Abstract
Objectives
Comorbidities are common in people with axial spondyloarthritis (axSpA). In this systematic review and meta-analysis, we aimed to: (i) describe the prevalence of commonly reported comorbidities, (ii) compare comorbidities between axSpA and control populations, and (iii) examine the impact of comorbidity burden on axSpA outcomes.
Methods
We systematically searched Medline, PubMed, Scopus and Web of Science using a predefined protocol in accordance with Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. We excluded studies of only one comorbid condition or a few closely related diseases within one organ system. Where possible, meta-analysis was performed using random-effects models.
Results
A total of 40 studies were included for analysis. 36 studies reported prevalence of comorbidities, amounting to a combined sample size of 119 427 patients. The number of comorbidities studied ranged from 3 to 43. The most prevalent individual comorbidities were hypertension (pooled prevalence 23%), hyperlipidaemia (17%) and obesity (14%). Eleven studies consistently showed higher prevalence of comorbidities in axSpA than controls, particularly large differences were seen for depression [pooled odds ratio (OR) 1.80] and heart failure (OR 1.84). Comorbidities (total number of and individual conditions) were also associated with axSpA disease activity, functional impairment, quality of life, work productivity and mortality.
Conclusions
Comorbidities are common in axSpA, particularly cardiovascular diseases and risk factors. Most comorbidities were more prevalent in axSpA patients than in control populations. Overall comorbidity burden, and many individual conditions, were associated with axSpA outcomes including worse disease severity, work productivity and mortality.
Keywords: Ankylosing spondylitis, axial spondyloarthritis, comorbidity, multimorbidity, systematic review, meta-analysis
Rheumatology key messages
Comorbidities are common in axSpA patients, particularly hypertension (prevalence 22%), hyperlipidaemia (17%) and obesity (14%).
Comorbidities were more prevalent in axSpA than controls, with ≥80% higher odds for heart failure and depression.
Comorbidities were associated with poorer patient-reported outcomes, work productivity, treatment response and mortality.
Introduction
Axial spondyloarthritis (axSpA) is a chronic inflammatory disease predominantly affecting the spine. It can be divided into ‘radiographic’ (ankylosing spondylitis, AS) and ‘non-radiographic’ (nr-axSpA), depending on whether definitive structural changes are evident on plain radiographs of sacroiliac joints. Patients with axSpA are at higher risk of other medical conditions than the general population, partly due to shared risk factors, consequences of inflammation or its treatment (e.g. long-term NSAIDs). The majority of axSpA patients have at least one comorbid medical condition in addition to any extra-articular manifestations [1]. The collective ‘burden’ of these comorbidities has been reported to associate with poorer function, quality of life and work-related outcomes [2]. They are also important considerations in routine clinical practice where renal impairment, infections, cardiovascular and gastrointestinal diseases will all influence treatment decisions [3]. Some are also key drivers of mortality [4]. A holistic, patient-centred care provision model is therefore essential in rheumatology, yet comorbidity research to inform such practices have been heterogeneous in design and quality.
The majority of prior research have focused on one or a few closely related comorbidities in one organ system; examples include cardiovascular diseases and bone health. While this approach is valid for assessing the impact of one comorbid disease on axSpA, it does not reflect the real-world setting where patients frequently have multiple inter-related comorbidities. When studies include several comorbidities, their methods are often diverse. Some count the number of conditions in varying lists (often arbitrarily) defined by the researchers, which may overlook important comorbidities, while others use indices that are weighted for outcomes unrelated to their topic of study (e.g. using the Charlson Comorbidity Index to study functional outcomes).
The aims of this systematic review and meta-analysis were to: (i) describe the prevalence of commonly reported comorbidities, (ii) compare the incidence and/or prevalence of comorbidities between axSpA and control populations, and (iii) examine the impact of comorbidity burden on axSpA outcomes.
Methods
A systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [5]. The protocol for this review was pre-registered in advance (PROSPERO: CRD42019151105). We searched Medline, PubMed, Scopus and Web of Science for relevant literature in September 2019, using the following search term: (ankylosing spondylitis OR axial spondyloarth*) AND (multimorbid* OR comorbid* OR polymorbid* OR multi-morbid* OR co-morbid* OR poly-morbid*).
Studies of axSpA (whether defined by classification criteria or otherwise) were included if they reported the prevalence or incidence of comorbidities or their impact on disease outcomes. We also included studies that did not primarily examine comorbidities but reported their prevalence in detail. Studies were excluded if they focused on only one comorbid condition (e.g. stroke only) or a few closely related diseases in one organ system (e.g. cardiovascular diseases only). This is to distinguish studies of comorbidity from, say, cardiovascular risk. We also excluded studies that used non-representative sampling (highly selective recruitment or criteria randomized controlled trials) or had a samples size of <30 (to avoid unreliable prevalence estimates). Published conference abstracts were considered, as some prevalence studies may not be published as full articles but nevertheless have sufficiently detailed methodology and results. Bibliographies of all eligible studies were also manually searched to identify additional titles. Reviews, comments and editorials were excluded.
Two independent reviewers screened titles and abstracts, assessed full-texts for eligibility and extracted data from qualifying studies. Any discrepancy at each stage was resolved through discussion moderated by a third reviewer. Information from included studies was extracted into predefined tabulated summaries. We excluded extra-articular manifestations (EAMs) from our list of extracted comorbidities, as they share pathogenesis with and aid diagnosis of axSpA [6, 7]. Studies were assessed for risk of bias using adapted versions of the Newcastle Ottowa Scale (details in supplementary materials, available at Rheumatology online).
For aims 1 and 2, we performed meta-analyses for comorbidities reported by at least three studies. Pooled prevalence estimates were reported as percentages (95% CI), using random-effects models (DerSimonian-Laird). Double arcsine transformation was used, as traditional weighting methods are problematic when proportions are close to the bound limits. Heterogeneity of meta-analysis estimates were presented using the I2 statistic. Funnel plots were used to assess risk of publication bias. Analyses were performed using MetaXL version 5.3 (Sunrise Beach, Australia).
Results
A total of 1522 publications were found from the literature search. After excluding duplicates, irrelevant and ineligible studies, 44 studies remained. Three used data from the ASAS-COMOSpA study [2, 8, 9], from which the paper by Nikiphorou et al. was selected because it restricted to participants fulfilling ASAS criteria. Two used the OASIS registry [10, 11]; we kept the paper by Stolwijk et al. as it reported a greater range of comorbidities. The larger of two studies using United States’ claims data by Walsh et al. was included [5, 12]. Flowchart of the selection process is shown in Supplementary Fig. S1, available at Rheumatology online.
The 40 included studies are summarized in Supplementary Table S1, available at Rheumatology online. Sample size ranged from 74 to 21 872. A total of 22 studies used European cohorts, seven were from Asia, six North America, one Argentina, one Australia and four were multinational. Mean age of study samples ranged from 29 (China) to 59 (UK). Mean BASDAI ranged from 3.4 (China) to 7.6 (Australian cohort initiating TNFi).
AxSpA was defined using classification criteria in 20 studies (seven using the modified New York criteria only, 13 using the ASAS ±mNY criteria), diagnostic codes in 14, physician diagnosis in three and self-report in one. The number of comorbidities studied ranged from three to 43 (excluding EAMs). Most studies used unvalidated lists, while 13 used a validated index either directly or indirectly (to inform which comorbidities to include, e.g. Kang et al. [13]): three used the Charlson Comorbidity Index (CCI), two the Elixhauser Comorbidity Index (ECI), three the self-reported comorbidity questionnaire (SCQ), two the Rheumatic Disease Comorbidity Index (RDCI), two the multimorbidity index and one the Functional Comorbidity Index (see reference [14] for descriptions of each). EAMs were included as comorbidity in a minority (five out of 40 studies), while two considered valvular heart disease and restrictive lung disease as EAMs. Two studies also included smoking as comorbidity. Most studies did not justify their sample size because they were not dedicated studies of comorbidities, thereby losing one score for bias. Taking this into account, scores were mostly 4–5 out of 6 stars (Supplementary Table S2 and Fig. S2, available at Rheumatology online) indicating minimal bias.
Prevalence of comorbidities
A total of 36 studies reported prevalence of individual comorbidities with a combined sample size of 119 427 patients [1, 2, 5, 11, 13, 15–45]. All studies reported one or more diseases of the cardiovascular system; 21 studies included a gastrointestinal or hepatic disorder; 21 included cancers; 18 pulmonary disorders; 16 mental health disorders (anxiety or depression). The most frequently studied individual comorbidities were hypertension (33 studies), diabetes (30) and stroke (18); all other were reported by 16 or fewer studies. Diverticulitis, irritable bowel syndrome, venous thromboembolism and bronchiectasis are examples of infrequently (reported by ≤2 studies) included conditions (full list in Supplementary Table S3, available at Rheumatology online).
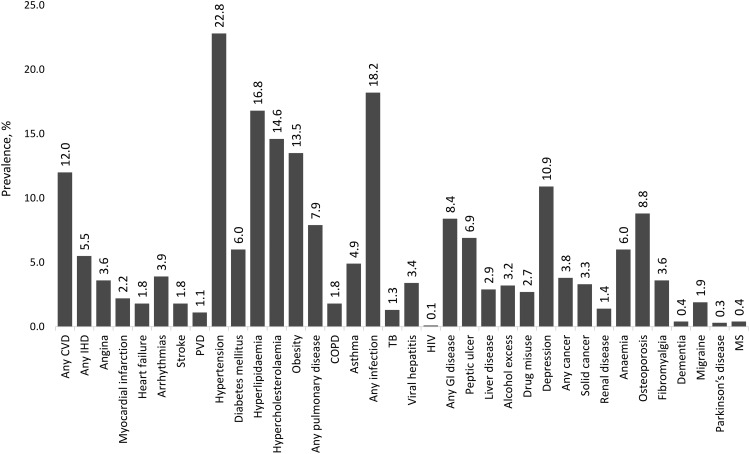
Pooled prevalence estimates of individual comorbidities are summarized in Fig. 1 with further details in Table 1. The top five most prevalent comorbidities were hypertension (22.3%), any infection (18.3%), hyperlipidaemia (17.1%), obesity (13.5%) and any cardiovascular disease (CVD, 12.3%). There was significant heterogeneity for the majority of meta-analyses. Stratifying by axSpA definition (i.e. diagnostic code, modified New York, ASAS±mNY criteria) did not improve heterogeneity or give significantly different prevalence estimates (data not shown). Forrest and funnel plots of the 36 meta-analyses are provided in supplementary materials, available at Rheumatology online.
Fig. 1.
Pooled prevalence of individual comorb conditions reported by ≥3 studies
Table 1.
Meta-analysis estimates for prevalence of individual comorbidities
| n | Pooled prevalence | 95% CI | I2, % | Range | |
|---|---|---|---|---|---|
| Any cardiovascular disease | 12 | 12.0 | 5.8, 19.9 | 100 | 2.7, 34.4 |
| Any ischaemic heart disease | 15 | 5.5 | 3.7, 7.5 | 99 | 0.9, 16.2 |
| Angina | 6 | 3.6 | 1.2, 6.9 | 96 | 1.2, 7.0 |
| Myocardial infarction | 11 | 2.2 | 1.4, 3.1 | 91 | 0, 7.2 |
| Heart failure | 10 | 1.8 | 1.2, 2.4 | 95 | 0.5, 5.8 |
| Arrhythmias | 7 | 3.9 | 1.2, 7.8 | 98 | 1.0, 14.0 |
| Stroke | 18 | 1.8 | 1.3, 2.3 | 96 | 0, 5.5 |
| Peripheral vascular disease | 9 | 1.1 | 0.6, 1.9 | 97 | 0.2, 2.8 |
| Hypertension | 33 | 22.8 | 16.4, 29.8 | 100 | 4.5, 73.0 |
| Diabetes mellitus | 30 | 6.0 | 4.6, 7.5 | 99 | 0.3, 18.0 |
| Hyperlipidaemia | 11 | 16.8 | 10.1, 24.7 | 100 | 4.2, 33.1 |
| Hypercholesterolaemia | 5 | 14.6 | 4.0, 29.6 | 99 | 4.3, 27.0 |
| Obesity | 7 | 13.5 | 2.2, 30.4 | 100 | 0.2, 27.3 |
| Any pulmonary disease | 8 | 7.9 | 2.6, 15.4 | 99 | 1.9, 23.4 |
| COPD | 8 | 1.8 | 0.9, 2.8 | 94 | 0.6, 5.0 |
| Asthma | 8 | 4.9 | 2.9, 7.3 | 98 | 0.5, 11.3 |
| Any infection | 3 | 18.2 | 3.9, 38.4 | 100 | 4.6, 32.9 |
| TB | 7 | 1.3 | 0.5, 2.4 | 93 | 0, 3.8 |
| Viral hepatitis | 6 | 3.4 | 0.9, 7.3 | 97 | 0.6, 18.6 |
| HIV | 3 | 0.1 | 0.04, 0.3 | 13 | 0, 0.3 |
| Any GI disease | 5 | 8.4 | 2.5, 16.9 | 99 | 1.0, 31.3 |
| Peptic ulcer | 12 | 6.9 | 3.3, 11.6 | 99 | 1.1, 20.9 |
| Liver disease | 9 | 2.9 | 0.7, 6.4 | 99 | 0, 12.0 |
| Alcohol excess | 4 | 3.2 | 0.0, 8.3 | 99 | 0.3, 9.4 |
| Drug misuse | 3 | 2.7 | 0.4, 6.6 | 96 | 1.1, 4.8 |
| Depression | 16 | 10.9 | 6.2, 16.7 | 100 | 2.0, 31.0 |
| Any cancer | 16 | 3.8 | 0.7, 9.0 | 100 | 0.3, 29.5 |
| Solid cancer | 5 | 3.3 | 0.3, 8.5 | 99 | 0.6, 12.0 |
| Renal disease | 15 | 1.4 | 1.0, 1.9 | 93 | 0.1, 2.7 |
| Anaemia | 6 | 6.0 | 2.0, 11.7 | 97 | 1.0, 14.1 |
| Osteoporosis | 12 | 8.8 | 5.1, 13.2 | 99 | 3.4, 31.0 |
| Fibromyalgia | 5 | 3.6 | 0.2, 9.7 | 100 | 0.4, 13.0 |
| Dementia | 4 | 0.4 | 0.1, 0.8 | 74 | 0, 0.8 |
| Migraine | 3 | 1.9 | 0.9, 3.3 | 83 | 1.3, 3.0 |
| Parkinson’s disease | 3 | 0.3 | 0.2, 0.4 | 0 | 0.1, 0.3 |
| MS | 4 | 0.4 | 0.3, 0.6 | 0 | 0.1, 0.5 |
Stroke includes cerebrovascular accidents and transient ischaemic attacks.
COPD: chronic obstructive pulmonary disease; GI: gastrointestinal; MS: multiple sclerosis.
Comorbidities in axSpA compared with controls
Eleven studies compared comorbidities between axSpA and control groups [5, 13, 15–18, 20, 26, 36, 37, 41]. Six studies selected controls without AS or inflammatory rheumatic diseases, while five others did not specify or selected from the whole population. All studies compared prevalence; nine used pairwise comparisons or odds ratios (OR) and two used standardized mortality ratios (SMR). All except one study matched for at least age and sex. Cardiovascular comorbidities were the most commonly described. Virtually all individual comorbidities were more prevalent in axSpA populations than matched controls (Supplementary Table S4, available at Rheumatology online).
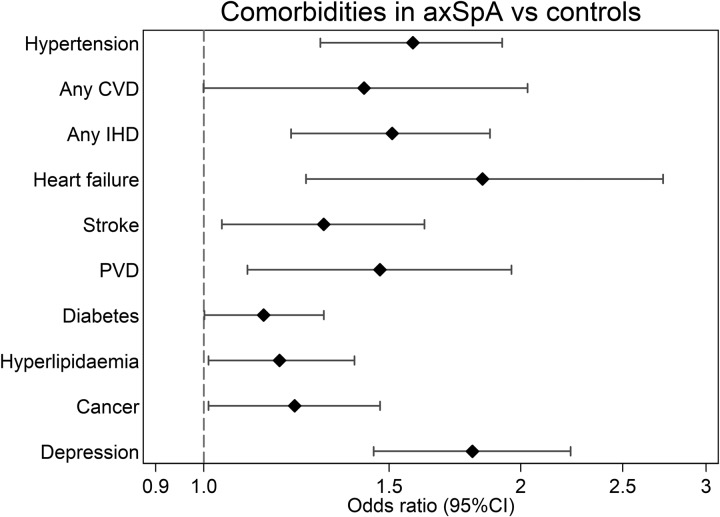
For the nine studies reporting OR (or from which OR would be calculated), comorbidities reported by ≥3 studies were pooled using meta-analysis (summarized in Fig. 2 with further details in Table 2). The three most frequently compared comorbidities were hypertension (axSpA groups had 58% higher odds than controls), diabetes (14% higher odds) and ischaemic heart disease (IHD, 51% higher odds). The largest effect sizes were: 84% higher odds of heart failure in axSpA compared with controls; and 80% higher odds for depression. Heterogeneity was high for all meta-analysis estimates. Forrest and funnel plots for 10 meta-analyses are shown in supplementary materials, available at Rheumatology online.
Fig. 2.
Summary of meta-analysis estimates for odds ratios comparing comorbidities between axSpA and control groups
Table 2.
Meta-analysis estimates for odds ratios (OR) of comorbidities compared between axSpA and control groups
| n | Pooled OR | 95% CI | I2, % | OR range | |
|---|---|---|---|---|---|
| Hypertension | 9 | 1.58 | 1.29, 1.92 | 98 | 1.09, 3.01 |
| Any cardiovascular disease | 3 | 1.42 | 0.999, 2.03 | 99 | 1.14, 1.97 |
| Any ischaemic heart disease | 7 | 1.51 | 1.21, 1.87 | 87 | 1.10, 2.74 |
| Heart failure | 4 | 1.84 | 1.25, 2.73 | 89 | 1.42, 2.74 |
| Stroke | 6 | 1.30 | 1.04, 1.62 | 81 | 0.95, 1.80 |
| Peripheral vascular disease | 5 | 1.47 | 1.10, 1.96 | 83 | 1.06, 2.21 |
| Diabetes | 8a | 1.14 | 1.001, 1.30 | 83 | 0.90, 1.31 |
| Hyperlipidaemia | 5 | 1.18 | 1.01, 1.39 | 94 | 1.02, 1.46 |
| Cancer | 5b | 1.22 | 1.01, 1.47 | 93 | 0.80, 1.59 |
| Depression | 4 | 1.80 | 1.45, 2.23 | 92 | 1.45, 2.10 |
Diabetes without complications selected.
Solid cancer without metastasis selected.
Stroke: includes cerebrovascular accidents and transient ischaemic attacks.
Two studies additionally reported incidence of comorbidities after axSpA diagnosis (Table 3). Cook et al. found higher risk of developing hypertension, myocardial infarction, stroke, COPD and depression in axSpA patients compared with controls [18]. When Essers et al. adjusted for NSAID-use, however, the difference for myocardial infarction and IHD were no longer significantly different between axSpA and controls [20].
Table 3.
Studies comparing comorbidity incidence between axSpA patients and controls
| Measure of incidence | Control group | Comorbidity | Effect size | 95% CI | |
|---|---|---|---|---|---|
| Cook 2018 [18] | HR (incidence after AS diagnosis), adjusted for age and sex | UK biobank participants without AS, RA, PsA or SLE |
|
|
|
| Essers 2016 [20] | HR (incidence after AS diagnosis), adjusted for age, sex, NSAID use, smoking, BMI and other medications | CPRD patients without RA, PsA, SLE or vasculitis |
|
|
|
| Incidence rate ratio, adjusted for age and sex |
|
|
|
COPD: chronic obstructive pulmonary disease; CPRD: Clinical Practice Research Datalink; CVA: cerebrovascular accident; MI: myocardial infarction.
Three studies compared comorbidities between male and females. Bremander et al. showed that the difference in osteoporosis prevalence between axSpA and controls were much higher in males than females (SMR 6.98 vs 3.24) but no different for other comorbidities that they studied [16]. Kang et al. reported significantly higher odds of migraine (conditional OR 2.3 vs 1.5), COPD (OR 6.8 vs 2.4) and asthma (OR 1.6 vs 0.8), in female axSpA vs female controls than the equivalent comparison in males [13]. They also found non-significantly higher odds for IHD (OR 4.5 vs 2.3), alcohol (OR 5.0 vs 1.3) and drug (OR 2.2 vs 1.1) abuse/dependence in females. Essers et al. reported higher incidence rate ratios for IHD in females than males (1.72 vs 1.07) [20].
Association between comorbidity burden and disease outcomes
Seventeen studies reported the association between comorbidity burden and axSpA outcomes (Table 4). In the majority of studies, axSpA patients with comorbidity had higher disease activity and function impairment, more severe pain and poorer quality of life than those without. ESR and CRP were generally not significantly different.
Table 4.
Studies examining the impact of comorbidity on axSpA outcomes
| How comorbidity was examined | Outcome | Results (shown as pairwise comparison, or ‘effect size; 95% confidence interval’) | |
|---|---|---|---|
| Ariza-Ariza 2009 [46] |
|
Quality of life (EQ5D) |
|
| Salaffi 2009 [47] | SCQ | BASDAI | SCQ was associated with increased BASDAI, no effect size or P-value reported. |
| Fernandez-Carballido 2019 [21] | Modified CCI (cancer definitions pooled) | BASFI | CCI was not associated with BASFI (ß =0.03; −0.13, 0.20) in multivariable linear model. |
| Redeker 2019 [abstract] [44] | ECI excluding rheumatic diseases |
|
|
| Zhao 2019 (US)a [33] | Modified MMI (39 comorbidities) |
|
|
| Boonen 2001 [48] |
|
Work disability (inability to perform paid work) |
|
| Stolwijk 2014 [11] |
|
|
|
| Garip 2016 [23] | Presence or absence (9 comorbidities) | Multiple outcomes |
|
| Ljung 2018 [29] | Each of 4 comorbidity categories | Multiple outcomes | In multivariable logistic regression: arrhythmia/valvular disease, atherosclerosis, fractures and obstructive sleep apnoea were not associated with peripheral or extra-articular manifestations, BASMI or CRP. |
| Nikiphorou 2018 [2] | RDCI | Multiple outcomes |
|
| Fitzgerald 2019 [22] | Presence or absence (12 comorbidities) | Multiple outcomes |
|
| Number of comorbidities |
|
||
| Zhao 2019 (UK) [1] | Presence or absence (38 comorbidities based on MMI) | Multiple outcomes |
|
| Lindström 2018 [28] | Each of 6 comorbidities | TNFi discontinuation |
|
| Iannone 2018 [49] | modified RCDI (adding obesity and renal disease) | Biologic drug use | In SpA patients, mRDCI correlated significantly with the number of biological drug switches (Spearman’s rank coefficient 0.26, P-value unreported) mRCDI was a significant independent predictor of drug discontinuation (HR 1.53; 1.02, 2.29) and ASDAS remission (HR 0.43; 0.20, 0.92) in multi-adjusted Cox models. |
| Haroon 2015 [26] | Each of 7 comorbidities including IBD | ‘Vascular’ (cardio- and cerebrovascular) mortality | Dementia (HR, 2.62; 1.32, 5.23) and PVD (HR, 6.79; 2.45, 18.84) were significantly associated with vascular mortality, but not diabetes, CKD, IBD or cancer. |
| Exarchou 2016 [36] | Each of 5 ‘general’ comorbidities | Mortality |
|
| Lee 2018 [50] | CCI |
|
In multivariable logistic models, CCI was associated with increased all-cause mortality (OR 1.07; 1.01, 1.13), but not physical disability (OR 1.01; 0.95, 1.08). |
Unpublished data. Absenteeism: time off due to health reasons; CCI: Charlson Comorbidity Index; ECI: Elixhauser Comorbidity Index; MMI: multimorbidity index; Presenteeism: reduced productivity at work; RDCI: Rheumatic Disease Comorbidity Index; SCQ: self-reported comorbidity questionnaire; Work status: working or not.
Three studies reported work-related outcomes. Nikiphorou et al. found that RDCI was associated with reduced employment, increased time off due to health reasons (absenteeism) and reduced productivity at work (presenteeism) [2]. Stolwijk et al. found that the SCQ score was associated with stopping work due to disability, but only in those with BASDAI < 4 [11]. Boonen et al. reported three times higher odds of inability to perform paid work in AS patients with comorbidities than without [48].
Two studies examined treatment outcomes. Iannone et al. reported correlation between a modified version of RDCI and number of biological drug switches [49]. The authors also found mRDCI to be a predictor of TNFi discontinuation and poor ASDAS remission response. Lindström et al. found CVD, affective disorders, chronic lung disease and malignancy to be associated with increased TNFi discontinuation in unadjusted Cox models, but not diabetes or chronic kidney disease (CKD) [28].
Three studies reported mortality outcomes. Lee et al. studied comorbidity burden using CCI, where each unit increase was associated with 7% higher odds of all-cause mortality [50]. Haroon et al. found that dementia and peripheral vascular disease (PVD) were associated with increased vascular mortality, but not diabetes, CKD, IBD or cancer [26]. All comorbidities in the study by Exarchou et al. were each significant associated with all-cause mortality; AS patients with chronic pulmonary disease were at particularly higher risk of death (HR 3.0) [36].
Discussion
Comorbidities are common and associated with disease outcomes in axSpA. Meta-analysis pooling results from >100 000 patients showed the most prevalent individual comorbidities to be hypertension, hyperlipidaemia and obesity. There was significant variation in the type and number of conditions included in each study, which will impact the precision of estimates. Almost all comorbidities examined were more prevalent in axSpA patients than age and sex-matched controls, with ≥80% higher odds for heart failure and depression. Comorbidities (total number of and individual conditions) were associated with patient-reported outcomes, work productivity, treatment response and mortality.
Despite the high prevalence of many comorbidities, randomized clinical trials—the gold-standard in evidence-based medicine—routinely exclude patients with these conditions. Clinicians should be mindful of extrapolating results from explanatory trials (i.e. under ideal conditions), while researchers should invest in pragmatic trials that measure effectiveness in routine clinical practice [51]. Comorbidities are essential considerations in the real-world management of axSpA patients. They influence treatment decisions (e.g. for NSAIDs and biologics [3]) and preliminary results also suggest that they impact treatment outcomes [28, 49]. Studies in this review consistently showed higher prevalence of comorbidities in axSpA patients than controls. Yet, in clinical practice, management of comorbidities for patients with chronic inflammatory rheumatic diseases are often worse than in the general population [52]. The 2016 EULAR points to consider for comorbidities recommend rheumatology teams to detect and collect information on comorbidities, liaise with appropriate healthcare providers to treat comorbidities, and repeat comorbidity reviews [52]. They focused on six conditions (CVD, malignancies, infections, peptic ulcer, osteoporosis and depression) that map almost exactly with high-prevalence comorbidities in our meta-analysis. It may, however, be that under-recognised comorbidities have under-estimated prevalence. Others have suggested including additional comorbidities [53], but this may be limited by feasibility in daily practice – the six comorbidities alone require a 93-item reporting form.
Almost all included comorbidities were more prevalent in axSpA patients than controls. axSpA patients had markedly higher odds for depression and cardiovascular diseases than controls. Symptoms of axSpA typically begin in early adulthood, which is a critical time for careers, relationships and general social and personal identity. Disruptive symptoms—sometimes undiagnosed for many years—may impact life-long mental health trajectory and contribute to depression rates. Unlike RA, axSpA is not typically associated with high levels of systemic inflammation – a key driver of CVD risk. Higher CVD prevalence may be related to treatment in addition to the disease process itself; incidence of myocardial infarction and IHD were no different between axSpA and controls after adjusting for NSAID-use [20]. Heart failure is downstream of many CVDs; thus, higher odds in axSpA may reflect the overall burden and severity of CVDs. It may also be due to more systematic identification when considering TNF inhibitors. These results are consistent with prior studies showing reduced systolic and diastolic function in axSpA patients compared with controls [54, 55]. Heart failure can have significant impact on function and quality of life [56], thus optimal symptom management is important for patients already burdened by their rheumatic disease.
The presence of comorbidities was consistently associated with worse patient-reported axSpA outcomes, such as the BASDAI and BASFI. Future studies should complement such analyses by interrogating the contribution of individual comorbidities, comorbidity clusters [1], as well as their combined impact. There is also a need to examine how robust various outcomes (e.g. BASDAI vs ASDAS) are to comorbidities such as depression, as they may influence assessment of treatment response. Whether outcomes such as treatment response and work productivity can be improved by optimizing management of certain comorbidities is an important unanswered question.
Methodological approach for comorbidity research could benefit from similar standardization as suggested for clinical practice [57]. The number of included comorbidities in this review ranged from 3 to 43. Most studies used author-defined lists that were not validated and selection of diseases was seldom justified. While all studies consistently included CVDs, some important conditions were underrepresented, such as fibromyalgia, alcohol or drug abuse [58] and neurological disorders. Validated comorbidity indices can include rare comorbidities in axSpA (e.g. AIDS and dementia) but not common and important conditions (e.g. depression [59]). None have been validated for use in axSpA patients except the modified SCQ. Stolwijk et al. showed that CCI poorly correlated with most axSpA outcomes (e.g. Spearman’s rho=−0.01 for BASDAI) while both CCI and RDCI were poorly associated with BASFI and quality of life (Short Form 36) in multivariable analyses [11]. Validation studies in axSpA are needed for other indices and comorbidity collection based on the ‘EULAR 6’. Studies should avoid using weighted indices that have not been validated for their main outcome of interest (e.g. CCI or ECI for functional impairment [21, 44]).
Meta-analysis results should be interpreted with limitations in mind. There was significant heterogeneity in the measurement of comorbidities and relative lack of data on severity. Study samples also differed in age, disease severity and other characteristics. The duration of study in which comorbid diseases were assessed was also variable. These factors will impact pooled prevalence estimates but also highlights the need for greater standardization for future research. Some case-control studies did not explicitly exclude patients with AS or other chronic inflammatory rheumatic diseases from their control population. Comorbidity prevalence in these control populations may therefore be inflated. This is unlikely to meaningfully change the overall result, as inflammatory rheumatic diseases will be uncommon among controls. Once patients develop symptoms of or are diagnosed with axSpA, it is likely that increased healthcare interaction will result in improved identification of comorbidities; therefore, prevalence may be higher than controls by this explanation alone. Well-established comorbidities such as hypertension may undergo more systematic screening and diagnosis than others (e.g. fibromyalgia or depression); results from cases-control comparisons will be inflated for the former group of comorbidities. We were unable to compare comorbidity burden between radiographic and non-radiographic axSpA. Stratified meta-analyses (by classification criteria) did not reveal statistically significant differences in prevalence estimates, which is consistent with the findings of one prior study [33].
In summary, comorbidities are common in axSpA, particularly cardiovascular diseases and risk factors. These items were consistently included in assessments of comorbidities, but diseases belonging to pulmonary, mental health and neurological systems were less frequently included. The vast majority of comorbidities assessed were more prevalent in axSpA patients than in control populations. Overall comorbidity burden, and many individual conditions, were associated with axSpA outcomes including disease severity, work productivity and mortality. Systematic and repeated assessments should therefore be integrated into routine clinical practice to ensure holistic patient-centred management. Additional studies are needed to validate comorbidities indices for axSpA research.
Funding: No specific funding was received from any funding bodies in the public, commercial or not-for-profit sectors to carry out the work described in this manuscript. This paper was published as part of a supplement funded by Novartis.
Disclosure statement : The authors have declared no conflicts of interest.
Supplementary Material
References
- 1. Zhao SS, Radner H, Siebert S et al. Comorbidity burden in axial spondyloarthritis: a cluster analysis. Rheumatology 2019;58:1746–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nikiphorou E, Ramiro S, van der Heijde D et al. Association of comorbidities in spondyloarthritis with poor function, work disability, and quality of life: results from the assessment of SpondyloArthritis International Society Comorbidities in Spondyloarthritis Study. Arthritis Care Res 2018;70:1257–62. [DOI] [PubMed] [Google Scholar]
- 3. González C, Curbelo Rodríguez R, Torre-Alonso JC et al. Recommendations for the management of comorbidity in patients with axial spondyloarthritis in clinical practice. Reumatol Clínica Engl Ed 2018;14:346–59. [DOI] [PubMed] [Google Scholar]
- 4. Zochling J, Braun J. Mortality in ankylosing spondylitis. Clin Exp Rheumatol 2008;26(5 Suppl 51):S80–84. [PubMed] [Google Scholar]
- 5. Walsh JA, Song X, Kim G, Park Y. Evaluation of the comorbidity burden in patients with ankylosing spondylitis using a large US administrative claims data set. Clin Rheumatol 2018;37:1869–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stolwijk C. Extra articular manifestations and comorbidities in spondyloarthritis: epidemiological and clinical aspects. PhD Thesis, Maastricht University, 2015.
- 7. Mielants H, Van den Bosch F. Extra-articular manifestations. Clin Exp Rheumatol 2009;27(4 Suppl 55):S56–61. [PubMed] [Google Scholar]
- 8. Moltó A, Etcheto A, van der Heijde D et al. Prevalence of comorbidities and evaluation of their screening in spondyloarthritis: results of the international cross-sectional ASAS-COMOSPA study. Ann Rheum Dis 2016;75:1016–23. [DOI] [PubMed] [Google Scholar]
- 9. Bautista-Molano W, Landewé R, Burgos-Vargas R et al. Prevalence of comorbidities and risk factors for comorbidities in patients with spondyloarthritis in Latin America: a comparative study with the general population and data from the ASAS-COMOSPA Study. J Rheumatol 2018;45:206–12. [DOI] [PubMed] [Google Scholar]
- 10. Webers C, Ramiro S, Landewé R et al. Sick leave and its predictors in ankylosing spondylitis: long-term results from the Outcome in Ankylosing Spondylitis International Study. RMD Open 2018;4:e000766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stolwijk C, van Tubergen A, Ramiro S et al. Aspects of validity of the self-administered comorbidity questionnaire in patients with ankylosing spondylitis. Rheumatology 2014;53:1054–64. [DOI] [PubMed] [Google Scholar]
- 12. Walsh JA, Song X, Kim G, Park Y. Evaluation of the comorbidity burden in patients with ankylosing spondylitis treated with tumour necrosis factor inhibitors using a large administrative claims data set. J Pharm Health Serv Res 2018;9:115–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kang J-H, Chen Y-H, Lin H-C. Comorbidity profiles among patients with ankylosing spondylitis: a nationwide population-based study. Ann Rheum Dis 2010;69:1165–8. [DOI] [PubMed] [Google Scholar]
- 14. Aslam F, Khan NA. Tools for the assessment of comorbidity burden in rheumatoid arthritis. Front Med 2018;5:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ahmed N, Prior JA, Chen Y et al. Prevalence of cardiovascular-related comorbidity in ankylosing spondylitis, psoriatic arthritis and psoriasis in primary care: a matched retrospective cohort study. Clin Rheumatol 2016;35:3069–73. [DOI] [PubMed] [Google Scholar]
- 16. Bremander A, Petersson IF, Bergman S, Englund M. Population-based estimates of common comorbidities and cardiovascular disease in ankylosing spondylitis. Arthritis Care Res 2011;63:550–6. [DOI] [PubMed] [Google Scholar]
- 17. Claudepierre P, Fagnani F, Cukierman G et al. Burden of severe spondyloarthritis in France: a nationwide assessment of prevalence, associated comorbidities and cost. Joint Bone Spine 2019;86:69–75. [DOI] [PubMed] [Google Scholar]
- 18. Cook MJ, Bellou E, Bowes J et al. The prevalence of co-morbidities and their impact on physical activity in people with inflammatory rheumatic diseases compared with the general population: results from the UK Biobank. Rheumatology 2018;57:2172–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dougados M, Etcheto A, Molto A et al. Clinical presentation of patients suffering from recent onset chronic inflammatory back pain suggestive of spondyloarthritis: the DESIR cohort. Joint Bone Spine 2015;82:345–51. [DOI] [PubMed] [Google Scholar]
- 20. Essers I, Stolwijk C, Boonen A et al. Ankylosing spondylitis and risk of ischaemic heart disease: a population-based cohort study. Ann Rheum Dis 2016;75:203–9. [DOI] [PubMed] [Google Scholar]
- 21. Fernández‐Carballido C, Martín‐Martínez MA, García‐Gómez C et al. Impact of comorbidity on physical function in patients with ankylosing spondylitis and psoriatic arthritis attending rheumatology clinics. Results from the CAR diovascular in rheu MA tology (CARMA) study. Arthritis Care Res 2019;doi:10.1002/acr.23910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fitzgerald G, Gallagher P, O’Shea F. Multimorbidity is common in axial spondyloarthropathy and is associated with worse disease outcomes: results from the ASRI cohort. J Rheumatol 2019;47:218–26. [DOI] [PubMed] [Google Scholar]
- 23. Garip Y, Eser F, Guler T et al. Comorbidity profiles among patients with ankylosing spondylitis. Marmara Med J 2016;29:23. [Google Scholar]
- 24. Gladman DD, Rahman P, Cook RJ et al. The Spondyloarthritis Research Consortium of Canada Registry for spondyloarthritis. J Rheumatol 2011;38:1343–8. [DOI] [PubMed] [Google Scholar]
- 25. Hammoudeh M, Al Rayes H, Alawadhi A et al. Clinical assessment and management of spondyloarthritides in the Middle East: a multinational investigation. Int J Rheumatol 2015;2015:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Haroon NN, Paterson JM, Li P, Inman RD, Haroon N. Patients with ankylosing spondylitis have increased cardiovascular and cerebrovascular mortality: a population-based study. Ann Intern Med 2015;163:409. [DOI] [PubMed] [Google Scholar]
- 27. Jiang Y, Zhang P, Tu L et al. Prevalence of comorbidities and evaluation of screening in Chinese patients with spondyloarthritis. Clin Rheumatol 2018;37:423–8. [DOI] [PubMed] [Google Scholar]
- 28. Lindström U, Olofsson T, Wedrén S, Qirjazo I, Askling J. Impact of extra-articular spondyloarthritis manifestations and comorbidities on drug retention of a first TNF-inhibitor in ankylosing spondylitis: a population-based nationwide study. RMD Open 2018;4:e000762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ljung L, Sundström B, Smeds J, Ketonen M, Forsblad-d’Elia H. Patterns of comorbidity and disease characteristics among patients with ankylosing spondylitis-a cross-sectional study. Clin Rheumatol 2018. ;37:647–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Oldroyd J, Schachna L, Buchbinder R et al. Ankylosing spondylitis patients commencing biologic therapy have high baseline levels of comorbidity: a report from the Australian Rheumatology Association Database. Int J Rheumatol 2009;2009:268569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Singh DK, Magrey M. Racial differences in clinical features and co-morbidities in ankylosing spondylitis in the United States. J Rheumatol 2019;doi:10.3899/jrheum.181019. [DOI] [PubMed] [Google Scholar]
- 32. Bodur H, Ataman Ş, Buğdaycı DS, et al. Description of the registry of patients with ankylosing spondylitis in Turkey: TRASD-IP. Rheumatol Int 2012;32:169–76. [DOI] [PubMed] [Google Scholar]
- 33. Zhao SS, Ermann J, Xu C et al. Comparison of comorbidities and treatment between ankylosing spondylitis and non-radiographic axial spondyloarthritis in the United States. Rheumatology 2019;58:2025–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhao S, Jones GT, Macfarlane GJ et al. Associations between smoking and extra-axial manifestations and disease severity in axial spondyloarthritis: results from the BSR Biologics Register for Ankylosing Spondylitis (BSRBR-AS). Rheumatology 2019;58:811–9. [DOI] [PubMed] [Google Scholar]
- 35. Ara RM, Packham JC, Haywood KL. The direct healthcare costs associated with ankylosing spondylitis patients attending a UK secondary care rheumatology unit. Rheumatology 2008;47:68–71. [DOI] [PubMed] [Google Scholar]
- 36. Exarchou S, Lie E, Lindström U et al. Mortality in ankylosing spondylitis: results from a nationwide population-based study. Ann Rheum Dis 2016;75:1466–72. [DOI] [PubMed] [Google Scholar]
- 37. Han C, Robinson DW, Hackett MV et al. Cardiovascular disease and risk factors in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. J Rheumatol 2006;33:2167–72. [PubMed] [Google Scholar]
- 38. Hong C, Kwan YH, Leung Y, Lui NL, Fong W. Comparison of ankylosing spondylitis and non‐radiographic axial spondyloarthritis in a multi‐ethnic Asian population of Singapore. Int J Rheum Dis 2019;22:1506–11. [DOI] [PubMed] [Google Scholar]
- 39. Kristensen LE, Jakobsen AK, Askling J, Nilsson F, Jacobsson L. Safety of etoricoxib, celecoxib, and nonselective nonsteroidal antiinflammatory drugs in ankylosing spondylitis and other spondyloarthritis patients: a Swedish National Population-Based Cohort Study: spondyloarthritis and Safety of COX Inhibitors. Arthritis Care Res 2015;67:1137–49. [DOI] [PubMed] [Google Scholar]
- 40. Maas F, Arends S, van der Veer E et al. Obesity is common in axial spondyloarthritis and is associated with poor clinical outcome. J Rheumatol 2016;43:383–7. [DOI] [PubMed] [Google Scholar]
- 41. Krüger K, von Hinüber U, Meier F et al. Ankylosing spondylitis causes high burden to patients and the healthcare system: results from a German claims database analysis. Rheumatol Int 2018;38:2121–31. [DOI] [PubMed] [Google Scholar]
- 42. Png WY, Kwan YH, Lee YX et al. Factors associated with initiation of biologics in patients with axial spondyloarthritis in an Urban Asian City: A PRESPOND study. J Clin Rheumatol 2019;25:59–64. [DOI] [PubMed] [Google Scholar]
- 43. Ward MM, Learch TJ, Gensler LS et al. Regional radiographic damage and functional limitations in patients with ankylosing spondylitis: differences in early and late disease. Arthritis Care Res 2013;65:257–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Redeker I, Callhoff J, Hoffmann F et al. Comorbid conditions are associated with higher disease activity and worse functional status in axial spondyloarthritis: a population-based analysis of insurance claims linked to patient survey data. Ann Rheum Dis 2019;78:1253–4. [Google Scholar]
- 45. Sommerfleck F, Schneeberger E, Citera G. Comorbidities in Argentine patients with axial spondyloarthritis: is nephrolithiasis associated with this disease? Eur J Rheumatol 2018;5:169–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ariza-Ariza R, Hernández-Cruz B, López-Antequera G, Navarro-Sarabia F. Variables related to utility in patients with ankylosing spondylitis. Clin Rheumatol 2009;28:207–11. [DOI] [PubMed] [Google Scholar]
- 47. Salaffi F, Carotti M, Gasparini S, Intorcia M, Grassi W. The health-related quality of life in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis: a comparison with a selected sample of healthy people. Health Qual Life Outcomes 2009;7:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Boonen A. Withdrawal from labour force due to work disability in patients with ankylosing spondylitis. Ann Rheum Dis 2001;60:1033–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Iannone F, Salaffi F, Fornaro M et al. Influence of baseline modified Rheumatic Disease Comorbidity Index (mRDCI) on drug survival and effectiveness of biological treatment in patients affected with Rheumatoid arthritis, Spondyloarthritis and Psoriatic arthritis in real-world settings. Eur J Clin Invest 2018;48:e13013. [DOI] [PubMed] [Google Scholar]
- 50. Lee JS, Oh B-L, Lee HY, Song YW, Lee EY. Comorbidity, disability, and healthcare expenditure of ankylosing spondylitis in Korea: A population-based study. Ramagopalan SV, editor. PLoS ONE 2018;13:e0192524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Roland M, Torgerson DJ. Understanding controlled trials: what are pragmatic trials? BMJ 1998;316:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Baillet A, Gossec L, Carmona L et al. Points to consider for reporting, screening for and preventing selected comorbidities in chronic inflammatory rheumatic diseases in daily practice: a EULAR initiative. Ann Rheum Dis 2016;75:965–73. [DOI] [PubMed] [Google Scholar]
- 53. Castañeda S, Vicente EF, González-Gay MA. Additional proposals to reduce comorbidity in patients with chronic inflammatory rheumatic diseases: comment on ‘Points to consider for reporting, screening for and preventing selected comorbidities in chronic inflammatory rheumatic diseases in daily practice: a EULAR initiative’ by Baillet et al. Ann Rheum Dis 2016;75:e55. [DOI] [PubMed] [Google Scholar]
- 54. Midtbø H, Semb AG, Matre K et al. Left ventricular systolic myocardial function in ankylosing spondylitis. Arthritis Care Res 2019;71:1276–83. [DOI] [PubMed] [Google Scholar]
- 55. Chen Y, Chung H-Y, Zhao C-T et al. Left ventricular myocardial dysfunction and premature atherosclerosis in patients with axial spondyloarthritis. Rheumatology 2015;54:292–301. [DOI] [PubMed] [Google Scholar]
- 56. Juenger J. Health related quality of life in patients with congestive heart failure: comparison with other chronic diseases and relation to functional variables. Heart 2002;87:235–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Radner H, Chatzidionysiou K, Nikiphorou E et al. 2017 EULAR recommendations for a core data set to support observational research and clinical care in rheumatoid arthritis. Ann Rheum Dis 2018;77:476–9. [DOI] [PubMed] [Google Scholar]
- 58. Zhao SS, Solomon DH, Goodson NJ. Comment on: comorbidity burden in axial spondyloarthritis: a cluster analysis: reply. Rheumatology 2020;59:692–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zhao S, Thong D, Miller N et al. The prevalence of depression in axial spondyloarthritis and its association with disease activity: a systematic review and meta-analysis. Arthritis Res Ther 2018;20:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.