Abstract
Background
Acute heart failure (AHF) usually requires urgent therapy. Myocardial damage, oxidative stress, and inflammation are major components in the pathology of AHF. This study was designed to investigate the effects of chrysophanol on AHF.
Material/Methods
Sprague-Dawley rats were injected with isoprenaline hydrochloride to construct AHF rat models. AHF rats were treated with normal saline (negative control), chrysophanol, the combination of chrysophanol and SP600125, or benazepril (positive control) using sham rats as blank controls. Echocardiography, histological staining, and enzyme activity analysis were performed to assess the heart functions and myocardial damage. Effects on apoptosis, oxidative stress (OS), and inflammation were evaluated by biochemical analysis, TUNEL staining, and ELISA.
Results
Chrysophanol improved the parameters of cardiac functions and alleviated the myocardial damage accompanied by the reduction of creatine kinase and lactate dehydrogenase activity. Meanwhile, chrysophanol inhibited the myocardial apoptosis along with the upregulation of Bcl-2 and downregulation of Bax and cleaved caspase-3. AHF-induced abnormal changes of OS parameters (MDA, GPx, CAT, SOD) and inflammatory markers (IL-6, IL-1β, TNF-α, IFN-γ) were alleviated by chrysophanol. Benazepril treatment showed similar results with chrysophanol, while the addition of SP600125 enhanced the chrysophanol-mediated protection effects in AHF rats. Western blot analysis demonstrated that chrysophanol inhibited the phosphorylation of JNK1/2 and its upstream/downstream factors.
Conclusions
Chrysophanol improved cardiac functions and protected against myocardial damage, apoptosis, OS, and inflammation by inhibiting activation of the JNK1/2 pathway in AHF rat models. These finding indicate that chrysophanol may be a promising approach for treatment of AHF.
MeSH Keywords: Apoptosis, Cardiomyopathies, Heart Failure
Background
Acute heart failure (AHF) is broadly defined as a gradual or rapid change in signs and symptoms of heart failure, resulting in a need for urgent therapy [1]. It is often a potentially life-threatening condition, associated with high mortality and morbidity rates [2]. Notably, AHF usually leads to repeated hospitalizations, emerging as a significant and growing health care problem worldwide [3]. The predominate therapeutic strategy for AHF is mostly symptomatic, centered on use of decongestive drugs, mainly diuretics supplemented by vasodilators or inotropes [4]. Although existing treatments substantially improve the clinical course and prognosis of AHF patients, treatment has not changed in recent decades, with no treatments showing improvement in outcomes [5]. As a consequence, there is an urgent need to discover novel therapeutic drugs and to understand the molecular mechanisms of drug action in AHF to improve long-term outcomes.
AHF can be caused by a variety of different pathophysiological mechanisms [6]. In addition to the abnormal hemodynamics of AHF patients, the myocardial injury is related to a decrease in coronary perfusion and/or further activation of neurohormones and renal dysfunction, which probably contributes to short-term and post-discharge cardiac events in AHF patients [7]. In addition, numerous heart failure studies have suggested that inflammatory and immune system activation are associated with the pathogenesis and outcome of AHF [8–10]. AHF therapy should not only to improve symptoms and hemodynamics, but also prevent myocardial damage, modulate neurohormonal and inflammatory activation, and improve renal function [11].
Chrysophanol, a member of the anthraquinone family, is a plant-derived herbal drug that is well known for its strong anti-inflammatory, anti-mutagenic, anti-microbial, hepatoprotective, and anti-carcinogenic activities [12,13]. Emerging evidence demonstrates that chrysophanol can alleviate the development of cardiovascular complications, such as diabetic cardiomyopathy [14], doxorubicin-induced cardiotoxicity [15], and isoproterenol-induced cardiac hypertrophy [16]. These pre-clinical studies have suggested the potential therapeutic value of chrysophanol in treating cardiac disease. More importantly, chrysophanol is reported to have protective effects against diabetic myocardial injury [17]. Thus, we hypothesized that the anti-inflammatory and myocardial-protective activities of chrysophanol could be applied in AHF treatment. To the best of our knowledge, the present study is the first to demonstrate the effects of chrysophanol on progression of AHF. This study was designed to elucidate the underlying effects of chrysophanol on AHF rats and to explore its molecular mechanisms of action.
Material and Methods
Animal and treatments
The protocol for this study was approved by Ethics Committee of Inner Mongolia Medical University Affiliated Hospital. All animal experiments were conducted in accordance with NIH guidelines (Guide for the Care and Use of Laboratory Animals). Fifty male Sprague-Dawley (SD) rats (weighing 200±20 g) were purchased from the Shanghai National Center for Laboratory Animals (Shanghai, China) and housed in a specific-pathogen-free, temperature- (25±2°C) and humidity-controlled environment (60±5% humidity) with a 12-h light/dark cycle and a standard diet.
All rats were randomly assigned to receive the isoprenaline hydrochloride (ISO) injection or equivalent saline (sham group, n=10). The rats were injected subcutaneously in the right thigh with ISO dissolved in 0.9% normal saline (85 mg/kg of body weight) for 2 consecutive days, at an interval of 24 h, to induce AHF. Real-time echocardiography was performed to evaluate the successful construction of the AHF model. Rats whose maximum rate of rise of left ventricular pressure (+LVdP/dtmax) decreased to less than 2/3 of the normal value and maintained for more than 5 min without ascending tendency were diagnosed with AHF. Then, the rats in the sham group were treated with normal saline and the AHF rats were randomly divided into 4 groups (each group, n=10) and intraperitoneally injected for 4 weeks with chrysophanol (0.1 mg/kg/day, Seebio Biotech, China), the chrysophanol (0.1 mg/kg/day) combined with SP600125 (50 mg/kg/day, Sigma-Aldrich, USA), benazepril (10 mg/kg/day, Novartis Pharma, China), or normal saline (AHF group). Benazepril was used as a positive control for intervention. After 4 weeks of treatment, rats were anesthetized or sacrificed under approved protocols, then the blood samples and myocardial tissues were collected and stored at −80°C until later use.
Cardiac functions examination
Rats were anesthetized with 1.5–2% isoflurane under approved protocols, and echocardiography of the heart was performed to evaluate the cardiac functions of rats. Left ventricular peak systolic pressure (LVPSP), left ventricular end-diastolic pressure (LVEDP), and maximum rate of rise and fall of left ventricular pressure (+LVdP/dtmax and −LVdP/dtmax) were calculated and recorded.
Tissue harvesting and hematoxylin and eosin (H&E) staining
Rats were sacrificed using CO2 under approved protocols, and a sample of left ventricular (LV) myocardial tissue was obtained for subsequent experiments. Tissues were fixed with paraformaldehyde (4%) for 2 h, embedded in paraffin for sectioning, and cut to 5-μm thickness. Then, paraffin-embedded sections were stained with H&E according to the standard protocol. Cross-sectional areas of cardiomyocytes were calculated using Cell^A software (Olympus Soft Imaging Solutions GmbH, Germany) under a microscope (Olympus Deutschland GmbH, Germany).
Enzyme activity and biochemical analysis of myocardial tissues
Activity analysis of creatine kinase-myoglobin (CK-MB) and lactate dehydrogenase (LDH) in myocardial tissues was performed using the commercially available Creatine Kinase Activity Assay Kit and LDH Assay Kit (Abcam, USA) according to the manufacturer’s instructions. We used the Malondialdehyde (MDA) Assay Kit, Glutathione Peroxidase (GPx) Assay Kit, Catalase (CAT) Activity Assay Kit, and Superoxide Dismutase (SOD) Activity Assay Kit purchased from Abcam to measure the levels of MDA, GPx, CAT, and SOD, following the manufacturer’s instructions.
Terminal deoxynucleotidyl transferase dUTP nick-end labeling (TUNEL) staining
Myocardial cell apoptosis was measured by TUNEL assay using a commercially available In Situ Cell Death Detection Kit (Roche Diagnostics, Germany). Briefly, paraffin-embedded sections were deparaffinized in xylene and rehydrated in graded alcohol, followed by incubation with 3% H2O2 for 10 min to block endogenous peroxidase activity. Then, sections were pretreated with proteinase K for 20 min at room temperature and labeled with TdT (50 μl) and biotinylated dUTP (450 μl) followed by treatment with TUNEL reagent (50 μl). Washed sections were incubated with peroxidase-labeled streptavidin for 30 min and then stained with diaminobenzidine (DAB). Finally, sections were counterstained with hematoxylin and visualized under a light microscope (Olympus Deutschland GmbH, Germany). The TUNEL-positive cells were counted using ImageJ software (National Institutes of Health, USA).
Western blotting assay
Western blotting was performed following the standard protocol. Total protein was extract from myocardial tissues using RIPA lysis buffer (ThermoFisher Scientific, Wilmington, USA). Equal amounts of proteins (20 μg) of each sample were loaded on 5–12% SDS-polyacrylamide gel for electrophoresis. Then, the proteins were transferred to a polyvinylidene fluoride (PVDF) membrane. PVDF membranes were blocked with 5% skim milk for 1 h at room temperature and probed overnight at 4°C with antibodies against Bcl-2 (dilution 1/2000), Bax (dilution 1/2000), p38 (dilution 1/2000), phospho-p38 (p-p38, dilution 1/1000), ERK1/2 (dilution 1/1000), p-ERK1/2 (dilution 1/1000), JNK1/2 (dilution 1/1000), p-JNK1/2 (dilution 1/1000), MEKK1 (dilution 1/1000), p-MEKK1 (dilution 1/1000), MEK4 (dilution 1/1000), p-MEK4 (dilution 1/1000), c-Jun (dilution 1/1000), p-c-Jun (dilution 1/1000), or GADPH (dilution 1/1000). Corresponding HRP-conjugated IgG antibodies were used as a secondary antibody and incubated for 1 h at room temperature. Finally, the signals were developed with a SuperSignal Protein Detection kit (Pierce Biotechnology, USA). Band intensity was quantified subsequent to normalization with the density of GAPDH using ImageJ software (National Institutes of Health, USA).
Enzyme-linked immunosorbent assay (ELISA)
Rats were sacrificed under approved protocols and blood was obtained by cardiac puncture. The serum levels of interleukin-6 (IL-6), IL-1β, tumor necrosis factor-α (TNF-α), and interferon-γ (IFN-γ) were analyzed by ELISA. ELISA was performed in accordance with the standard protocol using the commercial assay kits from R&D Systems. We used the Mouse IL-6 Quantikine ELISA Kit, Mouse IL-1 beta/IL-1F2 Quantikine ELISA Kit, Mouse TNF-alpha Quantikine ELISA Kit, and Mouse IFN-gamma Quantikine ELISA Kit.
Statistical analysis
Data are expressed as mean±standard error of mean (SEM) of at least 3 separate experiments. The statistical differences among multi-groups were analyzed by one-way ANOVA with Dunn’s least significant difference tests. The statistical analysis was performed by GraphPad PRISM (version 7.0; GraphPad Software, USA). Differences between groups were considered significant at p<0.05.
Results
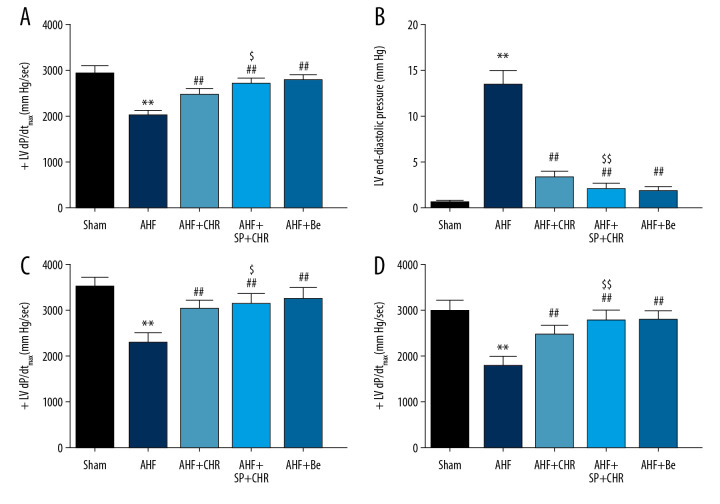
Chrysophanol improved the cardiac functions in AHF rats
As shown in Figure 1, the LVPSP, +LVdP/dtmax and −LVdP/dtmax of AHF rats were significantly decreased compared with that of sham rats, while LVEDP showed the opposite result, indicating the impairment of heart function in AHF rats. As expected, both chrysophanol and benazepril obviously enhanced the LVPSP, +LVdP/dtmax, and −LVdP/dtmax of AHF rats (Figure 1A, 1C, 1D) and reduced the LVEDP (Figure 1B), compared with the untreated AHF rats. These results demonstrated that chrysophanol improved the heart functions in AHF rats. Notably, SP600125 (a JNK inhibitor) showed a synergistic effect with chrysophanol, which further enhanced the chrysophanol-induced protective effects on heart function in AHF rats (Figure 1). Taken together, these results showed that chrysophanol could significantly improve the heart functions of AHF rats.
Figure 1.
Chrysophanol improved the heart functions in AHF rats. AHF rat models were constructed using Sprague-Dawley rats that then received different treatments. Echocardiography of the heart was performed to evaluate the heart functions. (A) Left ventricular peak systolic pressure; (B) Left ventricular end-diastolic pressure; (C) Maximum rate of rise of left ventricular pressure; (D) Maximum rate of fall of left ventricular pressure. Each experiment was repeated 3 times. Data are expressed as mean±SEM. * p<0.05, ** p<0.01 vs. sham; # p<0.05, ## p<0.01 vs. AHF; $ p<0.05, $$ p<0.01 vs. AHF+CHR. AHF – acute heart failure; CHR – chrysophanol; SP – SP600125; Be – benazepril.
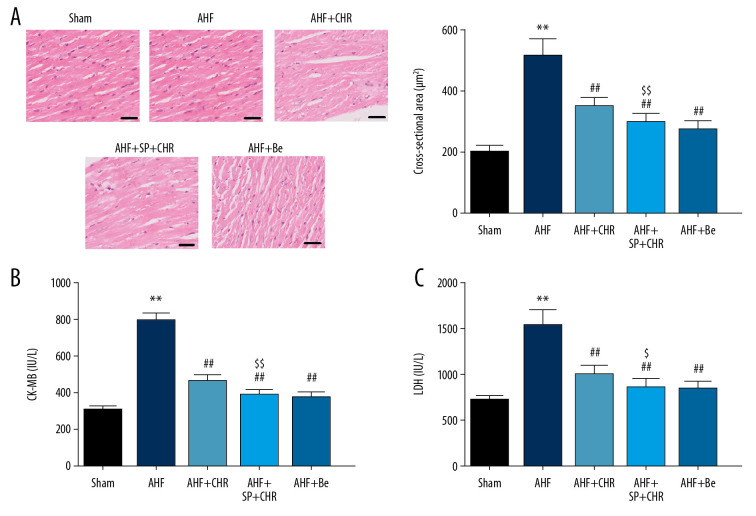
Chrysophanol alleviated the myocardial damage in AHF rats
As shown in Figure 2A, AHF rats showed obvious myocardial damage accompanied by increased cross-sectional area of cardiomyocytes compared with the sham group. Notably, both chrysophanol and benazepril obviously inhibited the cross-sectional area of cardiomyocytes compared to AHF rats without treatments. SP600125 further decreased the chrysophanol-induced reduction of the cross-sectional area of cardiomyocytes.
Figure 2.
Chrysophanol improved the myocardial damage in AHF rats. After various treatments, rats were sacrificed and myocardial tissues were obtained. (A) Hematoxylin and eosin staining was performed to evaluate the pathological damage and cross-sectional areas of cardiomyocyte were calculated. Scale bar: 100 μm. (B) Creatine kinase-myoglobin (CK-MB) activity and (C) lactate dehydrogenase (LDH) activity analysis in myocardial tissues was assessed using commercially available kits. Each experiment was repeated 3 times. Data are expressed as mean±SEM. * p<0.05, ** p<0.01 vs. sham; # p<0.05, ## p<0.01 vs. AHF; $ p<0.05, $$ p<0.01 vs. AHF+CHR. AHF – acute heart failure; CHR – chrysophanol; SP – SP600125; Be – benazepril.
With regard to the CK-MB and LDH activity, we observed that the increases of CK-MB and LDH activity in AHF rats were both significantly reduced by the chrysophanol and benazepril treatment (Figure 2B, 2C). In addition, the chrysophanol-induced reduction of CK-MB and LDH activity was obviously suppressed by SP600125 compared with AHF rats treated with chrysophanol (Figure 2B, 2C). Taken together, these results showed that the myocardial damage of AHF rats was alleviated by chrysophanol treatment.
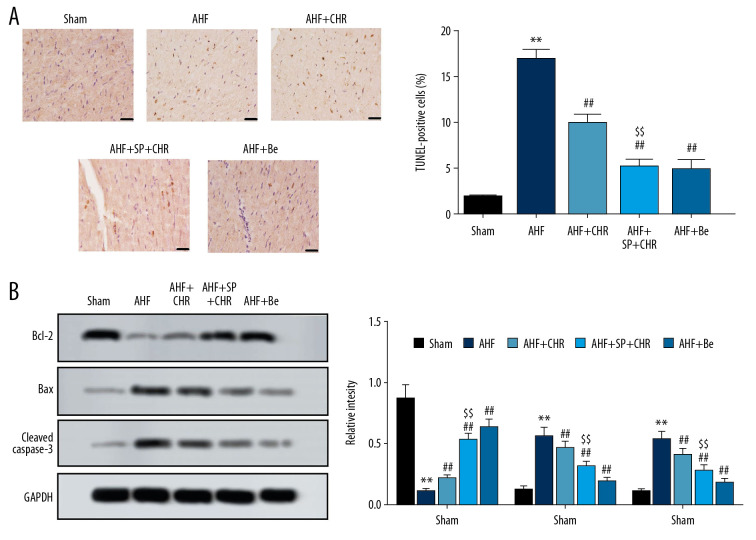
Chrysophanol inhibited myocardial apoptosis in AHF rats
Figure 3A and 3B show that the numbers of TUNEL-positive cells were significantly increased in the AHF rats, along with Bax and cleaved caspase-3 upregulation and Bcl-2 downregulation, compared with the sham group, which was obviously reversed by the chrysophanol and benazepril treatment. Moreover, SP600125 combined with chrysophanol treatment further decreased numbers of TUNEL-positive cells and the expression levels of Bax and cleaved caspase-3, but increased the expression levels of Bcl-2, compared with chrysophanol alone treatment (Figure 3A, 3B). Taken together, these results show that the chrysophanol treatment significantly inhibited myocardial apoptosis in AHF rats.
Figure 3.
Chrysophanol inhibited the myocardial apoptosis in AHF rats. After various treatments, rats were sacrificed and myocardial tissues were obtained. (A) TUNEL staining was performed to evaluate myocardial apoptosis, and TUNEL-positive cells were counted. Scale bar: 100 μm. (B) The expression levels of apoptosis-related proteins were analyzed using western blot. Each experiment was repeated 3 times. Data are expressed as mean±SEM. * p<0.05, ** p<0.01 vs. sham; # p<0.05, ## p<0.01 vs. AHF; $ p<0.05, $$ p<0.01 vs. AHF+CHR. AHF – acute heart failure; CHR – chrysophanol; SP – SP600125; Be – benazepril.
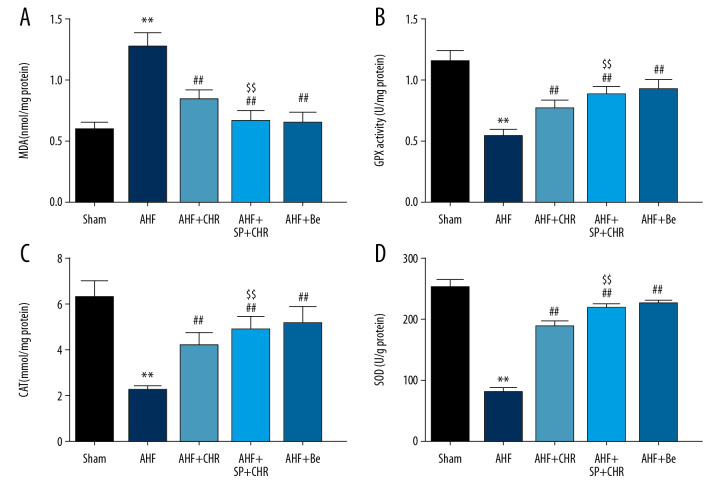
Chrysophanol alleviated oxidative stress in AHF rats
The MDA was enhanced in the AHF rats (Figure 4A), while the activity of GPx (Figure 4B), CAT (Figure 4C), and SOD (Figure 4D) were decreased compared to the sham group. Furthermore, the changes in MDA, GPx activity, CAT, and SOD were all reversed by chrysophanol or benazepril treatment. The addition of SP600125 in chrysophanol further promoted the improvement of chrysophanol in OS (Figure 4). Taken together, these results showed that treatment with chrysophanol alleviated OS in AHF rats.
Figure 4.
Chrysophanol alleviated the oxidative stress in AHF rats. After various treatment, rats were sacrificed and myocardial tissues were obtained. (A) MDA, (B) GPx, (C) CAT Activity, and (D) SOD Activity were detected. Each experiment was repeated 3 times. Data are expressed as mean±SEM. * p<0.05, ** p<0.01 vs. sham; # p<0.05, ## p<0.01 vs. AHF; $ p<0.05, $$ p<0.01 vs. AHF+CHR. AHF – acute heart failure; CHR – chrysophanol; SP – SP600125; Be – benazepril; MDA – malondialdehyde; GPx – glutathione peroxidase; CAT – catalase; SOD – superoxide dismutase.
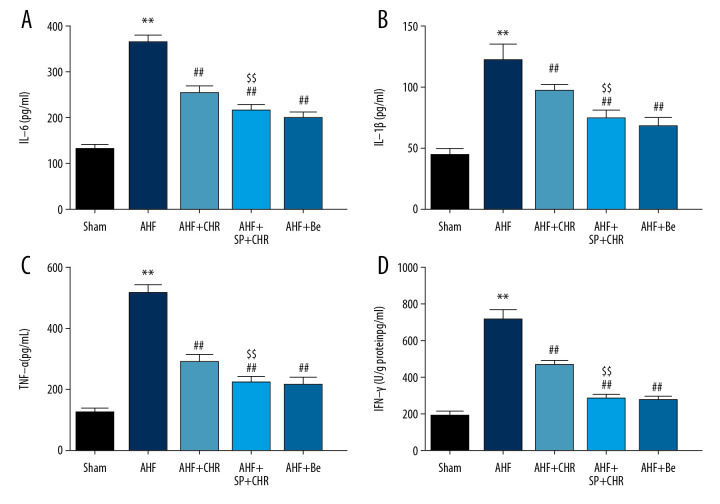
Chrysophanol alleviated inflammation in AHF rats
As shown in Figure 5A, the level of IL-6 was significantly enhanced in AHF rats, which was reversed by the chrysophanol or benazepril treatment. SP600125 facilitated the chrysophanol-induced reduction of IL-6 levels (Figure 5A). Not surprisingly, the levels of IL-1β (Figure 5B), TNF-α (Figure 5C) and IFN-γ (Figure 5D) showed change trends totally consistent with the results of IL-6 after corresponding treatment. Overall, the results showed that chrysophanol alleviated inflammation in AHF rats.
Figure 5.
Chrysophanol alleviated the inflammation in AHF rats. After various treatment, rats were sacrificed and blood samples were collected. (A) IL-6, (B) IL-1β, (C) TNF-α, and (D) IFN-γ levels were analyzed by ELISA. Each experiment was repeated 3 times. Data are expressed as mean±SEM. * p<0.05, ** p<0.01 vs. sham; # p<0.05, ## p<0.01 vs. AHF; $ p<0.05, $$ p<0.01 vs. AHF+CHR. AHF – acute heart failure; CHR – chrysophanol; SP – SP600125; Be – benazepril; IL-6 – interleukin-6; IL-1β – interleukin-1β; TNF-α – tumor necrosis factor-α; IFN-γ – interferon-γ.
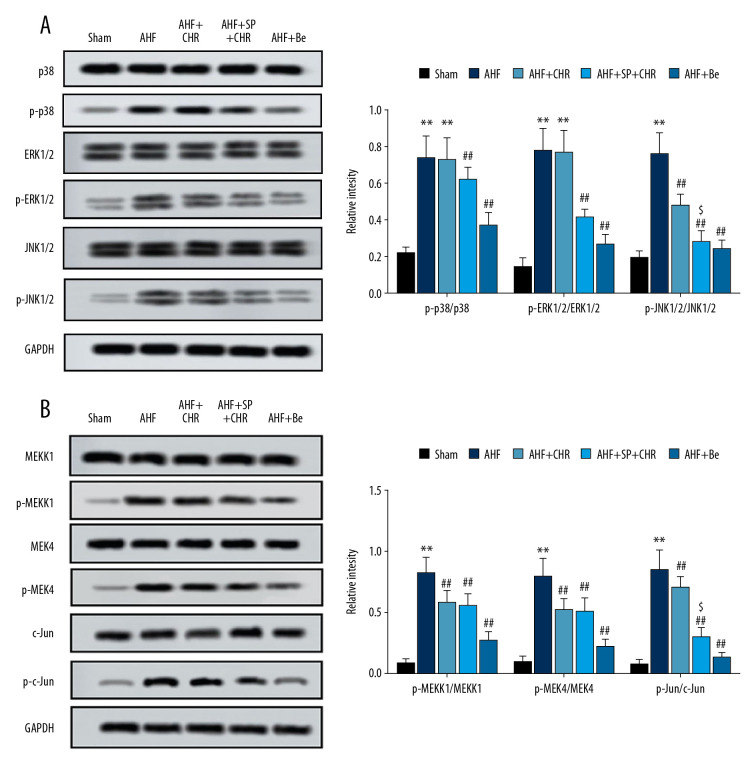
Chrysophanol inhibited the activation of JNK1/2 pathway
The results demonstrated that the phosphorylation of p38, ERK1/2, and JNK1/2 were all increased in the AHF rats compared with the sham control rats (Figure 6A). The chrysophanol treatment had no effect on the phosphorylation of p38 and ERK1/2, but it inhibited the phosphorylation of JNK1/2. The addition of SP600125 to chrysophanol inhibited the phosphorylation of p38, ERK1/2, and JNK1/2 compared with chrysophanol treatment alone. Meanwhile, the benazepril treatment significantly supressed the phosphorylation of p38, ERK1/2, and JNK1/2 in AHF rats. To further verify the effects of chrysophanol on the JNK1/2 pathway, we assessed the protein expression of its upstream and downstream factors. As expected, chrysophanol inhibited the phosphorylation of MEKK1, MEK4 (upstream factors), and c-Jun (downstream factor) in AHF model rats (Figure 6B). The phosphorylation of c-Jun was further suppressed by SP600125. Overall, the results showed that chrysophanol inhibited activation of the JNK1/2 pathway.
Figure 6.
(A, B) Chrysophanol inhibited the activation of JNK1/2 pathway. After various treatments, rats were sacrificed and myocardial tissues were collected to isolate proteins. The expression levels of protein related the MAPK pathway were determined by western blot. Each experiment was repeated 3 times. Data are expressed as mean±SEM. * p<0.05, ** p<0.01 vs. sham; # p<0.05, ## p<0.01 vs. AHF; $ p<0.05, $$ p<0.01 vs. AHF+CHR. AHF – acute heart failure; CHR – chrysophanol; SP – SP600125; Be – benazepril.
Discussion
AHF is recognized as an important public health problem with significant morbidity and mortality [18]. Rapid and sustained relief of AHF symptoms and signs remains an important goal of treatment [19]. Chrysophanol, a natural anthraquinone compound isolated from rhubarb, plays an important role in protecting against the inflammatory response, cerebral ischemia/reperfusion, diabetes, and lung and hepatic injury [20–22]. Chrysophanol has strong anti-inflammatory activity, and has been preliminarily demonstrated to protect against cardiac injury [14,16]. However, there has been little research on use of chrysophanol in cardiac disease, and further detailed verification is still needed. To date, the direct effects of chrysophanol on AHF have not been extensively explored. The present study was designed to evaluate the effects of chrysophanol on cardiac functions, myocardial damage, myocardial apoptosis, OS, and inflammation in AHF rats, to provide an alternative choice for AHF treatment.
AHF mostly occurs secondary to rapid deterioration in cardiac function due to myocardial damage, infarction, or severe myocarditis [23]. During the AHF event, the decreased cardiac function can lead to increased LV filling pressures and increased cardiac pre- and after-loads [24]. Thus, the improvement of cardiac function may provide greater clinical benefit for patients with AHF. The present study assessed the effects of chrysophanol on cardiac function, showing that chrysophanol increased LVPSP and ±LVdP/dtmax and reduced LVEDP in AHF rats. Hemodynamics are important indicators of cardiac function, among them, LVSP and +LVdp/dtmax reflect myocardial contractile function, while LVEDP and −LVdp/dtmax reflect myocardial relaxation [25]. Our results suggest that chrysophanol has positive inotropic effects and enhances the systolic function of LV. Consistent with our finding, Yuan et al. also demonstrated that chrysophanol ameliorated the abnormal changes in cardiac structure and function in rats [16]. In addition to chrysophanol, other anthraquinone compounds with anti-inflammatory properties, such as kanglexin, aloe-emodin, and diacerein, also improve cardiac function by reducing the inflammatory response after myocardial injury [26–28]. The protective role of chrysophanol is further supported by the above evidence.
Myocardial damage secondary to an episode of acute decompensation is a major component in the pathology of AHF [29]. Generally, pathological changes are visible and have a unique diagnostic significance in heart failure. Therefore, it is important to measure the myocardial damage related to the AHF episode [28]. Histological analysis revealed that chrysophanol relieved the pathological injury of myocardial tissue, which is further supported by the chrysophanol-induced reduction of CK-MB and LDH activity. In fact, CK-MB and LDH are traditional markers of myocardial damage in both pathological and physiological conditions, and CK-MB is more specific for myocardial damage [30]. Thus, the reduction of CK-MB and LDH activity provides sufficient evidence that chrysophanol ameliorates myocardial damage, and we explored how chrysophanol protects cardiac function in AHF.
Previous studies demonstrated that an early and persistent activation of myocardial apoptosis, OS, and inflammation contributes to the progression of heart failure [31–33]. OS induces myocardial apoptosis, activates redox-sensitive transcription factors, and induces transcription of proinflammatory cytokine (TNF-α and IL-6), eventually resulting in heart failure [34,35]. Therapeutic approaches targeting OS and inflammatory cascades have shown promise in patients with heart failure [36]. Chrysophanol treatment decreased the number of TUNEL-positive cells in AHF rats, indicating the inhibition of myocardial apoptosis. Meanwhile, chrysophanol treatment upregulated Bcl-2 expression and downregulated Bax and cleaved caspase-3 expression. As is well known, Bcl-2 functions as an anti-apoptotic gene, while Bax is a pro-apoptotic gene [37]. In turn, Bax leads to activation of the caspase cascade by release of cytochrome c [38]. More importantly, recent studies demonstrated that aberrant expression of Bax, Bcl-2, and cleaved caspase-3 can contribute to progression of heart failure [31]. Therefore, we concluded that chrysophanol suppressed myocardial apoptosis by regulating apoptosis-related genes and blocking caspase activation cascades, and it in turn plays a role in cardioprotection. Additionally, AHF-induced abnormal changes of OS parameters (MDA, GPx, CAT, SOD) and inflammatory markers (IL-6, IL-1β, TNF-α, IFN-γ) were alleviated by chrysophanol. Actually, broad evidence shows the strong anti-oxidant stress and anti-inflammatory activity of chrysophanol in various diseases [39,40]. For example, chrysophanol attenuates OS injury and inflammation in cerebral ischemia/reperfusion [41,42]. Additionally, chrysophanol relieves cognitive deficits and neuronal loss through inhibiting inflammation in diabetic mice [43]. Overall, chrysophanol shows promising anti-apoptosis, anti-oxidant stress, and anti-inflammatory activity in the inhibition of AHF progression.
Benazepril, an angiotensin-converting enzyme inhibitor, has been proved to be efficacious and safe in the management of congestive heart failure and chronic renal failure [44,45]. Hence, benazepril was selected as a positive control to chrysophanol, considering its clear utility in treatment of heart failure. Fortunately, the present study demonstrated that chrysophanol treatment showed similar cardioprotective effects with benazepril, showing that chrysophanol has the potential to be an effective alternative treatment for AHF.
Interestingly, we found that SP600125 facilitated the function of chrysophanol. SP600125, an anthrapyrazolone inhibitor of JNK, is widely used to inhibit JNK-mediated Bax activation and cell apoptosis [46]. Thus, we speculated that chrysophanol acts through the JNK1/2 pathway. Western blot analysis showed that chrysophanol inhibited the phosphorylation of JNK1/2, but did not affect the phosphorylation of p38 and ERK1/2. This means that chrysophanol can suppress activation of the JNK1/2 pathway, which could by also explained by the enhancement effects induced by SP600125. The activation of JNK is mediated by the phosphorylation of upstream MEK4/7, and MEK activation is regulated by the phosphorylation of upstream MEKK1 [47]. Activated JNK induces the activation of c-Jun [48,49], and the continuous expression of c-Jun is related to the differentiation and apoptosis of cardiomyocytes [50]. Therefore, we further analyzed the expression of the upstream factors MEKK1 and MEK4, as well as the downstream factor c-Jun of JNK. As expected, we found that the phosphorylation of MEKK1, MEK4 (upstream factors) and c-Jun (downstream factor) was also inhibited by chrysophanol, supporting the above hypothesis. In addition, the anthrapyrazolone inhibitor of JNK (SP600125) only suppressed the phosphorylation of c-Jun, but not the upstream factors, which further supports that chrysophanol suppresses activation of the JNK1/2 pathway. Coincidentally, multiple anthrapyrazolone compounds, such as emodin and SP60012, play a protective role by the inhibition of JNK1/2 [51,52]. The present study did not explore the relationship between chrysophanol and p38 or ERK1/2, but that does not mean that there is no association among them. Further research is needed on the mechanism of action of chrysophanol.
Conclusions
In the present study, we found that chrysophanol improved cardiac functions and protects against myocardial damage, myocardial apoptosis, OS, and inflammation in AHF rats. Furthermore, we proposed a potential mechanism by which chrysophanol exerts a protective effect by inhibiting activation of the JNK1/2 pathway. These findings indicate that chrysophanol may be a promising approach for treatment of AHF. An improved understanding of the molecular mechanism involved could facilitate a therapeutic shift toward molecular targets that could alter the course of AHF.
Footnotes
Source of support: Departmental sources
References
- 1.Kurmani S, Squire I. Acute heart failure: Definition, classification and epidemiology. Curr Heart Fail Rep. 2017;14(5):385–92. doi: 10.1007/s11897-017-0351-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suzuki T, Heaney LM, Bhandari SS, et al. Trimethylamine N-oxide and prognosis in acute heart failure. Heart. 2016;102(11):841–48. doi: 10.1136/heartjnl-2015-308826. [DOI] [PubMed] [Google Scholar]
- 3.Mebazaa A, Tolppanen H, Mueller C, et al. Acute heart failure and cardiogenic shock: A multidisciplinary practical guidance. Intensive Care Med. 2016;42(2):147–63. doi: 10.1007/s00134-015-4041-5. [DOI] [PubMed] [Google Scholar]
- 4.Gheorghiade M, Zannad F, Sopko G, et al. Acute heart failure syndromes: Current state and framework for future research. Circulation. 2005;112(25):3958–68. doi: 10.1161/CIRCULATIONAHA.105.590091. [DOI] [PubMed] [Google Scholar]
- 5.Arrigo M, Jessup M, Mullens W, et al. Acute heart failure. Nat Rev Dis Primers. 2020;6(1):16. doi: 10.1038/s41572-020-0151-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gheorghiade M, De Luca L, Fonarow GC, et al. Pathophysiologic targets in the early phase of acute heart failure syndromes. Am J Cardiol. 2005;96(6A):11G–17G. doi: 10.1016/j.amjcard.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 7.De Luca L, Fonarow GC, Adams KF, Jr, et al. Acute heart failure syndromes: Clinical scenarios and pathophysiologic targets for therapy. Heart Fail Rev. 2007;12(2):97–104. doi: 10.1007/s10741-007-9011-8. [DOI] [PubMed] [Google Scholar]
- 8.Milo-Cotter O, Cotter-Davison B, Lombardi C, et al. Neurohormonal activation in acute heart failure: results from VERITAS. Cardiology. 2011;119(2):96–105. doi: 10.1159/000330409. [DOI] [PubMed] [Google Scholar]
- 9.Peschel T, Schönauer M, Thiele H, et al. Invasive assessment of bacterial endotoxin and inflammatory cytokines in patients with acute heart failure [published correction appears in Eur J Heart Fail, 2004; 6(2): 245] Eur J Heart Fail. 2003;5(5):609–14. doi: 10.1016/s1388-9842(03)00104-1. [DOI] [PubMed] [Google Scholar]
- 10.Reina-Couto M, Bessa JP, Serrão P, et al. Inflammation resolution mediators in acute heart failure. J Hypertens. 2018;36:e211. [Google Scholar]
- 11.Miró Ò, Martínez G, Masip J, et al. Effects on short term outcome of non-invasive ventilation use in the emergency department to treat patients with acute heart failure: A propensity score-based analysis of the EAHFE Registry. Eur J Intern Med. 2018;53:45–51. doi: 10.1016/j.ejim.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Singh D, Rawat MSM, Semalty A, et al. Chrysophanol–phospholipid complex. J Therm Anal Calorim. 2012;111:2069–77. [Google Scholar]
- 13.Kim SJ, Kim MC, Lee BJ, et al. Anti-Inflammatory activity of chrysophanol through the suppression of NF-kappaB/caspase-1 activation in vitro and in vivo. Molecules. 2010;15(9):6436–51. doi: 10.3390/molecules15096436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lian Y, Xia X, Zhao H, et al. The potential of chrysophanol in protecting against high fat-induced cardiac injury through Nrf2-regulated anti-inflammation, anti-oxidant and anti-fibrosis in Nrf2 knockout mice. Biomed Pharmacother. 2017;93:1175–89. doi: 10.1016/j.biopha.2017.05.148. [DOI] [PubMed] [Google Scholar]
- 15.Lu J, Li J, Hu Y, et al. Chrysophanol protects against doxorubicin-induced cardiotoxicity by suppressing cellular PARylation. Acta Pharm Sin B. 2019;9(4):782–93. doi: 10.1016/j.apsb.2018.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yuan J, Hong H, Zhang Y, et al. Chrysophanol attenuated isoproterenol-induced cardiac hypertrophy by inhibiting Janus kinase 2/signal transducer and activator of transcription 3 signaling pathway. Cell Biol Int. 2019;43(6):695–705. doi: 10.1002/cbin.11146. [DOI] [PubMed] [Google Scholar]
- 17.Xue P, Zhao J, Zheng A, et al. Chrysophanol alleviates myocardial injury in diabetic db/db mice by regulating the SIRT1/HMGB1/NF-κB signaling pathway. Exp Ther Med. 2019;18(6):4406–12. doi: 10.3892/etm.2019.8083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernández Rodríguez JM, Casado J, Formiga F, et al. Consensus on basic conduct during the hospital admission of patients with acute heart failure. Rev Clin Esp. 2020 doi: 10.1016/j.rceng.2020.01.010. [Online ahead of print] [DOI] [PubMed] [Google Scholar]
- 19.Teerlink JR, Cotter G, Davison BA, et al. Serelaxin, recombinant human relaxin-2, for treatment of acute heart failure (RELAX-AHF): A randomised, placebo-controlled trial. Lancet. 2013;381(9860):29–39. doi: 10.1016/S0140-6736(12)61855-8. [DOI] [PubMed] [Google Scholar]
- 20.Yan J, Zheng M, Zhang D. Chrysophanol liposomes protects brain against cerebral ischemia-reperfusion injury by reducing expression of Caspase3 in mice. Latin American Journal of Pharmacy. 2014;33:973–81. [Google Scholar]
- 21.Jiang W, Zhou R, Li P, et al. Protective effect of chrysophanol on LPS/d-GalN-induced hepatic injury through the RIP140/NF-κB pathway. RSC Advances. 2016;6:38192–200. [Google Scholar]
- 22.Chae U, Min JS, Lee H, et al. Chrysophanol suppresses pro-inflammatory response in microglia via regulation of Drp1-dependent mitochondrial fission. Immunopharmacol Immunotoxicol. 2017;39(5):268–75. doi: 10.1080/08923973.2017.1344988. [DOI] [PubMed] [Google Scholar]
- 23.Arrigo M, Nijst P, Rudiger A. Optimising heart failure Therapies in the acute setting. Card Fail Rev. 2018;4(1):38–42. doi: 10.15420/cfr.2017:21:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmieder RE, Mitrovic V, Hengstenberg C. Renal impairment and worsening of renal function in acute heart failure: Can new therapies help? The potential role of serelaxin. Clin Res Cardiol. 2015;104(8):621–31. doi: 10.1007/s00392-015-0839-y. [DOI] [PubMed] [Google Scholar]
- 25.Li Y, Song P, Zhu Q, et al. Liguzinediol improved the heart function and inhibited myocardial cell apoptosis in rats with heart failure. Acta Pharmacol Sin. 2014;35(10):1257–64. doi: 10.1038/aps.2014.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bian Y, Li X, Pang P, et al. Kanglexin, a novel anthraquinone compound, protects against myocardial ischemic injury in mice by suppressing NLRP3 and pyroptosis. Acta Pharmacol Sin. 2020;41:319–26. doi: 10.1038/s41401-019-0307-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Torina AG, Reichert K, Lima F, et al. Diacerein improves left ventricular remodeling and cardiac function by reducing the inflammatory response after myocardial infarction. PLoS One. 2015;10(3):e0121842. doi: 10.1371/journal.pone.0121842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yu Y, Liu H, Yang D, et al. Aloe-emodin attenuates myocardial infarction and apoptosis via up-regulating miR-133 expression. Pharmacol Res. 2019;146:104315. doi: 10.1016/j.phrs.2019.104315. [DOI] [PubMed] [Google Scholar]
- 29.Sabbah HN. Pathophysiology of acute heart failure syndrome: A knowledge gap. Heart Fail Rev. 2017;22(6):621–39. doi: 10.1007/s10741-017-9651-2. [DOI] [PubMed] [Google Scholar]
- 30.Park CH, Kim KB, Han J, et al. Cardiac damage biomarkers following a triathlon in elite and non-elite triathletes. Korean J Physiol Pharmacol. 2014;18(5):419–23. doi: 10.4196/kjpp.2014.18.5.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moe GW, Naik G, Konig A, et al. Early and persistent activation of myocardial apoptosis, bax and caspases: Insights into mechanisms of progression of heart failure. Pathophysiology. 2002;8(3):183–92. doi: 10.1016/s0928-4680(02)00008-1. [DOI] [PubMed] [Google Scholar]
- 32.Yndestad A, Damås JK, Øie E, et al. Role of inflammation in the progression of heart failure. Curr Cardiol Rep. 2007;9(3):236–41. doi: 10.1007/BF02938356. [DOI] [PubMed] [Google Scholar]
- 33.Xu Q, Dalic A, Fang L, et al. Myocardial oxidative stress contributes to transgenic β2-adrenoceptor activation-induced cardiomyopathy and heart failure. Br J Pharmacol. 2011;162(5):1012–28. doi: 10.1111/j.1476-5381.2010.01043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang T, Zhang Y, Cui M, et al. CaMKII is a RIP3 substrate mediating ischemia- and oxidative stress-induced myocardial necroptosis. Nat Med. 2016;22(2):175–82. doi: 10.1038/nm.4017. [DOI] [PubMed] [Google Scholar]
- 35.Neri M, Fineschi V, Di Paolo M, et al. Cardiac oxidative stress and inflammatory cytokines response after myocardial infarction. Curr Vasc Pharmacol. 2015;13(1):26–36. doi: 10.2174/15701611113119990003. [DOI] [PubMed] [Google Scholar]
- 36.McKinsey TA. Targeting inflammation in heart failure with histone deacetylase inhibitors. Mol Med. 2011;17(5–6):434–41. doi: 10.2119/molmed.2011.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Opferman JT, Kothari A. Anti-apoptotic BCL-2 family members in development. Cell Death Differ. 2018;25:37–45. doi: 10.1038/cdd.2017.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gupta S, Knowlton AA. HSP60, Bax, apoptosis, and the heart. J Cell Mol Med. 2005;9:51–58. doi: 10.1111/j.1582-4934.2005.tb00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jeong HJ, Kim HY, Kim HM. Molecular mechanisms of anti-inflammatory effect of chrysophanol, an active component of AST2017-01 on atopic dermatitis in vitro models. Int Immunopharmacol. 2018;54:238–44. doi: 10.1016/j.intimp.2017.11.019. [DOI] [PubMed] [Google Scholar]
- 40.Wen Q, Mei L, Ye S, et al. Chrysophanol demonstrates anti-inflammatory properties in LPS-primed RAW 264.7 macrophages through activating PPAR-γ. Int Immunopharmacol. 2018;56:90–97. doi: 10.1016/j.intimp.2018.01.023. [DOI] [PubMed] [Google Scholar]
- 41.Zhao Y, Huang Y, Fang Y, et al. Chrysophanol attenuates nitrosative/oxidative stress injury in a mouse model of focal cerebral ischemia/reperfusion. J Pharmacol Sci. 2018;138:16–22. doi: 10.1016/j.jphs.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Zhang N, Zhang X, Liu X, et al. Chrysophanol inhibits NALP3 inflammasome activation and ameliorates cerebral ischemia/reperfusion in mice. Mediators Inflamm. 2014;2014 doi: 10.1155/2014/370530. 370530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chu X, Zhou S, Sun R, et al. Chrysophanol relieves cognition deficits and neuronal loss through inhibition of inflammation in diabetic mice. Neurochem Res. 2018;43:972–83. doi: 10.1007/s11064-018-2503-1. [DOI] [PubMed] [Google Scholar]
- 44.Yan X, Xu D, Huang J. [Effect of benazepril on cardiac function in Chinese patients with chronic heart failure: A meta-analysis of randomized controlled trials]. Zhonghua Yi Xue Za Zhi. 2014;94:2907–13. [in Chinese] [PubMed] [Google Scholar]
- 45.King JN, Font A, Rousselot JF, et al. Effects of benazepril on survival of dogs with chronic kidney disease: A multicenter, randomized, blinded, placebo-controlled clinical trial. J Vet Intern Med. 2017;31:1113–22. doi: 10.1111/jvim.14726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu YY, Chen TS, Wang XP, et al. The JNK inhibitor SP600125 enhances dihydroartemisinin-induced apoptosis by accelerating Bax translocation into mitochondria in human lung adenocarcinoma cells. FEBS Lett. 2010;584:4019–26. doi: 10.1016/j.febslet.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 47.Cobb MH. MAP kinase pathways. Prog Biophys Mol Biol. 1999;71:479–500. doi: 10.1016/s0079-6107(98)00056-x. [DOI] [PubMed] [Google Scholar]
- 48.Xu Z, Wu J, Xin J, et al. β3-adrenergic receptor activation induces TGFβ1 expression in cardiomyocytes via the PKG/JNK/c-Jun pathway. Biochem Biophys Res Commun. 2018;503:146–51. doi: 10.1016/j.bbrc.2018.05.200. [DOI] [PubMed] [Google Scholar]
- 49.Zheng M, Chen R, Chen H, et al. Netrin-1 promotes synaptic formation and axonal regeneration via JNK1/c-Jun pathway after the middle cerebral artery occlusion. Front Cell Neurosci. 2018;12:13. doi: 10.3389/fncel.2018.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saadane N, Alpert L, Chalifour LE. Expression of immediate early genes, GATA-4, and Nkx-2.5 in adrenergic-induced cardiac hypertrophy and during regression in adult mice. Br J Pharmacol. 1999;127:1165–76. doi: 10.1038/sj.bjp.0702676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu GD, Shen HM, Ong CN, et al. Aloe-emodin induces apoptotic cell death via oxidative stress and JNK activation in human hepatoma cells. Leuk Res. 2006;1:3–12. doi: 10.1093/carcin/bgm143. [DOI] [PubMed] [Google Scholar]
- 52.Guan QH, Pei DS, Zhang QG, et al. The neuroprotective action of SP600125, a new inhibitor of JNK, on transient brain ischemia/reperfusion-induced neuronal death in rat hippocampal CA1 via nuclear and non-nuclear pathways. Brain Res. 2005;1035:51–59. doi: 10.1016/j.brainres.2004.11.050. [DOI] [PubMed] [Google Scholar]