Abstract
Context:
Road traffic accidents (RTA) are a foremost rising cause of morbidity and mortality in developing countries like India. The Government of India enacted a new motor vehicle amendment act (MVA) on September 1st 2019 that permits heavy penalties for traffic rule offenders.
Aims:
To find out the early impact of “THE MOTOR VEHICLES (AMENDMENT) ACT, 2019”.
Settings and Design:
A retrospective observational study was performed during the time period July to October 2019 on RTA patients admitted to the Trauma and Emergency department.
Methods and Materials:
Patients studied in two groups – One Pre MVA group (n = 371) and one Post MVA group (n = 415). The data were extracted from medical case records of the department and filled up in a structured format. Detailed demographic profile, including the use of safety measure and clinical variables such as the pattern of injury and injury severity scores, were recorded.
Statistical Analysis Used:
Statistical analysis was done by R version 3.6.1.
Results:
There is a 41% drop in RTA victims post MVA implementation. Polytrauma reduced (25% vs 45.5%) significantly (P = 0.002) and so was Injury severity score (6.00 vs 13.00). More RTA victims were wearing helmets as compared to previous (42% vs 18%), and there was a steep decline in the alcohol driving (25% vs 10%) between the pre and post MVA group. A significant reduction noted in the under 18 yrs. Two-wheeler riders in the post MVA group compared to earlier (P = 0.016).
Conclusions:
The study reveals that there is a commendable reduction in the injury severity, violation of safety gears, alcohol use and rash driving following the implementation of MVA September 2019. Primary care and family physician can play a crucial role in creating public awareness about the personal safety measures, which will help in strengthening of this law to reduce the incidence of RTA and the associated mortality and morbidity
Keywords: Family physician, injury severity score, motor vehicle act, road traffic accidents
Introduction
Road traffic accidents (RTA) are a foremost rising cause of morbidity and mortality globally due to rapid modernization.[1,2] As per the projection given by the WHO global burden of disease, the incidence of RTA will be on the rise to 2049 making it the second leading cause of disability-adjusted life years (DALY) in the developing countries.[3] In India itself for the year 2017, the Ministry of Road, Transport and Highways, Government of India (GOI), have reported 4,64,910 unfortunate incidences of RTA which claimed 1,47,913 lives.[3] Thus, the burden is enormous and economic loss is considerable.
The increasing density of the motor vehicles is outpacing the development of infrastructures such as roads and highways on one hand.[2] On the other side, there is ignorance and many a time willful violations of the existing safety rules that are primarily responsible for these untoward incidents.[3] Over speeding, drunken driving, use of mobile phones while driving willfully not using safety devices (helmets or seat belts while driving) and lack of maintenance of vehicles comprises a few of the violation of traffic rules.[4] In a recent study by Woldu et al., it has been seen that >80% of RTA caused by these enumerated reasons only which are preventable.[5] The government has been tirelessly trying a lot to reduce the incidence of RTA and prevent premature deaths with frequent public awareness, strict traffic rules with the imposition of fines and imposing some solutions from the developed nations. Yet the problems in our country are more in the user's perception that strict enforcement of rules is not possible making them vulnerable to risk. Hence, the GOI has come up with a new motor vehicle amendment act (MVA) that was implemented nationwide from September 1st 2019.[6] The law permits stringent punishment and hefty penalties for offenders. The aim is to have behavioural changes among the motor users, which would directly impact the incidence as well as the severity of injuries associated with RTA.
The objective of this study was to find out the impact of the new MVA in terms of clinico-epidemiological profile of RTA victims attending a trauma and emergency (T and E) department of a tertiary care centre located in the city Bhubaneswar, in eastern India.
Methods
Study design
This retrospective observational study was performed in the Department of Trauma and Emergency (T and E) of All India Institute of Medical Sciences Bhubaneswar. The approval obtained from the Institutional Ethics Committee (IEC Ref No: T/IM-NF/T and EM/19/45). Patients studied in two groups. One PreMVA group included RTA victims before the implementation of new MVA act on September 1st, 2019 (n = 2 months) and in the Post-MVA group included patients after September 1st, 2019 (n = 2 months).
Participants
All RTA patients attending to the department of T and E of our institute, during four months (July 1st till October 31st) included for comparison in the study. Patient's case file having inadequate data excluded from the study.
Data collection and variables
The data extracted from medical case records from the medical record department and filled up in a customized structured format. The demographic variables entered included were – age, sex, type vehicle involved in the accident, time of injury, time of arrival, mode of arrival to T and E and type of victim (driver, pillion rider, and pedestrian, etc.). The most important data retrieved were the use of safety gears (helmets/seatbelts) and alcohol consumption while driving. Clinical variable noted include injured area that classified as head injury (HI), maxillofacial injury (MF), chest injury (CI), abdominal injury (AI), extremity injury (Ext I), and soft tissue injuries (STI). The injury severity score (ISS) of the trauma patient was calculated based on the injury pattern.
Study size
In total 371 patients having data on required parameters included in preMVA group and 415 patients included in postMVA group for final data analysis.
Statistical methods
Statistical analysis was done by R version 3.6.1. Categorical variables expressed as percentage. Numerical variables (non-parametric) expressed as median with IQR. Bivariate analysis between categorical variables done by Chi-square test, and between categorical and numeric variables (non-parametric) done using Kruskal–Wallis rank-sum test comparing more than two groups. P < 0.05 regarded as statistically significant.
Results
The flow diagram of the subjects included in the study depicted in Figure 1. A total of 912 RTA patients visited T and E in the Pre MVA group, of which 371 patients met the inclusion criterion and taken for analysis. Similarly, of a total of 537 patients in the postMVA group, 415 were analyzed. The trend of the monthly statistics of six months of the preMVA and two months the postMVA group shown in Figure 2. There are 41% drops in RTA victims postMVA implementation. The median age of patients in these four months was 29 years (20–41) (1–69). The gender distribution was M: F 82%:18%. The mode of transportation to T and E was ambulance (58%), police control room van (8%), self-transportation (6%), and private vehicles (26%). In total, 14% of patients reached the T and E within 1 h (i.e. golden hour). The most common time of accidents (23%) were in the evening time (4 p.m. to 8 p.m.) followed by noon (12 p.m. to 4 p.m.) as seen in Figure 3. Analysis of vehicles involved in RTA, revealed two-wheelers in 56%, three-wheelers in 15%, four-wheelers in 12%, and heavy vehicle (more than 4 wheels) in about 15%. In contrast, 2% were pedestrian who suffered injuries due to rash driving of vehicles. The use of safety gear, particularly the helmet statistically improved (P = 0.001) while alcohol consumption among drivers statistically reduced (P = 0.01) after MVA implementation in Figure 4. The ISS comparison between two-wheeler drivers with and without helmet and influence of alcohol were statistically significant (P < 0.01), as shown in Figure 5. The injury severity score of patients before and after MVA demonstrated in the jitter plot [Figure 6] which shows a statistically significant reduction (P = 0.0015). There was a significant reduction in the two-wheeler drivers under the age of 18 years in the postMVA group (P = 0.016). The early death rate also reduced though it is not statistically significant.
Figure 1.
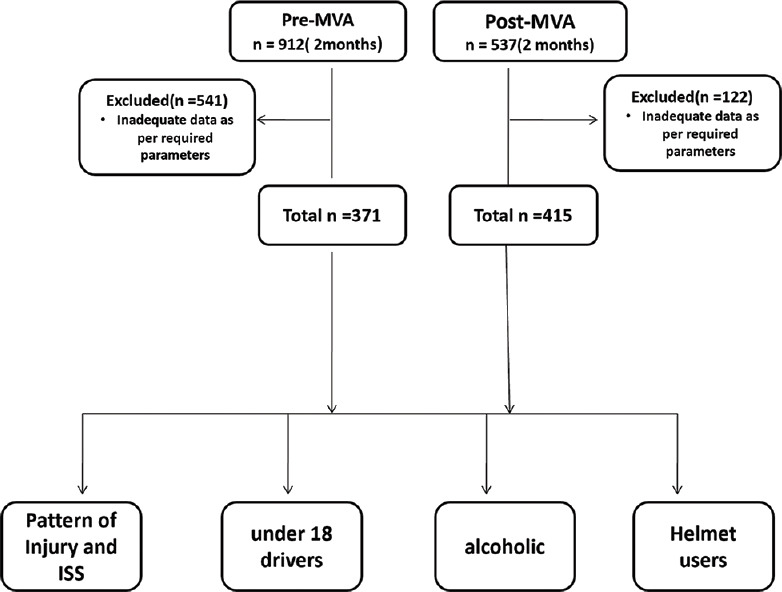
Flow diagram of patients recruited in the study
Figure 2.
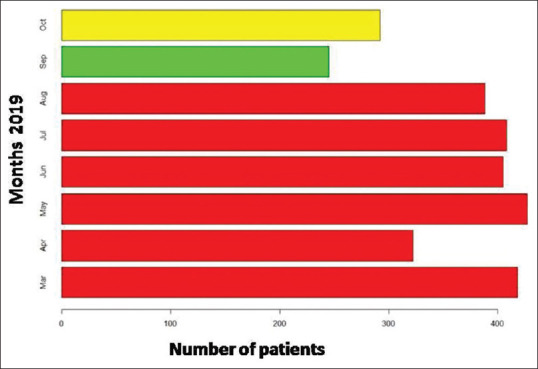
Bar diagram depicting the trend of monthly statistics of RTA victims
Figure 3.
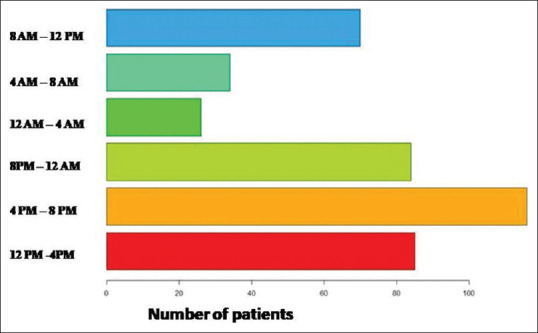
Bar diagram depicting the time of injury of RTA victims
Figure 4.
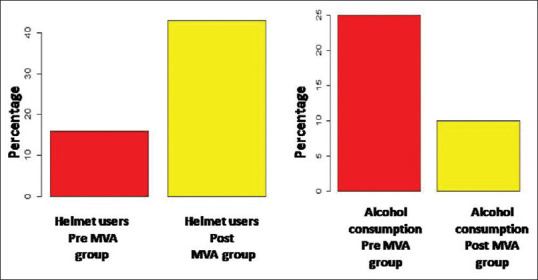
Percentage of helmet users and alcoholics before and after MVA act
Figure 5.
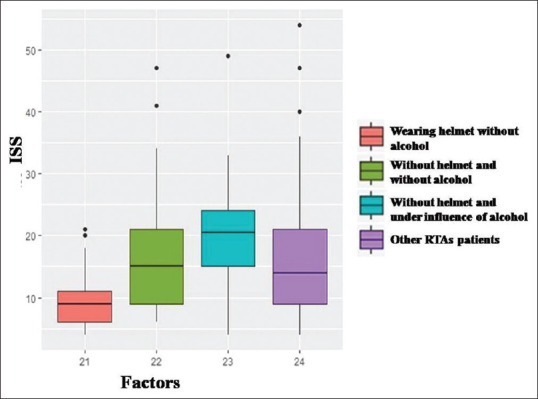
Boxplot depicting the ISS among the drivers with relation to helmet usage and alcohol consumption
Figure 6.
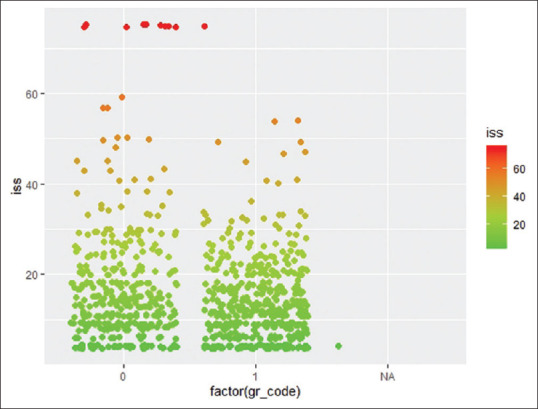
Jitter plot depicting the ISS in the pre- and post-MVA group
The comparative results summarized in Table 1.
Table 1.
Comparison of clinical profile of patients of both the groups
| Variables | Pre MVA (n=371) | Post MVA (n=415) | P value |
|---|---|---|---|
| Helmet users | 18% | 42% | 0.001* |
| Alcoholic | 25% | 10% | 0.01* |
| ISS | 14.00(9.00-22.00) [4.00-75.00] | 12.00 (8.00-20.00) [4.00-75.00] | 0.0015" |
| Polytrauma (ISS >15) | 167(45.6%) | 104(25%) | 0.002* |
| under 18 drivers (2 wheelers) | 24(6.46%) | 7(2.2%) | 0.016* |
| Head injury (HI) | 203(53.5%) | 168(40.4%) | 0.066 |
| Maxilla-facial (MFI)injury | 113(29.3%), | 96(23.1%) | 0.467 |
| Combined HI+MFI | 92(24.2%) | 82(19.7%) | 0.56 |
| Early death rates | 19(n=912) = 2% | 8(n=537) =1.4% | 0.74 |
*P<0.05- statistically significant.
Discussion
The global burden of RTA deaths per year is more than 1.2 million annually, and a whopping 90% of these come from the developing countries.[1,3] The world bank's traffic faculties and economic growth have projected a substantial rise up to 144% in the RTAs in the South Asian region in coming years and India tops the list.[3] The government of India (GOI) has recognized injury as a significant public health issue due to daily incurring an enormous economic loss. With the population of both the human and vehicle rising unprecedented, the challenge to curb the menace remains an uphill task. Majority of the RTA with the resulting morbidity and mortality are preventable, if the rules and regulations of the roads are strictly followed while driving. To the contrary, people are callous in obeying the traffic rules as the penalty before the MVA were either meager or the majority of the offenders could easily escape with. The Motor vehicle act 2019 by GOI is one of the new initiatives to the existing rules that have been implemented nationwide from September 1st. The imposition of hefty penalty, including cancellation of driving licenses and imprisonment, for breaking the traffic and driving rules aimed to change the behaviour of the road users towards safety.[7] Our study of the epidemiology of RTA victims brought to the T and E is an indirect measure of the outcome of the success of the MVA act whose ultimate goal is to reduce the injury burden.
After the nationwide implementation of the rules, we see a substantial reduction in the number of injured victims attending the T and E department in the very first month. There is a reduction, although not statistically significant in the number of head injuries (HI) and maxilla facial injuries (MFI) among the two-wheelers users, who unfortunately are the population at risk. This is due to the strict use of crash helmet and a hefty penalty for offenders that have increased to ten times than previous fees. The helmet users have risen from 18% to 42%, but still there is another 58% who were not using in our study. A universal acceptance with a higher percentage of users can make a significant impact in HI and MFI, which is protected by the helmets. The state government gave a time-bound waiver (3 months) of the implementation of MVA act after a week time,[8] and we can see a small rise in the RTA number in the subsequent month. However, the educated public that started to adopt and adhere to the new rules possibly, which may be the reason for lower monthly statistics of trauma victims.
Among the various parameters studied in the injured patient, the MVA had no effect on the gender distribution and time of injury. These remained more or less the same as compared to previous studies done in India.[2,4,9,10,11] Though the mean age of victims remains similar, the MVA had stringent rules for <18 aged drivers. When we compare the data of these non-adult (<18), there is a steep fall in this age group. Rolison et al. and Woldu et al. have noted that an increase in drivers age and experience has an inverse relationship with self-reported crashes.[12]
The two-wheeler riders remain the more affected population, which attributed to the inherently unstable type of vehicle.[2,10] The motorcycle remains the most popular mode of transpiration in our belt in both rural and urban places.[9] The pedestrian's injury has also seen a downslope. This may be due to fewer incidence of rash driving. Hayde et al. found that vehicles with speed exceeding 60 km/h were associated with an increased risk of fractures. MVA prohibits over speeding of vehicles. Also, the installed camera system having a constant vigilance on the roads creates a sense of fear among the motor vehicle riders so as not to violate the traffic rules.
The use of helmet had a protective effect as can be seen in our study. The MVA has caused a significant behavioural change, as more victims were wearing helmets in the post MVA phase (42% vs 18%) and there was also a decrease in the ISS (6.00 vs 13.00). Similarly, there is a significant reduction in the incidences of drunken driving postMVA (10% vs 25%). This is depicted in [Figure 3]. Fitzharris had reported five-times higher head injury and prehospital deaths among riders not wearing safety gear.[13] Hayde et al. and Woldu et al. have also reported drunkenness as an important distracter with higher odds ratio of injury.[5,11] Kirk et al. have found that ride-hailing has reduced the RTA in the suburbs by lowering the drunk driving. Cell-phone usage significantly increases the risk for the crash, as shown by studies abroad.[14,15] In India, Hayde et al. in their study found a significant relationship between RTA and mobile users.[11] However, we found there was a lot of concealment and apprehension among the users to declare the usage of phones. Hence the data could not be collected. MVA forbids alcohol consumption or mobile usage for the drivers.
The mode of transportation to our T and E has been manly by the ambulance, and patrolling police control room vans (57% and 8%, respectively). The GOI has made “108” a universal code for ambulance help for the pubic, which is mainly responsible for transportation.[16] Our hospital being close to the national highway is under constant police patrolling, and they bring in the victims immediately within the crucial hour of injury.
Soft tissue injuries, fractures and head injuries were the most common injuries in our study in both the pre and postMVA though the proportions have changed. The median ISS is less in postMVA and incidence of polytrauma has reduced (25% vs 46%). Some authors have noted limb injuries as more common pattern in other cities of India.[9,10,11] Elsewhere, Wui et al. have found HI as the most prevalent injury in their series.[16] Leg bones remain the common bone universally to have fractured and compounding as seen among the two-wheeler riders.[2,10,11]
The early death rate (<24 h of admission) after RTA showed a decrease from 2% to 1.4% after the MVA. In a study by Singh et al., they have reported a death rate of 6.3%.[17] Traumatic brain injury (TBI) was the most common cause of death and reported similarly in other studies.[17] Our study corroborates ISS > 16 were associated with increased morbidity and mortality. Byun et al. also found a higher ISS score among nonsurvivors than survivors.[18]
Our study is an immediate impact of the new MVA on injury epidemiology. However, the dilution of law by relaxation period for 3 months in our state must have reduced strength of the study. With time, the awareness among the people bound to increase and the actual impact can be assessed with the multicenter study.
In our state, after implementation of the law, there was public outrage due to imposition of a hefty amount of penalty, so the state government forced to give a relaxation period. Primary care and family physician can play a crucial role in creating public awareness about the personal safety measures and also to follow traffic rules and regulations which will help in strengthening of this law to reduce the incidence of RTA and the associated mortality and morbidity
Conclusion
New motor vehicle amendment act of 2019 has reduced the number of trauma victims presenting to the emergency department of our institute. There is also a decrease in injury severity score as well as polytrauma compared to the pre-implementation months. The number of helmet users has risen, and more drivers are abstaining from alcohol than previously. The adolescent drivers (<18 years) have also reduced significantly. These signals towards a positive impact on road traffic accidents and early success of this new law.
Declaration of ethical committee clearance
The approval obtained from the Institution Ethics Committee (IEC Ref No: T/IM-NF/T and EM/19/45) dated 4th November 2019.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pal R, Ghosh A, Kumar R, Galwankar S, Paul S, Pal S, et al. Public health crisis of road traffic accidents in India: Risk factor assessment and recommendations on prevention on the behalf of the Academy of Family Physicians of India. J Fam Med Prim Care. 2019;8:775–83. doi: 10.4103/jfmpc.jfmpc_214_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Misra P, Majumdar A, Misra M, Kant S, Gupta S, Gupta A, et al. Epidemiological study of patients of road traffic injuries attending emergency department of a trauma center in New Delhi. Indian J Crit Care Med. 2017;21:678–83. doi: 10.4103/ijccm.IJCCM_197_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Isaac M, Parr M. Comprehensive Trauma Life Support by International Trauma Care (Indian Chapter) 5th ed. Erode: 2016. Introduction; pp. 01–3. Available from: https://www. indiamart.com/comprehensive-traumalife/aboutus.html . [Google Scholar]
- 4.Liang M, Zhang Y, Qu G, Yao Z, Min M, Shi T, et al. Epidemiology of fatal crashes in an underdeveloped city for the decade 2008-2017. Int J Inj Contr Saf Promot. 2020;9:1–8. doi: 10.1080/17457300.2020.1737140. [DOI] [PubMed] [Google Scholar]
- 5.Woldu A, Desta A, Woldearegay T. Magnitude and determinants of road traffic accidents in Northern Ethiopia: Across-sectional study. BMJ Open. 2020;10:e034133. doi: 10.1136/bmjopen-2019-034133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Highways, Ministry of Road transport and Transport Research wing. Road accidents in India-2017 [Internet] 2018. Available from: https://morth.nic.in/sites/default/files/Road_Accidednt.pdf .
- 7.MINISTRY OF LAW AND JUSTICE. THE MOTOR VEHICLES (AMENDMENT) ACT [Internet]. India. 2019. Available from: http://egazette.nic.in/WriteReadData/2019/210413.pdf .
- 8.Odisha Relaxes New Traffic Rules for 3 Months After Mob Clashes With Police Over Hefty Fines. News 18 [Internet] 2019. Available from: https://www.news18.com/news/india/odisha-relaxes-new-traffic-rules-for-3-months-after-mob-clashes-with-police-over-hefty-fines-2302715.html .
- 9.Kashid M, Rai SK, Nath SK, Gupta TP, Shaki O, Mahender P. Epidemiology and outcome of trauma victims admitted in trauma centers of tertiary care hospitals-A multicentric study in India. Int J Crit Illn Inj Sci. 2020;10:9–15. doi: 10.4103/IJCIIS.IJCIIS_77_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pathak S, Jindal A, Verma A, Mahen A. An epidemiological study of road traffic accident cases admitted in a tertiary care hospital. Med J Armed Forces India. 2014;70:32–5. doi: 10.1016/j.mjafi.2013.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hadaye R, Rathod S, Shastri S. A cross-sectional study of epidemiological factors related to road traffic accidents in a metropolitan city. J Fam Med Prim Care. 2020;9:168–72. doi: 10.4103/jfmpc.jfmpc_904_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rolison J, Regev S, Moutari S. What are the factors that contribute to road accidents? an assessment of law enforcement views, ordinary drivers’ opinions, and road accident records. Accid Anal Prev. 2018;115:11–24. doi: 10.1016/j.aap.2018.02.025. [DOI] [PubMed] [Google Scholar]
- 13.Fitzharris M, Dandona R, Kumar G, Dandona L. Crash characteristics and patterns of injury among hospitalized motorised two-wheeled vehicle users in urban India. BMC Public Heal. 2009;9:11. doi: 10.1186/1471-2458-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lipovac K, Đerić M, Tešić M, Andric Z. Mobile phone use while driving-literary review. Transp Res Part F: Traffic Psychol Behav. 2017;47:132–42. [Google Scholar]
- 15.Caird J, Johmston K, Willness C, Asbridge M, Steel P. A meta-analysis of the effects of texting on driving. Accid Anal Prev. 2014;71:311–8. doi: 10.1016/j.aap.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 16.Wui L, Shaun G, Ramalingam G, Wai K. Epidemiology of trauma in an acute care hospital in Singapore. J Emerg Trauma Shock. 2014;7:174–9. doi: 10.4103/0974-2700.136860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh N, Singh R, Singh V, Jain P, Gupta P, Singh A. Clinico-epidemiological profile of trauma victims in a tertiary care hospital in rural setting of central Uttar Pradesh. Indian J Community Heal. 2017;29:424–8. [Google Scholar]
- 18.Byun C, Park I, Oh J, Bae K, Lee K, Lee E. Epidemiology of trauma patients and analysis of 268 mortality cases: Trends of a single center in Korea. Yonsei Med J. 2015;56:220–6. doi: 10.3349/ymj.2015.56.1.220. [DOI] [PMC free article] [PubMed] [Google Scholar]


