Abstract
In this era, grand challenges lies in biodiversity loss, climate change, and global noncommunicable diseases signify that planet and humanity are in crisis. Scholarly evidence from human and animal kingdom suggest that there is an optimism in planetary health which can provide a unique and novel concept where efforts toward survival and remediation can be made. With accurate navigation, the current challenges can be mitigated leading to a new reality, one in which the core value is the well-being of all. This paper discusses the drivers of planetary health and the role of community health workers (CHWs) in making health-care system more resilient that can produce multiple benefits to community and overall planetary health. A web-based international database such as Google, Google Scholar, SCOPUS/MEDLINE/PubMed, and JSTOR was searched relevant to a planetary health framework. The study findings suggest that CHWs can offer health care interventions through environmental health cobenefits across the spectrum of health effects of climate change cause and effects. These actions have been divided into four major categories (i. health care promotion and prevention, ii. health care strengthening, iii. advocacy, and iv. education and research) that CHWs perform through a variety of roles and functions they are engaged in protecting planetary health. CHWs contribute toward achieving sustainable development goals such as planetary health and focus on environment sustainability and well-being of entire mankind.
Keywords: Adaption, climate change, community health worker, health effects, mitigation, planetary health
Introduction
We are seeing a rapidly changing world in and around us. Multiple environmental changes such as huge scale biodiversity damage, environmental deviation, deforestation, land degradation, and ocean acidification have substantial effects but their implications on population health is still not fully understood.[1] The prospective of future global health is under threat with new emerging infectious disease and mounting noncommunicable disease burden that contributes much to the global burden of disease, displacement, growing nutritional vulnerability, mental health risks, and susceptibility to injury and accident, all of which disproportionately intimidate mankind mainly the elderly, the young, the poor, and the future generation.[2] The focus of planetary health characterizes the connections between human-caused disruptions of Earth's natural systems and the resulting impacts on human health and makes the case for globally concerted action.[3] Three recent reports emphasize the concerted efforts needed to preserve and protect planetary health.
First, the Intergovernmental Panel on Climate Change[4] reported that the world could be warmer by 1.5°C as early as 2040. Rapid and significant transitions should be carried out with respect to land, energy, buildings, industries, and transport system and in cities to limit global warming by 1.5°C. Any continuity of carbon dioxide (CO2) emission needs to be balanced to reduce global warming by expelling excess amount of CO2 from the air. On the global context, net human-caused emission of CO2 need to fall by 45% from 2010 levels by 2030 and reach “net zero” around 2050.
Second, the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services (IPBES)[5] has reported a harsh news for the future of mankind that the biosphere has been tampered to a large extent that it is highly affected and is declining very rapidly. The largest impacts are due to direct exploitation of organisms, pollution, climate changes, and invasive alien species, but mostly due to the alteration of flora and fauna. To tackle these crises, five interventions are recommended: capacity building and incentives, strengthening cross sectoral cooperation, pre-emptive actions, decision making in case of resilience and uncertainty; and formulation of environmental law and implementation.
Lastly, the UK's Committee on Climate Change (CCC)[6] focuses primarily on preparing for climate change. In addition, it provides independent advice to government on building a low carbon economy. It has also recommended a new target for the UK, i.e., to bring down greenhouse gases to level zero (net zero) by 2050 and to deliver on the commitment that the UK has signed in the Paris Agreement which states to bring improvements in people lives which could be achievable with known technologies. Nevertheless, it also states that this is possible only when there are clear, stable, and well-designed policies aiming to reduce emissions and it must be introduced across the economy without delay. The current policies are not sufficient to achieve the existing targets; hence, it must be revised.[6]
Role of Community Health Workers (CHWs)
Community health workers (CHWs) are frontline functionaries to deliver patient-centric, comprehensive primary health care, address social determinants of health, and respond to various health challenges and outcomes. CHWs not only promote preventive health measures to the population they serve but also enhance community resilience. A number of environmental hazards such as climate change, ocean acidification, extreme weather, ecosystem collapse, sea level rise, fresh water depletion, reduced agricultural productivity, biodiversity loss, air pollution, and toxic chemical exposure jeopardize the human health advancement that has been experienced in the last few decades. The role of CHWs, therefore, can be instrumental in creating awareness to address some of these environmental variations.[7] For instance, in climate change, actions and leadership of CHWs can boost the existing efforts to mitigate climate challenge, therefore, producing multiple benefits to community, health-care system, and overall planetary health.
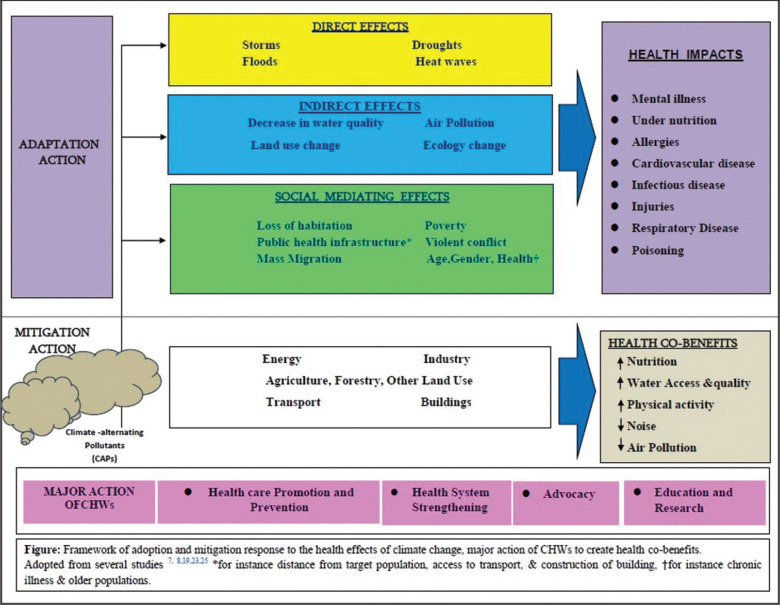
The health effects of extreme weather change can be classified as direct (such as flood or drought), indirect (such as ecosystem change after experiencing flood or drought leading to distribution of disease vectors), or through social mediating processes (such as mass migration after violent conflict or drought).[8,9] These three pillars interact with one another, amplifing climate risk, which are primarily driven by global development and demographic transitions. The other social determinants of health also affect population vulnerability to climate change and their impacts are unevenly distributed, with greater burden of risk in less-developed economics. The policies and provisions that address the reduction of social determinants empower various actors to support longer-term development and the drivers of climate change can encompass all sectors, including, energy, agriculture, health, transportation, and economy.[7] The mitigation and adaption action of climate change could lead to direct reduction in burden of disease, alleviate poverty, increase community resilience, and address global inequity.
CHWs have the potential to enhance primary health care and are particularly effective when they share common culture, ethnicity, economic status, language, and life experiences with communities they serve.[10] A growing body of evidence highlights that the diverse roles CHWs carry out in community and global settings can be utilized for primary care.[11,12] They can influence policy makers for favorable provisions to reduce environmental impact of health care and, thereby, provide health cobenefits. The evidence illustrated that CHWs are widely connected to the community and act as more trusted persons than government functionaries and other public health professionals.[13,14] They can act as a key leader in the community and advocate for evidence-based interventions for policy outreach and implication. They can offer health care interventions through environmental health cobenefits across the spectrum of health effects of climate change cause and effects [Figure 1]. These actions have been divided into four major categories that CHWs perform through a variety of roles and functions.
Figure 1.
Framework of adoption and mitigation response to the health effects of climate change & major action of CHWs to create health co-benefits
Health Care, Promotion, and Prevention
First, CHWs have a major role in providing health care, promotion and prevention apart from treating the patients. They can give advice to people for behavioral change that have environmental cobenefits. For example, CHWs could encourage for active transport through physical activity rather than motorized transport, take healthiest diets that have less environmental impact such as no to red meat, high intake of fruits, green leafs, and vegetables that are healthy for the planet and the individual. CHWs also adjust medications to adapt environmental stress who have already existing diseases. For example, proper guidance and follow-up along with modification of dosage, drug course, and self-medication is required for geriatric persons at the time of heat waves. In addition, CHWs are the first contact point of community for any illness and serve as important front-line health workers for the implementation of community health program and execute surveillance function for various infectious and noninfectious diseases, as seen in other countries such as in Brazil[15] and India.[16] More so, CHWs play a major role in the aftermath of climate-related events (e.g., disasters such as storms and floods) to provide necessary support in disaster risk reduction strategies especially to reduce mental and physical health effects of afflicted people.[17]
Health System Strengthening
Second, CHWs also play a very crucial role in health system strengthening. CHWs represent a robust proportion of human resources for health worldwide; so, they can give recommendation on workforce planning on the anticipated degradation of environmental conditions, such as zoonotic diseases that arise from animals and land use, respiratory diseases, and other climate changes.[18] Their active involvement to the communities help in addressing environmental and social determinants of health rather than looking at the fully biomedical research to care for vulnerable populations, such as older people and young children, people with disability, poor and marginalized communities, and disaster-prone populations. In addition, health effects of climate change can be mitigated by the improvement of the primary-health care infrastructure; for instance, by decreasing the emissions of climate-altering pollutants (CAPs) through improved low carbon energy sources or energy efficiency.[7,19]
Advocacy
Third, CHWs have an important part in advocacy for planetary health activities. They can take part in social marketing on climate change and advocate for mitigation and adaption actions to protect the planet.[13] CHWs can alert policy makers to take actions that affect climate change by addressing the health benefits.[7] For example, they may advocate the negative health outcomes due to increased fossil fuels and use of well-designed carbon taxes to reduce income inequality and improve overall quality life.[20] The various professional bodies such as World Federation of Public Health Association and World Organization of Family Doctors should take leadership roles in this process.[21] At the door step and local level, CHWs could lead community health initiatives and movements, join in community organizations, and act as role models, for instance, by leading active walk campaign, waste recycling, and low-carbon healthy lifestyles.
Education and Research
Fourth, CHWs are pivotal to introduce the concepts of planetary health research and education using education materials and training curriculum related to planetary health.[7,18] CHWs directly impart training to community on public health education and the planetary health material can be developed with inputs from the primary health care units. The policy makers also seek support from the expert opinions of CHWs on planetary health approach for policy outreach and informed decisions. This can be done through collaborative workshops, conferences, and deliberations with CHWs.[22] In teaching and research, CHWs can recommend priority areas of planetary health research for population health, such as recent examples of the phasing out of coal to replace it with cleaner energy[23] and air quality alert evaluation,[24] yielding positive gains for society. The climate change and other environmental variations may also have an impact on individual clinical manifestation or to population health changes (such as changes in health due to extended allergy periods or death of elderly population due to heat wave).
Relevance of Planetary Health to the Practice of Primary Care
Primary care plays a very crucial role in improving population health[25,26] and planetary health.[27,28] Primary care providers including CHWs worldwide counsel millions of patients every day and enjoy society's trust and recognition. These attributes offer them great personal and political attention not only in providing healing touch to patients’ health but also improving the health of the planet. In the promotion of healthy lifestyles, primary care must consider that global warming is human- induced[29,30] with live-stock contributing a tremendous share of the global greenhouse emissions.[31] Evidence suggest that livestock alone contribute to around 80% of the agricultural emissions,[31] out of which animal products contribute to around 20% of the global greenhouse emissions[32] leading to massive destructions of biodiversity.[31] Therefore, primary care teams including CHW can become role models and act as educators in their community for healthy lifestyles and to promote healthy public policies to protect public health and planetary health. Primary care can spread meaningful messages in various ways to their communities. For instance, the WONCA Air Health Train the Trainer programme in low- and middle-income countries, trains family doctors and medical workers that influence communities to improve air quality. As a result, the reduction of greenhouse gases has been envisioned.[33] In Borneo, a project named Health in Harmony that has stopped deforestation, transformed the landscape and increased human wellbeing.[34]
It has been evident that ecosystems across the globe are threatened by massive biodiversity loss and climate change.[1,31,35,36,37] We need to initiate a holistic approach to protect the health of the planet and place “wellbeing of all” as the fundamental aspect at the heart of decision making. Therefore, the cooperation of various governments, enforcement of existing laws, and formulation of new laws with all precautionary measures and incentives would be crucial to protect the planet. An urgent need requires for all key stakeholders (national and state governments, industries and corporates, institutions, communities, and individuals) to recognize the importance of planetary health. They should carry out their own planetary health impact assessment study and could inform feasible interventions to protect or at least minimize the harm to environment, health and biodiversity loss. At the same time, pragmatic decisions should be made on how we can make meaningful contribution toward the restoration and reparations of natural systems. By doing so, we can not only bring health cobenefits to mankind but also defeat some of the world's major public health challenges by improving nutritional security, improving air quality, and increasing physical activity which can reduce the huge cost and harm that arise while nurturing our present sick planet.[38,39,40,41] In moving forward, active outreach on planetary health must be intensified by the policy makers and general public to advocate the pressing issues faced at the health and environmental level and to participate in the promotion of global health and planetary health.
Conclusion
The association between human health and natural systems are complex and primary care is vital for restoring global commons which include land, water, minerals, and vegetation of the planet. This paper provides unique linkage between planetary health and primary care discussing the usefulness of more efficient engagement of CHWs, given their influential role in primary care, for improvement in planetary health. Our framework emphasizes the perfect equivalents between changes in health behaviors (e.g., nutrition, exercise, and smoking) and climate change mitigation and adaption actions. CHWs can serve as a strong mediator of these actions that can promote environmental change. The multifaceted and complex nature of climate change on health effects require the unique skill of CHWs that has to be embedded to their legitimacy to act as knowledge experts by upholding close professional liaison with the community they serve. We are confident that the policy makers and public health planners would recognize the critical role of CHWs and tailor-make the primary care policies for active participation of CHWs in protecting planetary health. The success of the future generation lies in caring and upholding the planet in good health.
Authors’ contribution
MRB conceived the study, conceptualized the article and led the searching and reviewing the literature. DB assisted in literature review and MRB, DB worked on the first draft. All authors read and approved the final manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank the School of Public Health, KIIT Deemed to be University for providing the necessary support for this research. Our special thanks to Mr. Shraban Kumar Behera and Ms. Gayatri Nayak for their assistance in editing the framework.
References
- 1.Frumkin H, Haines A. Global environmental change and noncommunicable disease risk.Annu. Rev Public Health. 2019;40:261–82. doi: 10.1146/annurev-publhealth-040218-043706. [DOI] [PubMed] [Google Scholar]
- 2.Myers S. Planetary health: Protecting human health on a rapidly changing planet. Lancet. 2017;390:2860–8. doi: 10.1016/S0140-6736(17)32846-5. [DOI] [PubMed] [Google Scholar]
- 3.Whitmee S, Haines A, Beyrer C, Boltz F, Capon AG, de Souza Dias BF, et al. Safeguarding human health in the Anthropocene epoch: Report of The Rockefeller Foundation–Lancet commission on planetary health. Lancet. 2015;386:1973–2028. doi: 10.1016/S0140-6736(15)60901-1. [DOI] [PubMed] [Google Scholar]
- 4.Intergovernmental Panel on Climate Change (IPCC). Special Report. Global warming of 1.5°C. [Last acessed on 2019 Dec 10]. Available from: https://www.ipcc.ch/sr15/
- 5.The Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services (IPBES). IPBES Global Assessment Summary for Policymakers (PDF) 2019. [Last accessed on 2019 Nov 10]. Available from: https://www.ipbes.Net/news/ipbes-globalassessment-summary-policymakers-pdf .
- 6.Committee on Climate Change. Net Zero – The UK's contribution to stopping global warming. 2019. [Last accessed on 2019 Dec 10]. Available from: https://www.theccc.org.uk/publication/net-zerothe-uks-contribution-to-stopping-global-warming/
- 7.Haines A, McMichael AJ, Smith KR, Roberts I, Woodcock J, Markandya A, et al. Public health benefits of strategies to reduce greenhouse-gas emissions: Overview and implications for policymakers. Lancet. 2009;374:2104–14. doi: 10.1016/S0140-6736(09)61759-1. [DOI] [PubMed] [Google Scholar]
- 8.Smith KR, Woodward A, Campbell-Lendrum D, et al. Human health: Impacts, adaptation, and co-benefits. In: Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, et al., editors. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Part A: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK, and New York, USA: Cambridge University Press; 2014. pp. 709–54. [Google Scholar]
- 9.Kelley CP, Mohtadi S, Cane MA, Seager R, Kushnir Y. Climate change in the Fertile Crescent and implications of the recent Syrian drought. Proc Natl Acad Sci. 2015;112:3241–6. doi: 10.1073/pnas.1421533112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hartzler AL, Tuzzio L, Hsu C, Wagner EH. Roles and functions of community health workers in primary care. Ann Fam Med. 2018;16:240–5. doi: 10.1370/afm.2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Public Health Association. Support for community health workers to increase health access and to reduce health inequities. Published. 2009. Nov, [Last accessed on 2019 Nov 19]. Available from: https://www.apha.org/policies-and-advocacy/public-healthpolicystatements/policy-database/2014/07/09/14/19/supportforcommunity-health-workers-to-increase-health-access-andto-reducehealth-inequities .
- 12.Koch E. A Summary of the National Community Health Advisor Study: Weaving the Future. Tucson, AZ: University of Arizona Health Sciences Center; 1998. [Google Scholar]
- 13.Walker R, Hassall J, Chaplin S, Congues J, Bajayo R, Mason W. Health promotion interventions to address climate change using a primary health care approach: A literature review. Health Promot J Austr. 2011;22:S6–12. doi: 10.1071/he11406. [DOI] [PubMed] [Google Scholar]
- 14.Maibach EW, Kreslake JM, Roser-Renouf C, Rosenthal S, Feinberg G, Leiserowitz AA. Do Americans understand that global warming is harmful to human health? Evidence from a national survey. Ann Glob Health. 2015;81:396–409. doi: 10.1016/j.aogh.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Roriz-Cruz M, Sprinz E, Rosset I, Goldani L, Teixeira MG. Dengue and primary care: A tale of two cities. Bull World Health Organ. 2010;88:244–5. doi: 10.2471/BLT.10.076935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saprii L, Richards E, Kokho P, Theobald S. Community health workers in rural India: Analyzing the opportunities and challneges Accredited Social Health Activists (ASHAs) face in realizing their multiple roles. Hum Resour Health. 2015;13:95. doi: 10.1186/s12960-015-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nahar N, Blomstedt Y, Wu B, Kandarina I, Trisnantoro L, Kinsman J. Increasing the provision of mental health care for vulnerable, disaster-affected people in Bangladesh. BMC Public Health. 2014;14:708. doi: 10.1186/1471-2458-14-708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blashki G, McMichael T, Karoly DJ. Climate change and primary health care. Aust Fam Physician. 2007;36:986–9. [PubMed] [Google Scholar]
- 19.Nichols A, Richardson J. Climate change, health and sustainability: A brief survey of primary care trusts in the south west of England. Perspect Public Health. 2011;131:82–4. doi: 10.1177/1757913910379196. [DOI] [PubMed] [Google Scholar]
- 20.Cuevas S, Haines A. Health benefits of a carbon tax. Lancet. 2016;387:7–9. doi: 10.1016/S0140-6736(15)00994-0. [DOI] [PubMed] [Google Scholar]
- 21.World Organization of National Colleges, Academies and Academic Associations of General Practitioners/Family Physicians Europe. Planetary Health & Primary Health Care. 2020. [Last accessed on 2020 June 19]. https://www.woncaeurope.org/kb/planetaryhealth-and-primary-care-%E2%80%93-67th-session-of-thewho-regional-committee-for-europe .
- 22.Watts N, Adger WN, Ayeb-Karlsson S, Bai Y, Byass P, Campbell-Lendrum D, et al. The Lancet countdown: Tracking progress on health and climate change. Lancet. 2017;389:1151–64. doi: 10.1016/S0140-6736(16)32124-9. [DOI] [PubMed] [Google Scholar]
- 23.Watts N, Adger WN, Agnolucci P, Blackstock J, Byass P, Cai W, et al. Health and climate change: Policy responses to protect public health. Lancet. 2015;386:1861–914. doi: 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- 24.Chen H, Li Q, Kaufman JS, Wang J, Copes R, Su Y, et al. Effect of air quality alerts on human health: A regression discontinuity analysis in Toronto, Canada. Lancet Planet Health. 2018;2:e19–26. doi: 10.1016/S2542-5196(17)30185-7. [DOI] [PubMed] [Google Scholar]
- 25.Behera MR, Behera D, Prutipinyo C. Examining the relationship between living conditions, work environment and intent to stay among nurses in current posts in rural areas of Odisha state, India. Bangladesh J Med Sci. 2020:19:527–36. [Google Scholar]
- 26.Behera M, Prutipinyo C, Sirichotiratana N, Viwatwongkasem C. Retention of medical doctors and nurses in rural areas of Odisha state, India – A policy analysis. Int J Workplace Health Manag. 2019;12:178–96. [Google Scholar]
- 27.Xie E, Falceto de Barros E, Abelson A, Tetelbom Stein A, Haines A. Challenges and opportunities in planetary health for primary care providers. Lancet. 2018;2:e185–7. doi: 10.1016/S2542-5196(18)30055-X. [DOI] [PubMed] [Google Scholar]
- 28.Kurth AE. Planetary health and the role of nursing: A call to action. J Nurs Scholarsh. 2017;49:598–605. doi: 10.1111/jnu.12343. [DOI] [PubMed] [Google Scholar]
- 29.Myers SS, Gaffikin L, Golden CD, Ostfeld RS, Redford KH, Ricketts TH, et al. Human health impact of ecosystem alteration. Proc Natl Acad Sci USA. 2013;110:18753–60. doi: 10.1073/pnas.1218656110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cook J, Oreskes N, Doran PT, Anderegg WRL, Verheggen B, Maibach EW, et al. Consensus on consensus: a synthesis of consensus estimates on human-caused global warming. Environ Res Lett. 2016;11:048002:1–7. [Google Scholar]
- 31.Marinova D, Bogueva D. Planetary health and reduction in meat consumption. Sustain Earth. 2019;2:1–12. [Google Scholar]
- 32.Tilman D, Clark M. Global diets link environmental sustainability and human health. Nature. 2014;515:518–22. doi: 10.1038/nature13959. [DOI] [PubMed] [Google Scholar]
- 33.WONCA. Global Family Doctor. Air Health Train the Trainer Program update. 2019. [Last acessed on 2020 Mar 29]. Available from: https://www.globalfamilydoctor.com/News/AirHealthupdate.aspx .
- 34.Helms J. Our Solution: How to Stop Deforestation in Borneo. Borneo: Health in Harmony; 2017. [Last accessed on 2020 Mar 29]. Available from: https://healthinharmony.org/2017/06/21/solution-haltdeforestation-borneo/ [Google Scholar]
- 35.Hinsely S. Planetary health research digest. Lancet Planetary Health. 2020;4:96–7. doi: 10.1016/S2542-5196(20)30276-X. [DOI] [PubMed] [Google Scholar]
- 36.Pongsiri MJ, Bickersteth S, Colón C, DeFries R, Dhaliwal M, Georgeson L, et al. Planetary health: From concept to decisive action. Lancet Planet Health. 2019;3:e402–4. doi: 10.1016/S2542-5196(19)30190-1. [DOI] [PubMed] [Google Scholar]
- 37.Veidis EM, Myers SS, Almada AA, Golden CD Clinicians for Planetary Health Working Group. A call for clinicians to act on planetary health. Lancet. 2019;393:2021. doi: 10.1016/S0140-6736(19)30846-3. [DOI] [PubMed] [Google Scholar]
- 38.Solomon CG, LaRocque RC. Climate change - A health emergency. N Engl J Med. 2019;380:209–11. doi: 10.1056/NEJMp1817067. [DOI] [PubMed] [Google Scholar]
- 39.Haines A, Ebie K. The imperative for climate action to protect health. N Engl J Med. 2019;380:263–73. doi: 10.1056/NEJMra1807873. [DOI] [PubMed] [Google Scholar]
- 40.Casassus B. Obituary per Fugelli. Lancet. 2017;390:2032. [Google Scholar]
- 41.Brondizio ES, O’Brien K, Bai X, Biermann F, Steffen W, Berkhout F, et al. Reconceptualizing the Anthropocene: A call for collaboration. Glob Environ Chang. 2016;39:318–27. [Google Scholar]