc.2009.19. [DOI] [PubMed] [Google Scholar]
- 122.Goto Y., Kurozumi A., Nohata N., Kojima S., Matsushita R., Yoshino H., Yamazaki K., Ishida Y., Ichikawa T., Naya Y., et al. The microRNA signature of patients with sunitinib failure: Regulation of UHRF1 pathways by microRNA-101 in renal cell carcinoma. Oncotarget. 2016;7:59070–59086. doi: 10.18632/oncotarget.10887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang H., Garzon R., Sun H., Ladner K.J., Singh R., Dahlman J., Cheng A., Hall B.M., Qualman S.J., Chandler D.S., et al. NF-kappaB-YY1-miR-29 regulatory circuitry in skeletal myogenesis and rhabdomyosarcoma. Cancer Cell. 2008;14:369–381. doi: 10.1016/j.ccr.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Chen B.F., Suen Y.K., Gu S., Li L., Chan W.Y. A miR-199a/miR-214 self-regulatory network via PSMD10, TP53 and DNMT1 in testicular germ cell tumor. Sci. Rep. 2014;4:6413. doi: 10.1038/srep06413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Roccaro A.M., Sacco A., Jia X., Azab A.K., Maiso P., Ngo H.T., Azab F., Runnels J., Quang P., Ghobrial I.M. microRNA-dependent modulation of histone acetylation in Waldenstrom macroglobulinemia. Blood. 2010;116:1506–1514. doi: 10.1182/blood-2010-01-265686. [DOI] [PMC free article] [PubMed] [Google Scholar]