Abstract
Background:
Prediabetes is increasingly being studied in the context of its association with cardiovascular disease (CVD). Besides raised HbA1c and sugar levels, the major underlying defect seems to be insulin resistance (IR). Subclinical atherosclerosis, measured by high sensitivity C reactive protein (hsCRP) and carotid artery intima media thickness (CIMT) underlies the pathogenesis of CVD in prediabetes. Heart-type fatty acid binding protein (H-FABP), a novel cardiac biomarker also might have a role in predictin prediabetic heart disease.
Aims:
The aim of the study is to compare serum levels of H-FABP in prediabetics and controls and correlate them with the atherosclerotic markers, hsCRP and CIMT.
Setting and Design:
50 prediabetic patients and 50 age, sex and BMI matched controls were employed in the case control study. Serum F & PPBS, (HbA1c), fasting insulin levels were measured in cases and controls. Serum H-FABP was measured in both cases and controls. All cases and controls were subjected to bilateral CIMT measurements and Serum hsCRP levels. The values were compared between both the groups and subjected to appropriate statistical analysis.
Statistical Analysis Used:
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected then non parametric test was used. Quantitative variables were compared using Independent t test/Mann-Whitney Test (when the data sets were not normally distributed) between the two groups. Qualitative variables were correlated using Chi-Square test/Fisher's Exact test. Spearman rank correlation coefficient was used to find out the correlation of various parameters with each other. Univariate linear regression was used to find out the cause and effect relationship between various parameters. A p <0.05 was considered statistically significant. The data analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Results:
The mean serum levels of H-FABP among cases and controls were 6.38± 2.76ng/ml and 3.24 ± 2.47 ng/ml respectively (p <0.0001). Mean CIMT was found to be higher in prediabetics (0.59 ± 0.11 mm ) compared to controls (0.45 ± 0.07mm) (p<0.0001). Serum hsCRP levels were also statistically higher in prediabetics (5.75± 4.16 mg/l) then that of controls (1.86± 1.67 mg/l) (p <0.0001). The correlations of the two variables, hsCRP and CIMT with H-FABP were both strongly positive (r = 0.687) & (r = 0.779) respectively [both cases (p < 0.0001)].
Conclusion:
The novel cardiac biomarker H-FAPB might be a good predictor of cardiovascular risks in prediabetics.
Keywords: CIMT, CVD, H-FABP, HOMA-IR, hsCRP, pre diabetes
Introduction
Diabetes mellitus (DM) is a group of metabolic diseases characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Pre diabetes is an interim condition associated with an increased risk of development of type 2 diabetes, the common denominator of the two being insulin resistance. An estimated 34% of adults worldwide have pre diabetes and it is also recognized as a reversible condition with improvement in lifestyle and activity.[1]
A study from South Asia found that there was an incidence of 22.2, 29.5, and 51.7 for every 1000 person years for DM, pre diabetes, and “any dysglycemia” respectively. The conversion degree of prediabetes to diabetes was 58.9%.[2]
India, being the “Diabetic capital of the world” leads the world with the largest number of diabetic subjects at least in part due to the so called “Asian Indian Phenotype” with certain unique genetic, clinical, and biochemical abnormalities such as increased insulin resistance, greater abdominal adiposity i.e. higher waist circumference despite lower body mass index and lower adiponectin levels.[3]
Deaths due to cardiovascular diseases (CVD) in India has increased from 1.3 million in 1990 to 2.8 million in 2016 and metabolic diseases have the maximum causative role.[4]
The incidence and prevalence of macrovascular {including coronary artery disease (CAD)} and microvascular (including nephropathy and retinopathy) complications can be noticed anytime during the course of the diabetic disease spectrum emphasizing on its long asymptomatic course before the development of clinical hyperglycemia.[5]
Studies on prediabetes and CVD also show an estimated relative risk (RR) for cardiovascular disease associated with impaired glucose tolerance (IGT) of 0.97 to 1.30 and with impaired fasting glucose (IFG) of 1.12 to 1.37.[6]
Since atherosclerosis is the basis for the development of cardiovascular diseases initiating as arterial wall lesions and endothelial dysfunction, a great deal of studies have been done to assess the same. Carotid intima-media thickness (CIMT) is a non invasive marker that correlates with CVD risk factors such as blood pressure, lipid profiles, age, and smoking as well as with the extent of coronary artery disease in both women and men. This has led the Federal Drug Agency (FDA) approve it as a valid technique to assess subclinical atherosclerosis.[7]
Since diabetes and the associated CVD are considered as inflammatory processes, measurement of highly sensitive C-reactive protein (hs-CRP) has been used to predict the risk of type 2 DM in patients with metabolic syndrome correlating with the stage of beta-cell dysfunction and insulin resistance. Based on multiple epidemiological and intervention studies, minor CRP elevation [high-sensitivity CRP (hs-CRP)] has been shown to be associated with cardiovascular risk.[8]
Heart-type fatty acid binding protein (H-FABP), the myocardial fraction of a group of novel lipid chaperones (14–15 k Da), was found to get released into the bloodstream when the myocardium is injured and hence found to increase in acute coronary syndromes (ACS) and various other cardiovascular diseases.[9]
The DM spectrum is thus the epidemic of the century and without effective diagnostic methods at an early stage, diabetes and its complications will continue to rise. By screening and risk-stratifying the individuals of prediabetes, we may be able to develop a strategy to prevent pre diabetes from progressing to diabetes and also to prevent the complications of dysglycemia. The identification and treatment of cardiovascular complications in prediabetics is therefore crucial, and this study focuses on H-FABP as one of the possible diagnostic methods of CVD in pre diabetes and correlating them with the atherosclerotic markers CIMT and hs CRP.
Materials and Methods
The study was conducted in the Departments of Medicine, Radio diagnosis and Biochemistry at Post Graduate Institute of Medical Education and Research and Dr. RML Hospital, New Delhi after getting clearance from the Institutional Ethics Committee vide letter number TP (MD/MS)(74/2017)/IEC/PGIMER/RMLH 17/7/17 dated 30.11.2017.
Study Design: A case control study.
Sample Size The study group consisted of 50 consecutive patients of prediabetes and 50 control subjects from Medicine OPD, Medicine Wards, and Medicine Emergencies of Dr. Ram Manohar Lohia Hospital after fulfilling all inclusion and exclusion criteria and matched for age, sex, and ethnicity.
Study period: 1st November 2017 to 31st March 2019
Calculation of sample size
The input for statistical sample size calculation was taken from the study by Basek Karbek et al., 2011.[10]
Patients with impaired glucose tolerance showed a mean (±SD) of 32.5 ± 34.2 ng/dl and controls showed a mean ± SD of 16.8 ± 14.9 ng/dl.
With the above inputs, we considered a minimum difference of about 50% in H-FABP levels in pre diabetics and controls.
With this information, the sample size was calculated as follows.
With an α of 0.05% and β of 0.2%, we get a sample size of 49 on each side.
Mean 1 = 16.8; SD1 = 14.9
Mean 2 = 25.2 (150% of 16.8)
Enrolment ratio of 1
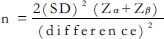
=49 ~ 50.
We require a sample size of 49 on each side (for convenience, 50) to achieve the primary objective of comparing H-FABP between prediabetics and controls.
Inclusion criteria
50 Cases of Prediabetes of age 18–65 years as defined by fasting plasma glucose between 100 to 125 mg/dL OR 2 hour postprandial glucose OR 2 hour oral glucose tolerance test (OGTT) (after 75 gm of glucose solution ingestion) between 140 to 199 mg/dL OR Hb A1 c = 5.7–6.4%.[11]
50 control subjects, matched for age, gender, ethnicity, and body mass index and with fasting blood glucose of less than 100mg/dl and 2 hour postprandial glucose/2 hour OGTT of less than 140mg/dl and HbA1C less than 5.7%, with no known co-morbidities as per exclusion criteria.
{An informed bilingual written consent was taken from each of the patient/relatives for inclusion}.
Exclusion criteria
Known Hypertensives.
Known Diabetics
Chronic smokers
Chronic alcoholics
Known cases of cerebrovascular accidents or transient ischemic attacks [TIA]
Known hypothyroid or hyperthyroid patients.
Known established cases of stroke, angina pectoris, and myocardial infarction.
Known cases of peripheral vascular disease and history of intermittent claudication.
Patients with history of pulmonary embolism
Known cases of chronic renal failure.
Known cases of cardiomyopathy and heart failure.
Known cases of systemic lupus erythematosus (SLE), Vasculitis, malignancy, and connective tissue disorders.
Known retrovirus positive patients
Patients on drugs like statins and other anti hyper lipidemic drugs and anti platelet or anti thrombotic drugs.
Methods
All the cases and controls underwent the following examinations and tests:
• Clinical examination:
The study participants were called to the Department of Medicine, Dr. RML hospital and asked to fill a pre determined questionnaire, which included baseline data about age, sex, race, ethnicity, and family history of diabetes or hypertension.
They then underwent a detailed clinical examination including measurement of height (using stadiometer), weight (using a weight measurement scale) and waist circumference at the upper borders of both hip bones (using a standard measuring tape). The body mass index (BMI) was calculated as weight (in kg) divided by the square of height (in meters). Resting systolic and diastolic blood pressures were recorded twice using an automated sphygmomanometer after a 5-min rest and average was calculated.
• Laboratory investigation:
Around 10 mL of fasting blood sample was collected after venipuncture. Investigations done were fasting plasma glucose, post prandial plasma glucose, glycated hemoglobin (HbA1c), fasting serum insulin levels (measured by chemiluminiscence immuno assay (CLIA) on Vitros ECiQ by Ortho clinical Diagnostics).
All of the samples were analyzed on a fully automated clinical chemistry analyzer in the Department of Biochemistry, PGIMER and Dr. RML hospital, New Delhi.
• Samples for H-FABP and hs CRP were centrifuged and stored in aliquots at -20°Cin the Department of biochemistry until batch analyzed.
Serum heart type fatty acid binding protein
Serum H-FABP kits were imported from RANDOX LABORATORIES, India. Separate kits for cases and controls along with the buffer agents and anti H-FABP latex coated reagents were used- catalogue number: FB 4025 and FB 4026. The stored serum samples were analyzed as a whole by immunoturbidimetric method [Figure 1].
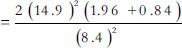
Figure 1.
Showing the measurement of CIMT from a patient in the Department of Radio diagnosis, RMLH. The value recorded was 0.6 mm.
Principle of the test
The samples were assayed on the principle of immunoturbidometry with the help of a H-FABP calibrator series. The samples were allowed to react with a buffer and anti H-FABP coated latex reagents and the formation of antigen-antibody complex during the reaction resulted in an increase in turbidity, the extent of which was measured as the amount of light absorbed at 700 nm. By constructing a standard curve from the absorbance of the standards, H-FABP concentration in the sample was measured.
Measuring range of the kits was 0.747–120 ng/ml.
Measurement of hsCRP
High sensitivity C reactive protein (hs CRP) reagent was used on the VITROS 5,1 FS/4600 Chemistry Systems and the VITROS 5600/XT 7600 Integrated Systems to quantitatively measure C-reactive protein (CRP) in the sample serum, initially stored at -20°C until batch analyzed.
Principles of the procedure
The VITROS Chemistry Products hs CRP Reagent is a dual chambered package containing ready-to-use liquid reagents. Samples, calibrators, and controls were mixed with Reagent 1 containing a buffer. Addition of anti-CRP antibodies coupled to latex microparticles (Reagent 2) produced an immunochemical reaction yielding CRP antigen/antibody complexes. The turbidity was measured spectrophotometrically at 660 nm. Once a calibration had been performed for each reagent lot, the CRP concentration in each sample was determined using the stored calibration curve and the measured absorbance obtained in the assay of the sample.
The interpretation of results were based on guidelines recommended by the U.S. Centers for Disease Control and Prevention, and the American Heart Association for the assessment of risk for cardiovascular disease in adults.[8] Classification for Cardiovascular Disease Risk Conventional and SI Units (mg/L) is as follows:
Low <1
Average 1–3
High 3–10
In determinant >10
• Ultrasonographic examination:
All cases and controls underwent high-resolution B-mode ultrasonography (USG) with a 7.5 MHz linear probe in the Department of Radiology, RMLH. CIMT was measured as the distance between the two echogenic lines (representing intima and media) as shown in the USG film from bilateral common carotids at a level proximal to the bifurcation of the common carotid artery (CCA) and the mean was calculated and tabulated. All scans and image measurements were carried out by the same investigator, blinded to the status of the participants [Table 1].
Table 1.
Demographic and anthropometric characteristics among cases and controls
| PARAMETER | CASES (n=50) | CONTROLS (n=50) | P |
|---|---|---|---|
| AGE (mean±SD) | 35.96±4.48 | 35.94±4.27 | 0.982 |
| SEX (%) | |||
| Males | 48(n=24) | 54(n=27) | 0.548 |
| Females | 52(n=26) | 46(n=23) | |
| BMI(mean±SD) | 24.07±2.71 | 24.08±2.7 | 0.99 |
| WAIST CIRCUMFERENCE (mean±SD) | 82.02±9.22 | 80.11±13.03 | 0.775 |
| SYSTOLIC BLOOD PRESURE(mean±SD) | 116.56±17.08 | 114.8±9.00 | 0.521 |
| DIASTOLIC BLOOD PRESURE (mean±SD) | 73.76±4.25 | 73.52±5.68 | 0.811 |
Statistical analysis
The categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median [Table 2]. The normality of data was tested by Kolmogorov–Smirnov test. If the normality was rejected then non parametric test was used [Table 3].
Table 2.
Biochemical parameters among cases and controls
| PARAMETER (mean±SD) | CASES (n=50) | CONTROLS (n=50) | P |
|---|---|---|---|
| FASTING BLOOD SUGAR | 110.86±9.79 | 86.68±7.14 | <0.0001 |
| POSTPRANDIAL BLOOD SUGAR | 161.3±21.97 | 119.68±12.1 | <0.0001 |
| HbA1c | 6±0.21 | 4.9±0.46 | <0.0001 |
| FASTING INSULIN LEVELS | 12.22±5.42 | 5.37±1.95 | <0.0001 |
| SERUM H-FABP | 6.38±2.76 | 3.24±2.47 | <0.0001 |
| SERUM hsCRP | 5.75±4.16 | 1.86±1.67 | <0.0001 |
| MEAN CIMT | 0.59±0.11 | 0.45±0.07 | <0.0001 |
Table 3.
Serum fasting insulin levels among cases and controls with a cutoff of 9 mL U/l
| GROUP | Total | P | |||
|---|---|---|---|---|---|
| Case | Control | ||||
| SERUM FASTING INSULIN LEVELS | <9 | 14 (28.00%) | 48 (96.00%) | 62 (62.00%) | <.0001 |
| >=9 | 36 (72.00%) | 2 (4.00%) | 38 (38.00%) | ||
| Total | 50 (100.00%) | 50 (100.00%) | 00.00%) | ||
Quantitative variables were compared using Independent t test/Mann–Whitney Test (when the data sets were not normally distributed) between the two groups. Qualitative variables were correlated using Chi-square test/Fisher's exact test [Table 4]. Spearman rank correlation coefficient was used to find out the correlation of various parameters with each other. Univariate linear regression was used to find out the cause and effect relationship between various parameters. A P value of < 0.05 was considered statistically significant. The data analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Table 4.
Serum heart type fatty acid binding protein (H-FABP)levels among cases and controls
| SERUM HEART TYPE FABP | Cases | Controls | |
|---|---|---|---|
| Sample size | 50 | 50 | P=<.0001 |
| Mean±SD | 6.38±2.76 | 3.24±2.47 | |
| Median | 5.93 | 2.15 | |
| Min-Max | 2.92-11.6 | 0.81-9.26 | |
| Inter quartile Range | 3.630-8.980 | -3.120 |
Observations and Results
Results
The primary aim of our study was to assess the serum levels of the variables H-FABP, CIMT, and hsCRP in patients with prediabetes and compare them with the same in normoglycemics [Table 5]. We also attempted to find a possible correlation between H-FABP and atherosclerotic markers, carotid intima-media thickness, and hsCRP.
Table 5.
Mean carotid artery intima media thickness (CIMT) among cases and controls
| MEAN CAROTID ARTERY INTIMA MEDIA THICKNESS(mm) | CASES | CONTROLS | |
|---|---|---|---|
| Sample size | 50 | 50 | P =<.0001 |
| Mean±SD | 0.59±0.11 | 0.45±0.07 | |
| Median | 0.6 | 0.45 | |
| Min-Max | 0.35-0.8 | 0.3-0.6 | |
| Inter quartile Range | 0.500-0.700 | -0.500 |
It was a case-control study and after calculating the sample size (50) as per statistical analysis, 50 cases and 50 controls were enrolled. Matching with respect to age, sex, BMI, blood pressure, and BMI was ensured.
The mean serum fasting insulin level among cases was 12.22 m IU/ml and that of the control group was 5.37 mI U/ml (P value < 0.0001). Among the cases, 72% of the total number were found to have a serum fasting insulin level of more than or equal to 9 mI U/ml, whereas only 4% of the controls were found to have so.
The mean H-FABP levels in cases and controls were 6.38ng/ml and 3.24ng/ml respectively and the difference in means gives a P value of < 0.0001 making it statistically significant.
The mean hsCRP levels in cases and controls were 5.75 mg/l and 1.86 mg/l respectively (P < 0.001). Our study also shows a significant proportion of prediabetics falling under the average and high risk categories for CVD based on hs CRP (28% cases with a value of 1–3 and 48% cases (around half of the subjects) with values 3–10 [Table 6].
Table 6.
hsCRP range among cases and controls - Risk stratificationof cardiovascular disease
| SERUM hsCRP | GROUP | Total | P | |
|---|---|---|---|---|
| Case | Control | |||
| 1)<1(LOW) | 2 (4.00%) | 18 (36.00%) | 20 (20.00%) | <.0001 |
| 2)1-<3(AVERAGE) | 14 (28.00%) | 26 (52.00%) | 40 (40.00%) | |
| 3)3-10(HIGH) | 24 (48.00%) | 6 (12.00%) | 30 (30.00%) | |
| 4)>10(INDETERMINANT) | 10 (20.00%) | 0 (0.00%) | 10 (10.00%) | |
| Total | 50 (100.00%) | 50 (100.00%) | 00.00%) | |
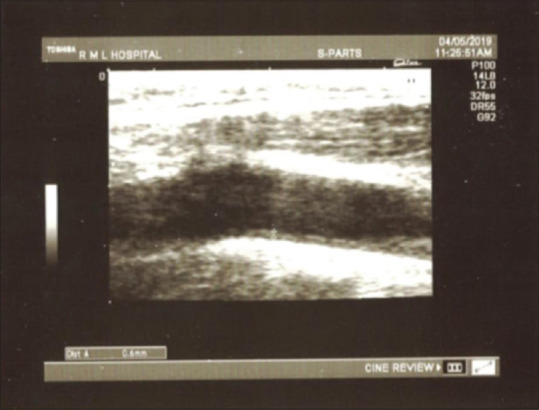
The hsCRP has been correlated with the serum H-FABP levels in cases and there was a moderate positive correlation between the two variables (P-< 0.001 and the correlation coefficient 0.687 as in Figure 2). The univariate linear regression analysis also showed that, for 1 unit increase in H-FABP, hsCRP increases by a unit of 0.927 [Table 7].
Figure 2.
Correlation of H-FABP and hs CRP
Table 7.
Linear regression
| MEAN CAROTID ARTERY INTIMA MEDIAL THICKNESS(mm) | ||||||
|---|---|---|---|---|---|---|
| Univariate linear regression | ||||||
| Unstandardized Coefficients Beta | Standardized Coefficients | P | 95.0% Confidence Interval for B | |||
| B | Sth. Error | Lower Bound | Upper Bound | |||
| SERUM HEART TYPE FABP | .032 | .004 | .767 | <.0001 | .024 | .040 |
| SERUM hsCRP | ||||||
| Univariate linear regression | ||||||
| Unstandardized Coefficients | Standardized Coefficients Beta | P | 95.0% Confidence Interval for B | |||
| B | Std. Error | Lower Bound | Upper Bound | |||
| SERUM HEART TYPE FABP | .927 | .172 | .614 | <.0001 | .581 | 1.273 |
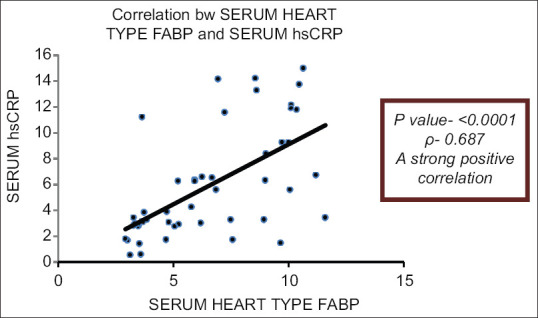
The mean values of mean CIMT of cases and controls are 0.59 mm and 0.45 mm respectively (P < 0.0001). There was also a significant positive correlation between the two variables, H-FABP and CIMT (P value < 0.0001) with a correlation coefficient of 0.779 (r-0.779) [Figure 3]. By analyzing logistic regression, we also noticed that for every unit increase in H-FABP, mean CIMT values increase by 0.032 [Table 7].
Figure 3.
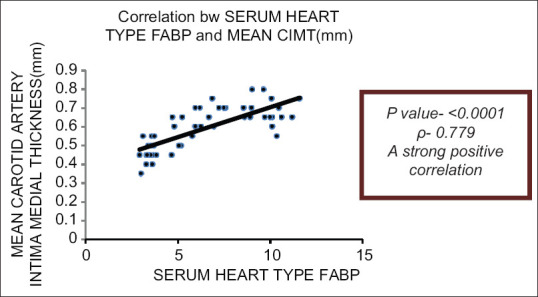
Correlation of H-FABP with CIMT
Discussion
Cardiovascular diseases are non communicable diseases like hypertension and diabetes and are the foremost cause of significant morbidity and mortality and the need for early screening and diagnosis cannot be overemphasized. Our study underscores the presence of CVD in the forerunner state of prediabetes itself with the classic markers of atherosclerosis, the central mechanism in the pathogenesis of endothelial and myocardial damage. Studies have shown links among the molecular pathways of insulin signaling, inflammation, and endothelial dysfunction.[12,13] The downregulation of anti atherogenic pathways and the maintained activity of the proatherogenic pathways in insulin-resistant states lead to accelerated atherosclerosis.[14]
Multiple studies have assessed the importance of the H-FABP in coronary and non coronary cardiac diseases. Okamato et al. and Azzazy HM et al. proposed that H-FABP was an excellent biochemical marker for the diagnosis of acute myocardial infarction (MI) in the early phase and also in predicting further cardiac events in such patients.[15,16] Pelsers MM et al. noticed that H-FABP proves to be an excellent early cardiac marker in detecting minor myocardial injury in heart failure and unstable angina, apart from acute coronary syndrome (ACS).[17] Puls M and his colleagues concluded that H-FABP might be a promising indicator of early right ventricular injury in acute pulmonary embolism (PE).[18]
H-FABP has also been studied in pump-related clinical contexts like dilated and hypertrophic cardiomyopathy, endocardial fibroelastosis, chronic obstructive lung diseases (COPD) with corpulmonale and left heart failure, showing significant differences in values pre and post treatments, with comparable or probably better results to pro-Brain natriuretic peptide (pro-BNP) and troponin T in heart failure syndromes.[19,20,21] A recent study by Hui-Wen Zhang and team published that H-FABP levels were independently associated with worse clinical outcomes in CAD patients in subjects with impaired glucose tolerance.[22]
Another study cited H-FABP as an independent predictor for CV outcomes in patients with stable coronary heart disease (SCHD), mainly in CV death and acute heart failure-related hospitalizations.[23]
Apart from the primary cardiac diseases, studies have been done in H-FABP and various metabolic conditions due to their associations with latent cardiac injury as with diabetes, pre diabetes, obesity, and non alcoholic fatty liver disease (NAFLD) and also to assess nocturnal ischemia in obstructive sleep apnea syndrome (OSAS).[24,25,26]
Our study, showing the significantly increased values of H-FABP in pre diabetes is yet another proof to the subclinical heart disease occurring much prior to the development of clinical diabetes. The study done by Basekkarbek et al.[10] also compared H-FABP with CIMT in patients with IFG and IGT and showed a significantly higher H-FABP and CIMT in the prediabetic groups (IFG and IGT) than in the control group (IFG: 0.6 ± 0.1, IGT: 0.6 ± 0.1, and control: 0.5 ± 0.1; P < 0.001). H-FABP was found to positively correlate with CIMT. The results of our study, the first ever of its kind in India are in par with this study done in Turkey.
The mean value of CIMT in cases in our study was 0.59 ± 0.11 mm, the most of the values exceeding the 75th percentile for age specific values of CIMT.[27] A cross-sectional study by Adolphe A showed that intima-media thickness increased with every additional component of the MetS, from 0.516 mm for 0 components to 0.688 mm for 4 or more components (P <.001).[28] David Faeh et al. studied that age-adjusted levels of the major CVD risk factors and IMT worsened gradually across IGR categories (NFG < IFG/NGT < IFG/IGT < DM).[29]
Our study showed increased values of hsCRP and CIMT in prediabetics and also a positive correlation of the atherogenic indices with HOMA-IR used as a measure of insulin resistance, which signifies the role of insulin resistance in contributing to the atherosclerotic risk in these patients. This was similar to a study by Hulya Parildar and his colleagues who found that serum hs-CRP levels, left, right and maximum CIMT were statistically higher among pre diabetics compared to control group and that there was also a positive, significant correlation among CIMT and fasting blood glucose, HbA1c, hs-CRP levels, and BMI.[30]
Thus, based on the results, we propose that H-FABP can represent early asymptomatic heart disease in the form of coronary diseases (myocardial infarction) and non coronary diseases such as heart failure, cardiomyopathy etc. in prediabetes and signifies a higher atherosclerotic propensity in these individuals when compared to normal subjects. This should pave way for the family physicians and primary health care personnel to stress upon lifestyle modifications and creating awareness to the high risk population about the ill effects of dysglycemia and also the tertiary centres to focus attention on diagnosing CVD in dysglycemic patients early and manage them with diet, lifestyle, and pharmacological measures wherever necessary.
Further studies are required in a wider and mixed population to establish a relationship bringing ethnicity and geographical distribution into account and find how they affect individually, the values of H-FABP. More follow up studies are also essential to propose the prognostic utility in cardiac diseases in these patients.
Conclusion
H-FABP is a promising marker of cardiac and atherosclerotic disease in diagnosing prediabetic heart disease at its incipient stage, which is crucial for the primary prevention of diabetes and CVD related morbidity and mortality.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Tuso P. Prediabetes and lifestyle modification: Time to prevent a preventable disease. Perm J. 2014;18:88–93. doi: 10.7812/TPP/14-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, et al. Prevalence of diabetes and prediabetes in 15 states of India: Results from the ICMR-INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5:585–96. doi: 10.1016/S2213-8587(17)30174-2. [DOI] [PubMed] [Google Scholar]
- 3.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125:217–30. [PubMed] [Google Scholar]
- 4.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: Areport from the American Heart Association. Circulation. 2017;135:e146–603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gill HK, Yadav SB, Ramesh V, Bhatia E. A prospective study of prevalence and association of peripheral neuropathy in Indian patients with newly diagnosed type 2 diabetes mellitus. J Postgrad Med. 2014;60:270–5. doi: 10.4103/0022-3859.138750. [DOI] [PubMed] [Google Scholar]
- 6.Ford ES, Zhao G, Li C. Pre-diabetes and the risk for cardiovascular disease. J Am CollCardiol. 2010;55:1310–7. doi: 10.1016/j.jacc.2009.10.060. [DOI] [PubMed] [Google Scholar]
- 7.Darabian S, Hormuz M, Latif MA, Pahlevan S, Budoff MJ. The role of carotid intimal thickness testing and risk prediction in the development of coronary atherosclerosis. CurrAtheroscler Rep. 2013;15:306. doi: 10.1007/s11883-012-0306-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kannel WB, McGee DL. Diabetes and glucose tolerance as risk factors for cardiovascular disease: The Framingham study. Diabetes Care. 1979;2:120–6. doi: 10.2337/diacare.2.2.120. [DOI] [PubMed] [Google Scholar]
- 9.Furuhashi M, Hotamisligil GS. Fatty acid-binding proteins: Role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov. 2008;7:489–503. doi: 10.1038/nrd2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karbek B, Özbek M, Bozkurt NC, Ginis Z, Güngünes A, Ünsal İÖ, et al. Heart-type fatty acid binding protein (H-FABP): Relationship with arterial ıntima-media thickness and role as diagnostic marker for atherosclerosis in patients with ımpaired glucose metabolism. CardiovascDiabetol. 2011;10:37. doi: 10.1186/1475-2840-10-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2016;39(Suppl 1):S13–22. [Google Scholar]
- 12.Festa A, Hanley AJ, Tracy RP, D’Agostino R, Jr, Haffner SM. Inflammation in the prediabetic state is related to increased insulin resistance rather than decreased insulin secretion. Circulation. 2003;108:1822–30. doi: 10.1161/01.CIR.0000091339.70120.53. [DOI] [PubMed] [Google Scholar]
- 13.Kim J, Koh KK, Quon MJ. The union of vascular and metabolic actions of insulin in sickness and in health. ArteriosclerThrombVascBiol. 2005;146:1978–85. doi: 10.1161/01.ATV.0000164044.42910.6b. [DOI] [PubMed] [Google Scholar]
- 14.Bansilal S, Farkouh ME, Fuster V. Role of insulin resistance and hyperglycemia in the development of atherosclerosis. Am J Cardiol. 2007;99:6–14. doi: 10.1016/j.amjcard.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 15.Okamoto F, Sohmiya K, Ohkaru Y, Kawamura K, Asayama K, Kimura H, et al. Human heart-type cytoplasmic fatty acid-binding protein (H-FABP) for the diagnosis of acute myocardial infarction. Clinical evaluation of H-FABP in comparison with myoglobin and creatine kinase isoenzyme MB. ClinChem Lab Med. 2000;38:231–8. doi: 10.1515/CCLM.2000.034. [DOI] [PubMed] [Google Scholar]
- 16.Azzazy HM, Pelsers MM, Christenson RH. Unbound free fatty acids and heart-type fatty acid-binding protein: Diagnostic assays and clinical applications. ClinChem. 2006;52:19–29. doi: 10.1373/clinchem.2005.056143. [DOI] [PubMed] [Google Scholar]
- 17.Pelsers MM, Hermens WT, Glatz JF. Fatty acid-binding proteins as plasma markers of tissue injury. ClinChimActa. 2005;352:15–35. doi: 10.1016/j.cccn.2004.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Puls M, Dellas C, Lankeit M, Olschewski M, Binder L, Geibel A, et al. Heart-type fatty acid-binding protein permits early risk stratification of pulmonary embolism. Eur Heart J. 2006;28:224–9. doi: 10.1093/eurheartj/ehl405. [DOI] [PubMed] [Google Scholar]
- 19.Zoair A, Mawlana W, Abo-Elenin A, Korrat M. Serum level of heart-type fatty acid binding protein (H-FABP) before and after treatment of congestive heart failure in children. PediatrCardiol. 2015;36:1722–7. doi: 10.1007/s00246-015-1223-4. [DOI] [PubMed] [Google Scholar]
- 20.Sun YP, Wei CP, Ma SC, Zhang YF, Qiao LY, Li DH, et al. Effect of carvedilol on serum heart-type fatty acid-binding protein, brain natriuretic peptide, and cardiac function in patients with chronic heart failure. J CardiovascPharmacol. 2015;65:480–4. doi: 10.1097/FJC.0000000000000217. [DOI] [PubMed] [Google Scholar]
- 21.Zhou FJ, Zhou CY, Tian YJ, Xiao AJ, Li PL, Wang YH, et al. Diagnostic value of analysis of H-FABP, NT-proBNP, and cTnI in heart function in children with congenital heart disease and pneumonia. Eur Rev Med PharmacolSci. 2014;18:1513–6. [PubMed] [Google Scholar]
- 22.Zhang HW, Jin JL, Cao YX, Liu HH, Zhang Y, Guo YL, et al. Prognostic utility of heart-type fatty acid-binding protein in patients with stable coronary artery disease and impaired glucose metabolism: Acohort study. CardiovascDiabetol. 2020;19:15. doi: 10.1186/s12933-020-0992-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ho SK, Wu YW, Tseng WK, Leu HB, Yin WH, Lin TH, et al. The prognostic significance of heart-type fatty acid binding protein in patients with stable coronary heart disease. SciRep. 2018;8:1–7. doi: 10.1038/s41598-018-32210-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oktay B, Akbal E, Firat H, Ardic S, Akdemir R, Kizilgun M. Evaluation of the relationship between heart type fatty acid binding protein levels and the risk of cardiac damage in patients with obstructive sleep apnea syndrome. Sleep Breath. 2008;12:223–8. doi: 10.1007/s11325-007-0167-1. [DOI] [PubMed] [Google Scholar]
- 25.Başar Ö, Akbal E, Köklü S, Tuna Y, Koçak E, Başar N, et al. Increased H-FABP concentrations in nonalcoholic fatty liver disease. Herz. 2013;38:417–22. doi: 10.1007/s00059-012-3714-x. [DOI] [PubMed] [Google Scholar]
- 26.Parsanathan R, Jain SK. Novel invasive and noninvasive cardiac-specific biomarkers in obesity and cardiovascular diseases. MetabSyndrRelatDisord. 2019;18:10–30. doi: 10.1089/met.2019.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kasliwal RR, Bansal M, Desai N, Kotak B, Raza A, Vasnawala H, et al. A Study to derive distribution of carotid intima media thickness and to determine its correlation with cardiovascular risk factors in asymptomatic nationwide Indian population (SCORE-India) Indian Heart J. 2016;68:821–7. doi: 10.1016/j.ihj.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adolphe A, Cook LS, Huang X. A cross-sectional study of intima-media thickness, ethnicity, metabolic syndrome, and cardiovascular risk in 2268 study participants. Mayo Clin Proc. 2009;84:221–8. doi: 10.4065/84.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faeh D, William J, Yerly P, Paccaud F, Bovet P. Diabetes and pre-diabetes are associated with cardiovascular risk factors and carotid/femoral intima-media thickness independently of markers of insulin resistance and adiposity. CardiovascDiabetol. 2007;24:6–32. doi: 10.1186/1475-2840-6-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Parildar H, Gulmez O, Cigerli O, Unal AD, Erdal R, Demirag NG. Carotid artery intima media thickness and HsCRP; predictors for atherosclerosis in prediabetic patients. Pak J Med Sci. 2013;29:495–9. doi: 10.12669/pjms.292.3133. [DOI] [PMC free article] [PubMed] [Google Scholar]


