Graphical abstract
Keywords: COVID-19, SARS-CoV-2, Water treatment, Pandemic, Environmental impacts, Disinfectants
Highlights
-
•
Literature reporting the presence of SARS-CoV-2 in wastewater is reviewed.
-
•
Evaluation of SARS-CoV-2 in water is vital for its detection and quantification.
-
•
Research opportunities in water research associated with COVID-19 are highlighted.
-
•
Favourable environment for the survival of SARS-CoV-2 in water need to be assessed.
-
•
Effective methods for the removal of SARS-CoV-2 from water need to be developed.
Abstract
The outbreak of COVID-19 has posed enormous health, social, environmental and economic challenges to the entire human population. Nevertheless, it provides an opportunity for extensive research in various fields to evaluate the fate of the crisis and combat it. The apparent need for imperative research in the biological and medical field is the focus of researchers and scientists worldwide. However, there are some new challenges and research opportunities in the field of water and wastewater treatment concerning the novel coronavirus 2 (SARS-CoV-2). This article briefly summarizes the latest literature reporting the presence of SARS-CoV-2 in water and wastewater/sewage. Furthermore, it highlights the challenges, potential opportunities and research directions in the water and wastewater treatment field. Some of the significant challenges and research opportunities are the development of standard techniques for the detection and quantification of SARS-CoV-2 in the water phase, assessment of favorable environments for its survival and decay in water; and development of effective strategies for elimination of the novel virus from water. Advancement in research in this domain will help to protect the environment, human health, and managing this type of pandemic in the future.
1. Introduction
The current global pandemic of COVID-19 caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been growing briskly [1,2]. Although the major transmission routes of SARS-CoV-2 are through respiratory droplets and direct contact [[3], [4], [5]], recent studies have reported the presence of viral RNA of SARS-CoV-2 in untreated and treated wastewater and human feces [3,[6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21]]. In most of the studies, the samples were collected from wastewater treatment plants (WWTPs), while one study reported in the presence of SARS-CoV-2 in wastewater from a cruise ship and commercial passenger aircraft [22]. Recent studies conducted in the Netherlands and France confirmed that a reasonably high viral load of SARS-CoV-2 RNA is found in the sewage/wastewater [19,23].
The presence of SARS-CoV-2 in feces and municipal wastewater poses a severe threat to the environment due to its potential spread via these routes [[24], [25], [26], [27], [28]]. Therefore, there are serious concerns regarding the spread of SARS-CoV-2 through virus-laden aerosols-borne and fecal-oral routes [8,[29], [30], [31], [32], [33], [34], [35], [36], [37], [38]]. It is important to take the necessary precautions to limit the spread of the virus in the environment [39].
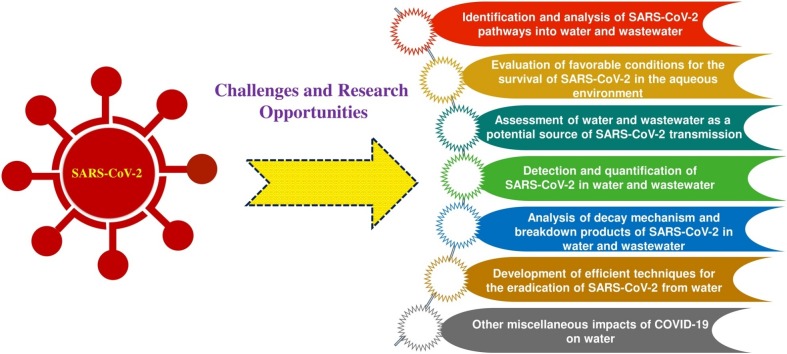
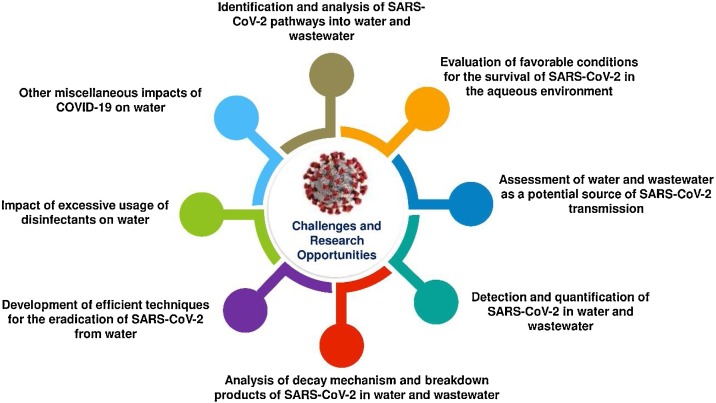
Nevertheless, it creates some new environmental challenges that demand an imperative need for research. Development of effective standard techniques for the detection and quantification of SARS-CoV-2 in water, assessment of the existing water purification technologies and development of novel advanced water treatment systems are major challenges and open research opportunities. Furthermore, careful surveillance of water and wastewater to be used as an early warning tool for such outbreaks in future, understanding the survival and decay mechanism of the novel virus in water and wastewater, analysis of potential pathways of SARS-CoV-2 into water bodies are other potential research opportunities for environmental researchers [[40], [41], [42], [43], [44]]. The major challenges and opportunities in the field of water and wastewater research are presented in Fig. 1 .
Fig. 1.
Potential challenges and opportunities in the field of water research.
The objective of this article is to highlight the potential opportunities and challenges in the field of water research concerning the novel SARS-CoV-2 virus. The directions for future research to safeguard human health, environment, and to predict and manage this type of pandemic in the future are also provided.
2. Research opportunities and challenges
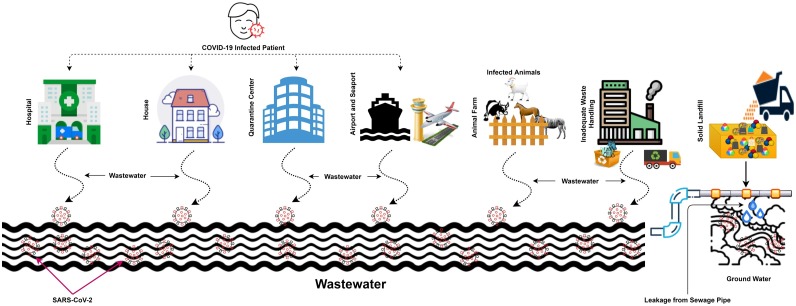
2.1. Identification and analysis of SARS-CoV-2 pathways into water and wastewater
Numerous studies have reported the presence of pathogenic viruses that enter into the water bodies through different sources [45,46]. Previous studies have demonstrated that SARS-CoV-2 can enter into the water bodies from hospital wastewater and sewage [5,[47], [48], [49]]. The waste and wastewater discharged from the quarantine facilities, airports/seaports, and residential buildings of infected humans and animals are the potential sources of SARS-CoV-2 than can enter into the water bodies. The SARS-CoV-2 may also find its ways to groundwater through possible leaching and infiltrations of effluents from health care facilities, sewage, solid landfill and drainage water. Another important source of viral contamination to the water environment is the leakage from sewage pipes. The possible sources and pathways of SARS-CoV-2 in water systems are depicted in Fig. 2 .
Fig. 2.
Sources and potential pathways of SARS-CoV-2 in the water systems.
Due to the fast-growing number of patients worldwide, the virus concentration in wastewater/sewage is expected to increase rapidly. The potential pathways of SARS-CoV-2 into wastewater are via shedding in the stool (for the viable virus), while through urine and stool (for the non-viable virus) [50]. A careful and extensive investigation of all the possible sources of water contamination by SARS-CoV-2 is needed that potentially includes wastewater dispatches from hospitals and greywater generated from washing personal protective equipment (PPE), surfaces and floors [51]. Table 1 summarizes the literature reporting the presence of SARS-CoV-2 RNA in wastewater in various parts of the world [3,17,19,42]. All the reported samples were collected during the period from Janruary 2020 to July 2020. The concentrations of SARS-CoV-2 RNA in untreated wastewater was in the range of 5.6 × 10 to 4.6 × 108 copies per liter [6,7,14,16,52,53]. Some studies also reported the detection of SARS-CoV-2 in treated water samples [3,16].
Table 1.
A summary of the literature reporting the presence of SARS-CoV-2 in wastewater/sewage.
| Sampling Period | Water Type | Location | Reference |
|---|---|---|---|
| (March- April) 2020 | Wastewater from WWTPs | Murcia (Spain) | [3] |
| (March- April) 2020 | Untreated wastewater (sewage) | Southeast Queensland (Australia) | [6] |
| (March- April) 2020 | Wastewater from WWTPs | Bozeman, Montana (USA) | [7] |
| (February- April) 2020 | Wastewater from WWTPs | Milan and Rome (Italy) | [17] |
| April 2020 | Wastewater from WWTPs | Istanbul (Turkey) | [18] |
| June 2020 | River water | Quito (Ecuador) | [20] |
| (April- May) 2020 | Aircraft and cruise ship wastewater | Passenger aircraft flight from Los Angeles – Brisbane Hongkong – Brisbane New Delhi– Sydney Cruise ship (Australia) |
[22] |
| March 2020 | Wastewater from the treatment facility | Massachusetts (USA) | [42] |
| (February- March) 2020 | Sewage/wastewater from WWTPs | Netherlands | [51] |
| May 2020 | Wastewater from WWTPs | Gujarat (India) | [53] |
| April 2020 | Raw and treated wastewater samples from WWTPs | Milano Metropolitan Area Italy) | [60] |
| (March- April) 2020 | Wastewater from WWTPs | Paris (France) | [73] |
| February 2020 | Sewage from hospital sewage disinfection pool | Hospital of Zhejiang University, China | [92] |
| May 2020 | Wastewater from WWTPs, influent pump stations, or interceptor lines | New York (USA) | [125] |
| (March- April) 2020 | Wastewater from WWTPs | Different localities in Israel | [126] |
| (February- April) 2020 | Wastewater from WWTPs | Valencia (Spain) | [127] |
| (March-May) 2020 | Secondary-treated wastewater | Yamanashi Prefecture (Japan) | [128] |
| (March- April) 2020 | Wastewater from WWTPs | Ishikawa and Toyama prefectures (Japan) | [129] |
| April 2020 | Wastewater from WWTPs | Ourense (Spain) | [130] |
| (May-June) 2020 | Wastewater from WWTPs | Jaipur (India) | [131] |
| (March- April) 2020 | Wastewater from the drainage of COVID-19 infected areas and quarantine center | Various districts in Pakistan | [132] |
| (January-April) 2020 | Wastewater from WWTPs | Southern Louisiana (USA) | [133] |
| (April-June 2020) | Untreated wastewater from WWTPs | Czech Republic | [134] |
| April 2020 | Wastewater from WWTPs | North-Rhine Westphalia (Germany) | [135] |
| (May-July) 2020 | Wastewater from WWTPs | Montpellier (France) | [136] |
2.2. Evaluation of favorable conditions for the survival of SARS-CoV-2 in the aqueous environment
Previous reports suggested that SARS-CoV-2 survival in an aqueous environment is strongly dependent on the characteristics of water/wastewater [[54], [55], [56]]. The pH, temperature, presence of antagonistic bacteria, organic matter, sunlight and oxidants might affect the survival of SARS-CoV-2 in aqueous environment [54,57,58]. A previous study reported that the inactivation of coronaviruses in the water is highly dependent on the level of organic matter, temperature, and presence of antagonistic bacteria [54]. The suspended solids and organic matter present in water can provide protection for viruses that adsorb to these particles, and they can survive up to several days [54]. However, some published reports suggested that coronaviruses are very sensitive to high temperature and oxidants such as chlorine [57].
Studies have reported that surrogate coronaviruses remained infectious in water and sewage for days to weeks [46]. A recent study estimated that the half-life of SARS-CoV-2 in wastewater is in the range of 4.8 and 7.2 h [44], while another study reported that the virus causing COVID-19 could survive in untreated wastewater from hours to days [59]. It is essential to understand the stability and decay mechanism of SARS-CoV-2 in water and wastewater.
The significant parameters that can predict the reduction kinetics need to be determined, to establish the favorable and unfavorable conditions for the survival of SARS-CoV-2 in aqueous environment. Detailed investigations of various water/wastewater samples with different characteristics are required to assess the potential exposure risk of water contaminated with this virus. Launching a monitoring program is vital to determine the fate of SARS-CoV-2 in water cycle [49]. Theoretical and computational analysis might help to provide a basis for experimental research.
2.3. Assessment of water and wastewater as a potential source of SARS-CoV-2 transmission
Until now, there is no evidence and enough data to confirm if the water and wastewater containing SARS-CoV-2 could be the potential source of its transmission. Although some studies predicted a low risk of SARS-CoV-2 transmission via wastewater (especially the treated water) [55,60], still extensive investigations need to be performed to validate these predictions and initial findings. The information regarding the viability of the closely related SARS-CoV-1 virus in wastewater may provide useful information about the survival of SARS-CoV-2 in an aqueous environment [54].
As a precaution, the wastewater/sewage treatment plants should be considered as the potential transmission routes. A recent study demonstrated the quantitative microbial risk assessment (QMRA) approach to investigate the potential health risks of SARS-CoV-2 in sewage to WWTPs workers [61]. Results revealed that the viral loads in wastewater/sewage at the entrance of WWTPs were above the WHO benchmark of tolerable risk used for virus infection of 10−3 [6,7,14,16,52,53]. It is essential to evaluate bioaerosol and airborne particle risks to nearby communities and WWTP workers. In general, it can be made mandatory for the WWTP workers that perform manual cleaning of screening to use face masks and face shields.
The aerosol formation during wastewater treatment needs to be carefully examined as a potential source of virus transmission [62]. Water-related exposures may occur in communities with weak sewage infrastructure, or that use wastewater for irrigation [63]. Viral aerosols from a leaking sewage pipe at Amoy Gardens complex in Hong Kong were identified as the transmission route for coronaviruses during the SARS-CoV-1 outbreak in 2003 [47].
The virus can also make its way into the drinking water distribution systems from the accidental contamination of drinking water with raw sewage and can enter individual homes. The presence of SARS-CoV-2 in water may also affect the water supply system by forming the biofilms that can compromise the water quality and endanger human health.
There is also an imperative need for research to investigate the fecal-oral transmission potential of SARS-CoV-2 [33,64]. It is crucial to examine if the SARS-CoV-2-contaminated wastewater has adverse impacts on aquatic life, soil, and wildlife. This needs careful examinations, risk analysis and thorough investigations to reach a conclusion. Furthermore, monitoring and control measures are essential along the wastewater treatment route to avert coronavirus spread.
It is recommended that the WWTP managers and stakeholders develop risk management strategies for the protection of WWTP workers and nearby communities [61]. The disinfection steps in both WWTPs and drinking water plants need to be developed carefully. The quantitative disinfection kinetics need to be established, and an optimum dose for inactivation of SARS-CoV-2 need to be determined. Decentralized virus inactivation treatment for water discharged from WWTPs and drinking water plants can also be beneficial in reducing the environmental load of SARS-CoV-2.
2.4. Detection and quantification of SARS-CoV-2 in water and wastewater
Detection and quantification of SARS-CoV-2 in water and wastewater is an essential but challenging step to track the infectious disease [50,65]. Due to complex nature of wastewater matrix, it is essential to develop new biomarker extraction techniques as well as selective, sensitive, and cost-effective tools for the analysis of wastewater samples containing the novel virus [66]. To avoid exposure to dangerous virus SARS-CoV-2 and to protect the safety of the lab analysts, it is recommended to use virus surrogates instead of harmful SARS-CoV-2 [34].
Wastewater-based epidemiology (WBE) has been recognized as a useful tool for evaluating, predicting and managing the disease outbreaks [40,43,44,67]. The concept is mainly based upon the detection, extraction, and analysis of biological and chemical compounds (referred to as biomarkers). Recent studies have reported the successful detection of the novel virus in municipal wastewater and human stool [6,7,15,42,51,[68], [69], [70]]. Surveillance of relative changes in concentrations of SARS-CoV- 2 RNA at the inlet of WWTP over time can serve as a useful tool for early warning for virus spread in the population [19]. Both upstream sampling (i.e., at sewerage maintenance holes) and downstream sampling (i.e., at the WWTP) approach can be used; however, upstream sampling is more appropriate due to variability in downstream samples. A GIS-based sewerage map and flow rates would aid in the selection of upstream sampling locations [71]. Quantification of SARS-CoV-2 RNA in settled solids in WWTPs may also be used as a reliable and sensitive target for WBE [72].
Moreover, monitoring of sewage discharged from international airports and seaports would allow very early detection of the entrance of the virus into a country. It could also help the relevant authorities in deciding the implementation or removal of lockdown [34]. It is essential to develop an integrated wastewater surveillance programs by considering both privacy and inequality concerns of the public [71].
Wurtzer et al. [73] performed the time-course quantitative analysis of SARS-CoV-2 in Paris sewage by reverse transcription-quantitative polymerase chain reaction (RT-qPCR) to investigate virus circulation in humans. However, these studies are at the initial stage, and a large pool of data from different parts of the world is necessary to develop a reliable and sensitive detection method for SARS-CoV-2 detection in wastewater/sewage [74].
A multidisciplinary research approach including engineers, microbiologists, chemists, and public health experts, will be productive to nurture more effective techniques for the quantification of SARS-CoV-2 in water. Since SARS-CoV-2 has a presumably short half-life in water, the detection technique must be valid for both viable and non-viable SARS-CoV-2 in water. The virus can be degraded into other products; it is essential to develop strategies that could use these degraded products as target materials for detection and quantification [50].
The lack of standardized and optimized protocol for the detection and quantification of SARS-CoV-2 in wastewater is another major challenge [59,75,76]. This may lead to discrepancies in the results obtained by different laboratories, as indicated by a recent study [3]. Currently, the RT-qPCR has been employed widely for detection of SARS-CoV-2 in water samples [77].
There is an imperative need to develop a standard operating procedure for accurate detection and quantification SARS-CoV-2 in water and wastewater. Furthermore, a standard sampling procedure must be developed to extract/isolate, detect and quantify the virus accurately. This is an essential step for the development of commercial laboratories in various parts of the world that can accurately detect and quantify the virus with reproducible results.
Advancements in the field of microbiology might play a key role in developing a low cost, efficient method for detection and quantification of viral RNA [78]. Recently, various innovative detection techniques have been reported in the literature [[79], [80], [81]]. Novel nanomaterials-based sensors were found to be useful for the detection of waterborne pathogens [82]. There is a research potential to develop techniques using a similar approach for the detection of SARS-CoV-2 by utilizing different novel nanomaterials. A reliable widely-accepted surveillance system needs to be developed for the accurate quantification of SARS-CoV-2 in water samples.
2.5. Analysis of decay mechanism and breakdown products of SARS-CoV-2 in water and wastewater
The persistence of SARS-CoV-2 in the water environment is assumed to be short due to the enveloped nature of the virus [49,60,83]. The half-life of SARS-CoV-2 in hospital wastewater was estimated to range between 4.8 and 7.2 h at 20 °C [44]. However, little is known about the vitality of SARS-CoV-2 in water [16]. Furthermore, the accurate survival period and concentration of SARS-CoV-2 in water are still indefinite, and these are open areas for research.
It is essential to understand the decay mechanism and breakdown products of SARS-CoV-2 in water and wastewater. It will not only help in developing effective techniques for accurate detection and quantification but also will be useful for proposing an efficient disinfection technique. A recent study reported the transcriptomic architecture of SARS-CoV-2 [84]. The SARS-CoV-2 may present in the water phase either in a viable state or in the non-viable form of viral debris [50]. However, the actual degradation products and accurate decay mechanism of SARS-CoV-2 in water phase need to be explored yet.
2.6. Development of efficient techniques for the eradication of SARS-CoV-2 from water and wastewater/sewage
The traditional treatment techniques for the removal of viruses from wastewater include sand filters, chlorine treatment, UV inactivation, ozone treatment, microbial treatment, membranes and pond systems [[85], [86], [87], [88], [89], [90]]. Though it is assumed that the current techniques used for wastewater treatment might be helpful to eliminate the novel virus; due to the global impact of this pandemic, experimental results are needed to validate this assumption [62,[91], [92], [93]]. Likewise, experimental shreds of evidence are required to confirm the effectiveness of household filtration systems, chlorination, densification and boiling for the elimination of the novel virus from water. It might be needed to upgrade the existing water and wastewater treatment systems or develop new treatment techniques to treat the SARS-CoV-2-contaminated water. The more stringent treatment above the current level is needed for virus reduction to ensure the safety of recycled water [94,95]. WHO has highlighted guidelines on the safe management of water in July 2020 [62]. A recent study stated that the current disinfection strategy recommended by WHO might not be adequate to deactivate SARS-CoV-2 in water [96]. The existing wastewater treatment system might need necessary alternation or additional pretreatment steps to deactivate the SARS-CoV-2. It should also be investigated if the presence of SARS-CoV-2 in wastewater affect the treatment process for the removal of other pollutants.
Recent advancement in nanotechnology, biotechnology and material sciences have opened many doors of applications and exhibited tremendous potential in water purification [[97], [98], [99], [100], [101], [102]]. The development of effective techniques for the inactivation of SARS-CoV-2 is vital to limit its presence in wastewater and lessen its potential adverse effects on human health and the environment. Significant treatment steps are essential to upgrade both the wastewater and drinking water treatment plants to eradicate SARS-CoV-2 or its RNA fragments.
Recent years have witnessed tremendous progress in the applications of various novel materials in water treatment [[103], [104], [105], [106]]. Nanomaterials and their composites might play a critical role in the development of an efficient method for the eradication of SARS-CoV-2 from water [[106], [107], [108], [109], [110]]. Advances in membrane systems provide an effective route for the removal of viruses from water [[111], [112], [113], [114], [115]].
For drinking water, a potable water straw or UV-based system can be developed to filter/kill the virus and to reduce the risk of waterborne viral infection [116]. A recent study reported that there is a negative correlation between sunlight UV dose and percent positive of SARS-CoV-2 [117]. Other techniques such as oxidation, coagulation and photocatalytic killing of the virus must also be explored to determine the effective treatment option for the deactivation of SARS-CoV-2 in water.
The efficiency of emerging disinfection technologies for SARS-CoV-2 inactivation need to be appraised. The water distribution systems may potentially host the novel virus due to biofilm growth and presence of bacterial colonies. Innovations and improvements in the water distribution and plumbing systems are vital to minimize the transmission of SARS-CoV-2 through the water [118]. As a general rule, it is the combination of different techniques in primary, secondary and tertiary treatments that would allow sufficient virus removal to limit the possibility of environmental contamination. The SARS-CoV-2 pandemic should develop a global awareness for improving the wastewater treatment systems even in developing countries, due to the possibility of its spread through the aquatic environment from inadequately treated wastewater. The presence of SARS-CoV-2 in wastewater may have consequences for public health in developing countries with poor water and sewage infrastructure, and inadequate institutional treatment/disinfection facilities.
Future research in these lines is essential for the protection of public health and the environment. In addition, robust policy intervention is essential to ensure reasonable compliance regarding the discharge of wastewater in various parts of the world.
2.7. Other miscellaneous impacts of COVID-19 on water
One of the major environmental concern associated with COVID-19 pandemic is the excessive use of disinfectants (such as alcohol-based hand sanitizers and disinfecting soaps). The usage of disinfectants during the COVID-19 pandemic increases environmental and energy footprints significantly. A recent report reveals that 2000 tons of disinfectants are dispensed at in sewage systems in Wuhan City of China from January 29 to February 18, 2020 [119,120]. These discharges not only poses a potential threat to the marine environment but can also contaminate drinking water resources. Another study estimated that excessive use of disinfectants and frequent handwashing could increase consumption of drinking water by 20 % and lead to the generation of 15–18 % more wastewater [121].
The alcohol-based hand sanitizer is not only associated with some health issues, but it may also result in adverse impacts on the environment [122,123]. A recent study highlighted that the extensive use of disinfectants poses a significant threat to urban wildlife [124]. These disinfectants may find their ways to reach water bodies and pollute them. It is, therefore, necessary to assess the exact hostile impacts of the disinfectants that discharge into water bodies and mitigate them to the maximum possible extent. In addition, the use of masks, gloves and other PPE have resulted in the generation of a massive amount of wastes in the environment. Strategies for proper management of waste must be developed to lessen its adverse environmental impacts.
3. Conclusion
In summary, besides severe threats to humanity, the ongoing pandemic offers the opportunity to environmental engineers and scientists to play a responsible role to control the potential spread of the virus from water. Development of effective standard techniques for the detection and quantification, assessment of the existing water purification technologies and development of novel effective systems for elimination of SARS-CoV-2 from water are critical challenges and open research areas. Furthermore, understanding the mechanism of virus survival and decay in the aqueous environment and the development of low cost, environmentally friendly techniques for the removal of virus are other opportunities for researchers. Progress in these research directions will also be beneficial in managing similar pandemics in the future and safeguard human health and the environment. Approaches for risk management must be established by considering the whole water cycle, from the sources of river basins, oceans, to wastewater discharge and water reuse. Multidisciplinary research involving engineers, microbiologists, chemists, and public health experts are needed to address these challenges and to safeguard the aquatic environments.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.WHO . 2020. Pneumonia of Unknown Cause – China.https://www.who.int/csr/don/en/, Accessed on 4th October 2020 [Google Scholar]
- 2.WHO . 2020. Coronavirus Disease (COVID-19) Pandemic.https://www.who.int/emergencies/diseases/novel-coronavirus-2019, Accessed on 4th October 2020 [Google Scholar]
- 3.Randazzo W., Truchado P., Cuevas-Ferrando E., Simón P., Allende A., Sánchez G. SARS-CoV-2 RNA in wastewater anticipated COVID-19 occurrence in a low prevalence area. Water Res. 2020:115942. doi: 10.1016/j.watres.2020.115942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meselson M. Droplets and aerosols in the transmission of SARS-CoV-2. N. Engl. J. Med. 2020;382:2063. doi: 10.1056/NEJMc2009324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adelodun B., Ajibade F.O., Ibrahim R.G., Bakare H.O., Choi K.-S. Snowballing transmission of COVID-19 (SARS-CoV-2) through wastewater: any sustainable preventive measures to curtail the scourge in low-income countries? Sci. Total Environ. 2020;742:140680. doi: 10.1016/j.scitotenv.2020.140680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed W., Angel N., Edson J., Bibby K., Bivins A., O’Brien J.W., Choi P.M., Kitajima M., Simpson S.L., Li J., Tscharke B., Verhagen R., Smith W.J.M., Zaugg J., Dierens L., Hugenholtz P., Thomas K.V., Mueller J.F. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewater surveillance of COVID-19 in the community. Sci. Total Environ. 2020:138764. doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nemudryi A., Nemudraia A., Surya K., Wiegand T., Buyukyoruk M., Wilkinson R., Wiedenheft B. Temporal detection and phylogenetic assessment of SARS-CoV-2 in municipal wastewater. MedRxiv. 2020;2020 doi: 10.1101/2020.04.15.20066746. 04.15.20066746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu Y., Guo C., Tang L., Hong Z., Zhou J., Dong X., Yin H., Xiao Q., Tang Y., Qu X., Kuang L., Fang X., Mishra N., Lu J., Shan H., Jiang G., Huang X. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol. 2020;5:434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amirian E.S. Potential fecal transmission of SARS-CoV-2: current evidence and implications for public health. Int. J. Infect. Dis. 2020;95:363–370. doi: 10.1016/j.ijid.2020.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quilliam R.S., Weidmann M., Moresco V., Purshouse H., O’Hara Z., Oliver D.M. COVID-19: The environmental implications of shedding SARS-CoV-2 in human faeces. Environ. Int. 2020;140:105790. doi: 10.1016/j.envint.2020.105790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng S.C., Tilg H. COVID-19 and the gastrointestinal tract: more than meets the eye. Gut. 2020;69:973–974. doi: 10.1136/gutjnl-2020-321195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gu J., Han B., Wang J. COVID-19: gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158:1518–1519. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collivignarelli M.C., Collivignarelli C., Carnevale Miino M., Abbà A., Pedrazzani R., Bertanza G. SARS-CoV-2 in sewer systems and connected facilities. Process Saf. Environ. Prot. 2020;143:196–203. doi: 10.1016/j.psep.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kitajima M., Ahmed W., Bibby K., Carducci A., Gerba C.P., Hamilton K.A., Haramoto E., Rose J.B. SARS-CoV-2 in wastewater: state of the knowledge and research needs. Sci. Total Environ. 2020:139076. doi: 10.1016/j.scitotenv.2020.139076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lodder W., de Roda Husman A.M. SARS-CoV-2 in wastewater: potential health risk, but also data source. Lancet Gastroenterol. Hepatol. 2020;5:533–534. doi: 10.1016/S2468-1253(20)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wurtzer S., Marechal V., Mouchel J.-M., Moulin L. Time course quantitative detection of SARS-CoV-2 in Parisian wastewaters correlates with COVID-19 confirmed cases. MedRxiv. 2020;2020 doi: 10.1101/2020.04.12.20062679. 04.12.20062679. [DOI] [Google Scholar]
- 17.La Rosa G., Iaconelli M., Mancini P., Bonanno Ferraro G., Veneri C., Bonadonna L., Lucentini L., Suffredini E. First detection of SARS-COV-2 in untreated wastewaters in Italy. MedRxiv. 2020;2020 doi: 10.1101/2020.04.25.20079830. 04.25.20079830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alpaslan Kocamemi B., Kurt H., Hacioglu S., Yarali C., Saatci A.M., Pakdemirli B. First data-set on SARS-CoV-2 detection for Istanbul wastewaters in Turkey. MedRxiv. 2020;2020 doi: 10.1101/2020.05.03.20089417. 05.03.20089417. [DOI] [Google Scholar]
- 19.Medema G., Heijnen L., Elsinga G., Italiaander R., Brouwer A. Presence of SARS-coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ. Sci. Technol. Lett. 2020;7:511–516. doi: 10.1021/acs.estlett.0c00357. [DOI] [PubMed] [Google Scholar]
- 20.Guerrero-Latorre L., Ballesteros I., Villacres I., Granda-Albuja M.G., Freire B., Rios-Touma B. First SARS-CoV-2 detection in river water: implications in low sanitation countries. MedRxiv. 2020;2020 doi: 10.1101/2020.06.14.20131201. 06.14.20131201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heller L., Mota C.R., Greco D.B. COVID-19 faecal-oral transmission: Are we asking the right questions? Sci. Total Environ. 2020;729:138919. doi: 10.1016/j.scitotenv.2020.138919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahmed W., Bertsch P.M., Angel N., Bibby K., Bivins A., Dierens L., Edson J., Ehret J., Gyawali P., Hamilton K., Hosegood I., Hugenholtz P., Jiang G., Kitajima M., Sichani H.T., Shi J., Shimko K.M., Simpson S.L., Smith W.J.M., Symonds E.M., Thomas K.V., DSC, Verhagen R., Zaugg J., Mueller J.F. Detection of SARS-CoV-2 RNA in commercial passenger aircraft and cruise ship wastewater: a surveillance tool for assessing the presence of COVID-19 infected travelers. J. Travel Med. 2020;27(5):1–11. doi: 10.1093/jtm/taaa116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leste-Lasserre C. Coronavirus found in Paris sewage points to early warning system. Science (80-.) 2020;368:6489. [Google Scholar]
- 24.Shutler J., Zaraska K., Holding T.M., Machnik M., Uppuluri K., Ashton I., Migdal L., Dahiya R. Risk of SARS-CoV-2 infection from contaminated water systems. MedRxiv. 2020;2020 doi: 10.1101/2020.06.17.20133504. 06.17.20133504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kassem I.I., Jaafar H. The potential impact of water quality on the spread and control of COVID-19 in Syrian refugee camps in Lebanon. Water Int. 2020:1–7. doi: 10.1080/02508060.2020.1780042. [DOI] [Google Scholar]
- 26.Carducci A., Federigi I., Liu D., Thompson J.R., Verani M. Making Waves: coronavirus detection, presence and persistence in the water environment: state of the art and knowledge needs for public health. Water Res. 2020;179:115907. doi: 10.1016/j.watres.2020.115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wartecki A., Rzymski P. On the coronaviruses and their associations with the aquatic environment and wastewater. Water. 2020;12 doi: 10.3390/w12061598. [DOI] [Google Scholar]
- 28.Cahill N., Morris D. Recreational waters – a potential transmission route for SARS-CoV-2 to humans? Sci. Total Environ. 2020;740:140122. doi: 10.1016/j.scitotenv.2020.140122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hindson J. COVID-19: faecal–oral transmission? Nat. Rev. Gastroenterol. Hepatol. 2020;17:259. doi: 10.1038/s41575-020-0295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhowmick G.D., Dhar D., Nath D., Ghangrekar M.M., Banerjee R., Das S., Chatterjee J. Coronavirus disease 2019 (COVID-19) outbreak: some serious consequences with urban and rural water cycle. Npj Clean Water. 2020;3:32. doi: 10.1038/s41545-020-0079-1. [DOI] [Google Scholar]
- 31.Wang J., Du G. COVID-19 may transmit through aerosol. Irish J. Med. Sci. (1971-) 2020;189:1143–1144. doi: 10.1007/s11845-020-02218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xiao F., Tang M., Zheng X., Li C., He J., Hong Z., Huang S., Zhang Z., Lin X., Fang Z., Lai R., Chen S., Liu J., Huang J., Xia J., Li Z., Jiang G., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. MedRxiv. 2020;2020 doi: 10.1101/2020.02.17.20023721. 02.17.20023721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yeo C., Kaushal S., Yeo D. Enteric involvement of coronaviruses: is faecal-oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol. Hepatol. 2020;5:335–337. doi: 10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lesimple A., Jasim S.Y., Johnson D.J., Hilal N. The role of wastewater treatment plants as tools for SARS-CoV-2 early detection and removal. J. Water Process Eng. 2020;38:101544. doi: 10.1016/j.jwpe.2020.101544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nouri-Vaskeh M., Alizadeh L. Fecal transmission in COVID-19: a potential shedding route. J. Med. Virol. 2020;92(10):1731–1732. doi: 10.1002/jmv.25816. n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Foladori P., Cutrupi F., Segata N., Manara S., Pinto F., Malpei F., Bruni L., La Rosa G. SARS-CoV-2 from faeces to wastewater treatment: what do we know? A review. Sci. Total Environ. 2020;743:140444. doi: 10.1016/j.scitotenv.2020.140444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dolfing J. The importance of sewage archiving in coronavirus epidemiology and beyond. Environ. Sci. Technol. 2020;54:7740–7741. doi: 10.1021/acs.est.0c02972. [DOI] [PubMed] [Google Scholar]
- 38.Xu Y., Li X., Zhu B., Liang H., Fang C., Gong Y., Guo Q., Sun X., Zhao D., Shen J., Zhang H., Liu H., Xia H., Tang J., Zhang K., Gong S. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat. Med. 2020;26:502–505. doi: 10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carraturo F., Del Giudice C., Morelli M., Cerullo V., Libralato G., Galdiero E., Guida M. Persistence of SARS-CoV-2 in the environment and COVID-19 transmission risk from environmental matrices and surfaces. Environ. Pollut. 2020;265:115010. doi: 10.1016/j.envpol.2020.115010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murakami M., Hata A., Honda R., Watanabe T. Letter to the editor: wastewater-based epidemiology can overcome representativeness and stigma issues related to COVID-19. Environ. Sci. Technol. 2020;54(9):5311. doi: 10.1021/acs.est.0c02172. [DOI] [PubMed] [Google Scholar]
- 41.Mao K., Zhang H., Yang Z. Can a paper-based device trace COVID-19 sources with wastewater-based epidemiology? Environ. Sci. Technol. 2020;54:3733–3735. doi: 10.1021/acs.est.0c01174. [DOI] [PubMed] [Google Scholar]
- 42.Wu F., Xiao A., Zhang J., Gu X., Lee W.L., Kauffman K., Hanage W., Matus M., Ghaeli N., Endo N., Duvallet C., Moniz K., Erickson T., Chai P., Thompson J., Alm E. SARS-CoV-2 titers in wastewater are higher than expected from clinically confirmed cases. MedRxiv. 2020;2020 doi: 10.1101/2020.04.05.20051540. 04.05.20051540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sims N., Kasprzyk-Hordern B. Future perspectives of wastewater-based epidemiology: monitoring infectious disease spread and resistance to the community level. Environ. Int. 2020;139:105689. doi: 10.1016/j.envint.2020.105689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hart O.E., Halden R.U. Computational analysis of SARS-CoV-2/COVID-19 surveillance by wastewater-based epidemiology locally and globally: feasibility, economy, opportunities and challenges. Sci. Total Environ. 2020;730:138875. doi: 10.1016/j.scitotenv.2020.138875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fong T.-T., Lipp E.K. Enteric viruses of humans and animals in aquatic environments: health risks, detection, and potential water quality assessment tools. Microbiol. Mol. Biol. Rev. 2005;69:357–371. doi: 10.1128/MMBR.69.2.357-371.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Casanova L., Rutala W.A., Weber D.J., Sobsey M.D. Survival of surrogate coronaviruses in water. Water Res. 2009;43:1893–1898. doi: 10.1016/j.watres.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hung L.S. The SARS epidemic in Hong Kong: what lessons have we learned? J. R. Soc. Med. 2003;96:374–378. doi: 10.1258/jrsm.96.8.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leung W.K., To K., Chan P.K.S., Chan H.L.Y., Wu A.K.L., Lee N., Yuen K.Y., Sung J.J.Y. Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology. 2003;125:1011–1017. doi: 10.1016/j.gastro.2003.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Naddeo V., Liu H. Editorial Perspectives: 2019 novel coronavirus (SARS-CoV-2): what is its fate in urban water cycle and how can the water research community respond? Environ. Sci. Water Res. Technol. 2020;6:1213–1216. doi: 10.1039/D0EW90015J. [DOI] [Google Scholar]
- 50.Daughton C. The international imperative to rapidly and inexpensively monitor community-wide Covid-19 infection status and trends. Sci. Total Environ. 2020;726:138149. doi: 10.1016/j.scitotenv.2020.138149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Medema G., Heijnen L., Elsinga G., Italiaander R., Brouwer A. Presence of SARS-Coronavirus-2 in sewage. MedRxiv. 2020;2020 doi: 10.1101/2020.03.29.20045880. 03.29.20045880. [DOI] [PubMed] [Google Scholar]
- 52.Peccia J., Zulli A., Brackney D.E., Grubaugh N.D., Kaplan E.H., Casanovas-Massana A., Ko A.I., Malik A.A., Wang D., Wang M., Warren J.L., Weinberger D.M., Omer S.B. SARS-CoV-2 RNA concentrations in primary municipal sewage sludge as a leading indicator of COVID-19 outbreak dynamics. MedRxiv. 2020;2020 doi: 10.1101/2020.05.19.20105999. 05.19.20105999. [DOI] [Google Scholar]
- 53.Kumar M., Patel A.K., Shah A.V., Raval J., Rajpara N., Joshi M., Joshi C.G. The first proof of the capability of wastewater surveillance for COVID-19 in India through the detection of the genetic material of SARS-CoV-2. MedRxiv. 2020;2020 doi: 10.1101/2020.06.16.20133215. 06.16.20133215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gundy P.M., Gerba C.P., Pepper I.L. Survival of coronaviruses in water and wastewater. Food Environ. Virol. 2008;1:10. doi: 10.1007/s12560-008-9001-6. [DOI] [Google Scholar]
- 55.Chin A., Chu J., Perera M., Hui K., Yen H.-L., Chan M., Peiris M., Poon L. Stability of SARS-CoV-2 in different environmental conditions. MedRxiv. 2020;2020 doi: 10.1101/2020.03.15.20036673. 03.15.20036673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ye Y., Ellenberg R.M., Graham K.E., Wigginton K.R. Survivability, Partitioning, and Recovery of Enveloped Viruses in Untreated Municipal Wastewater. Environ. Sci. Technol. 2016;50:5077–5085. doi: 10.1021/acs.est.6b00876. [DOI] [PubMed] [Google Scholar]
- 57.La Rosa G., Bonadonna L., Lucentini L., Kenmoe S., Suffredini E. Coronavirus in water environments: occurrence, persistence and concentration methods – a scoping review. Water Res. 2020;179:115899. doi: 10.1016/j.watres.2020.115899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Silverman A.I., Boehm A.B. Systematic review and meta-analysis of the persistence and disinfection of human coronaviruses and their viral surrogates in water and wastewater. Environ. Sci. Technol. Lett. 2020;7:544–553. doi: 10.1021/acs.estlett.0c00313. [DOI] [PubMed] [Google Scholar]
- 59.Barcelo D. An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J. Environ. Chem. Eng. 2020;8:104006. doi: 10.1016/j.jece.2020.104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rimoldi S.G., Stefani F., Gigantiello A., Polesello S., Comandatore F., Mileto D., Maresca M., Longobardi C., Mancon A., Romeri F., Pagani C., Moja L., Gismondo M.R., Salerno F. Presence and vitality of SARS-CoV-2 virus in wastewaters and rivers. MedRxiv. 2020;2020 doi: 10.1101/2020.05.01.20086009. 05.01.20086009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zaneti R.N., Girardi V., Spilki F.R., Mena K., Westphalen A.P.C., Colares E.Rda C., Pozzebon A.G., Etchepare R.G. QMRA of SARS-CoV-2 for workers in wastewater treatment plants. MedRxiv. 2020;2020 doi: 10.1101/2020.05.28.20116277. 05.28.20116277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.WHO , Water, Sanitation, Hygiene, and Waste Management for the COVID-19 Virus: Interim Guidance 23 April 2020 (2020), https://apps.who.int/iris/bitstream/handle/10665/331846/WHO-2019-nCoV-IPC_WASH-2020.3-eng.pdf?ua=1, Accessed on 4th October 2020.
- 63.Wigginton K.R., Boehm A.B. Environmental engineers and scientists have important roles to play in stemming outbreaks and pandemics caused by enveloped viruses. Environ. Sci. Technol. 2020;54:3736–3739. doi: 10.1021/acs.est.0c01476. [DOI] [PubMed] [Google Scholar]
- 64.He Y., Wang Z., Li F., Shi Y. Public health might be endangered by possible prolonged discharge of SARS-CoV-2 in stool. J. Infect. 2020;80:e18–e19. doi: 10.1016/j.jinf.2020.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Venugopal A., Ganesan H., Sudalaimuthu Raja S.S., Govindasamy V., Arunachalam M., Narayanasamy A., Sivaprakash P., Rahman P.K.S.M., Gopalakrishnan A.V., Siama Z., Vellingiri B. Novel wastewater surveillance strategy for early detection of coronavirus disease 2019 hotspots. Curr. Opin. Environ. Sci. Heal. 2020;17:8–13. doi: 10.1016/j.coesh.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.SanJuan-Reyes S., Gómez-Oliván L.M., Islas-Flores H. COVID-19 in the environment. Chemosphere. 2020:127973. doi: 10.1016/j.chemosphere.2020.127973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bivins A., North D., Ahmad A., Ahmed W., Alm E., Been F., Bhattacharya P., Bijlsma L., Boehm A.B., Brown J., Buttiglieri G., Calabro V., Carducci A., Castiglioni S., Cetecioglu Gurol Z., Chakraborty S., Costa F., Curcio S., de los Reyes F.L., Delgado Vela J., Farkas K., Fernandez-Casi X., Gerba C., Gerrity D., Girones R., Gonzalez R., Haramoto E., Harris A., Holden P.A., Islam M.T., Jones D.L., Kasprzyk-Hordern B., Kitajima M., Kotlarz N., Kumar M., Kuroda K., La Rosa G., Malpei F., Mautus M., McLellan S.L., Medema G., Meschke J.S., Mueller J., Newton R.J., Nilsson D., Noble R.T., van Nuijs A., Peccia J., Perkins T.A., Pickering A.J., Rose J., Sanchez G., Smith A., Stadler L., Stauber C., Thomas K., van der Voorn T., Wigginton K., Zhu K., Bibby K. Wastewater-based epidemiology: global collaborative to maximize contributions in the fight against COVID-19. Environ. Sci. Technol. 2020;54:7754–7757. doi: 10.1021/acs.est.0c02388. [DOI] [PubMed] [Google Scholar]
- 68.Zhang N., Gong Y., Meng F., Bi Y., Yang P., Wang F. Virus shedding patterns in nasopharyngeal and fecal specimens of COVID-19 patients. MedRxiv. 2020;2020 doi: 10.1101/2020.03.28.20043059. 03.28.20043059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang J., Wang S., Xue Y. Fecal specimen diagnosis 2019 novel coronavirus–infected pneumonia. J. Med. Virol. 2020;92:680–682. doi: 10.1002/jmv.25742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tang A., Tong Z., Wang H., Dai Y., Li K., Liu J., Wu W., Yuan C., Yu M., Li P., Yan J. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg. Infect. Dis. J. 2020;26 doi: 10.3201/eid2606.200301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thompson J.R., Nancharaiah Y.V., Gu X., Lee W.L., Rajal V.B., Haines M.B., Girones R., Ng L.C., Alm E.J., Wuertz S. Making waves: wastewater surveillance of SARS-CoV-2 for population-based health management. Water Res. 2020;184:116181. doi: 10.1016/j.watres.2020.116181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Graham K., Loeb S., Wolfe M., Catoe D., Sinnott-Armstrong N., Kim S., Yamahara K., Sassoubre L., Mendoza L., Roldan-Hernandez L., Li L., Wigginton K., Boehm A. SARS-CoV-2 in wastewater settled solids is associated with COVID-19 cases in a large urban sewershed. MedRxiv. 2020;2020 doi: 10.1101/2020.09.14.20194472. 09.14.20194472. [DOI] [Google Scholar]
- 73.Wurtzer S., Marechal V., Mouchel J.-M., Maday Y., Teyssou R., Richard E., Almayrac J.L., Moulin L. Evaluation of lockdown impact on SARS-CoV-2 dynamics through viral genome quantification in Paris wastewaters. MedRxiv. 2020;2020 doi: 10.1101/2020.04.12.20062679. 04.12.20062679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hata A., Honda R. Potential sensitivity of wastewater monitoring for SARS-CoV-2: comparison with norovirus cases. Environ. Sci. Technol. 2020;54:6451–6452. doi: 10.1021/acs.est.0c02271. [DOI] [PubMed] [Google Scholar]
- 75.Vogels C.B.F., Brito A.F., Wyllie A.L., Fauver J.R., Ott I.M., Kalinich C.C., Petrone M.E., Casanovas-Massana A., Muenker M.C., Moore A.J., Klein J., Lu P., Lu-Culligan A., Jiang X., Kim D.J., Kudo E., Mao T., Moriyama M., Oh J.E., Park A., Silva J., Song E., Takehashi T., Taura M., Tokuyama M., Venkataraman A., Weizman O.-E., Wong P., Yang Y., Cheemarla N.R., White E., Lapidus S., Earnest R., Geng B., Vijayakumar P., Odio C., Fournier J., Bermejo S., Farhadian S., Dela Cruz C., Iwasaki A., Ko A.I., Landry M.-L., Foxman E.F., Grubaugh N.D. Analytical sensitivity and efficiency comparisons of SARS-COV-2 qRT-PCR primer-probe sets. MedRxiv. 2020;2020 doi: 10.1101/2020.03.30.20048108. 03.30.20048108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jung Y.J., Park G.-S., Moon J.H., Ku K., Beak S.-H., Kim S., Park E.C., Park D., Lee J.-H., Byeon C.W., Lee J.J., Maeng J.-S., Kim S.J., Il Kim S., Kim B.-T., Lee M.J., Kim H.G. Comparative analysis of primer-probe sets for the laboratory confirmation of SARS-CoV-2. BioRxiv. 2020;2020 doi: 10.1101/2020.02.25.964775. 02.25.964775. [DOI] [PubMed] [Google Scholar]
- 77.Amoah I.D., Kumari S., Bux F. Coronaviruses in wastewater processes: source, fate and potential risks. Environ. Int. 2020;143:105962. doi: 10.1016/j.envint.2020.105962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Salipante S.J., Jerome K.R. Digital PCR—an emerging technology with broad applications in microbiology. Clin. Chem. 2019;66:117–123. doi: 10.1373/clinchem.2019.304048. [DOI] [PubMed] [Google Scholar]
- 79.Gunnarsdottir M.J., Gardarsson S.M., Figueras M.J., Puigdomènech C., Juárez R., Saucedo G., Arnedo M.J., Santos R., Monteiro S., Avery L., Pagaling E., Allan R., Abel C., Eglitis J., Hambsch B., Hügler M., Rajkovic A., Smigic N., Udovicki B., Albrechtsen H.-J., López-Avilés A., Hunter P. Water safety plan enhancements with improved drinking water quality detection techniques. Sci. Total Environ. 2020;698:134185. doi: 10.1016/j.scitotenv.2019.134185. [DOI] [PubMed] [Google Scholar]
- 80.Liao S.-C., Peng J., Mauk M.G., Awasthi S., Song J., Friedman H., Bau H.H., Liu C. Smart cup: a minimally-instrumented, smartphone-based point-of-care molecular diagnostic device. Sens. Actuators B Chem. 2016;229:232–238. doi: 10.1016/j.snb.2016.01.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rong Z., Wang Q., Sun N., Jia X., Wang K., Xiao R., Wang S. Smartphone-based fluorescent lateral flow immunoassay platform for highly sensitive point-of-care detection of Zika virus nonstructural protein 1. Anal. Chim. Acta. 2019;1055:140–147. doi: 10.1016/j.aca.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 82.Bhardwaj N., Bhardwaj S.K., Bhatt D., Lim D.K., Kim K.-H., Deep A. Optical detection of waterborne pathogens using nanomaterials. TrAC Trends Anal. Chem. 2019;113:280–300. doi: 10.1016/j.trac.2019.02.019. [DOI] [Google Scholar]
- 83.Wathore R., Gupta A., Bherwani H., Labhasetwar N. Understanding air and water borne transmission and survival of coronavirus: insights and way forward for SARS-CoV-2. Sci. Total Environ. 2020;749:141486. doi: 10.1016/j.scitotenv.2020.141486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim D., Lee J.-Y., Yang J.-S., Kim J.W., Kim V.N., Chang H. The architecture of SARS-CoV-2 transcriptome. Cell. 2020;181:914–921. doi: 10.1016/j.cell.2020.04.011. e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Prado T., de Castro Bruni A., Barbosa M.R.F., Garcia S.C., de Jesus Melo A.M., Sato M.I.Z. Performance of wastewater reclamation systems in enteric virus removal. Sci. Total Environ. 2019;678:33–42. doi: 10.1016/j.scitotenv.2019.04.435. [DOI] [PubMed] [Google Scholar]
- 86.Delanka-Pedige H.M.K., Cheng X., Munasinghe-Arachchige S.P., Abeysiriwardana-Arachchige I.S.A., Xu J., Nirmalakhandan N., Zhang Y. Metagenomic insights into virus removal performance of an algal-based wastewater treatment system utilizing Galdieria sulphuraria. Algal Res. 2020;47:101865. doi: 10.1016/j.algal.2020.101865. [DOI] [Google Scholar]
- 87.Samineni L., Xiong B., Chowdhury R., Pei A., Kuehster L., Wang H., Dickey R., Soto P.E., Massenburg L., Nguyen T.H., Maranas C., Velegol D., Kumar M., Velegol S. 7 log virus removal in a simple functionalized sand filter. Environ. Sci. Technol. 2019;53:12706–12714. doi: 10.1021/acs.est.9b03734. [DOI] [PubMed] [Google Scholar]
- 88.Sigmon C., Shin G.-A., Mieog J., Linden K.G. Establishing surrogate–virus relationships for ozone disinfection of wastewater. Environ. Eng. Sci. 2015;32:451–460. doi: 10.1089/ees.2014.0496. [DOI] [Google Scholar]
- 89.Simhon A., Pileggi V., Flemming C.A., Bicudo J.R., Lai G., Manoharan M. Enteric viruses in municipal wastewater effluent before and after disinfection with chlorine and ultraviolet light. J. Water Health. 2019;17:670–682. doi: 10.2166/wh.2019.111. [DOI] [PubMed] [Google Scholar]
- 90.Verbyla M.E., Mihelcic J.R. A review of virus removal in wastewater treatment pond systems. Water Res. 2015;71:107–124. doi: 10.1016/j.watres.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 91.CDC . 2020. Water and COVID-19 FAQs Information About Drinking Water, Treated Recreational Water, and Wastewater. [Google Scholar]
- 92.Wang J., Feng H., Zhang S., Ni Z., Ni L., Chen Y., Zhuo L., Zhong Z., Qu T. SARS-CoV-2 RNA detection of hospital isolation wards hygiene monitoring during the Coronavirus Disease 2019 outbreak in a Chinese hospital. Int. J. Infect. Dis. 2020;94:103–106. doi: 10.1016/j.ijid.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mohamad Mazuki N.I., Teow Y.H., Ho K.C., Mohammad A.W. Techno-economic analysis of single disinfection units and integrated disinfection systems for sewage effluent reclamation. J. Water Process Eng. 2020;36:101398. doi: 10.1016/j.jwpe.2020.101398. [DOI] [Google Scholar]
- 94.Gerba C.P., Betancourt W.Q., Kitajima M. How much reduction of virus is needed for recycled water: A continuous changing need for assessment? Water Res. 2017;108:25–31. doi: 10.1016/j.watres.2016.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Siddiqui R., Khamis M., Ibrahim T., Khan N.A. SARS-CoV-2: the increasing importance of water filtration against highly pathogenic microbes. ACS Chem. Neurosci. 2020;11:2482–2484. doi: 10.1021/acschemneuro.0c00468. [DOI] [PubMed] [Google Scholar]
- 96.Zhang D., Ling H., Huang X., Li J., Li W., Yi C., Zhang T., Jiang Y., He Y., Deng S., Zhang X., Wang X., Liu Y., Li G., Qu J. Potential spreading risks and disinfection challenges of medical wastewater by the presence of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) viral RNA in septic tanks of Fangcang Hospital. Sci. Total Environ. 2020;741:140445. doi: 10.1016/j.scitotenv.2020.140445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Le Ferrand H. How can materials science contribute to fighting against the new coronavirus? MRS Bull. 2020;45:327–330. doi: 10.1557/mrs.2020.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Faisal A.A.H., Al-Wakel S.F.A., Assi H.A., Naji L.A., Naushad M. Waterworks sludge-filter sand permeable reactive barrier for removal of toxic lead ions from contaminated groundwater. J. Water Process Eng. 2020;33:101112. doi: 10.1016/j.jwpe.2019.101112. [DOI] [Google Scholar]
- 99.Muthusaravanan S., Sivarajasekar N., Vivek J.S., Paramasivan T., Naushad M., Prakashmaran J., Gayathri V., Al-Duaij O.K. Phytoremediation of heavy metals: mechanisms, methods and enhancements. Environ. Chem. Lett. 2018;16:1339–1359. doi: 10.1007/s10311-018-0762-3. [DOI] [Google Scholar]
- 100.Carolin C.F., Kumar P.S., Saravanan A., Joshiba G.J., Naushad M. Efficient techniques for the removal of toxic heavy metals from aquatic environment: a review. J. Environ. Chem. Eng. 2017;5 doi: 10.1016/j.jece.2017.05.029. [DOI] [Google Scholar]
- 101.Chung Y.T., Mahmoudi E., Mohammad A.W., Benamor A., Johnson D., Hilal N. Development of polysulfone-nanohybrid membranes using ZnO-GO composite for enhanced antifouling and antibacterial control. Desalination. 2017;402:123–132. doi: 10.1016/j.desal.2016.09.030. [DOI] [Google Scholar]
- 102.Shahat A., Awual M.R., Khaleque M.A., Alam M.Z., Naushad M., Chowdhury A.M.S. Large-pore diameter nano-adsorbent and its application for rapid lead(II) detection and removal from aqueous media. Chem. Eng. J. 2015;273:286–295. doi: 10.1016/j.cej.2015.03.073. [DOI] [Google Scholar]
- 103.Naushad M. Surfactant assisted nano-composite cation exchanger: development, characterization and applications for the removal of toxic Pb2+ from aqueous medium. Chem. Eng. J. 2014;235:100–108. doi: 10.1016/J.CEJ.2013.09.013. [DOI] [Google Scholar]
- 104.Bakather O.Y., Kayvani Fard A., Ihsanullah, Khraisheh M., Nasser M.S., Atieh M.A. Enhanced adsorption of selenium ions from aqueous solution using Iron oxide impregnated carbon nanotubes. Bioinorg. Chem. Appl. 2017;2017 doi: 10.1155/2017/4323619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Asmaly H.A., Abussaud B., Ihsanullah, Saleh T.A., Alaadin A., Laoui T., Shemsi A.M., Gupta V.K., Atieh M.A., Asmaly H.A., Abussaud B., Saleh T.A., Alaadin A. Evaluation of micro- and nano-carbon-based adsorbents for the removal of phenol from aqueous solutions. Toxicol. Environ. Chem. 2015;97:1164–1179. doi: 10.1080/02772248.2015.1092543. [DOI] [Google Scholar]
- 106.Ihsanullah I. MXenes (two-dimensional metal carbides) as emerging nanomaterials for water purification: progress, challenges and prospects. Chem. Eng. J. 2020;388:124340. doi: 10.1016/j.cej.2020.124340. [DOI] [Google Scholar]
- 107.Khan S.T., Malik A. Engineered nanomaterials for water decontamination and purification: from lab to products. J. Hazard. Mater. 2019;363:295–308. doi: 10.1016/j.jhazmat.2018.09.091. [DOI] [PubMed] [Google Scholar]
- 108.Ojha A. In: Waterborne Pathog. Detect. Treat. Vara Prasad M.N., Grobelak A.B.T.-W.P., editors. Butterworth-Heinemann; 2020. Nanomaterials for removal of waterborne pathogens: opportunities and challenges; pp. 385–432. [DOI] [Google Scholar]
- 109.Hossain F., Perales-Perez Oscar J., Hwang S., Román F. Antimicrobial nanomaterials as water disinfectant: applications, limitations and future perspectives. Sci. Total Environ. 2014;466–467:1047–1059. doi: 10.1016/j.scitotenv.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 110.Salleh A., Naomi R., Utami N.D., Mohammad A.W., Mahmoudi E., Mustafa N., Fauzi M.B. The potential of silver nanoparticles for antiviral and antibacterial applications: a mechanism of action. Nanomaterial. 2020;10 doi: 10.3390/nano10081566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Fiksdal L., Leiknes T. The effect of coagulation with MF/UF membrane filtration for the removal of virus in drinking water. J. Memb. Sci. 2006;279:364–371. doi: 10.1016/j.memsci.2005.12.023. [DOI] [Google Scholar]
- 112.Zodrow K., Brunet L., Mahendra S., Li D., Zhang A., Li Q., Alvarez P.J.J. Polysulfone ultrafiltration membranes impregnated with silver nanoparticles show improved biofouling resistance and virus removal. Water Res. 2009;43:715–723. doi: 10.1016/j.watres.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 113.Chaudhry R.M., Nelson K.L., Drewes J.E. Mechanisms of pathogenic virus removal in a full-scale membrane bioreactor. Environ. Sci. Technol. 2015;49:2815–2822. doi: 10.1021/es505332n. [DOI] [PubMed] [Google Scholar]
- 114.Zheng X., Wang Q., Chen L., Wang J., Cheng R. Photocatalytic membrane reactor (PMR) for virus removal in water: performance and mechanisms. Chem. Eng. J. 2015;277:124–129. doi: 10.1016/j.cej.2015.04.117. [DOI] [Google Scholar]
- 115.Al-Attabi R., Rodriguez-Andres J., Schütz J.A., Bechelany M., des Ligneris E., Chen X., Kong L., Morsi Y.S., Dumée L.F. Catalytic electrospun nano-composite membranes for virus capture and remediation. Sep. Purif. Technol. 2019;229:115806. doi: 10.1016/j.seppur.2019.115806. [DOI] [Google Scholar]
- 116.Schlosser O., Robert C., Bourderioux C., Rey M., de Roubin M.R. Bacterial removal from inexpensive portable water treatment systems for travelers. J. Travel Med. 2006;8:12–18. doi: 10.2310/7060.2001.5143. [DOI] [PubMed] [Google Scholar]
- 117.Tang L., Liu M., Ren B., Wu Z., Yu X., Peng C., Tian J. Sunlight ultraviolet radiation dose is negatively correlated with the percent positive of SARS-CoV-2 and four other common human coronaviruses in the U.S. Sci. Total Environ. 2021;751:141816. doi: 10.1016/j.scitotenv.2020.141816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gormley M., Aspray T.J., Kelly D.A. COVID-19: mitigating transmission via wastewater plumbing systems. Lancet Glob. Heal. 2020;8:e643. doi: 10.1016/S2214-109X(20)30112-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhang H., Tang W., Chen Y., Yin W. Disinfection threatens aquatic ecosystems. Science (80-.) 2020;368:146–147. doi: 10.1126/science.abb8905. [DOI] [PubMed] [Google Scholar]
- 120.Klemeš J.J., Van Fan Y., Jiang P. The energy and environmental footprints of COVID-19 fighting measures – PPE, disinfection, supply chains. Energy. 2020;211:118701. doi: 10.1016/j.energy.2020.118701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Quintuña D.M.J. SSRN; 2020. Estimated Impact of COVID-19 on Water Needs and Volume and Quality of Wastewater. (n.d.) July 15. [Google Scholar]
- 122.Mahmood A., Eqan M., Pervez S., Alghamdi H.A., Tabinda A.B., Yasar A., Brindhadevi K., Pugazhendhi A. COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. Sci. Total Environ. 2020;742:140561. doi: 10.1016/j.scitotenv.2020.140561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang B., Zhai R., Ma L. 2019 novel coronavirus disease epidemic: skin protection for healthcare workers must not be ignored. J. Eur. Acad. Dermatol. Venereol. 2020;34(9):e434–e435. doi: 10.1111/jdv.16573. n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nabi G., Wang Y., Hao Y., Khan S., Wu Y., Li D. Massive use of disinfectants against COVID-19 poses potential risks to urban wildlife. Environ. Res. 2020;188:109916. doi: 10.1016/j.envres.2020.109916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Green H., Wilder M., Middleton F.A., Collins M., Fenty A., Gentile K., Kmush B., Zeng T., Larsen D.A. Quantification of SARS-CoV-2 and cross-assembly phage (crAssphage) from wastewater to monitor coronavirus transmission within communities. MedRxiv. 2020;2020 doi: 10.1101/2020.05.21.20109181. 05.21.20109181. [DOI] [Google Scholar]
- 126.Bar Or I., Yaniv K., Shagan M., Ozer E., Erster O., Mendelson E., Mannasse B., Shirazi R., Kramarsky-Winter E., Nir O., Abu-Ali H., Ronen Z., Rinott E., Lewis Y.E., Friedler E.F., Paitan Y., Bitkover E., Berchenko Y., Kushmaro A. Regressing SARS-CoV-2 sewage measurements onto COVID-19 burden in the population: a proof-of-concept for quantitative environmental surveillance. MedRxiv. 2020;2020 doi: 10.1101/2020.04.26.20073569. 04.26.20073569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Randazzo W., Cuevas-Ferrando E., Sanjuan R., Domingo-Calap P., Sanchez G. Metropolitan wastewater analysis for COVID-19 epidemiological surveillance. MedRxiv. 2020;2020 doi: 10.1101/2020.04.23.20076679. 04.23.20076679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Haramoto E., Malla B., Thakali O., Kitajima M. First environmental surveillance for the presence of SARS-CoV-2 RNA in wastewater and river water in Japan. Sci. Total Environ. 2020;737:140405. doi: 10.1016/j.scitotenv.2020.140405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Hata A., Honda R., Hara-Yamamura H., Meuchi Y. Detection of SARS-CoV-2 in wastewater in Japan by multiple molecular assays-implication for wastewater-based epidemiology (WBE) MedRxiv. 2020;2020 doi: 10.1101/2020.06.09.20126417. 06.09.20126417. [DOI] [Google Scholar]
- 130.Balboa S., Mauricio-Iglesias M., Rodríguez S., Martínez-Lamas L., Vasallo F.J., Regueiro B., Lema J.M. The fate of SARS-CoV-2 in wastewater treatment plants points out the sludge line as a suitable spot for incidence monitoring. MedRxiv. 2020;2020 doi: 10.1101/2020.05.25.20112706. 05.25.20112706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Arora S., Nag A., Sethi J., Rajvanshi J., Saxena S., Shrivastava S.K., Gupta A.B. Sewage surveillance for the presence of SARS-CoV-2 genome as a useful wastewater based epidemiology (WBE) tracking tool in India. MedRxiv. 2020;2020 doi: 10.1101/2020.06.18.20135277. 06.18.20135277. [DOI] [PubMed] [Google Scholar]
- 132.Sharif S., Ikram A., Khurshid A., Salman M., Mehmood N., Arshad Y., Ahmad J., Angez M., Alam M.M., Rehman L., Mujtaba G., Hussain J., Ali J., Akthar Ri., Malik M.W., Baig Z.I., Rana M.S., Usman M., Ali M.Q., Ahad A., Badar N., Umair M., Tamim S., Ashraf A., Tahir F., Ali N. Detection of SARS-Coronavirus-2 in wastewater, using the existing environmental surveillance network: an epidemiological gateway to an early warning for COVID-19 in communities. MedRxiv. 2020;2020 doi: 10.1101/2020.06.03.20121426. 06.03.20121426. [DOI] [Google Scholar]
- 133.Sherchan S.P., Shahin S., Ward L.M., Tandukar S., Aw T.G., Schmitz B., Ahmed W., Kitajima M. First detection of SARS-CoV-2 RNA in wastewater in North America: a study in Louisiana, USA. Sci. Total Environ. 2020;743:140621. doi: 10.1016/j.scitotenv.2020.140621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mlejnkova H., Sovova K., Vasickova P., Ocenaskova V., Jasikova L., Juranova E. Preliminary study of Sars-Cov-2 occurrence in wastewater in the Czech Republic. Int. J. Environ. Res. Public Heal. 2020;17 doi: 10.3390/ijerph17155508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Westhaus S., Weber F.-A., Schiwy S., Linnemann V., Brinkmann M., Widera M., Greve C., Janke A., Hollert H., Wintgens T., Ciesek S. Detection of SARS-CoV-2 in raw and treated wastewater in Germany – suitability for COVID-19 surveillance and potential transmission risks. Sci. Total Environ. 2021;751:141750. doi: 10.1016/j.scitotenv.2020.141750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Trottier J., Darques R., Ait Mouheb N., Partiot E., Bakhache W., Deffieu M.S., Gaudin R. Post-lockdown detection of SARS-CoV-2 RNA in the wastewater of Montpellier, France. One Heal. 2020;10:100157. doi: 10.1016/j.onehlt.2020.100157. [DOI] [PMC free article] [PubMed] [Google Scholar]