Abstract
Background
Metastatic Merkel cell carcinoma (mMCC) is an aggressive neuroendocrine malignancy of the skin with a poor prognosis. Immune checkpoint inhibitors (ICIs) have shown substantial efficacy and favorable safety in clinical trials.
Methods
Medical records of patients (pts) with mMCC treated with ICIs from August 2015 to December 2018 at Peter MacCallum Cancer Centre in Australia were analyzed. Response was assessed with serial imaging, the majority with FDG-PET/CT scans. RNA sequencing and immunohistochemistry for PD-L1, CD3 and Merkel cell polyomavirus (MCPyV) on tumor samples was performed.
Results
23 pts with mMCC were treated with ICIs. A median of 8 cycles (range 1 to 47) were administered, with treatment ongoing in 6 pts. Objective responses (OR) were observed in 14 pts (61%): 10 (44%) complete responses (CR) and 4 (17%) partial responses (PR). Median time to response was 8 weeks (range 6 to 12) and 12-month progression-free survival rate was 39%. Increased OR were seen in pts aged less than 75 (OR 80% vs 46%), no prior history of chemotherapy (OR 64% vs 50%), patients with an immune-related adverse event (OR 100% vs 43%) and in MCPyV-negative tumors (OR 69% vs 43%). Pts with a CR had lower mean metabolic tumor volume on baseline FDG-PET/CT scan (CR: 35.7 mL, no CR: 187.8 mL, p=0.05). There was no correlation between PD-L1 positivity and MCPyV status (p=0.764) or OR (p=0.245). 10 pts received radiation therapy (RT) during ICI: 4 pts started RT concurrently (OR 75%, CR 50%), 3 pts had isolated ICI-resistant lesions successfully treated with RT and 3 pts with multisite progression continued to progress despite RT. Overall, 6 pts (26%) had grade 1–2 immune-related adverse events.
Conclusion
ICIs showed efficacy and safety in mMCC consistent with trial data. Clinical and imaging predictors of response were identified.
Keywords: skin neoplasms, immunotherapy, gene expression profiling, tumor biomarkers
Background
Merkel cell carcinoma (MCC) is an aggressive neuroendocrine malignancy of the skin, with a historical 5-year overall survival (OS) rate of 15% to 27% for patients with metastatic disease.1 Until recently, chemotherapy was the mainstay of treatment for metastatic MCC (mMCC), resulting in a median progression-free survival (PFS) of 3 months.2 Merkel cell polyomavirus (MCPyV) and ultraviolet (UV) carcinogenesis are implicated in MCC development.3 4 While both mechanisms drive tumorigenesis, they also induce potent adaptive immune responses to either viral antigens or neoantigens. An increased incidence of MCC in immunosuppressed patients suggests that immune escape is essential for MCC development5 6 and that targeting immune evasion may be an effective treatment strategy.
Immune checkpoint inhibitors (ICIs) have emerged as an attractive treatment option for patients with mMCC. In the phase II JAVELIN Merkel 200 trial, 88 patients who had failed prior chemotherapy were treated with avelumab, with a response rate (RR) of 33%, 2-year PFS rate of 26% and median duration of response not yet reached.7 Responses appear to be superior in the first-line setting, with an interim analysis of part B of the Javelin Merkel 200 trial demonstrating an RR of 62% in 39 patients with no prior cytotoxic treatment for metastatic disease.8 Similar promising results have been seen with other ICIs; pembrolizumab achieved an RR of 56% in the first-line setting in 50 patients with advanced MCC (unresectable: 7, metastatic: 43), with 79% of responders in ongoing remission at 2 years and a 2-year OS rate of 68.7%.9
To date, there is limited published experience with ICIs in mMCC outside of a clinical trial setting, in which inclusion criteria, such as performance status and comorbid conditions, are restrictive. Further, predictive markers of response to ICIs in mMCC have not been well established. Herein, we describe our experience in using ICIs for mMCC as single agent therapy or concurrently with radiation at the Peter MacCallum Cancer Centre (PMCC) in Melbourne, Australia. We outline clinical, imaging and molecular characteristics of treatment response.
Methods
Study design and participants
All patients with mMCC treated with ICIs from August 1, 2015 to December 31, 2018 at PMCC were prospectively consented for inclusion in a longitudinal MCC biomarker study (HREC number: 14/113). Clinical data including patient demographics, staging, prior treatments, response and toxicity assessments were annotated prospectively. Formalin-fixed paraffin-embedded (FFPE) tissue from a primary or metastatic site was collected for all patients. Most patients had [18F]-fluoro-2-deoxyglucose-PET/CT (FDG-PET/CT) imaging at baseline and every 8–12 weeks to monitor treatment response (n=19), with CT alone used to assess response in a minority of patients (n=4).
Medical records and the study-specific database were retrospectively analyzed to collect information on patient and disease characteristics, treatment course and outcomes. Baseline FDG-PET/CT metabolic tumor volume (MTV) was evaluated by a nuclear medicine technologist (JC) using proprietary software (MIMencore, V.6.7). The MTV was contoured using a patient-specific threshold of 1.5× liver standardized uptake value (SUV) mean+2 standard deviations (SD) of the liver SUV.10 Manual adjustments were made for disease that was only mildly FDG-avid and fell below this threshold in consultation with an experienced FDG-PET/CT reader (RJH). Response evaluation was undertaken with PET Response Criteria in Solid Tumors (PERCIST) criteria for FDG-PET/CT10 and Response Evaluation Criteria in Solid Tumors (RECIST) 1.1 for CT scans.11 For convenience of reporting overall response rates, metabolic response criteria of complete and partial metabolic response (CMR and PMR) were combined with morphologic responses of complete and partial responses (CR and PR), respectively.
Immunohistochemistry (IHC)
IHC was performed on 4 µm FFPE sections. MCPyV (clone CM2B4; cat sc-136172, Santa Cruz Biotechnology, Santa Cruz, CA; dilution 1:100) and CD3 (clone LN10; cat NCL-L-CD3-565, Newcastle, UK; dilution 1:200) staining was performed on the Leica Bond III Autostainer. For programmed death-ligand 1 (PD-L1), IHC clone SP263 was used (Assay v1.00.0001, using the VENTANA OptiView DAB IHC Detection Kit on the BenchMark ULTRA autostainer). Semiquantitative scoring was performed by a single pathologist blinded to the clinical data. T cells were scored by counting the mean number of positive cells in tumor per high-power field (0.55 mm diameter). PD-L1 scoring was performed using a standardized approach that has been described previously.12 Briefly, two scores were derived; the tumor proportion score (TPS), which represents the percentage of tumor cells showing positive membranous expression of PD-L1, and the immune cell score (IC), which represents the proportion of tumor area occupied by PD-L1–positive immune cells. TPS and IC assessment was based on the entire tumor area on a single representative slide. A minimum of 50 tumor cells were required for a tumor to be considered assessable for TPS and IC. Four and three patients did not have sufficient material for PD-L1 and CD3 IHC, respectively, and were excluded from this analysis.
RNA-sequencing (RNA-Seq)
RNA was prepared using the NEBNext Ultra II Directional RNA Library Prep Kit for Illumina and libraries sequenced on the Illumina Nova-Seq 6000. For details on RNA-Seq bioinformatic analysis, including differential gene expression, gene set enrichment analysis, confirmation of viral status and variant calling, see the online supplemental methods. Three patients did not have sufficient material for RNA-Seq and were excluded from this analysis.
jitc-2020-000700supp001.pdf (270.4KB, pdf)
Statistical analysis
Baseline characteristics were summarized using standard descriptive statistics. Bivariate analyses using χ2 tests were used to compare treatment response by clinical and disease-specific biomarkers, including baseline FDG-PET/CT MTV. Univariable Cox proportional hazard regression was used to assess the association between CMR on early FDG-PET/CT scan and PFS and OS. All statistical analyses were performed using STATA (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
Results
Twenty-three patients with mMCC with a median age of 75 years (range 64 to 91) were treated with ICIs, with two-thirds (n=15, 65%) receiving treatment with the PD-L1 inhibitor avelumab. Ten patients (43%) had received prior chemotherapy, all within 6 months of starting ICI (4: adjuvant chemotherapy, 6: first-line treatment for mMCC). Baseline characteristics are summarized in table 1.
Table 1.
Baseline characteristics
| N (%) | |
| Age (years) | |
| Median (range) | 75 (64 to 91) |
| Sex | |
| Male | 18 (78) |
| Female | 5 (22) |
| ECOG Performance Status | |
| 0 | 8 (35) |
| 1 | 12 (52) |
| 2 | 3 (13) |
| Ethnicity | |
| Caucasian | 19 (83) |
| Mediterranean | 3 (13) |
| Pacific Islander | 1 (4) |
| Site of primary tumor | |
| Head and neck | 6 (26) |
| Upper limb | 5 (22) |
| Lower limb | 4 (17) |
| Trunk | 1 (4) |
| Unknown | 7 (30) |
| ICI | |
| Avelumab (PD-L1 inhibitor) | 15 (65) |
| Pembrolizumab (PD-1 inhibitor) | 5 (22) |
| Tislelizumab (PD-1 inhibitor) | 3 (13) |
| MCPyV status | |
| Positive | 7 (30) |
| Negative | 16 (70) |
| Presence of visceral disease | 17 (74) |
| Prior platinum-based chemotherapy | 10 (43) |
| Prior immunosuppression | 2 (9) |
| History of autoimmune disease | 2 (9) |
ECOG, Eastern Cooperative Oncology Group; ICI, immune checkpoint inhibitor; MCPyV, Merkel cell polyomavirus.
Clinical experience
A median of 8 cycles (range 1 to 47) of ICI were administered, with treatment ongoing in six patients. Objective responses (OR) were observed in 14 patients (61%), with CR as best response in 10 patients (44%) and PR in 4 patients (17%). Median time to response was 8 weeks (range 6 to 12), with all responders demonstrating a response on their first on-treatment scan. Median duration of response is not yet reached (95% CI 21 months to not reached). Twelve-month PFS rate was 39% for the entire cohort. Seventeen patients (74%) discontinued treatment: nine for progressive disease (PD), five for a treatment break given CR or stable PR, and three due to deterioration from a comorbid illness. The five patients who discontinued treatment in a CR or PR have maintained their response after an average of 8 months from treatment cessation.
Six patients (26%) had an immune-related adverse event (irAE), all of which were grade 1–2 (two maculopapular rash, one lichenoid rash, one Sweet’s syndrome, one arthritis, one hypothyroidism). All patients with an irAE had a response to ICI, with 5 of 6 (83%) achieving a CR. Two patients had a prior history of an autoimmune disease (rheumatoid arthritis) and were successfully treated with ICIs with no flare of their pre-existing condition and no irAEs.
Ten patients (43%) received radiation therapy (RT) during ICI treatment. Four patients received a palliative dose of RT (dose: 20 Gray (Gy) in 5 fractions) to a single site of disease concurrent with commencing ICI, with an OR of 75% and CR of 50%. Three patients had isolated ICI-resistant lesions treated with RT (dose: 20 Gy in 5 fractions), with a response at the irradiated site, allowing them to continue on ICI. This included a patient with a partial response elsewhere and an isolated progressive adrenal metastasis, a patient who achieved a CMR and then demonstrated oligoprogression in a liver lesion, and a patient who achieved a CMR apart from an ICI-resistant left cheek lesion. Three patients with globally progressive disease exhibited a response at the irradiated site but ongoing progressive disease elsewhere. Of note, only 2 (20%) patients who received RT during ICI treatment had an irAE, similar to the toxicity rate in the general cohort.
Clinical and FDG-PET/CT markers of ICI response
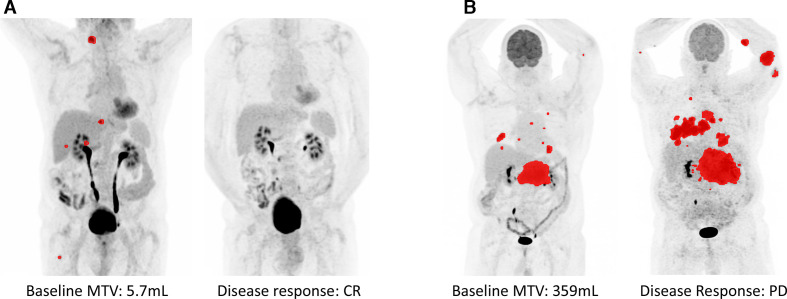
Increased OR was seen in patients aged less than 75 years (OR 8/10, 80% vs 46%), no history of prior chemotherapy (OR 9/14, 64% vs 50%), patients with an irAE (OR 6/6, 100% vs 47%) and in MCPyV-negative patients (OR 11/16, 69% vs 43%). These differences were not statistically significant, likely due to small patient numbers. For the 19 patients in whom FDG-PET/CT was used for response assessment, patients with a CMR had lower MTV on baseline scan (CMR: 35.7 mL, no CMR: 187.8 mL; p=0.05) (figure 1). Similarly, CMR on early FDG-PET/CT scan (performed within 12 weeks of ICI initiation) may be a surrogate for PFS (HR 0.31; p=0.38) and OS (HR 0.24; p=0.19), although this trend needs to be confirmed with greater patient numbers.
Figure 1.
Baseline FDG-PET/CT metabolic tumor volume. (A) Patient 113 with baseline metabolic tumor volume (MTV) of 5.7 mL had a complete response to immune checkpoint inhibitor (ICI). (B) Patient 110 with baseline MTV of 359 mL had primary refractory disease and progressed through ICI.
Molecular markers of ICI response
No correlation was seen between IHC tumor PD-L1 positivity and MCPyV status (p=0.764) or response to ICI (p=0.245). Similarly, no significant association was seen between ICI response and number of CD3+ T cells within the tumor, with an unexpected trend toward higher T-cell infiltration in non-responders (p=0.066).
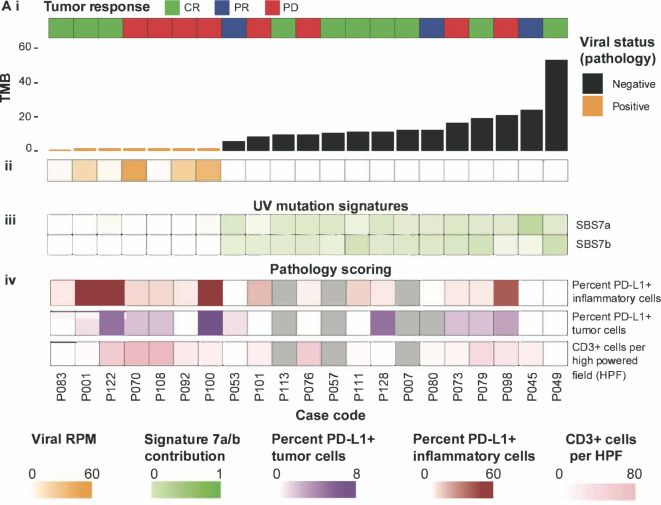
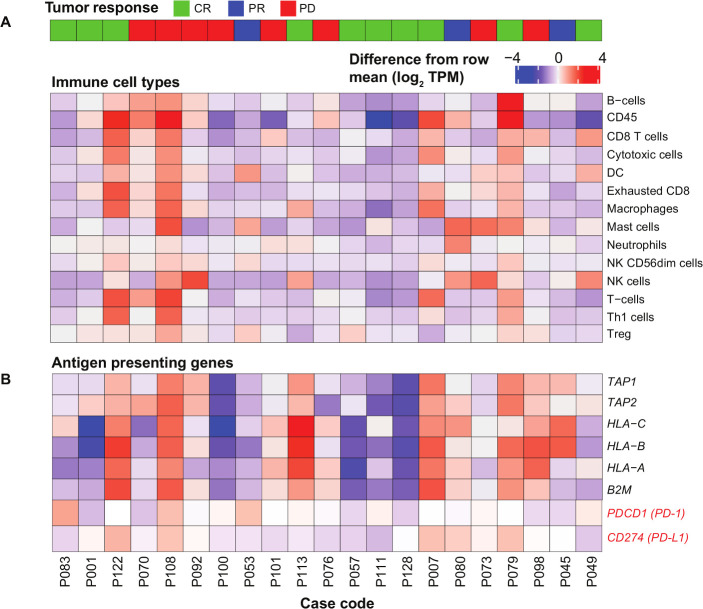
RNA-Seq confirmed the previously established hallmarks of MCC subtypes. Elevated MCPyV transcripts were restricted to MCPyV-positive tumors (validating MCPyV IHC), while MCPyV-negative tumors had higher tumor mutational burden (TMB) and characteristic UV-mutation signatures (COSMIC v3 Sig7a/b) (figure 2, i–iii). Consistent with results from IHC scoring (figure 2, iv), there was no association between ICI response and the averaged gene expression of immune cell type specific markers (figure 3A) identified from a large compendium of other cancer transcriptomic data (online supplemental table S1).13 Similarly, no association was observed between ICI response and antigen presentation machinery or PD1/PD-L1 mRNA expression (figure 3B).
Figure 2.
Immunotherapy response, TMB, viral status, UV-associated mutation signatures and PD-L1/CD3+ staining of the cohort. (i) The tumor mutational burden (TMB) calculated from RNA-Seq for each of the samples. Samples are ordered by TMB in this panel and throughout the rest of the figure. Samples are colored by viral status determined from viral antibody staining. The heatmap below (ii) shows the number of viral reads present in each sample as determined by Xenomapper30 divided by the number of mapped reads in each library multiplied by 1×106 (RPM). (iii) The relative contribution of UV-associated mutation signatures 7a and 7b to each sample in the cohort. Mutation signatures were generated for each sample in the cohort using MutationalPatterns.31 Samples were compared against single bases substitution (SBS) signatures from COSMIC v3.32 33 (iv) Pathology scoring of the percentage of PD-L1 positive tumor and immune cells from immunohistochemical staining of each sample as well as the number of CD3+ cells per high-power field studied. CR, complete response; PD, progressive disease; PR, partial response.
Figure 3.
Immune landscape of the cohort. (A) The expression of genes suggested to be associated with particular immune cell types.13 (B) The expression of genes known to be associated with antigen presentation machinery. The expression of PD-1 (PDCD1) and PD-L1 (CD274) is highlighted in red. Both panels are mean centered log2 (TPM+1). CR, complete response; PD, progressive disease; PR, partial response.
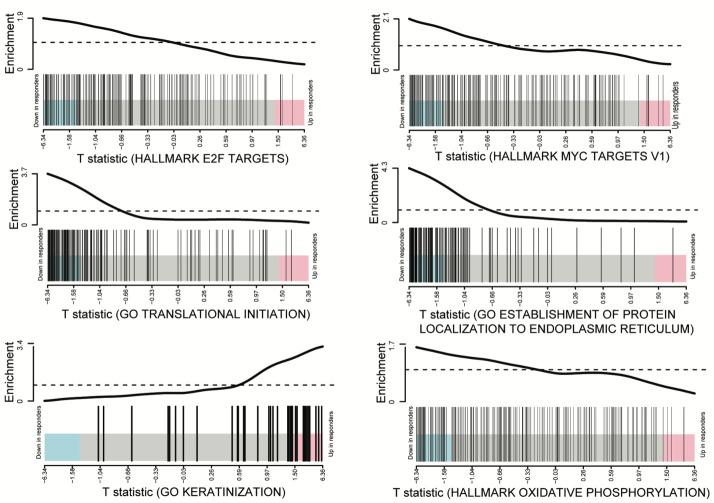
Differential expression analysis was done by comparing responders to non-responders while accounting for the effect of viral status. Only two genes were found to be significantly differentially expressed (COL9A3 and KIF19, false discovery rate (FDR)<0.05). Neither gene has any known biological relevance to ICI response, T-cell function or the biology of MCC. On the contrary, gene set enrichment analysis identified 7 significantly enriched (FDR<0.05) hallmark gene sets (online supplemental table S2) and 74 gene ontology (GO) gene sets (online supplemental table S3). Gene sets downregulated in the responders (compared with non-responders) included Hallmark gene sets E2F targets, MYC targets (v1) and Oxidative Phosphorylation as well as GO gene sets of translational initiation and protein localization to endoplasmic reticulum (figure 4). Gene sets upregulated in responders were associated with keratinocyte differentiation.
Figure 4.
Barcodeplots highlighting lower cellular growth markers in responders. Limma barcodeplots of the “E2F targets” and “MYC targets (V1)” gene sets from the MSigDB. There is a clear reduction in the expression of many of the genes in these gene sets in tumors that responded to immune checkpoint inhibitor, suggesting lower proliferation in these samples. Limma barcodeplots of the “GO translational initiation” and “GO establishment of protein localisation to the endoplasmic reticulum” gene sets from the MSigDB. These gene sets again highlight a signature of reduced proliferation in responders.
Discussion
Consistent with clinical trial data, the majority of patients (61%) responded to ICIs and these responses were notable for their durability, including ongoing disease remission after treatment cessation. Treatment was well tolerated in this elderly population, with no treatment-related deaths or discontinuation due to toxicity. This included patients who received concurrent RT during ICI therapy. Our experience highlights the safety and potential efficacy of combining ICIs and RT, both to enhance initial response and to manage oligoresistant lesions.
We identified clinical and imaging factors associated with increased responses, including lack of prior chemotherapy, younger age, MCPyV-negative tumors, lower baseline FDG-PET/CT MTV and development of treatment-related irAEs. The correlation between irAEs and improved response to ICIs is consistent with other tumor types,14–16 particularly with respect to cutaneous side effects, which comprised half of the toxicity seen in our cohort. However, this association has not previously been reported with MCC.
While previous studies have not found a statistically significant difference in ICI response based on MCPyV status,9 our cohort and others indicate that MCPyV-negative mMCC may have an enhanced response to ICIs,17 potentially attributed to higher TMB,17 18 a phenomenon described in multiple tumor types.19 MCPyV-negative MCCs have been found to harbor more tumor neoantigens than melanoma,18 a cancer highly responsive to ICI. A recent study that characterized the genomic landscape of 317 MCC tumors confirmed a bimodal distribution of TMB, with a strong negative association between TMB and MCPyV DNA.17 However, despite the likelihood of neoantigens being the major driver of immunogenicity in MCPyV-negative tumors, we did not see a correlation between TMB and ICI response within the MCPyV-negative tumors. This may be due to an insufficient number of cases for analysis or that ICI response in MCPyV-negative tumors is dependent on additional tumor intrinsic and/or extrinsic factors.
To our knowledge, this is the first study to identify a significant association between baseline FDG-PET/CT MTV and response to ICI in mMCC. FDG-PET/CT scans have been shown to be a sensitive and reliable imaging modality to stage patients with mMCC and assess treatment response. Further, a metabolic response on FDG-PET/CT has been shown to be significantly associated with overall survival in patients with mMCC.20 21 Previous studies have noted a trend toward increased response rates in patients with lower disease burden, as defined by the sum of the target lesion diameters,7 which is substantiated by our results. These findings mirror results from other cancers, particularly melanoma, where lower baseline tumor burden has been shown to be associated with both response to ICI and improved survival.22 23 This may be related to increased tumor heterogeneity with high-volume disease, with the former associated with less tumor immune cell infiltration and reduced activation of the immune response.24 Increased tumor cell volume may also contribute to enhanced secretion of cytokines stimulating regulatory T-cell development in the tumor microenvironment (TME),25 with a corresponding inhibitory effect on response to ICI. The presence of increased hypoxia in the TME of larger lesions may also be immunosuppressive.26 27 Overall, this finding underscores a potential benefit of routine surveillance imaging following treatment of early-stage MCC to enable earlier detection of lower volume recurrence, particularly during the first 2 years after locoregional treatment when risk of recurrence is highest.1
Identification of reliable biomarkers to predict ICI response in MCC has thus far proven challenging. In our cohort, we found several outlier cases that do not support the notion of increased ICI response corresponding to an inflamed TME. Patient P108 did not respond to ICI, despite having a highly inflamed tumor with strong expression of immune markers. The tumor biopsy was taken prior to treatment with chemotherapy; therefore, we cannot exclude the possibility that chemotherapy altered the immune profile of the tumor. In contrast, five patients (P001, P057, P083, P111, P128) with low expression of immune markers responded to ICI. The average MTV for four of these patients with baseline FDG-PET/CT scans was 29.49 mL, which was significantly lower than the general cohort (p<0.01), further supporting the finding that low-volume disease is an important factor in predicting robust responses to ICI, even in patients without an inflamed tumor phenotype.
RNA-Seq analysis identified a number of gene sets enriched in non-responders indicating increased ribogenesis, translational initiation and post-translational processing as well as upregulation of cell cycle checkpoints. These results are in keeping with increased cell growth and proliferation of tumor cells in the non-responders. ICI responders conversely had upregulation of gene sets associated with keratinocyte differentiation, which is intriguing considering that epidermal keratinocyte precursor cells are hypothesized to be a putative MCC cell of origin.28 Upregulation of a hallmark gene set of oxidative phosphorylation in the non-responders may indicate a higher level of aerobic metabolism in this group, which is consistent with a recent study reporting oxidative metabolism as a barrier to PD-1 blockade in other tumor types.27 The gene sets identified in this study will require validation in an independent MCC patient cohort, but they highlight potential resistance mechanisms to ICIs in this disease and point to opportunities for rational drug combinations to overcome this resistance. For example, metformin inhibits mitochondrial complex I and has been shown to decrease tumor oxygen consumption rate in preclinical models, with this reduction in tumor oxidative phosphorylation signaling able to remodel the hypoxic TME and enhance response to ICIs.29
This study is limited by the retrospective nature, although annotation of toxicity was undertaken prospectively and calculation of baseline MTV was done independent of medical records by a single molecular imaging technologist and independently reviewed by an expert with over 30 years of experience in PET imaging to ensure accuracy and consistency. A larger sample size would be needed to more formally assess for statistical significance of the trends noted in our cohort. Ongoing research with ICI therapy in patients with mMCC should focus on elucidating markers of response as well as investigating rational treatment combinations.
Conclusion
In this study, ICIs showed efficacy and safety in mMCC consistent with trial data, with durable responses that persisted even after treatment discontinuation. Clinical and imaging predictors of response were identified. While no clear molecular biomarker emerged, RNA-sequencing identified gene sets enriched in non-responders, identifying potential resistance mechanisms that warrant additional evaluation.
Footnotes
AMW, AP, RWT and SS contributed equally.
Contributors: AMW collated the clinical data, performed statistical analysis and was a major contributor in writing the manuscript. AP performed the RNA-sequencing and differential gene expression analysis and was a major contributor in writing the manuscript. SB helped with the translational aspects of the study. PB collated the clinical data and contributed in writing the manuscript. JR and AH prospectively consented patients to the study and collected biospecimens and clinical data. AJG performed IHC analysis on the samples. JC and RJH collected the FDG-PET/CT data and calculated baseline FDG-PET/CT MTV. PDI, MC, GA-Y and GAM contributed to the study concept and contributed in writing the manuscript. SS oversaw the study and data collection and was a major contributor in writing the manuscript. RWT led the translational aspects of the study and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the Peter MacCallum Cancer Centre Human Research Ethics Committee (HREC no. 14/113). All patients were prospectively consented to participate in the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request.
References
- 1.Harms KL, Healy MA, Nghiem P, et al. . Analysis of prognostic factors from 9387 Merkel cell carcinoma cases forms the basis for the new 8th edition AJCC Staging System. Ann Surg Oncol 2016;23:3564–71. 10.1245/s10434-016-5266-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iyer JG, Blom A, Doumani R, et al. . Response rates and durability of chemotherapy among 62 patients with metastatic Merkel cell carcinoma. Cancer Med 2016;5:2294–301. 10.1002/cam4.815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wong SQ, Waldeck K, Vergara IA, et al. . UV-associated mutations underlie the etiology of MCV-negative Merkel cell carcinomas. Cancer Res 2015;75:5228–34. 10.1158/0008-5472.CAN-15-1877 [DOI] [PubMed] [Google Scholar]
- 4.Feng H, Shuda M, Chang Y, et al. . Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science 2008;319:1096–100. 10.1126/science.1152586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Femia D, Prinzi N, Anichini A, et al. . Treatment of advanced Merkel cell carcinoma: current therapeutic options and novel immunotherapy approaches. Target Oncol 2018;13:567–82. 10.1007/s11523-018-0585-y [DOI] [PubMed] [Google Scholar]
- 6.Shirley M. Avelumab: a review in metastatic Merkel cell carcinoma. Target Oncol 2018;13:409–16. 10.1007/s11523-018-0571-4 [DOI] [PubMed] [Google Scholar]
- 7.Kaufman HL, Russell JS, Hamid O, et al. . Updated efficacy of avelumab in patients with previously treated metastatic Merkel cell carcinoma after ≥1 year of follow-up: JAVELIN Merkel 200, a phase 2 clinical trial. J Immunother Cancer 2018;6:7. 10.1186/s40425-017-0310-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.D'Angelo SP, Russell J, Lebbé C, et al. . Efficacy and safety of first-line avelumab treatment in patients with stage IV metastatic Merkel cell carcinoma: a preplanned interim analysis of a clinical trial. JAMA Oncol 2018;4:e180077. 10.1001/jamaoncol.2018.0077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nghiem P, Bhatia S, Lipson EJ, et al. . Durable tumor regression and overall survival in patients with advanced Merkel cell carcinoma receiving pembrolizumab as first-line therapy. J Clin Oncol 2019;37:693–702. 10.1200/JCO.18.01896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wahl RL, Jacene H, Kasamon Y, et al. . From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med 2009;50 Suppl 1:122S–50. 10.2967/jnumed.108.057307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eisenhauer EA, Therasse P, Bogaerts J, et al. . New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 2009;45:228–47. 10.1016/j.ejca.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 12.Tsao MS, Kerr KM, Kockx M, et al. . PD-L1 immunohistochemistry comparability study in real-life clinical samples: results of Blueprint Phase 2 Project. J Thorac Oncol 2018;13:1302–11. 10.1016/j.jtho.2018.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Danaher P, Warren S, Dennis L, et al. . Gene expression markers of tumor infiltrating leukocytes. J Immunother Cancer 2017;5:18. 10.1186/s40425-017-0215-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hua C, Boussemart L, Mateus C, et al. . Association of vitiligo with tumor response in patients with metastatic melanoma treated with pembrolizumab. JAMA Dermatol 2016;152:45–51. 10.1001/jamadermatol.2015.2707 [DOI] [PubMed] [Google Scholar]
- 15.Sanlorenzo M, Vujic I, Daud A, et al. . Pembrolizumab cutaneous adverse events and their association with disease progression. JAMA Dermatol 2015;151:1206–12. 10.1001/jamadermatol.2015.1916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freeman-Keller M, Kim Y, Cronin H, et al. . Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res 2016;22:886–94. 10.1158/1078-0432.CCR-15-1136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knepper TC, Montesion M, Russell JS, et al. . The genomic landscape of Merkel cell carcinoma and clinicogenomic biomarkers of response to immune checkpoint inhibitor therapy. Clin Cancer Res 2019;25:5961–71. 10.1158/1078-0432.CCR-18-4159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goh G, Walradt T, Markarov V, et al. . Mutational landscape of MCPyV-positive and MCPyV-negative Merkel cell carcinomas with implications for immunotherapy. Oncotarget 2016;7:3403–15. 10.18632/oncotarget.6494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yarchoan M, Hopkins A, Jaffee EM. Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med 2017;377:2500–1. 10.1056/NEJMc1713444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Byrne K, Siva S, Chait L, et al. . 15-Year experience of 18F-FDG PET imaging in response assessment and restaging after definitive treatment of Merkel cell carcinoma. J Nucl Med 2015;56:1328–33. 10.2967/jnumed.115.158261 [DOI] [PubMed] [Google Scholar]
- 21.Ben-Haim S, Garkaby J, Primashvili N, et al. . Metabolic assessment of Merkel cell carcinoma: the role of 18F-FDG PET/CT. Nucl Med Commun 2016;37:865–73. 10.1097/MNM.0000000000000523 [DOI] [PubMed] [Google Scholar]
- 22.Robert C, Ribas A, Hamid O, et al. . Durable complete response after discontinuation of pembrolizumab in patients with metastatic melanoma. J Clin Oncol 2018;36:1668–74. 10.1200/JCO.2017.75.6270 [DOI] [PubMed] [Google Scholar]
- 23.Joseph RW, Elassaiss-Schaap J, Kefford R, et al. . Baseline tumor size is an independent prognostic factor for overall survival in patients with melanoma treated with pembrolizumab. Clin Cancer Res 2018;24:6098–67. 10.1158/1078-0432.CCR-18-3340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McDonald K-A, Kawaguchi T, Qi Q, et al. . Tumor heterogeneity correlates with less immune response and worse survival in breast cancer patients. Ann Surg Oncol 2019;26:2191–9. 10.1245/s10434-019-07338-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landskron G, De la Fuente M, Thuwajit P, et al. . Chronic inflammation and cytokines in the tumor microenvironment. J Immunol Res 2014;2014:1–19. 10.1155/2014/149185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lequeux A, Noman MZ, Xiao M, et al. . Impact of hypoxic tumor microenvironment and tumor cell plasticity on the expression of immune checkpoints. Cancer Lett 2019;458:13–20. 10.1016/j.canlet.2019.05.021 [DOI] [PubMed] [Google Scholar]
- 27.Najjar YG, Menk AV, Sander C, et al. . Tumor cell oxidative metabolism as a barrier to PD-1 blockade immunotherapy in melanoma. JCI Insight 2019;4. 10.1172/jci.insight.124989. [Epub ahead of print: 07 Mar 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tilling T, Moll I. Which are the cells of origin in Merkel cell carcinoma? J Skin Cancer 2012;2012:1–6. 10.1155/2012/680410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scharping NE, Menk AV, Whetstone RD, et al. . Efficacy of PD-1 blockade is potentiated by metformin-induced reduction of tumor hypoxia. Cancer Immunol Res 2017;5:9–16. 10.1158/2326-6066.CIR-16-0103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.J. Wakefield M. Xenomapper: mapping reads in a mixed species context. JOSS 2016;1:18 10.21105/joss.00018 [DOI] [Google Scholar]
- 31.Blokzijl F, Janssen R, van Boxtel R, et al. . MutationalPatterns: comprehensive genome-wide analysis of mutational processes. Genome Med 2018;10:33. 10.1186/s13073-018-0539-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alexandrov L, Kim J, Haradhvala NJ, et al. . The repertoire of mutational signatures in human cancer. BioRxiv 2018:322859. [Google Scholar]
- 33.Tate JG, Bamford S, Jubb HC, et al. . COSMIC: the catalogue of somatic mutations in cancer. Nucleic Acids Res 2019;47:D941–7. 10.1093/nar/gky1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2020-000700supp001.pdf (270.4KB, pdf)