Abstract
Approximately 13,500 children each year are treated for non-powder gun injuries of which approximately one-quarter of these injuries are puncture wounds. Although rare, vascular migration of the bullet or pellet (otherwise known as the “wandering bullet”) may result in downstream organ damage secondary to vascular or venous occlusion, most commonly travelling anterograde and lodging within the lung venous system. Interestingly, we present a case of a 12-year-old female who was shot in the neck with a compressed-air gun loaded with ball-bearing pellets. Eventual retrograde vascular migration of the ball-bearing pellet from the right internal jugular vein to the hepatic vein caused hepatic venous occlusion and congestion. It is important for radiologists to remember the possibility of retrograde travel of bullets and pellets, and radiographs should be scrutinized for foreign bodies present in areas other than the region of injury. Bullet retrieval is determined by clinical evaluation and necessity, and if indicated, endovascular, percutaneous retrieval, or surgical exploration may be considered.
Keywords: Foreign bodies, Foreign-body migration, Embolization, Bullet embolism, Pediatric radiology, Emergency radiology
Introduction
Intravascular migration of foreign bodies, such as bullets or other projectiles, is a rare (0.3%) phenomenon wherein a penetrating missile (ie, bullet or pellet) forms an embolus from the initial area of a penetrating injury to a separate part of the body via the vasculature [1]. We present a case in which a pediatric patient was shot in the right anterior neck with a ball-bearing (BB) pellet gun and the pellet migrated from the right internal jugular vein to the hepatic vein leading to subsequent hepatic venous occlusion and congestion.
Case report
A 12-year-old female with no past medical history was brought to the emergency department (ED) by emergency medical technicians as a level 1 trauma activation for a gunshot wound to the right neck. The patient was involved in an altercation which led to another individual shooting the patient with a BB gun. At the time of injury, the patient was standing and subsequently fell onto her back after she was shot by the individual standing in front of her. Upon presentation to the ED, she was ambulatory but was asked to remain on the stretcher as a precautionary measure to the unknown extent of her possible injuries. Physical exam was significant for a 2-millimeter puncture wound along the anterior right neck without evidence of active bleeding or obvious hematoma formation. No other neck wound, including an exit site, was present. A review of systems was non-contributory.
Routine trauma-activation anteroposterior radiographs of the thorax demonstrated a metallic density projecting over the right hepatic lobe (Figs. 1A and B). Further imaging with computed tomography of the abdomen with contrast and delayed imaging showed the same metallic density within the right hepatic lobe segment 7, within a segmental right hepatic vein. Hypoattenuating areas were also seen in segments 6 and 7 (Figs. 2A-C). These areas were thought to represent edema and congestion secondary to venous obstruction. No active contrast extravasation or perihepatic fluid were identified. There was no evidence of an exit wound in the neck, chest, or abdominal wall.
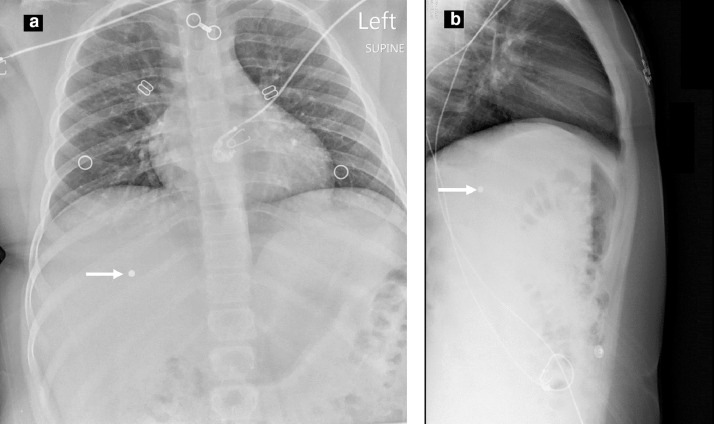
Fig. 1.
Supine anteroposterior (a) and cross-table left-lateral (b) radiographs of the thorax in the emergency department demonstrate a metallic-density focus overlying the right hepatic lobe (white arrows).
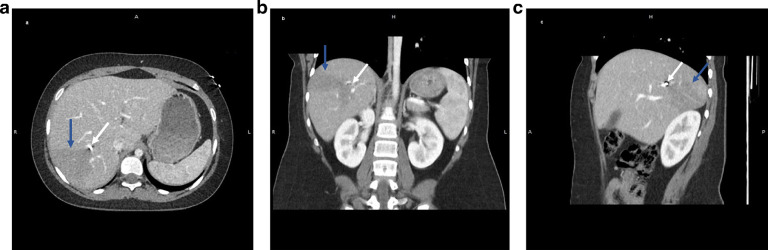
Fig. 2.
Axial (a), coronal (b), and sagittal (c) CT images of the abdomen demonstrate a metallic density foreign body (white arrows) within the right hepatic lobe. There is a wedge-shaped hypodense region distal to the foreign body (blue arrows). (Color version is available online.)
Interventional radiology was consulted for possible retrieval of the foreign body within the liver. Possible options included transvenous or percutaneous removal of the BB. Due to the significant risk of the BB migrating to more critical structures during the retrieval procedure, such as the heart, lung, or kidneys, it was agreed to manage the patient conservatively with serial radiographs. Should any sign of further migration of the BB occur, then removal and/or retrieval would be reconsidered.
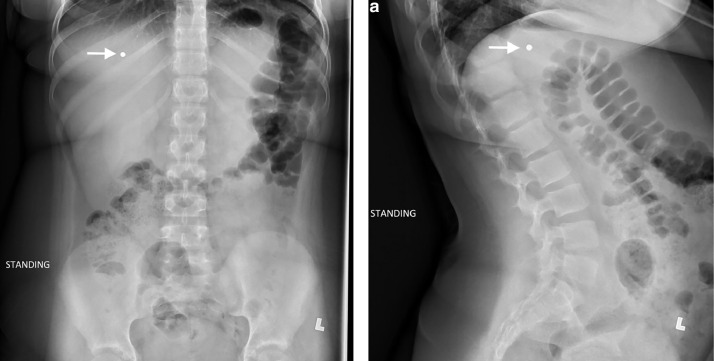
Serial abdominal radiographs over a year, spaced out monthly and eventually every 3 months, have consistently shown a stable position of the BB pellet within the right hepatic lobe (Fig. 3, Fig. 4, Fig 5). The patient remains asymptomatic.
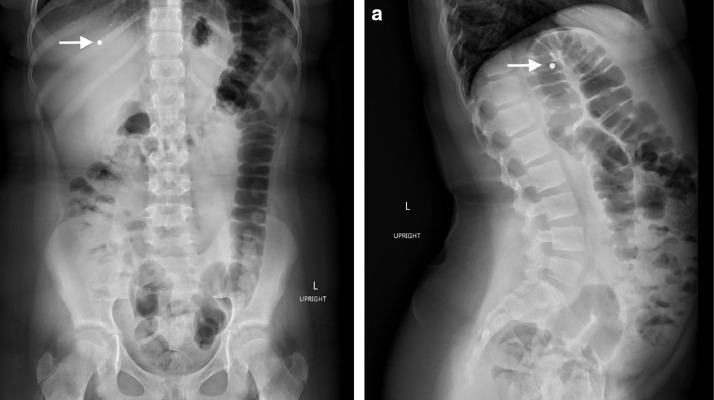
Fig. 3.
One-month follow-up upright anteroposterior (a) and left-lateral radiographs of the abdomen demonstrate stable position of the BB pellet, which overlies the right hepatic lobe (white arrows).
Fig. 4.
Six-month follow up upright anteroposterior (a) and left-lateral radiographs of the abdomen demonstrate stable position of the BB pellet, which overlies the right hepatic lobe (white arrows).
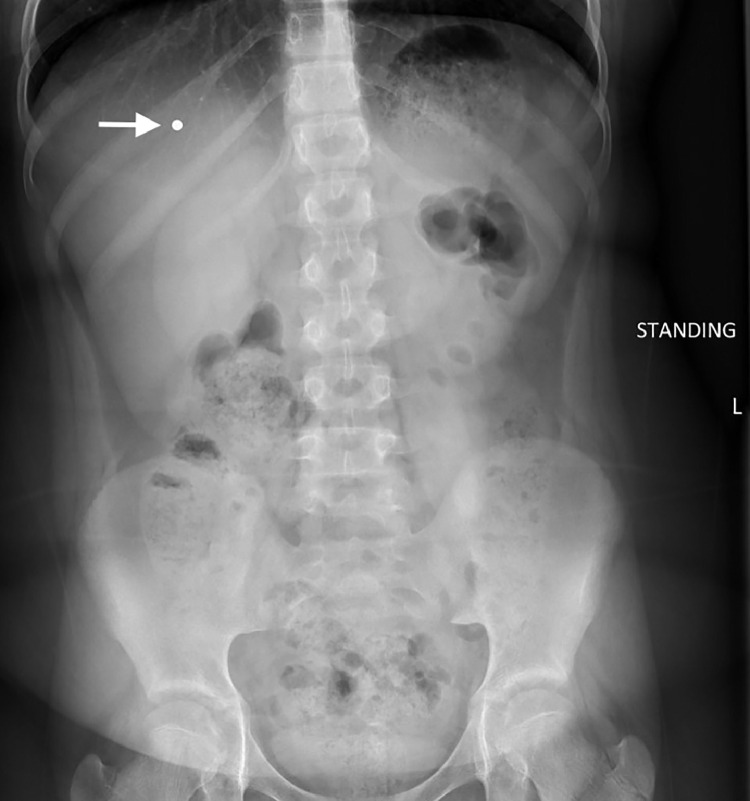
Fig 5.
Twelve-month follow up upright anteroposterior radiograph of the abdomen demonstrate stable position of the BB pellet, which overlies the right hepatic lobe (white arrows).
Discussion
Approximately 13,500 children are treated annually in United States EDs for injuries related to non-powder guns [2]. Most Injuries occurred between the ages of 6- to 12-years old (47.4%) and 13- to 17-years-old (47.0%). BB compressed air power guns were the most common cause (87.1%) [2]. Injuries vary significantly depending on the body region injured, nonpowder gun used, and age of the patient. The head and neck area are one of the most commonly injured body regions [2]. Among BB gun injuries, approximately 24.1% are puncture wounds [2].
Typically, BB gun pellets range in size from 4.5 mm to 6 mm in diameter, with a mass of approximately 0.2 grams [8]. Depending on the type of gun use, whether spring- or pneumatic-type, the velocity of the projectile can range from 82.5 m/s to 136 m/s. In contrast, the velocity of a bullet from a firearm is at least 227 m/s [9]; the variation in projectile velocity depends on the gun used, leading to the differentiation of projectiles into “low kinetic” energy and “high kinetic” energy. Projectiles with low kinetic energy, such as BB gun pellets, have the propensity to pass through soft tissue structures and only pierce 1 vessel wall, which results in the projectile stalling within the lumen of the vessel.
While vascular migration of pellets is a rare event, retrograde venous pellet migration and subsequent embolization is even less reported in literature [1,3]. It is estimated that only 15% of pellet that undergo vascular migration move retrograde, with gravity as the proposed underlying mechanism [4].
Pellet embolization should be considered if an exit wound is not seen on physical examination, the location of the projectile is located in an area that is inconsistent with its missile trajectory, or absence of radiologic evidence of the pellet in the expected area. The suspicion should be heightened with low-velocity, small-caliber gunshot wounds. Evaluation of vasculature and organs downstream of the entry point is critical; this can be easily accomplished with a skeletal survey set of radiographs. Projectiles that enter the venous system will often migrate antegrade to the right ventricle and/or pulmonary arterial system which may subsequently result in a pulmonary embolism [5]. However, in this patient, the BB pellet migrated both antegrade from the internal jugular vein into the right atrial lumen and, surprisingly, retrograde into the relatively straight and short inferior vena cava (IVC), before further embolizing into a segmental hepatic vein. Although uncertain, this instance of bullet migration may also be secondary to a relatively “straight path” from the respective ostium of the SVC and IVC via the right atrial lumen. The retrograde trajectory of the BB pellet through the right atrium into the IVC suggests that the bullet was merely following gravity as it travelled caudally.
Management of a suspected pellet emboli will depend on the patient's hemodynamic stability and location of the foreign body. This typically begins with radiologic imaging to determine the pellet location and, if needed, determine the best approach for pellet retrieval. Radiographs of the abdomen and chest will be valuable in order to quickly assess for a metallic foreign body. Suspicion for a “wandering bullet” should be raised if a metallic foreign body is projecting over the body in a region other than the area of the injury seen on the physical exam. Further assessment of the specific location of the embolized pellet will require cross-sectional imaging with contrast, if possible. Computed tomography is typically chosen for its short examination time, which is especially relevant if the patient is not hemodynamically stable and requires immediate intervention.
Specifically, in this case, the BB pellet was determined to likely have been lodged in a segmental hepatic vein. Complications of this event include venous occlusion leading to hepatic congestion. The increased sinusoidal pressures secondary to the occluded venous system may eventually lead to infarction of the hepatic segment; this will occur if the sinusoidal pressures surpass the hepatic arterial and portal venous perfusion pressure [7]. Therefore, it is imperative to consider a method of foreign body retrieval where the benefits will outweigh the risks of the procedure.
Despite a unified consensus on the decision to retrieve projectile foreign bodies, most authors generally recommend conservative management in asymptomatic cases and to use thorough clinical evaluation to determine if retrieval is necessary [6]. If pellet or bullet retrieval is clinically indicated, percutaneous extraction should be considered, though emergency surgical exploration will often be necessary [6]. As in our patient who had evidence of hepatic congestion, the decision for intervention was deemed necessary. Given the location of the BB pellet within the right lobe of the liver, it was felt that an endovascular approach would be most beneficial. However, this procedure proved to be technically difficult due to the location of the BB pellet within a segmental hepatic vein. Furthermore, the risk of BB pellet embolization to a more critical structure during retrieval outweighed the assumed benefit of the endovascular procedure. Therefore, it was decided to manage the patient conservatively with serial abdominal radiographs.
Conclusion
Pellets or bullets, especially those with low kinetic energy, may embolize via intravascular migration. Most projectiles migrate through anterograde flow through the arteries, but approximately 15% move retrograde through the venous system, thought to be due to gravity. Bullet retrieval is determined by clinical evaluation and necessity. If intervention is indicated, endovascular or percutaneous retrieval or surgical exploration may be used.
Ethics approval
This is a retrospective case report not requiring ethics approval.
Consent to participate All patient data has been removed and not informed consent is required to participate.
Consent for publication
All patient data has been removed and not informed consent is required to publish.
Availability of data and materials
Not applicable.
Code availability
Not applicable.
Authors’ contribution
All authors contributed to writing the manuscript. All authors read and approved the final manuscript.
Footnotes
Funding: No funding was received to assist with the preparation of this manuscript.
Competing interests: The authors declare that they have no conflict of interest.
REFERENCES
- 1.Rich NM, Collins GJ, Jr, Andersen CA, McDonald PT, Kozloff L, Ricotta JJ. Missile emboli. J Trauma. 1978;18(4):236–239. doi: 10.1097/00005373-197804000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Jones M, Kistamgari S, Smith GA. Nonpowder firearm injuries to children treated in emergency departments. Pediatrics. 2019;144(6) doi: 10.1542/peds.2019-2739. [DOI] [PubMed] [Google Scholar]
- 3.Bertoldo U, Enrichens F, Comba A, Ghiselli G, Vaccarisi S, Ferraris M. Retrograde venous bullet embolism: a rare occurrence-case report and literature review. J Trauma. 2004;57(1):187–192. doi: 10.1097/01.ta.0000135490.10227.5c. [DOI] [PubMed] [Google Scholar]
- 4.Bertoldo U, Enrichens F, Comba A, Ghiselli G, Vaccarisi S, Ferraris M. Retrograde venous bullet embolism: a rare occurrence-case report and literature review. J Trauma. 2004;57(1):187–192. doi: 10.1097/01.ta.0000135490.10227.5c. [DOI] [PubMed] [Google Scholar]
- 5.Nolan T, Phan H, Hardy AH, Khanna P, Dong P. Bullet embolization: multidisciplinary approach by interventional radiology and surgery. Semin Intervent Radiol. 2012;29(3):192–196. doi: 10.1055/s-0032-1326928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pereira RM, Souza JEDS, de Araújo AO, et al. Arterial bullet embolism after thoracic gunshot wound [published correction appears in J Vasc Bras. 2018 Jul-Sep;17(3):273]. J Vasc Bras. 2018;17(3):262-266. doi:10.1590/1677-5449.005315 [DOI] [PMC free article] [PubMed]
- 7.Mills A., Mellnick V. Imaging features of hepatic arterial and venous flow abnormalities. Clin Liver Dis. 2018;11:27–32. doi: 10.1002/cld.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laraque D. American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Injury risk of nonpowder guns. Pediatrics. 2004;114(5):1357–1361. doi: 10.1542/peds.2004-1799. [DOI] [PubMed] [Google Scholar]
- 9.Tsui C, Tsui K, Tang Y. Ball Bearing (BB) Gun Injuries. Hong Kong J Emerg Med. 2010;17(5):488–491. doi: 10.1177/102490791001700510. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.