Abstract
Pain conditions in childhood often continue into adulthood. Childhood chronic pain is related to a range of vulnerabilities that may have contributed to the onset of childhood pain or that may co-occur as a consequence of childhood pain. These vulnerabilities have been shown to maintain pain and disability during childhood but may also contribute to long-term developmental and health impairments that affect adult life. If progress is to be made in reducing the impact of pain and disability through the lifespan, greater efforts need to be directed toward understanding why, for whom, and how pain occurring in childhood affects subsequent adult pain and health. In this review, a developmental framework is applied to link childhood pain to adult pain highlighting childhood vulnerabilities (emotional, health behavior, social/family, and neurobiological) that may represent pathways for interventions in childhood to interrupt this trajectory. Psychological interventions can play a key role in addressing childhood pain and vulnerabilities associated with risk for maladaptive adult outcomes. The review summarizes the evidence base for the effectiveness of psychological interventions for childhood chronic pain and identifies gaps and opportunities to further develop and test early targeted interventions in childhood to reduce childhood chronic pain as well as build resiliency to promote positive adult outcomes. A future research agenda is delineated including the need for longitudinal cohort studies from childhood into adulthood and testing of both targeted early intervention to reduce risk and build resiliency to enhance long-term adult pain, health, developmental, and social outcomes.
Keywords: chronic pain, childhood, life course, developmental perspective, longitudinal, prevention, psychological interventions
1. Introduction
Pain that persists for longer than three months is common in childhood; 5–8% of youth report severe and disabling chronic pain[28]. Pain can affect virtually all aspects of a child’s life including physical, psychological, social, and academic/school functioning[43], and is associated with family and economic burden[21; 48]. Despite this negative impact, pediatric chronic pain has been relatively understudied, likely for many reasons. Children are a smaller segment of the population, symptoms occurring in childhood may be considered transitory, and children do not yet incur substantial societal burden. However, children with pain are at risk for growing up to become adults with pain, mental health comorbidities, and with socioeconomic disadvantage. Therefore, if progress is to be made in reducing the impact of pain and disability through the lifespan, greater efforts need to be directed toward understanding why, for whom, and how pain that occurs in childhood affects subsequent adult life. This includes health outcomes and risk for continued chronic pain in adulthood but also adult productivity, longevity, and generativity. An important priority stemming from an increased understanding of childhood risk for poor adult outcomes is to design prevention approaches to effectively intervene during childhood to prevent a lifelong trajectory of pain and disability and to enhance adult developmental outcomes. Psychological interventions can play a key role in addressing childhood pain and vulnerabilities associated with risk for maladaptive adult outcomes.
Despite the evidence linking childhood pain to maladaptive adult outcomes, prevention strategies have been underutilized. Applying a developmental framework to link childhood pain to adult pain highlights opportunities to implement interventions in childhood to interrupt this trajectory. Indeed, tackling the societal burden of chronic pain is complex and requires a range of different intervention approaches. Developmental frameworks will enable us to better understand if and how the experience of pain during sensitive periods of life leads to continued pain and other adversities in adulthood, informing the need and types of interventions that can strengthen and enhance outcomes across the lifespan.
The aims of this review are to: (1) present a developmental model of chronic pain describing the vulnerabilities related to the experience of childhood chronic pain that are important to adult health and development, (2) provide a brief summary of the evidence for the effectiveness of psychological interventions for childhood chronic pain, and (3) identify gaps and opportunities for further developing early targeted interventions in childhood to address emotional, social/family, health behavior, and neurobiological vulnerabilities, and build resiliency to enhance long-term adult pain, health, developmental, and social outcomes. Although there is an emerging area of research on adverse childhood experiences as increasing risk for pain and psychiatric disorders in adulthood (e.g., [41]), this topic is beyond the scope of the present review. Instead, the review is focused on the experiences of childhood pain as affecting later adult health and wellbeing.
2. Impact of childhood chronic pain on adult pain, health, and developmental outcomes
Available data from both clinical and community samples suggest that pain conditions in childhood often continue into adulthood[13; 72]. This is true for primary pain conditions such as migraine and functional abdominal pain as well as pain related to chronic disease. In fact, many chronic health conditions (e.g., sickle cell disease, chronic pancreatitis) have worsening symptoms from childhood to adulthood during which pain becomes more severe and exposure to opioids (as well as risk for addiction) also increases[12]. In a longitudinal evaluation of health status from childhood to adulthood among patients with juvenile idiopathic arthritis, pain increased and physical health-related quality of life declined in adulthood compared to controls[70]. In a clinical sample diagnosed with functional abdominal pain (FAP) in childhood, Walker et al[72] found that 35% of patients continued to report symptoms consistent with the Rome III criteria for abdominal pain-related FGIDs as adults. Moreover, the majority of this subgroup of FAP patients reported developing headache and other non-abdominal chronic pain in adulthood and thus appeared to mature into adults with FGIDs and comorbid chronic pain. Kashikar-Zuck[27] and colleagues conducted longitudinal follow up of a clinical cohort with juvenile fibromyalgia syndrome diagnosed in childhood. They found that 58.1% continued to meet full ACR 2010 criteria for adult fibromyalgia at young adult follow-up. In a community sample of youth with frequent headache, Larsson et al[29] found that 19.1% of youth with childhood headache continued with frequent weekly headaches in young adulthood. These studies highlight the risk of continued pain from childhood to adulthood.
In addition to the risk for continued pain, there are compelling data to indicate that childhood pain is related to poor adult psychological and developmental outcomes. Multiple studies have demonstrated that childhood chronic pain predicts depression and anxiety disorders in adulthood, controlling for co-occurring psychopathology in childhood (e.g., [65]). For example, in a population-based community sample, presence of adolescent chronic pain was associated with higher subsequently reported rates of lifetime anxiety disorders (21.1% vs 12.4%) and depressive disorders (24.5% vs 14.1%) in adulthood as compared with individuals without a history of adolescent chronic pain [42]. Within specific pain conditions, there are similar findings. Fearon and Hotopf[13] found an association between childhood headache and adult psychiatric morbidity after controlling for social class and child mental health comorbidities. In Kashikar-Zuck et al.’s[27] follow up study of youth with fibromyalgia, the majority of individuals continued in adulthood to have impairments across physical, social, and psychological domains. Evidence also indicates that having childhood chronic pain is itself an independent risk factor for future opioid misuse in adulthood[20].
Beyond psychological outcomes there are emerging data on the impact of childhood pain on adult developmental outcomes including social, vocational, and educational functioning. In a recent study, Murray et al.[39] characterized the impact of having chronic pain in adolescence on subsequent educational, vocational, and social functioning in young adulthood using data from the National Longitudinal Study of Adolescent to Adult Health (Add Health). The sample included 3,174 youth with chronic pain and 11,610 without chronic pain from the community. Findings demonstrated that the presence of chronic pain in adolescence was associated with higher likelihood of dropping out of high school, lower likelihood of graduating from college, poor vocational functioning, and social impairments in young adulthood.
3. Developmental models of chronic pain
One of the most accepted frameworks for understanding chronic pain is the biopsychosocial model of pain, which has been applied to pediatric pain[32]. This model proposes three key domains as influencing an individual’s pain experience: biological factors (e.g., how pain is processed by the central nervous system), psychological factors (e.g. cognitive and emotional processes related to pain), and social and demographic factors (e.g. socioeconomic status, family dynamics). This broad model has been adapted in several ways to emphasize developmental factors including pediatric-specific and lifespan perspectives. For example, Palermo, Valrie, and Karlson[52] proposed a developmental model that considers how changes in children’s physiological, psychological, social, and emotional processes during distinct periods of childhood affect both the individual pain experience as well as familial perceptions of and responses to pain. Walco and colleagues [71] consider a lifespan perspective on chronic pain for developing a chronic pain taxonomy. They highlight the importance of factors in childhood such as immaturity, developmental potential, plasticity of the central nervous system, child and family psychosocial functioning, and intellectual, education, and developmental stages of childhood. Finally, Rosenbloom, Palermo, and Rabbitts[56] focus on understanding chronic pain impact in older adolescents and young adults using a developmental perspective on the transition to adulthood including neurobiological, psychological, behavioral, and social changes that impact education and vocation, independence from family, and peer and romantic relationships.
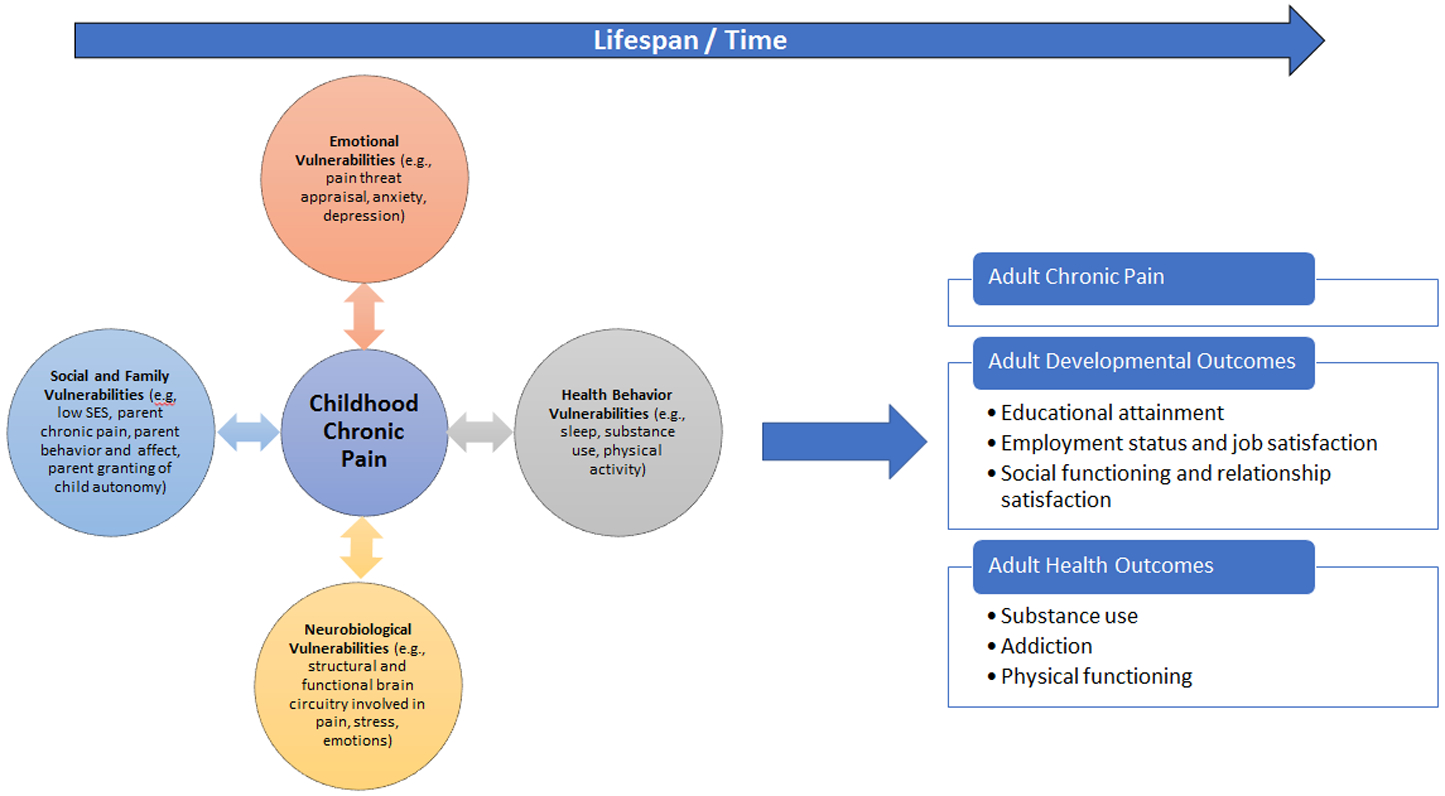
Building from these prior models and perspectives, I propose a developmental model identifying childhood vulnerabilities that influence childhood pain as well as adult outcomes. As shown in the left panel of Figure 1, childhood chronic pain is related to a range of vulnerabilities, which may be pre-morbid and predict the onset of childhood pain and/or may emerge as a consequence of childhood pain, co-occurring and maintaining pain and disability. Moreover, as shown in the right panel of Figure 1, childhood vulnerabilities may also amplify risk for poor adult outcomes including chronic pain (continuation of childhood pain or onset of new pain conditions in adulthood), substance use and addiction, poor physical functioning, and impairments in educational, vocational, and social functioning in adulthood linked to socio-economic disparities (e.g., difficulties with attaining higher education, employment, and economic independence). The model links childhood chronic pain to adult chronic pain and health outcomes through four pathways: emotional, health behavior, social and family, and neurobiological vulnerabilities. Examples of actionable targets are listed within each of these four pathways to illustrate how psychological interventions could interrupt and modify trajectories of pain throughout the lifespan.
Figure 1.
Developmental model of chronic pain from childhood to adulthood: implications for psychological treatment
3.1. Emotional vulnerabilities.
Examples of emotional vulnerabilities include pain-specific factors such as coping abilities and threat appraisal, as well as broader general symptoms of anxiety and depression or psychiatric conditions. Data available on premorbid emotional vulnerabilities for development of childhood chronic pain are primarily drawn from prospective population-based community cohort studies demonstrating that emotional concerns (e.g., anxiety, depression) detected on screening measures predict onset of chronic pain in childhood (e.g., [26]). A more robust literature exists on the co-occurrence of emotional vulnerabilities in children with chronic pain, including not only broader psychiatric conditions and symptoms such as anxiety[25], post-traumatic stress[23], and depression[63] but also pain-specific factors such as pain threat appraisal, pain-related fear, and pain catastrophizing [15]. These emotional vulnerabilities have been proposed to amplify or mutually maintain childhood pain and to predict poor long-term outcomes in adulthood. For example, studies have shown that anxiety and depression symptoms commonly co-occur in youth with chronic pain, and that these emotional vulnerabilities persist into young adulthood even as pain symptoms remit. Walker, et al [73] demonstrated that individuals falling in a high pain dysfunctional subgroup in adolescence, characterized by high severity of pain and gastrointestinal (GI) and non-GI symptoms, high pain threat appraisal, low pain coping efficacy, high catastrophizing, high negative affect, and high activity impairment had worse long-term adult outcomes compared to individuals in a low pain adaptive or high pain adaptive subgroup. Specifically, the high pain dysfunctional subgroup was more likely to continue to have functional gastrointestinal disorder (FGID) and comorbid non-abdominal chronic pain, and comorbid anxiety or depressive disorders in adulthood.
3.2. Health behavior vulnerabilities.
Lifelong health behaviors, including smoking and substance use, sleep, nutrition, and physical activity patterns develop during childhood and adolescence[7; 57; 77]. Limited data exist on the full range of health behavior vulnerabilities as predicting onset of childhood pain. Studies have demonstrated that sleep problems in childhood predict the development of subsequent chronic pain[24], highlighting sleep as an important antecedent factor. Most of the research on health behavior vulnerabilities focuses on concurrent associations with childhood chronic pain. For example, childhood chronic pain is associated with declines in physical activity and impairment in performing vigorous physical activities [75], which often leads to interference in school attendance and other normative childhood activities [43]. Studies examining the interrelationship of sleep and chronic pain have revealed that sleep deficiency, characterized by difficulties with quantity or quality of sleep, is highly comorbid in youth and adults with chronic pain [35; 53; 69], and is associated with diminished physical function, poor quality of life, impaired cognitive function, and increased anxiety and depressive symptoms[44; 49]. Health behavior vulnerabilities in childhood may impact adult outcomes. For example, in general populations, substance use in adolescence predicts adult substance use [68] including alcohol misuse [66] and opioid misuse[6]. Similarly adolescent patterns of physical activity predict adult patterns, including low activity predicting increased risk for metabolic disorders and obesity in adulthood[58]. In pain populations, longitudinal studies demonstrate that sleep problems in adolescence can become chronic, persisting over a one-year period[49] and impacting subsequent functioning and quality of life. Additional longitudinal studies are needed to understand how health behavior vulnerabilities associated with childhood chronic pain predict adult outcomes.
3.3. Social and family vulnerabilities.
Increasing attention has been directed toward understanding social and family vulnerabilities in the context of childhood chronic pain including the child’s own relational skills, age-appropriate autonomy/independence as well as the parenting and family context, including parent health, parenting behaviors, parental psychological distress, family dysfunction, and the broader family socioeconomic context [18; 52; 67]. Most of the research conducted on social and family factors as predictors of the onset of child pain has focused on parent pain status and socioeconomic indicators. Studies show that having one or both parents with chronic pain confers greater risk for the child to develop chronic pain in a dose-response fashion according to whether neither, one, or both parents have chronic pain [22] [38]. Specific parent and family cognitive, emotional, and behavioral factors and family socio-economic status have been identified as concurrently associated with chronic pain in childhood[18; 32; 47]. For instance, parent protective behaviors have been consistently associated with increased disability in children with chronic pain[5; 8; 54; 59; 74]. High levels of parental distress have also been clearly and consistently linked to increased pain and disability in children with chronic pain[52] [33]. More broadly, studies show that family and peer relationships are significantly impacted by chronic pain10,12,13. Social vulnerabilities also predict future adult health outcomes; socioeconomic conditions and housing quality in childhood are associated with an increased likelihood of adult onset chronic pain (e.g.,[40]) and low socioeconomic status in childhood predicts adult opioid use (e.g., [55]). Additional longitudinal research is needed to understand how the full range of parent and family vulnerabilities predict risk for poor adult outcomes.
3.4. Neurobiological vulnerabilities.
While there are many neurobiological vulnerabilities implicated in chronic pain, in the study of childhood pain it is particularly relevant to consider structural and functional brain circuitries involved in pain, emotion, stress and behavior; neuroplasticity plays an essential role in the development of brain circuitry from the neonatal period through to adolescence and young adulthood. Emerging studies to understand pain heritability provide some evidence that there may be neural correlates associated with risk for developing chronic pain. For example, in a novel pilot study using an emotion-cognition fMRI task, altered brain activity was found in adolescents who have a parent with chronic pain versus those adolescents who do not have a parent with chronic pain, suggesting that a phenotype associated with a chronic pain condition may emerge before youth have onset of significant pain symptoms [10]. Specifically, this study showed that youth with a parent with chronic pain had reduced brain activity in visual processing and affective brain regions, such as the amygdala, as well as differences in fronto-parietal regions, similar to what has been shown in adults and youth with chronic pain. There is also an emerging literature in youth with existing chronic pain (for a review of brain imaging studies see[2]), which demonstrate structural changes including widespread gray matter atrophy in motor, affective, motivational, emotional, cognitive, memory, and fear-related regions as well as functional connectivity changes in neural networks and amygdala-based covariance[60]. Whether any particular neurobiological vulnerability occurring in childhood is linked to future adult outcomes is not yet known. However, studies in neonates have demonstrated that the developing brain is vulnerable and that changes in pain-processing circuits in response to nociceptive stimuli can result in long-lasting anatomical and functional changes, which could contribute to adult pain and developmental outcomes.
4. Psychological Treatment to Address Childhood Pain and Vulnerabilities
4.1. Evidence base for psychological interventions for children and adolescents with chronic pain
Psychological treatment has been implemented primarily to treat ongoing chronic pain and disability in children and adolescents with chronic pain conditions. Cognitive-behavioral therapy (CBT) is the most frequently delivered psychological therapy to youth with chronic pain conditions. CBT for children is based on theories of behavior, cognition, learning, and emotion, similar to adult focused CBT. Specific strategies are focused on improving patient function by increasing patient activity level and involvement in pleasant and valued activities (“well behaviors”) as well as by altering cognitive content or what a patient thinks about pain [45]. In addition, given the influence of parents on children’s adjustment, social learning theory also plays a predominant role in treatment conceptualization where strategies are intended to alter parental responses to the child’s pain. Child-focused interventions typically include relaxation strategies, cognitive restructuring, behavior activation, and sleep or lifestyle interventions. Many treatment protocols incorporate several sessions to deliver parent-focused strategies intended to change behavioral responses to pain (operant strategies). To address the difficulties with children’s access to evidence-based pain treatment, digital health interventions using internet interventions and mobile applications are now being developed and evaluated (e.g., [51]).
The evidence base for psychological therapies for children with chronic pain is promising as summarized in several systematic reviews and meta-analyses of randomized controlled trials conducted either in person or remotely through digital health interventions [17] [16]. Among youth with headache disorders and youth with mixed chronic pain conditions, psychological therapies reduce pain severity and disability. Fewer studies have examined effects of psychological therapies on depression or anxiety symptoms but in a small number of studies effects were found for reducing anxiety (but not depression) in the short term in youth with mixed chronic pain conditions.
Several knowledge gaps remain that are important priorities for psychological intervention research in pediatric chronic pain including the need for more high-quality trials with adequate sample sizes, and trials including long-term follow up. There is an incomplete understanding of the full range of outcomes related to psychological treatment in pediatric chronic pain because of the more limited use of outcomes pertaining to pain impact and emotional functioning. Few data exist on long-term outcomes from psychological treatment in childhood to understand whether treatment is associated with positive young adult outcomes. In one of the few exceptions, Randall, et al [61] examined 5-year outcomes among youth who had previously received intensive interdisciplinary pain treatment, finding continued reductions in pain and disability as well as school completion and independent living in young adulthood. Further studies are needed to understand how interventions delivered to youth in childhood may affect long-term trajectories of pain or health outcomes.
4.2. Psychological treatment aimed at addressing childhood vulnerabilities
Although longitudinal studies have demonstrated risk for pain continuation from childhood to adulthood, as mentioned, there are very limited long-term studies of whether having received psychological treatment for chronic pain in childhood alters adult outcomes, likely due to the significant time and resource intense studies needed to address this question. Thus, much less is known about “why” and “how” pain in childhood is linked to specific adult outcomes, which has limited ability to create interventions to positively alter adult outcomes. However, as shown in Figure 1, intervention in childhood targeting emotional, health behavior, social and family, and neurobiological vulnerabilities may accomplish the proximal goal of reducing pain and disability and modifying vulnerability factors in childhood and may also contribute to the distal goal of preventing adult chronic pain and promoting positive adult development. Further research is also needed to develop preventive intervention approaches which may target vulnerabilities or focus on building resiliency in childhood and adolescence. In particular, research on transitional periods– such as the transition from middle childhood to adolescence and late adolescence to young adulthood, may be particularly important to consider in prevention strategies given these periods are defined by rapid change related to vulnerability factors. These are important avenues to consider in order to maximize the opportunity to use childhood interventions to positively affect adult trajectories.
Of interest in considering how psychological interventions may modify childhood vulnerabilities are data on the impact of interventions on neurobiological, emotional, health behavior, and social/family vulnerabilities. Changes in neurobiological vulnerabilities have been examined following intensive day-hospital treatment (consisting of rehabilitation therapies and CBT) in children with chronic pain. For example, Simons et al[60] demonstrated that intensive rehabilitation treatment including psychological interventions produced changes in youth’s neural connectivity (amygdala connectivity), which was associated with a decrease in self-reported pain. Researchers have purported that greater neuroplasticity in children compared to adults may lead to interventions producing more potent and lasting effects when delivered during childhood before irreversible brain changes have occurred[2].
Surprisingly, there are only a few pilot studies that have developed and implemented CBT interventions to address emotional vulnerabilities in children with chronic pain. Several studies focused on youth with comorbid anxiety or subclinical depression and pain aimed at prevention of poor psychological outcomes[64], enhancement of school functioning [34] and reduction of disability[11]. One case report presented a transdiagnostic intervention targeting emotion regulation and behavior change for treatment of chronic pain, anxiety, and depression in two adolescents[1]. There have also been a few studies to target mechanistic factors such as pain avoidance or pain threat. For example, in an exposure based psychological intervention for abdominal pain in children, reduced pain avoidance was a significant mediator of improved abdominal pain symptoms [4]. In an elegant single case design cohort series, in vivo graded exposure led to reductions in fear and pain avoidance, and pain-related disability in youth with mixed chronic pain conditions [62]. However, further data are needed to understand the potential benefits of these approaches.
A few studies have applied psychological interventions to address health behavior vulnerabilities, specifically sleep problems. Two small uncontrolled trials used CBT for insomnia (CBT-I) to treat co-occurring insomnia symptoms in youth with chronic pain[31; 46]. Delivering a four-session CBT-I protocol, Palermo et al[46] reported that youth made improvements in sleep hygiene and sleep quality, had reduced insomnia symptoms, and made improvements in physical and psychological health-related quality of life from pre-treatment to three-month follow up. This sample included adolescents with insomnia and comorbid physical or psychological difficulties, of whom approximately 50% had chronic pain. In a pilot study using a hybrid CBT intervention in youth with chronic migraine and insomnia, Law and colleagues found that youth made significant improvements from pre-treatment to post-treatment in reducing headache days and pain-related disability as well as improving sleep quality, patterns and insomnia symptoms[31].
Some evidence is available for targeted interventions in the social and family domain to modify parent behaviors and parent distress. A pilot randomized controlled trial of problem solving skills training (PSST) delivered to parent caregivers had positive findings for reducing parent psychological distress and produced downstream effects on reducing child distress as well [50]. In systematic reviews of parent interventions[30] psychological therapies showed some benefit in improving parenting behavior (e.g., reducing maladaptive behaviors) and parent mental health among parents of children with chronic pain. Overall, further work is needed to develop intervention strategies to effectively target childhood vulnerabilities that may influence long-term trajectories of pain and disability.
4.3. Using prevention focused strategies to build resiliency and promote positive development in childhood and adulthood
Given the high prevalence of chronic pain and tremendous personal and societal impact, it is surprising that prevention focused interventions have not yet been implemented. A key gap in knowledge that is likely preventing progress is understanding what familial and individual resilience resources and mechanisms are important for protecting against development of chronic pain across the lifespan. Such knowledge may lead to the development of resilience-enhancing interventions that target different developmental periods. In the field of mental health prevention, resiliency factors such as cognitive flexibility, problem solving, emotion regulation, and supportive social networks, have been targeted in community and school programs to address risk for stress, anxiety, depression, and substance use in adolescents[14]. Some programs target known periods of vulnerability for adolescents such as the transition from middle school to high school to build resiliency to prevent depression and anxiety[36].
There has been some call to arms in pediatric pain to measure resiliency including consideration of individual and familial resources and mechanisms [9] such as positive affect, positive social interactions, benefit finding, and self-regulation in response to pain. However, the context has been focused on children with existing chronic pain and their adaptation to pain. It will be critical to expand this focus and consider how resiliency factors can protect at risk populations in childhood (e.g., youth of parents with chronic pain, youth in low socioeconomic conditions) to prevent onset of pain, and how resiliency factors may relate to positive adult development and health outcomes. In particular, studies are needed that focus on the transition to young adulthood where both individual and familial resiliency resources may positively support transition to college, employment, and financial independence. Moreover, there have been developments in understanding the neurobiological underpinnings of resilience [37], with the implication that because of brain neuroplasticity in adolescence it is an ideal time to implement resilience-enhancing interventions that capitalize on potential for neural reorganization.
5. Summary and Future Research Directions
Childhood is a developmental period that conveys risk for or protection against subsequent chronic pain and disability across the lifespan. To address chronic pain at a societal level, pain prevention and management must begin in childhood and psychological interventions can play a key role. Although studies indicate a continuation of pain from childhood to adulthood, longitudinal cohort studies are needed to understand how pain in childhood is linked to adult outcomes including studying emotional, social/family, health behavior, and neurobiological vulnerabilities. As described in this review, although there is a body of evidence for psychological interventions for childhood chronic pain, there are limited targeted interventions aimed at modifying child vulnerabilities, most likely due to limited knowledge from longitudinal studies. Longitudinal cohort studies are needed that follow youth into adulthood. Future research is also needed to develop and evaluate the efficacy of targeted psychological interventions for youth with pain conditions addressing these vulnerabilities. For example, further work is needed to extend the few pilot interventions that have been developed for youth with comorbid anxiety or depression and chronic pain. Particularly relevant are the application of transdiagnostic interventions intended to be relevant across a range of mental disorders focused on emotion regulation. Trials are beginning to emerge in adults with chronic pain using this approach. Boersma et al[3] conducted an RCT to test the efficacy of a transdiagnostic emotion–focused exposure treatment for adults with chronic musculoskeletal pain and comorbid emotional problems. They found that compared to more traditional CBT for chronic pain, transdiagnostic intervention produced benefit for reducing pain catastrophizing, pain interference, and depression, although anxiety outcomes were not different. Similarly, transdiagnostic approaches could be implemented for youth with chronic pain and health behavior comorbidities (e.g., insomnia, obesity).
Building on the parent and family intervention research conducted to date, further research is needed to understand how and which specific childhood and social and family vulnerabilities impact long-term pain and other health and developmental outcomes in adulthood. Such research could lead to more focused interventions to prevent maladaptive lifespan trajectories, such as those that build and nurture autonomy and independence in adolescence, support an adaptive parent role, and specifically address attainment of developmental milestones in the transition from older adolescence to young adulthood (e.g., supporting transition to college, employment, and financial independence).
Given the scarcity of available pediatric chronic pain treatment in most communities, treatments need to be developed with accessibility in mind such as through using digital health interventions. Individuals should have easy access to psychological interventions across their lifespan – we shouldn’t expect pediatric patients to be “done” with treatment during childhood. There is a particularly crucial gap in treatment in young adulthood [56] in which risk for pain and poor developmental outcomes is increased and access to needed healthcare resources decline. There is an enormous need to focus on the transition to adult medical care in youth with chronic pain. Within other chronic health conditions recommendations have been made to support a transition process that starts in early adolescence[76]. Barriers to transition have been identified across a wide range of pediatric chronic conditions; the most common barriers include relationships with providers, difficulties with access and insurance, and beliefs and expectations about adult care[19]. Studies are needed in populations of youth with chronic pain to identify the service gaps in pain care that are experienced by older adolescents and young adults with chronic pain, and possible barriers to transition.
Further work is also needed to understand what individual and familial resiliency factors may prevent vulnerabilities that lead to chronic pain. Because the childhood vulnerabilities for chronic pain are shared with other negative health outcomes (e.g., mental health, substance use), prevention interventions may affect a wide range of behavioral and health outcomes. Prevention interventions could produce changes at a critical period of development and thereby reduce risk for many negative outcomes in young adulthood – or target those at risk (e.g, youth whose parent has chronic pain). As Dr. Maria Montessori stated “… in every child is the seed that will mature into an adult.”
Acknowledgments and conflict of interest
I would like to thank Caitlin Murray, PhD for offering comments on an earlier version of the manuscript. Dr. Palermo is supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number UG3HD102038. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health. There are no conflicts of interest.
References
- [1].Allen LB, Tsao JCI, Seidman LC, Ehrenreich-May J, Zeltzer LK. A Unified, Transdiagnostic Treatment for Adolescents With Chronic Pain and Comorbid Anxiety and Depression. Cogn Behav Pract 2012;19(1):56–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Bhatt RR, Gupta A, Mayer EA, Zeltzer LK. Chronic pain in children: structural and resting-state functional brain imaging within a developmental perspective. Pediatr Res 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Boersma K, Sodermark M, Hesser H, Flink IK, Gerdle B, Linton SJ. Efficacy of a transdiagnostic emotion-focused exposure treatment for chronic pain patients with comorbid anxiety and depression: a randomized controlled trial. Pain 2019;160(8):1708–1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bonnert M, Olen O, Lalouni M, Hedman-Lagerlof E, Sarnholm J, Serlachius E, Ljotsson B. Internet-Delivered Exposure-Based Cognitive-Behavioral Therapy for Adolescents With Functional Abdominal Pain or Functional Dyspepsia: A Feasibility Study. Behav Ther 2019;50(1):177–188. [DOI] [PubMed] [Google Scholar]
- [5].Brace MJ, Scott Smith M, McCauley E, Sherry DD. Family reinforcement of illness behavior: a comparison of adolescents with chronic fatigue syndrome, juvenile arthritis, and healthy controls. J Dev Behav Pediatr 2000;21(5):332–339. [DOI] [PubMed] [Google Scholar]
- [6].Capaldi DM, Kerr DCR, Tiberio SS, Owen LD. Men’s misuse of prescription opioids from early to middle adulthood: An examination of developmental and concurrent prediction models. J Consult Clin Psychol 2019;87(10):893–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Christoph MJ, Larson NI, Winkler MR, Wall MM, Neumark-Sztainer D. Longitudinal trajectories and prevalence of meeting dietary guidelines during the transition from adolescence to young adulthood. Am J Clin Nutr 2019;109(3):656–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Claar RL, Simons LE, Logan DE. Parental response to children’s pain: The moderating impact of children’s emotional distress on symptoms and disability. Pain 2008;138(1):172–179. [DOI] [PubMed] [Google Scholar]
- [9].Cousins LA, Kalapurakkel S, Cohen LL, Simons LE. Topical Review: Resilience Resources and Mechanisms in Pediatric Chronic Pain. J Pediatr Psychol 2015;40(9):840–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cservenka A, Stein H, Wilson AC, Nagel BJ. Neurobiological Phenotypes of Familial Chronic Pain in Adolescence: A Pilot fMRI Study. J Pain 2015;16(9):913–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Cunningham NR, Nelson S, Jagpal A, Moorman E, Farrell M, Pentiuk S, Kashikar-Zuck S. Development of the Aim To Decrease Anxiety and Pain Treatment (ADAPT) for pediatric functional abdominal pain disorders. J Pediatr Gastroenterol Nutr 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dampier C, Palermo TM, Darbari DS, Hassell K, Smith W, Zempsky W. AAPT Diagnostic Criteria for Chronic Sickle Cell Disease Pain. J Pain 2017;18(5):490–498. [DOI] [PubMed] [Google Scholar]
- [13].Fearon P, Hotopf M. Relation between headache in childhood and physical and psychiatric symptoms in adulthood: National birth cohort study. Br Med J 2001;322(7295):1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Feiss R, Dolinger SB, Merritt M, Reiche E, Martin K, Yanes JA, Thomas CM, Pangelinan M. A Systematic Review and Meta-Analysis of School-Based Stress, Anxiety, and Depression Prevention Programs for Adolescents. J Youth Adolesc 2019;48(9):1668–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Fisher E, Heathcote LC, Eccleston C, Simons LE, Palermo TM. Assessment of Pain Anxiety, Pain Catastrophizing, and Fear of Pain in Children and Adolescents With Chronic Pain: A Systematic Review and Meta-Analysis. J Pediatr Psychol 2018;43(3):314–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Fisher E, Law E, Dudeney J, Eccleston C, Palermo TM. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2019;4:CD011118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Fisher E, Law E, Dudeney J, Palermo TM, Stewart G, Eccleston C. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2018;9:CD003968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fryer BA, Cleary G, Wickham SL, Barr BR, Taylor-Robinson DC. Effect of socioeconomic conditions on frequent complaints of pain in children: findings from the UK Millennium Cohort Study. BMJ Paediatr Open 2017;1(1):e000093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Gray WN, Schaefer MR, Resmini-Rawlinson A, Wagoner ST. Barriers to Transition From Pediatric to Adult Care: A Systematic Review. J Pediatr Psychol 2018;43(5):488–502. [DOI] [PubMed] [Google Scholar]
- [20].Groenewald CB, Law EF, Fisher E, Beals-Erickson SE, Palermo TM. Associations Between Adolescent Chronic Pain and Prescription Opioid Misuse in Adulthood. J Pain 2019;20(1):28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Groenewald CB, Wright DR, Palermo TM. Health care expenditures associated with pediatric pain-related conditions in the United States. Pain 2015;156(5):951–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Higgins KS, Birnie KA, Chambers CT, Wilson AC, Caes L, Clark AJ, Lynch M, Stinson J, Campbell-Yeo M. Offspring of parents with chronic pain: a systematic review and meta-analysis of pain, health, psychological, and family outcomes. Pain 2015;156(11):2256–2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Holley AL, Wilson AC, Noel M, Palermo TM. Post-traumatic stress symptoms in children and adolescents with chronic pain: A topical review of the literature and a proposed framework for future research. Eur J Pain 2016;20(9):1371–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Incledon E, O’Connor M, Giallo R, Chalkiadis GA, Palermo TM. Child and Family Antecedents of Pain During the Transition to Adolescence: A Longitudinal Population-Based Study. J Pain 2016;17(11):1174–1182. [DOI] [PubMed] [Google Scholar]
- [25].Jastrowski Mano KE, O’Bryan EM, Gibler RC, Beckmann E. The Co-occurrence of Pediatric Chronic Pain and Anxiety: A Theoretical Review of a Developmentally Informed Shared Vulnerability Model. Clin J Pain 2019;35(12):989–1002. [DOI] [PubMed] [Google Scholar]
- [26].Jones GT, Silman AJ, Macfarlane GJ. Predicting the onset of widespread body pain among children. Arthritis Rheum 2003;48(9):2615–2621. [DOI] [PubMed] [Google Scholar]
- [27].Kashikar-Zuck S, Cunningham N, Peugh J, Black WR, Nelson S, Lynch-Jordan AM, Pfeiffer M, Tran ST, Ting TV, Arnold LM, Carle A, Noll J, Powers SW, Lovell DJ. Long-term outcomes of adolescents with juvenile-onset fibromyalgia into adulthood and impact of depressive symptoms on functioning over time. Pain 2019;160(2):433–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 2011;152(12):2729–2738. [DOI] [PubMed] [Google Scholar]
- [29].Larsson B, Sigurdson JF, Sund AM. Long-term follow-up of a community sample of adolescents with frequent headaches. J Headache Pain 2018;19(1):79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Law E, Fisher E, Eccleston C, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev 2019;3:Cd009660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Law EF, Tham SW, Aaron RV, Dudeney J, Palermo TM. Hybrid cognitive-behavioral therapy intervention for adolescents with co-occurring migraine and insomnia: A single-arm pilot trial. Headache 2018;58(7):1060–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Liossi C, Howard RF. Pediatric Chronic Pain: Biopsychosocial Assessment and Formulation. Pediatrics 2016;138(5). [DOI] [PubMed] [Google Scholar]
- [33].Logan DE, Scharff L. Relationships between family and parent characteristics and functional abilities in children with recurrent pain syndromes: an investigation of moderating effects on the pathway from pain to disability. J Pediatr Psychol 2005;30(8):698–707. [DOI] [PubMed] [Google Scholar]
- [34].Logan DE, Simons LE. Development of a group intervention to improve school functioning in adolescents with chronic pain and depressive symptoms: a study of feasibility and preliminary efficacy. J Pediatr Psychol 2010;35(8):823–836. [DOI] [PubMed] [Google Scholar]
- [35].Long AC, Krishnamurthy V, Palermo TM. Sleep disturbances in school-age children with chronic pain. J Pediatr Psychol 2008;33(3):258–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Makover H, Adrian M, Wilks C, Read K, Stoep AV, McCauley E. Indicated Prevention for Depression at the Transition to High School: Outcomes for Depression and Anxiety. Prev Sci 2019;20(4):499–509. [DOI] [PubMed] [Google Scholar]
- [37].Malhi GS, Das P, Bell E, Mattingly G, Mannie Z. Modelling resilience in adolescence and adversity: a novel framework to inform research and practice. Transl Psychiatry 2019;9(1):316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Moore SV, Davis MC, Lemery-Chalfant K. Children’s physical pain: relations with maternal and paternal pain and prediction from maternal depressive symptoms and hope during infancy. Psychol Health Med 2019:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Murray CB, Groenewald CB, de la Vega R, Palermo TM. Long-term impact of adolescent chronic pain on young adult educational, vocational, and social outcomes. Pain 2020;161(2):439–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Muthuri SG, Kuh D, Cooper R. Longitudinal profiles of back pain across adulthood and their relationship with childhood factors: evidence from the 1946 British birth cohort. Pain 2018;159(4):764–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Nelson S, Simons LE, Logan D. The Incidence of Adverse Childhood Experiences (ACEs) and Their Association With Pain-related and Psychosocial Impairment in Youth With Chronic Pain. Clin J Pain 2018;34(5):402–408. [DOI] [PubMed] [Google Scholar]
- [42].Noel M, Groenewald CB, Beals-Erickson SE, Gebert JT, Palermo TM. Chronic pain in adolescence and internalizing mental health disorders: a nationally representative study. Pain 2016;157(6):1333–1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Palermo TM. Impact of recurrent and chronic pain on child and family daily functioning: a critical review of the literature. J Dev Behav Pediatr 2000;21(1):58–69. [DOI] [PubMed] [Google Scholar]
- [44].Palermo TM. Sleep quality and efficiency in adolescents with chronic pain: relationship with activity limitations and health-related quality of life. J Pediatr Psychol 2008;6(4):234–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Palermo TM. Cognitive-behavioral therapy for chronic pain in children and adolescents. New York, NY: Oxford University Press, 2012. [Google Scholar]
- [46].Palermo TM, Beals-Erickson S, Bromberg M, Law E, Chen M. A Single Arm Pilot Trial of Brief Cognitive Behavioral Therapy for Insomnia in Adolescents with Physical and Psychiatric Comorbidities. J Clin Sleep Med 2017;13(3):401–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Palermo TM, Chambers CT. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain 2005;119(1–3):1–4. [DOI] [PubMed] [Google Scholar]
- [48].Palermo TM, Eccleston C. Parents of children and adolescents with chronic pain. Pain 2009;146(1–2):15–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Palermo TM, Law E, Churchill SS, Walker A. Longitudinal course and impact of insomnia symptoms in adolescents with and without chronic pain. Journal of Pain 2012;13(11):1099–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Palermo TM, Law EF, Bromberg M, Fales J, Eccleston C, Wilson AC. Problem-solving skills training for parents of children with chronic pain: a pilot randomized controlled trial. Pain 2016;157(6):1213–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Palermo TM, Law EF, Fales J, Bromberg MH, Jessen-Fiddick T, Tai G. Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: a randomized controlled multicenter trial. Pain 2016;157(1):174–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Palermo TM, Valrie CR, Karlson CW. Family and parent influences on pediatric chronic pain: a developmental perspective. Am Psychol 2014;69(2):142–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Palermo TM, Wilson AC, Lewandowski AS, Toliver-Sokol M, Murray CB. Behavioral and psychosocial factors associated with insomnia in adolescents with chronic pain. Pain 2011;152(1):89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Peterson CC, Palermo TM. Parental reinforcement of recurrent pain: The moderating impact of child depression and anxiety on functional disability. Journal of Pediatric Psychology 2004;29(5):331–341. [DOI] [PubMed] [Google Scholar]
- [55].Quinn PD, Rickert ME, Franck J, Sariaslan A, Boersma K, Lichtenstein P, Larsson H, D’Onofrio BM. Associations of mental health and family background with opioid analgesic therapy: a nationwide Swedish register-based study. Pain 2019;160(11):2464–2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Rosenbloom BN, Rabbitts JA, Palermo TM. A developmental perspective on the impact of chronic pain in late adolescence and early adulthood: implications for assessment and intervention. Pain 2017;158(9):1629–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Rovio SP, Yang X, Kankaanpaa A, Aalto V, Hirvensalo M, Telama R, Pahkala K, Hutri-Kahonen N, Viikari JSA, Raitakari OT, Tammelin TH. Longitudinal physical activity trajectories from childhood to adulthood and their determinants: The Young Finns Study. Scand J Med Sci Sports 2018;28(3):1073–1083. [DOI] [PubMed] [Google Scholar]
- [58].Santos M, Murtaugh T, Pantaleao A, Zempsky WT, Guite JW. Chronic Pain and Obesity Within a Pediatric Interdisciplinary Pain Clinic Setting: A Preliminary Examination of Current Relationships and Future Directions. Clin J Pain 2017;33(8):738–745. [DOI] [PubMed] [Google Scholar]
- [59].Simons LE, Claar RL, Logan DL. Chronic pain in adolescence: Parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. Journal of Pediatric Psychology 2008;33(8):894–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Simons LE, Pielech M, Erpelding N, Linnman C, Moulton E, Sava S, Lebel A, Serrano P, Sethna N, Berde C, Becerra L, Borsook D. The responsive amygdala: treatment-induced alterations in functional connectivity in pediatric complex regional pain syndrome. Pain 2014;155(9):1727–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Simons LE, Sieberg CB, Conroy C, Randall ET, Shulman J, Borsook D, Berde C, Sethna NF, Logan DE. Children With Chronic Pain: Response Trajectories After Intensive Pain Rehabilitation Treatment. J Pain 2018;19(2):207–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Simons LE, Vlaeyen JWS, Declercq L, A MS, Beebe J, Hogan M, Li E, C AK, Mahmud F, J RC, C BS, Ploski C. Avoid or engage? Outcomes of graded exposure in youth with chronic pain using a sequential replicated single-case randomized design. Pain 2020;161(3):520–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Soltani S, Kopala-Sibley DC, Noel M. The Co-occurrence of Pediatric Chronic Pain and Depression: A Narrative Review and Conceptualization of Mutual Maintenance. Clin J Pain 2019;35(7):633–643. [DOI] [PubMed] [Google Scholar]
- [64].Stapersma L, van den Brink G, van der Ende J, Szigethy EM, Groeneweg M, de Bruijne FH, Hillegers MHJ, Escher JC, Utens E. Psychological Outcomes of a Cognitive Behavioral Therapy for Youth with Inflammatory Bowel Disease: Results of the HAPPY-IBD Randomized Controlled Trial at 6- and 12-Month Follow-Up. J Clin Psychol Med Settings 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Stein K, Pearson RM, Stein A, Fazel M. The predictive value of childhood recurrent abdominal pain for adult emotional disorders, and the influence of negative cognitive style. Findings from a cohort study. PLoS One 2017;12(9):e0185643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Stephenson M, Barr P, Ksinan A, Aliev F, Latvala A, Viken R, Rose R, Kaprio J, Dick D, Salvatore JE. Which adolescent factors predict alcohol misuse in young adulthood? A co-twin comparisons study. Addiction 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Stone AL, Wilson AC. Transmission of risk from parents with chronic pain to offspring: an integrative conceptual model. Pain 2016;157(12):2628–2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Stormshak EA, DeGarmo DS, Chronister KM, Caruthers AS, Stapleton J, Falkenstein CA. The impact of substance use during middle school and young adulthood on parent-young adult relationships. J Fam Psychol 2019;33(7):797–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Tang NK, Wright KJ, Salkovskis PM. Prevalence and correlates of clinical insomnia co-occurring with chronic back pain. J Sleep Res 2007;16(1):85–95. [DOI] [PubMed] [Google Scholar]
- [70].Tollisen A, Selvaag AM, Aasland A, Lerdal A, Flato B. Longitudinal Health Status from Early Disease to Adulthood and Associated Prognostic Factors in Juvenile Idiopathic Arthritis. J Rheumatol 2019;46(10):1335–1344. [DOI] [PubMed] [Google Scholar]
- [71].Walco GA, Krane EJ, Schmader KE, Weiner DK. Applying a Lifespan Developmental Perspective to Chronic Pain: Pediatrics to Geriatrics. J Pain 2016;17(9 Suppl):T108–117. [DOI] [PubMed] [Google Scholar]
- [72].Walker LS, Dengler-Crish CM, Rippel S, Bruehl S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain 2010;150(3):568–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Walker LS, Sherman AL, Bruehl S, Garber J, Smith CA. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain 2012;153(9):1798–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Walker LS, Zeman JL. Parental response to child illness behavior. Journal of Pediatric Psychology 1992;17:49–71. [DOI] [PubMed] [Google Scholar]
- [75].Wilson AC, Palermo TM. Physical activity and function in adolescents with chronic pain: a controlled study using actigraphy. J Pain 2012;13(2):121–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Wright C, Steinway C, Jan S. The genesis of systems of care for transition to adulthood services: emerging models in primary and subspecialty care. Curr Opin Pediatr 2018;30(2):303–310. [DOI] [PubMed] [Google Scholar]
- [77].Zhang C, Brook JS, Leukefeld CG, De La Rosa M, Brook DW. Lack of Preventive Health Behaviors in the Early Forties: The Role of Earlier Trajectories of Cigarette Smoking From Adolescence to Adulthood. Subst Use Misuse 2017;52(12):1527–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]


