Abstract
Background
In a surgical setting, COVID-19 patients may trigger in-hospital outbreaks and have worse postoperative outcomes. Despite these risks, there have been no consistent statements on surgical guidelines regarding the perioperative screening or management of COVID-19 patients, and we do not have objective global data that describe the current conditions surrounding this issue. This study aimed to clarify the current global surgical practice including COVID-19 screening, preventive measures and in-hospital infection under the COVID-19 pandemic, and to clarify the international gaps on infection control policies among countries worldwide.
Methods
During April 2-8, 2020, a cross-sectional online survey on surgical practice was distributed to surgeons worldwide through international surgical societies, social media and personal contacts. Main outcome and measures included preventive measures and screening policies of COVID-19 in surgical practice and centers’ experiences of in-hospital COVID-19 infection. Data were analyzed by country’s cumulative deaths number by April 8, 2020 (high risk, >5000; intermediate risk, 100-5000; low risk, <100).
Results
A total of 936 centers in 71 countries responded to the survey (high risk, 330 centers; intermediate risk, 242 centers; low risk, 364 centers). In the majority (71.9%) of the centers, local guidelines recommended preoperative testing based on symptoms or suspicious radiologic findings. Universal testing for every surgical patient was recommended in only 18.4% of the centers. In-hospital COVID-19 infection was reported from 31.5% of the centers, with higher rates in higher risk countries (high risk, 53.6%; intermediate risk, 26.4%; low risk, 14.8%; P < 0.001). Of the 295 centers that experienced in-hospital COVID-19 infection, 122 (41.4%) failed to trace it and 58 (19.7%) reported the infection originating from asymptomatic patients/staff members. Higher risk countries adopted more preventive measures including universal testing, routine testing of hospital staff and use of dedicated personal protective equipment in operation theatres, but there were remarkable discrepancies across the countries.
Conclusions
This large international survey captured the global surgical practice under the COVID-19 pandemic and highlighted the insufficient preoperative screening of COVID-19 in the current surgical practice. More intensive screening programs will be necessary particularly in severely affected countries/institutions.
Study registration
Registered in ClinicalTrials.gov: NCT04344197
The global pandemic of Coronavirus Disease 2019 (COVID-19) was announced by the World Health Organization (WHO) on 11 March, 2020 [1] and as of April 17, 2020, more than 2.2 million cases and more than 140 000 deaths have been reported in 210 countries.[2] The rapid spread of the outbreak has changed the global health care system, including the field of surgery: currently, many hospitals are forced to stop or postpone elective surgical interventions [3-5].
Patients infected by COVID-19 may present without typical symptoms [6,7] such as fever, cough, shortness of breath, gastrointestinal symptoms [8-10] anosmia and ageusia. Such asymptomatic patients play an important role in the disease spread [11-14]. In a surgical setting, asymptomatic COVID-19 patients may potentially expose health care providers to virus-contaminated aerosol through surgical and anesthetic procedures, transmit the disease to other hospitalized patients and trigger in-hospital outbreaks [15-17]. Furthermore, it was reported that COVID-19 patients have worse postoperative outcomes [18-20] with an unexpectedly high morbidity and mortality, reaching 44% Intensive Care Unit (ICU) admission and 20.5% deaths [21], possibly due to the postoperative suppression of cell-mediated immunity [22-24]. Despite these risks for health care workers, other patients, and the COVID-19 patients themselves, there have been no consistent statements on surgical guidelines [25-30] regarding the perioperative screening or management of COVID-19 patients, and we do not have objective global data that describe the current conditions surrounding this issue.
This international survey aimed to clarify the current global situation of surgical practice including COVID-19 screening, preventive measures and in-hospital infection under the COVID-19 pandemic, and to clarify the international/institutional gaps on infection control policies among countries worldwide.
METHODS
Study design
A cross-sectional online survey study on surgical practices was conducted in April, 2020 [31]. The survey questionnaires were designed and developed by the steering committee composed of 5 surgeons (VB, TK, YA, GP, GSS) through international teleconferences and email exchanges. As the COVID-19 pandemic was an unprecedented event, there were no referable previous surveys during this process. A pilot version of the survey was circulated and tested by 47 participants between March 24 and 30, 2020, and the revised final version was approved by all the authors of this study on April 1st, 2020.
The survey consisted of itemized closed questions (single choice, multiple choice, and numeric) as shown in Table 1. Main outcome and measures included centers’ experiences of in-hospital COVID-19 infections, and preventive measures and screening policies of COVID-19 in surgical practices. All questions were mandatory, and the participants were asked to provide profiles and names of the institutions to exclude duplicated registration.
Table 1.
Survey questions
| Basic information |
|---|
| Your country |
| Your city |
| Name of your hospital |
| Your center is? (type of hospital) |
| Have any COVID-19 positive patients been admitted to your hospitals? (both medicine and surgery department, with number of caseloads) |
|
Surgical procedures and protective measures (tables 2-4) |
| To date, which kind of surgical procedures do you still perform at your hospital? |
| How do you perform surgery? |
| When is a surgical patient isolated in your center? |
| Are you doing hospital team-rotations at your center? (e.g.: divide department staff member in two separated groups that works separately on rotation) |
| When do you wear medical masks? |
| Which of the following are easily available at your hospital? |
|
Testing policies and In-hospital COVID-19 infection (tables 5-7) |
| If local guidelines are available at your center, which surgical patients do your local guidelines recommend testing? |
| Do you perform a diagnostic Chest CT scan preoperatively to rule out COVID-19? |
| When are hospital staff members tested at your hospital? |
| Which type of test do you perform? |
| How long does it take to get COVID-19 test results on average at your center? |
| Have you experienced any in-hospital COVID-19 infections in your center? |
| If yes, did you manage to trace the outbreak? |
| Did any of your staff develop symptoms and test positive for COVID-19? |
| If any hospital staff member is tested positive while being asymptomatic, they: |
The survey respondents were surgeons who represented the centers’ surgical departments, and the individual surgeons were responsible for providing data on surgical practice at the centers. The centers in this study included academic hospitals, cancer centers and local public or private hospitals that were equipped with surgical departments. Survey participation was on a voluntary basis. In light of the rapidly changing situation in each country, we conducted the online survey within one week (April 2 to 8, 2020). Google Forms (Google LLC, Menlo Park California, USA) was used to deliver the survey in 13 languages, and the Wenjuanxing platform (Changsha Ranxing Information Technology Co.,LTD, Hunan, China) was used to deliver a Chinese version in China. The survey was globally distributed to surgeons through emails, telephones, social media, and international surgical societies’ social media platforms (European Society of Surgical Oncology, Latin American Society of Surgical Oncology, Russian Society of Colorectal Surgeons and Società Italiana di Chirurgia Colo-Rettale).
The study was approved by the institutional review board of Tor Vergata University of Rome (n.49/20). The study was registered on ClinicalTrials.gov (NCT04344197). Reporting of this study follows the American Association for Public Opinion Research reporting guideline and Checklist for Reporting Results of Internet E-Surveys [32].
Statistical analyses
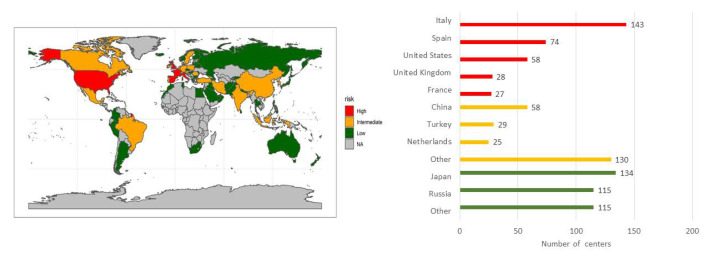
Data were analyzed by country’s risk category. Countries were classified into high (>5000), intermediate (between 100 and 5000) and low (<100) risk groups based on the number of cumulative deaths reported by the WHO on April 8, 2020 (Figure 1). These death thresholds were defined by the fact that the most severely affected countries reached over 5000 deaths, and most countries started lockdown when the deaths exceeded 100 [33]. Data from countries with ≥25 centers were separately analyzed. Data were also analyzed by the centers’ COVID-19 caseloads (>100, 50-100, 10-50, 1-10 and none). Only one representative respondent per center was included in the analyses, and duplicated registration from the same centers was manually excluded based on the provided profiles and names of the institutions. Comparison of the data was performed using the χ2 and Fisher exact tests for categorical variables and the t test for continuous variables. Two-sided P values <0.05 were considered statistically significant. Analyses were performed by a statistician (AP) using R software (R Core Team (2019). R: A language and environment for statistical computing (R Foundation for Statistical Computing, Vienna, Austria).
Figure 1.
Country’s risk category and number of centers. Countries were classified into high (>5000), intermediate (100-5000) and low (<100) risk groups based on the number of cumulative deaths reported by the WHO on April 8, 2020. Other countries in intermediate risk (n = 130): Mexico (24), Portugal (17), Romania (13), Austria (12), Germany, India, Ireland (10), Belgium (8), Brazil, Switzerland (5), Canada, Sweden (4), South Korea (3), Indonesia (2), Denmark, Iran, and Poland (1). Other countries in low risk (n = 115): Ukraina (11), Azerbaijan (9), Pakistan (8), Egypt, Israel (6), Greece, Lithuania, Norway (5), Belarus, Colombia, Lebanon (4), Australia, Czech Republic, Sri Lanka (3), Argentina, Armenia, Bulgaria, Finland, Latvia, Moldova, Puerto Rico, South Africa, Thailand (2), Afghanistan, Hungary, Iceland, Iraq, Israel, Korea, Kyrgyzstan, Morocco, Nepal, New Zealand, North Macedonia, Oman, Palestine, Panama, Perú, Philippines, Saudi Arabia, Serbia, Singapore, Tunisia, United Arab Emirates (1).
RESULTS
Study population
The survey was completed by a total of 1173 surgeons from 936 centers in 71 countries, involving 5 high risk countries (330 centers), 20 intermediate risk countries (242 centers) and 46 low risk countries (364 centers) (Figure 1). Five high risk countries (Italy, Spain, USA, UK and France), 3 intermediate risk countries (China, Turkey, Netherlands) and 2 low risk countries (Japan and Russia) had 25 or more participating centers. There were 201 COVID-19-free, 59 COVID-19-dedicated and 642 COVID-19-mixed hospitals. The Types of centers were 342 academic centers, 155 cancer centers and 435 local public or private centers. Centers’ COVID-19 caseloads were available in 813 centers (86.9%).
Surgical procedures and protective measures
Results of current surgical procedures and protective measures by countries’ risk group, country, and centers’ COVID-19 caseloads are summarized in Table 2, Table 3 and Table 4. Overall, the majority of the centers performed emergency surgery (92.2%) and oncologic elective surgeries (68.4%), whereas non-oncologic elective surgeries were performed in 28.1% of the centers, ranging from 8.5% in high-risk to 45.1% in low-risk countries. Among the high risk countries, centers that continue oncologic elective surgeries varied from 48.3% in the USA to >80% in Italy and France. Centers that avoided laparoscopic surgery were less than 30% across countries in each risk category, except for UK (64.3%) and Turkey (51.7%). The use of dedicated Personal Protective Equipment (PPE) and the use of smoke-aspiration devices during laparoscopic surgery were proportional to the country risk categories and centers’ caseloads. Over 30% of the centers in high and intermediate risk countries organized hospital team rotation, but the proportion per each country varied from 17.5% (Italy) to 69% (Turkey). Overall, 71.8% of the participants reported always wearing a medical mask in the hospital, but the proportion varied across the countries from 0% in the Netherlands, 21.4% in UK to >95% in Italy, France and China. Among PPEs, FFP2/FFP3 masks and eye protections were less available similarly across the countries.
Table 2.
Surgical procedures and protective measures by countries’ risk group
| Overall |
Countries’ risk group |
||||
|---|---|---|---|---|---|
|
High risk |
Int. risk |
Low risk |
P value |
||
|
936 |
330 |
242 |
364 |
||
|
Surgical procedures performed. No. (%):* | |||||
| Emergency |
863 (92.2) |
317 (96.1) |
230 (95.0) |
316 (86.8) |
<0.001 |
| Oncologic elective |
640 (68.4) |
222 (67.3) |
189 (78.1) |
229 (62.9) |
<0.001 |
| Non oncologic elective |
263 (28.1) |
28 (8.5) |
71 (29.3) |
164 (45.1) |
<0.001 |
| Office procedures and one-day surgery |
159 (17.0) |
17 (5.2) |
41 (16.9) |
101 (27.8) |
<0.001 |
|
How do you perform surgery? No. (%):* | |||||
| As usual |
398 (42.5) |
75 (22.7) |
93 (38.4) |
230 (63.2) |
<0.001 |
| Try to avoid laparoscopic cases |
187 (20.0) |
79 (23.9) |
63 (26.0) |
45 (12.4) |
<0.001 |
| With dedicated PPE |
320 (34.2) |
178 (53.9) |
74 (30.6) |
68 (18.7) |
<0.001 |
| If laparoscopic, use smoke aspiration devices |
238 (25.4) |
133 (40.3) |
57 (23.6) |
48 (13.2) |
<0.001 |
|
When is a surgical patient isolated? No. (%) | |||||
| Every patient is isolated until proved COVID-19 negative |
101 (10.8) |
62 (18.8) |
27 (11.2) |
12 (3.3) |
<0.001 |
| If symptomatic/suspected/COVID-19 positive |
722 (77.1) |
258 (78.2) |
202 (83.5) |
262 (72.0) |
|
| Others |
113 (12.1) |
10 (3.0) |
13 (5.4) |
90 (24.7) |
|
|
Are you doing hospital team-rotations? No. (%): | |||||
| Yes |
268 (28.6) |
105 (31.8) |
96 (39.7) |
67 (18.4) |
<0.001 |
| No |
668 (71.4) |
225 (68.2) |
146 (60.3) |
297 (81.6) |
|
|
When do you wear medical masks? No. (%):* | |||||
| When visiting symptomatic/suspected/COVID-19 positive patients |
141 (15.1) |
40 (12.1) |
48 (19.8) |
53 (14.6) |
0.04 |
| When visiting every patient |
124 (13.2) |
34 (10.3) |
29 (12.0) |
61 (16.8) |
0.04 |
| Always in hospital |
677 (71.8) |
265 (80.3) |
159 (65.7) |
253 (69.5) |
<0.001 |
|
Which are easily available: No. (%):* | |||||
| Gloves |
880 (94.0) |
309 (93.6) |
227 (93.8) |
344 (94.5) |
0.88 |
| Gowns |
573 (61.3) |
186 (56.4) |
130 (53.9) |
257 (70.6) |
<0.001 |
| Eye protection |
405 (43.3) |
121 (36.7) |
113 (46.7) |
171 (47.0) |
0.01 |
| Medical masks |
736 (78.6) |
259 (78.5) |
196 (81.0) |
281 (77.2) |
0.54 |
| FFP2/FFP3 or respirator N95 |
231 (24.7) |
83 (25.2) |
71 (29.3) |
77 (21.2) |
0.07 |
| Hand sanitizer | 791 (84.5) | 263 (79.7) | 216 (89.3) | 312 (85.7) | 0.005 |
Int – intermediate, PPE – personal protective equipment
*Percentages do not add up to 100 because of the multiple choice questions.
Table 3.
Surgical procedures and protective measures by country (countries with ≥25 centers)
| Overall |
Countries |
|||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Italy-H |
Spain-H |
USA-H |
UK-H |
France-H |
China-I |
Turkey-I |
Netherlands-I |
Japan-L |
Russia-L |
|||||||||||||||
| 936 |
143 |
74 |
58 |
28 |
27 |
58 |
29 |
25 |
134 |
115 |
||||||||||||||
|
Surgical procedures performed. No. (%):* | ||||||||||||||||||||||||
| Emergency |
863 (92.2) |
132 (92.3) |
73 (98.6) |
58 (100.0) |
28 (100.0) |
26 (96.3) |
54 (93.1) |
28 (96.6) |
25 (100.0) |
120 (89.6) |
84 (73.0) |
|||||||||||||
| Oncologic elective |
640 (68.4) |
115 (80.4) |
42 (56.8) |
28 (48.3) |
15 (53.6) |
22 (81.5) |
55 (94.8) |
24 (82.8) |
24 (96.0) |
131 (97.8) |
35 (30.4) |
|||||||||||||
| Non oncologic elective |
263 (28.1) |
16 (11.2) |
0 (0.0) |
7 (12.1) |
1 (3.6) |
4 (14.8) |
42 (72.4) |
4 (13.8) |
3 (12.0) |
111 (82.8) |
45 (39.1) |
|||||||||||||
| Office procedures and one-day surgery |
159 (17.0) |
7 (4.9) |
0 (0.0) |
9 (15.5) |
1 (3.6) |
0 (0.0) |
24 (41.4) |
1 (3.4) |
1 (4.0) |
68 (51.1) |
24 (20.9) |
|||||||||||||
|
How do you perform surgery? No. (%):* | ||||||||||||||||||||||||
| As usual |
398 (42.5) |
36 (25.2) |
9 (12.2) |
19 (32.8) |
2 (7.1) |
9 (33.3) |
36 (62.1) |
5 (17.2) |
12 (48.0) |
119 (88.8) |
67 (58.3) |
|||||||||||||
| Try to avoid laparoscopic cases |
187 (20.0) |
30 (21.0) |
21 (28.4) |
6 (10.3) |
18 (64.3) |
4 (14.8) |
7 (12.1) |
15 (51.7) |
1 (4.0) |
3 (2.2) |
7 (6.1) |
|||||||||||||
| With dedicated PPE |
320 (34.2) |
77 (53.8) |
47 (63.5) |
24 (41.4) |
20 (71.4) |
10 (37.0) |
14 (24.1) |
13 (44.8) |
4 (16.0) |
1 (0.7) |
34 (29.6) |
|||||||||||||
| If laparoscopic, use smoke aspiration devices |
238 (25.4) |
48 (33.6) |
46 (62.2) |
18 (31.0) |
7 (25.0) |
14 (51.9) |
14 (24.1) |
2 (6.9) |
13 (52.0) |
30 (22.4) |
0 (0.0) |
|||||||||||||
|
When is a surgical patient isolated? No. (%): | ||||||||||||||||||||||||
| Every patient is isolated until proved COVID-19 negative |
101 (10.8) |
35 (24.5) |
14 (18.9) |
8 (13.8) |
1 (3.6) |
4 (14.8) |
9 (15.5) |
2 (6.9) |
0 (0.0) |
2 (1.5) |
1 (0.9) |
|||||||||||||
| If symptomatic/ suspected/ COVID-19 positive |
722 (77.1) |
102 (71.3) |
56 (75.7) |
50 (86.2) |
26 (92.9) |
23 (85.2) |
45 (77.6) |
26 (89.7) |
25 (100.0) |
116 (86.6) |
57 (49.6) |
|||||||||||||
| Others |
113 (12.1) |
6 (4.2) |
4 (5.4) |
0 (0.0) |
1 (3.6) |
0 (0.0) |
4 (6.9) |
1 (3.4) |
0 (0.0) |
16 (11.9) |
57 (49.6) |
|||||||||||||
|
Are you doing hospital team-rotations? No. (%): | ||||||||||||||||||||||||
| Yes |
268 (28.6) |
25 (17.5) |
39 (52.7) |
22 (37.9) |
13 (46.4) |
6 (22.2) |
18 (31.0) |
20 (69.0) |
8 (32.0) |
5 (3.7) |
11 (9.6) |
|||||||||||||
| No |
668 (71.4) |
118 (82.5) |
35 (47.3) |
36 (62.1) |
15 (53.6) |
21 (77.8) |
40 (69.0) |
9 (31.0) |
17 (68.0) |
129 (96.3) |
104 (90.4) |
|||||||||||||
|
When do you wear medical masks? No. (%):* | ||||||||||||||||||||||||
| When visiting symptomatic/ suspected/ COVID-19 positive patients |
141 (15.1) |
0 (0.0) |
12 (16.2) |
13 (22.4) |
14 (50.0) |
1 (3.7) |
1 (1.7) |
4 (13.8) |
18 (72.0) |
13 (9.7) |
10 (8.7) |
|||||||||||||
| When visiting every patient |
124 (13.2) |
4 (2.8) |
11 (14.9) |
8 (13.8) |
11 (39.3) |
0 (0.0) |
1 (1.7) |
6 (20.7) |
3 (12.0) |
23 (17.2) |
22 (19.1) |
|||||||||||||
| Always in hospital |
677 (71.8) |
136 (95.1) |
60 (81.1) |
37 (63.8) |
6 (21.4) |
26 (96.3) |
56 (96.6) |
19 (65.5) |
0 (0.0) |
104 (77.6) |
77 (67.0) |
|||||||||||||
|
Which are easily available: No. (%):* | ||||||||||||||||||||||||
| Gloves |
880 (94.0) |
136 (95.1) |
71 (95.9) |
50 (86.2) |
28 (100.0) |
24 (88.9) |
52 (89.7) |
29 (100.0) |
25 (100.0) |
125 (93.3) |
111 (96.5) |
|||||||||||||
| Gowns |
573 (61.3) |
65 (45.5) |
44 (59.5) |
41 (70.7) |
23 (82.1) |
13 (48.1) |
19 (32.8) |
15 (51.7) |
23 (95.8) |
105 (78.4) |
77 (67.0) |
|||||||||||||
| Eye protection |
405 (43.3) |
48 (33.6) |
22 (29.7) |
35 (60.3) |
11 (39.3) |
5 (18.5) |
27 (46.6) |
12 (41.4) |
23 (92.0) |
77 (57.5) |
45 (39.1) |
|||||||||||||
| Medical masks |
736 (78.6) |
118 (82.5) |
47 (63.5) |
45 (77.6) |
23 (82.1) |
26 (96.3) |
51 (87.9) |
24 (82.8) |
25 (100.0) |
95 (70.9) |
97 (84.3) |
|||||||||||||
| FFP2/FFP3 or respirator N95 |
231 (24.7) |
30 (21.0) |
19 (25.7) |
22 (37.9) |
9 (32.1) |
3 (11.1) |
12 (20.7) |
9 (31.0) |
15 (60.0) |
38 (28.4) |
8 (7.0) |
|||||||||||||
| Hand sanitizer |
791 (84.5) | 109 (76.2) |
66 (89.2) |
47 (81.0) |
20 (71.4) |
21 (77.8) |
55 (94.8) |
25 (86.2) |
25 (100.0) |
107 (79.9) |
105 (91.3) |
|||||||||||||
Country-H – High risk country, Country-I – Intermediate risk country, Country-L – Low risk country, PPE – personal protective equipment
*Percentages do not add up to 100 because of the multiple choice questions.
Table 4.
Surgical procedures and protective measures by centers’ COVID-19 caseloads
| Overall |
Centers’ COVID-19 caseloads |
||||||
|---|---|---|---|---|---|---|---|
|
>100 |
50-100 |
10-50 |
1-10 |
None |
P value |
||
|
813 |
32 |
177 |
151 |
222 |
231 |
||
|
Surgical procedures performed. No. (%):* | |||||||
| Emergency |
746 (91.8) |
30 (93.8) |
173 (97.7) |
147 (97.4) |
205 (92.3) |
191 (82.7) |
<0.001 |
| Oncologic elective |
575 (70.7) |
21 (65.6) |
139 (78.5) |
116 (76.8) |
160 (72.1) |
139 (60.2) |
<0.001 |
| Non oncologic elective |
246 (30.3) |
1 (3.1) |
18 (10.2) |
33 (21.9) |
84 (37.8) |
110 (47.6) |
<0.001 |
| Office procedures and one-day surgery |
149 (18.3) |
2 (6.2) |
10 (5.6) |
17 (11.3) |
54 (24.4) |
66 (28.6) |
<0.001 |
|
How do you perform surgery? No. (%):* | |||||||
| As usual |
367 (45.1) |
6 (18.8) |
44 (24.9) |
65 (43.0) |
111 (50.0) |
141 (61.0) |
<0.001 |
| Try to avoid laparoscopic cases |
162 (19.9) |
10 (31.2) |
40 (22.6) |
37 (24.5) |
46 (20.7) |
29 (12.6) |
0.01 |
| With dedicated PPE |
273 (33.6) |
23 (71.9) |
97 (54.8) |
55 (36.4) |
55 (24.8) |
43 (18.6) |
<0.001 |
| If laparoscopic, use smoke aspiration devices |
212 (26.1) |
17 (53.1) |
78 (44.1) |
47 (31.1) |
41 (18.5) |
29 (12.6) |
<0.001 |
|
When is a surgical patient isolated? No. (%): | |||||||
| Every patient is isolated until proved COVID-19 negative |
90 (11.1) |
5 (15.6) |
41 (23.2) |
23 (15.2) |
13 (5.9) |
8 (3.5) |
<0.001 |
| If symptomatic/ suspected/ COVID-19 positive |
622 (76.5) |
26 (81.2) |
133 (75.1) |
126 (83.4) |
192 (86.5) |
150 (64.9) |
|
| Others |
101 (12.4) |
1 (3.1) |
3 (1.7) |
2 (1.3) |
17 (7.7) |
73 (31.6) |
|
|
Are you doing hospital team-rotations? No. (%): | |||||||
| Yes |
234 (28.8) |
10 (31.2) |
76 (42.9) |
52 (34.4) |
53 (23.9) |
43 (18.6) |
<0.001 |
| No |
579 (71.2) |
22 (68.8) |
101 (57.1) |
99 (65.6) |
169 (76.1) |
188 (81.4) |
|
|
When do you wear medical masks? No. (%)* | |||||||
| When visiting symptomatic/ suspected/ COVID-19 positive patients |
125 (15.4) |
2 (6.2) |
33 (18.6) |
31 (20.5) |
31 (14.0) |
28 (12.1) |
0.07 |
| When visiting every patient |
109 (13.4) |
6 (18.8) |
17 (9.6) |
20 (13.2) |
28 (12.6) |
38 (16.5) |
0.29 |
| Always in hospital |
590 (72.6) |
26 (81.2) |
128 (72.3) |
106 (70.2) |
165 (74.3) |
165 (71.4) |
0.71 |
|
Which are easily available: No. (%):* | |||||||
| Gloves |
764 (94.0) |
30 (93.8) |
170 (96.0) |
141 (93.4) |
207 (93.2) |
216 (93.5) |
0.78 |
| Gowns |
499 (61.4) |
22 (68.8) |
107 (60.8) |
89 (58.9) |
138 (62.2) |
143 (61.9) |
0.86 |
| Eye protection |
363 (44.6) |
13 (40.6) |
83 (46.9) |
60 (39.7) |
105 (47.3) |
102 (44.2) |
0.61 |
| Medical masks |
640 (78.7) |
25 (78.1) |
146 (82.5) |
118 (78.1) |
171 (77.0) |
180 (77.9) |
0.74 |
| FFP2/FFP3 or respirator N95 |
201 (24.7) |
11 (34.4) |
55 (31.1) |
45 (29.8) |
48 (21.6) |
42 (18.2) |
0.007 |
| Hand sanitizer | 707 (87.0) | 24 (75.0) | 154 (87.0) | 133 (88.1) | 199 (89.6) | 197 (85.3) | 0.19 |
PPE – personal protective equipment
*Percentages do not add up to 100 because of the multiple choice questions. Data were analyzed in centers that provided COVID-19 caseloads (N = 813).
Testing policies
Testing policies by countries’ risk group, country, and centers’ COVID-19 caseloads are summarized in in Table 5, Table 6 and Table 7. The majority (71.9%) of local guidelines recommended preoperative testing based on symptoms or suspicious radiologic findings. Local guidelines recommended testing every surgical patient in less than 20% of the centers. Routine screening by chest-Computer Tomography (CT) scan was used in only 22.8% of the overall centers, and the rates varied among the countries from 87.9% in China to 7.3% in the USA. Testing policies for staff members were also based on symptoms or risk contact in majority of the centers. Polimerase Chain Reaction (PCR) test without antibody testing was used in most of the countries, whereas nearly 30% of surgeons did not know which type of laboratory testing was used at their centers. The wait time to get test results was more than 1 day in 34.7% of the centers.
Table 5.
Testing policies and in-hospital COVID-19 infection by countries’ risk group
| Overall |
Countries’ risk group |
||||
|---|---|---|---|---|---|
|
High risk |
Int. risk |
Low risk |
P value |
||
| 936 |
330 |
242 |
364 |
||
|
Testing policies recommended by the local guidelines. No. (%):* | |||||
| Everyone |
172 (18.4) |
84 (25.5) |
54 (22.3) |
34 (9.3) |
<0.001 |
| All oncologic patients |
56 (6.0) |
32 (9.7) |
13 (5.4) |
11 (3.0) |
0.001 |
| All emergency patients |
101 (10.8) |
40 (12.1) |
27 (11.2) |
34 (9.3) |
0.49 |
| Symptomatic or suspicious radiological features |
673 (71.9) |
222 (67.3) |
164 (67.8) |
287 (78.8) |
0.04 |
|
Preoperative chest CT performed. No. (%): | |||||
| Yes |
213 (22.8) |
81 (24.5) |
88 (36.4) |
44 (12.1) |
<0.001 |
| No |
394 (42.1) |
144 (43.6) |
88 (36.4) |
162 (44.5) |
|
| Only if symptomatic |
320 (34.2) |
100 (30.3) |
66 (27.3) |
154 (42.3) |
|
| Others |
9 (1.0) |
5 (1.5) |
0 (0.0) |
4 (1.1) |
|
|
Testing policies on staff members. No. (%):* | |||||
| Everyone is routinely tested every two/four weeks |
23 (2.5) |
14 (4.2) |
2 (0.8) |
7 (1.9) |
0.02 |
| Mandatory if risk contact/symptoms present |
570 (60.9) |
186 (56.4) |
157 (64.9) |
227 (62.4) |
0.09 |
| On request if risk contact/symptoms present |
435 (46.5) |
174 (52.7) |
122 (50.4) |
139 (38.2) |
<0.001 |
| No test |
46 (4.9) |
14 (4.2) |
8 (3.3) |
24 (6.6) |
0.15 |
|
Testing type. No. (%): | |||||
| 1 PCR swab |
392 (41.9) |
186 (56.4) |
81 (33.5) |
125 (34.3) |
<0.001 |
| 2 PCR swabs |
216 (23.1) |
75 (22.7) |
67 (27.7) |
74 (20.3) |
|
| PCR + antibodies |
71 (7.6) |
16 (4.8) |
36 (14.9) |
19 (5.2) |
|
| I don't know |
257 (27.5) |
53 (16.1) |
58 (24.0) |
146 (40.1) |
|
|
Wait time for test results. No. (%): | |||||
| 1-6 h |
169 (18.1) |
63 (19.1) |
46 (19.0) |
60 (16.5) |
<0.001 |
| 6 h-1 d |
305 (32.6) |
126 (38.2) |
82 (33.9) |
97 (26.6) |
|
| More than 1 d |
325 (34.7) |
126 (38.2) |
84 (34.7) |
115 (31.6) |
|
| I don't know |
137 (14.6) |
15 (4.5) |
30 (12.4) |
92 (25.3) |
|
|
Experienced in-hospital COVID-19 infection. No. (%): | |||||
| Yes |
295 (31.5) |
177 (53.6) |
64 (26.4) |
54 (14.8) |
<0.001 |
| No/I don’t know |
641 (68.5) |
153 (46.4) |
178 (73.6) |
310 (85.2) |
|
|
If yes, source of the outbreak traced? No. (%):† | |||||
| We had hospital outbreak but could not trace them |
122 (41.4) |
92 (52.0) |
18 (28.1) |
12 (22.2) |
<.001 |
| Yes, started from a symptomatic staff/patient |
89 (30.2) |
42 (23.7) |
27 (42.2) |
20 (37.0) |
|
| Yes, started from an asymptomatic staff/patient |
58 (19.7) |
31 (17.5) |
14 (21.9) |
13 (24.1) |
|
| Others |
26 (8.8) |
12 (6.8) |
5 (7.8) |
9 (16.7) |
|
|
Staff testing positive with symptoms. No. (%): | |||||
| Yes |
296 (31.6) |
162 (49.1) |
89 (36.8) |
45 (12.4) |
<.001 |
| No/I don’t know |
640 (68.4) |
168 (50.9) |
153 (63.2) |
319 (87.6) |
|
|
Policies for asymptomatic infected staff. No. (%):* | |||||
| Placed in mandatory quarantine |
725 (77.5) |
249 (75.5) |
195 (80.6) |
281 (77.2) |
.35 |
| Placed in voluntary quarantine |
125 (13.4) |
40 (12.1) |
30 (12.4) |
55 (15.1) |
.45 |
| Continue working | 41 (4.4) | 25 (7.6) | 7 (2.9) | 9 (2.5) | .002 |
Int – intermediate, CT – computed tomography, PCR – polymerase chain reaction
*Percentages do not add up to 100 because of the multiple choice questions.
†The sum was the number of the respondents who answered “yes” in the question “Experienced in-hospital COVID-19 infection”.
Table 6.
Testing policies and in-hospital COVID-19 infection by country (countries with ≥25 centers)
| Overall |
Countries |
||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Italy-H |
Spain-H |
USA-H |
UK-H |
France-H |
China-I |
Turkey-I |
Netherlands-I |
Japan-L |
Russia-L |
||||||||||||||
| 936 |
143 |
74 |
58 |
28 |
27 |
58 |
29 |
25 |
134 |
115 |
|||||||||||||
|
Testing policies recommended by the local guidelines. No. (%):* | |||||||||||||||||||||||
| Everyone |
172 (18.4) |
45 (31.5) |
21 (28.4) |
7 (12.1) |
5 (17.9) |
6 (22.2) |
11 (19.0) |
5 (17.2) |
10 (40.0) |
10 (7.5) |
6 (5.2) |
||||||||||||
| All oncologic patients |
56 (6.0) |
17 (11.9) |
8 (10.8) |
1 (1.7) |
4 (14.3) |
2 (7.4) |
0 (0.0) |
4 (13.8) |
1 (4.0) |
4 (3.0) |
2 (1.7) |
||||||||||||
| All emergency patients |
101 (10.8) |
20 (14.0) |
10 (13.5) |
2 (3.4) |
4 (14.3) |
4 (14.8) |
5 (8.6) |
5 (17.2) |
3 (12.0) |
7 (5.2) |
7 (6.1) |
||||||||||||
| Symptomatic or suspicious radiological features |
673 (71.9) |
89 (62.2) |
47 (63.5) |
43 (74.1) |
21 (75.0) |
22 (81.5) |
46 (79.3) |
20 (69.0) |
13 (52.0) |
115 (85.8) |
89 (77.4) |
||||||||||||
|
Preoperative chest CT performed. No. (%): | |||||||||||||||||||||||
| Yes |
213 (22.8) |
35 (24.5) |
20 (27.0) |
4 (6.9) |
14 (50.0) |
8 (29.6) |
51 (87.9) |
13 (44.8) |
11 (44.0) |
22 (16.4) |
6 (5.2) |
||||||||||||
| No |
394 (42.1) |
51 (35.7) |
41 (55.4) |
37 (63.8) |
8 (28.6) |
7 (25.9) |
2 (3.4) |
3 (10.3) |
5 (20.0) |
40 (29.9) |
68 (59.1) |
||||||||||||
| Only if symptomatic |
320 (34.2) |
56 (39.2) |
12 (16.2) |
14 (24.1) |
6 (21.4) |
12 (44.4) |
5 (8.6) |
13 (44.8) |
9 (36.0) |
71 (53.0) |
38 (33.0) |
||||||||||||
| Others |
9 (1.0) |
1 (0.7) |
1 (1.4) |
3 (5.2) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
0 (0) |
1 (0.7) |
3 (2.6) |
||||||||||||
|
Testing policies on staff members. No. (%):* | |||||||||||||||||||||||
| Everyone is routinely tested every two/four weeks |
23 (2.5) |
13 (9.1) |
1 (1.4) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (0.7) |
4 (3.5) |
||||||||||||
| Mandatory if risk contact/symptoms |
570 (60.9) |
109 (76.2) |
35 (47.3) |
24 (41.4) |
5 (17.9) |
13 (48.1) |
29 (50.0) |
24 (82.8) |
19 (76.0) |
81 (60.4) |
74 (64.3) |
||||||||||||
| On request if risk contact/symptoms |
435 (46.5) |
51 (35.7) |
49 (66.2) |
38 (65.5) |
17 (60.7) |
19 (70.4) |
37 (63.8) |
12 (41.4) |
6 (24.0) |
64 (47.8) |
16 (13.9) |
||||||||||||
| No test |
46 (4.9) |
1 (0.7) |
0 (0.0) |
7 (12.1) |
5 (17.9) |
1 (3.7) |
1 (1.7) |
0 (0.0) |
1 (4.0) |
0 (0.0) |
19 (16.5) |
||||||||||||
|
Testing type. No. (%): | |||||||||||||||||||||||
| 1 PCR swab |
392 (41.9) |
74 (51.7) |
47 (63.5) |
33 (56.9) |
14 (50.0) |
18 (66.7) |
6 (10.3) |
7 (24.1) |
12 (48.0) |
53 (39.6) |
23 (20.0) |
||||||||||||
| 2 PCR swabs |
216 (23.1) |
41 (28.7) |
15 (20.3) |
6 (10.3) |
8 (28.6) |
5 (18.5) |
17 (29.3) |
11 (37.9) |
9 (36.0) |
12 (9.0) |
32 (27.8) |
||||||||||||
| PCR + antibodies |
71 (7.6) |
13 (9.1) |
2 (2.7) |
0 (0.0) |
0 (0.0) |
1 (3.7) |
23 (39.7) |
4 (13.8) |
0 (0.0) |
4 (3.0) |
9 (7.8) |
||||||||||||
| I don't know |
257 (27.5) |
15 (10.5) |
10 (13.5) |
19 (32.8) |
6 (21.4) |
3 (11.1) |
12 (20.7) |
7 (24.1) |
4 (16.0) |
65 (48.4) |
51 (44.3) |
||||||||||||
|
Wait time for test results. No. (%): | |||||||||||||||||||||||
| 1-6 h |
169 (18.1) |
31 (21.7) |
20 (27.0) |
2 (3.4) |
3 (10.7) |
7 (25.9) |
17 (29.3) |
2 (6.9) |
11 (44.0) |
18 (13.4) |
9 (7.8) |
||||||||||||
| 6 h-1 d |
305 (32.6) |
71 (49.7) |
30 (40.5) |
6 (10.3) |
7 (25.0) |
12 (44.4) |
16 (27.6) |
4 (13.8) |
13 (52.0) |
46 (34.3) |
13 (11.3) |
||||||||||||
| More than 1 d |
325 (34.7) |
35 (24.5) |
22 (29.7) |
46 (79.3) |
15 (53.6) |
8 (29.6) |
8 (13.8) |
18 (62.1) |
1 (4.0) |
35 (26.1) |
48 (41.7) |
||||||||||||
| I don't know |
137 (14.6) |
6 (4.2) |
2 (2.7) |
4 (6.9) |
3 (10.7) |
0 (0.0) |
17 (29.3) |
5 (17.2) |
0 (0.0) |
35 (26.1) |
45 (39.1) |
||||||||||||
|
Experienced in-hospital COVID-19 infection. No. (%): | |||||||||||||||||||||||
| Yes |
295 (31.5) |
93 (65.0) |
47 (63.5) |
11 (19.0) |
13 (46.4) |
13 (48.1) |
2 (3.4) |
12 (41.4) |
14 (56.0) |
11 (8.2) |
20 (17.4) |
||||||||||||
| No/I don’t know |
641 (68.5) |
50 (35.0) |
27 (36.5) |
47 (81.0) |
15 (53.6) |
14 (51.9) |
56 (96.6) |
17 (58.6) |
11 (44.0) |
123 (91.8) |
95 (82.6) |
||||||||||||
|
If yes, source of the outbreak traced? No. (%):† | |||||||||||||||||||||||
| We had hospital outbreak but could not trace them |
122 (41.4) |
48 (51.6) |
27 (57.4) |
2 (18.2) |
7 (53.8) |
8 (61.5) |
1 (50.0) |
0 (0.0) |
5 (35.7) |
2 (18.2) |
8 (40.0) |
||||||||||||
| Yes, started from a symptomatic staff member/patient |
89 (30.2) |
21 (22.6) |
9 (19.1) |
5 (45.5) |
3 (23.1) |
4 (30.8) |
1 (50.0) |
8 (66.7) |
6 (42.9) |
1 (9.1) |
8 (40.0) |
||||||||||||
| Yes, started from an asymptomatic staff member/patient |
58 (19.7) |
22 (23.7) |
7 (14.9) |
0 (0.0) |
1 (7.7) |
1 (7.7) |
0 (0.0) |
4 (33.3) |
2 (14.3) |
0 (0.0) |
4 (20.0) |
||||||||||||
| Others |
26 (8.8) |
2 (2.2) |
4 (8.5) |
4 (36.4) |
2 (15.4) |
0 (0.0) |
0 (0.0) |
0 (0) |
1 (7.1) |
8 (72.7) |
0 (0) |
||||||||||||
|
Staff testing positive with symptoms. No. (%): | |||||||||||||||||||||||
| Yes |
296 (31.6) |
62 (43.4) |
41 (55.4) |
25 (43.1) |
17 (60.7) |
17 (63.0) |
6 (10.3) |
15 (51.7) |
18 (72.0) |
9 (6.7) |
9 (7.8) |
||||||||||||
| No/I don’t know |
640 (68.4) |
81 (56.6) |
33 (44.6) |
33 (56.9) |
11 (39.3) |
10 (37.0) |
52 (89.7) |
14 (48.3) |
7 (28.0) |
125 (93.3) |
106 (92.2) |
||||||||||||
|
Policies for asymptomatic infected staff. No. (%):* | |||||||||||||||||||||||
| Placed in mandatory quarantine |
725 (77.5) |
117 (81.8) |
62 (83.8) |
35 (60.3) |
20 (71.4) |
15 (55.6) |
47 (81.0) |
21 (72.4) |
19 (76.0) |
111 (82.8) |
68 (59.1) |
||||||||||||
| Placed in voluntary quarantine |
125 (13.4) |
15 (10.5) |
3 (4.1) |
9 (15.5) |
6 (21.4) |
7 (25.9) |
10 (17.2) |
5 (17.2) |
3 (12.0) |
32 (23.9) |
16 (13.9) |
||||||||||||
| Continue working |
41 (4.4) | 7 (4.9) |
2 (2.7) |
7 (12.1) |
2 (7.1) |
7 (25.9) |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (0.7) |
6 (5.2) |
||||||||||||
Country-H - High risk country, Country-I - Intermediate risk country, Country-L - Low risk country, CT - computed tomography, PCR - polymerase chain reaction
*Percentages do not add up to 100 because of the multiple choice questions.
†The sum was the number of the respondents who answered “yes” in the question “Experienced in-hospital COVID-19 infection.”
Table 7.
Testing policies and in-hospital COVID-19 infection by centers’ COVID-19 caseloads
| Overall |
Centers’ COVID-19 caseloads |
||||||
|---|---|---|---|---|---|---|---|
|
>100 |
50-100 |
10-50 |
1-10 |
None |
P value |
||
| 813 |
32 |
177 |
151 |
222 |
231 |
||
|
Testing policies recommended by the local guidelines. No. (%)* | |||||||
| Everyone |
155 (19.1) |
22 (68.8) |
52 (29.4) |
27 (17.9) |
28 (12.6) |
26 (11.3) |
<0.001 |
| All oncologic patients |
49 (6.0) |
3 (9.4) |
18 (10.2) |
13 (8.6) |
5 (2.3) |
10 (4.3) |
0.006 |
| All emergency patients |
88 (10.8) |
4 (12.5) |
22 (12.4) |
23 (15.2) |
20 (9.0) |
19 (8.2) |
0.20 |
| Symptomatic or suspicious radiological features |
580 (71.3) |
6 (18.8) |
108 (61.0) |
115 (76.2) |
177 (79.7) |
174 (75.3) |
<0.001 |
|
Preoperative chest CT performed. No. (%) | |||||||
| Yes |
184 (22.6) |
13 (40.6) |
44 (24.9) |
41 (27.2) |
44 (19.8) |
42 (18.2) |
0.14 |
| No |
339 (41.7) |
10 (31.2) |
68 (38.4) |
64 (42.4) |
94 (42.3) |
103 (44.6) |
|
| Only if symptomatic |
282 (34.7) |
9 (28.1) |
64 (36.2) |
46 (30.5) |
81 (36.5) |
82 (35.5) |
|
| Others |
8 (1.0) |
0 (0) |
1 (0.6) |
0 (0) |
3 (1.4) |
4 (1.7) |
|
|
Testing policies on staff members. No. (%):* | |||||||
| Everyone is routinely tested every two/four weeks |
23 (2.8) |
4 (12.5) |
7 (4.0) |
3 (2.0) |
5 (2.3) |
4 (1.7) |
0.01 |
| Mandatory if risk contact/symptoms |
514 (63.2) |
20 (62.5) |
119 (67.2) |
100 (66.2) |
122 (55.0) |
153 (66.2) |
0.06 |
| On request if risk contact/symptoms |
381 (46.9) |
12 (37.5) |
92 (52.0) |
87 (57.6) |
115 (51.8) |
75 (32.5) |
<0.001 |
| No test |
34 (4.2) |
1 (3.1) |
5 (2.8) |
3 (2.0) |
10 (4.5) |
15 (6.5) |
0.21 |
|
Testing type. No. (%): | |||||||
| 1 PCR swab |
338 (41.6) |
24 (75.0) |
95 (53.7) |
64 (42.4) |
89 (40.1) |
66 (28.6) |
<0.001 |
| 2 PCR swabs |
189 (23.2) |
6 (18.8) |
48 (27.1) |
38 (25.2) |
45 (20.3) |
52 (22.5) |
|
| PCR + antibodies |
62 (7.6) |
1 (3.1) |
8 (4.5) |
12 (7.9) |
18 (8.1) |
23 (10.0) |
|
| I don't know |
224 (27.6) |
1 (3.1) |
26 (14.7) |
37 (24.5) |
70 (31.5) |
90 (39.0) |
|
|
Wait time for test results. No. (%) | |||||||
| 1-6 h |
148 (18.2) |
10 (31.2) |
39 (22.0) |
35 (23.2) |
33 (14.9) |
31 (13.4) |
<0.001 |
| 6 h-1 d |
265 (32.6) |
18 (56.2) |
79 (44.6) |
47 (31.1) |
73 (32.9) |
48 (20.8) |
|
| More than 1 d |
282 (34.7) |
4 (12.5) |
58 (32.8) |
58 (38.4) |
91 (41.0) |
71 (30.7) |
|
| I don't know |
118 (14.5) |
0 (0.0) |
1 (0.6) |
11 (7.3) |
25 (11.3) |
81 (35.1) |
|
|
Experienced in-hospital COVID-19 infection. No. (%): | |||||||
| Yes |
246 (30.3) |
27 (84.4) |
100 (56.5) |
52 (34.4) |
52 (23.4) |
15 (6.5) |
<0.001 |
| No/I don’t know |
567 (69.7) |
5 (15.6) |
77 (43.5) |
99 (65.6) |
170 (76.6) |
216 (93.5) |
|
|
If yes, source of the outbreak traced? No. (%):† | |||||||
| We had hospital outbreak but could not trace them |
94 (38.2) |
21 (77.8) |
43 (43.0) |
11 (21.2) |
12 (23.1) |
7 (46.7) |
<0.001 |
| Yes, started from a symptomatic staff member/patient |
78 (31.7) |
3 (11.1) |
30 (30.0) |
20 (38.5) |
21 (40.4) |
4 (26.7) |
|
| Yes, started from an asymptomatic staff member/patient |
53 (21.5) |
3 (11.1) |
22 (22.0) |
14 (26.9) |
11 (21.2) |
3 (20.0) |
|
| Others |
21 (8.5) |
0 (0) |
5 (5.0) |
7 (13.5) |
8 (15.4) |
1 (6.6) |
|
|
Staff testing positive with symptoms. No. (%): | |||||||
| Yes |
245 (30.1) |
21 (65.6) |
95 (53.7) |
68 (45.0) |
52 (23.4) |
9 (3.9) |
<0.001 |
| No/I don’t know |
568 (69.9) |
11 (34.4) |
82 (46.3) |
83 (55.0) |
170 (76.6) |
222 (96.1) |
|
|
Policies for asymptomatic infected staff. No. (%):* | |||||||
| Placed in mandatory quarantine |
640 (78.7) |
27 (84.4) |
142 (80.2) |
113 (74.8) |
187 (84.2) |
171 (74.0) |
0.05 |
| Placed in voluntary quarantine |
111 (13.7) |
2 (6.2) |
18 (10.2) |
24 (15.9) |
36 (16.2) |
31 (13.4) |
0.27 |
| Continue working | 31 (3.8) | 0 (0.0) | 11 (6.2) | 10 (6.6) | 2 (0.9) | 8 (3.5) | 0.01 |
CT – computed tomography, PCR – polymerase chain reaction
*Percentages do not add up to 100 because of the multiple choice questions.
Data were analyzed in centers that provided COVID-19 caseloads (N = 813)
†The sum was the number of the respondents who answered “yes” in the question “Experienced in-hospital COVID-19 infection”.
In-hospital COVID-19 infection
In-hospital COVID-19 infection by countries’ risk group, country, and centers’ COVID-19 caseloads are summarized in Table 5, Table 6 and Table 7. Overall, in-hospital COVID-19 infection was reported in 31.5% of the overall centers, and the rate was highest in the high risk countries (53.6%), but some intermediate risk countries (Netherland, Turkey) also reported relatively high rates which were comparable to high risk countries. Out of 295 centers that experienced in-hospital COVID-19 infection, 122 (41.4%) failed to trace it, and 58 (19.7%) reported the infection originating from asymptomatic patients/staff members. When analyzed by institutional caseload of COVID-19 patients, centers that had treated high number of COVID-19 patients reported high rates of in-hospital COVID-19 infection and staff member infection.
DISCUSSION
In this large international survey involving 936 centers from 71 countries, we revealed the current global situation of surgical practice including COVID-19 screening, preventive measures and in-hospital infection under the COVID-19 pandemic in early April 2020. To our knowledge, this is one of the largest international survey studies on COVID-19 in the field of surgery. The survey revealed two major findings. First, significant rates of centers had experienced in-hospital COVID-19 infection (31.5%) worldwide, and the majority of these centers failed to trace it or reported the infection originating from asymptomatic patients/staff members. The rates of in-hospital COVID-19 infection reached 53.6% in high risk counties and 84.4% in centers with >100 COVID-19 case load. Second, there were remarkable discrepancies among countries regarding the preoperative screening policies and perioperative preventive measures. We can conclude that under the current screening policies, COVID-19 patients impose problems with non-negligible frequency in surgical practice that may trigger hospital outbreaks, particularly in severely affected countries/institutions.
Since the early phase of COVID-19 pandemic, preventive measures and screening policies worldwide focused on symptomatic patients, mainly based on previous experience with the influenza virus and Corona Virus 1 Severe Acute Respiratory Syndrome (SARS-CoV-1). Our study was compatible with these findings, and confirmed wide prevalence of the initial symptom-based preoperative testing policies which may have missed the asymptomatic cases: less than 20% of local guidelines worldwide tested every surgical patient with huge variations among countries. Such limited use of preoperative testing may also be related to a worldwide shortage of testing capacity and to >1 day waiting periods for test results as reported from at least 34.5% of the centers.
Although we have no direct evidence on the benefit of universal testing for surgical patients, recent emerging evidence brought the international and local surgical guidelines to recommend preoperative testing when available and practical [25-30]. SARS-CoV-2 viral loads peak 5 days earlier than SARS-CoV-1, and is similarly detected in asymptomatic and symptomatic patients [34-36]. These traits of SARS-Cov-2 make asymptomatic patients more likely to transmit the disease than in the previous epidemics [37-39]. In hospital settings, a study from China reported a higher prevalence of asymptomatic COVID-19 infection in hospitalized patients (5.8%) compared to the community (1.2%),[40] and asymptomatic hospitalized patients were frequently reported as a source of in-hospital outbreaks [41]. In this study, local guidelines in the majority of the centers recommended testing based on symptoms or suspicious radiologic findings. Such testing policies may be challenged by the fact that over 30% of the centers worldwide experienced in-hospital COVID-19 infection, and almost 60% of those centers failed to trace it or reported originating from asymptomatic carriers. The proportion of centers with in-hospital COVID-19 infection was particularly high in severely affected countries/centers. In light of these findings, infection-control strategies focused solely on symptomatic patients may not be sufficient in surgical patients, particularly in highly affected countries/centers. A prospective universal testing program for surgical patients is warranted to clarify the prevalence of asymptomatic carriers, its potential impact on hospital outbreaks and the cost-benefit balance of the testing.
Another approach to deal with asymptomatic COVID-19 patients is the strict use of PPE and infection control measures. In this study, the universal use of dedicated PPE was proportional to the countries’ risk categories and centers’ caseloads, reaching 53.9% in the high risk countries and 71.9% in the highest caseload centers. This data implies surgeons’ high concern and awareness of asymptomatic COVID-19 patients in the highly-affected countries/centers. Unfortunately, the study also disclosed insufficient availability of the PPE across the countries, particularly Filter Face Piece2 (FFP)/FFP3 masks and eye protections. Large disparities existed in the availability of the PPE across the countries. Surgeons must consider the local testing capability as well as PPE availability to decide the best protective measures under the current risk of asymptomatic COVID-19 patients.
Policies on wearing a mask for health care workers have been debated. The WHO guidelines recommend that health care workers should wear a medical mask when entering a room where patients with suspected or confirmed COVID-19 are admitted [42]. Although 71.8% of the participants in this study reported that they always wore a mask in the hospital, the rates were not linearly correlated with countries’ risk category or centers’ caseload but varied significantly across the countries from 0% to >95%, which reflects the lack of international consensus and perhaps cultural differences on this subject. In contrast to mask policies, the use of dedicated PPE was linearly correlated with the country risk categories and centers’ caseloads. Interestingly, surgeons from UK reported the highest use of dedicated PPE in operation theatres (71.4%) but the lowest use of masks in hospital wards (21.4%) among the high risk countries. Further, our data showed that resource shortage was almost comparable in high caseload centers or high risk countries compared to the others. These findings suggest the use of PPE was dependent not only on supply but institutional or surgeons’ policies.
In this study, countries were classified into the 3 risk categories by the number of cumulative deaths in light of the epidemiological situations on April 8, 2020 as described in the Methods. Although there is no consensus about what is the best index for the countries’ pandemic status, this classification might be challenged as the number of deaths is not only dependent on the pandemic status but also on the population size and different definitions of the COVID-19-related deaths among the countries. Acknowledging these limitations, it is noteworthy that there were clear consistency between the results analyzed by the countries’ risk category and those analyzed by the centers’ COVID-19 caseload. For instance, centers with higher caseload (>100) adopted overall more preventive policies than lower caseload centers, including universal testing (in 100% of high caseload centers), routine testing of hospital staff and use of dedicated PPE in operation theatres. Similar trends were observed between these variables and the country risk category. The matching results between the two different risk categories (ie, countries’ risk category and centers’ caseloads) support the robustness of our analysis and results.
The strengths of this survey include large numbers and internationality of respondents and short period of recruitment to capture the current practice under rapid developments of COVID-19 crisis. However, this survey is subject to inherent systematic biases caused by unintended selection of centers at distribution, unequal number of centers per country and uneven geographical coverage. Only six countries (Italy, Spain, USA, China, Japan and Russia) were responsible for 62.2% of the participants, and the results may over-represent the situations in these countries. The response rate for the survey cannot be provided due to unlimited distribution through social media and academic societies, and the profiles or representativeness of the centers cannot be evaluated or compared between those did and did not respond to the survey. Voluntary participation of the survey may have resulted in recruiting respondents who have high interests in this topic and led to overestimation of the frequency and clinical impact of COVID-19 patients in surgical practice (a voluntary response bias). Acknowledging these limitations, this study tried to minimize the effect of such biases and obtain clinically meaningful results by collecting a large sample size and stratifying the data by countries’ death number and centers’ caseloads. We believe this survey does reflect current surgical practices, which highlights the emerging problems caused by COVID-19 patients.
In conclusion, this large international survey captured the global surgical practice under the COVID-19 pandemic and highlighted the insufficient preoperative screening of COVID-19 in the current surgical practice. We strongly believe that in the coming phase of pandemic, during which many medical centers will resume elective surgeries, a call for action in surgical departments is needed in global plans for infection control. More intensive screening programs will be necessary to prevent new potentially catastrophic outbreaks of infection in hospitals.
Acknowledgments
We acknowledge all health-care workers involved in the diagnosis and treatment of COVID-19 patients worldwide. We would like to thank all the collaborators of “S-COVID Collaborative Group” (listed in a separate sheet) for contribution to the study; the surgical societies (European Society of Surgical Oncology, Latin American Society of Surgical Oncology, Russian Society of Colorectal Surgeons and Società Italiana di Chirurgia Colo-Rettale) for helping us to distribute the survey; Dr Krishn Khanna for English editing; and all the surgeons who translated the original questionnaire into 13 languages and shared the project in their countries: A. Frontali, J. Carvas, L. Sanchez-Guillen, C. Blajut, M. Sbaih, E.Karbovnichaya, E. Samadov, N. Buchs, M. Ninkovic, T. Araki, G. Gallo, A. Sturiale.
Disclaimers: The views expressed in the submitted article are the authors’ own and not an official position of the institution or funder.
Footnotes
Funding: This research was funded in part by the European Society of Degenerative Disease.
The study was registered with an analysis plan on ClinicalTrials.gov (NCT04344197).
Authorship contributions: Study conception and design: VB, TK, GP, YA, BS, GS. Acquisition of data: VB, TK, YA, BS, LS, BP, MF, MC. Analysis and interpretation of data: VB, TK, YA, AP, KK, SE. Drafting of manuscript: VB, TK, YA. Critical revision: GP, AP, BS, LS, KK, BP, MF, MC, SE, GS. Final approval: All the authors.
Competing interests: The authors completed the ICMJE Unified Competing Interest form (available upon request from the corresponding author), and declare no conflicts of interest.
Contributor Information
on behalf of S-COVID Collaborative Group:
A Kefleyesus, AGM Hoofwijk, Abdullah Sami Eldaly, Abel Gonzalez, Adraoui Jawad, Ahmad Jooma, Ahmed Mousa Hafez, Ainhoa Valle Rubio, Aitor Landaluce-Olavarria, Aiwen Wu, Akihisa Nagatsu, Akira Inoue, Akira Kanamoto, Akira Ouchi, Alaa El-Hussuna, Alba Vazquez-Melero, Albert M Wolthuis, Alberto M Peral, Alejandra Cruz Lozano, Aleksandr Efremov, Aleksandr V Ryasantsev, Alessandra Di Giorgio, Alessandro Parente, Alessandro Tamburrini, Alessio Alò, Alexander Forero-Torres, Alexander L Vahrmeijer, Alexander Varabei, Siles Hinojosa, Ali Zeynel Abidin Balkan, Alice Frontali, Alikin Oleg, Álvaro Soler-Silva, Amin Makni, Ana André, Ana María García Cabrera, Ana María Gonzalez Fernández, Ana M Minaya-Bravo, Ana Rodríguez-Sánchez, Ana-Maria Musina, Anang Pangeni, Anastasia Zolotko, Andranik Tonoyan, Andrea Balla, Andrea Belli, Andrea Cavallaro, Andrea Chierici, Andrea Divizia, Andrea Fares Bucci, Andrea Jiménez Salido, Andrea Morini, Andrea Muratore, Andrea Vignali, Andrei Chitul, Diaconescu Andrei Sebastian, Andrejs Pcolkins, Andrey Shchegolev, Andrew Hollenbeck, Andrew Wisneski, Angelo Iossa, Anna D’Amore, Anndrew Hunter, Anthony J Hesketh, Andrea La Brocca, Antonino Spinelli, Antonio Caires, Antonio D’Alessandro, Antonio Francisco Sanchís López Correo, Antonio Macrì, Antonio Navarro-Sánchez, Apollo Pronk, Aram Akunc, Arash Mehri, Arie Pelta, Aristeidis Papadopoulos, Aristotelis Kechagias, Arshad Rashid, Artur Ramazanov, Ashfaq Chandio, Atsushi Kohyama, Atsushi Nishimura, Atsushi Ohkawa, Audrius Dulskas, Aun Jamal, Aurora Mariani, Ayse Gizem Unal, Ayse Karagoz, Bahar Busra Ozkan, Barham Salih, Baris Gülcü, Beatrice Pessia, Beatriz Martin-Perez, Benedetto Ielpo, Berenice Tulelli, Bin Yang, Boumadani Mhamed, Brenda Murphy, Bs Langenhoff, Bulent Belevi, Burak Güney, Caecilia Ng, Camilo Rueda, Campbell S Roxburgh, Carlo V Feo, Carlo Ferrari, Carlo Gazia, Carlo Pratesi, Carlo Ratto, Carlos Cerdán Santacruz, Carlos Rodolfo Martinez Arroyave, Carlos Macias, Carlota Garcia Fernandez, Carmen Cagigas Fernandez, Carolina Curtis-Martinez, Caroline Fortmann, Caroline Kim, Catalina Uribe Galeano, Catarina Barroso, Caterina Baldi, Caterina Foppa, Cesare Formisano, Changzai Li, Chao Ding, Chenyu Wang, Chiara Iacusso, Chongwei Yang, Christian Pizzera, Christoph Skias, Christos Chouliras, Christos Liakos, Chu Matsuda, Chun-yi Wu, Cihangir Ozaslan, Cinzia Tanda, Cipolat Mis Tommaso, Claire Dagorno, Claudia Patricia Arellano Ramos, Claudio Arcudi, Claudio Coco, Cleotilde Mateo Morales, Mujahid Zulfiqar Ali, Constança Teresa Miranda De Azevedo, Coral Cózar Lozano, Corrado Sala, Cosimo Alex Leo, Cosimo Riccardo Scarpa, Cristian Varela Ferro, Cristina Mosquera Fernandez, D Morales-Garcia, Daisuke Nakano, Daniel Cristian, Daniel Hechtl, Daniel Triguero Cánovas, Daniela Calabrese, Daniela Rega, Daniele Ferraro, Daniele Morezzi, Daniele Sommacale, Danielle Brogden, Danilo Miskovic, David Merlini, Davide Pertile, Denise Coniglio, Dexiang Zhu, Dianwen Wu, Diego Coletta, Diego Ramos Rubio, Diego Sasia, Dmitry Fillipov, Domenico Russiello, Dragomir Dardanov, ECJ Consten, Edgaras Smolskas, Edoardo Maria Muttillo, Edward Jones, Eiji Sunami, El-Helou Etienne, Elena Chalkiadaki, Elena Giacomelli, Elena Karbovnichaya, Elena Ruiz-Úcar, Eleonora Guaitoli, Elgun Samadov, Elio Jovine, Elio Treppiedi, Elisa Maria Vaterlini, Elisa Zambaiti, Elisabetta Moggia, Elmi Coetzee, Emanuele Chisari, Emanuele D’Errico, Emilia Ciofic, Emilio Peña, Emine Kurt, Emre Balık, Emre Gunay, Emre Sivrikoz, Enrico Andolfi, Enrico Araimo, Enrico Lucci, Enrico Opocher, Enrico Pinotti, Enrico Rubino, Enver Reyhan, Erica Mazzotta, Ernesto Barzola Navarro, Etienne El-Helou, Eugenio Licardie-Bolaños, Eva Iglesias Porto, Evelyn Contreras, Evert-Jan Boerma, Fabio Cianchi, Fabio Marino, Fabio Uggeri, Fanghai Han, Federica Calculli, Federica Falaschi, Federico Ghignone, Federico Perrone, Felice Borghi, Felipe García, Ferdinando Agresta, Ferdinando Carlo Maria Cananzi, Fernando Mendoza-Moreno, Fevzi Cengiz, Filipe Macedo Almeida, Filippo Baracchi, Filippo Carannante, Filippo La Torre, Flavio Fernandes, Florian Friedmacher, Florin Grama, Francesca Carissimi, Francesca Pecchini, Francesco Bianco, Francesco Colombo, Francesco Ferrara, Francesco Litta, Francesco Maria Carrano, Francesco Martignoni, Francesco Menegon Tasselli, Francesco Milone, Francesco Pata, Francesco Sammartino, Francesco Zambianchi, Francisco Barragan, Francisco Herrero, Francisco Schlottmann, Frank C Den Boer, Frank Pfeffer, Fumihiko Fujita, G Navarra, Gabriel Herrera-Almario, Gabriele Pozzo, Gabriella Teresa Capolupo, Gabrielle H Van Ramshorst, Gadiel Liscia, Gaetano Gallo, Ganesh Asawa, Gaoxiang Wang, Gaurang Raiyani, Geerard Beets, Gemma Sugrañes Naval, Genfeng Jin, George J Chang, George Saakian, Gerardo Kahane, Giacomo Borroni, Giacomo Lo Secco, Gian Luca Baiocchi, Gianluca Baronio, Gianluca Pagano, Gianmaria Casoni Pattacini, Giorgio Lisi, Giovanni Milito, Giovanni Sinibaldi, Giuditta Serrao, Giulia Bagaglini, Giuliano Sarro, Giuseppe Brisinda, Giuseppe Candilio, Giuseppe Mangiameli, Giuseppe Giuliani, Gonzalo Pablo Martin-Martin, Gordon Bodzin, Graat Leon, Graham Mackay, Granila Vasil, Graziano Palmisano, Grella Maria Giovanna, Guadalupe Campos Fernández, Guillermo Berrones Steingel, Guoyun Zhang, Gyu Seog Choi, Haipeng Chen, Hajime Hirose, Hajime Kayano, Hanife Seyda Ulgur, Harmony Impellizzeri, Hasani Ariola, Heli Liu, Heriberto Medina, Hideaki Miyauchi, Hidekazu Takahashi, Hideki Hayashi, Hideki Ishikawa, Hideyuki Ishida, Hilbert De Vries, Hilmican Ulman, Hirofumi Kon, Hirofumi Ota, Hiroki Akamatsu, Hiroshi Tamagawa, Hirotaka Shoji, Hiroyuki Egi, Hisahiro Matsubara, Hisanori Miki, Hossam Elfeki, Hung-Hsin Lin, Iacopo Giani, Iban Caravaca-García, Ichiro Takemasa, Imerio Angriman, Ionut Negoi, Irina Volkova, Iris Russo, Irmgard E Kronberger, Iskander Shageev, Ishak Aydin, Ismael Mora-Guzmán, Ivana Novak, Izzo Giuliano, Jacob Rachmuth, James Chi-Yong Ngu, James Glasbey, Jan Stoot, Jan Žatecký, Jarno Melenhorst, Van Der Wal JBC, Jeroen Leijtens, Jessica Bogach, Jessie Elliott, De Wilt JHW, Jiagang Han, Jian Cui, Jiaqi Liu, Jim Khan, Jimmy Panji Wirawan, Jinji Zhang, Joel Davis Osorio Manyari, Johannes Doerner, Jonathan Bock, Joop Konsten, Jorge Mario Castro, Jorge Pérez Grobas, José Pereira Pinto, Jovan Juloski, Juan Luis Blas Laina, Juan José Solórzano, Juan Ramón Gómez López, Jun Li, Jun Watanabe, Jung-Myun Kwak, Junichi Hasegawa, Junichiro Hiro, K Sergey, Kai Zhang, Kaoru Nagahori, Karla Martinez, Katsuji Tokuhara, Katsuki Danno, Kay Uehara, Kazuhiko Yoshimatsu, Kazuhisa Ehara, Kazuki Ueda, Kazuyoshi Suda, Kazuyuki Yamamoto, Kei Ishimaru, Kei Kimura, Keiji Hirata, Kemal Deen, Ken Imaizumi, Jenji Yamada, Kenta Tanakura, Khaled Rida, Kiichi Sugimoto, Kitani Kotaro, Kiwisure Shi, Koji Okabayashi, Koya Hida, Kozo Kataoka, Kumiko Hongo, Kunkun Xia, Larissa Tseng, Lars Reime, Laura Lorenzon, Laura Muiños Ruano, Lei Zhou, Lindsey De Nes, Lorena Brandariz, Lorenzo Morini, Lorenzo Petagna, Lorenzo Ripamonti, Lourdes Hernandez Martinez, Luca Pio, Luca Sacco, Lucia Carvalho, Luigi Zorcolo, Luis Eduardo Pérez-Sánchez, Luis Humberto Reyes Esparza, Luis Tallon Aguilar, Madeleine Garner, Maki Sugimoto, Makoto Nagashima, Manabu Shiozawa, Manfredelli Simone, Manuel Ferrer-Marquez, Marcia Carvalho, Marco Alifano, Marco Arganini, Marco Calussi, Marco Catarci, Marco Ettore Allaix, Marco Forlin, Marco Milone, Marco Paci, Margot Fodor, Maria Antipova, Maria Beltran Martos, Maria Carmela Giuffrida, María Diez Tabernilla, María José Alcaide Quirós, Maria Lemma, Maria Luisa Reyes Diaz Correo, Maria Małowiecka, Maria Paola Bellomo, Maria Ramos Fernandez, María Socias, Mariam Rizk, Mariani Aurora, Mariano Alvarez Antolinez, Marijana Ninkovic, Mario Giuffrida, Marjolein MN Leeuwenburgh, Marnix AJ De Roos, Marta Cañón Lara, Marta Climent Agustin, Marta Cuadrado, Marta Pascual, Martina Lemmerer, R Carlos, Masa Okamoto, Masaaki Miyo, Masafumi Inomata, Masakazu Ikenaga, Masaki Tsujie, Masamichi Yasuno, Masanori Kotake, Masanori Sato, Masayoshi Yasui, Matteo Lavazza, Matteo Rottoli, Matteo Zuin, Mauricio Zuluaga, Maurizio Cervellera, Maurizio Cesari, Maurizio Zizzo, Mauro Garino, Mauro Ghirardi, Mauro Montuori, Mauro Podda, Mauro Santarelli, Mehmet Ali Koc, Melissa Baini, Michael De Cillia, Michele De Rosa, Michele Manigrasso, Michele Zuolo, Miguel F Cunha, Mihaela Misca, Mihail Slavchev, Mikhail Danilov, Mikhail Shigaev, Milou Martens, Minako Kobayashi, Mingyang Ren, Mitsuru Ishizuka, Mohammed Mustafa Hassan, Mohamad Siblini, Mohamed Sahloul, Mohammad Reza Keramati, Monish Karunakaran, Moritz Markel, Mudassar Majeed, Muhammad Umar Younis, Muhammed Ikbal Akin, Munazza Laraibe, Murat Derebey, Murat Kendirci, Mutsumi Fukunaga, Nagahide Matsubara, Narce Eunice Cruz Ordaz, Narimantas Evaldas Samalavicius, Nattawut Keeratibharat, Nicola de Angelis, Nicolae Gica, Nicoló Maria Mariani, Nicolò Ramino, Nicolò Falco, Neil Smart, Niels De Korte, Niels FM Kok, Nigel B Jamieson, Nikolay Aberyasev, Nikolay Bruklich, Nobuki Ichikawa, Norikatsu Miyoshi, Norma De Palma, Nuno Figueiredo, Nuria Ortega Torrecilla, Oleg G Dybov, Oleg Yudin, Ollende Crepin, Oscar Gomez, Ozlem Zeliha Sert, Pablo Lozano Lominchar, Pablo Menéndez, Paola De Nardi, Patricia Tejedor, Patrick Jordan, Patrick Tan, Patrizia Marsanic, Pechnikova Natalya, Pedro Parra Baños, Pere Rebasa, Peter M Neary, Pieter Tanis, Piero Giustacchini, Pietro Anoldo, Pilar Concejo, Pin Cao, Pramodh Chandrasinghe, Prasad Abeyratne, Quan Wang, RJ Klicks, R Mukai, Rafael Ferrer Riquelme, Raffaele De Luca, Raffaele Galli, Raffaele Gianesini, Rajesh Gianchandani Moorjani, Rajkiran K Deshpande, Ramon Gorter, Raquel Leon Ledesma, Rategov Ruslan, Raunaq Chhabra, Reena Talreja-Pelaez, Rei Suzuki, Riccardo Balestri, Riccardo Rosati, Rim Kiblawi, Rita Martins, Roberta Angelico, Roberta Tutino, Roberto Persiani, Roberto Pollastri, Rocío González López, Rodrigo Oliva Perez, Roel Hompes, Roman Lukanin, Sera R Roser Termes, Rossella Brunaccino, Ryota Nakanishi, Samuel Stefan, Sandra Paola Sánchez Hernández, Sara Di Carlo, Sara Ingallinella, Satoru Domoto, Satoshi Ikeda, Saulius Mikalauskas, Seon Hahn Kim, Serena Mantova, Severius Barbuta, Shaotang Li, Shigeki Yamaguchi, Shigeru Yamagishi, Shigenori Homma, Shingo Tsujinaka, Shinichi Yoshioka, Shinichiro Mori, Shirish Tewari, Shlomi Rayman, Sho Horiuchi, Shuichiro Matoba, Shunji Morita, Sibel Yaman, Silvia Vigna, Silvio Testa, Simon Ng, Simona Deidda, Simone Cicconi, Simone Di Maria, Simone Sibio, Siyar Ersoz, Sofija Pejkova, Soliman Altarifi, Songbing He, Songphol Malakorn, Sosef Meindert, Sosuke Sumikawa, Stavan Parmar, Stefan Uranitsch, Stefano D’ugo, Stefano Giuliani, Stéphanie Breukink, Suk-Hwan Lee, Taishi Hata, Takahisa Ishikawa, Takashi Akiyoshi, Takashi Azuma, Takaya Kobatake, Takayuki Fukuzaki, Takeshi Aiyama, Takeshi Yamada, Tatiana Garmanova, Tatiana Gómez-Sánchez, Tatsuro Yamaguchi, Teresa De Jesús Flores, Teruyuki Usub, Tetsuhiro Tsuruma, Tetsuichiro Shimizu, Tihomir Georgiev Hristov, Ting Van Loon, Tohru Funakoshi, Tommaso Maria Manzia, Tomomichi Kiyomatsu, Tomonari Katayama, Tomonori Akagi, Tsunekazu Mizushima, Uemura Kazuhito, Ugo Elmore, Ugo Grossi, Vadim A Truchalev, Valentina Sosa Rodríguez, Valentina Testa, Valeria Tonini, Valerio Celentano, Valery M Nekoval, Vanessa Bettencourt, Vasif Mammadov, Verónica Alejandra Galue Leyva, Veronica Georgina Ortega Mariscal, Victor Edmond Seid, Victor Klemann, Víctor Turrado-Rodriguez, Vincenzo Papagni, Vincenzo Vento, Vincent Frering, Vincenzo Vigorita, Vitaliva V Petrove, Vladimir Lyadov, Wei Fu, Wei Mi, Woon Kyung Jeong, Wouter KG Leclercq, Xavier De Sousa, Xing Zhao, Xinxiang Li, Xinxin Wang, Xuanhua Yang, Xuelei Zhang, Ya'nan Zhen, Yan Dong, Yana Erushevich, Yasumasa Takii, Yasuo Sumi, Yeray Trujillo Loli, Yosef Lishtzinsky Yifat, Yoshifumi Shimada, Yoshihiro Nabeya, Yoshihito Ide, Yuan Wu, Yuichiro Tsukada, Yuji Miyamoto, Yuji Toiyama, Yujiro Fujie, Yuka Kaneko, Yukako Mokutani, Yuki Fujii, Yukihide Kanemitsu, Yulia Medkova, Yulong Chen, Yurema Gonzalez Ruiz, Yusuke Kinugasa, Zacaria Sow, Zeeshan Razzaq, Zejun Wang, Zheng Liu, Zhenguo Han, Zhihui Tai, Zhiyong Lai, Zi Qin Ng, and Zilvinas Dambrauskas
REFERENCES
- 1.World Health Organization. WHO Director-General's opening remarks at the media briefing on COVID-19—11 March 2020. Available: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. Accessed: 11 March, 2020.
- 2.Johns Hopkins CSSE. Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). ArcGIS. Available: https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed: 20 April 2020.
- 3.Nacoti M, Ciocca A, Giupponi A, Brambillasca P, Lussana F, Pisano M, et al. At the Epicenter of the Covid-19 Pandemic and Humanitarian Crises in Italy: Changing Perspectives on Preparation and Mitigation. NEJM Catalyst. 2020. [Google Scholar]
- 4.Pellino G, Spinelli A.How COVID-19 Outbreak Is Impacting Colorectal Cancer Patients in Italy: A Long Shadow Beyond Infection. Dis Colon Rectum. 2020;63:720-2. 10.1097/DCR.0000000000001685 [DOI] [PubMed] [Google Scholar]
- 5.Sica GS, Campanelli M, Bellato V, Monteleone G.Gastrointestinal cancer surgery and enhanced recovery after surgery (ERAS) during COVID-19 outbreak. Langenbecks Arch Surg. 2020;405:357. 10.1007/s00423-020-01885-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang C, Wang Y, Li X, Qu J, Gong F, Han Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen N, Zhou M, Dong X, Liu W, Wang M, Ma JP, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-13. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, et al. Clinical Characteristics of COVID-19 Patients With Digestive Symptoms in Hubei, China: A Descriptive, Cross-Sectional, Multicenter Study. Am J Gastroenterol. 2020;115:766-73. . 10.14309/ajg.0000000000000620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Redd WD, Zhou JC, Hathorn KE, McCarty TR, Bazarbashi AN, Thompson CC, et al. Prevalence and Characteristics of Gastrointestinal Symptoms in Patients with SARS-CoV-2 Infection in the United States: A Multicenter Cohort Study. Gastroenterology. 2020;S0016-5085:30564-3. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheung KS, Hung IF, Chan PP, Lung CK, Tso E, Liu R, et al. Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples from the Hong Kong Cohort and Systematic Review and Meta-analysis. Gastroenterology. 2020;159:81-95. 10.1053/j.gastro.2020.03.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514-23. 10.1016/S0140-6736(20)30154-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Danis K, Epaulard O, Bénet T, Gaymard A, Campoy S, Bothelo-Nevers E, et al. Cluster of coronavirus disease 2019 (Covid-19) in the French Alps, 2020. Clin Infect Dis. 2020;71:825-32. 10.1093/cid/ciaa424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lai CC, Liu YH, Wang CY, Wang YH, Hsueh SC, Yen MY, et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths. J Microbiol Immunol Infect. 2020;53:404-12. 10.1016/j.jmii.2020.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye F, Xu S, Rong Z, Xu R, Liu X, Deng P, et al. Delivery of infection from asymptomatic carriers of COVID-19 in a familial cluster. Int J Infect Dis. 2020;94:133-8. 10.1016/j.ijid.2020.03.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-9. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chu H, Chan JF, Wang Y, Yuen TT, Chai Y, Hou Y, et al. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV and implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. Lancet Microbe. 2020;1:e14-e23. 10.1016/S2666-5247(20)30004-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chu H, Chan JF, Wang Y, Yuen TT, Chai Y, Hou Y, et al. Comparative replication and immune activation profiles of SARS-CoV-2 and SARS-CoV in human lungs: an ex vivo study with implications for the pathogenesis of COVID-19. Clin Infect Dis. 2020;ciaa410. Online ahead of print. 10.1093/cid/ciaa410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aminian A, Safari S, Abdolali RJ, Ghorbani M, Delaney CP.COVID-19 Outbreak and Surgical Practice [Publish Ahead of Print 2020 March 26]. Ann Surg. 2020;272:e27-e29. 10.1097/SLA.0000000000003925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samsami M, Zebarjadi Bagherpour J, Nematihonar B, Tahmasbi H.COVID-19 Pneumonia in Asymptomatic Trauma Patients; Report of 8 Cases. Arch Acad Emerg Med. 2020;8:e46. [PMC free article] [PubMed] [Google Scholar]
- 20.Aminian A, Kermansaravi M, Azizi S, Alibeigi P, Safamanesh S, Mousavimaleki A, et al. Bariatric Surgical Practice During the Initial Phase of COVID-19 Outbreak. Obes Surg. 2020;30:3624-7. 10.1007/s11695-020-04617-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. Eclinical Medicine. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amodeo G, Bugada D, Franchi D, Moschetti G, Grimaldi S, Panerai A, et al. Immune function after major surgical interventions: the effect of postoperative pain treatment. J Pain Res. 2018;11:1297-305. 10.2147/JPR.S158230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roth JA, Golub SH, Grimm EA, Eilber FR, Morton DL.Effects of operation on immune response in cancer patients: sequential evaluation of in vitro lymphocyte function. Surgery. 1976;79:46-51. [PubMed] [Google Scholar]
- 24.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335-7. 10.1016/S1470-2045(20)30096-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Società Italiana di Chirurgia. COVID-19 Acoi guidelines. Available: https://www.sicitalia.org/wp-content/uploads/2020/04/20200330_Covid-19-Acoi_Sic.pdf. Accessed: 20 April 2020.
- 26.Spanish Society of Surgery. General recommendations of urgent surgical care in the context of the COVID-19 pandemic (SARS COV-2). Available: https://www.aecirujanos.es/files/noticias/158/documentos/4_-_Recomendaciones_for_URGENT_Surgical_care_during_the_pandemic_COVID_19__v_2.pdf. Accessed: 20 April 2020.
- 27.American College of Surgeon. Local resuption of elective surgery guidance. Available: https://www.facs.org/covid-19. Accessed: 7April 2020.
- 28.Intercollegiate of British Surgery Societies. Update of intercollegiate general surgery guidance on COVID-19. Available: https://www.asgbi.org.uk/userfiles/file/covid19/2nd-update-intercollegiate-general-surgery-guidance-on-covid-19-5-april.pdf. Accessed: 20 April 2020.
- 29.Society of American Gastrointestinal and Endoscopic Surgeons. Recommendation for surgical response during COVID-19. Available: https://www.sages.org/recommendations-surgical-response-covid-19/. Accessed: 20 April 2020.
- 30.European Society of Onclogic Surgery. Statement on COVID-19. Available: https://www.essoweb.org/news/esso-statement-covid-19/. Accessed: 20 April 2020.
- 31.Bellato V, Konishi T, Pellino G, An Y, Piciocchi A, Sensi B, et al. Impact of Asymptomatic COVID-19 Patients in Global Surgical Practice during the COVID-19 Pandemic. Br J Surg. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eysenbach G.Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES). J Med Internet Res. 2004;6:e34. 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available: https://covid19.who.int. Accessed: 8 April 2020.
- 34.To KK, Tsang OT-Y, Leung W-S, Tam AR, Wu TC, Lung DC, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20:565-74. 10.1016/S1473-3099(20)30196-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Muller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465-9. 10.1038/s41586-020-2196-x [DOI] [PubMed] [Google Scholar]
- 36.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 Viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177-9. 10.1056/NEJMc2001737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cheng PK, Wong DA, Tong LK, Ip SM, Lo AC, Lau CS, et al. Viral shedding patterns of coronavirus in patients with probable severe acute respiratory syndrome. Lancet. 2004;363:1699-700. 10.1016/S0140-6736(04)16255-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ip DKM, Lau LLH, Leung NHL, Fang VJ, Chan KH, Chu DK, et al. Viral shedding and transmission potential of asymptomatic and paucisymptomatic influenza virus infections in the community. Clin Infect Dis. 2017;64:736-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gandhi M, Yokoe DS, Havlir DV.Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19. N Engl J Med. 2020;382:2158-60. 10.1056/NEJMe2009758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.He G, Sun W, Fang P, Huang J, Gamber M, Cai J, et al. The clinical feature of silent infections of novel coronavirus infection (COVID-19) in Wenzhou. J Med Virol. 2020. Online ahead of print. 10.1002/jmv.25861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pang KH, Osman NI.Asymptomatic COVID-19 infection in a patient evaluated for ureteric colic: Radiological findings and impact on management. Urology. 2020;141:183-4. 10.1016/j.urology.2020.04.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.World Health Organization. Advice on the use of masks in the community during home care and in the healthcare settings in the context of the novel coronavirus outbreak. Available: https://www.who.int/publications-detail/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak. Accessed: 20 April 2020.