Abstract
Background
Natural disasters, including earthquakes, tsunamis, tornadoes, and hurricanes, are traumatic events that simultaneously affect the lives of many people. Although much is known about the effects that natural disasters have on mental health, little is known about how natural disasters affect physical health. These analyses add to the literature by examining the ways in which four types of disaster exposure (geographic, peri-traumatic stress, personal and property loss, and poststorm hardship) experienced by older people during and after Hurricane Sandy affected functional limitations.
Methods
We analyzed five waves of data from the ORANJ BOWL panel (“Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life”) using multilevel mixed-effects models.
Results
We found that although peri-traumatic stress and poststorm hardship each had independent effects on functional limitations, the effects of peri-traumatic stress dominated and were evident 6 years after the hurricane. Geographic exposure and personal/property loss were not associated with functional limitations.
Conclusions
These findings add important information to what is known about older people who experience a natural disaster and suggest opportunities for intervention. Finding that an individual’s emotional response during the disaster plays an important role in the development of functional limitations suggests that reduction of exposure to traumatic stress during a storm (ie, evacuation from a storm area) may be important for older people. Likewise, interventions immediately after a disaster that target older people who experience high levels of peri-traumatic distress may be needed in order to alleviate functional limitations before they develop.
Keywords: Disaster exposure, Functional limitations, Hurricane Sandy
Between 2008 and 2018, 3,751 natural disasters struck worldwide (1). Together these disasters, 84% of which are weather-related, wreaked havoc for two billion people and resulted in damages of $1,658 billion. Natural disasters, including earthquakes, tsunamis, tornadoes, and hurricanes, are traumatic events that simultaneously affect the lives of many people. Although older people may not inherently be vulnerable to disasters (2), factors associated with aging, including reduced mobility and chronic health conditions, have the potential to increase the likelihood that disasters will have harmful effects on older people. In fact, many studies find that older people are among those most vulnerable to natural disasters (3–5).
Hurricane Sandy, the largest Atlantic hurricane on record, struck the Eastern United States on October 29, 2012, killing 117 people, injuring countless others (6), and forcing more than three-quarters of a million people to leave their homes (7). The effects of the hurricane, which caused $70 billion dollars in damages (8), were exacerbated by an unseasonably early snowstorm and frigid temperatures that left over eight million people without power for weeks (9). In New Jersey mortality rates were particularly high in communities most severely affected by the storm; all-cause mortality rates of people aged 76 and older increased 10% in the month following the hurricane (10).
Although the effects of disasters on PTSD (11,12) and mental health (13–16) are known, few studies have examined the effects of disaster on the physical health of older people. Studies that have focused on health outcomes have design limitations that can affect our understanding about disasters’ effects. These include: (i) lack of information about people prior to the disaster, (ii) reliance on convenience samples, and (iii) defining disaster exposure as a simple function of geographic proximity.
The analyses that follow are based on data from several thousand community-dwelling older people in New Jersey who were recruited using random-digit dial procedures for a longitudinal panel in 2006. Prior to the hurricane, many of these people had participated in up to three waves of data collection in which they provided information about their physical and mental well-being. As such, a unique opportunity to learn about the impact of disaster on older people existed. Using data collected over 12 years, we examined the effects of four different types of disaster exposure (geographic, peri-traumatic stress, personal and property loss, and poststorm hardship) on functional limitations, an early marker of disability with strong associations to morbidity, mortality, and quality of life (17–19).
Disasters and Physical Health
Few studies have examined the effects that natural disasters have on physical health of older adults. Not surprisingly, findings vary widely, depending on how physical health and disaster exposure are measured and the length of time between the disaster and data collection. Prior work has relied on use of the SF-36 following disaster exposure without explicit measures of exposure (20) or focused on only the 2-week period following a disaster (21). While yielding important information, these studies which defined exposure as a function of geographic location, address neither the elements of exposure associated with health declines nor the effects that a disaster has on dimensions of functioning needed to enable older people to continue living in the community.
Disasters and Functional Limitations
Functional limitations are an early marker of disability with strong associations to morbidity, mortality, and quality of life (17,22). As such, functional limitations may be a more sensitive measure of change in health than either physical health or healthcare utilization. Chronic conditions, including diabetes (23), cardiovascular disease (19), obesity (24), depression (25), cognitive decline (22), and impaired pulmonary functioning (26), as well as low levels of physical activity, hypertension, and poor lung function (27) are known risks for functional limitations, making functional limitations a key health outcome.
Prior natural disaster work has found that people experiencing high levels of psychological distress after a disaster also had the highest risk of incident functional disability (28) 1 year after a disaster and disability rates were higher in areas affected by the disaster than in nondisaster areas (29). Furthermore, in considering long-term effects of disaster on functional ability (3 years later), rates of disability in affected regions have been found to remain higher than those in nondisaster areas, but the degree of increase in disability prevalence between the disaster-stricken and nondisaster areas shrink each year (30). Additional work on disasters triggered by technology failure and terrorist acts also highlight the impact that proximity to trauma and experience of PTSD can have on functional limitations (18, 31). In contrast, other scholars, examining the association of community-level disaster exposure with individual-level changes in functional limitations, have found no evidence that the presence of a disaster within the previous 2 years was associated with an increase in functional limitations (32). These findings altogether suggest the potential for disasters to affect functional limitations, yet conclusions are limited given studies’ crude indicators of disaster exposure, reliance on convenience samples, and lack of predisaster information.
Taking advantage of a unique natural experiment using a national cohort established 7 months prior to the Great Earthquake, Tsuboya and colleagues (33) conducted the first study to use predisaster individual-level information to examine the impact of disaster on functional limitations assessed using a 13-item scale of IADLs in community-dwelling adults. They examined the experiences of 3,547 community-dwelling older people who provided data 7 months before and 3 years after the disaster. Exposure was assessed at the individual-level using personal reports of damage. These investigators found that complete house loss and disrupted internal medicine appointments were associated with an increase in functional limitations. Interestingly, loss of family, friends, pets, and car as well as disruption of medical services other than internal medicine appointments was not associated with functional limitations. The powerful effects that the earthquake had on functional limitations raises questions about the impact that other natural disasters, such as a hurricane, might have and whether the effects of disaster might extend even beyond 3 years.
Current Study
The analyses that follow build on prior literature and tie closely to Tsuboya and colleagues’s (33) findings by taking advantage of another natural experiment. In this case, three waves of predisaster data had been gathered from a large, state-wide sample of older people allowing us to examine how different types of exposure to Hurricane Sandy (geography, peri-traumatic stress, personal and property loss, and poststorm hardship) impacted functional limitations over a 12-year period. We controlled for age, gender, socioeconomic status, and preexisting health conditions as they have known associations with functional limitations (34–40) and we tested the following hypotheses:
Older people living in counties hardest hit by Hurricane Sandy would have more functional limitations 6 years later than older people not living in these counties.
Older people who experienced higher levels of peri-traumatic stress during Hurricane Sandy would have more functional limitations 6 years later than older people who experienced lower levels of peri-traumatic stress.
Older people experiencing higher levels of personal and property loss following Hurricane Sandy would have more functional limitations 6 years later than older people experiencing lower levels of personal and property loss.
Older people who experienced higher levels of poststorm hardship would have more functional limitations 6 years after the storm than older people who experienced lower levels of poststorm hardship.
After testing the effect of each type of exposure individually, we examined, in an exploratory fashion, the relative contributions that peri-traumatic stress, geographic location, personal and property loss, and poststorm hardship had on functional limitations.
Methods
Participants
Between 2006 and 2008, we recruited and completed interviews with 5,688 people (Wave 1) who were part of the ORANJ BOWL (Ongoing Research on Aging in New Jersey: Bettering Opportunities for Wellness in Life) panel. ORANJ BOWL has as its goal identifying factors that influence successful aging. We recruited participants using cold calling and list-assisted random-digit-dialing (RDD) procedures. Eligible participants were between the ages of 50 and 74, living in New Jersey, and able to participate in a one-hour, English-language telephone interview at baseline. Coverage loss due to cell phone-only households was small due to sample demographics (41). ORANJ BOWL achieved a response rate of 58.73%, using standard American Association for Public Opinion Research calculations, and a Cooperation Rate of 72.88%, consistent with or better than average RDD response rates. Details regarding sample development are presented in Pruchno and colleagues (42). Participants were representative of older adults (aged 50–74) living in New Jersey in 2006, except for a slightly higher rate of women and people with more years of education. Because we were unable to translate the interview into Spanish, ORANJ BOWL under-represents Hispanics. At Wave 1, ORANJ BOWL participants lived in 1,644 of New Jersey’s 1,912 census tracts. Table 1 includes sample descriptive statistics.
Table 1.
Sample Descriptives by Wave
| Wave 1 N = 5,688 | Wave 3 N = 3,387 | Wave 4 N = 3,608 | Wave 5 N = 3,076 | Wave 6 N = 3,137 | |
|---|---|---|---|---|---|
| Age (M [SD]) | 60.79 (7.10) | 65.37 (7.01) | 67.66 (6.92) | 69.14 (6.73) | 70.39 (6.66) |
| Sex (female) | 3,621 (63.7) | 2,202 (65.0) | 2,326 (64.5) | 1,956 (63.6) | 1,996 (63.6) |
| African American | 646 (11.4) | 276 (8.1) | 314 (8.7) | 222 (7.2) | 250 (8.0) |
| Income | |||||
| <$15K | 365 (6.4) | 152 (4.5) | 156 (4.3) | 85 (2.8) | 102 (3.3) |
| $15K–$30K | 601 (10.6) | 289 (8.5) | 297 (8.2) | 221 (7.2) | 215 (6.9) |
| $30K–$50K | 862 (15.2) | 502 (14.8) | 509 (14.1) | 419 (13.6) | 431 (13.7) |
| $50K–$80K | 1,133 (19.9) | 698 (20.6) | 736 (20.4) | 639 (20.8) | 646 (20.6) |
| $80K–$150K | 1,291 (22.7) | 875 (25.8) | 954 (26.4) | 864 (28.1) | 881 (28.1) |
| >$150K | 770 (13.5) | 520 (15.4) | 573 (15.9) | 516 (16.8) | 534 (17.0) |
| Missing | 666 (11.7) | 351 (10.4) | 383 (10.6) | 332 (10.8) | 328 (10.5) |
| Educational attainment | |||||
| Not high school (HS) graduate | 306 (5.4) | 115 (3.4) | 113 (3.1) | 59 (1.9) | 61 (1.9) |
| HS graduate or GED | 1,607 (28.3) | 863 (25.5) | 900 (24.9) | 686 (22.3) | 706 (22.5) |
| Some college | 852 (15.0) | 487 (14.4) | 515 (14.3) | 452 (14.7) | 459 (14.6) |
| 2 y college degree | 530 (9.3) | 320 (9.4) | 356 (9.9) | 313 (10.2) | 312 (9.9) |
| 4 y college degree | 1,108 (19.5) | 697 (20.6) | 769 (21.3) | 681 (22.1) | 714 (22.8) |
| Some postbaccalaureate | 220 (3.9) | 162 (4.8) | 164 (4.5) | 148 (4.8) | 153 (4.9) |
| Masters | 743 (13.1) | 521 (15.4) | 563 (15.6) | 516 (16.8) | 517 (16.5) |
| Some postmasters | 73 (1.3) | 50 (1.5) | 52 (1.4) | 47 (1.5) | 45 (1.4) |
| Doctorate | 236 (4.1) | 168 (5.0) | 171 (4.7) | 171 (5.6) | 167 (5.3) |
| Missing | 13 (0.2) | 4 (0.1) | 5 (0.1) | 3 (0.1) | 3 (0.1) |
| Functional limitations (M [SD]) | 40.08 (6.55) | 40.78 (5.75) | 40.95 (5.64) | 41.22 (5.42) | 41.26 (5.45) |
| Chronic illnesses (M [SD]) | 1.76 (1.40) | 1.70 (1.35) | 1.66 (1.32) | 1.60 (1.29) | 1.57 (1.28) |
| Storm exposure | |||||
| Peri-traumatic stressors | — | — | 0.86 (1.01) | — | — |
| Personal and property loss | — | — | 0.54 (0.74) | — | — |
| Poststorm hardship | — | — | 0.13 (0.37) | — | — |
Note: GED = tests of general education development.
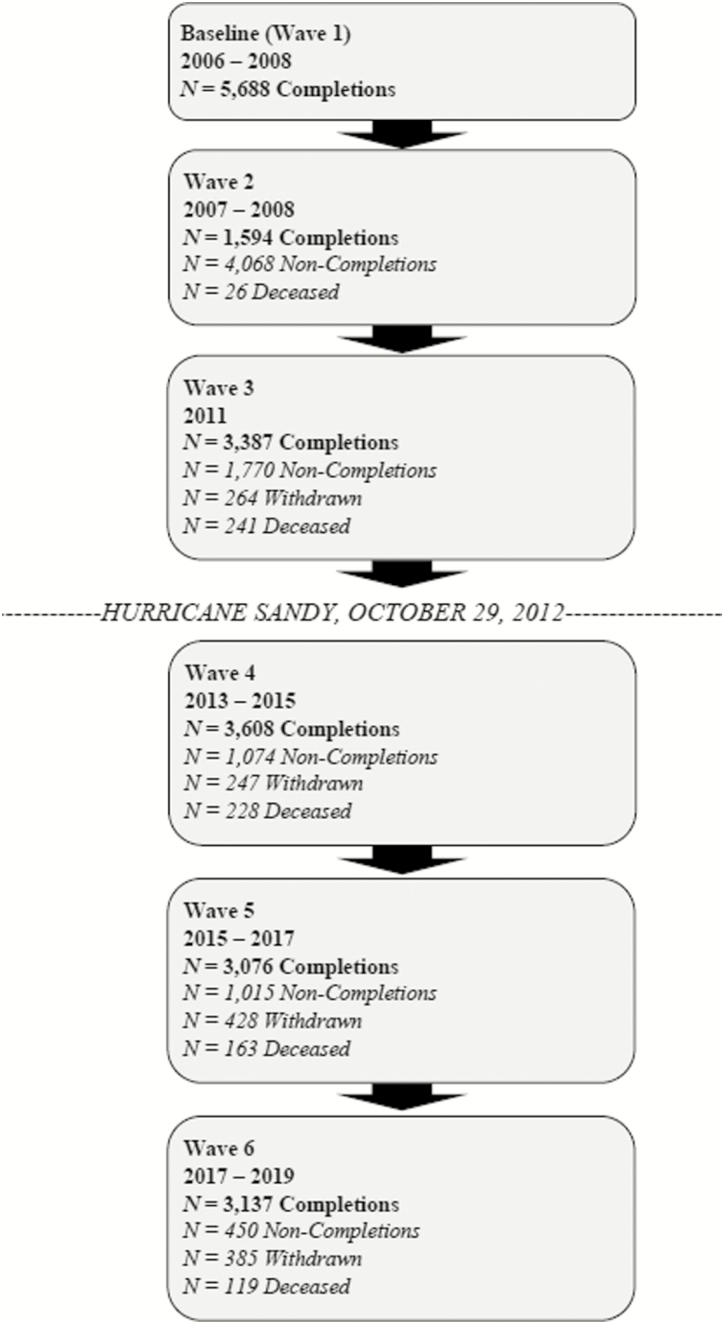
One year after their baseline interview, a subsample of participants was re-contacted and asked to complete a personality measure (Wave 2). We excluded data from this wave in these analyses because we did not collect information about functional limitations at that wave. In 2011, we mailed a questionnaire (Wave 3) to all ORANJ BOWL respondents; 3,387 participants completed the survey. In 2014, approximately 18 months after Hurricane Sandy struck, we mailed a questionnaire (Wave 4) to all ORAN BOWL respondents known to be alive at Wave 3. We called participants who did not complete the interview and whenever possible, we completed the interview by telephone; 3,608 individuals completed the survey. The availability of additional funds for sample follow-up at Wave 4 resulted in a larger sample at Wave 4 than Wave 3. Wave 5 was then completed approximately 18-months after completion of Wave 4 (2015–2017; N = 3,076). Wave 6 was completed approximately 18 months after completion of Wave 5 (2017–2019; N = 3,137). See Figure 1 for full sample flow in relation to Hurricane Sandy. At each wave, completers significantly differed from noncompleters. Completers reported higher levels of education and income than those who had died, withdrew, or did not complete each wave. Completers were significantly older than noncompleters and younger than those that withdrew or died. Completers were more likely to be female than those who died and less likely to be African American than noncompleters.
Figure 1.
ORANJ BOWL data flow chart across six waves.
The Rowan University Institutional Review Board reviewed and approved all human subject activity.
Measures
Disaster exposure
Exposure was assessed using four measures of exposure: peri-traumatic stress, personal and property loss, poststorm hardship, and geographic exposure. We assessed peri-traumatic stress at Wave 4 by asking participants to report whether they felt: (i) in immediate physical danger during Hurricane Sandy, and (ii) distressed or fearful during Hurricane Sandy. Bell and colleagues (43) and Wilson-Genderson and colleagues (15) asked similar questions. Responses to each question were recorded on a three-point scale: 0 (no), 1 (a little), or 2 (a lot). We summed responses to these two questions to create a peri-traumatic stress score. The sample mean was 0.86 (SD = 1.0) with a range of 0–4.
We measured personal and property loss at Wave 4 by asking participants if they experienced: (i) physical injury, (ii) a need for medical attention, (iii) any home damage, (iv) family or close friends injured or killed, (v) loss of utilities, and/or (vi) damage to a personal automobile as a result of Hurricane Sandy. Consistent with the approach used by scholars of life events (44) and disasters (15,16,45,46), responses were summed. As only six people experienced four or more of these stressors, we capped this variable at three, yielding a range of 0–3.
We assessed poststorm hardship at Wave 5 by asking participants if, because of Hurricane Sandy, they had: (i) stopped working, (ii) left their home, (iii) had mold problems at home, and/or (iv) lost income. Lowe and colleagues (47) and Wilson-Genderson and colleagues (15) asked similar questions. As with personal and property loss, we summed responses. We capped this variable at 2 because only four people experienced 3 of these stressors, yielding a range of 0–2.
Finally, we defined geographic exposure as living in one of the nine counties identified by HUD (48) as hardest hit by Hurricane Sandy at the Wave 4 assessment. These included Atlantic, Bergen, Cape May, Essex, Hudson, Middlesex, Monmouth, Ocean, and Union counties. Brilleman and colleagues (32) and Wilson-Genderson and colleagues (15) also operationalized geographic exposure based on FEMA classifications. Living in a storm-exposed area was denoted “1”; not being in the defined area was coded “0”; 3,216 (56.5%) of participants were living in a county affected by the storm.
Functional limitations
At each of the five waves of data collection, respondents reported the extent of difficulty they had with nine indicators of functional limitations (Walk a 1/4 mile, walk up 10 steps without resting, stand or be on your feet for about 2 hours, sit for about 2 hours, stoop, bend, or kneel, reach up over your head, use your fingers to grasp or handle small objects, lift or carry something as heavy as 10 lbs., such as a full bag of groceries, and push or pull large objects like a living room chair) using a 5-point Likert scale ranging from 1 (can’t do it at all) to 5 (not at all difficult), with higher scores indicating fewer functional limitations.
Chronic health conditions
At baseline, participants indicated whether a physician had ever told them they had: Parkinson’s disease, multiple sclerosis, HIV, osteoarthritis of the knee, arthritis, a heart condition, cancer, diabetes, osteopenia/osteoporosis, stroke, lung problems, or liver disease. Responses were coded as 0 (no) or 1 (yes) and the responses were summed.
Demographic covariates
At baseline, respondents reported their age, gender (0 = male, 1 = female), income (range from 1 = less than $15,000 to 6 = more than $150,000), educational attainment (range from 1 = less than high school to 9 = doctoral degree) and race (0 = not African American, 1 = African American).
Statistical Analysis
We examined sample descriptive information for each wave of data collection on demographic characteristics, chronic health conditions, storm exposure, and functional limitations, and computed bivariate correlations for the storm exposure variables. Next, we ran multilevel mixed-effects models that account for the nesting of observations within participants and permit the inclusion of neighborhood characteristics at Level 2 of the model. These analyses examined the association between exposure to Hurricane Sandy and functional limitations using all available waves of data for each participant and unbiased estimates for missing data. Following Singer and Willett (49), we report findings based on all waves of data.
Participants included in the multilevel models participated in the baseline interview and at least one interview after the storm. After confirming a substantial within-person ICC of 0.67 over time, we created a within-person unconditional model (Yit = π0i + π1i (waveit)+ π2i (lagit) + eit) to estimate average linear and person-specific change over time in functional limitations. In this model, Yit is the functional limitation score at time t for participant i; π0i is initial status of functional limitation for participant i. The linear time parameter π1i was coded as 1, 3, 4, 5, 6 (wave) and represents the point of measurement for the linear change in functional limitation. A lag variable was included to capture the exact amount of time that had passed for each individual participant since baseline (lagit); eit is the error for participant i at time t.
Once the form of the change and average slopes was determined, we introduced additional variables as follows: Model B added demographic characteristics (age, gender, income, and education) and prior diagnosed chronic health conditions to account for associations between person-level characteristics and functional limitations. Models C-1 through C-3 added one of the individual-level exposure variables (peri-traumatic stress, personal/property loss, poststorm hardship) at Level 1 and the geographic indicator of exposure at Level 2. Model D simultaneously included all three individual-level exposure variables at Level 1 and the geographic indicator at Level 2.
Model results are presented as regression parameter estimates (β) with the associated standard errors reflecting the strength of the association of each variable and change in functional limitations (see Yit above) and the significance test assessed as p-values less than .05. Fit indices are presented for the sake of model comparison including -2 Log Likelihood, AIC, AICC, BIC, and χ 2, all of which are interpreted as smaller is better. To assess the robustness of the models given missing data on income, we tested the models in the following three ways: (i) using data from participants who had complete data, (ii) using SAS Proc MI for multiple imputation, and (iii) removing the income variable from the model. The model results were similar and the parameter interpretations were the same under all three conditions. As a result, we retained the full sample for which data were available. In order to account for risk of death throughout the study period, sensitivity analyses were conducted following procedures described by Berry and colleagues (50). Death status did not affect other findings and as a result, death status was not included in the models in favor of parsimony. SAS 9.4 was used for all analyses.
Results
Table 1 presents descriptive statistics for the sample at each wave of data collection. Table 2 shows that the bivariate correlations among the disaster exposure variables for people living in and out of counties identified by FEMA as affected by Hurricane Sandy were similar.
Table 2.
Bivariate Correlations Among Exposure Variables
| Peri-traumatic stress | Personal and property loss | Poststorm hardship | |
|---|---|---|---|
| Peri-traumatic stress | 1 | 0.30*** | 0.14*** |
| Personal and property loss | 0.26*** | 1 | 0.33*** |
| Poststorm hardship | 0.14*** | 0.29*** | 1 |
Note: Values above the diagonal pertain to people living in a county designated by FEMA as affected by Hurricane Sandy; values below the diagonal refer to people not living in a FEMA designated county.
***p < .001.
The initial multi-level model (Model A; see Table 3) revealed a significant linear increase in functional limitations over time (Wave) with no additional change over time attributable to how much time had passed for the individual participant (Lag). This indicates that the exact amount of time passed neither amplified nor dampened the linear increase in functional limitations that is accounted for by Wave over time.
Table 3.
Results of Multilevel Model Analyses
| Model A | Model B | Model C-1 | Model C-2 | Model C-3 | Model D | |
|---|---|---|---|---|---|---|
| Effect | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | β (SE) |
| Individual level | ||||||
| Intercept | 43.51 (1.7) | 40.7 (1.8) | 41.36 (2.02) | 40.51 (2.0) | 41.6 (1.9) | 41.3 (2.0) |
| Wave | −0.43 (0.02)*** | −0.51 (0.02)*** | −0.52 (0.02)*** | −0.52 (0.02)*** | −0.52 (0.02)*** | −0.52 (0.02)*** |
| Laga | 0.0007 (0.0005) | −0.0007 (0.0005) | −0.0008 (0.0005) | −0.0008 (0.0005) | −0.0006 (0.0005) | −0.0009 (0.0005) |
| Age | 0.015 (0.013) | 0.01 (0.01) | 0.019 (0.01) | 0.007 (0.01) | 0.011 (0.01) | |
| Education | 0.24 (0.042)*** | 0.26 (0.04)*** | 0.25 (0.04)*** | 0.27 (0.04)*** | 0.26 (0.04)*** | |
| Gender | −0.97 (0.17)*** | −0.87 (0.18)*** | −0.94 (0.18)*** | −0.72 (0.18)*** | −0.86 (0.18)*** | |
| Income | 0.96 (0.07)*** | 0.93 (0.07)*** | 0.97 (0.08)*** | 0.90 (0.07)*** | 0.93 (0.08)*** | |
| Chronic illness | −1.82 (0.08)*** | −1.81 (0.08)*** | −1.82 (0.08)*** | −1.7 (0.08)*** | −1.81 (0.08)*** | |
| Peri-traumatic stress | −0.23 (0.09)*** | −0.24 (0.09)*** | ||||
| Personal/property loss | −0.06 (0.11) | 0.10 (0.12) | ||||
| Poststorm hardship | −0.34 (0.12)* | −0.24 (0.22) | ||||
| Neighborhood level | ||||||
| County affected by Sandy | 0.14 (0.18) | 0.084 (0.18) | 0.12 (0.17) | 0.15 (0.18) | ||
| Fit indices | ||||||
| −2 LLb | 81,318.2 | 66,020.2 | 61,844.4 | 62,500.7 | 61,925.7 | 61,846.3 |
| AIC | 81,326.2 | 66,028.2 | 61,852.4 | 62,508.7 | 61,933.7 | 61,854.3 |
| AICC | 81,326.2 | 66,028.2 | 61,852.4 | 62,508.7 | 61,933.7 | 61,854.3 |
| BIC | 81,350.5 | 66,052.5 | 61,876.3 | 62,532.7 | 61,957.6 | 61,878.2 |
| χ | 12,358.62 | 6,673.93 | 6,397.76 | 6,489.43 | 6,388.00 | 6,396.64 |
Note: * p < .05, *** p < .001. aLag is the exact amount of time that has passed for the individual since baseline data collection. bLL = log likelihood.
Model B revealed that women and people with more chronic illnesses had more functional limitations. People with higher education and income had fewer functional limitations. The linear effect of time (Wave) remained significant indicating that over time functional limitations increased.
Model C-1 revealed that all the previously tested parameters remained the same as in Model B and that peri-traumatic stress at the individual level was significantly associated with functional limitations. People experiencing more peri-traumatic stress reported more functional limitations over time. Living in a county identified by FEMA as storm affected was not associated with functional limitations.
Model C-2 revealed that all the previously tested parameters remained the same as in Model B and that personal and property loss at the individual level was not significantly associated with functional limitations. In this model, living in a FEMA-defined storm damaged county (Level 2) was not associated with functional limitations.
Model C-3 revealed that all the previously tested parameters remained the same as in Model B and that experiencing poststorm hardship (at the individual level) had a significant association with functional limitations. People experiencing more poststorm hardship also had more functional limitations. Here too, living in a FEMA-defined storm damaged county (Level 2) was not associated with functional limitations.
Fit indices comparing Model C-1, C-2, and C-3 to Model B suggested an improvement in fit for each model (see Table 3); model C-1 with peri-traumatic stress having better fit indices than either personal and property loss or poststorm hardship. Finally, Model D, which included all four forms of disaster exposure, revealed that all the previously tested parameters remained the same as in Model B and that peri-traumatic stress at the individual level was the only exposure variable associated with functional limitations. Personal and property loss, poststorm hardship (Level 1 variables), and living in a FEMA-defined storm damaged county (Level 2) were not associated with functional limitations. Thus, when accounting for all four types of exposure in one model, people with higher levels of peri-traumatic stress had an increase in functional limitations. Fit indices comparing Model D to Model B suggested an improvement in fit; however, the fit indices were similar to that of model C-1 (peri-traumatic stress).
Discussion
These results extend Tsuboya and colleagues (33) findings and demonstrate the effects of a natural disaster—in this case Hurricane Sandy—on functional limitations. Using a large, representative sample and data collected before and after the hurricane, we found that peri-traumatic stress and poststorm hardship each had a significant negative association with trajectories of functional limitations, but personal and property loss was not associated with functional limitations. Moreover, when the exposure variables were all included in the model simultaneously, we found the sole predictor of functional limitations was peri-traumatic stress.
These results along with previous findings (14,15,43) identify the critical role peri-traumatic stress plays for both the physical and emotional health of older people confronted by a natural disaster and beg for interventions focused on older people experiencing natural disasters. The analyses suggest that when possible, it might be wise for older people to evacuate before a natural disaster strikes, although doing so may create other stress not measured in our data. If this is not possible, our analyses suggest the importance of attending to older people who experience fear in the face of disaster as soon as possible. Consistent with earlier studies, our findings affirm that fear experienced during a natural disaster is linked to physical functioning following the disaster (18,28). The mechanisms for this association are not tested here. However, in accordance with prior work focused on chronic stress (51), it may be that exposure to the stressful life event may have a cumulative effect with other stressors these individuals have experienced and cause changes in the brain and subsequently the body’s functioning. Further work should explore this pathway.
By classifying exposure in four distinct ways, we were able to tease apart the effects of storm exposure on functional limitations. We did not find effects of disaster exposure on functional limitations when treating either personal and property loss or geographic location as exposure. Geographic location may be too crude of an exposure indicator. As is true for other hurricanes, there was some randomness to the path taken by Hurricane Sandy. Homes within just a few blocks of one another sustained very different effects, with some homes totally destroyed while others bore no damage. Other research finds that personal and property loss following a disaster have inconsistent relationships with psychological well-being (46,47,52). These inconsistencies may be explained at least partly as a function of the time between the disaster and when the data were collected. It is possible that over time, people are able to cope with personal and property losses; hence their effects on functional limitations are minimal. Finally, although functional limitation trajectories were associated with poststorm hardship when this was the only exposure variable in the model, when modeled with geographic exposure, peri-trauma stress, and personal and property loss, the effect of poststorm hardship became nonsignificant.
These findings affirm the need to expand disaster exposure definitions beyond geographic proximity and to utilize individual-level assessments of exposure to advance disaster research. As we strive to understand the mechanisms by which exposure affects functional limitations and then develop interventions to break the relationship, it will be important to develop alternative ways of measuring what it means to be exposed to a disaster.
These findings add important new information to the literature, as they show that disasters affect physical health as well as emotional health. Given the importance of functional limitations for mortality, morbidity, and quality of life in older adults, it is critical to understand the role of disasters in influencing functional limitations over time. Where scholars have attempted to examine the impact of exposure on functional limitations, general indicators of exposure (ie, geographic region) have been used and prestorm data have been lacking, with the exception of Tsuboya and colleagues (33) study with the Great Earthquake.
While this study is strengthened by its use of data from a large prospective longitudinal panel study of older adults and its analytic approach that modeled exposure at both the level of the individual and county, it is not without limitation. The findings here are restricted to the experiences of those living in the state of New Jersey that were retained in our sample. Attrition over time resulted in an underrepresentation of people with lower education, lower income, and/or of minority status and therefore is not representative of all populations. Second, storm exposure was assessed between 12 and 53 months after the Hurricane and is subject to biased recall of the events. Future studies should attempt to collect data more proximal to the disaster on hand. Third, our measure of peri-traumatic stress was also limited in that it only included two items; future work should develop and test additional measures of peri-traumatic stress to see whether the findings here hold. Finally, our measure of functional ability is one of self-report. While self-reported physical function has been found to be associated with disability (53), given that individuals who experience greater psychological distress are more likely to experience pain and fatigue, those with greater distress may also be self-reporting greater functional limitation due to their psychological state. Use of an objective measure of functional ability may be better able to disentangle the association between reported distress and physical health outcomes and future work should explore this possibility.
Overall, despite limitations, findings from this work advance our understanding of the impact of disasters on older adults’ health. Beyond known mental health impacts of a disaster, we find that peri-storm psychological stress can affect an individual’s functional limitations following a disaster. We also see that how disaster exposure is assessed matters for conclusions drawn. Future work is needed to determine whether individual-level reports of disaster exposure in the context of other types of disaster also show similar findings and to determine the mechanisms by which peri-traumatic stress impacts functional limitations to develop poststorm interventions for older people exposed to a disaster.
Funding
This work was supported by the University of Medicine and Dentistry of New Jersey, the Assistant Secretary for Preparedness & Response (1 HITEP130008), and the National Institute on Aging (R01AG046463).
Acknowledgments
R.P. developed the idea for the paper and developed the Introduction. M.W.-G. ran all analyses and developed the Results section. A.R.H. developed the Methods section. F.P.C. assisted with literature review. All authors participated in writing and editing the manuscript.
Conflict of Interest
None reported.
References
- 1. Red Cross IFo. World Disasters Report: Leaving no one Behind. 2018. https://media.ifrc.org/ifrc/wp-content/uploads/sites/5/2018/10/B-WDR-2018-EN-LR.pdf. Accessed May 23, 2019. [Google Scholar]
- 2. Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J Consul Clin Psychol. 2007;75:671–682. doi:10.1037/0022-006X.75.5.671 [DOI] [PubMed] [Google Scholar]
- 3. Somes J, Stephens Donatelli N. Disaster planning considerations involving the geriatric patient: part I. J Emerg Nurs. 2012;38:479–481. doi:10.1016/j.jen.2012.05.024 [DOI] [PubMed] [Google Scholar]
- 4. Claver M, Dobalian A, Fickel JJ, Ricci KA, Mallers MH. Comprehensive care for vulnerable elderly veterans during disasters. Arch Gerontol Geriatr. 2013;56:205–213. doi:10.1016/j.archger.2012.07.010 [DOI] [PubMed] [Google Scholar]
- 5. Zhu XX, Sun BQ. Study on earthquake risk reduction from the perspectives of the elderly. Saf Sci. 2017;91:326–334. doi:10.1016/j.ssci.2016.08.028 [Google Scholar]
- 6. CDC. Deaths Associated with Hurricane Sandy; 2013. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6220a1.htm. Accessed June 28, 2019. [Google Scholar]
- 7. IDMC. Global Estimates 2012: People Displaced by Disasters. Geneva, Switzerland; 2013. http://www.internal-displacement.org/assets/publications/2013/2012-global-estimates-corporate-en.pdf. Accessed June 28, 2019. [Google Scholar]
- 8. FEMA. FEMA Fact Sheet: Mitigation Assessment Team Results—Hurricane Sandy. Washington, DC; 2018. https://www.fema.gov/mat-results-hurricane-sandy. Accessed July 1, 2019. [Google Scholar]
- 9. Commerce USDo. Service Assessment Hurricane/Post-tropical Cyclone Sandy. Washington, DC; 2013. https://www.weather.gov/media/publications/assessment/Sandy13.pdf. Accessed July 1, 2019. [Google Scholar]
- 10. Kim S, Kulkarni PA, Rajan M, et al. Hurricane sandy (new jersey): mortality rates in the following month and quarter. Am J Public Health. 2017;107:1304–1307. doi:10.2105/AJPH.2017.303826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38:467–480. doi:10.1017/S0033291707001353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310:507–518. doi:10.1001/jama.2013.107799 [DOI] [PubMed] [Google Scholar]
- 13. Kessler RC, Galea S, Gruber MJ, Sampson NA, Ursano RJ, Wessely S. Trends in mental illness and suicidality after Hurricane Katrina. Mol Psychiatry. 2008;13:374–384. doi:10.1038/sj.mp.4002119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tang B, Liu X, Liu Y, Xue C, Zhang L. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health. 2014;14:623. doi:10.1186/1471-2458-14-623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wilson-Genderson M, Heid AR, Pruchno RA. Long-term effects of disaster on depressive symptoms: type of exposure matters. Soc Sci Med. 2018;217:84–91. doi:10.1016/j.socscimed.2018.09.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry. 2014;71:1025–1031. doi:10.1001/jamapsychiatry.2014.652 [DOI] [PubMed] [Google Scholar]
- 17. Freedman VA, Spillman BC, Andreski PM, et al. Trends in late-life activity limitations in the United States: an update from five national surveys. Demography. 2013;50:661–671. doi:10.1007/s13524-012-0167-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Clouston SA, Guralnik JM, Kotov R, Bromet EJ, Luft BJ. Functional limitations among responders to the world trade center attacks 14 years after the disaster: implications of chronic posttraumatic stress disorder. J Trauma Stress. 2017;30:443–452. doi:10.1002/jts.22219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295:2018–2026. doi:10.1001/jama.295.17.2018 [DOI] [PubMed] [Google Scholar]
- 20. Brown JS, Cherry KE, Marks LD, et al. After hurricanes Katrina and Rita: gender differences in health and religiosity in middle-aged and older adults. Health Care Women Int. 2010;31:997–1012. doi:10.1080/07399332.2010.514085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wu J, Xiao J, Li T, et al. A cross-sectional survey on the health status and the health-related quality of life of the elderly after flood disaster in Bazhong city, Sichuan, China. BMC Public Health. 2015;15:163. doi:10.1186/s12889-015-1402-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clouston SA, Brewster P, Kuh D, et al. The dynamic relationship between physical function and cognition in longitudinal aging cohorts. Epidemiol Rev. 2013;35:33–50. doi:10.1093/epirev/mxs004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moreira B, Sampaio RF, Furtado SR, Dias RC, Kirkwood RN. The relationship between diabetes mellitus, geriatric syndromes, physical function, and gait: a review of the literature. Curr Diabetes Rev. 2016;12:240–251. doi:10.2174/1573399811666150615142746 [DOI] [PubMed] [Google Scholar]
- 24. Zutler M, Singer JP, Omachi TA, et al. Relationship of obesity with respiratory symptoms and decreased functional capacity in adults without established COPD. Prim Care Respir J. 2012;21:194–201. doi:10.4104/pcrj.2012.00028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Geerlings SW, Beekman AT, Deeg DJ, Twisk JW, Van Tilburg W. The longitudinal effect of depression on functional limitations and disability in older adults: an eight-wave prospective community-based study. Psychol Med. 2001;31:1361–1371. doi:10.1017/s0033291701004639 [DOI] [PubMed] [Google Scholar]
- 26. Choi HC, Son KY, Cho B, Park SM, Cho SI. An implication of the short physical performance battery (SPPB) as a predictor of abnormal pulmonary function in aging people. Arch Gerontol Geriatr. 2012;54:448–452. doi:10.1016/j.archger.2011.03.010 [DOI] [PubMed] [Google Scholar]
- 27. Brunner EJ, Welch CA, Shipley MJ, et al. Midlife risk factors for impaired physical and cognitive functioning at older ages: a cohort study. J Gerontol A Biol Sci Med Sci. 2017;72:237–242. doi:10.1093/gerona/glw092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tanji F, Sugawara Y, Tomata Y, et al. Psychological distress and the incident risk of functional disability in elderly survivors after the great east Japan earthquake. J Affect Disord. 2017;221:145–150. doi:10.1016/j.jad.2017.06.030 [DOI] [PubMed] [Google Scholar]
- 29. Tomata Y, Suzuki Y, Kakizaki M, Kawado M, Hashimoto S, Tsuji I. Impact of the 2011 great east Japan earthquake and tsunami on functional disability among older people: a longitudinal comparison of disability prevalence among Japanese municipalities. J Epidemiol Community Health. 2014;68:530–533. doi:10.1136/iech-2013-203541 [DOI] [PubMed] [Google Scholar]
- 30. Tomata Y, Suzuki Y, Kawado M, et al. Long-term impact of the 2011 great east Japan earthquake and tsunami on functional disability among older people: a 3-year longitudinal comparison of disability prevalence among Japanese municipalities. Soc Sci Med. 2015;147:296–299. doi:10.1016/j.socscimed.2015.11.016 [DOI] [PubMed] [Google Scholar]
- 31. Deeg DJ, Huizink AC, Comijs HC, Smid T. Disaster and associated changes in physical and mental health in older residents. Eur J Public Health. 2005;15:170–174. doi:10.1093/eurpub/cki126 [DOI] [PubMed] [Google Scholar]
- 32. Brilleman SL, Wolfe R, Moreno-Betancur M, et al. Associations between community-level disaster exposure and individual-level changes in disability and risk of death for older Americans. Soc Sci Med. 2017;173:118–125. doi:10.1016/j.socscimed.2016.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tsuboya T, Aida J, Hikichi H, et al. Predictors of decline in IADL functioning among older survivors following the great east Japan earthquake: a prospective study. Soc Sci Med. 2017;176:34–41. doi:10.1016/j.socscimed.2017.01.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gulley SP, Rasch EK, Bethell CD, et al. At the intersection of chronic disease, disability and health services research: a scoping literature review. Disabil Health J. 2018;11:192–203. doi:10.1016/j.dhjo.2017.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Jindai K, Nielson CM, Vorderstrasse BA, Quinones AR. Multimorbidity and functional limitations among adults 65 or older, NHANES 2005–2012. Prev Chronic Dis. 2016;13:E151. doi:10.5888/pcd13.160174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lin J. Inter-individual variability in trajectories of functional limitations by race/gender. J Gerontol B Psychol Sci Soc Sci. 2019. doi:10.1093/geronb/gby156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Potente C, Monden C. Disability pathways preceding death in England by socio-economic status. Popul Stud (Camb). 2018;72:175–190. doi:10.1080/00324728.2018.1458993 [DOI] [PubMed] [Google Scholar]
- 38. Rector JL, Marceau K, Friedman EM. Moderation of the association between chronic medical conditions and functional limitations over time by physical activity: effects of age. J Gerontol A Biol Sci Med Sci. 2019. doi:10.1093/gerona/glz020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Timmermans EJ, Hoogendijk EO, Broese van Groenou MI, et al. Trends across 20 years in multiple indicators of functioning among older adults in the Netherlands. Eur J Public Health. 2019. doi:10.1093/eurpub/ckz065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. von dem Knesebeck O, Vonneilich N, Ludecke D. Income and functional limitations among the aged in Europe: a trend analysis in 16 countries. J Epidemiol Community Health. 2017;71:584–591. doi:10.1136/jech-2016-208369 [DOI] [PubMed] [Google Scholar]
- 41. Blumberg SJ, Luke JV. Coverage bias in traditional telephone surveys of low-income and young adults. Public Opinion Quarterly. 2007;71:734–749. doi:10.1093/poq/nfm047 [Google Scholar]
- 42. Pruchno RA, Wilson-Genderson M, Rose M, Cartwright F. Successful aging: early influences and contemporary characteristics. Gerontologist. 2010;50:821–833. doi:10.1093/geront/gnq041 [DOI] [PubMed] [Google Scholar]
- 43. Bell CJ, Boden JM, Horwood LJ, Mulder RT. The role of peri-traumatic stress and disruption distress in predicting symptoms of major depression following exposure to a natural disaster. Aust N Z J Psychiatry. 2017;51:711–718. doi: 10.1177/0004867417691852 [DOI] [PubMed] [Google Scholar]
- 44. Slopen N, Williams DR, Fitzmaurice GM, Gilman SE. Sex, stressful life events, and adult onset depression and alcohol dependence: are men and women equally vulnerable? Soc Sci Med. 2011;73:615–622. doi:10.1016/j.socscimed.2011.06.022 [DOI] [PubMed] [Google Scholar]
- 45. Lieberman-Cribbin W, Liu B, Schneider S, Schwartz R, Taioli E. Self-reported and FEMA flood exposure assessment after hurricane sandy: association with mental health outcomes. PLoS ONE. 2017;12:e0170965. doi:10.1371/journal.pone.0170965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Schwartz R, Gillezeau CN, Liu B, Lieberman-Cribbin W, Taioli E. Longitudinal impact of hurricane sandy exposure on mental health symptoms. Int J Environ Res Public Health. 2017;14. doi: 10.3390/ijerph14090957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lowe SR, Sampson L, Gruebner O, Galea S. Psychological resilience after hurricane sandy: the influence of individual- and community-level factors on mental health after a large-scale natural disaster. PLoS ONE. 2015;10:e0125761. doi:10.1371/journal.pone.0125761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. HUD. Second allocation, waivers, and alternative requirements for grantees receiving community development block grant (CDBG) disaster recovery funds in response to hurricane sandy. Washington DC: Federal Register; 2013. 2013–27506. https://www.federalregister.gov/documents/2013/11/18/2013–27506/second-allocation-waivers-and-alternative-requirements-for-grantees-rece. Accessed July 1, 2019. [Google Scholar]
- 49. Singer JD, Willet JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 50. Berry SD, Ngo L, Samelson EJ, Kiel DP. Competing risk of death: an important consideration in studies of older adults. J Am Geriatr Soc. 2010;58:783–787. doi:10.1111/j.1532-5415.2010.02767.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Conrad CD, Ortiz B, Judd JM. Review: chronic stress and hippocampal dendritic complexity: methodological and functional considerations. Physiol Behav. 2017:178;66–81. doi:10.1016/j.physbeh.2016.11.017 [DOI] [PubMed] [Google Scholar]
- 52. Tsuboya T, Aida J, Hikichi H, et al. Predictors of depressive symptoms following the great east Japan earthquake: a prospective study. Soc Sci Med. 2016;161:47–54. doi:10.1016/j.socscimed.2016.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mayhew AJ, Griffith LE, Gilsing A, et al. The association between self-reported and performance-based physical function with activities of daily living disability in the Canadian Longitudinal Study of Aging. J Gerontol A Biol Sci Med Sci. 2019. doi:10.1093/gerona/glz122 [DOI] [PMC free article] [PubMed] [Google Scholar]