Abstract
The antiretroviral drug lopinavir/ritonavir has been recently repurposed for the treatment of COVID-19. Its empirical use has been associated with multiple cardiac adverse reactions pertaining to its ancillary multi-channel blocking properties, vaguely characterized until now. We aimed to characterize qualitatively the cardiotoxicity associated with lopinavir/ritonavir in the setting of COVID-19.
Spontaneous notifications of cardiac adverse drug reactions reported to the national Pharmacovigilance Network were collected for 8 weeks since March 1st 2020. The Nice Regional Center of Pharmacovigilance, whose scope of expertise is drug-induced long QT syndrome, analyzed the cases, including the reassessment of all available ECGs. QTc ≥ 500 ms and delta QTc > 60 ms from baseline were deemed serious.
Twenty-two cases presented with 28 cardiac adverse reactions associated with the empirical use of lopinavir/ritonavir in a hospital setting. Most adverse reactions reflected lopinavir/ritonavir potency to block voltage-gated potassium channels with 5 ventricular arrhythmias and 17 QTc prolongations. An average QTc augmentation of 97 ± 69 ms was reported. Twelve QTc prolongations were deemed serious. Other cases were likely related to lopinavir/ritonavir potency to block sodium channels: 1 case of bundle branch block and 5 recurrent bradycardias. The incidence of cardiac adverse reactions of lopinavir/ritonavir was estimated between 0.3% and 0.4%.
These cardiac adverse drug reactions offer a new insight in its ancillary multi-channel blocking functions. Lopinavir/ritonavir cardiotoxicity may be of concern for its empirical use during the COVID-19 pandemic. Caution should be exerted relative to this risk where lopinavir/ritonavir summary of product characteristics should be implemented accordingly.
Keywords: Lopinavir-ritonavir drug combination, Cardiotoxicity, COVID-19, Drug-related side effects and adverse reactions, Long QT syndrome, Cardiac arrhythmia, Conduction disorder
Highlights
-
•
Lopinavir/ritonavir induces cardiotoxicity in COVID-19
-
•
Featured cardiac adverse events reflect ancillary multiple channel blocking properties
-
•
Caution should prevail with off-label use because of its cardiotoxicity
-
•
It summary of product characteristics must signal that risk
1. Introduction
The association of lopinavir/ritonavir (LPV/r), two anti-HIV protease inhibitor (PI) drugs, aroused interest recently due to COVID-19. LPV/r is effective against HIV by interfering with the polyprotein gag-pol and conducting to the production of immature and non-infectious virions. Experimental efficacy on SARS-CoV and MERS-CoV [1] made it one of the first drugs envisioned for possible antiviral effect in COVID-19 [2]. To date, the effectiveness of LPV/r in COVID-19 treatment has not been proven despite several studies, including two randomized clinical trials [3].
Like other PIs, LPV/r has been associated with metabolic [4] and cardiac disorders [[5], [6], [7], [8], [9], [10], [11]], as well as numerous drug interactions, since its launch over two decades ago. Part of these tender to its ancillary sodium, calcium and potassium channels blocking properties [12] assimilating LPV/r as a mild “multichannel blocker”. PIs as a class block human ether-a-go-go related gene (hERG) potassium channels which recapitulate the cardiac native potassium current I Kr [13]. The inhibition of K+ outward conductance is associated with profound disturbances of cardiac refractory periods and facilitates the emergence of ventricular arrhythmias. This inhibition is reflected by an increase of the QT interval duration corrected for heart rate (QTc) on the electrocardiogram which may lead to polymorphic ventricular arrhythmias such as Torsades de Pointes and to sudden deaths [14]. Experimental LPV/r-dependent sodium and calcium blockade may also lead to chronotropic and dromotropic effects, resulting in an array of rhythm and conduction problems [[15], [16], [17]].
If the risk of Atrio-Ventricular (AV) block is mentioned in the LPV/r Summary of Product Characteristics (SmPC), information concerning QTc prolongation resulted in rather vague mentions on respective European and North-American initial SmPCs.
Although there is no approved drug to prevent or treat SARS-CoV-2 infection yet, the COVID-19 pandemic led to a wide empirical and off-label use of LPV/r by clinicians despite the lack of any strong evidence or convincing scientific rationale. COVID-19 infection can also induce cardiac damages [18], and is often accompanied with electrolyte disturbances [19] which are known risk factors of QTc prolongation and ventricular arrhythmias. Thus, focusing on LPV/r cardiac toxicity is legitimate in COVID-19, as it had been for the empirical use of hydroxychloroquine [20]. In this study, long after its launch, we aimed to characterize LPV/r-associated cardiotoxicity in the setting of COVID-19, through spontaneous notifications of adverse drug reactions (ADRs).
2. Methods
The Pharmacovigilance network consists of a ring of 31 regional pharmacovigilance centers (RCPV) dotted around the French territory. The French Pharmacovigilance database (FPDB) centralizes all spontaneous reports of ADRs, in order to accrue the European database EudraVigilance. Such ADR reporting is mandatory for every health professional and respects the anonymity of both patients and notifiers. As the Nice RCPV has drug-induced Long QT syndrome and cardiac safety of drugs within its scope of expertise, in March 2020, the National drug Agency (ANSM) appointed us to investigate all cases of cardiotoxicity associated with the empirical use of LPV/r against COVID-19 that had spontaneously been reported by any of the 31 RCPVs.
After a first expertise by the RCPV of origin, all cases of cardiotoxicity were consecutively included in this study. Cases were analyzed, validated and a score of imputability was associated with each of them [21,22] for causality assessment. Cases were not included if chronological and semiological data ruled out the role of the designated drug in the notified effect (i.e. the effect was preexisting before the drug administration). To assess the completeness of the case-series we performed an extraction of the FPDB back-dated to March 1st, 2020, involved a research by treatment indication “coronavirus infection” or “COVID-19” and by drugs. Cases related to another indication than COVID-19 were excluded.
Each cardiac ADR transmitted was reviewed by a pharmacovigilant first, to assess missing data required for expertise, and in particular the electrocardiograms (ECGs) before, during and after treatment discontinuation, when necessary. Symptoms, patient characteristics (sex, age, comorbidities), therapeutic regimens and prescription dates, time-to-onset, outcome of ADR, drug concentrations when available, concomitant drugs (especially those known to induce QT prolongation), kalemia, magnesemia, renal function and other reported possible risk factors were gathered. Missing data were requested of the initial health professional reporter through the RCPV of origin. When available, lopinavir residual plasma concentration were averaged and compared with normal values [23].
Two residents and a cardiologist trained in the field measured all available ECGs with classical methods [24] and the help of a digital caliper (Iconico®, CardioCalipers®). QT intervals were calculated on 3 consecutive complexes, in lead D2 if possible (most of the times), and corrected according to the Bazett formula (QTcB). If discrepancies were identified, ECGs and measurements were double-checked by the Department of Cardiology, particularly the QTc value i.e. in the presence of a pacemaker, of a complete bundle branch block, or an atrioventricular block. Furthermore, the available ECGs before, during and after discontinuation of treatment were analyzed. QTc beyond 450 ms for men and 460 ms for women were considered abnormal [25] and QTc ≥ 500 ms or prolongation from baseline (delta QTc) > 60 ms during treatment were deemed as serious. ADRs were grouped by main suspected pharmacological mechanism: inhibition of K currents (ventricular arrhythmias, QTc prolongations) or Na/Ca currents (conduction problems). Additional research of concomitant drugs knows for QTc lengthening was made using the SmPC and the list of drugs prolonging the QT from the website CredibleMeds [26].
Despite uncertainties attached to spontaneous reporting and completeness of prescriptions, we evaluated the incidence of cardiac ADRs associated with LPV/r in COVID-19. This drug is distributed under several packaging (blisters, vials) and formulations (tablets, oral solution). We therefore considered consumption in mg rather than unit of dispensation. Monthly LPV/r national hospital consumption was compared before and during COVID-19. We characterized LPV/r overconsumption in March 2020, with LPV/r daily doses of 800 mg for 10–14 days, corresponding to its off-label use in COVID-19. Thus LPV/r cumulative dose per patient amounted to a minimum of 8000 mg to 11,200 mg maximum.
We queried the FPDB for all cases reported with LPV/r in adults, involving any adverse drug reaction according to MedDRA terms [27] from 2001 (first commercialization in France) to 2019, December 31st. A scrupulous screening was then performed to identify each cardiac adverse effect.
Descriptive statistics are expressed as mean ± standard deviation with minimal and maximal values according to the model mean ± SD [min;max]. Percentages were calculated for qualitative data. For kalemia and QTc the difference between the value at the time of the ADR and the value at LPV/r instauration was calculated under the description “delta”. Normality of data was assessed with the Shapiro-Wilk test. QTc mean comparisons were made using paired Student “t” two-sided test with results given as point estimates and 95% confidence intervals (CI95). Chi 2 test was performed to evaluate the association between high residual loponavir values and severity of the ADR. P values lower than 0.05 were considered as statistically significant. Incidence was calculated using Fisher's exact method (Clopper-Pearson) and results given as point estimates and 95% confidence intervals. All the calculations were performed using the statistical software “R” [28].
3. Results
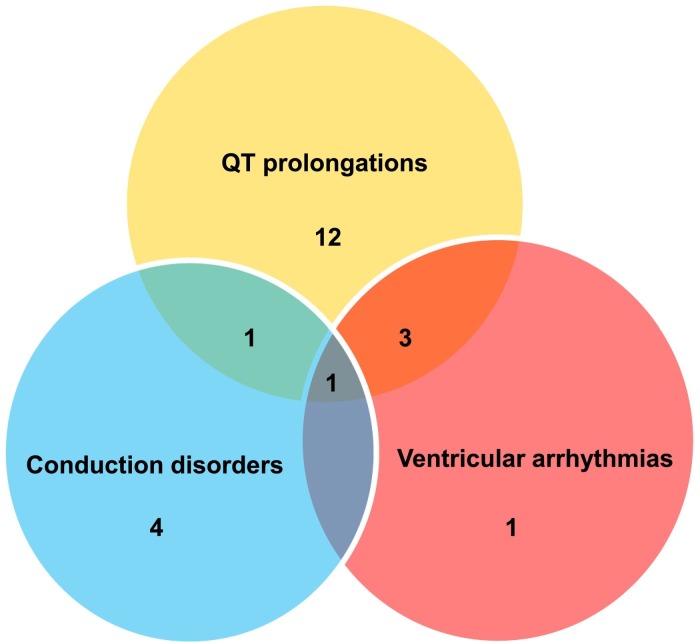
Over the course of 8 weeks, 176 cases of cardiotoxicity involving a drug used against COVID-19 were reported. Among these, 22 were associated with the use of LPV/r (12.5%), representing a total of 28 cardiac ADRs (Fig. 1 ). The mean age of these 22 cases (15 M, 7F) was 72 ± 9 yrs [49;92].
Fig. 1.
Repartition of cardiac adverse drug reactions cases.
All patients had received in-hospital treatment: 8 cases in intensive-care and 14 in specialized COVID-19 units. There was no case associated with ambulatory or self-medication treatment. On average, the ADRs occurred on day 4 ± 3 [0;11] of treatment. All patients had received a dose of 400/100 mg LPV/r twice a day except, one who received 600/150 mg BID. All cases were notified as serious and comprised: 1 death (4.5%), 3 life-threatening situations (13.6%), 13 prolongations of hospitalization (59.1%) and 5 other serious medical situations (22.7%). LPV/r imputability was plausible or very plausible in 15 out of 22 cases (68.2%).
3.1. Ventricular arrhythmias and QTc prolongations
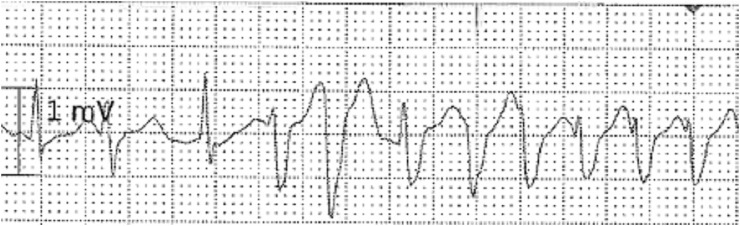
Five ventricular arrhythmias (17.9%) were reported including one case of polymorphic ventricular tachycardia requiring 2 cardioversions (Fig. 2 ) and one case of ventricular fibrillation (with confounders) leading to a cardiac arrest. Ventricular arrhythmia regressed spontaneously after treatment's discontinuation in 2 of the remaining cases and the evolution was unknown for the last one.
Fig. 2.
Torsade de Pointes ventricular tachycardia after the start of LPV/r 400/100 mg twice a day in a 61 y.o. man hospitalized for COVID-19 in intensive care unit. Baseline Bazett-corrected QTs was measured at 408 ms, prolonged to 520 ms at the time of the arrhythmia. Outcome was favorable after cardioversion and LPV/r withdrawal.
QTcs were specified in 18 cases, and above normal limit in 17 (94.4%). Among these, 12 (70.6%) were considered serious with 11 QTc ≥ 500 ms and 7 delta QTc > 60 ms. The average mentioned QTc before treatment was 409 ± 38 ms [340;483], and at the time of the ADR 511 ± 47 ms [427;601] with a mean difference of 97 ± 69 ms [−3;201] (p < 0.001, CI 95: 502–520). The QTc returned to normal after LPV/r's interruption in 15 cases (2 cases with unknown evolution).
3.2. Conduction disorders
Six cases of conduction disorders (21.4%), were reported, including 5 bradycardias and one bundle branch block. These ADRs regressed upon LPV/r discontinuation and did not require any temporary or permanent pace-maker.
3.3. Risk factors and associated coprescriptions
Among the 22 patients, 9 (40.9%) presented with at least 1 risk factor decreasing the cardiac repolarization reserve: hypokalemia or significant decrease thereof (1 mM) in 3 cases, hypomagnesemia in one case and 5 cases of ischemic heart disease.
LPV/r was associated in 14 cases with at least one drug known to prolong the QTc. In 8 cases (36.4%), it was a COVID-19 co-prescription: 4 cases in association with hydroxychloroquine, 3 cases in association with azithromycin and 1 case with erythromycin (COVID-19 indication), which are three relevant IKr blockers. Ten cases were associated with the use of one drug only, 2 drugs in 2 cases, and 3 drugs or more in 2 cases. No other known drug interaction was associated with the occurrence of the reported cardiac ADRs, either from a pharmacokinetic or pharmacodynamic point of view.
Lopinavir therapeutic drug monitoring was notified for 11 (50.0%) patients. Ten out of 11 patients (90.9%) had a lopinavir residual plasma concentration above the normal limit of 8 mg/L with a mean concentration of 18.6 ± 8.8 mg/L [0.7;34.4]. There was no significant correlation between lopinavir residual concentration above the limit and the severity of the case (p > 0.05).
3.4. ECG's reassessment
Out of 22 reports, 15 (68.2%) were supported by available ECGs and the 7 remaining ones had enough specific information notified to perform a conclusive analysis.
In our department, QTc was re-measured in 10 cases. The mean QTcB at the time of the ADR was measured at 483 ± 52 ms [413;585] with a delta QTc of 86 ± 60 ms [13;161], without significant difference with declared values (p = 0.35, CI95: 473–193). However, discrepancies were present at an individual level.
A QTc above the normal limit was confirmed in 8/10 (80.0%) cases. The causality of LPV/r was not retained in 2 cases which did not display a significant QTc prolongation after ECGs reassessment. The severity was confirmed in 4/7 cases with one non-serious QT prolongation reclassified as serious.
3.5. Estimated incidence of LPV/r's cardiac ADRs
In the FPDB between 2001 and 2019 a total of 63 reports of cardiac ADRs have been associated with LPV/r. Since its commercialization in 2001, our cases represent more than a quarter (25.9%) of the total notifications of cardiotoxicity. This represents ~ a 45 fold increase of notifications since the beginning of COVID-19.
The average monthly consumption of LPV/r in 2020 before COVID-19 pandemic was 3616 g. In March 2020 it increased more than 10-fold to 40,780 g. Therefore, we estimate at ~37,000 g the quantity of LPV/r consumed for COVID-19 within one month, representing ~ between 3300 and 4600 patients treated either for 14 or 10 days. This yields an incidence of 0.3% to 0.4% [0.15;0.67] of cardiac ADRs during the month of March (notwithstanding a possible strong ADRs underreporting).
4. Discussion
We shed some new light on LPV/r cardiotoxicity by characterizing its cardiac safety during COVID-19. We clearly confirm the previous suspicions of LPV/r impact on cardiac repolarization. We had previously raised concerns of possible QT prolongation with LPV/r during its development, but only vague and non-specific mentions of such a risk figured in the SmPC, and deemed important only at supratherapeutic doses in the risk management plan.
Few cases of LPV/r cardiotoxicity have been reported and most describe cardiac conduction problems like AV blocks [6,7,[9], [10], [11],29], notwithstanding a case of sudden cardiac death after drug interactions [8]. Even if LPV/r is considered a drug with a risk of torsade de pointes based on its hERG liability at therapeutic levels [13,30,31], rare and conflicting studies concerning LPV/r-induced QT prolongation have been published [15,16,31]. Therefore, spontaneous pharmacovigilance reports represent an invaluable tool to explore the possible cardiotoxicity of drugs [32].
Our study reports 22 cases of cardiac ADRs in 8 weeks, which is substantially greater than pre-COVID-19 and most probably reflects the wide and sudden empirical use of LPV/r. Indeed, a global increase of pharmacovigilance's notifications was observed for LPV/r with 475 reports in 2019 vs 611 from the first semester of 2020 alone (Uppsala monitoring center) [33]. The resulting incidence of cardiac ADRs estimated is 0.3 to 0.4%, corresponding to a frequency qualified as “uncommon” on a regulatory aspect (ADRs ≥1/1000, < 1/100). Furthermore, that incidence is likely to be underestimated, when taking into consideration the strong underreporting of ADRs in pharmacovigilance which can reach up to 94% [34]. Indeed, the COVID-19 pandemic is not the most favorable context for ADRs notifications, despite their frequency, due to hospitals' saturation, the subsequent stress it generates and the lack of time for health professionals to deal with such issues as reporting side effects. Because our calculations did not include the constraints due to drug packaging or dispensation processes, the number of patients treated might be overestimated, hence underestimated the incidence. Finally, and not the least, the ANSM regulates ADRs occurring during clinical trials –a non-negligible part of LPV/r prescription in COVID-19- differently from spontaneous notifications, dodging therefore RCPVs scrutiny.
All reported LPV/r-associated cardiac ADRs were well documented with ECGs available in over two thirds of the cases. After QTc re-measurement, the causality link with LPV/r was missing in two cases only. ADRs reported can be associated with LPV/r potency to block ionic channels. Most can reliably be traced to hERG inhibition [13] with 17 QT prolongation and 5 ventricular arrhythmias. Indeed, the mean blood concentration of 18.6 mg/L of lopinavir observed corresponds to ~30 μM which largely encompass (by two to three fold) the range of hERG blocking potencies of either ritonavir or lopinavir (~8 to 9 μM [13]).
The cases of conduction disorders including bradycardias are also consistent with inhibitory action on sodium/calcium channels, all of these reflecting the mild multi-channel-block drug [35] exerted by LPV/r. We are not aware of any consensus on follow-up ECGs during LPV/r for HIV treatment. A regular ECG's monitoring (every year) during long time treatment with LPV/r might prevent some of these cardiac ADRs.
Plasma concentrations observed in our study were quite elevated and at odds with what has previously been published (1–8 mg/L [23,36]). Lopinavir residual plasma concentrations of 8 ± 6 mg have been described previously [37]. This discrepancy has also been observed in other COVID-19 units [38,39]. This might be of concern, since the off-label use of LPV/r in COVID-19 requires the same regular posology as HIV treatment. The unbound fraction that represents the active part of the drug seems unchanged despite increased overall concentrations [40]. If part of the discrepancy originates in the undervalued normal range, inflammation has been recently shown to potently augment lopinavir bioavailability through inhibition of CYP450 3A4 [41]. Indeed, the augmented lopinavir concentrations correlate with those of CRP, mediated by Interleukin-6 (IL-6), in COVID-19 patients, and are prevented by the administration of the IL-6 inhibitor tocilizumab [42]. Our study though, relied solely on spontaneous notifications, and IL6 or CRP concentrations were not measured/notified. We could not relate lopinavir high residual concentrations and the severity of the case either.
Systemic and cardiac inflammatory states associated with COVID-19 is indeed a significant risk factor [42]. Whether by direct cytokine-dependent QT prolongation or secondary to CYP450 inhibition resulting in augmented bioavailability of QT prolonging drugs [43], COVID-19 definitely predisposes to the occurrence of cardiac arrhythmia [42,43]. The different monitoring protocols put in place in COVID-19 hospital units have taken this into account in their propositions [[42], [43], [44]].
Our study presents limitations though. The occurrence of cardiac ADRs may be facilitated by COVID-19, as for SARS CoV-2 induced hypokalemia [19] or cardiomyopathy [18,45,46]. Hypomagnesemia is also present in COVID-19 [47], as are confounding drugs, like in all real conditions of use. Finally, if spontaneous reporting of ADRs is paramount for the qualitative characterization of drug adverse reactions (i.e.specificity), it is not optimal for their quantitative aspects (sensitivity) [48].
Other drugs tested in COVID-19 also prolong the QTc interval [20,42], and even casual ones frequently used in lay patients such as domperidone or escitalopram. Because of the overwhelmingly male representation [49] of severe COVID-19 cases, the low percentage of women (25%) in our study, does not preclude the usual female sex propensity of drug-acquired QT prolongation usually observed [50].
5. Conclusion
As for hydroxychloroquine, we report an increase of cardiac ADRs associated with the empirical use of LPV/r during COVID-19 pandemic. These ADRs likely reflect LPV/r multichannel blocking properties of clinical significance, including hERG blockade. The risk of QT prolongation, suspected since the launch of LPV/r is now assessed with its array of “classical” cardiac ADRs reported during the COVID-19 pandemic. LPV/r SmPC should be implemented and its benefit/risk use, still questionable in the absence of effectiveness, reassessed during COVID-19 [3].
Declaration of Competing Interest
None.
Acknowledgments
The views expressed in this article are the personal views of the author(s) and may not be understood or quoted as being made on behalf of or reflecting the position of the Agence Nationale de Sécurité du Médicament et des produits de santé [ANSM] or one of its committees or working parties.
We thank Michael O'Dell for proofreading and useful comments.
Bibliography
- 1.de Wilde A.H., Jochmans D., Posthuma C.C., Zevenhoven-Dobbe J.C., van Nieuwkoop S., Bestebroer T.M., van den Hoogen B.G., Neyts J., Snijder E.J. Screening of an FDA-approved compound library identifies four small-molecule inhibitors of Middle East respiratory syndrome coronavirus replication in cell culture. Antimicrob. Agents Chemother. 2014;58:4875–4884. doi: 10.1128/AAC.03011-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nutho B., Mahalapbutr P., Hengphasatporn K., Pattaranggoon N.C., Simanon N., Shigeta Y., Hannongbua S., Rungrotmongkol T. Why are Lopinavir and ritonavir effective against the newly emerged coronavirus 2019? Atomistic insights into the inhibitory mechanisms. Biochemistry. 2020;59:1769–1779. doi: 10.1021/acs.biochem.0c00160. [DOI] [PubMed] [Google Scholar]
- 3.Dorward J., Gbinigie K. Lopinavir/Ritonavir: A Rapid Review of Effectiveness in COVID-19. 2020. https://covid19-evidence.paho.org/handle/20.500.12663/1087
- 4.Chandwani A., Shuter J. Lopinavir/ritonavir in the treatment of HIV-1 infection: a review. Ther. Clin. Risk Manag. 2008;4:1023–1033. doi: 10.2147/tcrm.s3285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaubey S.K., Sinha A.K., Phillips E., Russell D.B., Falhammar H. Transient cardiac arrhythmias related to lopinavir/ritonavir in two patients with HIV infection. Sex. Health. 2009;6:254–257. doi: 10.1071/SH09005. [DOI] [PubMed] [Google Scholar]
- 6.Jiménez F.J., Pinilla J., Repiso M., Labarga P. Bloqueo auriculoventricular completo en paciente tratado con lopinavir/ritonavir. Enfermedades Infecc. Microbiol. Clínica. 2002;20:415–418. doi: 10.1016/s0213-005x(02)72835-8. [DOI] [PubMed] [Google Scholar]
- 7.Kikuchi Y., Genka I., Ishizaki A., Sunagawa K., Yasuoka A., Oka S. Serious Bradyarrhythmia that was possibly induced by Lopinavir-ritonavir in 2 patients with acquired immunodeficiency syndrome. Clin. Infect. Dis. 2002;35:488–490. doi: 10.1086/341975. [DOI] [PubMed] [Google Scholar]
- 8.Kobayashi M., Takata Y., Goseki Y., Mizukami H., Hara S., Kuriiwa F., Fukutake K., Yoshida K. A sudden cardiac death induced by sildenafil and sexual activity in an HIV patient with drug interaction, cardiac early repolarization, and arrhythmogenic right ventricular cardiomyopathy. Int. J. Cardiol. 2015;179:421–423. doi: 10.1016/j.ijcard.2014.11.090. [DOI] [PubMed] [Google Scholar]
- 9.Puech R., Gagnieu M.-C., Planus C., Charpiat B., Boibieux A., Ferry T., Tod M. Extreme bradycardia due to multiple drug–drug interactions in a patient with HIV post-exposure prophylaxis containing lopinavir–ritonavir. Br. J. Clin. Pharmacol. 2011;71:621–623. doi: 10.1111/j.1365-2125.2010.03849.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sasaki S., Yanagisawa N., Suganuma A., Imamura A., Ajisawa A. Sick sinus syndrome possibly due to lopinavir-ritonavir: report of two cases. Kansenshogaku Zasshi. 2013;87:613–617. doi: 10.11150/kansenshogakuzasshi.87.613. [DOI] [PubMed] [Google Scholar]
- 11.Yotsumoto M., Kitano K., Saito H. Bradycardia–tachycardia syndrome induced by lopinavir–ritonavir in a patient with AIDS. AIDS. 2005;19:1547–1548. doi: 10.1097/01.aids.0000183942.05849.1b. [DOI] [PubMed] [Google Scholar]
- 12.Crumb W.J., Vicente J., Johannesen L., Strauss D.G. An evaluation of 30 clinical drugs against the comprehensive in vitro proarrhythmia assay (CiPA) proposed ion channel panel. J. Pharmacol. Toxicol. Methods. 2016;81:251–262. doi: 10.1016/j.vascn.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Anson B.D., Weaver J.G., Ackerman M.J., Akinsete O., Henry K., January C.T., Badley A.D. Blockade of HERG channels by HIV protease inhibitors. Lancet. 2005;365:682–686. doi: 10.1016/S0140-6736(05)17950-1. [DOI] [PubMed] [Google Scholar]
- 14.Drici M., Barhanin J. Cardiac K+ channels and drug-acquired long QT syndrome. Thérapie. 2000;55:185–193. [PubMed] [Google Scholar]
- 15.Soliman E.Z., Lundgren J.D., Roediger M.P., Duprez D.A., Temesgen Z., Bickel M., Shlay J.C., Somboonwit C., Reiss P., Stein J.H., Neaton J.D. Boosted protease inhibitors and the electrocardiographic measures of QT and PR durations. AIDS Lond. Engl. 2011;25:367–377. doi: 10.1097/QAD.0b013e328341dcc0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rathbun C.R., Liedtke M.D., Blevins S.M., Harrison D., Lockhart S.M., Salvaggio M., Acosta E.P. Electrocardiogram abnormalities with Atazanavir and Lopinavir/ritonavir. HIV Clin. Trials. 2009;10:328–336. doi: 10.1310/hct1005-328. [DOI] [PubMed] [Google Scholar]
- 17.Klein C., Chiu Y., Da Silva B., Noertersheuser P., Awni W., Holas C., Doan T., Bernstein B. Evaluation of the impact of lopinavir/ritonavir (LPV/r) and ritonavir (RTV) on QTcF: results of a thorough QT study. J. Int. AIDS Soc. 2008;11:P95. doi: 10.1186/1758-2652-11-S1-P95. [DOI] [Google Scholar]
- 18.Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M., Madhur M.S., Tomaszewski M., Maffia P., D’Acquisto F., Nicklin S.A., Marian A.J., Nosalski R., Murray E.C., Guzik B., Berry C., Touyz R.M., Kreutz R., Wang D.W., Bhella D., Sagliocco O., Crea F., Thomson E.C., McInnes I.B. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc. Res. 2020 doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen D., Li X., Song Q., Hu C., Su F., Dai J. Hypokalemia and Clinical Implications in Patients with Coronavirus Disease 2019 (COVID-19) MedRxiv. 2020 doi: 10.1101/2020.02.27.20028530. 2020.02.27.20028530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gérard A., Romani S., Fresse A., Viard D., Parassol N., Granvuillemin A., Chouchana L., Rocher F., Drici M.-D. 2020. “Off-Label” Use of Hydroxychloroquine, Azithromycin, Lopinavir-Ritonavir and Chloroquine in COVID-19: A Survey of Cardiac Adverse Drug Reactions by the French Network of Pharmacovigilance Centers, Therapies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Begaud B., Evreux J.C., Jouglard J., Lagier G. Imputabilité des effets inattendus ou toxiques des médicaments: actualisation de la méthode utilisée en France. Thérapie. 1985;40:111–118. [PubMed] [Google Scholar]
- 22.Miremont-Salamé G., Théophile H., Haramburu F., Bégaud B. Causality assessment in pharmacovigilance: the French method and its successive updates. Therapies. 2016;71:179–186. doi: 10.1016/j.therap.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Back D., Gibbons S., Khoo S. An update on therapeutic drug monitoring for antiretroviral drugs. Ther. Drug Monit. 2006;28:468–473. doi: 10.1097/01.ftd.0000211825.57984.41. [DOI] [PubMed] [Google Scholar]
- 24.Suzanne Vink Arja, Benjamin Neumann, Lieve Krystien V.V., Sinner Moritz F., Nynke Hofman, Soufiane el Kadi, Schoenmaker Melissa H.A., Slaghekke Hanneke M.J., de Jong Jonas S.S.G., Clur Sally-Ann B., Blom Nico A., Stefan Kääb, Wilde Arthur A.M., Postema Pieter G. Determination and Interpretation of the QT Interval. Circulation. 2018;138:2345–2358. doi: 10.1161/CIRCULATIONAHA.118.033943. [DOI] [PubMed] [Google Scholar]
- 25.Rautaharju P.M., Surawicz B., Gettes L.S., Bailey J.J., Childers R., Deal B.J., Gorgels A., Hancock E.W., Josephson M., Kligfield P., Kors J.A., Macfarlane P., Mason J.W., Mirvis D.M., Okin P., Pahlm O., van Herpen G., Wagner G.S., Wellens H., American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology, American College of Cardiology Foundation, Heart Rhythm Society, AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society Endorsed by the International Society for Computerized Electrocardiology. J. Am. Coll. Cardiol. 2009;53:982–991. doi: 10.1016/j.jacc.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 26.CredibleMeds, (n.d.). https://www.crediblemeds.org/ (accessed April 29, 2020).
- 27.MedDRA. Medical dictionary for regulatory activities., (n.d.). https://www.meddra.org/ (accessed June 2, 2020).
- 28.R Development Core Team . R Found. Stat. Comput; Vienna Austria: 2005. R: A language and environment for statistical computing.http://www.R-project.org [Google Scholar]
- 29.McArthur M.A., Kalu S.U., Foulks A.R., Aly A.M., Jain S.K., Patel J.A. Twin preterm neonates with cardiac toxicity related to lopinavir/ ritonavir therapy. Pediatr. Infect. Dis. J. 2009;28:1127–1129. doi: 10.1097/INF.0b013e3181acd17e. [DOI] [PubMed] [Google Scholar]
- 30.Hazell L., Raschi E., Ponti F.D., Thomas S.H.L., Salvo F., Helgee E.A., Boyer S., Sturkenboom M., Shakir S. Evidence for the hERG liability of antihistamines, antipsychotics, and anti-infective agents: a systematic literature review from the ARITMO project. J. Clin. Pharmacol. 2017;57:558–572. doi: 10.1002/jcph.838. [DOI] [PubMed] [Google Scholar]
- 31.Sánchez-Chapula J.A., Navarro-Polanco R.A., Culberson C., Chen J., Sanguinetti M.C. Molecular determinants of voltage-dependent human ether-a-go-go related gene (HERG) K+ channel block. J. Biol. Chem. 2002;277:23587–23595. doi: 10.1074/jbc.M200448200. [DOI] [PubMed] [Google Scholar]
- 32.Drici M.-D., Knollmann B.C., Wang W.-X., Woosley R.L. Cardiac actions of erythromycin: influence of female sex. JAMA. 1998;280:1774–1776. doi: 10.1001/jama.280.20.1774. [DOI] [PubMed] [Google Scholar]
- 33.VigiLyze, (n.d.). https://vigilyze.who-umc.org/ (accessed September 8, 2020).
- 34.Hazell L., Shakir S.A.W. Under-reporting of adverse drug reactions. Drug Saf. 2006;29:385–396. doi: 10.2165/00002018-200629050-00003. [DOI] [PubMed] [Google Scholar]
- 35.Vicente J., Zusterzeel R., Johannesen L., Ochoa-Jimenez R., Mason J.W., Sanabria C., Kemp S., Sager P.T., Patel V., Matta M.K., Liu J., Florian J., Garnett C., Stockbridge N., Strauss D.G. Assessment of multi-Ion Channel block in a phase I randomized study design: results of the CiPA phase I ECG biomarker validation study. Clin. Pharmacol. Ther. 2019;105:943–953. doi: 10.1002/cpt.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jackson A., Hill A., Puls R., Else L., Amin J., Back D., Lin E., Khoo S., Emery S., Morley R., Gazzard B., Boffito M. Pharmacokinetics of plasma lopinavir/ritonavir following the administration of 400/100 mg, 200/150 mg and 200/50 mg twice daily in HIV-negative volunteers. J. Antimicrob. Chemother. 2011;66:635–640. doi: 10.1093/jac/dkq468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Klein C., Xiong J., Causemaker S., Li J., Chiu Y., Woulfe M., Da Silva B., Bernstein B. Abbott Park; IL, USA: 2008. Comparison of Lopinavir and Ritonavir Tablet and Soft Gelatin Capsule (SGC) Pharmacokinetics in Antiretroviral-Naïve HIV-1 Infected Subjects, in: Abbott. [Google Scholar]
- 38.S. Baldelli, M. Corbellino, E. Clementi, D. Cattaneo, C. Gervasoni, Lopinavir/ritonavir in COVID-19 patients: maybe yes, but at what dose?, J. Antimicrob. Chemother. (n.d.). doi: 10.1093/jac/dkaa190. [DOI] [PMC free article] [PubMed]
- 39.Venisse N., Peytavin G., Bouchet S., Gagnieu M.-C., Garraffo R., Guilhaumou R., Solas C. Concerns about pharmacokinetic (PK) and pharmacokinetic-pharmacodynamic (PK-PD) studies in the new therapeutic area of COVID-19 infection. Antivir. Res. 2020;181:104866. doi: 10.1016/j.antiviral.2020.104866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gregoire M., Le Turnier P., Gaborit B.J., Veyrac G., Lecomte R., Boutoille D., Canet E., Imbert B.-M., Bellouard R., Raffi F. Lopinavir pharmacokinetics in COVID-19 patients. J. Antimicrob. Chemother. 2020 doi: 10.1093/jac/dkaa195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marzolini C., Stader F., Stoeckle M., Franzeck F., Egli A., Bassetti S., Hollinger A., Osthoff M., Weisser M., Gebhard C.E., Baettig V., Geenen J., Khanna N., Tschudin-Sutter S., Mueller D., Hirsch H.H., Battegay M., Sendi P. Effect of Systemic Inflammatory Response to SARS-CoV-2 on Lopinavir and Hydroxychloroquine Plasma Concentrations. Antimicrob. Agents Chemother. 2020;64 doi: 10.1128/AAC.01177-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Naksuk N., Lazar S., Bee T. Peeraphatdit, Cardiac safety of off-label COVID-19 drug therapy: a review and proposed monitoring protocol. Eur. Heart J. Acute Cardiovasc. Care. 2020;9:215–221. doi: 10.1177/2048872620922784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lazzerini P.E., Boutjdir M., Capecchi P.L. COVID-19, arrhythmic risk, and inflammation: mind the gap! Circulation. 2020;142:7–9. doi: 10.1161/CIRCULATIONAHA.120.047293. [DOI] [PubMed] [Google Scholar]
- 44.Funck-Brentano C., Salem J.-E., Nguyen L.S., Drici M.-D., Roden D.M. Response to the editorial “COVID-19 in patients with cardiovascular diseases”: Covid-19 treatment with hydroxychloroquine or chloroquine and azithromycin: a potential risk of Torsades de pointes. Arch. Cardiovasc. Dis. 2020;113:367–368. doi: 10.1016/j.acvd.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Inciardi R.M., Lupi L., Zaccone G., Italia L., Raffo M., Tomasoni D., Cani D.S., Cerini M., Farina D., Gavazzi E., Maroldi R., Adamo M., Ammirati E., Sinagra G., Lombardi C.M., Metra M. Cardiac Involvement in a Patient with Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kang Y., Chen T., Mui D., Ferrari V., Jagasia D., Scherrer-Crosbie M., Chen Y., Han Y. Heart Br. Card Soc; 2020. Cardiovascular Manifestations and Treatment Considerations in Covid-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.D’Amico F., Baumgart D.C., Danese S., Peyrin-Biroulet L. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol Assoc; 2020. Diarrhea during COVID-19 Infection: Pathogenesis, Epidemiology, Prevention and Management. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Drici M.-D. Estimates of population-based incidence of malignant arrhythmias associated with medication use – a narrative review. Fundam. Clin. Pharmacol. 2020;34:416–417. doi: 10.1111/fcp.12582. [DOI] [PubMed] [Google Scholar]
- 49.Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir. Med. 2020;8 doi: 10.1016/S2213-2600(20)30117-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Drici M.-D., Clément N. Is gender a risk factor for adverse drug reactions? Drug Saf. 2001;24:575–585. doi: 10.2165/00002018-200124080-00002. [DOI] [PubMed] [Google Scholar]