Abstract
Objective
In vivo functional changes in white matter during the progression of Alzheimer’s disease (AD) have not been previously reported. Our objectives are to measure changes in white matter functional connectivity (FC) in an elderly population undergoing cognitive decline as AD develops, to establish their relationship to neuropsychological scores of cognitive abilities, and to assess the performance in prediction of AD using white matter FC measures as features.
Methods
Analyses were conducted using resting state functional MRI and neuropsychological data from 383 ADNI participants, including 136 cognitive normal (CN) controls, 46 with significant memory concern, 83 with early mild cognitive impairment (MCI), 37 with MCI, 46 with late MCI, and 35 with AD dementia. FC metrics between segregated white matter tracts and discrete gray matter volumes or between white matter tracts were quantitatively analyzed and characterized, along with their relationships to 6 cognitive measures. Finally, supervised machine learning was implemented on white matter FCs to classify the participants and performance of the classification was evaluated.
Results
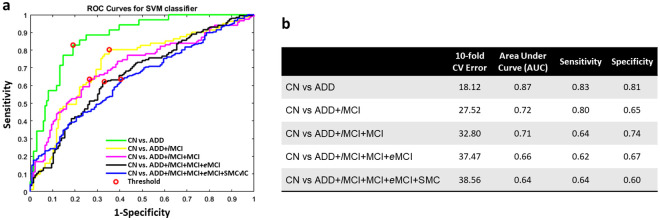
Significant decreases in FC measures were found in white matter with prominent, specific, regional deficits appearing in late MCI and AD dementia patients from CN. These changes significantly correlated with neuropsychological measurements of impairments in cognition and memory. The sensitivity and specificity of distinguishing AD dementia and CN using white matter FCs were 0.83 and 0.81 respectively.
Conclusions and relevance
The white matter FC decreased in late MCI and AD dementia patients compared to CN participants, and this decrease was correlated with cognitive measures. White matter FC is valuable in the prediction of AD. All these findings suggest that white matter FC may be a promising avenue for understanding functional impairments in white matter tracts during AD progression.
Introduction
Alzheimer’s disease (AD) is the most common progressive neurodegenerative disorder, which begins at a pre-symptomatic stage before subjects exhibit increasingly severe cognitive impairments and ultimately, dementia [1, 2]. Histopathological evidence of degeneration during this progression has been observed in human brains in both gray matter (GM) and white matter (WM) [3, 4]. While there has been considerable emphasis on GM changes, pathological alterations of WM post mortem have also been reported not only in late stages of AD (associated with loss of axons and oligodendrocytes [5] and concomitant with vascular abnormalities [6, 7]), but also in earlier, pre-clinical stages, probably related to amyloid toxicity [8]. Moreover, atrophy has been found to be even more prominent in WM than in GM in early stage disease [3]. Consequently, appropriate measures of changes within WM may be valuable biomarkers of neurodegeneration in AD. To date, structural changes of WM have been intensively investigated [9–11], however, there have been no studies investigating functional changes in WM, which presumably link structure and behavioral performance, in the progression towards AD dementia (ADD).
Functional magnetic resonance imaging (fMRI) has been previously used to detect functional alterations arising in AD [12–14] but to date such studies have been almost exclusively focused on GM, with very limited exceptions [15, 16]. FMRI detects changes in MRI images caused by variations in blood oxygenation (blood oxygenation level dependent (BOLD) effects) that in GM correspond to changes in neural activity [17]. Temporal correlation of BOLD signals arising from different GM regions reflects the functional synchronization among these regions, defined as functional connectivity (FC), and has been widely used in neuroimaging studies [18]. By contrast, BOLD signals in WM are expected to be much smaller than those in GM and consequently are excluded from image analyses. However, recently we demonstrated that BOLD fluctuations in WM share common features with those from GM and they correlate significantly with BOLD signals from specific GM regions to which they connect [19, 20]. Relationships between WM tracts and GM regions may be summarized by a functional correlation matrix (FCM) of their pair-wise correlations at rest, while different WM tracts can be inter-related using a similar approach. Those FCs reflect synchronizations of the hemodynamics between WM tracts and GM regions or between two WM tracts, which are hypothesized to be adversely influenced due to biological degeneration, e.g., tissue degeneration and cerebrovascular disorder, occurring during AD evolution.
In this study, we extended these new findings and analyses, originally described in our previous work [19–22], to quantify changes in WM fMRI metrics during the progression to ADD. We measured the differences in the FCMs for WM-GM correlations (FCMWG) and WM-WM correlations (FCMWW) between a healthy group and each of five participant groups at different stages of cognitive impairments. We also subsequently evaluated the correlations between these FC metrics and neuropsychological measures of cognition and memory. Finally, we explored the use of machine learning to differentiate between the controls and patients at different AD stages to evaluate how well WM FC can predict AD progression.
Materials and methods
Participants
Data used in this study were all obtained from the database of the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (adni.loni.usc.edu). The participants included in our study were selected as following. First, the participants must have unprocessed images of both resting state fMRI (rsfMRI) and T1-weighted (T1w) modalities at baseline available in ADNI 2 or ADNI 3. If one participant had multiple datasets, then only the dataset acquired most recently was selected. Second, the participants whose ages were less than 60 or more than 90 years old were excluded. Third, the participants with only multiband rsfMRI were excluded due to the inconsistent acquisition protocol.
The participants were grouped as cognitive normal (CN), significant memory concerns (SMC), early mild cognitive impairments (eMCI), mild cognitive impairments (MCI), late MCI (lMCI) and ADD. The full criteria for clinical classifications are described in the ADNI manual [23].
MRI
3T rsfMRI and T1w data, acquired at multiple institutions with the same imaging protocol, were preprocessed using the Data Processing Assistant for Resting State fMRI (DPARSFA) [24], a package based on SPM (https://www.fil.ion.ucl.ac.uk/spm). First, the rsfMRI images were corrected for slice timing and head motion. Twenty-four motion parameters [25] and mean CSF signal were regressed out. The resulting rsfMRI data were filtered (passband = 0.01–0.1Hz), coregistered to MNI space [26], detrended, and then normalized voxel-wise into a time-course with zero mean and unit variance. Next, WM, GM, and cerebrospinal fluid (CSF) were segmented using the T1w images [27] and their tissue probability maps were spatially normalized to the MNI space.
Calculation of functional correlation matrix (FCM)
The calculations of correlations for each participant were restricted to 48 WM and 82 GM regions of interest (ROIs, listed in Table 1) that were defined by the Eve atlas [28] (21 deep WM tracts in each hemisphere and 6 commissure tracts, see S1 Fig) and PickAtlas [29] (41 Brodmann areas in each hemisphere) and were further constrained within masks generated by thresholding the WM and GM probability maps at 0.8. The preprocessed time-courses were averaged over the voxels within each ROI and for each pair of WM and GM ROIs they were then cross correlated, excluding any time points with large motions (framewise displacement [30] >0.5). The resulting 48x82 correlation coefficients formed an FCM of WM-GM pairs (FCMWG). Similarly, the mean time-courses for each pair of WM ROIs were cross correlated and the 48x48 correlation coefficients formed an FCM of WM-WM pairs (FCMWW). Meanwhile, we generated FCM of GM-GM pairs (FCMGG) to confirm the validity of our processing pipeline. The possible influences of covariates, including age, gender, years of education and acquisition-site, were regressed out from FCMWG or FCMWW element by partialling out procedure via a generalized linear model.
Table 1. List of WM and GM ROIs.
| White Matter (WM) ROIs | Gray Matter (GM) ROIs | ||
|---|---|---|---|
| CST (l, r): | Corticospinal Tract (left, right) | BA1 (l, r): | Primary Somatosensory Cortex 1 (left, right) |
| ML (l, r): | Medial Lemniscus (left, right) | BA2 (l, r): | Primary Somatosensory Cortex 2 (left, right) |
| ICP (l, r): | Inferior Cerebellar Peduncle (left, right) | BA3 (l, r): | Primary Somatosensory Cortex 3 (left, right) |
| SCP (l, r): | Superior Cerebellar Peduncle (left, right) | BA4 (l, r): | Primary Motor Cortex (left, right) |
| CP (l, r): | Cerebral Peduncle (left, right) | BA5 (l, r): | Somatosensory Association Cortex (left, right) |
| ALIC (l, r): | Anterior Limb of Internal Capsule (left, right) | BA6 (l, r): | Premotor and Supplementary Motor (left, right) |
| PLIC (l, r): | Posterior Limb of Internal Capsule (left, right) | BA7 (l, r): | Visuo-Motor Coordination (left, right) |
| RLIC (l, r): | Retrolenticular Limb of Internal Capsule (left, right) | BA8 (l, r): | Frontal Eye Fields (left, right) |
| ACR (l, r): | Anterior Corona Radiata (left, right) | BA9 (l, r): | Dorsolateral Prefrontal Cortex (left, right) |
| SCR (l, r): | Superior Corona Radiata (left, right) | BA10 (l, r): | Anterior Prefrontal Cortex (left, right) |
| PCR (l, r): | Posterior Corona Radiata (left, right) | BA11 (l, r): | Orbitofrontal Area (left, right) |
| PTR (l, r): | Posterior Thalamic Radiation (include Optic Radiation) (left, right) | BA13 (l, r): | Insular Cortex (left, right) |
| SS (l, r): | Sagittal Stratum (include inferior longitudinal fasciculus and fronto-occipital fasciculus) (left, right) | BA17 (l, r): | Primary Visual Cortex (V1) (left, right) |
| EC (l, r): | External Capsule (left, right) | BA18 (l, r): | Secondary Visual Cortex (V2) (left, right) |
| CGC (l, r): | Cingulum (Cingulate) (left, right) | BA19 (l, r): | Associative Visual Cortex (V3-5) (left, right) |
| CGH (l, r): | Cingulum (Hippocampus) (left, right) | BA20 (l, r): | Inferior Temporal Gyrus (left, right) |
| FXC (l, r): | Fornix (Cres) (left, right) | BA21 (l, r): | Middle Temporal Gyrus (left, right) |
| SLF (l, r): | Superior Longitudinal Fasciculus (left, right) | BA22 (l, r): | Superior Temporal Gyrus (left, right) |
| SFO (l, r): | Superior Fronto-Occipital Fasciculus (left, right) | BA23 (l, r): | Ventral Posterior Cingulate Cortex (left, right) |
| UF (l, r): | Uncinate Fasciculus (left, right) | BA24 (l, r): | Ventral Anterior Cingulate Cortex (left, right) |
| TAP (l, r): | Tapetum (left, right) | BA25 (l, r): | Subgenual Area (left, right) |
| MCP: | Middle Cerebellar Peduncle | BA26 (l, r): | Ectosplenial Portion of Retrosplenial Region (left, right) |
| PCT: | Pontine Crossing Tract | BA27 (l, r): | Piriform Cortex (left, right) |
| GCC: | Genu of Corpus Callosum | BA28 (l, r): | Ventral Entorhinal Cortex (left, right) |
| BCC: | Body of Corpus Callosum | BA29 (l, r): | Retrosplenial Cingulate Cortex (left, right) |
| SCC: | Splenium of Corpus Callosum | BA30 (l, r): | Part of Cingulate Cortex (left, right) |
| FX: | Fornix | BA32 (l, r): | Dorsal Anterior Cingulate Cortex (left, right) |
| BA34 (l, r): | Dorsal Entorhinal Cortex (left, right) | ||
| BA35 (l, r): | Perirhinal Cortex (left, right) | ||
| BA36 (l, r): | Ectorhinal Area (left, right) | ||
| BA37 (l, r): | Occipitotemporal Area (part of fusiform gyrus and interior temporal gyrus (left, right) | ||
| BA38 (l, r): | Temporopolar Area (left, right) | ||
| BA39 (l, r): | Angular Gyrus (left, right) | ||
| BA40 (l, r): | Supramarginal Gyrus (left, right) | ||
| BA41 (l, r): | Auditory Cortex 1 (left, right) | ||
| BA42 (l, r): | Auditory Cortex 2 (left, right) | ||
| BA43 (l, r): | Primary Gustatory Cortex (left, right) | ||
| BA44 (l, r): | Pars Opercularis (left, right) | ||
| BA45 (l, r): | Pars Triangularis (left, right) | ||
| BA46 (l, r): | Dorsolateral Prefrontal Cortex (left, right) | ||
| BA47 (l, r): | Pars Orbitalis (left, right) | ||
Neuropsychological test
Neuropsychological scores included the Mini-Mental State Examination (MMSE) score, Clinical Dementia Rating (CDR) global score, CDR Sum of Boxes (CDR-SOB), Global Deterioration Scale (GDS), Functional Assessment Questionnaire (FAQ) total score, Wechsler Memory Scale-Logical Memory II Subscale (WMS-LMII), Alzheimer’s Disease Assessment Scale-Cognitive subscale (ADAS-Cog) and Hachinski scale, which are the most commonly used scores for clinical assessment and AD studies.
Statistical analysis
The characteristics of the six subject groups were summarized, and the differences among groups were tested by one-way ANOVA or chi-squared test.
The FCMs (FCMWG or FCMWW) within each clinical group were averaged to produce a mean matrix (mFCM). Differences in the mFCM values, and the effect sizes of these differences [31] between the CN group and every other group were calculated. To assess the statistical significance of FC difference between groups, the permutation test (10,000 permutations) was conducted for each FCM element across all participants within any two comparison groups. The resulting P-values were corrected for multiple comparisons using a false discovery rate (FDR, [32]). Each corrected P-value was denoted as PFDR. To estimate the FC within one WM tract, the so-called WM-tract-wise FC, all the 82 FCMWG elements or 48 FCMWW elements corresponding to this WM ROI were averaged. The mean and standard deviation of each WM-tract-wise FC across participants within each group were then calculated. The WM-tract-wise FCs in the CN group were compared with every non-CN group using unpaired-sample t-tests.
To measure the general trend of WM FC as AD progresses, all the elements of each participant’s FCMWG or FCM WW were averaged, defined by overall-FC, and then the group mean and standard deviation of the overall-FC within each clinical group were evaluated, and finally normalized by linear scaling. More specifically, normalization included converting the mean value of CN group into 1 and the mean value of ADD group into 0, calculating the parameters for this linear transformation and then applying the transformation to all the means and standard deviations. On the other hand, the mean and standard deviation of each neuropsychological score within each clinical group were also calculated and normalized by the same linear scaling procedure.
The association between each single FCM element and each neuropsychological score was evaluated by calculating the linear correlation coefficient between the element and the score across all participants. To gauge the integrated correlation of a WM tract’s connectivity with the score, all the correlation coefficients corresponding to the same WM tract were averaged.
To further evaluate the associations between combined FCM elements and each neuropsychological score, a random forest (RF) regression model was trained to predict the score after feature selection from all FCM elements. The value of goodness of fit, R2 was calculated based on comparing true and predicted scores. Subjects that did not have any neuropsychological scores were excluded from the regression study.
Machine learning classification
A support vector machine (SVM) with a radial-basis function kernel was used to classify the CN group and different combinations of groups of impaired subjects (i.e., ADD alone; lMCI and ADD; MCI, lMCI and ADD; eMCI, MCI, lMCI and ADD; and SMC, eMCI, MCI, lMCI and ADD). We used all FCMWG and FCMWW elements as initial features and implemented an RF algorithm to select those features that provided more accurate classifications, a similar procedure to our previous study [33]. In detail, the number of trees for the RF classifier was chosen to be 200 as it was observed that increasing the number of trees further resulted in no significant reduction of classification error. The splitting criterion for RF was based on the GUIDE algorithm [34]. Individual feature importance was computed by measuring how much the predictive accuracy of the RF classifier deteriorates when the feature’s values were randomly permuted [35]. The idea is that altering the value of an important feature will degrade the performance of a classifier. After the importance of each feature obtained individually, the features that did not improve performance at all were at first removed from the set. The remaining features were arranged in descending order of their importance. Features were added sequentially, and classification error was noted for this cumulative feature set. The optimal feature set was taken to be the one which provided the lowest classification error. A similar method was used for feature selection in the case of regression analysis abovementioned. There were 5064 WM FCs in this study, so the features arranged in descending order of importance, were added five at a time sequentially to reduce the computational load. In the case of the classification task, SVM with a radial-basis function (RBF) kernel was optimized with respect to C and Gamma, the two hyper-parameters. C regularized the classifier, and Gamma denoted variance of the RBF kernel and controlled the width of the kernel. Mean squared error of a 10-fold cross-validation (CV) was calculated to measure the classification error. More specifically, the data were split into 10 subsets. The SVM model was trained on 9 subsets and then evaluated on the remaining subsets. This process was repeated 10 times, with a different subset as testing data each time. One error was estimated at each time and the final error was the average of the 10 errors. Also, the penalty involved for misclassification of the disease group versus control group was manually varied so that data imbalance between the groups did not tilt the model accuracy towards one group [36]. Moreover, the receiver-operating characteristic (ROC) analysis was performed and the area under curve (AUC), sensitivity and specificity were noted.
Results
Participant characteristics
Table 2 shows characteristics of all 383 participants, grouped into CN (n = 136), SMC (n = 46), eMCI (n = 83), MCI (n = 37), lMCI (n = 46) and ADD (n = 35), in order of disease severity. Among these groups, no significant differences in age (P = 0.93), sex (P = 0.22), handedness (P = 0.99), years of education (P = 0.23), brain volume (P = 0.41) or Hachinski scale (P = 0.25) were observed. The scanner vendor breakdown, MMSE, CDR global, CDR-SOB, GDS, FAQ, WMS-LMII and ADAS-Cog scores did differ significantly among groups (P <0.001).
Table 2. Characteristics of participant groups.
| Characteristics | CN (n = 136) | SMC (n = 46) | eMCI (n = 83) | MCI (n = 37) | lMCI (n = 46) | ADD (n = 35) | P-value (ANOVA or chi-square) |
|---|---|---|---|---|---|---|---|
| Age, mean (SD), y | 74.5 (7.1) | 75.3 (5.8) | 74.5 (7.0) | 74.3 (7.2) | 74.6 (6.8) | 75.6 (6.8) | 0.93 |
| Female sex, No. (%) | 82(60) | 26(57) | 42 (51) | 15 (41) | 21 (46) | 16 (46) | 0.22 |
| Handedness, No. (%) | 126 (92) | 42 (91) | 76 (92) | 34 (92) | 42 (91) | 33 (94) | 0.99 |
| Education, mean (SD), y | 16.8 (2.3) | 16.8 (2.6) | 16.0 (2.7) | 16.3 (2.5) | 16.4 (2.9) | 16.2 (2.7) | 0.23 |
| Scanner vendor (S:G:P) | 86:27:24 | 18:15:13 | 31:11:41 | 18:9:10 | 19:6:21 | 6:3:26 | <0.001 |
| Brain volume (SD) X105 | 10.6 (0.9) | 10.7 (0.9) | 10.6 (2.2) | 10.4 (1.0) | 10.4 (1.1) | 10.2 (1.2) | 0.41 |
| MMSE score, mean (SD) | 29.1 (1.7) | 29.1 (1.0) | 27.4 (2.9) | 28.0 (1.5) | 25.8 (5.6) | 22.4 (3.2) | <0.001 |
| CDR global score, mean (SD) | 0.0 (0.2) | 0.1 (0.2) | 0.4 (0.3) | 0.5 (0.0) | 0.6 (0.5) | 0.8 (0.2) | <0.001 |
| CDR-SOB score, mean (SD) | 0.3 (1.0) | 0.1 (0.4) | 1.7 (2.2) | 1.2 (0.8) | 2.6 (3.2) | 4.7 (1.5) | <0.001 |
| GDS score, mean (SD) | 0.8 (1.5) | 1.3 (1.3) | 1.8 (2.0) | 1.5 (1.3) | 1.8 (2.3) | 1.5 (1.3) | <0.001 |
| FAQ score, mean (SD) | 1.0 (3.7) | 0.4 (0.8) | 4.2 (6.5) | 3.1 (4.4) | 6.5 (8.7) | 14.6 (6.2) | <0.001 |
| WMS-LMII score, mean (SD) | 15.4 (3.3) | 15.4 (3.0) | 12.4 (5.1) | 9.2 (3.8) | 9.7 (5.0) | 4.5 (3.1) | <0.001 |
| ADAS-Cog score, mean (SD) | 9.6 (4.4) | 8.2 (3.1) | 12.0 (6.0) | 12.3 (3.4) | 14.0 (8.3) | 22.7 (7.4) | <0.001 |
| Hachinski scale, mean (SD) | 0.5 (0.7) | 0.6 (1.0) | 1.0 (1.2) | 0.8 (1.2) | 0.7 (0.9) | 0.9 (0.9) | 0.25 |
Note: S = Siemens; G = GE Medical Systems; P = Philips Medical System and Philips Healthcare.
WM functional connectivity deficits in progression to AD
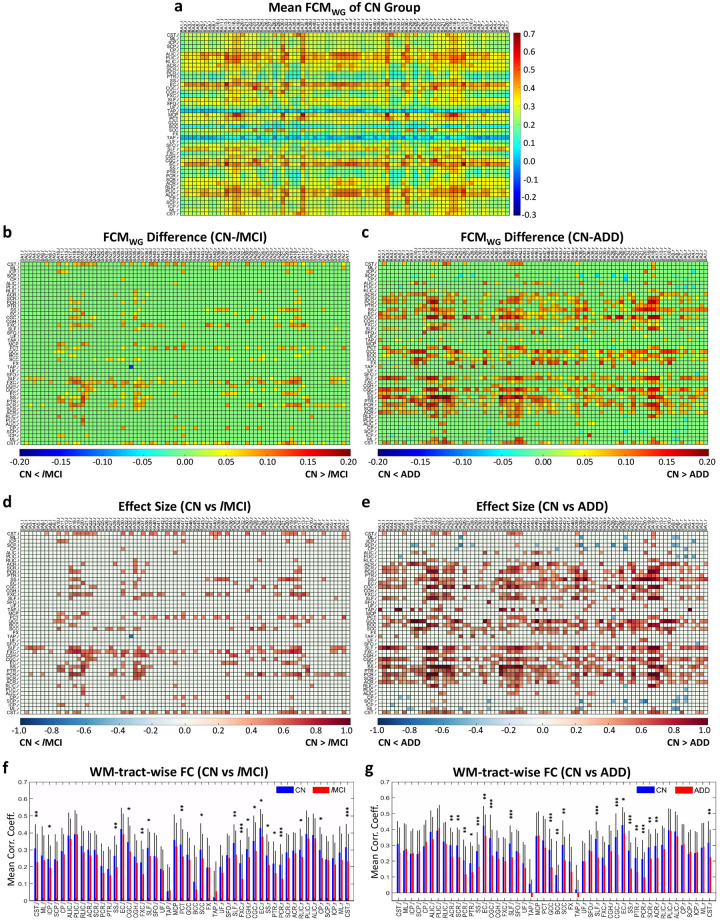
Fig 1a presents the mean FCMWG (mFCMWG) for CN group, which reveals the general synchronization pattern between whole-brain WM ROIs and GM ROIs during resting state. By comparing this FCMWG to other non-CN groups, we found significant FC decreases (PFDR<0.05) in lMCI and ADD patients relative to controls in a number of WM-GM pairs (Fig 1b and 1c). The effect sizes of group difference for those WM-GM pairs were mostly larger than 0.3, shown in Fig 1d and 1e. Furthermore, there were obvious horizontal patterns observed in the difference matrices (Fig 1b and 1c), which appeared to correspond to specific WM tracts. In turn, an in-depth comparison on WM-tract-wise FC, derived from FCMWG, between groups was conducted and revealed that the WM-tract-wise FC decreased significantly (p<0.05) in the lMCI group relative to CN group (Fig 1f) in the following WM tracts: splenium of corpus callosum, pontine crossing fibers, bilateral superior longitudinal fasciculus, bilateral fornix (cres), bilateral cingulum (cingulate), bilateral sagittal stratum, bilateral corticospinal tract, left inferior cerebellar peduncle, right cingulum (hippocampus), right external capsule, right posterior thalamic radiation, right posterior corona radiata, right retrolenticular limb of internal capsule and right cerebral peduncle. Similarly, ADD patients had reduced FC (p<0.05) (Fig 1g) in corpus callosum, bilateral superior longitudinal fasciculus, bilateral cingulum (cingulate), bilateral external capsule, bilateral sagittal stratum, bilateral posterior thalamic radiation, bilateral corona radiata, and right corticospinal tract.
Fig 1. Significant differences in mean FCMWG (mFCMWG) and WM-tract-wise FC between controls (CN) and patients with lMCI or ADD.
(a) mFCMWG of CN group. (b, c) Difference of subtracting mFCMWG of lMCI (b) or ADD (c) from mFCMWG of CN group. The P-value for each element was derived from permutation-test (10,000 permutations) across all participants within groups, and then adjusted using an FDR. Those elements with PFDR >0.05 were set to be zero. (d, e) Effect size of the mFCMWG difference between CN and lMCI (d) or ADD (e), thresholded by PFDR. (f, g) GM-averaged correlation coefficients of WM tracts, i.e., WM-tract-wise FC, in CN group (blue) and lMCI group (red) (f) and in CN group (blue) and ADD group (red) (g). Mean and standard deviation of each WM-tract-wise FC are shown, and * indicates p <0.05, ** indicates p<0.01 and *** indicates p<0.001, calculated by unpaired-sample t-test.
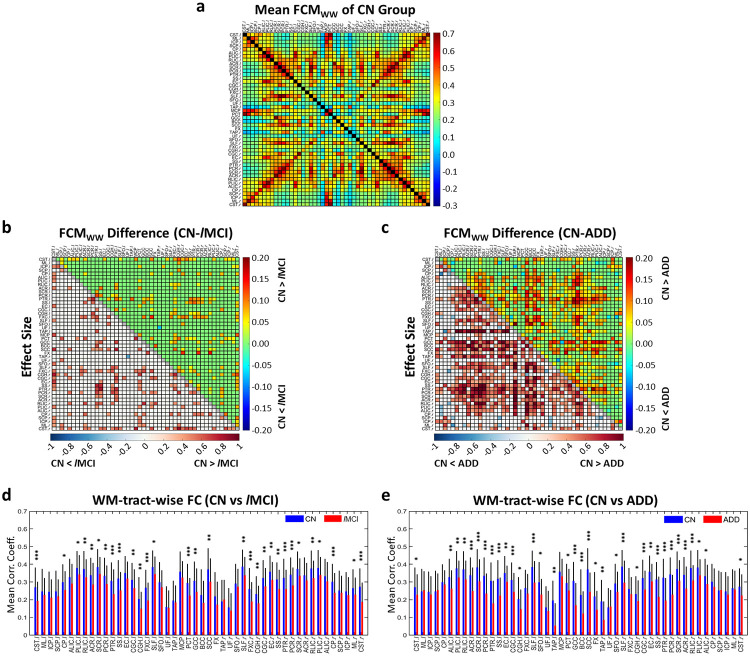
Likewise, Fig 2a exhibits the mean FCMWW (mFCMWW) for CN group. The FC significantly decreased (PFDR<0.05) in lMCI and ADD patients relative to CN group in a number of WM-WM pairs (upper triangles in Fig 2b and 2c) and the effect sizes of group differences for those WM-WM pairs were mostly greater than 0.3 (lower triangles in Fig 2b and 2c). In terms of WM-tract-wise FC derived from FCMWW, significant declines (p<0.05) appeared in several tracts in both the lMCI and ADD groups relative to the CN group (Fig 2d and 2e), including corpus callosum, superior longitudinal fasciculus, fornix (cres), cingulum (cingulate and hippocampus), external capsule, sagittal stratum, posterior thalamic radiation, corona radiata, internal capsule, and corticospinal tract. There were also a number of WM tracts presenting declined FC only in the ADD groups relative to the CN group, such as fornix, tapetum and superior fronto-occipital fasciculus. The significances of all WM tracts with respect to the decline of WM-tract-wise FC derived from both FCMWG and FCMWW are all summarized in S1 Table.
Fig 2. Significant differences in mean FCMWW (mFCMWW) and WM-tract-wise FC between controls (CN) and patients with lMCI or ADD.
(a) mFCMWW of CN group. (b, c) Difference of mFCMWW between CN and lMCI or ADD (upper triangle) and effect size of the mFCMWW difference (lower triangle). (d, e) WM-averaged correlation coefficients of WM tracts, i.e., WM-tract-wise FC, in CN group (blue) and lMCI group (red) (d) and in CN group (blue) and ADD group (red) (e). * indicates p< 0.05, ** indicates p<0.01 and *** indicates p<0.001.
By contrast, no significant changes in FCMWG or FCMWW between CN and any of the early disease groups (i.e., SMC, eMCI and MCI) were observed at the same P-value threshold (PFDR<0.05). Moreover, comparisons between mFCMWW and the group mean of GM-GM FCM (mFCMGG, S2 Fig) show a generally lower level of WM-WM correlation, with a relative decrease of 25–30% in overall average of FCM for every study group.
Correlation between WM FC and neuropsychological scores
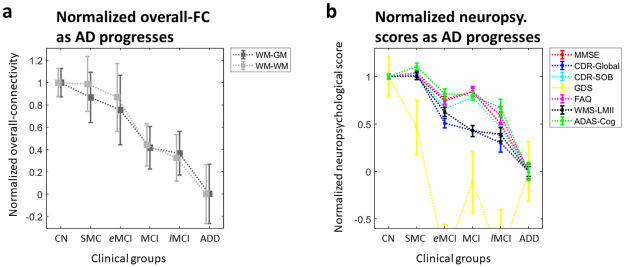
The normalized group means of overall-FC presented in Fig 3a decreased gradually as AD progressed, which in general conforms to current hypothetical models of AD evolution [37]. The normalized overall trends in 7 neuropsychological measures across groups (Fig 3b) show a striking similarity with this overall-FC trend.
Fig 3. Normalized overall-FC and neuropsychological scores for each clinical group in AD progression.
(a) Normalized group mean (gray square) and standard deviation of mean (gray bar) of the overall-FC for each clinical group. The six clinical groups are CN, SMC, eMCI, MCI, lMCI and ADD groups. (b) Normalized mean (colored square) and standard deviation (colored bar) of the neuropsychological scores for each clinical group.
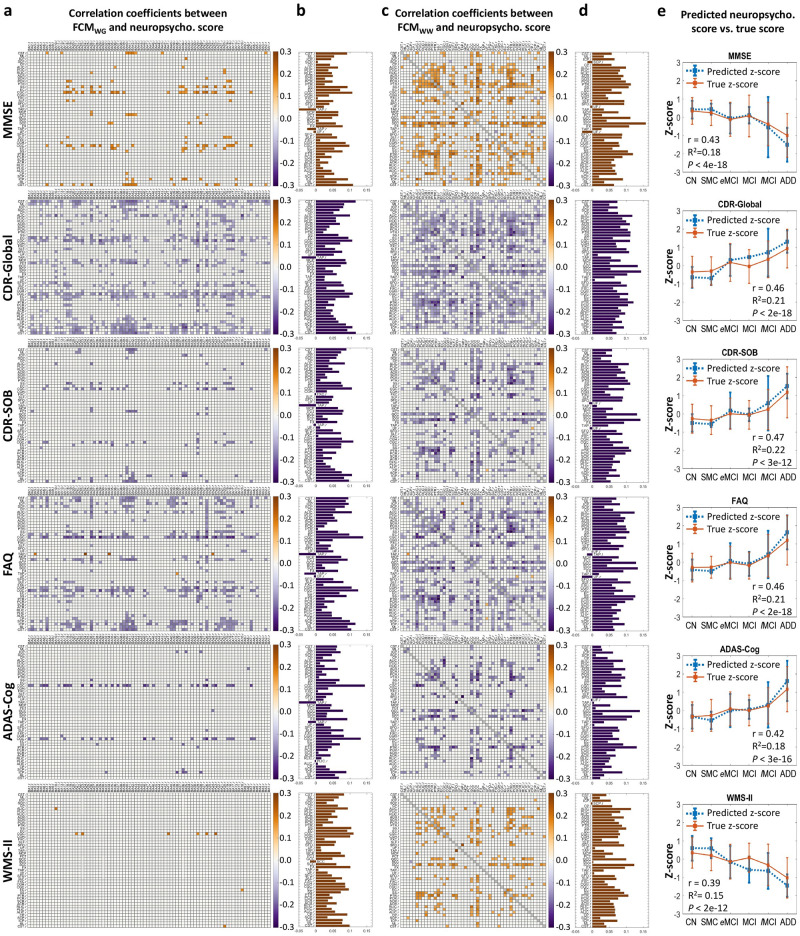
Fig 4a–4d shows correlation coefficients between elements in FCMWG or FCMWW and neuropsychological scores which are significantly different from zero (PFDR<0.05). No significant correlations were found between any element in FCM and the Hachinski scale or GDS score.
Fig 4. Correlations between WM FC and neuropsychological scores across all subjects.
(a or c) Matrix of Pearson’s correlation coefficients between single element in FCMWG or FCMWW and MMSE score, CDR-Global score, CDR-SOB score, FAQ score, ADAS-Cog score, or WMS-LMII score. Each correlation coefficient with PFDR > 0.05 was set to be zero. (b or d) Average of correlation coefficients along each WM tract in a or c. See Table 1 for the lists of WM and GM ROIs. (e) Group means and standard deviations of Z-scores of true neuropsychological scores and predicted scores using RF regression model with all WM FC as initial features. The r, R2 and P in each plot are the Pearson’s correlation coefficient between true scores and predicted scores across all subjects, R-square value and P-value, respectively.
FCMWG and FCMWW elements within bilateral sagittal stratum, bilateral cingulum (cingulate), left cingulum (hippocampus), bilateral fornix (cres), splenium of corpus callosum, bilateral posterior thalamic radiation, and bilateral cerebrospinal tract showed significant positive associations with MMSE scores [38] (Fig 4a–4d), indicating that reduced WM FC corresponds to more severe cognitive impairment.
The CDR-global [39] and CDR-SOB scores are indicators of dementia severity [40]. The sum of negative correlations along WM tracts between FCM and CDR-global was strong in bilateral sagittal stratum, bilateral cingulum (cingulate), bilateral fornix (cres), right superior longitudinal fasciculus, genu and splenium of corpus callosum, fornix, bilateral posterior corona radiata, bilateral posterior thalamic radiation, left anterior limb of internal capsule, and bilateral corticospinal tract (Fig 4a–4d). For the linkage between FCM elements and CDR-SOB score, clear negative correlations were found in bilateral sagittal stratum, bilateral cingulum (cingulate), left fornix (cres), bilateral posterior thalamic radiation, bilateral posterior corona radiata, genu and splenium of corpus callosum, left anterior limb of internal capsule, right retrolenticular limb of internal capsule, and right corticospinal tract.
Negative correlations were dominant in bilateral sagittal stratum, bilateral cingulum (cingulate), bilateral posterior thalamic radiation, bilateral posterior corona radiata, right superior longitudinal fasciculus, left anterior limb of internal capsule, left posterior limb of internal capsule, genu and splenium of corpus callosum between FCM and FAQ [41] that describes the level of performance of daily function activities (Fig 4a–4d).
Bilateral cingulum (cingulate) showed the most significant negative correlations between FCMWG and the ADAS-Cog [42] score, the overall degree of cognitive decline (Fig 4a–4d). Genu and splenium of corpus callosum, fornix, bilateral posterior thalamic radiation, left posterior corona radiata, left cingulum (cingulate), left sagittal stratum, showed significant correlation between FCMWW and ADAS-Cog (Fig 4c and 4d).
Genu and splenium of corpus callosum, bilateral sagittal stratum, left anterior limb of internal capsule, right posterior thalamic radiation, and left cingulum (cingulate) showed stronger positive correlations between FC and the WMS-LMII [43] score, a measure of episodic memory (Fig 4a–4d).
Correlation between combined WM FCs and neuropsychological scores
The correlation coefficients between the true and RF-predicted scores of ADAS-Cog, CDR-Global, CDR-SOB, FAQ and MMSE were 0.39–0.47 with highly significant P-value (<0.001) (Fig 4e). The R2 values in Fig 4e indicate that 15%-22% of the variances of those individual scores could be explained by the variance of the combined WM FCs, and vice versa.
Prediction of AD stages
The performance of the SVM classification using WM FC features was best for distinguishing ADD from CN group with sensitivity of 0.83 and specificity of 0.81 (AUC = 0.87). The performance of prediction reduced monotonically with addition of patients from earlier stages to the ADD group (Fig 5).
Fig 5. ROC curves of SVM classifications and a summary of their CV errors, AUC, sensitivity and specificity.
(a) ROC curves of SVM algorithm for distinguishing patients from CN. Different color represents different cumulative group of patients. (b) The errors of 10-fold CV and ROC related indices-AUC, sensitivity and specificity for the classifications.
Discussion
In conventional rsfMRI studies, correlations in BOLD signals between GM regions are interpreted as revealing FC. Extending this concept, we investigated the FC between WM and GM regions or between WM regions for 383 ADNI participants from six clinical groups. We mainly found that: 1) lMCI and ADD have significant deficits in regional WM FC relative to CN, 2) regional WM FC was significantly associated with neuropsychological scores (i.e., MMSE, CDR, FAQ, ADAS-Cog and WMS-LMII), and 3) the sensitivity and specificity in prediction of late stages of AD using FC as features reach a reasonable range. To the best of our knowledge, this is the first investigation of FC degeneration in WM throughout the evolution of AD pathology. Our findings indicate that FC of WM from MRI may serve as a novel in vivo biomarker to understand functional impairments of WM in AD, especially for the patients at late stages (i.e., lMCI and ADD).
Our first batch of findings focused on changes in WM FC as AD progresses. Significant decreases in FC were observed in several localized WM tracts in lMCI and ADD patients compared with elderly controls (Figs 1f, 1g, 2d and 2e, or S1 Table). These functional declined WM tracts were mainly projection fibers, association fibers and commissural fibers and have been demonstrated with microstructural degenerations in previous diffusion MRI literature on ADD patients from ADNI [44]. Similar structural degeneration was also observed in brainstem fibers such as corticospinal tract in our study, yet with less consistency across previous studies [44, 45]. Meanwhile, the canonical neuropathological evidence provided by Braak et al. [4] also explains the extensive WM hypofunction in the late stages of AD. As to the earlier stages of AD (i.e., SMC, eMCI and MCI), although no significant changes (PFDR < 0.05) were observed in FCMWG or FCMWW in these groups relative to controls, their mean effect sizes were 0.14, 0.14, and 0.19, respectively, suggesting a progression towards non-trivial group differences. Previous studies on brain microstructure reported alterations in a few selected WM regions in MCI participants, involving cingulate bundle, inferior fronto-occipital fasciculus and parahippocampal subgyral fibers [46, 47], where the FC deficits were found in our lMCI and ADD groups.
From a pathophysiological perspective, the decreases in WM FC metrics observed in late AD stages may be attributable to GM abnormalities, WM degeneration, metabolic changes and/or cerebrovascular changes. GM abnormalities in AD include the appearance of neurofibrillary/senile plaques, neuronal loss, cell shrinkage, reduced dendritic density and synaptic losses [48, 49]. The consequent neural dysfunction could lead to less engagement of WM in transmission of neural information. WM degeneration during AD progression [50–52] includes demyelination [53] and axonal damage [54], which may also weaken the ability of WM to transfer neural signals between regions. WM degeneration has been reported as a direct consequence of amyloid deposition and tau phosphorylation in GM, and of damage to oligodendrocytes, possibly initiated by ischemia, excitotoxicity, oxidative stress and/or iron overload in AD [55]. Cerebral hypometabolism is found in both MCI and ADD patients throughout limbic structures, involving hippocampal complex, medial thalamus, mammillary bodies and posterior cingulate, yet only in ADD patients in amygdala, temporoparietal and frontal association cortex [56, 57]. Hypometabolism may have direct effects on BOLD signals in GM and WM. Further studies to understand the relationship between the GM changes and decreases in WM connectivity in AD are clearly needed and may reflect a combination of factors including direct causes and effects, comorbidities and mutual dependences.
The second batch of our findings mainly revealed the association between WM FC declines and cognitive impairments, manifest in the WM routes serving limbic network. For example, correlations between WM FC and scores of MMSE, CDR as well as ADAS-Cog were mostly found within sagittal stratum, cingulum, fornix and posterior thalamic radiation, which are the major bundles connecting fronto-occipital pair, cingulate-entorhinal pair, hippocampus-mamillary body pair, thalamus-parietal pair, respectively. Those neural circuits are well-known for playing crucial roles in cognition functioning, such as memory and attention, and suffering from impairment during AD [58–62]. Moreover, the structural damages of those WM tracts were also strongly associated with scores of MMSE, CDR and ADAS-Cog [63, 64]. Similarly, the intrinsic FC between hippocampus and posterior cingulate cortex has been reported to be closely associated with WMS-LM scores in elderly people [65]. In addition, WM tracts in left hemisphere appear to correlate with WMS-LMII scores more widely and strongly (Fig 4a–4d), consistent with previous findings that verbal memory tasks are more sensitive to left hemisphere dysfunction [66] and damage to left temporal lobe has consistently been associated with an impairment of verbal memory [67]. In summary, the consistency between our function-behavior findings and previous structural-behavior evidence suggests that the FC in WM adds a new dimension to connectivity measures and in turn assists in filling the gap of our knowledge between structure in WM and neuropsychological performance.
The performances of our SVM classifications indicate that it is feasible to predict late stages of AD using WM FC only. The performance decreased as patients at earlier stages of AD were included sequentially (Fig 5), just as the sensitivities were lower for detecting FCM difference at earlier stages of AD. However, this does not indicate WM FC is never able to reflect the change in early stages. First, Pearson’s correlation coefficient is the most commonly used metric to measure the FC among GM regions, but its accuracy has been proven to be limited [68]. Given the lower SNR in WM BOLD signals compared to GM signals and the difference in hemodynamic response function between WM and GM [20, 69], the Pearson’s correlation coefficient appears to be even less accurate to represent WM-GM FC. In future, it will be interesting to find better metrics for detecting earlier stages of AD. Second, the FDR we used to conduct multiple comparison turned out to be too strict due to the big size of the matrix (e.g., FCMWG: 48x82 = 3936), so the false negative rate might be non-negligible. Moreover, as artificial intelligence developed, such as deep learning algorithms [70], there will be certain method(s) able to distinguish early AD stages from CN. Similarly, we recognize that, while the proposed WM FC metrics allow for determination of neural substrates, currently it is not likely to outperform neuropsychology tests, the primary criteria for staging the disease, in differentiating the study groups. Nevertheless, as our methodology continues evolving, along with advances in MRI technologies, greatly improved performance can be anticipated.
In our analyses, we constrained ROIs to GM or WM only in order to avoid partial volume averaging effects which potentially could overestimate the correlation of time-courses between regions. These correlations of WM with GM or other WM volumes are unlikely caused by drainage effects from adjacent GM because GM drainage occurs outwards, towards the brain surface while deeper WM veins drain inwards to sub-ependymal veins near the lateral ventricles, so there is no direct vascular communication between them [71]. In our analysis we did not regress out global signals because there is growing evidence that they may contain valuable information [72, 73]. Other physiological noises (such as that caused by variations in heart rate and respiration) were, however, regressed out. With these factors in mind, we believe that the WM FC we measured is neither noise effect nor simply a reflection of GM changes.
Conclusions
The present study indicates that WM FCs 1) decline regionally in lMCI and ADD groups relative to a CN group, 2) are significantly related to cognitive scores, and 3) can serve as machine learning features to predict lMCI and ADD with a reasonable sensitivity and specificity. These findings suggest the potential of WM FC, which has been largely overlooked to date, as a novel neuroimaging biomarker to assess AD progression.
Supporting information
The colored WM ROIs are overlaid on the T1 template.
(TIF)
(a-f) mFCMGG (lower triangle) and mFCMWW (upper triangle) for group of CN (a), SMC (b), eMCI (c), MCI (d), lMCI (e) and ADD (f). Each element in mFCMGG or mFCMWW is the group mean of correlation coefficient of the averaged BOLD time courses between two GM regions or two WM regions. See Table 1 for the list of GM ROIs and WM ROIs.
(TIF)
* p<0.05, ** p<0.01, *** p<0.001.
(DOCX)
Acknowledgments
We thank the Vanderbilt Advanced Computing Center for Research and Education (ACCRE) for the support of cluster computation. We also thank ADNI group. The investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Data Availability
All the original fMRI data and cognitive scores are in ADNI database (https://ida.loni.usc.edu/login.jsp?project=adni&page=HOME). The unprocessed fMRI/T1wdata are all stored in the “Image Collection” section of the ADNI database. The spreadsheets of all cognitive scores are all stored in the “Study Data” section(category of “neuropsychological assessments") of the ADNI database.
Funding Statement
The project is supported by the NIH grant R01 NS093669 and R01 NS113832 received by J.C.G. The full name of this funder is National Institute of Neurological Disorders and Stroke (https://www.ninds.nih.gov/). This project is also supported by Vanderbilt University Discovery Grant 600670, received by Y.G. and B.P.R. The full name of this funder is Vanderbilt University (https://www.vanderbilt.edu/provost/internal-funding/discovery-grants/). The two funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Francis PT, Palmer AM, Snape M, Wilcock GK. The cholinergic hypothesis of Alzheimer’s disease: a review of progress. Journal of Neurology, Neurosurgery & Psychiatry. 1999;66(2):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease. Neurology. 1984;34(7):939 10.1212/wnl.34.7.939 [DOI] [PubMed] [Google Scholar]
- 3.de la Monte SM. Quantitation of cerebral atrophy in preclinical and end-stage alzheimer’s disease. Annals of Neurology. 1989;25(5):450–9. 10.1002/ana.410250506 [DOI] [PubMed] [Google Scholar]
- 4.Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathologica. 1991;82(4):239–59. 10.1007/BF00308809 [DOI] [PubMed] [Google Scholar]
- 5.Behrendt G, Baer K, Buffo A, Curtis MA, Faull RL, Rees MI, et al. Dynamic changes in myelin aberrations and oligodendrocyte generation in chronic amyloidosis in mice and men. Glia. 2012;61(2):273–86. 10.1002/glia.22432 [DOI] [PubMed] [Google Scholar]
- 6.Brun A, Englund E. A white matter disorder in dementia of the Alzheimer type: A pathoanatomical study. Annals of Neurology. 1986;19(3):253–62. 10.1002/ana.410190306 [DOI] [PubMed] [Google Scholar]
- 7.Arvanitakis Z, Capuano AW, Leurgans SE, Bennett DA, Schneider JA. Relation of cerebral vessel disease to Alzheimer’s disease dementia and cognitive function in elderly people: a cross-sectional study. The Lancet Neurology. 2016;15(9):934–43. 10.1016/S1474-4422(16)30029-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lue L-F, Kuo Y-M, Roher AE, Brachova L, Shen Y, Sue L, et al. Soluble Amyloid β Peptide Concentration as a Predictor of Synaptic Change in Alzheimer’s Disease. The American Journal of Pathology. 1999;155(3):853–62. 10.1016/s0002-9440(10)65184-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hanyu H, Shindo H, Kakizaki D, Abe K, Iwamoto T, Takasaki M. Increased Water Diffusion in Cerebral White Matter in Alzheimer’s Disease. Gerontology. 1997;43(6):343–51. 10.1159/000213874 [DOI] [PubMed] [Google Scholar]
- 10.Rose SE, Chen F, Chalk JB, Zelaya FO, Strugnell WE, Benson M, et al. Loss of connectivity in Alzheimer’s disease: an evaluation of white matter tract integrity with colour coded MR diffusion tensor imaging. Journal of Neurology Neurosurgery and Psychiatry. 2000;69(4):528–30. 10.1136/jnnp.69.4.528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barber R, Scheltens P, Gholkar A, Ballard C, McKeith I, Ince P, et al. White matter lesions on magnetic resonance imaging in dementia with Lewy bodies, Alzheimer’s disease, vascular dementia, and normal aging. Journal of neurology, neurosurgery, and psychiatry. 1999;67(1):66–72. 10.1136/jnnp.67.1.66 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agosta F, Pievani M, Geroldi C, Copetti M, Frisoni GB, Filippi M. Resting state fMRI in Alzheimer’s disease: beyond the default mode network. Neurobiology of Aging. 2012;33(8):1564–78. 10.1016/j.neurobiolaging.2011.06.007 [DOI] [PubMed] [Google Scholar]
- 13.Binnewijzend MAA, Schoonheim MM, Sanz-Arigita E, Wink AM, van der Flier WM, Tolboom N, et al. Resting-state fMRI changes in Alzheimer’s disease and mild cognitive impairment. Neurobiology of Aging. 2012;33(9):2018–28. 10.1016/j.neurobiolaging.2011.07.003 [DOI] [PubMed] [Google Scholar]
- 14.Dennis EL, Thompson PM. Functional Brain Connectivity Using fMRI in Aging and Alzheimer’s Disease. Neuropsychology Review. 2014;24(1):49–62. 10.1007/s11065-014-9249-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo H, Song X, Sun Z, Beyea SD, Zhang J, Zhang Y, et al. White matter fMRI activation induced by processing speed tasks in Alzheimer’s disease and healthy aging: Preliminary results of a Canada-China Joint Health Research Initiative Project. Radiological Society of North America; Chicago2013.
- 16.Song X, Guo H, Sun Z, Beyea SD, Zhang J, Zhang Y, et al. Functional MRI activation of the white matter in Alzheimer’s disease—Preliminary Results from a Canada-China Joint Health Research Initiative Project. International Society for Vascular Behavioural and Cognitive Disorders; Toronto2013.
- 17.Ogawa S, Lee TM, Kay AR, Tank DW. Brain magnetic resonance imaging with contrast dependent on blood oxygenation. Proceedings of the National Academy of Sciences of the United States of America. 1990;87(24):9868–72. 10.1073/pnas.87.24.9868 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biswal B, Zerrin Yetkin F, Haughton VM, Hyde JS. Functional connectivity in the motor cortex of resting human brain using echo-planar mri. Magnetic Resonance in Medicine. 1995;34(4):537–41. 10.1002/mrm.1910340409 [DOI] [PubMed] [Google Scholar]
- 19.Ding Z, Huang Y, Bailey SK, Gao Y, Cutting LE, Rogers BP, et al. Detection of synchronous brain activity in white matter tracts at rest and under functional loading. Proceedings of the National Academy of Sciences. 2018;115(3):595–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gore JC, Li M, Gao Y, Wu T-L, Schilling KG, Huang Y, et al. Functional MRI and resting state connectivity in white matter—a mini-review. Magnetic Resonance Imaging. 2019;63:1–11. 10.1016/j.mri.2019.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gao Y, Li M, Zu Z, Rogers B, Anderson A, Ding Z, et al. Progressive degeneration of white matter functional connectivity in Alzheimer’s Disease. SPIE Medical Imaging; San Diego, California, United States: 2019. [Google Scholar]
- 22.Gao Y, Li M, Huang AS, Anderson AW, Ding Z, Heckers SH, et al. Declined functional connectivity of white matter during rest and working memory tasks associates with cognitive impairments in schizophrenia. medRxiv. 2020:2020.05.16.20091397. 10.1101/2020.05.16.20091397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weiner M. Study population. Alzheimer’s Disease Neuroimaging Initiative 3 (ADNI3) Protocol2016.
- 24.Yan C-G, Wang X-D, Zuo X-N, Zang Y-F. DPABI: Data Processing & Analysis for (Resting-State) Brain Imaging. Neuroinformatics. 2016;14(3):339–51. 10.1007/s12021-016-9299-4 [DOI] [PubMed] [Google Scholar]
- 25.Friston KJ, Williams S, Howard R, Frackowiak RS, Turner R. Movement-related effects in fMRI time-series. Magn Reson Med. 1996;35(3):346–55. Epub 1996/03/01. 10.1002/mrm.1910350312 . [DOI] [PubMed] [Google Scholar]
- 26.Ashburner J. A fast diffeomorphic image registration algorithm. NeuroImage. 2007;38(1):95–113. 10.1016/j.neuroimage.2007.07.007 [DOI] [PubMed] [Google Scholar]
- 27.Ashburner J, Friston KJ. Unified segmentation. NeuroImage. 2005;26(3):839–51. 10.1016/j.neuroimage.2005.02.018 [DOI] [PubMed] [Google Scholar]
- 28.Mori S, Oishi K, Jiang H, Jiang L, Li X, Akhter K, et al. Stereotaxic white matter atlas based on diffusion tensor imaging in an ICBM template. NeuroImage. 2008;40(2):570–82. Epub 2008/01/03. 10.1016/j.neuroimage.2007.12.035 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lancaster JL, Woldorff MG, Parsons LM, Liotti M, Freitas CS, Rainey L, et al. Automated Talairach Atlas labels for functional brain mapping. Human Brain Mapping. 2000;10(3):120–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. NeuroImage. 2012;59(3):2142–54. Epub 2011/10/14. 10.1016/j.neuroimage.2011.10.018 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York1988.
- 32.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society Series B (Methodological). 1995;57(1):289–300. [Google Scholar]
- 33.Sengupta A, Ramaniharan AK, Gupta RK, Agarwal S, Singh A. Glioma Grading Using a Machine-Learning Framework Based on Optimized Features Obtained From T1 Perfusion MRI and Volumes of Tumor Components. Journal of Magnetic Resonance Imaging. 2019;0(0). 10.1002/jmri.26704 [DOI] [PubMed] [Google Scholar]
- 34.Loh W-Y. Regression trees with unbiased variable selection and interaction detection. Statistica Sinica. 2002;12:361–86. [Google Scholar]
- 35.Breiman L. Random Forests. Machine Learning. 2001;45(1):5–32. 10.1023/A:1010933404324 [DOI] [Google Scholar]
- 36.Zadrozny B, Langford J, Abe N, editors. Cost-sensitive learning by cost-proportionate example weighting. Third IEEE International Conference on Data Mining; 2003 22–22 Nov. 2003.
- 37.Jack CR Jr., Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. The Lancet Neurology. 2010;9(1):119–28. 10.1016/S1474-4422(09)70299-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Folstein MF, Folstein ES, McHugh RP. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–98. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 39.Morris JC. The Clinical Dementia Rating (CDR). Neurology. 1993;43(11):2412. [DOI] [PubMed] [Google Scholar]
- 40.O’Bryant SE, Waring SC, Cullum CM, Hall J, Lacritz L, Massman PJ, et al. Staging dementia using Clinical Dementia Rating Scale Sum of Boxes scores: a Texas Alzheimer’s research consortium study. Archives of neurology. 2008;65(8):1091–5. 10.1001/archneur.65.8.1091 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pfeffer RI, Kurosaki TT, Harrah CH Jr., Chance JM, Filos S. Measurement of functional activities in older adults in the community. J Gerontol. 1982;37(3):323–9. Epub 1982/05/01. 10.1093/geronj/37.3.323 . [DOI] [PubMed] [Google Scholar]
- 42.Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer’s disease. Am J Psychiatry. 1984;141(11):1356–64. Epub 1984/11/01. 10.1176/ajp.141.11.1356 . [DOI] [PubMed] [Google Scholar]
- 43.Wechsler D. WMS-R: Wechsler memory scale-revised: manual1987.
- 44.Mayo CD, Mazerolle EL, Ritchie L, Fisk JD, Gawryluk JR. Longitudinal changes in microstructural white matter metrics in Alzheimer’s disease. NeuroImage: Clinical. 2017;13:330–8. 10.1016/j.nicl.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Y, Schuff N, Du A-T, Rosen HJ, Kramer JH, Gorno-Tempini ML, et al. White matter damage in frontotemporal dementia and Alzheimer’s disease measured by diffusion MRI. Brain. 2009;132(9):2579–92. 10.1093/brain/awp071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fellgiebel A, Schermuly I, Gerhard A, Keller I, Albrecht J, Weibrich C, et al. Functional relevant loss of long association fibre tracts integrity in early Alzheimer’s disease. Neuropsychologia. 2008;46(6):1698–706. 10.1016/j.neuropsychologia.2007.12.010 [DOI] [PubMed] [Google Scholar]
- 47.Rose SE, McMahon KL, Janke AL, O’Dowd B, de Zubicaray G, Strudwick MW, et al. Diffusion indices on magnetic resonance imaging and neuropsychological performance in amnestic mild cognitive impairment. J Neurol Neurosurg Psychiatry. 2006;77(10):1122–8. Epub 2006/06/07. 10.1136/jnnp.2005.074336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Uylings HB, de Brabander JM. Neuronal changes in normal human aging and Alzheimer’s disease. Brain Cogn. 2002;49(3):268–76. Epub 2002/07/26. 10.1006/brcg.2001.1500 . [DOI] [PubMed] [Google Scholar]
- 49.Gómez-Isla T, Hollister R, West H, Mui S, Growdon JH, Petersen RC, et al. Neuronal loss correlates with but exceeds neurofibrillary tangles in Alzheimer’s disease. Annals of Neurology. 1997;41(1):17–24. 10.1002/ana.410410106 [DOI] [PubMed] [Google Scholar]
- 50.Lee S, Viqar F, Zimmerman ME, Narkhede A, Tosto G, Benzinger TL, et al. White matter hyperintensities are a core feature of Alzheimer’s disease: Evidence from the dominantly inherited Alzheimer network. Ann Neurol. 2016;79(6):929–39. Epub 2016/03/27. 10.1002/ana.24647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Medina D, DeToledo-Morrell L, Urresta F, Gabrieli JD, Moseley M, Fleischman D, et al. White matter changes in mild cognitive impairment and AD: A diffusion tensor imaging study. Neurobiol Aging. 2006;27(5):663–72. Epub 2005/07/12. 10.1016/j.neurobiolaging.2005.03.026 . [DOI] [PubMed] [Google Scholar]
- 52.Roher AE, Weiss N, Kokjohn TA, Kuo YM, Kalback W, Anthony J, et al. Increased A beta peptides and reduced cholesterol and myelin proteins characterize white matter degeneration in Alzheimer’s disease. Biochemistry. 2002;41(37):11080–90. Epub 2002/09/11. 10.1021/bi026173d . [DOI] [PubMed] [Google Scholar]
- 53.Gouw AA, Seewann A, Vrenken H, van der Flier WM, Rozemuller JM, Barkhof F, et al. Heterogeneity of white matter hyperintensities in Alzheimer’s disease: post-mortem quantitative MRI and neuropathology. Brain. 2008;131(Pt 12):3286–98. Epub 2008/10/18. 10.1093/brain/awn265 . [DOI] [PubMed] [Google Scholar]
- 54.Scheltens P, Barkhof F, Leys D, Wolters EC, Ravid R, Kamphorst W. Histopathologic correlates of white matter changes on MRI in Alzheimer’s disease and normal aging. Neurology. 1995;45(5):883–8. Epub 1995/05/01. 10.1212/wnl.45.5.883 . [DOI] [PubMed] [Google Scholar]
- 55.Nasrabady SE, Rizvi B, Goldman JE, Brickman AM. White matter changes in Alzheimer’s disease: a focus on myelin and oligodendrocytes. Acta Neuropathol Commun. 2018;6(1):22 Epub 2018/03/04. 10.1186/s40478-018-0515-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nestor PJ, Fryer TD, Smielewski P, Hodges JR. Limbic hypometabolism in Alzheimer’s disease and mild cognitive impairment. Ann Neurol. 2003;54(3):343–51. Epub 2003/09/04. 10.1002/ana.10669 . [DOI] [PubMed] [Google Scholar]
- 57.Minoshima S, Giordani B, Berent S, Frey KA, Foster NL, Kuhl DE. Metabolic reduction in the posterior cingulate cortex in very early Alzheimer’s disease. Ann Neurol. 1997;42(1):85–94. Epub 1997/07/01. 10.1002/ana.410420114 . [DOI] [PubMed] [Google Scholar]
- 58.Vann SD, Nelson AJD. The mammillary bodies and memory: more than a hippocampal relay. Progress in brain research. 2015;219:163–85. Epub 2015/05/16. 10.1016/bs.pbr.2015.03.006 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou Y, Dougherty JH Jr., Hubner KF, Bai B, Cannon RL, Hutson RK. Abnormal connectivity in the posterior cingulate and hippocampus in early Alzheimer’s disease and mild cognitive impairment. Alzheimers Dement. 2008;4(4):265–70. Epub 2008/07/18. 10.1016/j.jalz.2008.04.006 . [DOI] [PubMed] [Google Scholar]
- 60.Pievani M, Agosta F, Pagani E, Canu E, Sala S, Absinta M, et al. Assessment of white matter tract damage in mild cognitive impairment and Alzheimer’s disease. Hum Brain Mapp. 2010;31(12):1862–75. Epub 2010/02/18. 10.1002/hbm.20978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aggleton JP, Pralus A, Nelson AJD, Hornberger M. Thalamic pathology and memory loss in early Alzheimer’s disease: moving the focus from the medial temporal lobe to Papez circuit. Brain: a journal of neurology. 2016;139(Pt 7):1877–90. Epub 2016/04/28. 10.1093/brain/aww083 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wheeler ME, Buckner RL. Functional-anatomic correlates of remembering and knowing. Neuroimage. 2004;21(4):1337–49. Epub 2004/03/31. 10.1016/j.neuroimage.2003.11.001 . [DOI] [PubMed] [Google Scholar]
- 63.Nir TM, Jahanshad N, Villalon-Reina JE, Toga AW, Jack CR, Weiner MW, et al. Effectiveness of regional DTI measures in distinguishing Alzheimer’s disease, MCI, and normal aging. NeuroImage: Clinical. 2013;3:180–95. 10.1016/j.nicl.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bozzali M, Falini A, Franceschi M, Cercignani M, Zuffi M, Scotti G, et al. White matter damage in Alzheimer’s disease assessed in vivo using diffusion tensor magnetic resonance imaging. J Neurol Neurosurg Psychiatry. 2002;72(6):742–6. Epub 2002/05/23. 10.1136/jnnp.72.6.742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang L, LaViolette P, O’Keefe K, Putcha D, Bakkour A, Van Dijk KRA, et al. Intrinsic connectivity between the hippocampus and posteromedial cortex predicts memory performance in cognitively intact older individuals. NeuroImage. 2010;51(2):910–7. 10.1016/j.neuroimage.2010.02.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lee TMC, Yip JTH, Jones-Gotman M. Memory Deficits after Resection from Left or Right Anterior Temporal Lobe in Humans: A Meta-Analytic Review. Epilepsia. 2002;43(3):283–91. 10.1046/j.1528-1157.2002.09901.x [DOI] [PubMed] [Google Scholar]
- 67.Pillon B, Bazin B, Deweer B, Ehrle N, Baulac M, Dubois B. Specificity of memory deficits after right or left temporal lobectomy. Cortex. 1999;35(4):561–71. Epub 1999/11/26. 10.1016/s0010-9452(08)70819-0 . [DOI] [PubMed] [Google Scholar]
- 68.Mohanty R, Sethares WA, Nair VA, Prabhakaran V. Rethinking Measures of Functional Connectivity via Feature Extraction. Scientific Reports. 2020;10(1):1298 10.1038/s41598-020-57915-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li M, Newton AT, Anderson AW, Ding Z, Gore JC. Characterization of the hemodynamic response function in white matter tracts for event-related fMRI. Nature Communications. 2019;10(1):1140 10.1038/s41467-019-09076-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jo T, Nho K, Saykin AJ. Deep Learning in Alzheimer’s Disease: Diagnostic Classification and Prognostic Prediction Using Neuroimaging Data. Frontiers in Aging Neuroscience. 2019;11:220 10.3389/fnagi.2019.00220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.San Millán Ruíz D, Yilmaz H, Gailloud P. Cerebral developmental venous anomalies: Current concepts. Annals of Neurology. 2009;66(3):271–83. 10.1002/ana.21754 [DOI] [PubMed] [Google Scholar]
- 72.Murphy K, Birn RM, Handwerker DA, Jones TB, Bandettini PA. The impact of global signal regression on resting state correlations: Are anti-correlated networks introduced? NeuroImage. 2009;44(3):893–905. 10.1016/j.neuroimage.2008.09.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saad ZS, Gotts SJ, Murphy K, Chen G, Jo HJ, Martin A, et al. Trouble at rest: how correlation patterns and group differences become distorted after global signal regression. Brain connectivity. 2012;2(1):25–32. 10.1089/brain.2012.0080 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The colored WM ROIs are overlaid on the T1 template.
(TIF)
(a-f) mFCMGG (lower triangle) and mFCMWW (upper triangle) for group of CN (a), SMC (b), eMCI (c), MCI (d), lMCI (e) and ADD (f). Each element in mFCMGG or mFCMWW is the group mean of correlation coefficient of the averaged BOLD time courses between two GM regions or two WM regions. See Table 1 for the list of GM ROIs and WM ROIs.
(TIF)
* p<0.05, ** p<0.01, *** p<0.001.
(DOCX)
Data Availability Statement
All the original fMRI data and cognitive scores are in ADNI database (https://ida.loni.usc.edu/login.jsp?project=adni&page=HOME). The unprocessed fMRI/T1wdata are all stored in the “Image Collection” section of the ADNI database. The spreadsheets of all cognitive scores are all stored in the “Study Data” section(category of “neuropsychological assessments") of the ADNI database.