Abstract
The pandemic caused by the coronavirus disease of 2019 (COVID-19) challenged primary care providers (PCPs) to continue to deliver care for their patients, while also remaining financially stable. Most practices have experienced declining revenue due to fewer in-person patient visits. To help offset this and to continue to provide safe patient care, practices have shifted toward using remote options. Chronic Care Management (CCM) and Remote Patient Monitoring (RPM) are benefits available to Medicare fee-for-service patients, which allow a medical practice to deliver expanded care and generate much-needed revenue. These services can be delivered by clinical staff called care managers. A top health priority for most seniors is to effectively self-isolate to reduce risk of COVID-19, while maintaining mental and physical health. We developed a Safe at Home program, designed to be run by care managers through CCM and RPM, with the use of a remote monitoring technology. Safe at Home tracks signs and symptoms of COVID-19, mental and physical health, and lifestyle behaviors that can affect immune function. We project that this service can complement regular telehealth PCP visits and deliver population health monitoring services, while generating substantial revenue for the practice.
Keywords: COVID-19, elderly, remote physiologic monitoring, primary care, lifestyle medicine
‘As the patient answers questions, the Care Manager monitors incoming answers in a real-time dashboard provided by our Remote Patient Monitoring vendor.’
The coronavirus pandemic of 2019 (COVID-19) resulted in many primary care providers (PCPs) wanting to help their patients stay safe from this deadly disease, yet feeling as if they had few services to offer. Payment models and primary care workflows have traditionally been set up to address medical problems in person, on a one-on-one basis. Due to the need to socially distance and isolate, elderly patients have felt disconnected from their doctor offices and wary of the customary in-person office visits.
The most vulnerable from COVID-19 are the elderly,1-3 particularly those with chronic conditions. In the setting of this pandemic, Medicare permitted telehealth visits through a video connection.4 While such telehealth visits can enable a primary care practitioner to reach their at-risk population more easily, it still requires one-on-one visits by the provider, and thus limited reach to the larger patient population. Many of these elderly lack social support and require more careful guidance and monitoring than can be provided by the occasional one-on-one PCP visit.
Fortunately, Medicare Fee-for-Service offers 2 programs that permit a PCP to employ clinical staff and monitoring technology to deliver day-to-day monitoring and connection with their seniors. Chronic Care Management (CCM) has been offered since 2015,5 and reimburses roughly $40 per month for clinical staff members to spend 20 or more minutes per month managing at least 2 chronic conditions. When clinical staff spend 40, 60, or more minutes, reimbursement scales accordingly (Table 1). Our practice has used CCM effectively since 2018 to deliver valuable, intimate care and also generate significant revenue above costs.
Table 1.
Chronic Care Management (CCM) Billing Codes.
| Billing code | Requirements |
|---|---|
| Code G0506 = ~$63Comprehensive assessment of and care planning by the physician or other qualified health care professional for patients requiring chronic care management services. | Practitioners who furnish a CCM initiating visit and personally perform extensive assessment and CCM care planning outside of the usual effort described by the initiating visit code may also bill HCPCS code G0506Billable once per CCM billing practitioner, in conjunction with CCM initiation |
| Code 99490 = ~$42Chronic care management services, at least 20 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month | Multiple (2 or more) chronic conditions expected to last at least 12 months, or until the death of the patientChronic conditions place the patient at significant risk of death, acute exacerbation/decompensation, or functional decline |
| Code G2058 = ~$37Each additional 20 minutes of clinical staff time in CCM | Must have billed 99490Billable a maximum of twice per monthCovers minutes 21-60 |
| Code 99487 = ~$93Complex chronic care management services, at least 60 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month | Alternative to 99490; may not bill bothModerate or high complexity medical decision making |
| Code 99489 = ~$46Each additional 30 minutes of clinical staff time in Complex CCM | Must also bill 99487 that monthMay be billed multiple times |
Remote Patient Monitoring (RPM) is a newer Medicare provision,6 which reimburses a medical practice to monitor physiologic data such as vital signs (blood pressure, heart rate, body weight). RPM similarly requires 20 minutes of staff time per month in reviewing the monitored data and reimburses roughly $120 per month (Table 2). Thus, RPM could be regarded as a technology-enriched monitoring service, with almost 3 times the reimbursement rate relative to CCM. RPM typically requires the use of a technology vendor to provide the monitoring device. Such vendors use a variety of technologies to collect data. Examples include pedometer watches, Bluetooth scales, or blood pressure monitors. These devices frequently connect through a smartphone to transmit the data to a central server. The RPM vendor will typically offer a dashboard for clinical staff, which they can use to view the incoming data in real time.
Table 2.
Remote Patient Monitoring (RPM) Billing Codes.a
| Billing code | Requirements |
|---|---|
| Code 99453 = ~$21Set-up and patient education on use of remote monitoring equipment | Billable one time |
| Code 99454 = ~$69Device(s) supply with daily recording(s) or programmed alert(s) transmission, each 30 days | Billable once per 30 daysPatient must have and be able to use the device for at least 16 days in the calendar month |
| Code 99457 = ~$5320 minutes or more of clinical staff/physician/other qualified health care professional time in a calendar month requiring interactive communication with the patient/caregiver during the month | Billable once per 30 daysPatient must have and be able to use the device for at least 16 days in the calendar month |
| Code 99458 = ~$43Additional 20 minutes or more of clinical staff/physician/other qualified health care professional time | Must also have billed 99457Billable once per 30 days |
RPM requires remote monitoring of physiologic parameter(s) (eg, weight, blood pressure, pulse oximetry, respiratory flow rate).
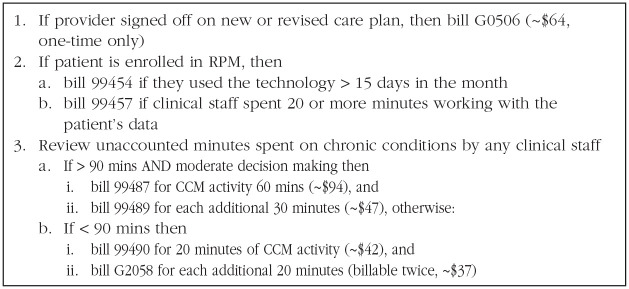
Both CCM and RPM may be delivered by a care manager, who can be a medical assistant, nurse, or other health professional. A care manager typically is assigned a panel of patients to manage. The care manager reviews incoming information such as requests from the patient or provider. The care manager addresses any concern, and will frequently speak with their patients, to gather information, provide counseling, or relay provider messages. The care manager must document their activities and track time spent for RPM and CCM. If 20 minutes were reached, the care manager submits a bill to Centers for Medicare & Medicaid Services (CMS) for the service. Figure 1 summarizes a simple algorithm to bill Medicare for RPM and CCM services, while maximizing revenue.
Figure 1.
Simplified billing algorithm for a patient on CCM and/or RPM. Follow this practice at the end of each month, when you review your log of time spent for each patient.
COVID-19
Due to the COVID-19 pandemic, millions of seniors attempted to practice isolation at home in order to minimize their risk of this deadly disease. Significant fear and uncertainty arose about what isolation practices were most important to follow, which symptoms to take seriously, and when to go to seek acute care. This created an opportunity for PCPs to help these individuals follow best practices and ensure safety. In March of 2020, our practice rolled out a program designed to accomplish this, which we called Safe at Home.
Safe at Home employed our care managers providing both CCM and RPM. Our RPM vendor7 provided COVID-specific monitoring and information, which helped automate much of the provision of key information to patients. Our Care Manager helped patients enroll in the program over the phone. The RPM onboarding process involved installing a free smartphone app on the patient’s device. The patient was then asked to use the app to do a Daily Check-in, which collected temperature and signs and symptoms of illness (Table 3). The Safe at Home program further tried to engage patients to track their mental and physical health (Table 4), and the healthy lifestyle factors which may influence their immune function and overall health (Table 5).
Table 3.
Daily Check-In Questions for COVID-19 Safety.
| Question | Care manager response |
|---|---|
| What is your temperature? | If >100.0 °F, alert provider. |
| Do you have any of these symptoms? 1. Fever or feeling feverish (chills, sweating) 2. Shortness of breath 3. Cough 4. Runny or stuffy nose 5. Sore throat 6. Muscle aches, body aches, or headache 7. Tiredness or fatigue 8. Nausea, vomiting, or diarrhea 9. Loss of sense of taste or smell10. Other concerning symptoms |
If 1-3, schedule for telehealth appointment with provider. If any other, follow up with patient directly. |
| How many people total did you come into contact with (Within 6 feet for more than a few minutes)? 1. Just me 2. The same people who live with me 3. Unknown 4. Too many to count |
If #3 or #4, explore ways to reduce the number. |
| Can you reduce the number of people you come into close contact with tomorrow? | Consolidate trips, infrequent outings. Can someone do their shopping for them? |
| How many times did you wash or disinfect your hands immediately after touching things that may have been touched by others? 1. Every time 2. Sometimes 3. Occasionally 4. I do not clean my hands regularly |
Recommend that they clean their hands 100% of the time. When possible, avoid touching anything touched by others. |
| When going out, do you wear a mask? 1. I do not go out 2. Always 3. Sometimes 4. Never |
If #3 or #4, explore ways to get a mask for them to use. |
Table 4.
Daily Check-In Questions for Measuring Mental and Physical Health.
| Question | Care manager response |
|---|---|
| How connected do you feel with any support network (eg, community, spiritual, friends/family, nature, yoga, or meditation)? | If not connected, explore ways of finding connection. Virtual social groups? Memberships? Old friends? More frequent calls with family? |
| Do you feel . . . 1. Anxious? 2. Depressed? 3. Sad? 4. Lonely? 5. Scared? 6. In pain? 7. Tired? 8. Sick? |
Explore the source of the ill feelings. Recommend telehealth visit with provider to address. |
| Do you feel . . . 1. Calm? 2. Happy? 3. At peace? 4. Loved? 5. Confident? 6. Free of pain? 7. Energetic? 8. Healthy? |
Explore the positive things going on in their life. Can any of these be built upon? Repeat the behaviors that elicited the positive feelings? |
| On a scale of 0 to 10, where 10 is the healthiest you can be, how healthy do you feel now? | If the number has declined or is below 5, explore further. |
| Do you have any medical concerns that your provider should know about? If so, what are they? | Pass concerning problems on to provider. |
Table 5.
Daily Check-In Questions for Behaviors Affecting Immune Function.
| Question | Care manager response |
|---|---|
| How many hours did you sleep last night? | Goal is 7-8. If less than 6, do sleep hygiene assessment and counseling. |
| How many alcohol-containing beverages did you consume in the last day? | If >0, recommend abstain from alcohol to maximize immune function. |
| Do you smoke? | If yes, counsel to quit. |
| How many fruits and vegetables servings do you consume per day? | Goal is 10 or more. |
| How many minutes of moderate intensity exercise (where you can talk but not sing) did you get in the last day? | Goal is 25+ minutes per day, to get to 150 minutes per week. Also patients should do resistance training at least twice per week. |
Normally, RPM requires measurement of a traditional vital sign and thus requires the patient to be set up with a smart monitoring device (such as a Bluetooth blood pressure cuff, glucose meter, scale, heart rate monitor). In the setting of the COVID-19 pandemic, CMS recognized that RPM can play a role in remote monitoring for COVID-19 symptoms and progression.8 CMS modified some rules regarding RPM, to allow its use on new patients who have not yet been established with the medical practice. They also clarified that RPM can be used for acute and chronic conditions.
An advantage of deploying RPM for monitoring for COVID-19 safety is that a key vital sign to monitor is body temperature. Patients can easily monitor temperature using a low-cost thermometer. They can then manually enter that information in their smartphone. Thus, we believe that RPM can be conducted for COVID-19 surveillance using the patient’s smartphone alone, without an additional smart monitoring device. This reduces time and cost to the practice to set up RPM, allowing a Safe at Home program to be scaled up rapidly.
As the patient answers questions, the Care Manager monitors incoming answers in a real-time dashboard provided by our RPM vendor. The patient alerts the provider to change in clinical status or other concerns. The Care Manager reaches out to the patient as needed to collect more information, or provide targeted counseling for less acute concerns.
When a patient begins to manifest symptoms concerning for COVID-19 or other respiratory illness, the care manager asks questions to track these signs and symptoms (Table 6). In higher acuity cases, care managers ensure that the provider is aware of the patient’s clinical status, and checks frequently on the patient through the app, the telephone, or other means. The technology can help them more easily identify who needs closer monitoring and who does not.
Table 6.
| Question | Care manager response |
|---|---|
| What is your pulse oximeter reading? | Notify provider at least daily |
| Which of these conditions do you have? 1. Age >60 2. Diabetes mellitus 3. Hypertension 4. Immunosuppression 5. Heart disease 6. Lung disease |
If one or more of these, the patient is at increased risk, and is higher risk of needing hospitalization. |
| How do you feel today relative to yesterday? 1. Better 2. The Same 3. Worse |
Any worsening raises concern that the patient may need to be evaluated promptly. Have the provider contact the patient directly if they report getting worse. |
| Is there someone who checks on you several times per day? | Recommend that a healthy individual check on you and attend to your needs at least several times per day. Ideally this person should wear a mask and live in an isolated part of your home. |
| How much have you been able to isolate yourself from others who do not have COVID in your house? 1. Completely 2. Mostly 3. Partially 4. Not much |
We recommend complete isolation from all other people, other than a single caregiver to check on you several times per day. You should be under strict self-quarantine. Explore ways to achieve this with the patient. |
It is expected that the provider be involved with these patients on a daily basis.
It is not entirely clear from CMS policy, however, if the manual entry of a thermometer reading into a HIPAA-compliant RPM smartphone app qualifies as remote monitoring. Our interpretation is that it is billable, especially in the setting of the COVID crisis, and given that Bluetooth-enabled thermometers are not generally available. It is possible that CMS will not agree now or in the future that such manual entry is billable under RPM.
Under a stricter interpretation of CMS billing policy around RPM, it is still possible to bill for RPM in the setting of COVID. Our office distributed pedometer watches to some of our Safe at Home participants, which allow us to monitor heart rate, pedometer steps, and sleep. Also, a Bluetooth-enabled pulse oximeter could be used.
A program similar to Safe at Home can be administered without a smartphone or RPM vendor. In such cases, the care manager can deliver the monitoring questions (summarized in Tables 3–6) manually, and bill the CCM codes, provided the patient has given consent to CCM and that CCM conditions are met (ie, time is spent managing 2 or more chronic conditions).
Financial Rewards
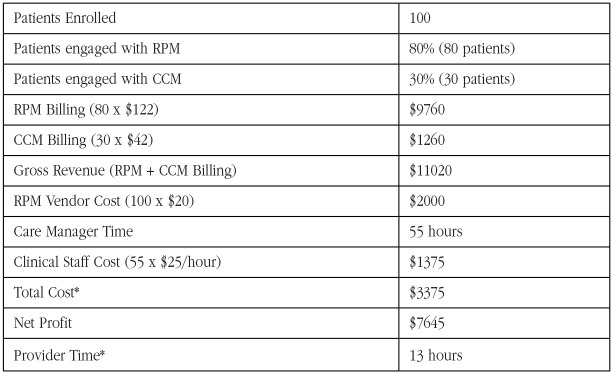
Another challenge presented by the COVID-19 pandemic is the financial solvency of medical practices. While most practices have switched to mostly telehealth encounters, overall volume of patients (and consequent reimbursement) have dropped significantly. Most practices need a source of revenue to make up for falling revenue from clinical encounters. Fortunately, CCM and RPM offer significant rewards. Monthly revenue projections are summarized in Figure 2. In a given month, for a panel of 100 patients enrolled in Safe at Home, one or more care managers can manage these patients in about 55 hours. We estimate that the provider will need to spend an average of 10 minutes per active participant per month, or a modest 13 hours for this panel of 100. Assuming the ability to bill RPM for 80% of enrollees and CCM in 30% of enrollees in a given month, gross revenue generated is approximately $11 020. Personnel costs come to approximately $1375 (not including provider time), and RPM vendors typically cost approximately $20 per patient per month, or $2000 for this example panel. In this specific example, revenue is approximately $7645 for the month, after covering cost of care manager time.
Figure 2.
Monthly revenue projections for a Safe at Home RPM + CCM program with 100 enrollees.
*The cost of a Provider’s time is not included in the Total Cost.
Conclusion
We conclude that running a Safe at Home program can be financially rewarding, generating significant revenue for a medical practice at a time of declining revenue, while delivering a valuable service to patients in this time of crisis.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
References
- 1. Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Infect. 2020;80:e14-e18. doi: 10.1016/j.jinf.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. doi: 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. CDC COVID-19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:382-386. doi: 10.15585/mmwr.mm6913e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Medicare & Medicaid Services. Medicare telemedicine health care provider fact sheet. Published March 17, 2020. Accessed April 4, 2020 https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- 5. Moore KJ. Chronic care management and other new CPT codes. Fam Pract Manag. 2015;22:7-12. [PubMed] [Google Scholar]
- 6. Centers for Medicare & Medicaid Services. Medicare and Medicaid programs. Policy and regulatory revisions in response to the COVID-19 public health emergency. Federal Register. Published April 6, 2020. Accessed April 4, 2020 https://www.federalregister.gov/d/2020-06990
- 7. Carium. Accessed April 4, 2020 https://www.carium.com/
- 8. Centers for Medicare & Medicaid Services. CMS takes action to modernize Medicare home health. Published October 31, 2018. Accessed April 4, 2020 https://www.cms.gov/newsroom/press-releases/cms-takes-action-modernize-medicare-home-health-0
- 9. World Health Organization. Home care for patients with COVID-19 presenting with mild symptoms and management of their contacts. Published March 17, 2020. Accessed April 4, 2020 https://www.who.int/publications-detail/home-care-for-patients-with-suspected-novel-coronavirus-(ncov)-infection-presenting-with-mild-symptoms-and-management-of-contacts