Introduction
Psoriasis is a chronic, immune-mediated disorder mainly affecting the skin and joints. The pathogenesis involves keratinocyte hyperproliferation, complex cytokine and interleukin (IL) interactions, polygenic predisposition, and known association with environmental triggers, including infections, medications, trauma, and stress.1 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), is associated with not only flares of psoriasis in patients with well-documented disease2, 3, 4 but also other cutaneous diseases.5, 6, 7 However, there have yet to be any reports showing new-onset psoriasis in patients with SARS-CoV-2/COVID-19. We report such a case in a 62-year-old woman.
Case report
A 62-year-old woman with obesity, asthma, diabetes mellitus type 2, hypertension, and atrial fibrillation presented to her primary care provider with a 3-day history of fatigue, cough, shortness of breath, night sweats, chills, and myalgia. SARS-CoV-2 testing via nasopharyngeal swab was positive and the patient remained symptomatic for the next 2 weeks. Two weeks after the resolution of her symptoms, she developed blisters on her palms, which continued to progress over the ensuing 2 weeks, prompting her to seek medical attention at a local urgent care facility, where she was prescribed 0.1% triamcinolone ointment for “dyshidrotic eczema.” As the pruritic rash continued to spread and involve her forearms, trunk, and scalp, she returned to her primary care physician, who referred her to the emergency department.
A well-appearing nontachypneic woman with a temperature of 97.4°F, heart rate of 110 beats/min (irregularly irregular), blood pressure of 138/90 mmHg, and oxygenation of 99% on room air presented to the emergency room. Medications of 3 years included metoprolol, apixaban, beclomethasone and albuterol inhalers, vitamin B12, and folate. She denied having medication allergies. Her social history was notable for a 23-pack-year history of cigarette smoking (quit in 1994) and consumption of 4 drinks of alcohol weekly. Her family history was notable for an aunt and a cousin with psoriasis. She denied having joint pain or stiffness. A review of systems was otherwise noncontributory. Skin examination revealed palmoplantar pustules, palmar erythema with hyperkeratosis and desquamation, pink papulopustules on the extremities, and psoriasiform plaques on the trunk and scalp (Fig 1, Fig 2, Fig 3). Laboratory examination was notable for AST/ALT 40/35, alkaline phosphatase 114 BUN/CR 12/0.66, negative SARS-CoV-2 rRT-PCR, negative skin pustule culture, and bilateral trace pleural effusions on P-A/lateral chest X-ray.
Fig 1.
The progression of psoriasis 4 weeks after the resolution of SARS-CoV-2 symptoms, showing palmar erythema with pustules, hyperkeratosis, and desquamation. SARS-CoV-2, Severe acute respiratory syndrome coronavirus 2.
Fig 2.
Oval, pink, scaly psoriasiform plaques on the back.
Fig 3.
Oval, pink, scaly plaque on the scalp.
Three 4-mm punch biopsies were obtained from the right palm, left wrist, and right forearm, which revealed epidermal acanthosis with subtle-to-mild diffuse spongiosis, few dilated papillary dermal capillaries, large subcorneal neutrophilic pustules, and overlying parakeratosis with neutrophils (Munro microabscesses), consistent with psoriasis (Fig 4).
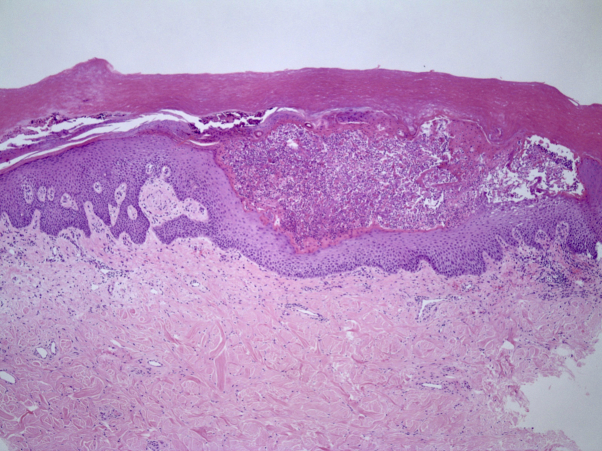
Fig 4.
A punch biopsy of the right palm revealing epidermal acanthosis, focal neutrophilic spongiosis, large subcorneal neutrophilic pustules, and overlying hyperkeratosis with neutrophils (Munro microabscesses). (Hematoxylin-eosin stain; original magnification: ×20.)
Review of the literature and discussion
Numerous and varied cutaneous associations with SARS-CoV-2 infection have been described.5, 6, 7 Only a subset of SARS-CoV-2 cases have reported association with psoriatic flares.2, 3, 4 The first case reported a 71-year-old woman with a known history of psoriasis in whom a flare developed on day 4 of SARS-CoV-2 treatment with oseltamivir and hydroxychloroquine.2 The second case reported a 73-year-old man on maintenance cyclosporine and methotrexate for psoriasis whose medications were discontinued in the setting of a SARS-CoV-2 infection, prompting a psoriasis flare 2 weeks later, followed by improvement once his medications were restarted.3 The third case reported a 48-year-old woman with a 30-year history of psoriasis in whom a flare developed with an active SARS-CoV-2 infection but improved after treatment with hydroxychloroquine, azithromycin, oseltamivir, and inhaled ipratropium and budesonide.4
This report is unique as it describes new-onset pustular psoriasis in the setting of SARS-CoV-2/COVID-19. Psoriasis, and in particular pustular psoriasis, has been associated with a number of triggers, including infection (i.e., Streptococcus spp, human immunodeficiency virus) and medications (i.e., terbinafine, beta-blockers, hydroxychloroquine), including rapid withdrawal of corticosteroids,8 none of which pertained to our patient. Although she was taking metoprolol, she had been on it for years without complication. In our predisposed patient with several comorbid conditions, including obesity, diabetes, and hypertension, as well as a positive family history, psoriasis developed 2 weeks after her SARS-CoV-2 infection. Inflammatory cytokines, including IL-2, IL-10, IL-12, IL-17, granulocyte colony-stimulating factor, macrophage inflammatory protein 1, and tumor necrosis factor-α, have been associated with SARS-CoV-2 infection, many of which are also associated with psoriasis.1 The 2-week delay in the onset of cutaneous disease after the resolution of respiratory symptoms suggests that SARS-CoV-2–related inflammation had not yet resolved despite the patient being otherwise asymptomatic. Further studies are needed to help elucidate the relationship between SARS-CoV-2 and psoriasis, including skin biopsies in patients with active or recent SARS-CoV-2 infection for clinicopathologic correlation.
In summary, this case describes a patient who developed an acral rash 2 weeks after the acute respiratory phase of COVID-19 had passed. Despite not having a history of psoriasis personally, she did have a positive family history of psoriasis in an aunt and a cousin. She denied taking any new precipitating medications prior to the onset of her rash. Skin biopsies revealed features consistent with pustular psoriasis. To our knowledge, this is the first report of new-onset psoriasis in the setting of SARS-CoV-2/COVID-19 in the literature.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Not applicable.
References
- 1.Hawkes J.E., Chan T.C., Krueger J.G. Psoriasis pathogenesis and the development of novel targeted immune therapies. J Allergy Clin Immunol. 2017;140(3):645–653. doi: 10.1016/j.jaci.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kutlu O., Metin A. A case of exacerbation of psoriasis after oseltamivir and hydroxychloroquine in a patient with COVID-19: will cases of psoriasis increase after COVID-19 pandemic? Dermatol Ther. 2020:e13383. doi: 10.1111/dth.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nasiri S., Araghi F., Tabary M., Gheisari M., Mahboubi-Fooladi Z., Dadkhahfar S. A challenging case of psoriasis flare-up after COVID-19 infection. J Dermatolog Treat. 2020:1–6. doi: 10.1080/09546634.2020.1764904. [DOI] [PubMed] [Google Scholar]
- 4.Ozaras R., Berk A., Ucar D.H., Duman H., Kaya F., Mutlu H. Covid-19 and exacerbation of psoriasis. Dermatol Ther. 2020:e13632. doi: 10.1111/dth.13632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diaz-Guimaraens B., Dominguez-Santas M., Suarez-Valle A. Petechial skin rash associated with severe acute respiratory syndrome coronavirus 2 infection. JAMA Dermatol. 2020;156(7):820–822. doi: 10.1001/jamadermatol.2020.1741. [DOI] [PubMed] [Google Scholar]
- 6.Galvan Casas C., Catala A., Carretero Hernandez G. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol. 2020;183(1):71–77. doi: 10.1111/bjd.19163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34:e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- 8.Bachelez H. Pustular psoriasis and related pustular skin diseases. Br J Dermatol. 2018;178(3):614–618. doi: 10.1111/bjd.16232. [DOI] [PubMed] [Google Scholar]