Abstract
Aim:
This study aims to assess the diagnostic accuracy of new custom-made pulse oximeter sensor holder in assessment of actual pulp status with three pulp sensibility tests.
Materials and Methods:
Seventy-nine single canal teeth requiring endodontic therapy was included in the study. The tooth that was requiring root canal treatment was tested with heat test, cold test, electric pulp test, and pulse oximeter. Between each test, a time period of 2 min was allowed. The response from three pulp sensibility tests and the reading from pulse oximeter were recorded. Following which root canal treatment was performed. The result obtained from four pulp tests were correlated with the clinical finding after access cavity preparation. The data obtained was statistically assessed. Receiver operator characteristic (ROC) curve analysis was performed to assess the efficacy of the pulp tests. In the above statistical tools, the probability value. 05 is considered as significant level.
Results:
The overall diagnostic accuracy was found to be significantly higher with pulse oximeter when compared with other three pulp sensibility tests. The ROC curve demonstrates the results obtained from pulse oximeter was found to be more reliable than other pulp tests.
Conclusion:
Within the limitation of the study, diagnostic accuracy of pulse oximeter with custom made sensor holder was reliable and accurate in assessment of actual pulp status.
Keywords: Cold test, electric pulp test, heat test, pulse oximeter
Introduction
Primary care is the essential need for a human population where they receive care for most of their everyday health needs. Accurate diagnosis of clinical condition, treatment of symptomatic illness, disease prevention, health maintenance, counselling, and patient education are the various bodies which the primary care includes.[1] It is the foremost duty of a dental clinician to accurately diagnose the clinical condition in case of symptomatic patients who report to dental clinic with pain. When we introspect the role of dentistry, it is a known fact that the practice of general dentistry is primary care.
Diagnosis of the clinical condition plays a decisive role in dental treatment plan. Accurate and reliable diagnosis of the actual condition of the tooth plays a significant role in the prognosis of the treatment. In order to achieve this there should be appropriate, accurate, reliable, and objective pulp test that can identify the actual status of pulp whether healthy (vital), symptomatic irreversible pulpitis, or pulp necrosis.[2]
The pulp tests, which are traditionally used in endodontic practice, are the pulp sensibility tests. There are numerous studies in the literature, which had reported the diagnostic accuracy of heat test, cold test, and electric pulp test. At different clinical situations one cannot rely on these pulp tests to arrive at a diagnosis especially in traumatic injuries. These pulp sensibility test may not always translate the actual clinical condition of pulp.[3] Also, we know that the diagnosis cannot be made only by performing the pulp test, it requires a combined assessment of clinical and radiographic examination. These pulp tests are based on patient's subjective response, so the reliability of these tests is questionable. Because there might be possibility for an apprehensive patient to misinterpret and provide an inappropriate result to the operator.
Pulse oximeter, a non-invasive device has been introduced into endodontics for assessing the vascular response in the pulp. This device has pulse oximeter monitor, sensor holder, and sensor holding probe. The blood supply to the pulp can be assessed based on the oxygen saturation levels to the tooth. This serves to be a reliable indicator and objective test in assessing the actual status of the pulp.[4]
The authors of the present study have designed a custom-made pulse oximeter sensor holding device, which aids in effective positioning of the sensor in order to record the pulpal status of the tooth.
Therefore, the aim of this study is to design a customized pulse oximeter sensor probe holder in determining the vitality of permanent teeth and to evaluate the diagnostic accuracy of pulse oximeter, heat test, cold test and electric pulp test to identify the actual status of pulp in the teeth requiring root canal treatment.
Materials and Method
It is a prospective observational diagnostic trail. Approval for the study was obtained from the Institutional Review Board of Saveetha Institute of Medical and Technical Sciences, Chennai, India [SRB Ref No: SRB/SDMDS11/17ODS/11]. Institutional ethical committee approval has been obtained and approval number has been mentioned as (SRB Ref No). Date of approval 28.11.2017. The sample size was determined from the previous study[5] using G power 3.1 version. The sample size of 79 single rooted teeth was arrived by assuming alpha error- 0.05 and power of the study as 0.95. Single rooted teeth requiring endodontic therapy, teeth that require intentional root canal treatment for prosthodontic considerations and teeth with deep carious lesions were included in the study.
Patients with systemic complications, inability to respond to pulp testing (Intellectual disabilities), presence of developmental defects, presence of resorption, pulp canal obliteration were excluded from the study.
Seventy-nine single rooted teeth matching the inclusion criteria were included in the study. The study participants were recruited from the pool of patients in the Department of Conservative Dentistry and Endodontics at Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Chennai, India. 18 to 56-year-old male and female patients were included in the study.
Three blinded operators were involved in the study. First operator recorded the clinical and radiographic examination, second operator performed all the pulp vitality tests, and the third operator performed the access cavity preparation. The order of testing was the cold test, heat test followed by electric pulp tester, and then the pulse oximeter, with a time lag of 2 minutes between each test for the central sensitization to occur. In every patient all 4 pulp tests were performed i.e. cold test, heat test, electric pulp tester, and pulse oximeter.
Pulp testing
Cold test: Double ended ear bud was saturated with 1, 1, 1, 2- tetrafluoroethene spray outside the range of subject's vision. The bud was held back until it was frosty, following which, it was applied on the middle third of the labial surface of the tooth. An interval of 2 minutes was allowed to minimize the influence of one test over the other.
Heat test: Following isolation and drying the tooth a layer of petroleum jelly was smeared on the labial surface of the tooth to avoid sticking of gutta percha to the surface. One end of the gutta percha stick was heated on the flame out of the subject's sight to the point till it gets softened and just begins to glisten. Heated gutta percha stick was gently applied on middle third of the labial surface for 10 seconds or until a sensation was felt, which ever was earlier.
Electric pulp tester: After cleaning the probe of electric pulp tester with alcohol, an electrolyte was applied and placed on middle third of the labial surface of the tooth. Tip of the probe was placed on the tooth and lip clip was placed. The contra lateral tooth was used as control. If the current required to gain a response from the test tooth was the same as needed to excite the control, the pulp of the test group was considered normal, and was recorded as a positive response. The pulp of the test group was considered to be degenerating when much more current was required to gain a response compared to the control and was recorded as a negative response. Lack of response was also recorded as a negative response. Two readings were taken for each tooth, with an interval of 5 min, and the average was recorded.
Pulse Oximeter: Pulp testing was carried out with pulse oximeter using the probe. Reading for oxygen saturation was noted on the index finger of each subject, which was kept as a gold standard for comparison of the readings obtained on teeth. Probe was placed on the labial surface in middle third of the crown in order to fit closely to the tooth surface. Care was taken to place the sensor on the palatal surface so that the red - infrared rays pass from labial to palatal surface through the middle of the crown thereby, creating a long axis that was perpendicular to the axis of the crown. Each tooth was evaluated for 30 seconds following which the readings obtained on the pulse oximeter were recorded. After performing pulp vitality test, access cavity preparation was performed and presence or absence of bleeding from the canal orifice was noted. Bleeding from the canal orifice is inferred to be vital and absence of bleeding was considered to be pulp necrosis.
The response was tabulated and was analyzed statistically.
Statistical analysis
The collected data were analyzed with IBM. SPSS statistics software 23.0 Version. To describe about the data descriptive statistics, frequency analysis and percentage analysis was used. To analyze the diagnostic accuracy of pulp tests Receiver Operator Characteristic (ROC) curve analysis, Sensitivity, Specificity, Positive Predictive Value (PPV) and Negative Predictive Value (NPV) was performed. In the above statistical tools, the probability value. 05 is considered as significant level.
Results
Sensitivity, Specificity, Positive and Negative predictive value of pulse oximeter, thermal and electric pulp test was performed [Tables 1-4]. Outcome results of all the pulp tests was compared with clinical finding (i.e direct visual examination of access cavity) [Table 5, Figure 1]. ROC curve analysis was performed [Graph 1]. From the results of the present study it can be interpreted that, pulse oximeter is more reliable in diagnosing the actual pulpal status and was in correlation with the actual clinical finding. The results were found to be highly significant with P < 0.01 level [Table 6].
Table 1.
Heat test- % of accuracy
| Sensitivity | 55.00 |
| Specificity | 79.49 |
| PPV | 73.33 |
| NPV | 63.27 |
| Accuracy | 67.24 |
Table 4.
Pulse oximeter - % of accuracy
| Sensitivity | 97.50 |
| Specificity | 100.00 |
| PPV | 100.00 |
| NPV | 97.50 |
| Accuracy | 98.75 |
Table 5.
Outcome comparison of pulp tests
| Heat test | Cold test | EPT | Pulse oximeter | Clinical finding | |
|---|---|---|---|---|---|
| Response | 38.0 | 49.4 | 55.7 | 49.4 | 50.6 |
| No Response | 62.0 | 50.6 | 44.3 | 50.6 | 49.4 |
Figure 1.
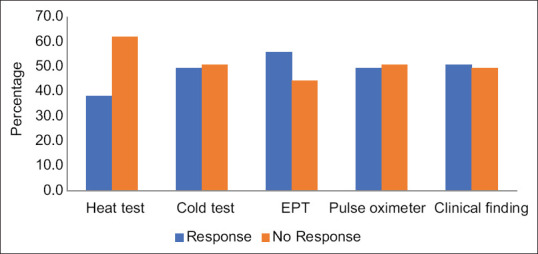
Outcome comparison
Graph 1.
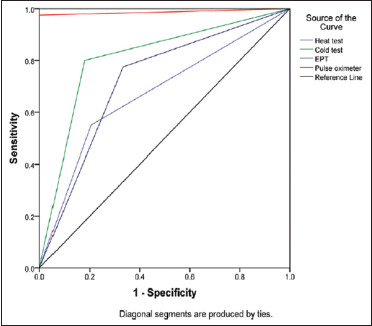
ROC Curve
Table 6.
Area under the curve
| Area Under the Curve | ||||
|---|---|---|---|---|
| Test Result Variable(s) | Area | P | 95% C. I | |
| Lower Bound | Upper Bound | |||
| Heat test | 0.672 | 0.008 ** | 0.552 | 0.793 |
| Cold test | 0.810 | 0.0005 ** | 0.710 | 0.911 |
| EPT | 0.721 | 0.001 ** | 0.606 | 0.836 |
| Pulse oximeter | 0.988 | 0.0005 ** | 0.959 | 1.000 |
** Highly significant at P<0.01 level
Table 2.
Cold test- % of accuracy
| Sensitivity | 80.00 |
| Specificity | 82.05 |
| PPV | 82.05 |
| NPV | 80.00 |
| Accuracy | 81.03 |
Table 3.
EPT- % of accuracy
| Sensitivity | 77.50 |
| Specificity | 66.67 |
| PPV | 70.45 |
| NPV | 74.29 |
| Accuracy | 72.08 |
Discussion
The assessment of pulp vitality plays a crucial role in deciding the treatment plan. It is the well-known fact that it is not always advisable to decide the treatment plan only on the basis of pulp sensibility tests, which most of the dentists practice in their routine clinical scenario. The authors of the present study keep a standpoint that the major reason for most of the clinicians who are not using pulp vascularity test in day to day dental practice is due to difficulty in procuring the device as it has been not commercialized yet.
Based on the recent systematic review[6] it was evident that previously published articles had high risk of bias. Most of the studies did not incorporate reference standard in their article.[7]
Over the recent years, clinical trial performed on paediatric age group did not mention the type of sensor and sensor holder used in their study[8]
There are previous reports on the usage of pulse oximeter device for the assessment of oxygen saturation levels in pulpal diseases.[2,5,9,10,11,12,13,14,15,16,17] Different studies used different sensor and sensor holding probes. Sensor and sensor holding probes varied among different studies.
There were many drawbacks in all the previously mentioned studies. Therefore, the present study was performed to address the existing lacunae. Though the previous authors have customised their own pulse oximeter device to assess the actual pulp status, few studies failed to assess its accuracy along with the other sensibility tests,[10,13] It is not possible to assess the accuracy of the device without comparing other pulp tests. Therefore, the present study was designed to test the accuracy of pulse oximter in comparison with thermal and electrical pulp tests.
Moreover, correlating the results of the pulp tests with the actual clinical finding is considered to be the gold standard method in assessing the accuracy of the device. Due to ethical constrains, it is not always possible to correlate with the direct inspection of the access cavity, especially in conditions with vital pulp, which does not require an endodontic treatment. The authors of the present study correlated the findings of pulp tests to the direct examination of the access cavity. The teeth that showed vital response with pulse oximeter were not included for the direct visual examination of access cavity assessment.
An important part of this study was to make a specific dental probe for utilizing the pulse oximeter in endodontic diagnosis. Special dental probes have not been manufactured for the dental market, and this is a major limitation of the use pulse oximetr in endodontics. Noblett et al.[18] designed an invitro model to assess the pulpal circulation using pulse oximeter. He used a rubber dam clamp as the sensor. Kahan et al.[17] and Gopikrishna et al.,[5] Karayilmaz et al.[19] used innovative probes in their studies. Finger or ear sensors has been used in few previous studies.[5,9,15,20] The authors of this study keep a standpoint that though finger or ear sensors are been employed, the size of these sensor are much larger, so when these are embedded in the sensor holding probe its total size becomes larger to adapt to the external tooth surface.[9,12] In the present study neonatal sensor was used and the sensor holder was designed and custom made to aid in accurate placement on the tooth surface. 3D printing method was used to fabricate the flexible sensor holder, which facilitated the ease of placement on the tooth surface.
There are so many factors which influence the results of the pulp vitality. They are the type of the sensor and sensor holding probe, the age of the patient, gender of the patient, and general systemic conditions. Gender to a certain extent influence the interpretation of pulp sensibility tests as it is based on patient's subjective response. Apprehensive female patients fail to interpret the exact response, which might eventually lead to misdiagnosis. When it comes to the use of pulse oximeter, there is also probability that patients with systemic disorder (cardiovascular disease, high venous pressure, low peripheral perfusion and hypotension) might have correlation with oxygen saturation level.[20] The results of Goho et al.[21] reported that patient's systemic circulation does not has any correlation with oxygen saturation levels.
The author of the study strongly opines that age of the patients influence the oxygen saturation levels of the pulp. It is a well known that as age advances, pulp volume deceases with increased deposition of mineralized tissue.[22] The above-mentioned mechanism leads to atherosclerotic changes in the blood vessels.[18] Therefore, in older patients the oxygen saturation reading of a healthy normal pulp tends to be a reduced value. Under such instance the dentists should not falsely interpret and perform unnecessary endodontic management. Keeping this in focus, the authors of this study interpreted the results of pulse oximeter values when performed on older individuals.
In the present study the overall diagnostic accuracy of four pulp tests were assessed. Amongst all the pulp tests, pulse oximeter showed highest diagnostic accuracy. Receiver operating characteristic curve was plotted against sensitivity and specificity. The test is said to be accurate when the ROC curve originates from the left handed border and reaches the top border of ROC space, away from 45-degree diagonal line. This shows pulse oximeter test to be reliable in assessing the actual pulp status.
The other interesting point is that three investigators were involved in the present study, which was not employed in the previous studies. This reduces the operator induced bias and review bias. Therefore, the authors of this study strongly opine the reliability and accuracy of the results obtained from the pulp tests.
Future implication
The efficiency of pulse oximeter in assessing the pulpal status of the tooth that had undergone revascularization treatment would bring about revolution and change the future scope of endodontics.
Conclusion
Within the limitations of the study, it can be concluded that customized pulse oximeter sensor holder proves to be accurate, reliable, and objective in assessing the actual condition of the tooth.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gambhir RS. Primary care in dentistry-An untapped potential. J Fam Med Prim Care. 2015;4:13–8. doi: 10.4103/2249-4863.152239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dastmalchi N, Jafarzadeh H, Moradi S. Comparison of the efficacy of a custom-made pulse oximeter probe with digital electric pulp tester, cold spray, and rubber cup for assessing pulp vitality. J Endod. 2012;38:1182–6. doi: 10.1016/j.joen.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 3.Yanpiset K, Vongsavan N, Sigurdsson A, Trope M. Efficacy of laser Doppler flowmetry for the diagnosis of revascularization of reimplanted immature dog teeth. Dent Traumatol Off Publ Int Assoc Dent Traumatol. 2001;17:63–70. doi: 10.1034/j.1600-9657.2001.017002063.x. [DOI] [PubMed] [Google Scholar]
- 4.Krishna VG, Kandaswamy D, Gupta T. Assessment of the efficacy of an indigeniously developed pulse oximeter dental sensor holder for pulp vitality testing. Indian J Dent Res. 2006;17:111–3. doi: 10.4103/0970-9290.29880. [DOI] [PubMed] [Google Scholar]
- 5.Gopikrishna V, Tinagupta K, Kandaswamy D. Evaluation of efficacy of a new custom-made pulse oximeter dental probe in comparison with the electrical and thermal tests for assessing pulp vitality. J Endod. 2007;33:411–4. doi: 10.1016/j.joen.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Lima TFR, dos Santos SL, da Silva Fidalgo TK, Silva EJNL. Vitality tests for pulp diagnosis of traumatized teeth: A systematic review. J Endod. 2019;45:490–9. doi: 10.1016/j.joen.2019.01.014. [DOI] [PubMed] [Google Scholar]
- 7.Ahn S-Y, Kim D, Park S-H. Long-term prognosis of pulpal status of traumatized teeth exhibiting contradictory results between pulp sensibility test and ultrasound Doppler flowmetry: A retrospective study. J Endod. 2018;44:395–404. doi: 10.1016/j.joen.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Mishra S, SSharma D, Bhusari C. Assessing inflammatory status of pulp in irreversible pulpitis cases with pulse oximeter and dental hemogram. J Clin Pediatr Dent. 2019;43:314–9. doi: 10.17796/1053-4625-43.5.2. [DOI] [PubMed] [Google Scholar]
- 9.Anusha B, Madhusudhana K, Chinni SK, Paramesh Y. Assessment of pulp oxygen saturation levels by pulse oximetry for pulpal diseases –A diagnostic study. J Clin Diagn Res JCDR. 2017;11:ZC36–9. doi: 10.7860/JCDR/2017/28322.10572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sadique M, Ravi SV, Thomas K, Dhanapal P, Simon EP, Shaheen M. Evaluation of efficacy of a pulse oximeter to assess pulp vitality. J Int Oral Health JIOH. 2014;6:70–2. [PMC free article] [PubMed] [Google Scholar]
- 11.Cerqueira M, Ferreira M, Caramelo F. Development and initial testing of a pulse oximetry prototype for measuring dental pulp vitality. J Phys Conf Ser. 2015;616:012001. [Google Scholar]
- 12.Samuel A comparative study of pulse oximetry with the conventional pulp testing methods to assess vitality in immature and mature permanent maxillary incisors [Internet] [Cited 2019 Dec 15]. Available from: http://www.cjhr.org/article.asp?issn=2348-3334;year=2014;volume=1;issue=4;spage=235;epage=240;aulast=Samuel .
- 13.Bargrizan M, Ashari MA, Ahmadi M, Ramezani J. The use of pulse oximetry in evaluation of pulp vitality in immature permanent teeth. Dent Traumatol Off Publ Int Assoc Dent Traumatol. 2016;32:43–7. doi: 10.1111/edt.12215. [DOI] [PubMed] [Google Scholar]
- 14.Mansi J. Pulp vitality tests in deciduous teeth: A comparative evaluation: An in vivo study. Uni JMed Dent Sci. 2014;2:90–5. [Google Scholar]
- 15.Pozzobon MH, de Sousa Vieira R, Alves AM, Reyes-Carmona J, Teixeira CS, de Souza BD, et al. Assessment of pulp blood flow in primary and permanent teeth using pulse oximetry. Dent Trauma. 2011;27:184–8. doi: 10.1111/j.1600-9657.2011.00976.x. [DOI] [PubMed] [Google Scholar]
- 16.Caldeira CL, Barletta FB, Ilha MC, Abrão CV, Gavini G. Pulse oximetry: A useful test for evaluating pulp vitality in traumatized teeth. Dent Traumatol Off Publ Int Assoc Dent Traumatol. 2016;32:385–9. doi: 10.1111/edt.12279. [DOI] [PubMed] [Google Scholar]
- 17.Kahan RS, Gulabivala K, Snook M, Setchell DJ. Evaluation of a pulse oximeter and customized probe for pulp vitality testing. J Endod. 1996;22:105–9. doi: 10.1016/S0099-2399(96)80283-4. [DOI] [PubMed] [Google Scholar]
- 18.Noblett WC, Wilcox LR, Scamman F, Johnson WT, Diaz-Arnold A. Detection of pulpal circulation in vitro by pulse oximetry. J Endod. 1996;22:1–5. doi: 10.1016/S0099-2399(96)80226-3. [DOI] [PubMed] [Google Scholar]
- 19.Karayilmaz H, Kirzioǧlu Z. Comparison of the reliability of laser Doppler flowmetry, pulse oximetry and electric pulp tester in assessing the pulp vitality of human teeth. J Oral Rehabil. 2011;38:340–7. doi: 10.1111/j.1365-2842.2010.02160.x. [DOI] [PubMed] [Google Scholar]
- 20.Chan ED, Chan MM, Chan MM. Pulse oximetry: Understanding its basic principles facilitates appreciation of its limitations. Res Med. 2013;107:789–99. doi: 10.1016/j.rmed.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Goho C. Pulse oximetry evaluation of vitality in primary and immature permanent teeth. Pediatr Dent. 1999;21:125–7. [PubMed] [Google Scholar]
- 22.Ikawa M, Komatsu H, Ikawa K, Mayanagi H, Shimauchi H. Age-related changes in the human pulpal blood flow measured by laser Doppler flowmetry. Dent Traumatol. 2003;19:36–40. doi: 10.1034/j.1600-9657.2003.00120.x. [DOI] [PubMed] [Google Scholar]


