Abstract
Context:
Competitive exams conducted for undergraduate and postgraduate medical courses in India are tough. The undergraduate course is additionally taxing to the students’ health. Lack of physical activity, the stress of studies, and universal adoption of different gadgets make the undergraduate medical students prone to develop musculoskeletal pain-related issues.
Aims:
This study aimed to evaluate the prevalence of neck pain and the associated factors including gadget use among undergraduate medical students of a premier medical college in central India.
Settings and Design:
All undergraduate medical students including the interns of our institute were enrolled for this cross-sectional study.
Methods and Materials:
A self-explanatory internet-based questionnaire prepared using Kobo Toolbox was circulated via WhatsApp and email by the class representative of each batch of students. The responses obtained were analyzed using Statistical Package for the Social Sciences (SPSS).
Statistical Analysis Used:
Proportions and means were calculated. Chi-square test and univariable logistic regression analysis were used.
Results:
Three hundred thirty-one valid responses out of 423 responses were analyzed. In total, 58.3% of 331 students suffered from neck pain within the last one year. Students in the 3rd and 4th year had 2.9 times higher odds of current neck pain in comparison to 1st-year students. History of neck pain before joining the course was associated with a higher risk of having current neck pain. Self-perceived aggravation of pain from gadget use had significantly higher odds of contributing to the current episode of neck pain.
Conclusions:
Neck pain is not uncommon among undergraduate medical students. History of previous neck pain including that during schooling makes a student prone for the current episode of pain. Academic stress, smartphone and laptop use tend to aggravate the pain in those who have neck pain.
Keywords: Laptops, musculoskeletal pain, neck pain, smartphones, stress
Introduction
In India, the demand for doctors for serving the ever-increasing population is always there. Although many forms of medicine are practiced in India, the undergraduate program for obtaining the degree of modern medicine, i.e. Bachelor of Medicine and Bachelor of Surgery (MBBS) is much sought after. Students often start preparation for getting selected in one of the colleges offering the program during their adolescence. They frequently study for hours at a stretch, even joining dedicated coaching classes for entrance exam preparation; often at the cost of physical and recreational activities.[1] After joining the undergraduate course, students must study the basics of all modern medical subjects in a short span of four and a half years. Mid-way through the program, they are faced with the next challenge of getting selected in one of the post-graduate residency programs in reputed institutes, while continuing their undergraduate studies, which becomes clinically oriented over time. This additional burden forces the students to dedicate extra study hours, at times neglecting their own health.
The Global Burden of Disease (GBD) 2017 reported the musculo-skeletal conditions to be the second highest contributor of global disability.[2] While not found to be associated with mortality, neck pain was found to cause discomfort, disability, and impaired quality of life.[2,3] Undergraduate students have been reported to have a high prevalence of neck and upper extremity pains. The prevalence of neck pain has been reported as 48-78%.[3,4]
The rapid development and easy availability of communication technologies have led to their widespread use by the general public. Increasing usage of electronic gadgets like laptops, smartphones, tablets, and other wearable devices has been found to increase the incidence of neck pain in general and among students in particular.[5,6,7] It has been postulated that these devices force the user to keep the neck in a specific position for a long time, thereby putting a strain on the neck muscles and thus producing neck discomfort and pain.[5]
There are a few reported studies of the prevalence of neck pain in dental students and in undergraduate students of medicine from other parts of the world.[8,9,10] There are limited studies from India, which have focussed on the musculoskeletal pain (MSP) in undergraduate medical students (MBBS students). While Aggarwal et al.[11] have reported on the prevalence of low back pain and Gupta et al.[12] have reported on the prevalence of gadget use in Indian medical students, there is no study from India on the prevalence of neck pain among undergraduate medical students. With several undergraduate medical students reporting for neck pain at the Orthopaedic outpatient clinic of our hospital, we conceptualized and conducted this study to evaluate the prevalence and patterns of neck pain among undergraduate. Additionally, we have analyzed the demographic, clinical, and contextual factors, which might predict neck pain among the students.
Subjects and Methods
This was a cross-sectional study conducted on all the undergraduate medical students from the first year to the intern batch of our institute which is a premier tertiary care teaching hospital of central India. After obtaining clearances from the institutional research review board and the institutional human ethics committee (Approval number - LOP/2018/IM0204, 26/12/2018), a web-based self-administered questionnaire was developed using the Kobo Toolbox (Harvard Humanitarian Initiative), which is free for non-commercial use. Students who consented were required to proceed further with the questionnaire. There were no other exclusion criteria.
The questionnaire consisted of three broad sections – general demographic details, questions about neck pain along with further details about the presence of neck pain in their pre-medical years, and patterns of gadget use. Personal identification details were not collected to maintain confidentiality. The study was designed to be anonymous with no direct communication of researchers with the students. The class representatives were roped in for indirect communication. They were briefed about the study and a link to the questionnaire, participant information sheet, and figures were shared with them on WhatsApp (Facebook Corp) and by email. Two of the investigators then visited each class with a short Power Point (Microsoft corporation) presentation to brief the students. Two pictures, i.e. the Visual Analogue Scale (VAS) and that of the human neck region (with further sub-regions marked) were also displayed. After the presentation, the class representative shared the link, participant information sheet, and the figures with the entire batch using the WhatsApp group of their batch (which the students were already using for communication among themselves) and as e-mail attachments. The students were then asked to fill their responses in the next 15 minutes. Three reminder messages at the interval of three days were also sent by the class representatives to ensure maximum participation.
The data collected using Kobo Toolbox was exported as a Microsoft Excel sheet, which was then checked for missing responses and the same were excluded from or included in the analysis, depending on how much missing data were present. In case, for a single participant, significant missing data (>5%) was found in most of the variables, the participant was excluded from the analysis. Additionally, the date and time stamps from each response were deleted. This data was then exported into Statistical Package for the Social Sciences (SPSS) version 24 (IBM Corp, Armonk, NY, USA) for analysis. Proportions and means were calculated, along with 95% confidence interval (CI) and standard deviation (SD), respectively. Chi-square test was used to compare proportions among groups and to test associations. P value < 0·05 was taken as statistically significant. Univariable logistic regression analysis was conducted to understand the predictors of current neck pain, especially the socio-demographic, clinical, contextual, and gadget use-related factors among the participants. Multivariable logistic regression analysis was not performed since some of the variables had significant missing data.
Results
Of 492 students, 423 (86%) students responded to the questionnaire, out of which, 413 agreed to participate (97.6%). Another 82 responses out of 413 had a significant amount of missing data due to some software-related issues. Hence, the final number of participants who were included for analysis was 331.
The socio-demographic and the clinical characteristics of the participants have been described in Table 1. The majority of the participants were ≥20 years of age, males, had normal body mass index (BMI), did not currently use tobacco or alcohol, and were free from chronic diseases. The mean (SD) age of participants was 20.5 (1.7) years, the mean (SD) height was 168.1 (9.8) cm, the mean (SD) weight and mean (SD) BMI were 64.4 (13.2) kg and 22.7 (3.8) kg/m2. The most common chronic diseases prevalent among the participants were asthma, followed by hypertension, hypothyroidism, and hemophilia A.
Table 1.
Socio-demographic and clinical characteristics of the participants (n=331)
| Variable and category | Number (% in the parentheses) |
|---|---|
| Age (in years) | |
| <20 | 99 (29.9) |
| ≥20 | 232 (70.1) |
| Gender | |
| Male | 221 (66.8) |
| Female | 110 (33.2) |
| Academic year | |
| 1st | 64 (19.3) |
| 2nd | 70 (21.1) |
| 3rd | 69 (20.8) |
| 4th | 81 (24.5) |
| Internship | 47 (14.2) |
| BMI | |
| <18.5 | 41 (12.4) |
| 18.5-22.9 | 209 (63.2) |
| 23-24.9 | 62 (18.7) |
| >25 | 19 (5.7) |
| Current tobacco use | |
| Yes | 28 (8.5) |
| No | 303 (91.5) |
| Current alcohol use | |
| Yes | 54 (16.3) |
| No | 277 (83.1) |
| Chronic disease | |
| Present | 27 (8.2) |
| Absent | 304 (91.8) |
| Regular physical activity | |
| Yes | 155 (46.8) |
| No | 176 (54.2) |
Figure 1a shows the prevalence, patterns, and care seeking behavior of current neck pain among the participants. The majority of the participants, i.e. 58.3% suffered from neck pain within the last one year, with most of them (87.8%) experiencing the most recent episode within the last six weeks. Figure 1b shows the distribution of neck pain within various regions of the neck area. The mean (SD) score of VAS for pain among the participants was 7.7 (3.5) which amounts to moderate pain. Figure 2 describes the prevalence, patterns and related contextual factors of past neck pain among the participants.
Figure 1.
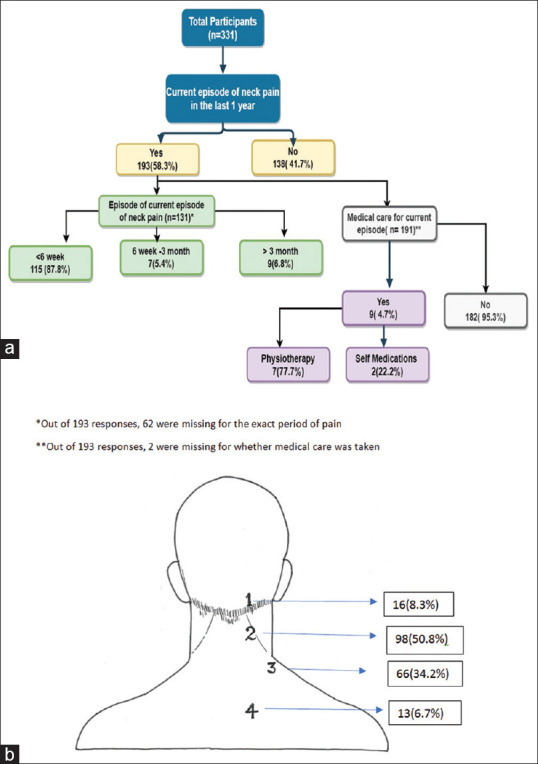
(a) Prevalence, patterns, and care-seeking behavior of current neck pain among the participants. (b) Distribution of current neck pain within various regions of the neck area (there were multiple responses were possible for this image question)
Figure 2.
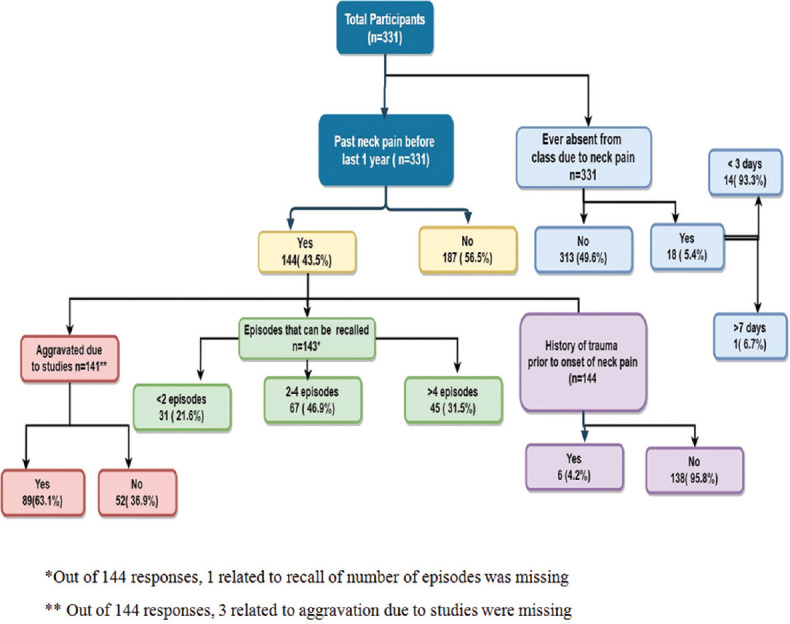
Prevalence, patterns, and related contextual factors of past neck pain among the participants
Table 2 describes the results of univariable logistic regression analysis to find out the demographic, clinical and contextual factors predicting the presence of current neck pain among the participants. Participants in both 3rd and 4th year had 2.9 times higher odds of current neck pain when compared to the 1st year students and this was statistically significant. Performing regular physical activity was found to be protective against neck pain (P = 0.037). Those who had a history of past pain had 13.7 higher odds of having current neck pain when compared with participants with no history of past neck pain (P< 0.001). Those with 2-4 hours of self-study had 2.1 times higher odds of having current neck pain (=0.005), while those with > 4 hours of self-study had 3.2 higher odds (P = 0.002) when compared with those with < 2 hours of self-study. Participants who self-reported aggravation of neck pain and attributed it to academic stress had 3.5 times higher odds of having current neck pain (P < 0.001) as compared to those who did not report aggravation of pain due to studies.
Table 2.
Results of univariable logistic regression analysis to find out the demographic, clinical and contextual factors predicting the presence of current neck pain among the participants. (n=331)
| Variable and category | Current neck pain present n (%) | Current neck pain absent n (%) | Total | Unadjusted Odd’s Ratio | 95% CI | p |
|---|---|---|---|---|---|---|
| Age (in years) | ||||||
| <20 | 53 (53.5) | 46 (46.5) | 99 | - | - | - |
| ≥20 | 140 (60.3) | 92 (39.7) | 232 | 1.3 | 0.8-2.1 | 0.251 |
| Gender | ||||||
| Male | 122 (55.2) | 99 (44.8) | 221 | 0.7 | 0.4-1.1 | 0.105 |
| Female | 71 (64.5) | 39 (35.5) | 110 | - | - | - |
| Academic year | ||||||
| 1st | 27 (42.2) | 37 (57.8) | 64 | - | - | - |
| 2nd | 38 (54.3) | 32 (45.7) | 70 | 1.6 | 0.8-3.2 | 0.163 |
| 3rd | 47 (68.1) | 22 (31.9) | 69 | 2.9 | 1.4-6.0 | 0.003# |
| 4th | 55 (67.9) | 26 (32.1) | 81 | 2.9 | 1.5-5.7 | 0.002# |
| Internship | 26 (55.3) | 21 (44.7) | 47 | 1.7 | 0.8-3.6 | 0.172 |
| BMI | ||||||
| <18.5 | 22 (53.7) | 19 (46.3) | 41 | - | - | - |
| 18.5-22.9 | 122 (58.4) | 87 (41.6) | 209 | 1.2 | 0.6-2.4 | 0.577 |
| 23-24.9 | 36 (58.1) | 26 (41.9) | 62 | 1.2 | 0.5-2.7 | 0.659 |
| >25 | 13 (68.4) | 6 (31.6) | 19 | 1.9 | 0.6-5.9 | 0.284 |
| Current tobacco use | ||||||
| Yes | 17 (60.7) | 11 (39.3) | 28 | 1.1 | 0.5-2.5 | 0.787 |
| No | 176 (58.1) | 127 (41.9) | 303 | - | - | - |
| Current alcohol use | ||||||
| Yes | 34 (63) | 20 (37) | 54 | 1.3 | 0.7-2.3 | 0.449 |
| No | 159 (57.4) | 118 (42.6) | 277 | - | - | - |
| Chronic disease | ||||||
| Present | 19 (70.4) | 8 (29.6) | 27 | 1.8 | 0.8-4.2 | 0.190 |
| Absent | 174 (57.2) | 130 (42.8) | 304 | - | - | - |
| Physical Activity | ||||||
| Yes | 81 (52.2) | 74 (47.7) | 155 | 0.6 | 0.4-0.9 | 0.036# |
| No | 112 (63.6) | 64 (36.4) | 176 | - | - | - |
| History of past pain | ||||||
| Yes | 127 (88.2) | 17 (11.8) | 144 | 13.7 | 7.6-24.7 | <0.001# |
| No | 66 (35.3) | 121 (64.7) | 187 | - | - | - |
| Episodes of pain* among those who had past pain | ||||||
| <2 | 26 (83.9) | 5 (16.1) | 31 | - | - | - |
| 2-4 | 60 (89.5) | 7 (10.4) | 67 | 1.7 | 0.5-5.7 | 0.428 |
| >4 | 41 (91.9) | 4 (8.8) | 45 | 2.0 | 0.5-8.0 | 0.343 |
| Self-study hours** | ||||||
| <2 | 81 (49.4) | 83 (50.6) | 164 | - | - | - |
| 2-4 | 74 (66.7) | 37 (33.3) | 111 | 2.1 | 1.2-3.4 | 0.005# |
| >4 | 37 (75.5) | 12 (24.5) | 49 | 3.2 | 1.5-6.5 | 0.002# |
| Place of self-study | ||||||
| Library | 147 (59.8) | 99 (40.2) | 79 | - | - | - |
| Hostel | 41 (51.9) | 38 (48.1) | 246 | 0.7 | 0.5-1.2 | 0.219 |
| Others | 5 (83.3) | 1 (16.7) | 6 | .3.4 | 0.4-29.3 | 0.274 |
| Preferred posture of self study | ||||||
| Table and chair | 95 (57.2) | 71 (42.8) | 166 | - | - | - |
| On bed/floor in sitting position | 54 (54.5) | 45 (45.5) | 99 | 0.9 | 0.5-1.5 | 0.670 |
| On bed/floor with a table to support books | 14 (63.6) | 8 (36.4) | 22 | 1.3 | 0.5-3.4 | 0.568 |
| On bed lying prone | 25 (67.6) | 12 (32.4) | 37 | 1.6 | 0.7-3.3 | 0.250 |
| Others | 5 (71.4) | 2 (28.6) | 7 | 1.9 | 0.4-9.9 | 0.463 |
| Pain aggravated due to studies | ||||||
| Yes | 115 (75.2) | 38 (24.8) | 153 | 3.5 | 2.1-5.5 | <0.001# |
| No | 76 (46.9) | 86 (53.1) | 162 | - | - | - |
*Out of 144 who had past pain, one response had missing data, hence n=143 here. ** Out of 331, seven responses had missing data, hence n=324 here. $ Most commonplace of self-studying place being home. # Statistically significant (P<0.05)
Table 3 describes the results of univariable logistic regression analysis to find out factors related to patterns of gadget use predicting the presence of current neck pain among the participants. Self-perceived aggravation of pain due to laptop and smart phone use were found to have 3.7 times (P < 0.001) and 3.4 times (P < 0.001) higher odds of contributing to the current episode of neck pain as compared to those who did not report aggravation of pain. Those who had previous neck pain even before joining the undergraduate medical course were found to have 5.7 times higher odds of having current neck pain than those who did not have any neck pain before joining the course (P < 0.001).
Table 3.
Results of univariable logistic regression analysis to find out factors related to patterns of gadget use predicting the presence of current neck pain among the participants (n=331)
| Variable and category | Current neck pain present n (%) | Current neck pain absent n (%) | Total | Unadjusted Odd’s Ratio | 95% CI | p |
|---|---|---|---|---|---|---|
| Watch television | ||||||
| Yes | 20 (45.5) | 24 (54.5) | 44 | 0.6 | 0.3-1.0 | 0.066 |
| No | 173 (60.3) | 114 (39.7) | 287 | - | - | - |
| Laptop use | ||||||
| Yes | 118 (61.8) | 73 (38.2) | 191 | 1.4 | 0.9-2.2 | 0.135 |
| No | 75 (53.6) | 65 (46.4) | 140 | - | - | - |
| Hours of laptop use 1* | ||||||
| <1 hr | 71 (67.6) | 34 (32.4) | 105 | - | - | - |
| 1-3 hrs | 31 (56.4) | 24 (43.6) | 55 | 1.6 | 0.3-1.2 | 0.161 |
| >3 hrs | 15 (55.6) | 12 (44.4) | 27 | 1.0 | 0.4-2.6 | 0.952 |
| Purpose of laptop use1# | ||||||
| Leisure | 82 (59.9) | 55 (40.1) | 137 | - | - | - |
| Studies | 35 (68.6) | 16 (31.4) | 51 | 1.5 | 0.7-2.9 | 0.271 |
| Preferred posture of laptop use1# | ||||||
| As a desktop on a table | 50 (64.1) | 28 (35.9) | 78 | - | - | - |
| On the lap | 15 (75) | 5 (25) | 20 | 1.7 | 0.6-5.2 | 0.361 |
| On the bed while lying prone | 27 (58.7) | 19 (41.3) | 46 | 0.8 | 0.4-1.7 | 0.549 |
| On the bed while sitting | 25 (56.8) | 19 (43.2) | 44 | 0.7 | 0.4-1.6 | 0.428 |
| Position of eyes with respect to computer screen1@ | ||||||
| Approximately at midpoint of screen | 35 (53) | 31 (47) | 66 | - | - | - |
| Above the top of screen | 64 (68.1) | 30 (31.9) | 94 | 1. | 1.0-3.6 | 0.055 |
| Below the bottom of screen | 11 (68.7) | 5 (31.3) | 16 | 1.95 | 0.6-6.2 | 0.261 |
| Pain aggravated by laptop use1^ (self-perceived) | ||||||
| Yes | 48 (81.4) | 11 (18.6) | 59 | 3.7 | 1.8-7.7 | <0.001# |
| No | 69 (54.3) | 58 (45.7) | 127 | - | - | - |
| Smart phone use | ||||||
| Yes | 193 (58.3%) | 138 (41.7%) | 331 | - | - | - |
| No | Nil | Nil | Nil | - | - | - |
| Hours of smart phone use2# | ||||||
| <2 | 33 (60) | 22 (40) | 55 | - | - | - |
| 2-4 | 72 (53.7) | 62 (46.3) | 134 | 0.8 | 0.4-1.5 | 0.431 |
| >4 | 87 (62.6) | 52 (37.4) | 139 | 1.2 | 0.6-2.1 | 0.738 |
| Purpose of smart phone use 2* | ||||||
| Communication | 34 (64.2) | 19 (35.8) | 53 | 1.2 | 0.5-3.2 | 0.669 |
| Social Media | 113 (56.8) | 86 (43.2) | 199 | 0.9 | 0.4-2.1 | 0.807 |
| Games | 29 (60.4) | 19 (39.6) | 48 | 1.1 | 0.4-2.7 | 0.922 |
| Studies | 16 (59.3) | 11 (40.7) | 27 | - | - | - |
| Preferred posture of phone use2^ | ||||||
| Lying down | 69 (57) | 52 (43) | 121 | 1.3 | 0.3-6.8 | 0.735 |
| Sitting | 80 (56.7) | 61 (43.3) | 141 | 1.3 | 0.3-6.7 | 0.745 |
| Semi reclining | 40 (69) | 18 (31) | 58 | 2.2 | 0.4-12.1 | 0.451 |
| Standing | 3 (50) | 3 (50) | 6 | - | - | - |
| Pain aggravated by previous smart phone use2@ | ||||||
| Yes | 100 (76.3) | 31 (23.7) | 131 | 3.4 | 2.1-5.6 | <0.001# |
| No | 90 (48.6) | 95 (51.4) | 185 | - | - | - |
| History of previous neck pain before joining MBBS course 2* | ||||||
| Yes | 108 (81.2) | 25 (18.8) | 133 | 5.7 | 3.4-9.6 | <0.001# |
| No | 84 (43.3) | 110 (56.7) | 194 | - | - | - |
| Timing of first episode of previous neck pain before joining MBBS course 3* | ||||||
| While still in school | 91 (82.7) | 19 (17.3) | 110 | - | - | - |
| After leaving school | 17 (73.9) | 6 (26.1) | 23 | 0.6 | 0.2-1.7 | 0.329 |
| Time spent in studies while preparing for MBBS Entrance examination3# (in hours) | ||||||
| <4 | 4 (66.7) | 2 (33.3) | 6 | - | - | - |
| 4-8 | 33 (82.5) | 7 (17.5) | 40 | 2.4 | 0.4-15.5 | 0.372 |
| 8-12 | 42 (80.8) | 10 (19.2) | 52 | 2.1 | 0.3-13.1 | 0.427 |
| >12 | 30 (83.3) | 6 (16.7) | 36 | 2.5 | 0.3-16.9 | 0.347 |
| Perception whether previous pain aggravated due to studies3^ | ||||||
| Yes | 82 (80.4) | 20 (19.6) | 102 | 0.8 | 0.3-2.4 | 0.718 |
| No | 25 (83.3) | 5 (16.7) | 30 | - | - | - |
| Perception whether previous neck pain was affected by pressure of selection/ success3# | ||||||
| Yes | 37 (77.1) | 11 (22.9) | 48 | 0.7 | 0.3-1.6 | 0.346 |
| No | 72 (83.7) | 14 (16.3) | 86 | - | - | - |
1*, 2*, 3* - 4 responses were missing in each; hence the denominator is n=187, 327, and 133, respectively. 1#, 2#, 3# - 3 responses were missing in each; hence the denominator is 188, 328, and 134, respectively. 1@, 2@ - 15 responses were missing in each; hence the denominator is 176 and 316 respectively. 1^, 2^, 3^- 5 responses were missing in each, hence the denominator is 186, 326, and 132, respectively. # statistically significant (P < 0.05)
Discussion
Inadequate focus on posture, devotion of too little time for physical activity, and mental stress have been reported to be contributing to MSP in students of coaching classes in India.[1] Additionally, smartphone and computer use has been postulated to be contributing to poor posture and are believed to be influencing MSP.[5,7,11,12] Medical students in India are additionally burdened with the pressure of preparing for a very competitive entrance exam for getting into a post-graduate program. They are thus prone to develop MSP.
There are limited reported studies on MSP in undergraduate medical students. Studies have reported the prevalence of MSP in undergraduate medical students of Malaysia, China, Australia, Saudi Arabia, and Ethiopia.[8,10,13,14,15] While neck pain was the most common MSP in Australian[14] medical students, it was the second most common in Chinese,[15] Saudi Arabian,[8] and Malaysian[13] students. From an Indian context, there is no reported study examining the prevalence of neck pain.
In this study, the focus was specifically on neck pain. The reported prevalence of neck pain during the past one year was 58.3%, with 87.8% of participants experiencing neck pain within the past six weeks. This prevalence is much higher than that reported in Australian, Arabian, Chinese, Malaysian, and Ethiopian medical students.[8,10,13,14,15] When considered with the fact that students in our study who had neck pain even before joining the undergraduate medical course had 5.7 times higher odds of having current neck pain than those who did not have any neck pain before joining the course, we believe that Indian students are more prone to develop neck pain, probably due to the stresses they face even before joining the medical course.
We found no influence of factors like gender, age, BMI, tobacco use, and alcohol consumption on the presence of current neck pain. This is similar to the findings reported by Algarni et al.[8] and Haroon et al.[10] In contrast, Smith et al.[14] reported a higher rate of neck pain among female students and that alcohol consumption increased the chances of low back pain with no comment on neck pain. Alshagga et al.[13] reported no difference in MSPs in terms of gender and age but added that BMI was higher among students who had MSP compared to those with no MSP. Smith et al.[15] reported that female medical students had a higher prevalence of MSP than their male counterparts. Dighriri et al.[16] reported no gender related differences in their study of Saudi Arabian medical students.
In our study, the prevalence of neck pain was least in the 1st year; which is the pre-clinical year of the medical curriculum. Prevalence increased in the 2nd, 3rd, and 4th years (clinical years) and then declined during the internship. While the exact cause for such a trend is difficult to be identified, we believe that the already increasing curriculum pressure, along with the addition of clinical classes and coaching classes for postgraduate entrance preparation might be responsible. The decrease in prevalence during the internship can be attributed to the fact that interns have already passed their undergraduate exam and thus are probably less burdened psychologically. Other studies too concur that MSP is higher among students of clinical years than those in pre-clinical years.[8,13,14]
In this study, the odds of having neck pain increased with the number of self-study hours put in by the students. The place and posture of self-study had no relation to neck pain. However, a history of neck pain in the past increased the odds of having current neck pain. Also, a significant number of respondents who had neck pain reported that pressure due to academics aggravated their pain. While we found that regular exercise has some protective role in neck pain, Smith et al.[14] reported that students performing regular exercise were more likely to report pain in the upper back region. There was no specific mention of the impact of exercise on neck pain. Differences in the type of exercises performed and the exact site of pain might account for this contradictory observation.
All the participants of this study routinely used smartphones. The number of computer users was less though. While 134 students were using their smartphones for 2-4 hours per day and 139 students were using it for more than 4 hours per day, there was no significant influence of duration of smartphone use on the prevalence of neck pain. The position in which the smartphone was used or the purpose of its usage did not influence neck pain. None of the previous studies conducted on medical students had analyzed the effect of smartphone use. Yang et al.[7] in their study on junior college students found that MSP was associated with the duration and purpose of smartphone use. In this study though, the duration, position, and purpose of computer use did not influence the neck pain prevalence. This is in contradiction to the reports of Alshagga et al.[13] and Smith et al.[15], which showed that prolonged computer use was associated with MSPs. The participants in this study, who had neck pain, reported that the use of smartphones and computers had a tendency of aggravating the existing neck pain.
A significant number of participants reported that they had experienced one or more episodes of neck pain even before joining the undergraduate medical course. Interestingly, majority had neck pain right from the time they were in schools. One study from South India reported that 86% of 7th and 8th grade students had experienced MSP in the preceding 2 weeks, out of which the second most common region of pain was the neck (39%).[17] The duration of study and pressure of selection in the entrance exam did not lead to any aggravation of pain.
When we look at the strengths of the study, then the response rate of 96% to our web-based questionnaire study was much higher than the 19.9% reported by Algarni et al.[8] and 36.1% reported by Alshagga et al.[13] The higher response rate was probably due to the use of WhatsApp as well as e-mail for the circulation of the questionnaire and filling up responses in the classroom itself. Two studies used e-mail as the only method of circulation of their questionnaire. Other reported studies[3,9,10,11,14,15,16] had used the conventional paper-based data collection method. Maintaining anonymity also helped in getting unbiased responses. Additionally, we have analyzed the influence of smartphone use on neck pain, which was not done in previous investigations.
This study has few lacunae too. A relatively high number of responses were not received by the investigators and were found missing even though the participants had duly responded. This probably resulted from software glitches and prevented us from including a valuable amount of data which would have probably made the findings and as a corollary the conclusions more robust. This study was conducted in a centrally funded institute in a reasonably large city having coaching facilities. Inclusion of data from other medical colleges in different environments such as the state government and private colleges would have increased the generalizability of the study. The questionnaire lacked questions for assessing the mental and emotional states of students. These could have helped in getting an insight into the psychological factors associated with neck pain. Last but not the least, our study had a fair risk of having response bias and recall bias as the questionnaire was exhaustive and as many questions were about events in past. Also, one may argue that having a control group was desirable. However, being a questionnaire-based survey, this was not feasible.
As MSP conditions can become chronic and can lead to impairment in a person's profession, we believe that corrective and remedial steps addressing the current educational system are a must. Timely screening of neck pain in school students should be conducted by involving primary care physicians before referral to specialists. Primary care physicians should encourage health promoting behaviors like increased physical activity among students during their routine care. They should also educate the adolescents having neck pain who have approached them for care, along with their parents to cut down on the use of electronic gadgets. The curriculum for teaching and the emphasis on stress management to handle increased academic pressure and competitive exams should be appropriately addressed, starting in schools itself. Additionally, ergonomic ways of handling gadgets must be taught from elementary school level itself and this should be reinforced periodically.
The key messages from the current study are a) even though most cases go unreported, more than 50% of students reported neck pain in the last one year b) 3rd and 4th year students had a higher odds of current pain when compared to 1st year students c) students with past history of neck pain had higher odds of having current pain d) those who had neck pain before joining undergraduate medical course were predisposed to having current neck pain e) it cannot be concluded that modern gadgets influenced the onset of neck pain even though they can aggravate it and e) physical activity had protective role on neck pain. Primary care physicians and educational institutes can play a key role in health promotion and education, bringing ergonomic changes, screening, and initial management before referral to specialists in case the need arises.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Santoshi JA, Jain S, Popalwar HJ, Pakhare AP. Musculoskeletal disorders and associated risk factors in coaching students: A cross-sectional study. J Family Med Prim Care. 2019;8:929–33. doi: 10.4103/jfmpc.jfmpc_54_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional and national incidence, prevalence and years lived with disability for 354 diseases and injuries for 195 countries, and territories, 1990-2017: A systematic analysis for the global burden of disease study. Lancet. 2018;392:1789–858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanchanomai S, Janwantanakul P, Pensri P, Jiamjarasrangsi W. Risk factors for the onset and persistence of neck pain in undergraduate students: 1-year prospective cohort study. BMC Public Health. 2011;11:566. doi: 10.1186/1471-2458-11-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanvold TN, Wærsted M, Mengshoel AM, Bjertness E, Twisk J, Veiersted KB. A longitudinal study on risk factors for neck and shoulder pain among young adults in the transition from technical school to working life. Scand J Work Environ Health. 2014;40:597–609. doi: 10.5271/sjweh.3437. [DOI] [PubMed] [Google Scholar]
- 5.Woo EHC, White P, Lai CWK. Musculoskeletal impact of the use of various types of electronic devices on university students in Hong Kong: An evaluation by means of self-reported questionnaire. Man Ther. 2016;26:47–53. doi: 10.1016/j.math.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Shan Z, Deng G, Li J, Li Y, Zhang Y, Zhao Q. Correlational analysis of neck/shoulder pain and low back pain with the use of digital products, physical activity and psychological status among adolescents in Shanghai. PLoS One. 2013;8:1–9. doi: 10.1371/journal.pone.0078109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang SY, Chen MD, Huang YC, Lin CY, Chang JH. Association between smartphone use and musculoskeletal discomfort in adolescent students. J Community Health. 2017;42:423–30. doi: 10.1007/s10900-016-0271-x. [DOI] [PubMed] [Google Scholar]
- 8.Algarni AD, Al-Saran Y, Al-Moawi A, Bin Dous A, Al-Ahaideb A, Kachanathu SJ. The prevalence of and factors associated with neck, shoulder, and low-back pains among medical students at university hospitals in Central Saudi Arabia. Pain Res Treat. 2017;2017:1235706. doi: 10.1155/2017/1235706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benlidayi IC, Al-bayati Z, Guzel R, Sarpel T. Neither got a good bill of musculoskeletal health : A comparative study among medical and dental students. Acta Clin Belg. 2018;3286:1–4. doi: 10.1080/17843286.2018.1483564. [DOI] [PubMed] [Google Scholar]
- 10.Weleslassie GG, Meles HG, Haile TG, Hagos GK. Burden of neck pain among medical students in Ethiopia. BMC Musculoskeletal Disorders. 2020;21:14. doi: 10.1186/s12891-019-3018-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aggarwal N, Anand T, Kishore J, Ingle GK. Low back pain and associated risk factors among undergraduate students of a medical college in Delhi. Educ Heal Chang Learn Pract. 2013;26:103–8. doi: 10.4103/1357-6283.120702. [DOI] [PubMed] [Google Scholar]
- 12.Gupta N, Krishnamurthy V, Majhi J, Gupta S. Gadget dependency among medical college students in Delhi article cycle citation. Ind J Comm Health. 2013;25:362–6. [Google Scholar]
- 13.Alshagga MA, Nimer AR, Yan LP, Ibrahim IAA, Al-Ghamdi SS, Radman Al-Dubai SA. Prevalence and factors associated with neck, shoulder and low back pains among medical students in a Malaysian medical college. BMC Res Notes. 2013;6:244. doi: 10.1186/1756-0500-6-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith DR, Leggat PA. Prevalence and distribution of musculoskeletal pain among Australian medical students. J Musculoskelet Pain. 2007;15:39–46. [Google Scholar]
- 15.Smith DR, Wei N, Ishitake T, Wang RS. Musculoskeletal disorders among Chinese medical students. Kurume Med J. 2005;52:139–46. doi: 10.2739/kurumemedj.52.139. [DOI] [PubMed] [Google Scholar]
- 16.Dighriri YH, Akkur MA, Alharbi SA, Madkhali NA, Matabi KI, Mahfouz MS. Prevalence and associated factors of neck, shoulder, and low-back pains among medical students at Jazan University, Saudi Arabia: A cross-sectional study. J Family Med Prim Care. 2019;8:3826–31. doi: 10.4103/jfmpc.jfmpc_721_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parthibane S, Majumdar A, Kalidoss V, Roy G. Prevalence and patterns of musculoskeletal pain among school students in Puducherry and its association with sociodemographic and contextual factors. Indian J Pain. 2017;31:119–26. [Google Scholar]


