Abstract
Objective
During COVID-19, government measures to prevent disease spread included advice to work from home. In addition to occupational risk factors, the increased use of telecommunication and changed work environment may contribute to voice and vocal tract discomfort (VTD). This study established the prevalence, incidence, characteristics and impact of self-perceived dysphonia and VTD in those working from home during COVID-19.
Methods
A cross-sectional, observational study using an online survey recruited 1575 participants. It captured information about dysphonia and VTD presence, onset, and severity. Those with dysphonia completed the voice-related quality of life to measure impact. Regression analyses identified risk factors for voice and vocal tract problems.
Results
Dysphonia and VTD prevalence rates were 33% and 68%, respectively, incidences were 28% and 50%. Perceived dysphonia severity was mild in 72% of cases. Dry throat was the most common VTD symptom at 66%. Mean voice-related quality of life score was 82.4 (standard deviation ± 13.2). Raising or straining the voice while working predicted new onset dysphonia and VTD. Increasing telecommunication use was associated with worse dysphonia and VTD onset.
Conclusion
Those working from home have seen a rise in dysphonia and VTD, which were associated with communication modality and change in environment. If home offices become the ‘new normal’ post-COVID, workplaces should consider voice training for employees to limit potential difficulties.
Key words: Vocal hygiene—Telecommunications—Workplace—Occupational Voice—Epidemiology
INTRODUCTION
The global COVID-19 pandemic caused many countries to adopt measures to “flatten the curve”, primarily through the introduction of social or physical distancing. In the Republic of Ireland, significant movement restrictions (informally called lockdown) were implemented on March 27, 2020. These restrictions included a ban on travelling to work, unless that work was an essential service. This requirement saw many individuals forced to work from home. Change of workplace venue necessitated hasty construction of home office spaces. It also saw increased use of telecommunication, with many individuals adopting video calling technologies.
It is well-established that certain occupational groups are at increased risk of dysphonia due to the demands of their job. Studies have identified potential contributory factors including environmental noise, exposure to laryngeal irritants, length of working day, type of communication devices used and vocal loading.1, 2, 3 These risk factors are in addition to nonoccupational modifiers such as age, gender and response to stress.4, 5, 6, 7 Attention to adequate air quality, ergonomics, hydration and posture are also considered important.8, 9, 10, 11 When an individual experiences dysphonia, they may also develop symptoms of vocal tract discomfort (VTD).12 , 13
Self-perceived voice difficulties adversely affect quality of life.14, 15, 16 They also affect individuals’ occupational performance and prospects. Voice difficulties are associated with absence from work, considering career change, inability to complete occupational requirements and limiting interactions with colleagues.14 , 17 , 18 Voice disorders are a significant healthcare cost,6 , 19 and delayed assessment and management leads to rising cost.20
The widespread introduction of home working during the global pandemic may have led to much of the workforce being placed at higher risk of developing occupational voice problems and associated VTD. The change to increased online and telephone communication may cause increased vocal load. It seems unlikely that many home workspaces were designed with vocal health in mind. This study hypothesized a high number of self-perceived voice and vocal tract difficulties in the general population during lockdown. It therefore aimed to identify the prevalence, incidence, characteristics and impact of self-perceived voice difficulties and VTD during lockdown in Ireland.
MATERIALS AND METHODS
Ethics and consent
Ethical approval was obtained from the author's institution. Data processing procedures were reviewed and approved by an Information Compliance officer. Participants were informed at the survey outset that response submission implied consent. Partially-completed responses were considered withdrawals and were not included in analysis. Responses were fully anonymous, containing no identifiable information.
On survey completion, all participants received vocal hygiene information via a hyperlinked document authored by the researcher. This document advised participants to contact their general practitioner if they had an abnormal voice quality lasting longer than two weeks, and described the roles of the laryngologist and speech and language therapist. It also recommended that participants try a headset with microphone to see whether this reduces vocal strain. Participants were encouraged to ensure sufficient systemic hydration, use steam inhalation for surface hydration and ensure adequate posture while voicing. They were educated about the relationship between reflux and voice and to seek medical advice if symptomatic for reflux. They were also encouraged to examine their daily routine to avoid episodes of vocal loading. Finally, they were given a link to a YouTube video demonstrating the yawn/sigh technique to ameliorate vocal strain.
Instrument design
An online survey was generated using Qualtrics (SAP, Walldorf) to address the study aims. The survey required responses from each question to avoid missing data. It obtained information about gender, occupation and age. Participants were asked about changes to communication style during lockdown, including amount of telephone and video calling use. Questions used bold font to contrast time points of interest, for example, How often do you use video calling (like Skype or Zoom) as part of your job since the lockdown? Responses were obtained about ergonomic, environmental and personal factors in their home working environment. Ergonomics included use of accessories like headsets, as well as seated/standing posture and computer monitor placement. Air quality was an environmental factor. Personal factors were self-reported water intake and stress (Do you feel that working from home has made your job more stressful overall?). Each of these were independent variables.
Dependent variables included a set of measures related to presence, characteristics, onset, and impact of voice and vocal tract difficulties. Participants were asked to describe their voice quality using a system based on GRBAS,21 but which also included an option for hoarse and the option to self-describe voice features. Vocal tract discomfort symptoms were based on the Vocal Tract Discomfort Scale,22 but with the option to self-describe additional symptoms. Impact was measured using the voice-related quality of life (V-RQOL).23 This 10-item questionnaire is scored out of 100, with higher scores indicating lower impact of dysphonia on quality of life. In order to reduce participant burden, those without self-reported voice difficulties were not required to complete the V-RQOL and were assumed to be within the normal range. Participants were asked to describe voice quality and vocal tract discomfort during telephone and video calling activities, for example, When you use the telephone or video calling (like Skype or Zoom) while working from home, do you feel like you raise or strain your voice?
Validity was established by two means. First, the questions were designed to be clear, precise, well-presented and with no errors in display logic, in accordance with recommended practices.24 Second, a pilot phase was conducted. Volunteers were sought by advertisement on social media. Five volunteers responded, who varied in their gender, occupations and ages. Piloting revealed slight difficulties with occupation selection, but these could not be addressed. Occupations were taken from an existing European Union database25 and could not be modified.
V-RQOL procedures were modified slightly based on pilot feedback. Prior to seeing the V-RQOL, participants were reminded that the questions related to impact of voice on daily life, because of concerns that problem statements in the V-RQOL could be due to nonvoice factors. Each V-RQOL question was changed to start with “How much of a problem is this for you now?”, followed by the problem statement. For example, the first item was How much of a problem is this for you now?: "Because of my voice, I have trouble speaking loudly or being heard in noisy situations." This was to anchor the responses to the lockdown period, rather than allow participants to respond based on a different time frame. A full version of the finalized survey with question numbers is in the supplemental file attached to this text.
Sampling
By sample size calculation, 385 individuals were required to obtain an accurate prevalence, but the survey remained open and recruited a number in excess of this to facilitate statistical analysis. Greater participant numbers allowed more precise estimates of effect sizes and permitted investigation into the effects of multiple independent variables simultaneously.
The population of interest was those who were working from home during lockdown. The survey was disseminated via social media accounts owned by the author's institution. The study was also publicized in the national media and via a paid social media advertising campaign. A snowball sampling strategy was used, where participants were encouraged to share the survey with other interested parties. The sampling methodology was intended to obtain a diverse sample, in order to better represent the population.
The survey was opened on May 1, 2020 and closed on June 19, 2020. Participants had therefore been working from home for a one month period before the study opened. The survey closure date was timed to coincide with reduction in movement restrictions, whereby some workers were permitted to return to their workplace.
Inclusion/exclusion criteria
Adults (≥18) from the Republic of Ireland who were working from home during lockdown were recruited. Those outside of the Republic of Ireland were excluded in order to make the sample more homogeneous, since other countries implemented lockdowns at different time points and using different criteria. Those who were studying (rather than working) from home were excluded, since the focus was on paid occupations. Individuals who were aphonic prior to lockdown were also excluded, since it would be impossible to identify any new onset or exacerbation of voice difficulties. The survey introduction excluded aphonic individuals by asking those who were “unable to produce any voice since before the lockdown anyway” not to participate. Those with pre-existing dysphonia were not excluded, because exacerbation of their voice difficulties was of interest to this study.
Statistical analysis
Minitab 17 (Minitab LLC, Pennsylvania) was used for descriptive and inferential statistics. All test assumptions were met. Binary and ordinal logistic regression were used for inferential statistics and significance was α ≤ 0.05. Significant associations were initially identified by univariate analysis, then combined into a multivariate model. A parsimonious model was created by removing least nonsignificant predictors iteratively.
Derived variables
Some variables were derived by applying a function to survey responses. Participants were asked Do you think you have a problem with how your voice sounds on a day-to-day basis right now? and later asked Did you have a problem with the sound of your voice on a day-to-day basis before the lockdown? Those with current, but no previous dysphonia were considered to have a new onset dysphonia, which was also used for incidence calculation. Question 12 asked participants Which of the following physical sensations do you experience in your throat while working from home on a day-to-day basis? Select all that apply. Any participant who selected at least one symptom was considered to have VTD. Those who answered negatively to Did you have these physical sensations in your throat before the lockdown? were considered to have new onset VTD, which was also used to calculate incidence.
Change in the amount of telephone and video calling use before and after lockdown were derived mathematically. For example, participants were asked How often did you use the telephone as part of your job before the lockdown? then asked an identical question about since lockdown. Likert-type frequency responses were provided from never to very frequently. These were treated numerically as ordinal responses. Increasing or decreasing frequency was therefore calculated by examining the difference between pre- and postlockdown.
Survey question 38 was concerned with ambient air quality and asked participants Would you say that any of the following describe how your home working environment usually is? Select all that apply. Responses included adverse conditions such as dry air, dusty, and damp or moldy. Any adverse condition was taken to indicate poor quality, while no problems were taken to indicate good quality.
RESULTS
Participant characteristics
2258 responses were collected, with 683 excluded from analysis due to partial completion. The final dataset was therefore n=1575. Participant age was non-normally distributed. Median age was 46 years (the interquartile range [IQR] 17), range was 18-78. Gender distribution was 222 (14%) male, 1353 (86%) female, while none selected other. Participants’ occupational sectors are in Table 1 .
TABLE 1.
Participant Occupation by Sector
| Sector | n | % |
|---|---|---|
| Education, research, training | 489 | 31 |
| Finance, banking, insurance | 154 | 10 |
| Health care, paramedics, laboratory | 137 | 9 |
| Legal, administration, inspection, policy adviser | 134 | 9 |
| IT, automation, telecommunication | 119 | 8 |
| Management, direction | 89 | 7 |
| Care, children, welfare, social work | 85 | 5 |
| Clerks, secretaries, post, telephone | 64 | 4 |
| Media, graphic, printing, culture, design | 56 | 4 |
| Marketing, PR, advertising | 32 | 2 |
| Hospitality, tourism, leisure, sports | 30 | 2 |
| Commercial, shop, buy and sale | 27 | 2 |
| HRM, labor intermediary, organization | 27 | 2 |
| Language, library, archive, museum | 25 | 2 |
| Industrial promotion, manufacture, metal | 19 | 1 |
| Agriculture, nature, animals, environment | 17 | 1 |
| Other sectors & no response | 71 | 5 |
Sectors representing <1% grouped together.
Prevalence and incidence
Self-reported dysphonia prevalence was 516 of 1575 (33%) and incidence was 441 of 1575 (28%). Within the dysphonic group, incidence was 441 of 516 (85%). Of those with new onset dysphonia, 14 of 441 (3%) had received a diagnosis from a healthcare professional. Sixty-six of 1575 participants (4%) had dysphonia prior to lockdown, which resolved by the time of survey completion. Of those in whom dysphonia resolved, 43 of 66 (65%) were educators. Participants were asked if they had symptoms of VTD at the time of survey completion. Prevalence was 1076 of 1575 (68%), incidence was 785 of 1575 (50%) within the whole study cohort. Within the subgroup of those with VTD, incidence was 785 of 1076 (73%).
Characteristics and impact
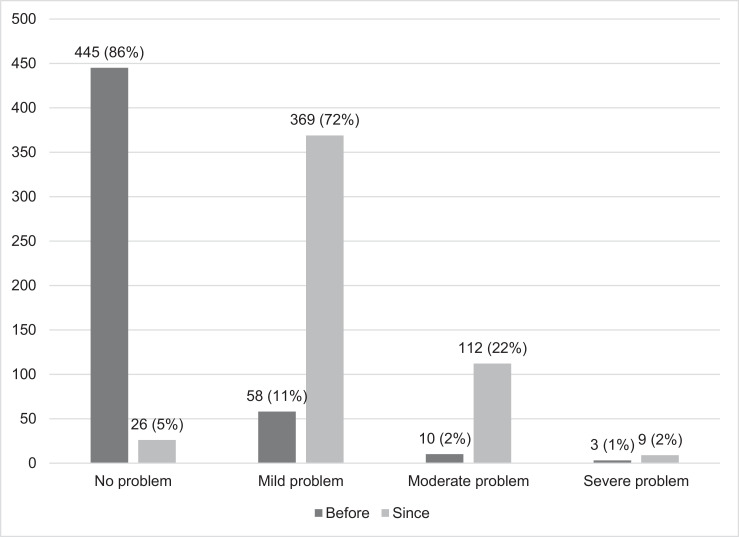
Those with dysphonia at the time of survey completion (n = 516) were asked to rate the severity of their voice problem before and since lockdown (Figure 1 ). The results indicate worsening voice quality since lockdown. These participants were also asked to describe their voice quality (Table 2 ) and VTD symptoms (Table 3 ) using survey options and self-report. Median number of VTD symptoms was 2 (IQR 2, range 1-7).
FIGURE 1.
Self-perceived dysphonia severity before and since lockdown in n=516 participants with dysphonia at the time of survey completion.
TABLE 2.
Self-Reported Voice Quality Problems in n = 516 Participants With Dysphonia at the Time of Survey Completion
| Voice Quality Problem | n | % |
|---|---|---|
| Hoarse | 265 | 51% |
| Strained | 208 | 40% |
| Rough/gravelly | 177 | 34% |
| Weak (esthetic) | 148 | 29% |
| Breathy | 70 | 14% |
| Pitch problems | 16 | 3% |
| No voice quality problems | 6 | 1% |
| Synonym of dysphonia | 6 | 1% |
| Aphonia | 4 | 1% |
| Too loud | 2 | <1% |
| Fatigue | 2 | <1% |
TABLE 3.
Self-Reported VTD Symptoms in n=785 Participants With New Onset VTD at the Time of Survey Completion
| VTD Symptom | n | % |
|---|---|---|
| Dry | 519 | 66% |
| Irritable (a nonspecific, annoying feeling) | 296 | 38% |
| Tickling | 210 | 27% |
| Tight | 176 | 22% |
| Sore | 140 | 18% |
| Lump in the throat | 135 | 17% |
| Aching | 58 | 7% |
| Burning | 37 | 5% |
| Need to throat clear | 15 | 2% |
| Weak/tired | 12 | 2% |
| Mucous/phlegm in throat | 7 | 1% |
| Strained | 4 | 1% |
| Itchy | 2 | <1% |
| Swollen | 2 | <1% |
| Stretched | 1 | <1% |
Participants with dysphonia since lockdown completed the V-RQOL. Mean score was 82.4 (SD ±13.2), median was 85 (IQR 15), range was 27.5-100. According to the tool's authors,23 mean score for dysphonic individuals is 53.5 (SD 22.0) and for nondysphonic individuals is 98.0 (SD ± 3.9). Within the survey, 419/516 (81%) of those with voice difficulties at the time of survey completion fell below the V-RQOL's lower boundary for nondysphonic individuals (ie, below the normal range), while 127/516 (25%) fell below the upper boundary for dysphonic individuals (ie, within the dysphonic range).
New onset dysphonia
Binary regression determined which independent variables predicted new onset dysphonia (Table 4 ). Those who already had these problems before lockdown could not have developed a new onset, and so were excluded from analyses. Older, stressed males who frequently strain or raise their voices and work in an environment with poor air quality were most at risk. It was noted that increasing telephone use (p= 0.056) and increasing water intake (p = 0.061) closely approached significance as predictors of new onset dysphonia.
TABLE 4.
Univariate and Multivariate Predictors of New Onset Dysphonia
| Predictor | Uni p-value | Uni OR (95% CI) | Multi p- Value | Multi OR (95% CI) | Level |
|---|---|---|---|---|---|
| Gender (Q2) | 0.019 | 1.45 (1.07-1.97) | 0.002 | 1.72 (1.22-2.43) | Male |
| Age (Q4) | 0.002 | 1.02 (1.01-1.03) | 0.002 | 1.02 (1.01-1.03) | Older |
| Frequently raising/straining voice (Q32) | <0.001 | 1.58 (1.43-1.74) | <0.001 | 1.54 (1.4-1.71) | Higher frequency |
| Air quality (Q38) | <0.001 | 1.71 (1.36-2.14) | 0.002 | 1.48 (1.15-1.91) | Poor quality |
| Stress (Q40) | <0.001 | 1.92 (1.53-2.41) | <0.001 | 1.59 (1.24-2.05) | Stressed |
Self-rated dysphonia severity
Participants were asked How would you rate the severity of your voice problem right now? using none/mild/moderate/severe responses. Ordinal regression identified predictors for worse voice quality (Table 5 ). Poor posture while working from home and computer monitor placement were significant on univariate analysis, but not multivariate analysis. Those who did not use a computer monitor for work were significantly more likely to have worse voice quality than those who used a monitor, but had it positioned sub-optimally. On multivariate analysis, frequently raising or straining the voice and using video calling less often than before lockdown were associated with worse voice quality.
TABLE 5.
Univariate and Multivariate Predictors of Worse Self-Perceived Voice Quality
| Predictor | Uni p-value | Uni OR (95% CI) | Multi p-value | Multi OR (95% CI) | Level |
|---|---|---|---|---|---|
| Change in video call use (Q28, Q29) | 0.001 | 1.23 (1.09-1.4) | <0.001 | 1.3 (1.13-1.5) | Less use |
| Frequently raising/straining voice (Q32) | 0.023 | 0.79 (0.64-0.97) | 0.008 | 0.75 (0.61-0.93) | Higher frequency |
| Posture (Q36) | 0.011 | 0.57 (0.37-0.88) | - | - | Poor posture |
| Computer monitor placement (Q37) | 0.013 | 1.85 (0.87-3.93) | - | - | No monitor use vs poor placement |
New onset VTD
Binary regression identified factors predictive of new onset VTD (Table 6 ). Occupation significantly predicted new onset VTD. By proportion, the top most affected sectors were (1) Hospitality, tourism, leisure, sports (83%); (2) care, children, welfare, social work (78%); (3) clerks, secretaries, post, telephone (73%). Within at-risk sectors, those who experienced an increase in telephone and video call use, frequently raised or strained their voices, had a poor ambient air quality and felt stressed by working from home were most likely to develop VTD.
TABLE 6.
Univariate and Multivariate Predictors of New Onset VTD
| Predictor | Uni p-value | Uni OR (95% CI) | Multi p-Value | Multi OR (95% CI) | Level |
|---|---|---|---|---|---|
| Occupationa (Q3) | 0.014 | Various | 0.002 | Various | Various |
| Change in telephone use (Q26, Q27) | <0.001 | 1.15 (1.07-1.24) | 0.005 | 1.15 (1.04-1.26) | Higher use |
| Change in video call use (Q28, Q29) | <0.001 | 1.16 (1.09-1.24) | 0.018 | 1.12 (1.02-1.23) | Higher use |
| Frequently raising/straining voice (Q32) | <0.001 | 2.01 (1.82-2.23) | <0.001 | 1.97 (1.76-2.19) | Higher frequency |
| Air quality (Q38) | <0.001 | 2.36 (1.87-3.0) | <0.001 | 2.01 (1.52-2.67) | Poor quality |
| Stress (Q40) | <0.001 | 2.3 (1.82-2.89) | <0.001 | 1.96 (1.48-2.6) | Stressed |
Odds ratios compare each sector vs each other sector. Proportions are provided in the text above for brevity.
V-RQOL
Predictors of worse V-RQOL scores were examined within those who had new onset dysphonia (Table 7 ). In both univariate and multivariate ordinal regression, those who frequently raised or strained their voice during calls, who did not use a computer monitor (as compared to those who used a properly-placed monitor) and those who drank more water were most likely to have worse scores on this tool.
TABLE 7.
Univariate and Multivariate Predictors of Worse V-RQOL Scores
| Predictor | Uni p-Value | Uni OR (95% CI) | Multi p-value | Multi OR (95% CI) | Level |
|---|---|---|---|---|---|
| Frequently raising/straining voice (Q32) | <0.001 | 1.38 (1.18-1.6) | <0.001 | 1.36 (1.17-1.59) | Higher frequency |
| Computer monitor placement (Q37) | 0.006 | 2.42 (1.29-4.57) | 0.009 | 2.63 (1.28-5.56) | No monitor use vs good placement |
| Water intake (Q39) | 0.002 | 1.28 (1.1-1.51) | 0.033 | 1.2 (1.01-1.41) | Increasing intake |
DISCUSSION
The dysphonia prevalence rate of 33% in this research is higher than reported rates of 1.7%-7.6% in the United States4 , 6 , 26 and 16.9% in Sweden,7 but lower than the 38.5% rate reported in Greece.27 Some difference in prevalence rates may be expected due to differing diagnostic criteria between studies, and some perhaps due to linguistic or cultural differences, but the prevalence here was nevertheless high. More telling was the incidence rate, which showed that 85% of those with self-reported dysphonia developed their voice problems since the lockdown began. Observational studies such as this are not well-equipped to examine causation, but this high incidence associated with the lockdown period seems unusual and may infer a link.
The 68% prevalence rate of VTD in this study was in fact lower than that of a study that examined VTD in a Flemish population.28 That study found an 88% VTD prevalence in those without self-reported voice problems, despite using the same diagnostic criterion; at least one symptom on the Vocal Tract Discomfort Scale. The authors of that study reported a median of three VTD symptoms, higher than the two symptoms reported here. A Brazilian study found an average of two VTDS symptoms in those without self-reported voice problems and four in those with self-reported difficulties.13 This could indicate that the VTD prevalence in this study is perhaps within expectations, but the incidence rate once again speaks to a strong association with the lockdown period. It would be useful in the future to have well-established prevalence rates for healthy populations for comparison.
Self-reported dysphonia was considered mild in almost three-quarters of cases and while it did have an impact on daily life according to V-RQOL scores, the median score indicates that the impact was low. This is potentially reassuring, since only 3% of participants who reported voice problems had gotten a formal diagnosis. If participants’ difficulties were mild, they could perhaps be managed with an effective vocal hygiene program. Voice programs have been demonstrated to be effective for dysphonia management in call center employees,29 , 30 who are similar to this study's cohort in that they rely on telecommunication. Early intervention for voice problems may also be cost-saving for healthcare services.20 Occupational voice problems are recognized as an ongoing problem, especially for at-risk groups, with poor supports in workplaces.31 Whether employers have a legal requirement to ensure the vocal welfare of those working from home is a matter for each jurisdiction, but this may become an increasing concern in a post-COVID era if working from home becomes commonplace and could potentially lead to litigation.
This study showed that older age and male gender were associated with new onset dysphonia. While older age is a recognized risk factor, voice problems are typically more common in females.4 , 7 , 32 Occupation was not associated with voice problems in this study, but was associated with VTD. Comparison with other studies is difficult, since different studies use different occupational classification systems, a well-described problem in the literature.33 Nevertheless, the top three most affected sectors here were ones that typically involve significant voice use, so the results were not surprising. More unexpectedly, 4% of participants saw a dysphonia resolve during the lockdown period and most of these were educators. The timing of the study was such that the academic year was drawing to a close, so responses may simply be reflective of more vocal rest, but they may equally show that for some, a change from vocal projection in the classroom to telecommunication might be beneficial.
This study was predicated upon the fact that difficulties may be encountered while working from home, rather than in a regular workplace environment. It was therefore notable that increasing telephone and video use compared to the prelockdown period was also associated with new onset VTD. An unusual finding was that those who used video calling seldomly were more likely to have worse dysphonia than those who use video calling frequently. The reason for this is unknown and bears further examination. It could be the case for example that those who do not rely on video calling instead use the telephone and that this is more vocally harmful. Information about participants’ use of tools like hands-free kits, free-standing microphones and headsets were collected as part of this study. An analysis of their influence on voice and vocal tract (dis)comfort would be lengthy and so will be reported in a separate study.
Less surprisingly, those who noted themselves to raise or strain their voices during telephone or video calls were most likely to develop new dysphonia and VTD, have worse dysphonia, and have a greater impact of that dysphonia upon their lives. Such behaviors could indicate the onset of a muscle tension dysphonia pattern. They may also be an avenue for voice intervention. Vocal hygiene programs for those using telecommunication should start with building awareness of maladaptive speaking patterns before correcting those behaviors, akin to how traditional voice therapy works.
Questions about posture and computer monitor placement were included to examine whether body position had an effect on voice production. A recent systematic review concluded that “An effective posture allows a subject in a static posture or while moving to more easily shift the tension between muscles, allowing for a free movement of the larynx without blockages and with benefits to voice production.”11 It was considered here that hastily constructed home office spaces may involve inadequate seating, desks, computer monitor placement and perhaps even laptop use. These could cause protracted periods of compression or tension of the muscles of breathing or voice. While posture and computer monitor placement did contribute to worse voice quality in univariate analysis, they were not significant when combined with other factors in multivariate analysis. An unexpected finding was that those who do not use a monitor for their job were more likely to have worse dysphonia and worse V-RQOL scores than those that do. The reason for this was not captured, but it is possible that those who do not use a computer monitor are involved in vocally demanding jobs, or that they use the telephone more.
This study asked participants whether they felt that working from home has made their job more stressful. Stress in this context was associated with new onset dysphonia and VTD. Given that distress and perceived control are associated with voice problems,5 this was not without precedent. Air quality played a role in predicting dysphonia and VTD, with poor quality increasing likelihood of having either problem. It would be interesting to observe in the future whether perceived problems with air quality are related to the dry symptom on the VTDS. These factors may explain why increasing water intake was associated with voice and vocal tract problems; it seems likely that those who experienced such difficulties were hydrating more in an attempt to remedy them.
Strengths and limitations
This was the first study to examine the impact of home working on voice and vocal tract discomfort. It utilized existing tools and scales with minimal modification to improve robustness. This study benefited from the participation of a large number of individuals, which aids generalizability of findings. A broad range of participant ages and occupations also makes results applicable to a wider demographic, but it was noted that most respondents were female and none were transgender, nonbinary or gender nonconforming.
The difficulties encountered by participants in this study were assumed to be predominantly occupational in nature, but other potentially relevant factors (eg, social voice use, medical history, and smoking status) were not captured and therefore not controlled. Another potential limitation is that research participants were self-selecting. While the research was advertised to the general public to recruit a representative sample, it is possible that a selection bias occurred, where those with voice or vocal tract complaints were more likely to complete the survey. Well-designed experimental studies comparing office and home workers, and comparing face-to-face versus telecommunication would be useful, particularly if a random sampling technique could be employed.
CONCLUSION
Dysphonia prevalence in those working from home appears higher than previously reported values for the general population. It is unclear whether VTD prevalence is significantly higher. Dysphonia and VTD incidence were however connected to the lockdown period and indicate a likely association. While dysphonia was usually mild and VTD symptoms were few, these could potentially develop into more serious complaints if left unmanaged.
Data from this study suggest that the home office environment and telecommunication practices play a role in the development of self-perceived dysphonia and VTD. With home working becoming increasingly common, workers’ voices need to be protected. Workplaces should consider equipment and training to maintain vocal wellness while working from home.
DISCLOSURES
Survey dissemination via a paid social media campaign was made possible through funding obtained from the Arts and Social Sciences Benefaction Fund, Trinity College Dublin. The funding source had no involvement in study design, data collection, analysis, interpretation of findings or dissemination.
Acknowledgments
The author is extremely grateful to the volunteers who examined the survey content during the pilot phase and to those who gave generously of their time to participate.
Footnotes
Supplementary data related to this article can be found online at doi:10.1016/j.jvoice.2020.10.010.
Appendix. SUPPLEMENTARY DATA
REFERENCES
- 1.Williams NR. Occupational voice disorders due to workplace exposure to irritants–a review of the literature. Occup Med (Lond) 2002;52:99–101. doi: 10.1093/occmed/52.2.99. [DOI] [PubMed] [Google Scholar]
- 2.Williams NR. Occupational groups at risk of voice disorders: a review of the literature. Occup Med (Lond) 2003;53:456–460. doi: 10.1093/occmed/kqg113. [DOI] [PubMed] [Google Scholar]
- 3.Johns-Fiedler H, van Mersbergen M. The prevalence of voice disorders in 911 emergency telecommunicators. J Voice. 2015;29 doi: 10.1016/j.jvoice.2014.08.008. 389 e381-310. [DOI] [PubMed] [Google Scholar]
- 4.Roy N, Merrill RM, Thibeault S, et al. Prevalence of voice disorders in teachers and the general population. J Speech Lang Hear Res. 2004;47:281–293. doi: 10.1044/1092-4388(2004/023). [DOI] [PubMed] [Google Scholar]
- 5.Misono S, Meredith L, Peterson CB, et al. New perspective on psychosocial distress in patients with dysphonia: the moderating role of perceived control. J Voice. 2016;30:172–176. doi: 10.1016/j.jvoice.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benninger MS, Holy CE, Bryson PC, et al. Prevalence and occupation of patients presenting with dysphonia in the United States. J Voice. 2017;31:594–600. doi: 10.1016/j.jvoice.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Lyberg-Ahlander V, Rydell R, Fredlund P, et al. Prevalence of voice disorders in the general population, based on the stockholm public health cohort. J Voice. 2018;33:900–905. doi: 10.1016/j.jvoice.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Geneid A, Ronkko M, Airaksinen L, et al. Pilot study on acute voice and throat symptoms related to exposure to organic dust: preliminary findings from a provocation test. Logoped Phoniatr Vocol. 2009;34:67–72. doi: 10.1080/14015430902845711. [DOI] [PubMed] [Google Scholar]
- 9.Rantala LM, Hakala S, Holmqvist S, et al. Associations between voice ergonomic risk factors and acoustic features of the voice. Logoped Phoniatr Vocol. 2015;40:99–105. doi: 10.3109/14015439.2013.831947. [DOI] [PubMed] [Google Scholar]
- 10.Alves M, Kruger E, Pillay B, et al. The effect of hydration on voice quality in adults: a systematic review. J Voice. 2019;33 doi: 10.1016/j.jvoice.2017.10.001. 125 e113-125 e128. [DOI] [PubMed] [Google Scholar]
- 11.Cardoso R, Lumini-Oliveira J, Meneses RFP. Associations between posture, voice, and dysphonia: a systematic review. J Voice. 2019;33 doi: 10.1016/j.jvoice.2017.08.030. 124 e121-124 e112. [DOI] [PubMed] [Google Scholar]
- 12.Lopes LW, Cabral GF, Figueiredo de, et al. Vocal tract discomfort symptoms in patients with different voice disorders. J Voice. 2015;29:317–323. doi: 10.1016/j.jvoice.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 13.Lopes LW, de Oliveira Florencio V, Silva POC, et al. Vocal tract discomfort scale (VTDS) and voice symptom scale (VoiSS) in the evaluation of patients with voice disorders. J Voice. 2019;33 doi: 10.1016/j.jvoice.2017.11.018. 381 e323-381 e332. [DOI] [PubMed] [Google Scholar]
- 14.Smith E, Verdolini K, Gray S, et al. Effect of voice disorders on quality of life. J Med Speech Lang Path. 1996;4:223–244. [Google Scholar]
- 15.Slavych B, Engelhoven A, Zraick R. Quality of life in persons with voice disorders: a review of patient-reported outcome measures. Int J Ther Rehabil. 2013;20:308–315. [Google Scholar]
- 16.Romak JJ, Orbelo DM, Maragos NE, et al. Correlation of the voice handicap index-10 (VHI-10) and voice-related quality of life (V-RQOL) in patients with dysphonia. J Voice. 2014;28:237–240. doi: 10.1016/j.jvoice.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 17.Roy N, Merrill RM, Thibeault S, et al. Voice disorders in teachers and the general population: effects on work performance, attendance, and future career choices. J Speech Lang Hear Res. 2004;47:542–551. doi: 10.1044/1092-4388(2004/042). [DOI] [PubMed] [Google Scholar]
- 18.Roy N, Merrill RM, Gray SD, et al. Voice disorders in the general population: prevalence, risk factors, and occupational impact. Laryngoscope. 2005;115:1988–1995. doi: 10.1097/01.mlg.0000179174.32345.41. [DOI] [PubMed] [Google Scholar]
- 19.Cohen SM, Kim J, Roy N, et al. Direct health care costs of laryngeal diseases and disorders. Laryngoscope. 2012;122:1582–1588. doi: 10.1002/lary.23189. [DOI] [PubMed] [Google Scholar]
- 20.Cohen SM, Kim J, Roy N, et al. Delayed otolaryngology referral for voice disorders increases health care costs. Am J Med. 2015;128 doi: 10.1016/j.amjmed.2014.10.040. 426.e411-428. [DOI] [PubMed] [Google Scholar]
- 21.Hirano M. Springer-Verlag; Vienna: 1981. Clinical Examination of Voice. [Google Scholar]
- 22.Mathieson L, Hirani SP, Epstein R, et al. Laryngeal manual therapy: a preliminary study to examine its treatment effects in the management of muscle tension dysphonia. J Voice. 2009;23:353–366. doi: 10.1016/j.jvoice.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Hogikyan ND, Sethuraman G. Validation of an instrument to measure voice-related quality of life (V-RQOL) J Voice. 1999;13:557–569. doi: 10.1016/s0892-1997(99)80010-1. [DOI] [PubMed] [Google Scholar]
- 24.Dillman DA, Smyth JD, Christian LM, et al. 3rd ed. Wiley; Hoboken, N.J.: 2009. Internet, Mail, and Mixed-Mode Surveys: the Tailored Design Method. [Google Scholar]
- 25.WageIndicator. Developing a detailed 8-country occupations database for comparative socio-economic research in the European Union. https://wageindicator.org/Wageindicatorfoundation/projects/euroccp/. Accessed August 19, 2020.
- 26.Bhattacharyya N. The prevalence of voice problems among adults in the United States. Laryngoscope. 2014;124:2359–2362. doi: 10.1002/lary.24740. [DOI] [PubMed] [Google Scholar]
- 27.Spantideas N, Drosou E, Karatsis A, et al. Voice disorders in the general Greek population and in patients with laryngopharyngeal reflux. Prevalence and risk factors. J Voice. 2015;29 doi: 10.1016/j.jvoice.2014.08.006. 389 e327-332. [DOI] [PubMed] [Google Scholar]
- 28.Luyten A, Bruneel L, Meerschman I, et al. Prevalence of vocal tract discomfort in the flemish population without self-perceived voice disorders. J Voice. 2016;30:308–314. doi: 10.1016/j.jvoice.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 29.Lehto L, Alku P, Bäckström T, et al. Voice symptoms of call-centre customer service advisers experienced during a work-day and effects of a short vocal training course. Logoped Phoniatr Vocol. 2005;30:14–27. doi: 10.1080/14015430510006659. [DOI] [PubMed] [Google Scholar]
- 30.Schneider-Stickler B, Knell C, Aichstill B, et al. Biofeedback on voice use in call center agents in order to prevent occupational voice disorders. J Voice. 2012;26:51–62. doi: 10.1016/j.jvoice.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 31.Phyland D, Miles A. Occupational voice is a work in progress: active risk management, habilitation and rehabilitation. Curr Opin Otolaryngol Head Neck Surg. 2019;27:439–447. doi: 10.1097/MOO.0000000000000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Remacle A, Petitfils C, Finck C, et al. Description of patients consulting the voice clinic regarding gender, age, occupational status, and diagnosis. Eur Arch Oto-Rhino-L. 2017;274:1567–1576. doi: 10.1007/s00405-016-4332-7. [DOI] [PubMed] [Google Scholar]
- 33.Mannetje A, Kromhout H. The use of occupation and industry classifications in general population studies. Int J Epidemiol. 2003;32:419–428. doi: 10.1093/ije/dyg080. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.