Abstract
Although stigma is a major barrier to treatment for those with mental health concerns, it is poorly understood when stigma is more or less influential in mental health treatment decisions. In the current work, we examined whether psychological distance – the removal of an event from direct experience – reduced the influence of internalized stigma on willingness to seek treatment. Specifically, we tested the hypothesis that psychological distance versus proximity (e.g., seeking treatment in three months vs. in two days, respectively) decreases the negative influence of stigma on willingness to seek treatment. We focused on a population for whom mental health treatment decisions are personally-relevant: individuals who had previously sought mental health treatment. Experiment 1 showed that the extent to which these individuals internalized (i.e., personally endorsed) stigma about mental illness predicted lower intentions to make an appointment with a mental health care provider for themselves (but not another person). Experiment 2 replicated this result using a different measure of psychological distance (temporal distance) and extended this finding to behavior (time spent reading mental health resources). Overall, this research demonstrated that internalized stigma disrupts mental health treatment-seeking intentions and behaviors when they are psychologically proximal, but not when they are distant. Potential applications of these results are discussed.
Keywords: social stigma, social distance, help-seeking behavior, mental health, clinical decision-making, prejudice, patient health questionnaire
Mental health services under-utilization is a major public health concern. Although approximately 18 percent of adults in the United States suffer from mental illness (Center for Behavioral Health Statistics and Quality [CBHSQ], 2015a), nearly two-thirds of them do not seek mental health treatment (Han, Hedden, Lipari, Copello, & Kroutil, 2015). There are numerous reasons why individuals suffering from mental illness do not seek treatment, including concerns associated with cost, time, and access to treatment (Han et al., 2015). However, the fear of being discriminated against (i.e., stigmatized) is one of the most significant barriers to treatment (CBHSQ, 2015b). Indeed, recent work shows that higher stigma is associated with greater perceptions of other barriers to treatment (e.g., structural barriers such as cost; Arnaez, Krendl, McCormick, Chen, & Chomistek, 2019). Although much work has focused on stigma-reduction interventions, these have had mixed success (Dalky, 2012; Griffiths, Carron-Arthur, Parsons, & Reid, 2014; Thornicroft et al., 2016). An alternative strategy is to uncouple the negative influence of stigma on treatment decisions. The goal of the current work was to provide a theoretical test of this possibility that were informed by the social psychological literature.
Stigma about mental illness can be characterized in two ways (Corrigan, 2004; Rüsch, Angermeyer, & Corrigan, 2005): the perceived negative beliefs of the general public towards those with mental illness (Link, 1987), and the extent to which these negative beliefs are then internalized (i.e., personally endorsed; Ritsher, Otilingam, & Grajales, 2003). Perhaps because individuals may not necessarily endorse the stigmas of which they are aware (Devine, 1989), the extent to which individuals internalize stigma about mental illness, in particular, predicts reduced treatment-seeking (Bathje & Pryor, 2011; Clement et al., 2015; Eisenberg, Downs, Golberstein, & Zivin, 2009; Lannin, Vogel, Brenner, Abraham, & Heath, 2016). For instance, higher baseline internalized stigma predicted worse psychological outcomes (e.g., higher symptomology) in treatment-seeking samples over the next 4–12 months (Oexle et al., 2018; Ritsher & Phelan, 2004). Internalized stigma also predicts reduced engagement in unobservable mental health care behaviors (e.g., searching online for mental health resources; Lannin et al., 2016). The latter point suggests that internalized stigma interferes with treatment-seeking even if the fear of discrimination by others is not present. For this reason, we chose to focus on individuals’ internalized stigma of mental illness. It is important to note that while help-seeking also stigmatized (Vogel, Wade, & Ascheman, 2009; Vogel, Wade, & Haake, 2006) and related to internalized stigma about mental illness, prior work suggests these are conceptually distinct (Tucker, Vogel, Bitman, & Wade, 2013).
Despite the fact that internalizing stigma about mental illness interferes with initiating and adhering to mental health treatment (Corrigan, 2004; Livingston & Boyd, 2010), individuals do, at times, seek treatment despite their stigma concerns. Indeed, individuals with high internalized stigma comprise a significant proportion of those in outpatient treatment (Picco et al., 2016; Ritsher & Phelan, 2004). This finding suggests that stigma may be a transient, but not sustained, barrier to treatment. In other words, stigma may exert a more powerful influence on decisions to seek treatment at different points in the decision-making process. This is an important question to answer because interventions are more effective when deployed under the right circumstances (Walton, 2014). Thus, understanding whether stigma is a temporary or sustained barrier to treatment could inform when to intervene to reduce the negative effect of stigma on treatment decisions.
To manipulate the influence of stigma on treatment decisions, we relied on a well-established phenomenon from social psychology: psychological distance (i.e., removing an event from direct experience; Trope & Liberman, 2010). Psychological distance, relative to proximity, promotes making decisions and enacting behaviors that may be onerous, yet provide valued benefits (e.g., saving for retirement; Ainslie, 1975; Eyal, Sagristano, Trope, Liberman, & Chaiken, 2009; Pronin, Olivola, & Kennedy, 2008; Rogers & Bazerman, 2008; Thaler & Benartzi, 2004). Psychological distance has been manipulated in several ways (e.g., social, temporal, spatial) with similar psychological effects (Bar-Anan, Liberman, & Trope, 2006; Liberman & Trope, 2014). One explanation as to why individuals are more likely to commit to psychologically distant behaviors is that they are less sensitive to the negative consequences associated with enacting onerous behaviors (Cacioppo & Berntson, 1994; Eyal, Liberman, Trope, & Walther, 2004; Miller, 1944). For example, Miller (1944) found that sensitivity to negativity increases (decreases) as a function of spatial proximity (distance), while Eyal et al. (2004) and others (Pennington & Roese, 2003) report similar findings regarding temporal proximity versus distance. Psychological distance – regardless of its manifestation – appears to diminish the impact of negativity (relative to positivity) on decisions. In the mental health context, stigma may be viewed as a negative consequence of seeking treatment (e.g., Vogel, Wester, & Larson, 2007), and thus have less impact on psychologically distant (vs. proximal) treatment decisions.
In the current work, we employed two of the most well-understood dimensions of the psychological distance: (1) social distance (e.g., the likelihood you would enact a behavior or someone else would; Pronin, Olivola, & Kennedy, 2008), and (2) temporal distance (e.g., the likelihood of enacting a behavior in one week or one year; Liberman, Sagristano, & Trope, 2002; Liberman & Trope, 1998). Although we predicted that different dimensions of distance would have similar effects (Bar-Anan et al., 2006; Liberman & Trope, 2014), confirming this generalizability had the added benefit of implicating multiple routes for future intervention on individuals’ treatment-seeking. We chose to first examine social distance because prior research has found a disparity between what individuals recommend for others versus do themselves (Danziger, Montal, & Barkan, 2012; Howell, Sweeny, & Shepperd, 2014; Pronin et al., 2008). This disparity can be explained, at least in part, by individuals’ greater emphasis on pros vs. cons of behaviors when making recommendations to others (vs. own choices; Danziger et al., 2012). To the extent that internalized stigma is perceived as a negative consequence of seeking mental health treatment, it should be lesser emphasized in treatment decisions with increased social distance. We established this effect in Experiment 1 by manipulating social distance and conducted a conceptual replication using temporal distance in Experiment 2. Temporal distance is a natural extension of social distance because individuals are similarly less likely to enact demanding behaviors in the near versus distant future (e.g., within 2 weeks vs. next semester; Howell et al., 2014). Temporal distance may thus have clinical implications and ecological validity for patients’ decisions about when to seek treatment (e.g., Wang et al., 2007). The conceptual replication in Experiment 2 confirmed the broader theoretical framework of psychological distance. It was also designed to provide evidence that internalized stigma not only influences treatment intentions (Experiment 1) but also a behavior (time spent reading mental health resources) that may inform treatment decisions.
An additional goal of Experiment 1 was to identify the population for which psychological distance had the largest impact. We anticipated that individuals who had (versus who did not have) prior mental health treatment experience would benefit the most from this manipulation. This prediction was based on prior work from our lab that suggested that this population was more likely to find treatment-seeking to be personally-relevant.1 That is, individuals are unlikely to respond to an intervention promoting them to seek mental health treatment if they do not find treatment relevant to their situation. By identifying among whom the psychological distance manipulation is effective at reducing the influence of stigma on treatment intentions, we will be able to better tailor future interventions (Walton, 2014). Finally, to generalize our results across sample types, the two experiments presented here were conducted with college undergraduate (Experiment 1) and online community (Experiment 2) samples.
Experiment 1
We first examined whether manipulating social distance (Soderberg et al., 2015; Trope & Liberman, 2010) affected the negative impact of internalized stigma on mental health treatment decisions. We manipulated social distance by asking undergraduate students to estimate the likelihood that they (socially proximal condition) or another person (socially distant condition) would make an appointment with a mental health care provider (Danziger, Montal, & Barkan, 2012; Howell, Sweeny, & Shepperd, 2014). This manipulation is commonly used to understand how making a decision from another person’s perspective makes negative barriers to enacting behaviors less psychological salient (Danziger et al., 2012; Soderberg et al., 2015; Trope & Liberman, 2010). We thus hypothesized that internalized stigma would predict lower treatment intentions in the socially proximal, but not distant, condition. This finding would establish that psychological distance – elicited by considering others’ decisions – uncoupled the influence of internalized stigma on decisions. An alternate possibility was that internalized stigma might, in general, be unrelated to decisions made for others because of the mismatch between who holds the belief (internalized stigma) and who enacts the behavior (seeking treatment). However, past work has shown that individuals have difficulty adjusting for their own perspective when considering another person’s perspective (Epley, 2008; Eyal, Steffel, & Epley, 2018). This finding suggests that own stigma beliefs could plausibly relate to socially distant treatment intentions.
Experiment 1 was also designed to test our hypothesis that the effect of psychological distance would be most pronounced among individuals for whom the target behavior (i.e., treatment-seeking) was personally-relevant (e.g., individuals with any prior mental health treatment experience). We examined this hypothesis in Experiment 1 among undergraduates at a large Midwestern university. This population was relevant to our research question because, even though depression rates are most prevalent among this population (CBHSQ, 2015b), they are less likely seek treatment at a lower rate compared to other age groups (Han et al., 2015).
Method
Participants
A recent meta-analysis estimated that psychological distance elicits a moderate effect size on outcome intentions and behaviors (Soderberg et al., 2015). An a priori power analysis in G*Power (Faul, Erdfelder, Lang, & Buchner, 2007) identified a target sample of N = 89 to detect a moderate interaction effect size (f2 = .15; Perugini et al., 2018) with 95% power and α = .05. Because we wanted to identify participants who had previously sought treatment, we oversampled in order to ensure we recruited a sufficient number of participants. In total, 293 undergraduates from a large Midwestern university participated in exchange for course credit. Data from 19 participants was excluded because they did not complete the manipulation and/or stigma measure. The sample of 274 participants consisted of undergraduates between the ages of 18 and 41 (Mage = 19.50, SDage = 2.14, 3 participants did not report their age), and 186 participants were female (67.9%). Most participants identified as White (71.5%), Black/African-American (10.9%), or Asian (10.6%). Of the 73 participants (27%) who had previously sought mental health treatment, participants’ ages ranged between 18 and 24 (Mage = 19.40, SDage = 1.45, 1 participant did not report their age), 56 participants (76.7%) were female, and most were White (82.2%; 5.5% Black/African-American, 5.5% Asian). The experiment was carried out with approval from the Institutional Review Board at Indiana University, and all participants gave informed consent for their data to be used in the research.
Materials and Procedure
Participants were randomly assigned to either the socially proximal condition or socially distant condition. First, participants were instructed to imagine they (proximal condition) or their classmate (distant condition) had the opportunity to “visit a physician for a free mental health exam.” In the socially proximal condition, participants were asked: “How likely are you to set up an appointment with a mental health care provider?” on a 7-point scale from 1 (very unlikely) to 7 (very likely). In the socially distant condition, participants indicated the likelihood that a classmate they knew “fairly but not extremely well” would be to engage in the same behavior using the same scale.
Next, participants completed a modified version of the Internalized Stigma of Mental Illness (ISMI) Scale (Ritsher et al., 2003) that measured the extent that individuals would stigmatize themselves for having a mental illness. Because the original version was intended for people with mental illness (e.g., “I am embarrassed or ashamed that I have a mental illness”), we modified the wording of 16 of the original 29 items to generalize to a broader population (e.g., “I would be embarrassed or ashamed if I had a mental illness”).2 Items that could not be modified (e.g., pertaining to having experienced discrimination due to one’s mental illness) were excluded. Participants responded to each item on a scale from 1 (strongly disagree) to 4 (strongly agree). The modified ISMI items had good reliability (Cronbach’s α = .87), and were thus summed to create a single measure of internalized stigma. Participants also indicated via self-report (yes or no) whether they had previously sought mental health treatment, whether they had ever been diagnosed with depression or an anxiety disorder (the two most common mental illnesses in the United States; CBHSQ, 2015a), and if they were currently taking antidepressant medication. Finally, participants reported their depression symptoms over the past two weeks on the 2-item Patient Health Questionnaire (PHQ-2; Kroenke, Spitzer, Williams, & Löwe, 2010), which has a sensitivity of 83% and specificity of 92% for diagnosing major depression (Kroenke, Spitzer, & Williams, 2003). The PHQ-2 items had good reliability among this sample (Cronbach’s α = .83) and were thus summed to create a single measure of current depression symptomology.3
Results
See Table 1 for a full description of the clinical and treatment characteristics (e.g., self-reported diagnoses) of participants who had previously sought mental health treatment. Supporting the distinction based on prior treatment experience, participants who had (M = 4.53, SD = 1.82) versus had not (M = 3.90, SD = 1.93) previously sought mental health treatment had higher intentions to make an appointment with a mental health care provider, t(272) = 2.46, p = .02, d = .33, 95% CI [.06, .60]; and higher current depressive symptomology (had previously sought treatment: M = 2.08, SD = 1.77; had not previously sought treatment: M = 1.11, SD = 1.35), t(272) = 4.83, p < .001, d = .66, 95% CI [.39, .93]. Participants who had previously sought mental health treatment (M = 30.11, SD = 6.95) also had lower internalized stigma relative to those who had not (M = 34.15, SD = 6.54), t(269) = 4.40, p < .001, d = .61, 95% CI [.34, .88]. Of those who had previously sought treatment, the majority self-reported a clinical diagnosis (39.4% reported both depression and anxiety; 17.8% depression, 13.7% anxiety disorder, 30.1% neither) and current anti-depressant use (71.2%; see Table 1).
Table 1.
Clinical and treatment characteristics of participants who had previously sought mental health treatment in Experiment 1 and 2.
| Experiment 1 (N = 73) |
Experiment 2 (N = 245) |
|||
|---|---|---|---|---|
| Characteristics | N | % | N | % |
| Self-reported diagnosis | ||||
| Depression | 13 | 17.81 | 43 | 17.55 |
| Anxiety Disorder | 10 | 13.70 | 26 | 10.61 |
| Both | 28 | 38.36 | 126 | 51.43 |
| Neither | 22 | 30.14 | 50 | 20.41 |
| Self-reported antidepressant use | ||||
| Yes | 52 | 71.20 | 142 | 58 |
| No | 21 | 28.80 | 103 | 42 |
| Source of treatment | ||||
| Mental healthcare provider | - | - | 118 | 48.20 |
| Primary care physician | - | - | 26 | 10.60 |
| Both | - | - | 93 | 38 |
| Other/Unreported | - | - | 8 | 3.30 |
| Most recent treatment contact | - | - | ||
| ≤ 1 year ago | - | - | 111 | 45.30 |
| > 1 year ago & < 5 years ago | - | - | 60 | 24.50 |
| ≥ 5 years ago | - | - | 50 | 20.40 |
| Unreported/Could not be coded | - | - | 24 | 9.80 |
Note. The categories are independent groups. Data on source of treatment and most recent treatment contact was not available for the sample in Experiment 1.
Given these differences, we conducted a hierarchical linear regression to test the hypothesis that previous treatment experience and social distance moderated the effect of internalized stigma on intentions to make an appointment with a mental health care provider. Simply put, we predicted that the social distance manipulation would have a greater impact for individuals with prior treatment experience compared to those without prior treatment experience. Accordingly, we entered current previous treatment experience, social distance condition, and internalized stigma in the first step, corresponding two-way interactions in the second step, and the 3-way interaction between previous treatment experience, social distance condition, and internalized stigma in the third step. Depression symptoms measured by the PHQ-2 were included as a control variable in the first step of the regression.
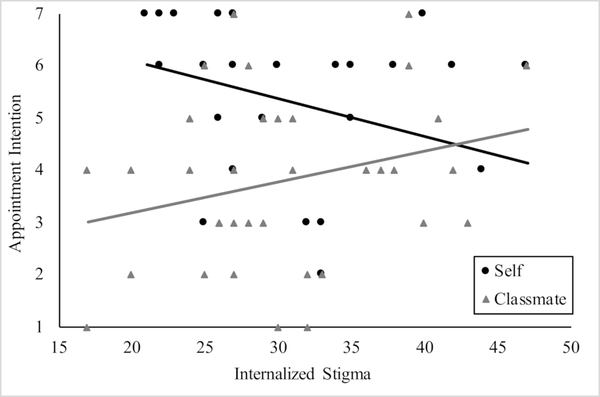
Indeed, the model including the three-way interaction between previous treatment experience, social distance, and internalized stigma was significant and accounted for 15% of the variance in appointment intentions, F(8, 270) = 5.64, p < .001; ΔF(1,262) = 6.01, β = 1.04, p = .015 (see Table 2 for a full description of the model’s results). To unpack this three-way interaction, we conducted a hierarchical linear regression for each subgroup (those who had previously sought treatment vs. had not) to test whether the hypothesized interaction between social distance condition and internalized stigma predicted appointment intentions. Among participants who had not previously sought treatment, the amount of variance explained by the interaction between social distance and stigma was not significant, ΔF(1,195) = .90, p = .35. However, the model was significant among the subgroup of participants who had previously sought treatment; the model including the interaction term accounted for 28% of the variance in the appointment intentions, F(4,70) = 6.44, p < .001; ΔF(1,66) = 6.82, p = .01 (see Table 3). Consistent with our hypothesis, internalized stigma predicted lower appointment intentions for the socially proximal condition (self; β = −.33, p = .08), but not the socially distant condition (classmate; β = .27, p = .09; see Figure 1).1
Table 2.
Summary of hierarchical regression analysis for variables predicting willingness to make an appointment with a mental health care provider in Experiment 1 (N = 274).
| Step 1 | Step 2 | Step 3 | ||||
|---|---|---|---|---|---|---|
| β | t | β | t | β | t | |
| Previous Treatment Experience | .12 | 1.93 | .11 | .40 | .81 | 2.03* |
| Social Distance | −.30 | 5.16** | −.37 | 1.21 | .09 | .24 |
| Internalized Stigma | −.03 | .43 | −.06 | .66 | .02 | .19 |
| Depression Symptoms | .12 | 1.60 | .10 | 1.65 | .12 | 1.90 |
| Treatment Experience X Social Distance | – | – | −.09 | .95 | −1.14 | 2.60* |
| Treatment Experience X Internalized Stigma | – | – | .07 | .26 | −.63 | 1.62 |
| Social Distance X Internalized Stigma | – | – | .11 | .36 | −.35 | .99 |
| Treatment Experience X Social Distance X Internalized Stigma | – | – | – | – | 1.04 | 2.45* |
| F(4,270) = 30.46, p < .001, R2 = .12 | F(7,270) = 18.07, p < .001, R2 = .13 | F(8,270) = 18.24, p < .001, R2 = .15 | ||||
Note. Previous treatment experience (0 = no, 1 = yes) and social distance (0 = self; 1 = classmate) were represented as dummy variables.
p ≤ .05.
p ≤ .001.
Table 3.
Summary of hierarchical regression analysis for variables predicting willingness to make an appointment with a mental health care provider among participants with prior mental health treatment experience in Experiment 1 (N = 73).
| Step 1 | Step 2 | |||
|---|---|---|---|---|
| β | t | β | t | |
| Social Distance | .43 | 3.93** | −1.65 | 3.45** |
| Internalized Stigma | .002 | .02 | −.33 | 2.00* |
| Depression Symptoms | .13 | 1.17 | .18 | 1.64 |
| Social Distance X Internalized Stigma | – | – | 1.29 | 2.61* |
| F(3,70) = 5.81, p = .001, R2 = .21 | F(4,70) = 6.44, p < .001, R2 = .28 | |||
Note. Social distance (0 = self; 1 = classmate) was represented as a dummy variable.
p ≤ .001
p ≤ .05
Figure 1.
Internalized stigma predicted lower appointment intentions in the socially proximal condition (self) relative to the socially distant condition (classmate) in Experiment 1.
Experiment 1 Discussion
Experiment 1 demonstrated that internalized stigma influenced socially proximal, but not distant, treatment intentions. Critically, this effect only emerged among the subgroup of the sample who had previously sought mental health treatment. We found the same pattern of results with a larger online community sample,4 which suggests that this effect is not limited undergraduates. Rather, the fact that participants with prior treatment experience from both undergraduate and online community samples were responsive to psychological distance justified focusing on those individuals in Experiment 2. This finding may have occurred because future treatment was more personally-relevant to individuals with prior experience, as may be evidenced by the fact that they had both higher intentions to seek treatment and higher current depressive symptomology (see also Footnote 1). An important caveat in Experiment 1, however, was that we focused on the effect of psychological distance on treatment intentions. Although intentions are, at times, good predictors of actual behavior (Webb & Sheeran, 2006), the goal of Experiment 2 was to determine whether greater psychological distance reduced the negative impact of stigma on treatment-relevant behaviors. Experiment 2 was also designed to address the theoretical and practical limitations of the social distance manipulation. Based on the broader theoretical framework provided by psychological distance, manipulating different dimensions (e.g., social, temporal) should have similar psychological effects (Bar-Anan et al., 2006; Liberman & Trope, 2014). To test this theoretical premise, we manipulated temporal distance of treatment intentions in Experiment 2 by examining how individuals make treatment decisions given near or distant temporal deadlines. This also had the practical benefit of comparing treatment intentions within the individual (vs. between individuals) who both endorsed internalized stigma and will enact the behavior (treatment-seeking).
Experiment 2
We had two goals in Experiment 2. First, we examined whether manipulating a different dimension of psychological distance (temporal distance) would elicit the same pattern of results that we observed in Experiment 1. In addition to providing a broader theoretical framework for this study, this was important because temporal distance might be more relevant for improving treatment-seeking and adherence. Patients often face the decision about when to seek treatment (Wang et al., 2007), so understanding when stigma influences treatment decisions is more directly relevant for ultimately developing interventions (Walton, 2014). By encouraging individuals to commit to seeking treatment when stigma is less influential (i.e., in advance; (Ariely & Wertenbroch, 2002; Rogers & Bazerman, 2008; Thaler & Benartzi, 2004), we may be able to prevent long delays in eventual initiation of treatment (Wang et al., 2007) due to stigma concerns (e.g., Arnaez, Krendl, McCormick, Chen, & Chomistek, 2019). The second goal of Experiment 2 was to examine whether psychological distance moderated the influence of internalized stigma on a treatment-related behavior: time spent reading mental health resources. We chose this measure because it is a plausible behavioral step for seeking treatment used in other work studying health behaviors and help-seeking (Belding, Naufel, & Fujita, 2015; Lannin et al., 2016). We predicted that internalized stigma would disrupt reading time for participants given a psychologically proximal, but not distant temporal deadline to seek mental health treatment. Based on the results from Experiment 1, Experiment 2 focused only on participants who had previously sought mental health treatment.
Method
Participants
Online community participants were recruited on Amazon Mechanical Turk. Samples from Amazon Mechanical Turk are more demographically diverse (Paolacci & Chandler, 2014) and have comparable data validity and quality to undergraduate samples (Paolacci & Chandler, 2014), and match the prevalence of clinical levels of depression and general anxiety in the United States population (Shapiro, Chandler, & Mueller, 2013). An a priori power analysis in G*Power (Faul et al., 2007) identified a target sample of N = 95 to detect the interaction effect size (Perugini et al., 2018) from Experiment 1 (f2 = .14) with 95% power and α = .05. Because we wanted to identify participants who had previously sought treatment, we oversampled in order to ensure we recruited a sufficient number of participants.
In total, we recruited 289 participants who reported previous mental health treatment experience (see Experiment 1 Method) from Amazon Mechanical Turk in exchange for monetary compensation. Data from 44 participants was excluded for failing at least one attention check question. The final sample of 245 participants (44.4% of total respondents) were between the ages of 19 and 72 (Mage = 35.64, SDage = 11.46), 144 were female (58.8%; 1 person did not report their gender), and most participants identified as White (80.8%), Asian (10.6%), or Black/African-American (4.1%). See Table 1 for a full description of the clinical and treatment characteristics (e.g., self-reported diagnoses) of participants who had previously sought mental health treatment. The experiment was carried out with approval from the Institutional Review Board at Indiana University, and all participants gave informed consent for their data to be used in the research.
Procedure
As a validation of our dependent measure (seeking out resources online), participants completed a pre-test questionnaire at the beginning of the study before the manipulation. The questionnaire asked: “When making mental health decisions, people may consult a variety of sources of information. Where would you get information about mental illness and mental health treatment?” Participants were instructed to select as many sources that apply from a list that included: “a friend,” “a family member,” “the internet (e.g., a web search),” “social media,”, “a book,” “a religious or spiritual leader,” “other”. For the last category, participants could write in any source not listed. The internet was the most commonly selected resource with 83% of participants endorsing it.
Participants were then randomly assigned to one of two temporal deadlines to seek treatment: 2 days or 90 days. Participants were asked to imagine they had the opportunity to “visit a physician for a free mental health exam within the next 2 [90] days.” Before making their decision, participants were given the option of first reading mental health resources. They were told that this option was intended to help them make the decision. Participants then viewed a website from the National Institute of Mental Health (https://www.nimh.nih.gov/health/topics/index.shtml) that presented information on specific mental disorders (e.g., depression) and related topics such as mental health treatments (e.g., psychotherapy). A hidden timer recorded how long (in seconds) each participant spent on the website. Because the main focus of Experiment 2 was to examine a behavioral outcome, we did not ask participants to subsequently report their intentions to seek treatment. This approach is consistent with prior work (e.g., Belding et al., 2015; Lannin et al., 2016). Although participants were told they would be making a subsequent behavioral intention, the purpose of this was to provide a rationale for why they were being asked to explore the NIMH website (which was the dependent variable of interest). We did not subsequently collect the intentions for two reasons. First, we can infer intentions from the behavioral measure which provided a conceptual replication of Experiment 1. Second, the intentions would not be comparable to those reported in Experiment 1 because we were not controlling the amount or type of information to which participants were exposed on the NIMH website.
Participants then completed the same measures of internalized stigma and self-reported clinical characteristics (e.g., depression symptoms) as in Experiment 1. We also asked participants to self-report further details of their past treatment experience to provide a better descriptive characterization of that treatment. Specifically, we asked participants to indicate whether they had sought mental health treatment from a: “mental health care provider (i.e., a doctor or therapist who specializes in mental health),” “general practitioner or primary care physician (i.e., a doctor who does not specialize in mental health),” and/or “other”. We also asked participants how long it had been since their last treatment appointment. Because the response option was open-ended, we binned responses into three categories for descriptive purposes: equal to or less than a year ago, greater than one year but less than 5 years ago, or equal to or greater than 5 years ago (see Table 1).
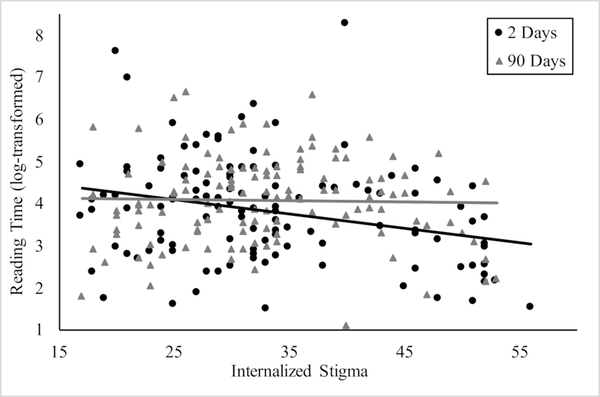
Results
The measures of internalized stigma (Cronbach’s α = .90) and depression symptoms (Cronbach’s α = .86) were calculated as described in Experiment 1. The dependent variable of time spent reading mental health resources was log-transformed to adjust for skew, consistent with prior work (Belding et al., 2015). In order to assess the face validity of the reading time measure in predicting treatment decisions, we examined whether it was negatively related to internalized stigma. Indeed, the two measures were negatively correlated, r(243) = −.17, p = .008. Importantly, the amount of variance explained by the interaction between temporal deadline and internalized stigma was significant and accounted for 6% of the variance in reading time, F(4,244) = 4.11, p = .003; ΔF(1,240) = 4.01, p = .046 (see Table 4). That is, internalized stigma was associated with significantly less reading time for participants given the proximal (2 days: β = −.21, p = .03), but not distant (90 days: β = −.05, p = .64) temporal deadline (see Figure 2).
Table 4.
Summary of hierarchical regression analysis for variables predicting log-transformed reading time among participants with prior mental health treatment experience in Experiment 2 (N = 245).
| Step 1 | Step 2 | |||
|---|---|---|---|---|
| β | t | β | t | |
| Temporal Deadline | .10 | 1.60 | .34 | 1.49 |
| Internalized Stigma | −.14 | 2.05* | −.25 | 2.86* |
| Depression Symptoms | −.09 | 1.34 | −.10 | 1.45 |
| Social Distance X Internalized Stigma | – | – | .47 | 2.00* |
| F(3,244) = 4.09, p = .007, R2 = .05 | F(4,244) = 4.11, p = .003, R2 = .06 | |||
Note. Temporal deadline (0 = 2 days, 1 = 90 days) was represented as a dummy variable.
p ≤ .05.
Figure 2.
Internalized stigma predicted less time spent reading the NIMH website (log-transformed) when participants were given a proximal (2 days) versus distant (90 days) temporal deadline in Experiment 2.
Discussion
The results of Experiment 2 replicated those from Experiment 1 and extended them in two key ways. First, we found that, as with social distance (Experiment 1), greater temporal distance reduced the impact of internalized stigma on treatment decisions for individuals with (vs. without) prior treatment experience. Specifically, higher internalized stigma was associated with less time spent reading mental health resources – a behavior that may inform treatment decision-making – given a psychologically proximal, but not distant, deadline to seek treatment. Second, we extended the findings of Experiment 1 using treatment intentions to show that this effect persists for participants’ engagement in treatment-related behavior (i.e., searching online for information of mental illnesses and mental health treatment). A potential limitation of Experiment 2 is that the effect of psychological distance [temporal deadline] was less pronounced than in Experiment 1. One possibility for this inconsistency was that participants were allowed to freely interact with the NIMH website while time spent on the website was recorded. The noisiness of this measure, which we would expect to be equal across conditions, might have thus obscured the strength of the effect found for behavioral intentions in Experiment 1. Alternately, the psychological distance between oneself and a relatively unfamiliar classmate in Experiment 1 may have been greater than 2 and 90 days in Experiment 2. Greater psychological (e.g., temporal or social) distance between conditions (e.g., 15 minutes vs. 10 years) would increase the size of the effect (Soderberg et al., 2015). Future work could elaborate on the strength of the psychological distancing effect across a wider range of behavioral intentions and treatment-related behaviors.
General Discussion
Overall, we demonstrated that stigma disrupts treatment decisions when behaviors they are psychologically proximal, but not when they are psychologically distant. This same pattern emerged irrespective of the distance manipulation (e.g., social in Experiment 1; temporal in Experiment 2) and population (e.g., college undergraduates in Experiment 1; an online community sample in Experiment 2). It is important to note, however, that Experiment 1 demonstrated that this effect was unique to individuals who had previously sought mental health treatment. Experiment 2 replicated and extended the effect on intentions to behavior, such that participants with higher internalized stigma engaged in less information-seeking behavior in the psychologically proximal, but not distant, condition. Although the appointment intention and the behavior of reading mental health resources are not directly analogous, this work provides initial evidence that changing the psychological distance of treatment-related may be a promising method by which to counteract the influence of internalized stigma on treatment-seeking in clinical and intervention contexts.
The current work also extends extant theoretical models of the negative impact of stigma on treatment-seeking by demonstrating that internalized stigma’s impact on treatment intentions and behavior is malleable. Specifically, internalized stigma exerts a stronger influence on treatment decisions when those decisions are psychologically proximal, but not when they are distant. It is important to note that increasing psychological distance did not reduce internalized stigma directly, but rather reduced its influence on treatment-seeking. Because much prior work has elucidated several distinct features that vary with psychological distance (e.g., the weighting of cons vs. pros of behaviors; Cacioppo & Berntson, 1994; Eyal et al., 2004; Miller, 1944), these findings can be used in future work to characterize how internalized stigma acts as a barrier to treatment.
Psychological distance was effective at moderating internalized stigma among those for whom seeking mental health treatment was more personally-relevant– i.e., individuals who had prior mental health treatment experience. That this finding was limited to those with prior treatment experience was relatively unsurprising given that individuals who had (vs. had not) previously sought mental health treatment had higher current depressive symptomology and were more willing to engage in future treatment. That is, individuals with prior treatment experience may have been more responsive to the manipulation because both mental health treatment itself and the potential threat of being stigmatized as a result (Thoits, 2016; Vogel et al., 2007) were more relevant to this group. It is thus interesting to note that we found this pattern across samples of individuals whose mental health and treatment experiences were diverse: approximately one-third to one-half reported that they had been diagnosed with both depression and an anxiety disorder, while most had sought treatment from at least a mental health care provider (see Table 1). However, a limitation of this work is that we do not have a sufficiently large sample to disentangle how stigma affects treatment behaviors based on these clinical and treatment characteristics. Future research should investigate these questions, and also consider ways to promote treatment-seeking among individuals with high stigma but no prior treatment experience.
Although we have suggested that stigma is more influential at certain times, we do not mean to suggest that stigma is only a barrier when individuals make initial treatment decisions. Prior work has shown that internalized stigma is a major barrier throughout the treatment process – approximately 20% of patients discontinue treatment early (Edlund et al., 2002) and treatment discontinuation is higher in psychiatry than other medical domains (Mitchell & Selmes, 2007). Moreover, internalized stigma predicts these higher rates of treatment discontinuation and nonadherence and, as a potential consequence, worse symptomology (Livingston & Boyd, 2010). Therefore, one interpretation of the current work is that stigma could affect a person’s decision each time he/she decides, for example, to attend the next treatment appointment.
But, the current work suggests that strategies could be used to help individuals overcome stigma to seek treatment to improve their mental health. One potential application of this work would be to directly manipulate psychological distance via the times when individuals make treatment decisions. For instance, pre-commitment (e.g., having individuals agree in advance to perform behaviors and face penalties if they do not) is one strategy that relies on the same underlying psychological phenomenon as temporal distance to increase goal-directed intentions and behavior (Ariely & Wertenbroch, 2002; Rogers & Bazerman, 2008; Thaler & Benartzi, 2004). Pre-commitment capitalizes on people’s increased willingness to engage in a behavior despite its costs when it is psychologically distant relative to proximal, and then binds them to those decisions – making it difficult to “back out” of those commitments later (Ariely & Wertenbroch, 2002; Loewenstein & Prelec, 1993; Rogers & Bazerman, 2008; Thaler & Benartzi, 2004). Because we have shown that psychological distance can be elicited in multiple ways, there are multiple routes by which these findings can be applied. For instance, another potential application of these findings would be to employ existing therapeutic strategies such as self-distancing – a process by which a person considers their experiences from another person or outside perspective (Beck, 1970; Shepherd, Coifman, Matt, & Fresco, 2016) – to help clients manage their stigmatization concerns about treatment. However, because stigma may arise as a barrier each time an individual is faced with a treatment decision, these results also suggest that multiple strategies may need to be enacted to improve treatment-seeking and adherence. For example, coupling pre-commitment with self-distancing may be most successful. Taken together, this work demonstrates that understanding when internalized stigma acts as a barrier to treatment will be important for developing interventions that are effective at removing stigma from the decision process for people with mental health concerns.
Acknowledgments
This research was supported in part by the NIMH [T32MH103213 (CH)]; grant numbers KL2TR002530 and UL1TR002529 (A. Shekhar, PI) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award (ACK); and grants from The John Templeton Foundation’s Philosophy and Science of Self-Control Project (#15462; KF) and the National Science Foundation (#1626733; KF).
Footnotes
An independent sample of online community participants (N=248) were asked: “How relevant is seeking mental health treatment to you?” (1=not at all relevant; 7=very much relevant). Participants who had previous mental health treatment experience (N=106; M=5.15, SD=1.82) reported that treatment-seeking was more personally-relevant than those without prior mental health treatment experience (N=142; M=3.13, SD=2.03), t(246)=8.09, p<.001, d=1.04, 95% CI [.77, 1.31].
Similar modifications to the ISMI scale have been used in prior work (e.g., Arnaez, Krendl, McCormick, Chen, & Chomistek, 2019). In that work, the authors found that the modified ISMI more strongly predicted respondents’ self-reported barriers to seeking mental health treatment (e.g., perceived need, structural barriers, negative expectations about treatment) than did their public stigma (Link, 1987). Higher internalized stigma has been previously shown to predict more negative attitudes toward mental health treatment (Clement et al., 2015), and higher depression symptoms (Ritsher & Phelan, 2004). Thus, to validate the modified version of the ISMI, we had an independent sample of online community participants (N=354) complete the modified ISMI, a measure of mental health treatment attitudes (Fischer & Farina, 1995), and a well-validated measure of depression symptoms (Kroenke, Spitzer, & Williams, 2001). We found the revised ISMI negatively predicted mental health treatment attitudes, r(352)=−.47, p<.001 and positively predicted depression symptoms, r(352)=.23, p<.001.
Because participants were asked to report their mental health treatment history prior to completing the measure of current depressive symptoms, it is possible that this affected their self-reported symptoms. We examined possible order effects in an independent sample of undergraduates (N=337) by counterbalancing the order of these measures. There was no effect of order on the extent of depression symptoms (PHQ-2 1st: M=1.47, SD=1.58; PHQ-2 2nd: M=1.57, SD=1.53; t(335)=.59, p=.55) suggesting, at least in part, that order effects here may have been minimal.
We conducted a direct replication of Experiment 1 using an online community sample (N = 150; from Amazon Mechanical Turk) who had previously sought mental health treatment. Participants in the socially distant condition considered the likelihood that an acquaintance would make an appointment with a mental health care provider. Replicating Experiment 1, participants who had previously sought mental health treatment had lower appointment intentions in the socially proximal condition (self: β = −.39, p = .001), but not the socially distant condition (acquaintance: β = −.11, p = .92).
References
- Ainslie G (1975). Specious reward: A behavioral theory of impulsiveness and impulse control. Psychological Bulletin, 82(4), 463–496. 10.1037/h0076860 [DOI] [PubMed] [Google Scholar]
- Ariely D, & Wertenbroch K (2002). Procrastination, deadlines, and performance: Self-control by precommitment. Psychological Science, 13(3), 219–224. 10.1111/1467-9280.00441 [DOI] [PubMed] [Google Scholar]
- Arnaez JM, Krendl AC, McCormick BP, Chen Z, & Chomistek AK (2019). The association of depression stigma with barriers to seeking mental health care: a cross-sectional analysis. Journal of Mental Health, 1–9. 10.1080/09638237.2019.1644494 [DOI] [PubMed] [Google Scholar]
- Bar-Anan Y, Liberman N, & Trope Y (2006). The association between psychological distance and construal level: Evidence from an implicit association test. Journal of Experimental Psychology: General, 135(4), 609–622. 10.1037/0096-3445.135.4.609 [DOI] [PubMed] [Google Scholar]
- Bathje G, & Pryor J (2011). The relationships of public and self-stigma to seeking mental health services. Journal of Mental Health Counseling, 33(2), 161–176. 10.17744/mehc.33.2.g6320392741604l1 [DOI] [Google Scholar]
- Beck AT (1970). Cognitive therapy: Nature and relation to behavior therapy. Behavior Therapy, 1(2), 184–200. 10.1016/S0005-7894(70)80030-2 [DOI] [Google Scholar]
- Belding JN, Naufel KZ, & Fujita K (2015). Using high-level construal and perceptions of changeability to promote self-change over self-protection motives in response to negative feedback. Personality and Social Psychology Bulletin, 41(6), 822–838. 10.1177/0146167215580776 [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, & Berntson GG (1994). Relationship between attitudes and evaluative space: A critical review, with emphasis on the separability of positive and negative substrates. Psychological Bulletin, 115(3), 401–423. 10.1037/0033-2909.115.3.401 [DOI] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2015a). 1.5 million young adults do not receive needed mental health services. The CBHSQ Report. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2015b). 2014 National Survey on Drug Use and Health: Mental health detailed tables. Rockville, MD. [Google Scholar]
- Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, … Thornicroft G (2015). What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 11–27. 10.1017/S0033291714000129 [DOI] [PubMed] [Google Scholar]
- Corrigan P (2004). How stigma interferes with mental health care. Am Psychol, 59(7), 614–625. 10.1037/0003-066X.59.7.614 [DOI] [PubMed] [Google Scholar]
- Dalky HF (2012). Mental Illness Stigma Reduction Interventions: Review of Intervention Trials. Western Journal of Nursing Research, 34(4), 520–547. 10.1177/0193945911400638 [DOI] [PubMed] [Google Scholar]
- Danziger S, Montal R, & Barkan R (2012). Idealistic advice and pragmatic choice: A psychological distance account. Journal of Personality and Social Psychology, 102(6), 1105–1117. 10.1037/a0027013 [DOI] [PubMed] [Google Scholar]
- Devine PG (1989). Stereotypes and prejudice: Their automatic and controlled components. Journal of Personality and Social Psychology, 56(1), 5–18. 10.1037/0022-3514.56.1.5 [DOI] [Google Scholar]
- Edlund MJ, Wang PS, Berglund PA, Katz SJ, Lin E, & Kessler RC (2002). Dropping out of mental health treatment: Patterns and predictors among epidemiological survey respondents in the United States and Ontario. American Journal of Psychiatry, 159(5), 845–851. 10.1176/appi.ajp.159.5.845 [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Downs MF, Golberstein E, & Zivin K (2009). Stigma and help seeking for mental health among college students. Medical Care Research and Review, 66(5), 522–541. 10.1177/1077558709335173 [DOI] [PubMed] [Google Scholar]
- Epley N (2008). Solving the (Real) Other Minds Problem. Social and Personality Psychology Compass, 2(3), 1455–1474. 10.1111/j.1751-9004.2008.00115.x [DOI] [Google Scholar]
- Eyal T, Liberman N, Trope Y, & Walther E (2004). The pros and cons of temporally near and distant action. Journal of Personality and Social Psychology, 86(6), 781–795. 10.1037/0022-3514.86.6.781 [DOI] [PubMed] [Google Scholar]
- Eyal T, Sagristano MD, Trope Y, Liberman N, & Chaiken S (2009). When values matter: Expressing values in behavioral intentions for the near vs. distant future. Journal of Experimental Social Psychology, 45(1), 35–43. 10.1016/J.JESP.2008.07.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyal T, Steffel M, & Epley N (2018). Perspective mistaking: Accurately understanding the mind of another requires getting perspective, not taking perspective. Journal of Personality and Social Psychology, 114(4), 547–571. 10.1037/pspa0000115 [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. 10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- Fischer EH, & Farina A (1995). Attitudes toward seeking professional psychologial help: A shortened form and considerations for research. Journal of College Student Development. [Google Scholar]
- Griffiths KM, Carron-Arthur B, Parsons A, & Reid R (2014). Effectiveness of programs for reducing the stigma associated with mental disorders. A meta-analysis of randomized controlled trials. World Psychiatry : Official Journal of the World Psychiatric Association (WPA), 13(2), 161–175. 10.1002/wps.20129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Hedden SL, Lipari R, Copello EAPP, & Kroutil LA (2015). Receipt of services for behavioral health problems: Results from the 2014 National Survey on Drug Use and Health. National Survey on Drug Use and Health Data Review, (September). [Google Scholar]
- Howell JL, Sweeny K, & Shepperd JA (2014). Psychological distance and the discrepancy between recommendations and actions. Basic and Applied Social Psychology, 36(6), 502–514. 10.1080/01973533.2014.958229 [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2003). The Patient Health Questionnaire-2: validity of a two-item depression screener. Medical Care, 41(11), 1284–1292. 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, & Löwe B (2010). The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. General Hospital Psychiatry, 32(4), 345–359. 10.1016/j.genhosppsych.2010.03.006 [DOI] [PubMed] [Google Scholar]
- Lannin DG, Vogel DL, Brenner RE, Abraham WT, & Heath PJ (2016). Does self-stigma reduce the probability of seeking mental health information? Journal of Counseling Psychology, 63(3), 351–358. 10.1037/cou0000108 [DOI] [PubMed] [Google Scholar]
- Liberman N, Sagristano MD, & Trope Y (2002). The effect of temporal distance on level of mental construal. Journal of Experimental Social Psychology, 38(6), 523–534. 10.1016/S0022-1031(02)00535-8 [DOI] [Google Scholar]
- Liberman N, & Trope Y (1998). The role of feasibility and desirability considerations in near and distant future decisions: A test of temporal construal theory. Journal of Personality and Social Psychology, 75(1), 5–18. 10.1037/0022-3514.75.1.5 [DOI] [Google Scholar]
- Liberman N, & Trope Y (2014). Traversing psychological distance. Trends in Cognitive Sciences, 18(7), 364–369. 10.1016/J.TICS.2014.03.001 [DOI] [PubMed] [Google Scholar]
- Link BG (1987). Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review, 52(1), 96 10.2307/2095395 [DOI] [Google Scholar]
- Livingston JD, & Boyd JE (2010). Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine, 71(12), 2150–2161. 10.1016/j.socscimed.2010.09.030 [DOI] [PubMed] [Google Scholar]
- Loewenstein GF, & Prelec D (1993). Preferences for sequences of outcomes. Psychological Review, 100(1), 91–108. 10.1037/0033-295X.100.1.91 [DOI] [Google Scholar]
- Miller NE (1944). Experimental studies of conflict In Hunt JM (Ed.), Personality and the Behavior Disorders (pp. 431–465). Oxford, England: Ronald Press. [Google Scholar]
- Mitchell AJ, & Selmes T (2007). Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Advances in Psychiatric Treatment, 13(6). [Google Scholar]
- Oexle N, Müller M, Kawohl W, Xu Z, Viering S, Wyss C, … Rüsch N (2018). Self-stigma as a barrier to recovery: a longitudinal study. European Archives of Psychiatry and Clinical Neuroscience, 268(2), 209–212. 10.1007/s00406-017-0773-2 [DOI] [PubMed] [Google Scholar]
- Paolacci G, & Chandler J (2014). Inside the Turk: Understanding Mechanical Turk as a participant pool. Current Directions in Psychological Science, 23(3), 184–188. 10.1177/0963721414531598 [DOI] [Google Scholar]
- Pennington GL, & Roese NJ (2003). Regulatory focus and temporal distance. Journal of Experimental Social Psychology, 39(6), 563–576. 10.1016/S0022-1031(03)00058-1 [DOI] [Google Scholar]
- Perugini M, Gallucci M, & Costantini G (2018). A practical primer to power analysis for simple experimental designs. International Review of Social Psychology, 31(1). 10.5334/irsp.181 [DOI] [Google Scholar]
- Picco L, Pang S, Lau YW, Jeyagurunathan A, Satghare P, Abdin E, … Subramaniam M (2016). Internalized stigma among psychiatric outpatients: Associations with quality of life, functioning, hope and self-esteem. Psychiatry Research, 246, 500–506. 10.1016/J.PSYCHRES.2016.10.041 [DOI] [PubMed] [Google Scholar]
- Pronin E, Olivola CY, & Kennedy KA (2008). Doing unto future selves as you would do unto others: Psychological distance and decision making. Personality and Social Psychology Bulletin, 34(2), 224–236. 10.1177/0146167207310023 [DOI] [PubMed] [Google Scholar]
- Ritsher JB, Otilingam PG, & Grajales M (2003). Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Research, 121(1), 31–49. 10.1016/J.PSYCHRES.2003.08.008 [DOI] [PubMed] [Google Scholar]
- Ritsher JB, & Phelan JC (2004). Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Research, 129(3), 257–265. 10.1016/j.psychres.2004.08.003 [DOI] [PubMed] [Google Scholar]
- Rogers T, & Bazerman MH (2008). Future lock-in: Future implementation increases selection of ‘should’ choices. Organizational Behavior and Human Decision Processes, 106(1), 1–20. 10.1016/j.obhdp.2007.08.001 [DOI] [Google Scholar]
- Rüsch N, Angermeyer MC, & Corrigan PW (2005). Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. 10.1016/j.eurpsy.2005.04.004 [DOI] [PubMed]
- Shapiro DN, Chandler J, & Mueller PA (2013). Using Mechanical Turk to study clinical populations. Clinical Psychological Science, 1(2), 213–220. 10.1177/2167702612469015 [DOI] [Google Scholar]
- Shepherd KA, Coifman KG, Matt LM, & Fresco DM (2016). Development of a self-distancing task and initial validation of responses. Psychological Assessment, 28(7), 841–855. 10.1037/pas0000297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soderberg CK, Callahan SP, Kochersberger AO, Amit E, & Ledgerwood A (2015). The effects of psychological distance on abstraction: Two meta-analyses. Psychological Bulletin, 141(3), 525–548. 10.1037/bul0000005 [DOI] [PubMed] [Google Scholar]
- Thaler RH, & Benartzi S (2004). Save More Tomorrow™: Using behavioral economics to increase employee saving. Journal of Political Economy, 112(S1), S164–S187. 10.1086/380085 [DOI] [Google Scholar]
- Thoits PA (2016). “I’m Not Mentally Ill”: Identity deflection as a form of stigma resistance. Journal of Health and Social Behavior, 57(2), 135–151. 10.1177/0022146516641164 [DOI] [PubMed] [Google Scholar]
- Thornicroft G, Mehta N, Clement S, Evans-Lacko S, Doherty M, Rose D, … WHO. (2016). Evidence for effective interventions to reduce mental-health-related stigma and discrimination. The Lancet, 387(10023), 1123–1132. 10.1016/S0140-6736(15)00298-6 [DOI] [PubMed] [Google Scholar]
- Trope Y, & Liberman N (2010). Construal-level theory of psychological distance. Psychological Review, 117(2), 440–463. 10.1037/a0018963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker J, Vogel DL, Bitman R, & Wade NG (2013). Disentangling Self-Stigma: Are Mental Illness and Help-Seeking Self-Stigmas Different? ARTICLE in JOURNAL OF COUNSELING PSYCHOLOGY. 10.1037/a0033555 [DOI] [PubMed] [Google Scholar]
- Vogel DL, Wade NG, & Ascheman PL (2009). Measuring perceptions of stigmatization by others for seeking psychological help: Reliability and validity of a new stigma scale with college students. Journal of Counseling Psychology, 56(2), 301–308. 10.1037/a0014903 [DOI] [Google Scholar]
- Vogel DL, Wade NG, & Haake S (2006). Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology, 53(3), 325–337. 10.1037/0022-0167.53.3.325 [DOI] [Google Scholar]
- Vogel DL, Wester SR, & Larson LM (2007). Avoidance of counseling: Psychological factors that inhibit seeking help. Journal of Counseling & Development, 85(4), 410–422. 10.1002/j.1556-6678.2007.tb00609.x [DOI] [Google Scholar]
- Walton GM (2014). The new science of wise psychological interventions. Current Directions in Psychological Science, 23(1), 73–82. 10.1177/0963721413512856 [DOI] [Google Scholar]
- Wang PS, Angermeyer M, Borges G, Bruffaerts R, Tat Chiu W, DE Girolamo G, … Ustün TB (2007). Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry, 6(3), 177–185. [PMC free article] [PubMed] [Google Scholar]
- Webb TL, & Sheeran P (2006). Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin, 132(2), 249–268. 10.1037/0033-2909.132.2.249 [DOI] [PubMed] [Google Scholar]