Abstract
About 30% of all newly diagnosed renal cell carcinoma (RCC) patients present with synchronous metastatic disease. Usual organs of involvement are lung (75%), soft tissues (36%), bone (20%), liver (18%), cutaneous sites (8%), and central nervous system (8%). Metastases to the paranasal sinuses (PNS) are relatively common and may be a part of synchronous multiorgan involvement or present in follow-up after radical nephrectomy (metachronous); but primary presentation as isolated paranasal mass before the diagnosis of RCC is extremely rare. Here, we report a case of 74-year-old female presented with epistaxis and nasal obstruction. On evaluation by magnetic resonance imaging (MRI), a heterogeneously enhancing mass was found involving left PNS. Biopsy from mass revealed clear cell RCC. Later on, contrast-enhanced computed tomography (CECT) of chest, abdomen, and pelvis showed enhancing mass from the upper pole of the left kidney with no evidence of metastasis elsewhere. The patient was started on pazopanib 800 mg once a day. At 6 months follow-up scan, there was a partial response at both primary as well as metastatic site.
Keywords: Epistaxis, metastatic renal cell carcinoma, paranasal sinus, tyrosine kinase inhibitor
Introduction
Metastatic renal cell carcinoma (RCC) is almost always fatal and survival at 1 year, 5 years, and 10 years are approximately <50%, 5–30%, and 0–5%, respectively.[1,2] Prognosis of RCC depends on multiple variables comprising clinical, anatomical, biochemical, and pathological factors. Symptomatic metastasis, metastatic burden, and site of metastasis have its own prognostic significance. Although metastasis of RCC to paranasal sinuses (PNS) are rare; it is one of the common malignant tumors to metastasize to PNS and is often reported years after radical or partial nephrectomy.[3] Unusual metastatic symptoms and the site of metastasis of RCC prompted us to report this case and to do a literature review. A primary care physician must be aware that epistaxis may be the first presentation of metastatic RCC.
Case Details
A 74-year-old diabetic and hypertensive female presented to the otorhinolaryngology department with bleeding from the nose and left side nasal obstruction. Magnetic resonance imaging (MRI) head and neck showed T2 hyperintense soft tissue mass lesion of size 5.9 × 4.5 × 2.2 cm3 occupying frontal and ethmoidal sinuses on the left side with anterior cranial fossa extension without obvious brain involvement [Figure 1]. Rhinoscopy showed proliferative mass occupying left nasal fossa [Figure 2]. Histopathological report after punch biopsy showed tumoral tissue composed of diffuse sheets, glands, and trabeculae of clear cells having vacuolated clear cytoplasm, rounded nuclei, and prominent nucleoli with infiltration of tumor cells into the surrounding fibromuscular tissue [Figure 3]. Tumor cells were positive for RCCAg [Figure 4] and vimentin. The features were consistent with metastatic clear cell RCC. Subsequently, contrast-enhanced computed tomography (CECT) of abdomen and pelvis showed heterogeneously enhancing mass lesion of size 3.9 × 6.2 × 6.3 cm3 arising from upper and mid pole of left kidney with tumor thrombus limited to the renal vein [Figure 5]. In view of poor performance status and comorbidities; the patient was started on tyrosine kinase inhibitor (TKI), pazopanib 800 mg once a day, considering shared decision with the patient. Follow-up imaging at 6 months showed partial response according to RECIST 1.1 criteria.
Figure 1.
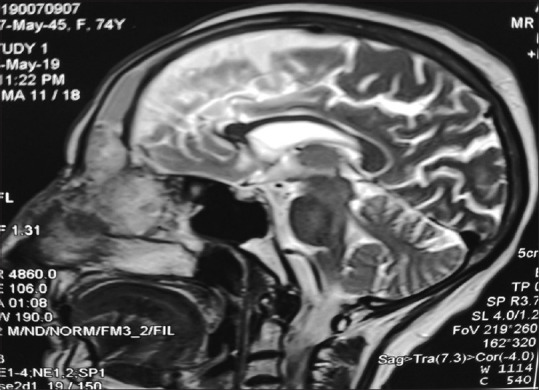
MRI head and neck showing T2 hyperintense lesion involving left frontal and ethmoid sinus with anterior cranial fossa extension
Figure 2.

Rinoscopy showing proliferative mass
Figure 3.

Diffuse spread of tumor cells in sheets, glands, and trabeculae having vacuolated clear cytoplasm and rounded nuclei and prominent nucleoli consistent with clear cell RCC (H & E ×40)
Figure 4.

Tumor cells positive of RCCag (×40)
Figure 5.

Coronal section CECT of the abdomen and pelvis showing heterogeneous enhancing mass at the mid and lower pole of the left kidney
Discussion
RCC is the most common infraclavicular tumor to metastasize to the PNS and accounts for about 49% of cases.[4] Approximately, 110 cases of RCC metastasizing to PNS have been reported in the literature and most of the reported cases were 2–10 years after nephrectomy.[5] Out of them, in only 20 cases, metastasis to the PNS was the first presentation of the disease (without a diagnosis of RCC). The survival of these patients ranged from 3 months to 3 years.[5] The most common presentation of metastasis to PNS was epistaxis (55%, 11/20) followed by nasal obstruction, headache, and diplopia [Table 1]. Our index case had a similar presentation. These symptoms and radiological features of hypervascular mass in PNS raised suspicion of a primary sinonasal tumor such as angiofibroma, hemangiopericytoma, hemangioma, or sinonasal glomus tumors.[6] There are no specific radiological findings to differentiate the primary hypervascular lesion of PNS from RCC metastasizing to PNS. The only way to confirm the diagnosis is by biopsy and immunohistochemistry.[9,10,11] The multimodality approach of treatment like surgery of primary and secondary with and without radiotherapy has been described in the literature with variable prognosis. Treatment with tyrosine kinase inhibitors and checkmate inhibitors is showing a promising result. Cytoreductive nephrectomy can be considered in good and intermediate-risk patients but the CARMENA trial showed that sunitinib only is not inferior to sunitinib and nephrectomy in the management of these patients.[24] Our patient opted for targeted molecular therapy over surgery and showed a partial response at 6 months and she is under regular follow-up.
Table 1.
Summary of literature review of metastasis from RCC to PNS as the first presentation
| Authors | Age/sex | Presenting symptoms | Metastatic site (PNS) | Treatment | Survival after diagnosis |
|---|---|---|---|---|---|
| Index case | 74/M | Epistaxis and Nasal obstruction | Frontal and Ethmoid | TKI | No recurrent episode up to 6 months |
| Lee et al., 2016[7] | 62/M | Epistaxis and anemia | Ethmoid | Endoscopic excision of metastasis and nephrectomy | Disease-free at 5 months |
| Berkiten et al., 2016[8] | 61/M | NA | Ethmoid | Radiotherapy to metastasis and nephrectomy | Disease-free at 1 year |
| Sountoulides et al., 2011[3] | 73/M | Epistaxis | Ethmoid | NA | NA |
| Hainăroşie R et al., 2017[9] | 60/m | Epistaxis and Frontal swelling | Ethmoid and maxillary | Excision of metastasis and nephrectomy | No recurrence at 3 months |
| Ralli M et al., 2017[10] | 72/M | Epistaxis | Ethmoid | Excision of metastasis only | Death after 4 months |
| Ikeuchi T et al., 1998[11] | 58/M | Frontal swelling | Frontal | Surgical extirpation and nephrectomy | NA |
| Maheshwari G et al., 2003[12] | 57/M | Headache and epistaxis | Ethmoid | Near-total excision of metastasis | No recurrence at 30 months |
| Fyrmpas G et al., 2011[13] | 79/F | Epistaxis | Ethmoid and Frontal sinus | TKI | No recurrence at 9 months |
| Morvan JB et al., 2011[14] | 53/M | Rhinorrhea | Sphenoid | Sphenoidectomy | NA |
| Bechara GR et al., 2012[15] | 65/M | Epistaxis and sinusitis | Maxillary | Nephrectomy followed by TKI and local radiotherapy | NA |
| Nayak DR et al., 2006[16] | 70/M | Diplopia | Sphenoid | Radiotherapy | Lost to follow-up |
| Kokenek-Unal TD et al., 2016[17] | 50/M | Nasal obstruction and snoring | Maxillary | NA | Recurrence at 1 year |
| Sgouras N et al., 1995[18] | 85/M | Epistaxis | Frontal and ethmoidal sinus | NA | NA |
| Homer JJ et al., 1995[19] | 59/M | Diplopia | Ethmoid | NA | No recurrence at 2 yrs |
| Matsumoto Y et al., 1982[20] | 73/M | Epistaxis | Maxillary and Ethmoid | NA | Death at 1 year because of generalized metastasis |
| Matsumoto Y et al., 1982[20] | 73/M | Epistaxis | Ethmoid | NA | No recurrence at 3 years |
| Gottlieb MD et al., 1998[21] | 58/M | Headache and proptosis | Ethmoid and maxillary | Local excision of the mass | No recurrence at 62 months |
| He YF et al., 2014[22] | 35/M | Mass in maxillary | maxillary | Excision and nephrectomy | Death after 2 years |
| Singh I et al., 2004[23] | 70/M | Diplopia | sphenoid | NA | Lost to follow-up after 3 months |
NA:Not available, TKI:Tyrosine kinase inhibitor, RN:Radical nephrectomy
Conclusions
Isolated metastasis of RCC to PNS is quite unusual and should be considered during the evaluation of sinonasal lesion. The multidisciplinary approach of treatment can considerably improve the quality of life and survival in selected patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
Ashwini Kumar Singh Kandari.
References
- 1.Heng DY, Xie W, Regan MM, Harshman LC, Bjarnason GA, Vaishampayan UN, et al. External validation and comparison with other models of the international metastatic renal-cell carcinoma database consortium prognostic model: A population-based study. Lancet Oncol. 2013;14:141–8. doi: 10.1016/S1470-2045(12)70559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haddad H, Rini BI. Current treatment considerations in metastatic renal cell carcinoma. Curr Treat Options Oncol. 2012;13:212–29. doi: 10.1007/s11864-012-0182-8. [DOI] [PubMed] [Google Scholar]
- 3.Sountoulides P, Metaxa L, Cindolo L. Atypical presentations and rare metastatic sites of renal cell carcinoma: A review of case reports. J Med Case Rep. 2011;5:429. doi: 10.1186/1752-1947-5-429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evgeniou E, Menon KR, Jones GL, Whittet H, Williams W. Renal cell carcinoma metastasis to the paranasal sinuses and orbit. BMJ Case Rep. 2012;2012:2–5. doi: 10.1136/bcr.01.2012.5492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petruzzelli GJ, Shook T, Campbell WJ, Gupta S. Paranasal sinus metastases of renal cell carcinoma: A case report and comprehensive literature review. Ann Clin Case Rep. 2019;4:1642. [Google Scholar]
- 6.Razek AA, Huang BY. Soft tissue tumors of the head and neck: Imaging based review of the WHO classification. Radiographics. 2011;31:192354. doi: 10.1148/rg.317115095. [DOI] [PubMed] [Google Scholar]
- 7.Lee SM, Kim YM, Kim BM. Epistaxis as the first manifestation of silent renal cell carcinoma: A case report with relevant literature review. Iran J Radiol. 2016;13:e31208. doi: 10.5812/iranjradiol.31208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berkiten G, Kumral T, Yildirim G, Atar Y, Salturk Z, Dogan M, et al. Metastasis of renal cell carcinoma to head and neck region. Otolaryngol Online J. 2016;6:133. [Google Scholar]
- 9.Hainăroşie R, Anghelina F, Ioniţă IG, Zoican OI, Pietroşanu C, Piţuru SM, et al. Rare metastasis of renal carcinoma in the frontoethmoid-orbital region – case report and review of the literature. Rom J Morphol Embryol. 2017;58:1497–504. [PubMed] [Google Scholar]
- 10.Ralli M, Altissimi G, Turchetta R, Rigante M. Metastatic renal cell carcinoma presenting as a paranasal sinus mass: The importance of differential diagnosis. Case Rep Otolaryngol. 2017;2017:9242374. doi: 10.1155/2017/9242374. doi: 10.1155/2017/9242374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ikeuchi T, Hori T, Hirao N, Tozawa K, Yamada Y, Kori K. Renal cell carcinoma detected by metastasis to the frontal sinus: A case report. Hinyokika Kiyo. 1998;44:89–92. [PubMed] [Google Scholar]
- 12.Maheshwari G, Baboo H, Patel M, Usha G. Metastatic renal cell carcinoma involving ethmoid sinus at presentation. J Postgraduate Med. 2003;49:96–7. doi: 10.4103/0022-3859.915. [DOI] [PubMed] [Google Scholar]
- 13.Fyrmpas G, Adeniyi A, Baer S. Occult renal cell carcinoma manifesting with epistaxis in a woman: A case report. J Med Case Rep. 2011;5:79. doi: 10.1186/1752-1947-5-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morvan JB, Veyrires JB, Mimouni O, Cathelinaud O, Allali L, Verdalle P. Clear-cell renal carcinoma metastasis to the base of the tongue and sphenoid sinus: Two very rare atypical ENT locations. European Ann Otorhinolaryngol Head Neck Dis. 2011;128:91–4. doi: 10.1016/j.anorl.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Bechara GR, Anacleto J, Resende D, Gouveia HA. Metastasis to paranasal sinuses as the first presenting sign of renal cell carcinoma. Open J Eurol. 2012;2:28–31. [Google Scholar]
- 16.Nayak DR, Pujary K, Ramnani S, Shetty C, Parul P. Metastatic renal cell carcinoma presenting with epistaxis. Indian J Otolaryngol Head Neck Surg. 2006;58:406–8. doi: 10.1007/BF03049615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kokenek-Unal TD, Gumuskaya B, Ocal B, Alper M. A rare cause of nasal obstruction: Metastatic renal cell carcinoma. Case Rep Pathol. 2016;2016:3. doi: 10.1155/2016/2560749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sgouras N, Gamatsi I, Porfyris E, Lekka J, Harkiolakis G, Nikolopoulou SM, et al. An unusual presentation of a metastatic hypernephroma to the frontonasal region. Ann Plast Surg. 1995;34:653–6. doi: 10.1097/00000637-199506000-00016. [DOI] [PubMed] [Google Scholar]
- 19.Homer JJ, Jones NS. Renal cell carcinoma presenting as a solitary paranasal sinus metastasis. J Laryngol Otol. 1995;109:968–9. doi: 10.1017/s0022215100131822. [DOI] [PubMed] [Google Scholar]
- 20.Matsumoto Y, Yanagihara N. Renal clear cell carcinoma metastatic to the nose and paranasal sinuses. Laryngoscope. 1982;92:1190–3. [PubMed] [Google Scholar]
- 21.Gottlieb MD, Roland JT., Jr Paradoxical spread of renal cell carcinoma to the head and neck. Laryngoscope. 1998;108:1301–5. doi: 10.1097/00005537-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 22.He YF, Chen J, Xu WQ, Ji CS, Du JP, Luo HQ, et al. Case report metastatic renal cell carcinoma to the left maxillary sinus. Genet Mol Res. 2014;13:7465–9. doi: 10.4238/2014.September.12.12. [DOI] [PubMed] [Google Scholar]
- 23.Singh I, Khaitan A. Diplopia an unusual primary manifestation of metastatic renal cell carcinoma. Urol Int. 2004;73:285–6. doi: 10.1159/000080845. [DOI] [PubMed] [Google Scholar]
- 24.Méjean A, Ravaud A, Thezenas S, Colas S, Beauval JB, Bensalah K, et al. Sunitinib alone or after nephrectomy in metastatic renal-cell carcinoma. N Engl J Med. 2018;379:417–27. doi: 10.1056/NEJMoa1803675. [DOI] [PubMed] [Google Scholar]


